Abstract
An impairment in pragmatic communication is a core feature of schizophrenia, often associated with difficulties in social interactions. The pragmatic deficits regard various pragmatic phenomena, e.g., direct and indirect communicative acts, deceit, irony, and include not only the use of language but also other expressive means such as non-verbal/extralinguistic modalities, e.g., gestures and body movements, and paralinguistic cues, e.g., prosody and tone of voice. The present paper focuses on the identification of those pragmatic features, i.e., communicative phenomena and expressive modalities, that more reliably discriminate between individuals with schizophrenia and healthy controls. We performed a multimodal assessment of communicative-pragmatic ability, and applied a machine learning approach, specifically a Decision Tree model, with the aim of identifying the pragmatic features that best separate the data into the two groups, i.e., individuals with schizophrenia and healthy controls, and represent their configuration. The results indicated good overall performance of the Decision Tree model, with mean Accuracy of 82%, Sensitivity of 76%, and Precision of 91%. Linguistic irony emerged as the most relevant pragmatic phenomenon in distinguishing between the two groups, followed by violation of the Gricean maxims, and then extralinguistic deceitful and sincere communicative acts. The results are discussed in light of the pragmatic theoretical literature, and their clinical relevance in terms of content and design of both assessment and rehabilitative training.
Subject terms: Schizophrenia, Biomarkers, Human behaviour
Introduction
Pragmatics is classically defined as the ability to use language to convey a specific communicative meaning in a given context1–3. More recently, this definition has also included the use of other expressive means such as non-verbal/extralinguistic modalities, e.g., gestures and body movements, and paralinguistic cues, e.g., prosody and tone of voice4. Schizophrenia is associated with a specific language impairment5–7. Patients’ difficulties refer to different levels of language processing, ranging from phonological aspects to word and semantic production8–10. The term schizophasia was coined to include some of these difficulties, including clanging, neologism, and unintelligible utterances11–13. However, several studies have also pointed out that communicative difficulties may persist even when the syntactic and semantic abilities of patients with schizophrenia are preserved14–16.
In the current literature, a well-established notion is that patients with schizophrenia show pervasive difficulties in terms of communicative-pragmatic ability17–22. Pragmatic ability relies on inferential processes in order to fill the gap that often exists between the literal meaning of an utterance and what the speaker actually intends to communicate as, for example, in the statement “What a nice person!” referring to an individual acting very impolitely. A large number of studies have pointed out that patients with schizophrenia specifically have more difficulty than healthy controls with the comprehension of non-literal language23. Non-literal language refers to those communicative acts that imply a gap between the literal and the intended meaning: this is the case of indirect speech acts24, as well as figurative expressions like irony25–28, metaphors, idioms, and proverbs29–33. Furthermore, patients with schizophrenia may also encounter communicative difficulties when having to deal with other pragmatic phenomena, such as recognizing and repairing communicative failures34, as well as understanding deceit35. Moreover, patients with schizophrenia may often display difficulties in detecting violations of the Gricean maxims of communication28,36. Gricean maxims, i.e., quantity (violated by providing extra and redundant details), quality (violated when a speaker says something that is obviously false), relation (violated when the information that is provided is not related to the context of the communicative interaction) and manner (violated when the speaker uses expressions that are rude and inappropriate), represent those communicative rules to which communicative partners adhere, in order to make their communicative contributions effective and ensure a meaningful exchange of information37. Other difficulties have been reported in tasks assessing narrative ability38 and conversational skills39,40.
Non-verbal/extralinguistic expressive behavior, though less investigated than linguistic ability, is also impaired in schizophrenia, and represents a characterizing element of the disease41. Such difficulties range from perception, comprehension, and production of communicative gestures42–44 to facial expression recognition (for a review see refs. 45–47).
Moreover, patients with schizophrenia display atypical prosodic patterns, in terms of flat intonation, increased pauses, distinctive tone, and abnormal voice quality48,49. Previous studies indicated slower speech50, more pronounced pauses51,52, and reduced prosodic variability53,54. A recent meta-analysis55 confirmed that voice atypicalities, especially those related to duration and pitch variability measures, represent a characteristic feature of schizophrenia. Further, the ability to recognize linguistic and emotional prosodic cues has also been reported to be impaired in schizophrenia56–58, as shown, for example, by a difficulty in decoding sarcasm based upon voice tone59.
Despite this evidence, few previous studies have attempted to provide a multimodal assessment of communicative-pragmatic ability in schizophrenia, evaluating different communicative phenomena expressed through different expressive modalities within the same experimental sample. Among these, Meilijson and colleagues60 tested verbal, non-verbal, and paralinguistic aspects of conversation to evaluate communicative performance across different clinical populations. The authors pointed out that participants with schizophrenia performed less well than controls in all the expressive modalities. Linscott40 investigated communicative-pragmatic performance in patients with schizophrenia by assessing linguistic conversational ability and non-verbal aspects, i.e., those expressive behaviors used to facilitate the listener’s engagement. The authors reported that patients with schizophrenia demonstrated a higher level of pragmatic impairment as compared to healthy controls. More recently, Pawelczyk and colleagues61 tested different aspects of pragmatic ability in individuals with schizophrenia, i.e., inferential meaning (implicit understanding), lexical-semantic processing, written metaphors, picture-metaphors, humor, discourse analysis, emotional and linguistic prosody. The results showed that, as compared to controls, patients experienced difficulties in almost all the tasks investigated, namely, in the comprehension of implicit information and humor, in processing lexical-semantic information, in emotional and linguistic prosody, and in the discourse test. However, individuals with schizophrenia and controls performed equally well in understanding written and depicted metaphors. This last finding, though, is in contrast with the results of Deamer and colleagues62, who found that, in a picture metaphor comprehension task, when the experimental material is presented as a picture, and the answer does not require the use of language (i.e., choosing the correct answer from among different images), patients with schizophrenia perform less well than healthy controls. Colle and colleagues20 assessed the ability of individuals with schizophrenia to comprehend and produce different types of pragmatic phenomena, such as sincere, direct, and indirect communicative acts, deceit and irony, and, at the same time, investigated the linguistic and extralinguistic expressive modalities. The results of the study indicated that participants with schizophrenia performed significantly worse than healthy controls in all the tasks investigated, involving the use of both the linguistic and extralinguistic modalities. Considered as a whole, the above-mentioned studies provide a clear picture of communicative-pragmatic deficits in patients with schizophrenia; further, this evidence clearly suggests that such difficulties concern not only the linguistic modality, but other expressive modalities as well, such as the non-verbal/extralinguistic and paralinguistic modalities.
Meta-analytic evidence has demonstrated the presence of large differences between patients with schizophrenia and healthy controls in the various communicative-pragmatic domains. Parola and colleagues63 found a large difference between patients and controls in the comprehension of indirect speech acts (Cohen’s d = −0.70, p = 0.09), deceit (d = −0.92, p < 0.001), irony (d = −1.22, p < 0.001) and violations of Gricean maxims (d = −1.33, p < 0.001). As far as the recognition of emotional and linguistic prosodic cues is concerned, different meta-analyses have shown large differences for emotional prosody (Hoekert et al.56: d =−1.24, CI = − 1.55 to −0.93; Lin et al.64: d = −0.95, CI = −0.80 to −1.11). As for vocal expression, previous meta-analytic evidence21,56 has pointed out large differences in the qualitative rating of emotional prosody (d = −1.11, CI = − 1.78 to −0.43), and less robust differences for quantitative acoustic measures (g = −0.55 for pitch variability, g between −0.75 and −1.89 for proportion of spoken time, speech rate, and pauses). However, most of the previous studies used pragmatic tasks for assessing linguistic and prosodic ability, while the gestural modality received less attention and thus no meta-analytic evidence exists for gesture recognition and gesture production. As a whole, this evidence confirms that the impairment in the different communicative-pragmatic domains in schizophrenia is severe and widespread, with large differences between patients and controls in the various pragmatic domains.
Although previous literature clearly indicated that communicative disorder is a core deficit in schizophrenia, it remains unclear which communicative features, i.e., which pragmatic phenomena expressed via different expressive modalities, are the most informative for discriminating between patients with schizophrenia and healthy controls. In part, this reflects the complexity of communicative-pragmatic ability. Indeed, pragmatic deficits can vary as a function of the different tasks used to assess the ability and the specific pragmatic phenomena evaluated. Moreover, deficits can affect different expressive modalities, and it is thus important to provide a multimodal assessment of communicative-pragmatic ability. However, no previous studies have provided a comprehensive assessment of communicative-pragmatic ability with the primary aim of identifying the specific communicative phenomena and expressive modalities able to best discriminate between patients with schizophrenia and healthy controls. The identification of the communicative-pragmatic phenomena and the communicative expressive modalities in which patients experience greater difficulty could be a valuable aid for clinicians throughout the diagnostic procedure, helping them to identify the disease during the early stages of evaluation and improving the effectiveness of rehabilitative treatment specifically focused on these features65,66.
The aim of the present research is to identify the pragmatic features—communicative phenomena expressed through different communicative modalities, i.e., linguistic, extralinguistic, and paralinguistic—that are the most informative for discriminating between patients with schizophrenia and healthy controls. For this purpose, we assessed the abilities of patients with schizophrenia and healthy controls in a wide range of communicative-pragmatic phenomena, i.e., basic speech acts (statements, questions, commands, and orders67), sincere (direct and indirect), ironic and deceitful communicative acts, violation of the Gricean maxims, prosodic mismatch, social appropriateness, conversational ability (turn-taking and adherence to the topic). Compared to our previous studies18,21, this research analyzes a wider range of pragmatic phenomena, as well as additional expressive means, i.e., paralinguistic modalities. Furthermore, the present study focuses on a new research question, i.e., the identification of the communicative phenomena and expressive modalities that more reliably discriminate between patients with schizophrenia and healthy controls, and to this aim it applies a different methodology, i.e., a Machine Learning (ML) approach, and specifically Decision Tree (DT) analysis. DT analysis can be used to find the pragmatic features that best separate the data into the two groups, i.e., individuals with schizophrenia and healthy controls. This ML technique has several advantages compared to regression models as, unlike linear regression methods, it can handle nonlinear interactions between multiple predictors. Further, it provides an intuitive and intelligible representation (tree diagram) of which variables combined with which configuration can better predict the outcome, i.e., belonging to the schizophrenia vs. healthy controls groups. In this way, we aim to move a step further also with respect to our previous work21, by providing a more detailed picture of the communicative profile of patients with schizophrenia, and exploring which communicative phenomena, expressed using multiple communication modalities, best discriminate between patients with schizophrenia and healthy controls.
On the basis of the previous meta-analytic evidence, we hypothesize that the most informative communicative-pragmatic phenomena for distinguishing between patients with schizophrenia and controls are irony, Gricean maxims, and recognition of prosodic cues. However, no meta-analytic evidence is available for the comprehension and production of communicative acts expressed using the gestural modality, and no predictions can be made for these phenomena. Further, no previous studies have directly compared a wide range of communicative-pragmatic phenomena expressed using different communicative modalities. Thus, this study also has an explorative aim and intends to provide an initial basis for the identification of the multimodal communicative-pragmatic features which best discriminate between patients with schizophrenia and healthy controls.
Results
Assessment of pragmatic abilities in schizophrenia using a DT model
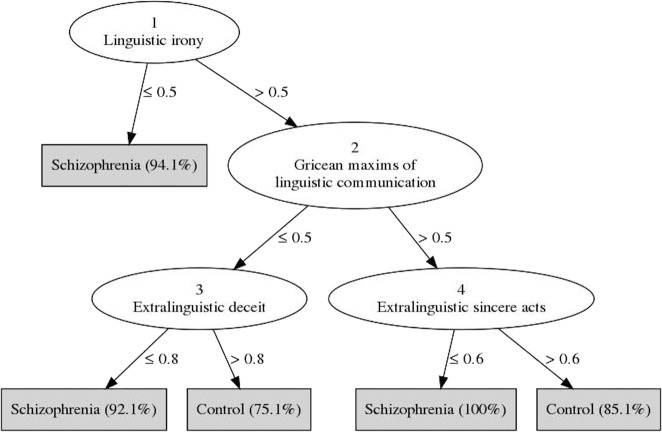
Figure 1 shows the DT model generated. The leaf nodes (gray squares) represent the classes (schizophrenia or healthy controls), and the number in parentheses indicates the expected likelihood of new cases being classified as patients with schizophrenia or healthy controls after going through the previous decision nodes, i.e., after performing a conditional test on a specific feature (for example, new cases are classified as schizophrenia if their score on Linguistic irony is below 0.5 as indicated by the value in the branch between the two nodes). The main factors able to discriminate between the two classes (schizophrenia and healthy controls) in the generated tree are linguistic irony, Gricean maxims of linguistic communication, extralinguistic deceit, and extralinguistic sincere (direct and indirect) communicative acts. The strongest predictor for classifying patients with schizophrenia vs. healthy controls is linguistic irony (node 1): if the score on linguistic irony is below 0.5, a new case is classified as schizophrenia (with probability = 94.1%). The next decision point is Gricean maxims of linguistic communication (node 2) which, depending on whether its value is below 0.5 or above 0.5, leads to the evaluation of extralinguistic deceit (node 3) or extralinguistic sincere (direct and indirect) communicative acts (node 4), respectively. If extralinguistic deceit is below 0.8, the individual is classified as a patient with schizophrenia (probability = 92.1%), otherwise as a healthy control (probability = 75.1%). Similarly, if the score for extralinguistic sincere (direct and indirect) communicative acts is below 0.6, the individual is classified as a patient with schizophrenia (probability = 100%), otherwise as a healthy control (probability = 85.1%). Overall model Accuracy was 0.821 (SD = 0.118), Sensitivity was 0.758 (SD = 0.285), Precision was 0.910 (SD = 0.151), Specificity was 0.900 (SD = 0.175), and the area under the ROC curve (AUC) was 0.894 (SD = 0.143).
Fig. 1. DT model.
A decision tree is used to classify an example by starting at the root of the tree (testing the value of Linguistic irony) and moving through it (testing the other features) until a leaf node (gray squares), which provides the classification of the instance (schizophrenia or healthy controls).
Discussion
In the present paper, we provided a comprehensive multimodal assessment of communicative-pragmatic ability in patients with schizophrenia in order to investigate the communicative phenomena and expressive modalities most informative for discriminating between patients with schizophrenia and healthy controls. To this aim, we applied a DT analysis to identify the pragmatic features that best distinguish between the two groups.
First, we found that the overall performance of the DT model was good. Accuracy was 82%, indicating that the model was able to reliably distinguish between the two populations. Sensitivity was 76%, with 24 patients with schizophrenia classified correctly, and Precision was 91%, showing a low number (4) of false-positive errors.
The results showed that linguistic irony emerged as the most important pragmatic phenomenon for determining the class of a new case, i.e., the classification of an individual as a patient with schizophrenia or healthy control. Irony is one of the most investigated phenomena in the pragmatic literature, and a wide body of research has reported that irony comprehension is severely impaired in patients with schizophrenia18,25,27,68,69. A recent meta-analysis63 showed a large and robust difference in irony recognition between patients with schizophrenia and healthy controls (d = −1.22, p < 0.0001), thus suggesting a high level of impairment in irony comprehension in schizophrenia.
Understanding irony is a high-level linguistic task and requires the interplay of different cognitive functions. Previously, several studies found an association between irony comprehension and different cognitive functions, such as the theory of mind (ToM)42, i.e., the ability to infer the speaker’s mental states70, executive functions (EF)71–73, and level of intelligence23,40,74. More recently, some authors proposed that the additional cognitive effort required for irony comprehension, compared to other communicative expressions, may be due to the complexity of the inferential ability necessary to identify the ironic communicative intention (see refs. 18,75–77). Recent neuroimaging studies confirmed that comprehension of irony, with respect to literal statements, engages an extended bilateral brain network including several fronto-temporal and fronto-parietal areas, which underlies the cognitive effort related to the use of different cognitive functions such as ToM, executive controls, and inferential processes (e.g.,78–81). Irrespective of the specific cognitive substrates at the origin of patients’ deficits in irony recognition, previous studies clearly showed how irony comprehension is a high-level task that recruits an extended cerebral network corresponding to the interplay of different cognitive functions78,81. In line with this literature, the results of the present study confirm that, of the pragmatic features evaluated, the linguistic irony was the most complex for patients with schizophrenia to understand, and the most informative for distinguishing between patients and controls.
The second most important factor in classifying patients with schizophrenia or healthy controls in the DT model was the recognition of violation of the Gricean maxims of linguistic communication. Gricean maxims refer to the norms which regulate the discourse between two or more individuals, and serve as rules for rational and effective communication, by ensuring that the information provided by the interlocutors is as informative as necessary (maxim of quantity), the contribution is true (maxim of quality), relevant (maxim of relation), and clear (maxim of manner). More in detail, in the present investigation the items composing our experimental task assessed participants’ ability to recognize the interlocutor’s non-intentional violation of one of the Gricean maxims by providing a confused, or not precise, or not relevant or prolix contribution to the communicative interaction.
The difficulties encountered by patients with schizophrenia in appreciating Gricean maxims of communication are well known, with several studies reporting a pronounced impairment in the ability to attune to and recognize the maxims10,20,23,35,36,69,82, and a recent meta-analysis63 showing a large difference between patients with schizophrenia and healthy controls in tasks assessing the detection of violation of Gricean maxims (d = −1.33, p < 0.001). Frith and Corcoran35 evaluated the comprehension of Gricean maxims in individuals with schizophrenia, and found that patients exhibiting negative symptoms, such as anhedonia, reduced social drive, and loss of motivation, committed more errors than controls with all the maxims except the maxim of relation. Binz and Brune82 investigated the ability of patients with schizophrenia to adhere to the Gricean maxims of relation and quantity, and found significant differences between patients and healthy controls in these two maxims, with patients using more words than necessary and reporting irrelevant or unnecessary details. Mazza and colleagues69 found significant differences between patients with schizophrenia and healthy controls in recognizing non-intentional violations of all four maxims in conversational exchanges and reported that these differences correlated with ToM impairment. Further, some authors have proposed that non-intentional violations of the Gricean maxims of communication are associated with relevant clinical features of the disorder. For example, Abu-Akel83 claimed that positive symptoms, among which formal thought disorder, may be associated with incoherence, illogicality, and the tendency to provide irrelevant and unnecessary information, i.e., tangentiality. The results of the present study confirm that the difficulties in adhering to the social norms of communication, which result in frequent disruptions of communication in conversational exchange as reported by clinicians and relatives, are a key feature in schizophrenia. In addition, our results indicated that the first two tasks able to discriminate between patients with schizophrenia and controls, i.e., irony and violation of Gricean maxims, are both expressed through linguistic means. This datum is in line with a wide body of literature showing specific language impairment in patients with schizophrenia (e.g.,11,25,40). The remaining relevant tasks identified by the DT model in classifying patients with schizophrenia or healthy controls were the comprehension and production of sincere communicative acts (direct and indirect speech acts) and deceit expressed through the extralinguistic, i.e., gestural, modality. As regards the role played by sincere communicative acts in our results, the tasks used in the present investigation are composed of items investigating direct and indirect sincere communicative acts. Indirect acts are those by which the speaker communicates more than what s/he is actually literally saying to the listener84, as in the example “This soup is insipid” (example of unconventional indirect act) proffered in order to obtain the salt from the interlocutor. Several studies in the literature reported that patients with schizophrenia have difficulty with the comprehension of indirect speech acts85,86 and proposed that such difficulty is principally explained by a patient’s deficit in Theory of Mind42, i.e., the ability to conceptualize another person’s mental states70. A similar explanation holds for deceitful tasks, that are often used to investigate ToM difficulties in patients with schizophrenia35,87–89.
Moreover, empirical research in schizophrenia has traditionally focused on assessing language impairments, considered a hallmark of the disease ever since the first definitions of the disorder. However, it is only more recently that some studies have begun to report the presence of deficits affecting the extralinguistic, i.e., non-verbal modality. These studies found patients with schizophrenia to be impaired in non-verbal communication, especially in the production of communicative and social gestures43,44,90, and showed that these deficits cannot merely be accounted for by patients’ motor disorders90. Moreover, deficits have also been reported in the perception and recognition of communicative gestures, as well as in the recognition of facial expressions (for a review see refs. 45,47,91). Finally, deficits affecting non-verbal modalities have been found to be associated with functional outcome92. The present results are in line with theserecent evidence and point to the importance of focusing the assessment of pragmatic ability in schizophrenia not only on the linguistic modality, but also on the extralinguistic communicative modality.
Finally, we should also acknowledge the limitations of the present work. First of all, this is an exploratory analysis. ML methods benefit from larger sample size and different samples to perform out-of-sample validation, while the sample included in the present study is relatively small (n = 67). Further, schizophrenia is a heterogeneous disorder, and clinical samples can vary widely with respect to patients’ clinical features. Thus, the present results need to be replicated in future studies with larger samples and across different clinical profiles. Second, the pragmatic ability can be measured in different ways, and previous studies in the literature have used different batteries and tasks (e.g.,17,39,40,86). These tasks can vary widely with respect to the cognitive and inferential load. For this reason, the communicative features we found to be the most informative for classifying patients and controls need to be confirmed in future studies across different pragmatic tasks and contexts.
To conclude, pragmatic ability includes a wide range of different skills, all of which contributing to successful communication. While previous studies reported a wide array of communicative impairments in schizophrenia, it is hard to identify which of the skills affected are the most informative for distinguishing between schizophrenia and healthy controls. However, the identification of these features may be relevant as a valuable aid for clinicians throughout the diagnostic process, improving the effectiveness of rehabilitative treatment, and targeting future research. Further, recent studies reported that pragmatic and language impairments represent a risk factor for developing psychosis5,93–95, and thus the identification of the most distinctive pragmatic features is crucial for targeting early effective intervention to enhance these skills and which may diminish the risk. Indeed, some authors recently proposed pragmatic impairment as a marker for schizophrenia21,61,96,97. In this perspective, it will be fundamental to identify which pragmatic behaviors can most reliably be associated with schizophrenia. In this work, we moved a step in this direction, showing how, in our sample, some communicative features and expressive means, i.e., linguistic irony processing, adherence to and recognition of Gricean maxims of linguistic communication, and comprehension and production of extralinguistic sincere and deceitful communicative acts, were the most informative features for distinguishing between patients and controls. A deeper understanding of the relevance of these deficits in patients with schizophrenia will also be useful in order to promote the creation and implementation of rehabilitation programs specifically designed (see for example65,66) to help patients overcome such difficulties.
Methods
Participants
Thirty-two individuals with schizophrenia (seven females; age: M = 40.17; years; SD = 10.19; education: M = 10.59; SD = 2.45) and 35 healthy controls (six females; age: M = 39.46; SD = 10.95; education: M = 10.57; SD = 2.46) took part in the research. Patients and controls were matched for gender, education, and age (see Table 1). All patients with schizophrenia met the Diagnostic and Statistical Manual of Mental Disorders98 criteria for schizophrenia diagnosis. Inclusion criteria for patients were: (1) not in an acute stage: all patients were in the chronic stage of the illness and clinically stable (2) Italian native speaker (3) achievement of a cut-off score in the following neuropsychological tests in order to exclude the presence of severe cognitive or linguistic deficits: (a) Mini-Mental State Examination (MMSE99). Cut-off 24/30; (b) Token Test100. Cut-off 5/6; (c) Denomination scale of the Aachener Aphasie test (AAT101). Cut-off: no deficit. (4) must have provided their informed consent.
Table 1.
Clinical details of patients with schizophrenia (N = 32).
| ID Patients with schizophrenia | ||||||||||||||||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | 31 | 32 | |
| Sex | M | F | F | M | M | M | M | M | F | M | M | M | M | M | M | M | M | M | M | F | M | M | M | M | M | F | M | M | F | M | M | F |
| Age | 56 | 48 | 44 | 23 | 35 | 53 | 30 | 40 | 38 | 53 | 30 | 31 | 24 | 43 | 26 | 35 | 45 | 22 | 27 | 49 | 50 | 47 | 43 | 57 | 47 | 24 | 47 | 25 | 56 | 30 | 47 | 46 |
| Education (Yrs) | 8 | 13 | 13 | 13 | 8 | 11 | 8 | 13 | 8 | 13 | 13 | 13 | 10 | 13 | 13 | 8 | 14 | 13 | 8 | 13 | 10 | 8 | 13 | 8 | 8 | 13 | 8 | 8 | 8 | 8 | 8 | 8 |
| Treatment | ||||||||||||||||||||||||||||||||
| Typical neuroleptics | • | • | • | • | • | • | • | |||||||||||||||||||||||||
| Atypical neuroleptics | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | |||||||||
| PANSS | ||||||||||||||||||||||||||||||||
| Negative symptoms | 10 | 21 | 17 | 13 | 35 | 17 | 42 | 18 | 7 | 19 | 33 | 16 | 15 | 42 | 20 | 16 | 21 | 15 | 11 | 18 | 24 | 29 | 8 | 11 | 32 | 25 | 22 | 14 | 11 | 42 | 29 | 12 |
| Positive symptoms | 12 | 9 | 9 | 13 | 22 | 18 | 42 | 29 | 10 | 25 | 34 | 23 | 12 | 31 | 18 | 14 | 10 | 10 | 17 | 18 | 26 | 20 | 25 | 18 | 29 | 23 | 11 | 16 | 7 | 42 | 13 | 9 |
| General symptoms | 30 | 51 | 32 | 39 | 62 | 24 | 94 | 41 | 32 | 36 | 88 | 48 | 37 | 69 | 31 | 32 | 40 | 29 | 40 | 35 | 58 | 38 | 8 | 32 | 64 | 53 | 48 | 24 | 16 | 94 | 40 | 26 |
| Total score | 52 | 81 | 58 | 65 | 119 | 59 | 178 | 88 | 49 | 80 | 155 | 87 | 64 | 142 | 69 | 62 | 71 | 54 | 68 | 71 | 108 | 87 | 33 | 61 | 125 | 101 | 81 | 54 | 34 | 178 | 82 | 47 |
Exclusion criteria were: (1) current and/or prior neurological disorder, (2) anamnesis of head injury, (3) history of substance abuse, (4) impaired hearing or vision. This study was approved by the ‘A.S.L. TO3-TO4-TO5 A.O.U. San Luigi Gonzaga ethics committee, protocol number: 0008187 and all the participants provided a written informed consent to take part in the study.
Material and procedures
The participants were administered the Assessment Battery for Communication (ABaCo102), a validated tool showing good psychometric proprieties, i.e., content validity, high inter-rater agreement, and internal consistency103,104. The tool is theoretically grounded on the Cognitive Pragmatics theory4, it is available in Italian105 and has previously shown to be able to discriminate between patients with schizophrenia and controls18,20,77. The Battery includes five different scales assessing the comprehension and production of a wide range of pragmatic phenomena. The linguistic scale evaluates the comprehension and production of different communicative phenomena, i.e., basic speech acts, sincere communicative acts, deceit, irony, expressed using the linguistic modality. The extralinguistic scale assesses the same communicative acts, but expressed using the extralinguistic modality, i.e., gestures. The paralinguistic scale assesses the comprehension and production of those communicative aspects that complement the interaction, such as facial expressions, prosody, eye-gaze, etc. This scale evaluates communicative phenomena, i.e., basic communicative acts, communicative acts expressing an emotion, and paralinguistic contradiction. The context scale evaluates the adequacy of a communicative act with respect to the norms of discourse (i.e., Gricean maxims) and social norms of communication. The conversational scale assesses the ability to take part in a conversation appropriately, adhering to the topic and respecting turn-taking rules.
Taken together, the five scales of the ABaCo comprise 72 items in the form of live interviewer-interviewee interactions and 100 short clips (20–25 s each). These clips are shown to the participants using a laptop and their administration takes ~90 min. At the end of each clip, the examiner investigates the correct comprehension of the protagonist’s conclusive communicative act or else elicits the production of a communicative act in response to the protagonist’s utterance or gesture, and then asks specific open questions for each item. The specific pragmatic phenomena and skills assessed in each scale are described, with examples, in Table 2.
Table 2.
Description of the structure of the Assessment Battery for Communication.
 |
All items are scored as correct (1 point) or incorrect (0 points), based on precise coding rules that are set out in the ABaCo administration manual105. See also refs. 77,102,106,107, for a more detailed description of the administration and scoring procedures.
Data analysis
We analyzed the data using a DT108 classifier in order to identify the pragmatic phenomena most relevant for discriminating between patients with schizophrenia and healthy controls. DT is a commonly used ML method for classifying and predicting a target variable based on multiple covariates. It is a classifier with a tree structure, where each node is either: (1) A leaf node which represents the final outcome of a series of decisions and indicates the value on the target attribute (class). For example, in our case, it indicates whether a new case is classified as a patient with schizophrenia or a control (target attribute: class). (2) A decision node that represents a conditional test on a specific feature. For example, in our case, if the feature considered is Linguistic irony, the decision node represents the threshold scores on Linguistic irony for which an individual is classified as a patient with schizophrenia or healthy control. For example, if the participant’s score on Linguistic irony (feature) is below or above 0.5, that individual is respectively classified as a patient with schizophrenia or healthy control. Each branch of the subtree represents a possible outcome of the test, with subtrees representing conjunctions of features (and the tests performed on these features, i.e., decision nodes) that lead, in the end, to the class attribute, i.e., whether a case is classified as a patient with schizophrenia or healthy control. For example, if we consider the decision node of Linguistic irony (see Fig. 1), this gives origin to two branches based on the test performed on this feature: first branch: if Linguistic irony is below 0.5 a new case is classified as a patient with schizophrenia; second branch: if Linguistic irony is above 0.5, a further test is performed on a different feature (Gricean maxims of linguistic communication), which in turn gives origin to two further branches, and so on until a leaf node is reached and a case is classified as a patient with schizophrenia or healthy control.
The estimation criterion in the DT algorithm is the selection of a feature to test at each decision node in the tree. The goal of the estimation criterion is to select the feature that is most useful for classifying the cases. A good quantitative measure of the worth of a feature is a statistical property called information gain that measures how well a given feature discriminates the cases based on the class to which they are attributed. This measure is used to select the best feature from among the possible candidates at each step of the growing tree.
In the present study we used the J48 algorithm (an implementation of Quinlan’s algorithm C4.5) in the Weka workbench for ML, version 3.8.3109 to generate the DT model. We estimated the generalization performance of the DT model using 10-fold cross-validation, which is a technique for evaluating predictive models by partitioning the original sample into a training set to create the model, and a test set to evaluate it. We reported the following performance metrics: Accuracy, Sensitivity, Precision, Specificity, and the area under the ROC curve (AUC). Accuracy refers to the proportion of the total number of classifications that were correct in both classes (SCZ and HC), Sensitivity gives the proportion of cases of schizophrenia classified correctly, Precision gives the proportion of cases classified as schizophrenia that was correct, and Specificity gives the proportion of control cases classified correctly. The ROC (Receiver Operating Characteristic) curve tells us how well the model can distinguish between the two classes (schizophrenia and healthy controls). ROC is a probability curve, and AUC represents a degree or measure of separability which tells how capable the model is of distinguishing between the two classes. Metrics presented are collected across all folds and are related to the test sets.
We performed additional analysis to assess whether pragmatic phenomena were able to predict symptoms and medications in the group of patients with schizophrenia only. These analyses are reported in Supplementary Information.
Supplementary information
Role of medications and clinical features on pragmatic performance
Acknowledgements
This work was supported by the Compagnia di San Paolo under Grant Bando Ex-post Università di Torino, grant number D11G19000220007 and by FAPEG Mobility Confap-Italy (MCI-2018).
Author contributions
Study design: A.P., R.S., I.G., and F.M.B. Data curation: A.P., R.S., and I.G. Formal analysis: R.S. Investigation: I.G., A.P., and L.B. Supervision: F.M.B. Original draft and revised versions: A.P., R.S., and I.G., F.M.B. Final approval of the completed version: A.P., R.S., I.G., L.B., and F.M.B.
Data availability
Please note that the datasets generated and/or analyzed during the current study are not publicly available for ethical reasons: Due to the anonymity guaranteed in the informed consent form at the time of data collection, data cannot be publicly shared, and are controlled by the A.S.L.To2 ethics committee. Qualified researchers who wish to request access to these data may contact direzione.psicologia@unito.it (Department of Psychology, University of Turin, Italy) or the corresponding author.
Code availability
All experiments were performed on the Weka workbench for machine learning, version 3.8.3, available to download in https://www.cs.waikato.ac.nz/ml/weka/. The decision tree was the J48 classifier with the following parameters: confidence factor at 0.5 and the number of minimum instances per node (minNumObj) at 2. Details regarding the analysis are available upon request to rogeriosalvini@ufg.br
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41537-021-00153-4.
References
- 1.Cummings, L. Clinical pragmatics. (Cambridge University Press, 2009).
- 2.Levinson, S. C. Pragmatics. (Cambridge University Press, 1983).
- 3.Morris, C. Foundations of the Theory of Signs. pure.mpg.de (Chicago University Press, 1938).
- 4.Bara, B. G. Cognitive Pragmatcis. (Press, MIT, 2010).
- 5.Corcoran CM, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17:67–75. doi: 10.1002/wps.20491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pauselli L, et al. Computational linguistic analysis applied to a semantic fluency task to measure derailment and tangentiality in schizophrenia. Psychiatry Res. 2018;263:74–79. doi: 10.1016/j.psychres.2018.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Le TP, Najolia GM, Minor KS, Cohen AS. The effect of limited cognitive resources on communication disturbances in serious mental illness. Psychiatry Res. 2017;248:98–104. doi: 10.1016/j.psychres.2016.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rieber RW, Vetter H. The problem of language and thought in schizophrenia: a review. J. Psycholinguist. Res. 1994;23:149–195. doi: 10.1007/BF02143921. [DOI] [PubMed] [Google Scholar]
- 9.Stassen HH, Albers M, Tewesmeier M, Woggon B. Pergamon. Speaking behavior and voice sound characteristics associated with negative schizophrenia. J. Psichiatr Res. 1995;29:4–6. doi: 10.1016/0022-3956(95)00004-o. [DOI] [PubMed] [Google Scholar]
- 10.DeLisi LE. Speech disorder in schizophrenia: review of the literature and exploration of its relation to the uniquely human capacity for language. Schizophr. Bull. 2001;27:481–496. doi: 10.1093/oxfordjournals.schbul.a006889. [DOI] [PubMed] [Google Scholar]
- 11.Covington MA, et al. Schizophrenia and the structure of language: the linguist’s view. Schizophr. Res. 2005;77:85–98. doi: 10.1016/j.schres.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 12.Kraepelin E. Dementia Precox and Paraphrenia. (Edinburgh, UK: University of Edinburgh, 1919).
- 13.Lecours A, Vanier-Clément M. Schizophasia and jargonaphasia: a comparative description with comments on Chaika’s and Fromkin’s respective looks at “schizophrenic” language. Brain Lang. 1976;3:516–565. doi: 10.1016/0093-934X(76)90046-8. [DOI] [PubMed] [Google Scholar]
- 14.Andreasen NC, Grove WM. Thought, language, and communication in schizophrenia: diagnosis and prognosis. Schizophr. Bull. 1986;12:348–359. doi: 10.1093/schbul/12.3.348. [DOI] [PubMed] [Google Scholar]
- 15.Frith, C. D., & Allen, H. A. Language disorders in schizophrenia and their implications for neuropsychology. in Schizophrenia: The major issues (eds. Bebbington P. & McGuffin P.) p. 172–186 (Heinemann Medical Books/Heinemann Professional Publishing, 1988).
- 16.Moro A, et al. Detecting syntactic and semantic anomalies in schizophrenia. Neuropsychologia. 2015;79:147–157. doi: 10.1016/j.neuropsychologia.2015.10.030. [DOI] [PubMed] [Google Scholar]
- 17.Bambini V, et al. The communicative impairment as a core feature of schizophrenia: frequency of pragmatic deficit, cognitive substrates, and relation with quality of life. Compr. Psychiatry. 2016;71:106–120. doi: 10.1016/j.comppsych.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 18.Bosco FM, Berardinelli L, Parola A. The ability of patients with schizophrenia to comprehend and produce sincere, deceitful, and ironic communicative intentions: the role of theory of mind and executive functions. Front. Psychol. 2019;10:827. doi: 10.3389/fpsyg.2019.00827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bucca, A. “Pragmatics disorders and indirect reports in psychotic language,” in Indirect Reports and Pragmatics in the World Languages, (eds. Capone A., García-Carpintero M. & Falzone A.) 439–453 (Cham: Springer, 2018).
- 20.Colle L, et al. Understanding the communicative impairments in schizophrenia: a preliminary study. J. Commun. Disord. 2013;46:294–308. doi: 10.1016/j.jcomdis.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 21.Parola A, et al. Pragmatics, theory of mind and executive functions in schizophrenia: disentangling the puzzle using machine learning. PLoS ONE. 2020;15:e0229603. doi: 10.1371/journal.pone.0229603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parola A, Brasso C, Morese R, Rocca P, Bosco FM. Understanding communicative intentions in schizophrenia using an error analysis approach. Npj Schizophr. 2021;7:45–50. doi: 10.1038/s41537-021-00142-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Varga E, et al. Compensatory effect of general cognitive skills on non-literal language processing in schizophrenia: a preliminary study. J. Neurolinguist. 2014;29:1–16. doi: 10.1016/j.jneuroling.2014.01.001. [DOI] [Google Scholar]
- 24.Corcoran R. Inductive reasoning and the understanding of intention in schizophrenia. Cogn. Neuropsychiatry. 2003;8:223–235. doi: 10.1080/13546800244000319. [DOI] [PubMed] [Google Scholar]
- 25.Gavilán JM, García-Albea JE. Theory of mind and language comprehension in schizophrenia: poor mindreading affects figurative language comprehension beyond intelligence deficits. J. Neurolinguist. 2011;24:54–69. doi: 10.1016/j.jneuroling.2010.07.006. [DOI] [Google Scholar]
- 26.Herold R, Tényi T, Lénárd K, Trixler M. Theory of mind deficit in people with schizophrenia during remission. Psychol. Med. 2002;32:1125–1129. doi: 10.1017/S0033291702005433. [DOI] [PubMed] [Google Scholar]
- 27.Langdon R, Coltheart M, Ward PB, Catts SV. Disturbed communication in schizophrenia: the role of poor pragmatics and poor mind-reading. Psychol. Med. 2002;32:1273–1284. doi: 10.1017/S0033291702006396. [DOI] [PubMed] [Google Scholar]
- 28.Mazza M, Di Michele V, Pollice R, Casacchia M, Roncone R. Pragmatic language and theory of mind deficits in people with schizophrenia and their relatives. Psychopathology. 2008;41:254–263. doi: 10.1159/000128324. [DOI] [PubMed] [Google Scholar]
- 29.Schettino A, et al. The comprehension of idiomatic expressions in schizophrenic patients. Neuropsychologia. 2010;48:1032–1040. doi: 10.1016/j.neuropsychologia.2009.11.030. [DOI] [PubMed] [Google Scholar]
- 30.Pesciarelli F, et al. Is the comprehension of idiomatic sentences indeed impaired in paranoid Schizophrenia? A window into semantic processing deficits. Front. Hum. Neurosci. 2014;8:799. doi: 10.3389/fnhum.2014.00799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saban-Bezalel R, Mashal N. Comprehension and hemispheric processing of irony in schizophrenia. Front. Psychol. 2017;8:943. doi: 10.3389/fpsyg.2017.00943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haas, M. H. et al. Evidence of pragmatic impairments in speech and proverb interpretation in schizophrenia. J. Psycholinguist. Res. 10.1007/s10936-014-9298-2 (2014). [DOI] [PubMed]
- 33.Bambini V, et al. A leopard cannot change its spots: a novel pragmatic account of concretism in schizophrenia. Neuropsychologia. 2020;139:107332. doi: 10.1016/j.neuropsychologia.2020.107332. [DOI] [PubMed] [Google Scholar]
- 34.Bosco FM, Bono A, Bara BG. Recognition and repair of communicative failures: the interaction between theory of mind and cognitive complexity in schizophrenic patients. J. Commun. Disord. 2012;45:181–197. doi: 10.1016/j.jcomdis.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 35.Frith CD, Corcoran R. Exploring ‘theory of mind’ in people with schizophrenia. Psychol. Med. 1996;26:521. doi: 10.1017/S0033291700035601. [DOI] [PubMed] [Google Scholar]
- 36.Tényi T, Herold R, Szili IM, Trixler M. Schizophrenics show a failure in the decoding of violations of conversational implicatures. Psychopathology. 2002;35:25–27. doi: 10.1159/000056212. [DOI] [PubMed] [Google Scholar]
- 37.Grice, H. in Syntax and Semantics, 3: Speech Acts (ed. P. Cole, J. M.) (Academic Press, 1975).
- 38.Marini, A. et al. The language of schizophrenia: an analysis of micro and macrolinguistic abilities and their neuropsychological correlates. Schizophr. Res. 105, 144–155 (2008). [DOI] [PubMed]
- 39.Bazin N, Sarfati Y, Lefrère F, Passerieux C, Hardy-Baylé M-C. Scale for the evaluation of communication disorders in patients with schizophrenia: a validation study. Schizophr. Res. 2005;77:75–84. doi: 10.1016/j.schres.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 40.Linscott RJ. Thought disorder, pragmatic language impairment, and generalized cognitive decline in schizophrenia. Schizophr. Res. 2005;75:225–232. doi: 10.1016/j.schres.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 41.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). (2013). [DOI] [PubMed]
- 42.Frith, CD. Theory of mind in schizophrenia. in The Neuropsychology of Schizophrenia, (eds. David, A. & Cutting, J.) pp. 147–161 (Hillsdale, N.J.: Erlbaum,1994).
- 43.Nagels A, Kircher T, Grosvald M, Steines M, Straube B. Evidence for gesture-speech mismatch detection impairments in schizophrenia. Psychiatry Res. 2019;273:15–21. doi: 10.1016/j.psychres.2018.12.107. [DOI] [PubMed] [Google Scholar]
- 44.Troisi A, Spalletta G, Pasini A. Non-verbal behaviour deficits in schizophrenia: an ethological study of drug-free patients. Acta Psychiatr. Scand. 1998;97:109–115. doi: 10.1111/j.1600-0447.1998.tb09971.x. [DOI] [PubMed] [Google Scholar]
- 45.Del-Monte J, et al. Nonverbal expressive behaviour in schizophrenia and social phobia. Psychiatry Res. 2013;210:29–35. doi: 10.1016/j.psychres.2013.05.034. [DOI] [PubMed] [Google Scholar]
- 46.Edwards, J., Jackson, H. J. & Pattison, P. E. Erratum to “Emotion recognition via facial expression and affective prosody in schizophrenia: A methodological review” [Clinical Psychology Review 22 (2002) 789–832]. Clin. Psychol. Rev. 22, 1267–1285 (2002). [DOI] [PubMed]
- 47.Kupper Z, Ramseyer F, Hoffmann H, Kalbermatten S, Tschacher W. Video-based quantification of body movement during social interaction indicates the severity of negative symptoms in patients with schizophrenia. Schizophr. Res. 2010;121:90–100. doi: 10.1016/j.schres.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 48.Stein J. Brief reports. J. Nerv. Ment. Dis. 1993;181:59–62. doi: 10.1097/00005053-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 49.Stassen HH, et al. Speaking behavior and voice sound characteristics associated with negative schizophrenia. J. Psychiatr. Res. 1995;29:277–296. doi: 10.1016/0022-3956(95)00004-O. [DOI] [PubMed] [Google Scholar]
- 50.Tavano A, et al. Specific linguistic and pragmatic deficits in Italian patients with schizophrenia. Schizophr. Res. 2008;102:53–62. doi: 10.1016/j.schres.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 51.Rapcan V, et al. Acoustic and temporal analysis of speech: a potential biomarker for schizophrenia. Med. Eng. Phys. 2010;32:1074–1079. doi: 10.1016/j.medengphy.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 52.Cannizzaro MS, Cohen H, Rappard F, Snyder PJ. Bradyphrenia and bradykinesia both contribute to altered speech in schizophrenia. Cogn. Behav. Neurol. 2005;18:206–210. doi: 10.1097/01.wnn.0000185278.21352.e5. [DOI] [PubMed] [Google Scholar]
- 53.Compton MT, et al. The aprosody of schizophrenia: computationally derived acoustic phonetic underpinnings of monotone speech. Schizophr. Res. 2018;197:392–399. doi: 10.1016/j.schres.2018.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Martínez-Sánchez F, et al. Can the acoustic analysis of expressive prosody discriminate schizophrenia? Span. J. Psychol. 2015;18:E86. doi: 10.1017/sjp.2015.85. [DOI] [PubMed] [Google Scholar]
- 55.Parola A, Simonsen A, Bliksted V, Fusaroli R. Voice patterns in schizophrenia: a systematic review and Bayesian meta-analysis. Schizophrenia Res. 2020;216:24–40. doi: 10.1016/j.schres.2019.11.031. [DOI] [PubMed] [Google Scholar]
- 56.Hoekert M, Kahn RS, Pijnenborg M, Aleman A. Impaired recognition and expression of emotional prosody in schizophrenia: Review and meta-analysis. Schizophrenia Res. 2007;96:135–145. doi: 10.1016/j.schres.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 57.Pinheiro AP, et al. Abnormalities in the processing of emotional prosody from single words in schizophrenia. Schizophr. Res. 2014;152:235–241. doi: 10.1016/j.schres.2013.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pinheiro AP, et al. Emotional self-other voice processing in schizophrenia and its relationship with hallucinations: ERP evidence. Psychophysiology. 2017;54:1252–1265. doi: 10.1111/psyp.12880. [DOI] [PubMed] [Google Scholar]
- 59.Leitman DI, Ziwich R, Pasternak R, Javitt DC. Theory of Mind (ToM) and counterfactuality deficits in schizophrenia: Misperception or misinterpretation? Psychol. Med. 2006;36:1075–1083. doi: 10.1017/S0033291706007653. [DOI] [PubMed] [Google Scholar]
- 60.Meilijson SR, Kasher A, Elizur A. Language performance in chronic schizophrenia: a pragmatic approach. J. Speech, Lang. Hear. Res. 2004;47:695–713. doi: 10.1044/1092-4388(2004/053). [DOI] [PubMed] [Google Scholar]
- 61.Pawełczyk A, Kotlicka-Antczak M, Łojek E, Ruszpel A, Pawełczyk T. Schizophrenia patients have higher-order language and extralinguistic impairments. Schizophr. Res. 2018;192:274–280. doi: 10.1016/j.schres.2017.04.030. [DOI] [PubMed] [Google Scholar]
- 62.Deamer F, et al. Non-literal understanding and psychosis: metaphor comprehension in individuals with a diagnosis of schizophrenia. Schizophr. Res. Cogn. 2019;18:100159. doi: 10.1016/j.scog.2019.100159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Parola A, Aimonetto R, Bosco FMFM. Pragmatic comprehension in schizophrenia: a systematic review and meta-analysis. Schizophr. Bull. 2020;46:S78–S79. doi: 10.1093/schbul/sbaa031.182. [DOI] [Google Scholar]
- 64.Lin Y, Ding H, Zhang Y. Emotional prosody processing in schizophrenic patients: a selective review and meta-analysis. J. Clin. Med. 2018;7:363. doi: 10.3390/jcm7100363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bosco FM, Gabbatore I, Gastaldo L, Sacco K. Communicative-pragmatic treatment in schizophrenia: a pilot study. Front. Psychol. 2016;7:166. doi: 10.3389/fpsyg.2016.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gabbatore, I. et al. Cognitive pragmatic rehabilitation program in schizophrenia: a single case fMRI study. Neural Plast. 2017, 1–9 (2017). [DOI] [PMC free article] [PubMed]
- 67.Kasher, A. in The Chomskyan Turn (ed. Kasher, A.) 122–149 (Blackwell, 1991).
- 68.Champagne-Lavau M, Charest A. Theory of mind and context processing in schizophrenia: the role of social knowledge. Front. Psychiatry. 2015;6:3. doi: 10.3389/fpsyt.2015.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mazza M, Di Michele V, Pollice R, Roncone R, Casacchia M. Pragmatic language and theory of mind deficits in people with schizophrenia and their relatives. Psychopathology. 2008;41:254–263. doi: 10.1159/000128324. [DOI] [PubMed] [Google Scholar]
- 70.Premack D, Woodruff G. Does the chimpanzee have a theory of mind? Behav. Brain Sci. 1978;34:1401–1407. [Google Scholar]
- 71.Sponheim SR, Surerus-Johnson C, Leskela J, Dieperink ME. Proverb interpretation in schizophrenia: the significance of symptomatology and cognitive processes. Schizophr. Res. 2003;65:117–123. doi: 10.1016/S0920-9964(02)00525-X. [DOI] [PubMed] [Google Scholar]
- 72.Thoma P, et al. Proverb comprehension impairments in schizophrenia are related to executive dysfunction. Psychiatry Res. 2009;170:132–139. doi: 10.1016/j.psychres.2009.01.026. [DOI] [PubMed] [Google Scholar]
- 73.Li X, et al. Pragmatic ability deficit in schizophrenia and associated theory of mind and executive function. Front. Psychol. 2017;8:2164. doi: 10.3389/fpsyg.2017.02164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mossaheb N, et al. Comprehension of metaphors in patients with schizophrenia-spectrum disorders. Compr. Psychiatry. 2014;55:928–937. doi: 10.1016/j.comppsych.2013.12.021. [DOI] [PubMed] [Google Scholar]
- 75.Bosco FM, Bucciarelli M. Simple and complex deceits and ironies. J. Pragmat. 2008;40:583–607. doi: 10.1016/j.pragma.2007.05.004. [DOI] [Google Scholar]
- 76.Bosco FM, Gabbatore I. Sincere, deceitful, and ironic communicative acts and the role of the theory of mind in childhood. Front. Psychol. 2017;08:21. doi: 10.3389/fpsyg.2017.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Parola A, Berardinelli L, Bosco FM. Cognitive abilities and theory of mind in explaining communicative-pragmatic disorders in patients with schizophrenia. Psychiatry Res. 2018;260:144–151. doi: 10.1016/j.psychres.2017.11.051. [DOI] [PubMed] [Google Scholar]
- 78.Bosco FM, Parola A, Valentini MC, Morese R. Neural correlates underlying the comprehension of deceitful and ironic communicative intentions. Cortex. 2017;94:73–86. doi: 10.1016/j.cortex.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 79.Herold CJ, et al. Neurological soft signs and psychopathology in chronic schizophrenia: a cross-sectional study in three age groups. Front. Psychiatry. 2018;9:98. doi: 10.3389/fpsyt.2018.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rapp AM, Steinhäuser AE. Functional MRI of sentence-level language comprehension in schizophrenia: a coordinate-based analysis. Schizophr. Res. 2013;150:107–113. doi: 10.1016/j.schres.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 81.Filik R, Ţurcan A, Ralph-Nearman C, Pitiot A. What is the difference between irony and sarcasm? An fMRI study. Cortex. 2019;115:112–122. doi: 10.1016/j.cortex.2019.01.025. [DOI] [PubMed] [Google Scholar]
- 82.Binz B, Brune M. Pragmatic language abilities, mentalising skills and executive functioning in schizophrenia spectrum disorders. Clin. Neuropsychiatry. 2010;7:91–100. [Google Scholar]
- 83.Abu-Akel A. Impaired theory of mind in schizophrenia. Pragmat. Cogn. 1999;7:247–282. doi: 10.1075/pc.7.2.02abu. [DOI] [Google Scholar]
- 84.Searle, J. in Syntax and Semantics. Volume 3: Speech Acts (eds Cole, P & Morgan, J. L.) 59–82 (Academic Press, 1975).
- 85.Corcoran R, Mercer G, Frith CD. Schizophrenia, symptomatology and social inference: investigating ‘theory of mind’ in people with schizophrenia. Schizophr. Res. 1995;17:5–13. doi: 10.1016/0920-9964(95)00024-G. [DOI] [PubMed] [Google Scholar]
- 86.Champagne-Lavau M, Stip E. Pragmatic and executive dysfunction in schizophrenia. J. Neurolinguist. 2010;23:285–296. doi: 10.1016/j.jneuroling.2009.08.009. [DOI] [Google Scholar]
- 87.Shryane NM, et al. Deception and false belief in paranoia: modelling theory of mind stories. Cogn. Neuropsychiatry. 2008;13:8–32. doi: 10.1080/13546800701748805. [DOI] [PubMed] [Google Scholar]
- 88.Moore R, et al. Misunderstanding the intentions of others? An exploratory study of the cognitive etiology of persecutory delusions in very late-onset schizophrenia-like psychosis. Am. J. Geriatr. Psychiatry. 2006;14:410–418. doi: 10.1097/01.JGP.0000200604.47367.38. [DOI] [PubMed] [Google Scholar]
- 89.Langdon R, Siegert RJ, Mcclure J, Harrington L. Schizophrenia, theory of mind, and persecutory delusions. Cogn. Neuropsychiatry. 2005;10:87–104. doi: 10.1080/13546800344000327. [DOI] [PubMed] [Google Scholar]
- 90.Walther S, et al. Social communication and gesture control in schizophrenia. Schizophr. Bull. 2015;41:338–345. doi: 10.1093/schbul/sbu222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Edwards J, Jackson HJ, Pattison PE. Emotion recognition via facial expression and affective prosody in schizophrenia: a methodological review. Clin. Psychol. Rev. 2002;22:789–832. doi: 10.1016/S0272-7358(02)00130-7. [DOI] [PubMed] [Google Scholar]
- 92.Stegmayer K, et al. Gesture performance in first- and multiple-episode patients with schizophrenia spectrum disorders. Neuropsychobiology. 2016;73:201–208. doi: 10.1159/000446116. [DOI] [PubMed] [Google Scholar]
- 93.Sullivan K, Winner E, Hopfield N. How children tell a lie from a joke: the role of second-order mental state attributions. Br. J. Dev. Psychol. 1995;13:191–204. doi: 10.1111/j.2044-835X.1995.tb00673.x. [DOI] [Google Scholar]
- 94.Bedi, G. et al. Automated analysis of free speech predicts psychosis onset in high-risk youths. npj Schizophr. 1, 15030 (2015). [DOI] [PMC free article] [PubMed]
- 95.Sullivan SA, et al. A longitudinal investigation of childhood communication ability and adolescent psychotic experiences in a community sample. Schizophr. Res. 2016;173:54–61. doi: 10.1016/j.schres.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bambini V, et al. Communication and pragmatic breakdowns in amyotrophic lateral sclerosis patients. Brain Lang. 2016;153:1–12. doi: 10.1016/j.bandl.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 97.Pawełczyk A, Łojek E, Żurner N, Gawłowska-Sawosz M, Pawełczyk T. Higher-order language dysfunctions as a possible neurolinguistic endophenotype for schizophrenia: evidence from patients and their unaffected first degree relatives. Psychiatry Res. 2018;267:63–72. doi: 10.1016/j.psychres.2018.05.070. [DOI] [PubMed] [Google Scholar]
- 98.American Psychiatric Association. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders | JAMA | JAMA Network. (American Psychiatric Press Inc, 1994).
- 99.Folstein MF, Folstein SE, McHugh PR. Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 100.De Renzi E, Vignolo LA. The token test: a sensitive test to detect receptive disturbances in aphasics. Brain. 1962;85:665–678. doi: 10.1093/brain/85.4.665. [DOI] [PubMed] [Google Scholar]
- 101.Huber W, Poeck K, Willmes K. The Aachen Aphasia Test. Adv. Neurol. 1983;42:291–303. [PubMed] [Google Scholar]
- 102.Angeleri R, Bosco FM, Gabbatore I, Bara BG, Sacco K. Assessment battery for communication (ABaCo): normative data. Behav. Res. Methods. 2012;44:845–861. doi: 10.3758/s13428-011-0174-9. [DOI] [PubMed] [Google Scholar]
- 103.Sacco, K. et al. Assessment battery for communication—ABaCo: a new instrument for the evaluation of pragmatic abilities. J. Cogn. Sci.9, 111–157 (2008).
- 104.Bosco FM, Angeleri R, Zuffranieri M, Bara BG, Sacco K. Assessment battery for communication: development of two equivalent forms. J. Commun. Disord. 2012;45:290–303. doi: 10.1016/j.jcomdis.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 105.Angeleri, R., Bara, B. G., Bosco, F. M., Colle, L. & Sacco, K. Batteria Per L’Assessment Della Comunicazione (ABaCO). (Giunti OS Organizzazioni Speciali, 2015).
- 106.Angeleri, R., Gabbatore, I., Bosco, F. M., Sacco, K. & Colle, L. Pragmatic abilities in children and adolescents with autism spectrum disorder: a study with the ABaCo battery. Minerva Psichiatr. 57, 93–103 (2016).
- 107.Parola A, et al. Assessment of pragmatic impairment in right hemisphere damage. J. Neurolinguist. 2016;39:10–25. doi: 10.1016/j.jneuroling.2015.12.003. [DOI] [Google Scholar]
- 108.Ross Quinlan, B. J., Kaufmann Publishers, M.& Salzberg, S. L. Programs for Machine Learning. 16, (1994).
- 109.Frank, E., Hall, M. A. & Witten, I. H. The WEKA workbench. Online Appendix for ‘Data Mining: Practical Machine Learning Tools and Techniques’. Online Appendix for ‘Data Mining: Practical Machine Learning Tools and Techniques’ (2016).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Role of medications and clinical features on pragmatic performance
Data Availability Statement
Please note that the datasets generated and/or analyzed during the current study are not publicly available for ethical reasons: Due to the anonymity guaranteed in the informed consent form at the time of data collection, data cannot be publicly shared, and are controlled by the A.S.L.To2 ethics committee. Qualified researchers who wish to request access to these data may contact direzione.psicologia@unito.it (Department of Psychology, University of Turin, Italy) or the corresponding author.
All experiments were performed on the Weka workbench for machine learning, version 3.8.3, available to download in https://www.cs.waikato.ac.nz/ml/weka/. The decision tree was the J48 classifier with the following parameters: confidence factor at 0.5 and the number of minimum instances per node (minNumObj) at 2. Details regarding the analysis are available upon request to rogeriosalvini@ufg.br