Abstract
Early childhood caries (ECC) recurrence occurs in approximately 40% of treated cases within one year. The association of Streptococcus mutans and Candida albicans with the onset of ECC is well known. Also, S. mutans strains harboring collagen-binding proteins (Cbps) avidly bind to collagen-rich dentin and are linked to increased caries risk. Here, we investigated the presence of Cbp+ S. mutans and C. albicans in saliva and dental plaque of children with varying caries statuses, and their salivary microbiome. In this cross-sectional study, 143 children who were caries-free (n = 73), treated for ECC with no signs of recurrence after 6 months (n = 45), or treated for ECC and experiencing recurrence within 6 months following treatment (n = 25) were enrolled. Co-infection with C. albicans and S. mutans, especially Cbp+ S. mutans, was strongly associated with caries recurrence. Subjects of the recurrence group infected with Cbp+ S. mutans showed a greater burden of Candida spp. and of Mutans streptococci in dentin than those infected with Cbp- strains. Salivary microbiome analysis revealed that Streptococcus parasanguinis was overrepresented in the caries recurrence group. Our findings indicate that Cbp+ S. mutans and C. albicans are intimately associated with caries recurrence, contributing to the establishment of recalcitrant biofilms.
Subject terms: Oral diseases, Microbiology, Diseases
Introduction
Early childhood caries (ECC) is a prevalent chronic disease characterized by the presence of one or more decayed (noncavitated or cavitated lesions), missing (due to caries), or filled tooth surfaces in any primary tooth (dmft) in a child under the age of six1 that rapidly and disproportionately affects low- and middle-income countries and communities2. Children younger than 3 years of age with any sign of smooth-surface caries, as well as children from ages 3 through 5 with dmft score of ≥ 4 (age 3), ≥ 5 (age 4), or ≥ 6 (age 5) surfaces are classified as severe early childhood caries (S-ECC)1. The clinical management of ECC often requires surgical interventions, and despite advances in etiology knowledge and treatment approaches, ECC recurrence happens in about 40% of treated cases within one year3. This has led to a shift in management from solely operative treatment to more emphasis on prevention and monitoring of caries as a disease4.
The dental pathogen Streptococcus mutans (S. mutans) is consistently associated with caries initiation and development5. The cariogenic potential of S. mutans resides in three core attributes: (1) the ability to synthesize large quantities of extracellular polymers of glucan from sucrose that aid in the permanent colonization of hard surfaces and in the development of the extracellular polymeric matrix in situ, (2) the ability to transport and metabolize a wide range of carbohydrates into organic acids (acidogenicity), and (3) the ability to thrive under environmental stress conditions, particularly low pH (aciduricity)6. Strains of S. mutans are classified into four serotypes (c, e, f and k) with over 70% of strains isolated from dental plaque belonging to serotype c, 20% to serotype e, and the remaining to serotyped f and k6. Most individuals usually harbor a single serotype of S. mutans, however colonization with multiple serotypes has been reported7. While the overall detection of S. mutans in saliva is not a strong predictor of caries risk8, it has been proposed that the presence of S. mutans harboring bona-fide collagen-binding proteins (Cbps) Cnm or Cbm can be linked to increased caries risk9. Specifically, Cbp+ S. mutans is associated with increased caries incidence and poor caries outcomes in children9–11. While Cnm and Cbm are found in nearly 20% of S. mutans isolates10, they are thought to be prevalent in the less common serotypes e, f and k (~ 85% isolates)10. Importantly, the presence of Cbps was associated with the expression of virulence traits that facilitate the persistence of S. mutans in the oral cavity such as adhesion to and invasion of oral cell lines and binding to collagen-rich surfaces (dentin and roots), that ultimately resulted in increased caries severity in a rat caries model11.
Clinical studies have also shown a strong association of Candida albicans (C. albicans) with ECC12–14. In fact, Xiao et al.14, reported that children colonized with C. albicans have approximately 5 times greater risk of developing ECC than those that are not infected14. Moreover, it is well known that co-infection with S. mutans and C. albicans is strongly associated with severe caries in children (S-ECC)14–17. These clinical observations are supported by an in vivo study showing that co-infection with S. mutans and C. albicans can cause more severe and extensive caries in rats18. Thus, a better understanding of the dynamics of cariogenic oral biofilm in patients experiencing ECC is paramount to identify optimal methods for prevention of caries initiation, progression and recurrence.
The present study builds on the premise that the association of S. mutans and C. albicans can result in highly cariogenic biofilms that are intimately associated ECC; and that Cbp+ S. mutans can colonize multiple sites in the oral cavity, especially collagen-rich surfaces such as dentin, contributing to S. mutans niche expansion and caries severity. Here, to determine whether co-infection with S. mutans and C. albicans is also associated with ECC recurrence, we investigated the presence of S. mutans, including Cbp+ strains, and C. albicans in saliva and site-specific dental plaque of children who were caries free (CF), caries experienced without recurrence (CE-NR), and had active recurrent caries (CR). In addition, to gain insight on the microbiota associated with ECC recurrence, and in an attempt to find potential biomarkers for caries recurrence, the salivary microbiome of children with different caries statuses was also investigated.
Results
Study sample characteristics
A total of 163 children were initially enrolled in this study, but 20 of them were excluded due to loss of specimen during storage and transportation. Then, 143 children [73 caries free (CF), 45 caries experienced without recurrence (CE-NR) and 25 with active recurrent caries (CR)] were included in the analyses (Table 1). The age average of all participants was 40 months, but children in the CE-NR group were significantly older (average of 47.8 months) than the CF and CR groups (p < 0.0001). Then, because of the age difference between CE-NR and the other two groups, age in months was included as a covariate in the subsequent analyses. There was no statistically significant difference in the biological sex distribution among the three groups [X2 (2, N = 143) = 0.01, p = 0.99]. About 38% of the children enrolled were non-Hispanic White, 23% were non-Hispanic Black or African American, and 14% were Hispanic. CF group had a significant greater proportion of non-Hispanic Black or African American children (45.21%), while the CE-NR and CR groups were composed of a significantly larger proportion of Hispanic children (24.44%) and other or not reported race/ethnicities (56%), respectively [X2 (6, N = 143) = 61.54, p < 0.0001]. Of the 70 children with ECC enrolled in the CE-NR and CR groups, most of them (82.85%) had severe ECC (S-ECC), with dmft averages of 8.9 and 8.7, respectively (Table 1).
Table 1.
Selected demographic and clinical characteristics of the study subjects.
| Variable | Groups | All subjects (n = 143) |
|||
|---|---|---|---|---|---|
| CF (n = 73) | CE-NR (n = 45) | CR (n = 25) | P value | ||
| Age in months, mean ± SD | 35.8 ± 16.2 | 47.8 ± 9.1 | 38.5 ± 12.7 | < .0001a | 40.0 ± 14.7 |
| Sex | .99b | ||||
| Female | 37 (50.7) | 23 (51.1) | 13 (52.0) | 73 (51.0) | |
| Male | 36 (49.3) | 22 (48.9) | 12 (48.0) | 70 (49.0) | |
| Race/ethnicity | < .0001b | ||||
| White, non-Hispanic | 30 (41.1) | 17 (37.8) | 8 (32.0) | 55 (38.4) | |
| Black or African American, non-Hispanic | 33 (45.2) | 0 (0.0) | 0 (0.0) | 33 (23.1) | |
| Hispanic | 6 (8.2) | 11 (24.44) | 3 (12.0) | 20 (13.9) | |
| Other or not reported | 4 (5.5) | 17 (37.8) | 14 (56.0) | 35 (24.4) | |
| dmft | 0 ± 0 | 8.9 ± 5.0 | 8.7 ± 5.2 | < .0001a,c | 4.3 ± 5.6 |
| dmft/erupted teeth, % ± SD | 0 ± 0 | 50.9 ± 30.7 | 45.9 ± 26.6 | < .0001a,c | 24.0 ± 32.0 |
| S-ECC | 0 (0.0) | 36 (80.0) | 22 (88.0) | < .0001b,c | 58 (40.6) |
Values are presented as mean ± SD or number (%).
CF caries free, CE-NR caries experienced—no recurrence, CR active caries—recurrence, dmft decayed, missing (due to caries), or and filled primary teeth, S-ECC severe early childhood caries.
aGeneralized linear modeling.
bChi-square test.
cAdjusted for age.
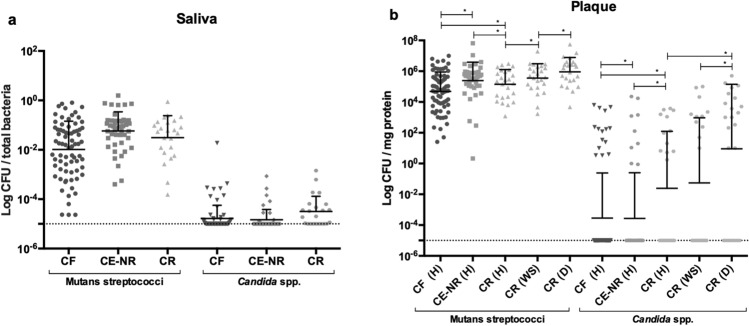
Microbiological analysis reveals that CR subjects have an increased burden of Mutans streptococci and Candida spp. in plaque
To estimate the infection levels with Mutans streptococci and Candida spp. among the three groups, we collected saliva and site-specific plaque samples from enamel surfaces from all children enrolled in this study. No statistically significant differences in Mutans streptococci and Candida spp. counts were found among the three groups in saliva. However, the CR group showed higher counts of Mutans streptococci and Candida spp. in healthy plaque (H) than the CF subjects (p < 0.0001) (Fig. 1a,b). Additionally, to determine the infection burden in diseased sites, we collected plaque samples from a white spot lesion (WS) on the edge of a carious lesion and from a cavitated lesion that visibly extend into the dentin (D) from CR children and found that dentin plaque presented the highest counts of Mutans streptococci and Candida spp. when compared to white spot and healthy plaques (p < 0.05) (Fig. 1b).
Figure 1.
Microbiological analysis of saliva and plaque samples from caries free (CF), caries experienced—no recurrence (CE-NR), and active recurrent caries (CR) groups. Panels A and B depict Mutans streptococci and Candida spp. counts in saliva samples and in healthy plaque (H), white spot lesion plaque (WS) and cavitated dentin plaque (D) from the study groups, respectively. The CFU counts among the three caries status groups were compared using general linear mixed modeling, controlling by age. Data shown are mean ± SD values of log total colony count of Mutans streptococci and Candida spp. colonies.
Presence of Cbp+S. mutans is strongly associated with ECC relapse
Next, we determined the prevalence of S. mutans, including strains harboring genes coding for cnm or cbm, and its serotypes in the study groups. When compared to CF and CE-NR groups, children in the CR group had a larger prevalence of S. mutans (80%) [X2 (2, N = 143) = 99.84, p < 0.0001] (Table 2). All S. mutans isolates were classified as serotypes c, e, f or k with serotype c being the most prevalent in this cohort (20.3% of all children). Although the presence of multiple serotypes (c + e and e + k) was found in some children (7.7% of all subjects), most of the them were infected with a single serotype. Infection with serotype c [X2 (2, N = 143) = 31.13, p < 0.0001] or mixed infection with serotypes e and k [X2 (2, N = 143) = 9.03, p = 0.01] were associated with caries recurrence (Table 2). Strikingly, cnm+ or cbm+ (Cbp+) S. mutans strains were only found in CR subjects and were strongly associated with the ECC recurrence group [X2 (2, N = 143) = 28.23, p < 0.0001] (Table 2). Of a total of 25 CR cases, cnm+ strains were found in 20% of the subjects and cbm+ strains in 8% of the subjects; most of the isolates harboring the Cbp genes (cnm or cbm) belonged to serotype c (71.4%). The overall prevalence of Cbp+ strains (cnm+ or cbm+) among all the S. mutans strains isolated in our study was about 15% (Table 2). When breaking down the CR group into subjects infected with Cbp+ and Cbp− S. mutans and comparing their demographics and clinical characteristics as depicted in Table 3, no significant differences regarding age, sex, dmft score and severity of ECC were found (p > 0.05). Finally, all children infected with Cbp+ S. mutans strains (cnm+ or cbm+) were younger than 3 years of age (mean age ± SD = 27.8 ± 5 months) and classified as S-ECC cases (Table 3).
Table 2.
Presence of S. mutans, its molecular characterization, and presence of Candida spp.
| Variable | Groups | All subjects (n = 143) |
|||
|---|---|---|---|---|---|
| CF (n = 73) n (%) |
CE-NR (n = 45) n (%) |
CR (n = 25) n (%) |
P value* | ||
| S. mutans presence | 11 (15.1) | 14 (31.1) | 20 (80.0) | < .0001 | 45 (31.5) |
| Serotype distribution | |||||
| Ser c only | 6 (8.2) | 8 (17.8) | 15 (60.0) | < .0001 | 29 (20.3) |
| Ser e only | 1 (1.4) | 2 (4.4) | 1 (4.0) | .56 | 4 (2.8) |
| Ser f only | 0 (0.0) | 1 (2.2) | 0 (0.0) | .33 | 1 (0.7) |
| Ser k only | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Ser c + e | 1 (1.4) | 3 (6.7) | 0 (0.0) | .15 | 4 (2.8) |
| Ser e + k | 3 (4.1) | 0 (0.0) | 4 (16.0) | .01 | 7 (4.9) |
| Genes coding for Collagen Binding Proteins | |||||
| Cbp (cnm + cbm) | 0 (0.0) | 0 (0.0) | 7 (28.0) | < .0001 | 7 (4.9) |
| cnm | 0 (0.0) | 0 (0.0) | 5 (20.0) | .0002 | 6 (4.2) |
| cbm | 0 (0.0) | 0 (0.0) | 2 (8.0) | .03 | 2 (1.4) |
| Candida spp. presence | 29 (39.7) | 16 (35.6) | 20 (80.0) | .0007 | 65 (45.5) |
| Candida albicans presence | 15 (20.6) | 9 (20.0) | 17 (68.0) | < .0001 | 41 (28.7) |
| Presence of more than one species of Candida | 9 (12.3) | 2 (4.4) | 5 (20.0) | .30 | 16 (11.2) |
| Co-infection with S. mutans and C. albicans | 7 (9.6) | 7 (15.6) | 17 (68.0) | < .0001 | 31 (21.7) |
CF caries free, CE-NR caries experienced—no recurrence, CR active caries—recurrence.
*P-values based on Cochran-Mantel–Haenszel test of general association, controlling for age by stratification.
Table 3.
Demographic and clinical characteristics of the subjects with caries recurrence.
| Variable | Caries recurrence group | Total subjects CR group (n = 25) | ||
|---|---|---|---|---|
| Cbp– (n = 18) | Cbp+ (n = 7) | P value | ||
| Age in months, mean ± SD | 42 ± 13 | 27.8 ± 5 | .12 | 38.5 ± 12.7 |
| Sex | .19 | |||
| Female | 8 (44.4) | 5 (71.4) | 13 (52.0) | |
| Male | 10 (55.6) | 2 (28.6) | 12 (48.0) | |
| Race/ethnicity | .03 | |||
| White, non-Hispanic | 8 (44.4) | 0 (0.0) | 8 (32.0) | |
| Black or African American, non-Hispanic | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Hispanic | 1 (5.6) | 2 (28.6) | 3 (12.0) | |
| Other or not reported | 9 (50.0) | 5 (71.4) | 14 (56.0) | |
| dmft | 9.3 ± 5.7 | 7.1 ± 3.4 | .45 | 8.7 ± 5.2 |
| dmft/erupted teeth, % ± SD | 49.1 ± 29.0 | 37.7 ± 18.2 | .40 | 45.9 ± 26.6 |
| S-ECC | 15 (83.3) | 7 (100.0) | .59 | 22 (88.0) |
Values are presented as mean ± SD or number (%).
CF caries free, CE-NR caries experienced—no recurrence, CR active caries—recurrence, dmft decayed, missing (due to caries), or and filled primary teeth, S-ECC severe early childhood caries.
Co-infection with C. albicans and S. mutans is strongly associated with caries relapse
We evaluated the prevalence of infection with Candida spp. among the different study groups. About 80% of the subjects in the CR group were infected with Candida spp., an incidence that was significantly greater than that observed for the CF and CE-NR groups in which Candida spp. were found in less than 40% of the subjects [X2 (2, N = 143) = 14.49, p = 0.0007] (Table 2). At species level, C. albicans was isolated in 68% of the CR subjects whereas it was found in only 20% of the CF and CE-NR subjects [X2 (2, N = 143) = 21.41, p < 0.0001]. Importantly, Table 2 shows that co-infection with S. mutans and C. albicans was most prevalent in the CR group compared to CF and CE-NR [X2 (2, N = 143) = 39.42, p < 0.0001].
CR children infected with Cbp+S. mutans strains have a higher burden of Mutans streptococci and Candida spp. than those infected with Cbp- strains
Since we observed that Cbp+ S. mutans strains were only found in the CR group, we compared the infection characteristics of CR subjects infected with Cbp+ S. mutans versus those infected with Cbp- S. mutans. We observed that subjects infected with Cbp+ S. mutans tended to have overall higher counts of Candida spp. and Mutans streptococci in white spot lesions (WS) or healthy plaque (H) than those who were colonized with Cbp- S. mutans (Fig. 2), but the differences were not statistically significant. However, in dentin sites, Mutans streptococci counts were significantly higher (eightfold) in subjects infected with Cbp+ S. mutans in comparison to subjects that were infected Cbp- S. mutans (p = 0.0077). Although not statistically significant, Candida spp. counts were 13-fold higher in dentin in the Cbp+ S. mutans group than in Cbp- S. mutans subjects.
Figure 2.
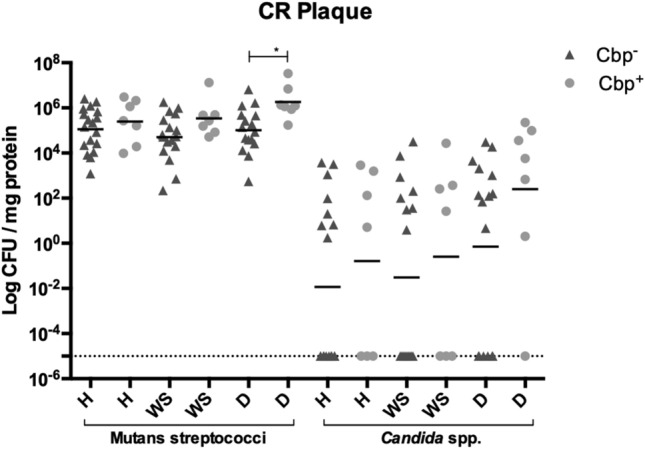
Microbiological analysis of plaque samples collected from subjects with active recurrent caries (CR group). Graph shows Mutans streptococci and Candida spp. counts in healthy plaque (H), white spot lesion plaque (WS) and cavitated dentin plaque (D) of CR subjects in relation to infection with S. mutans strains harboring either cnm or cbm genes (Cbp+). The CFU counts of the Cbp+ and Cbp- CR subjects were compared using general linear mixed modeling. Data shown are mean ± SD values of log total colony count of Mutans streptococci and Candida spp. colonies.
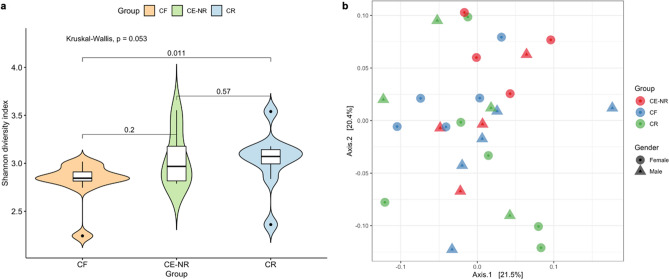
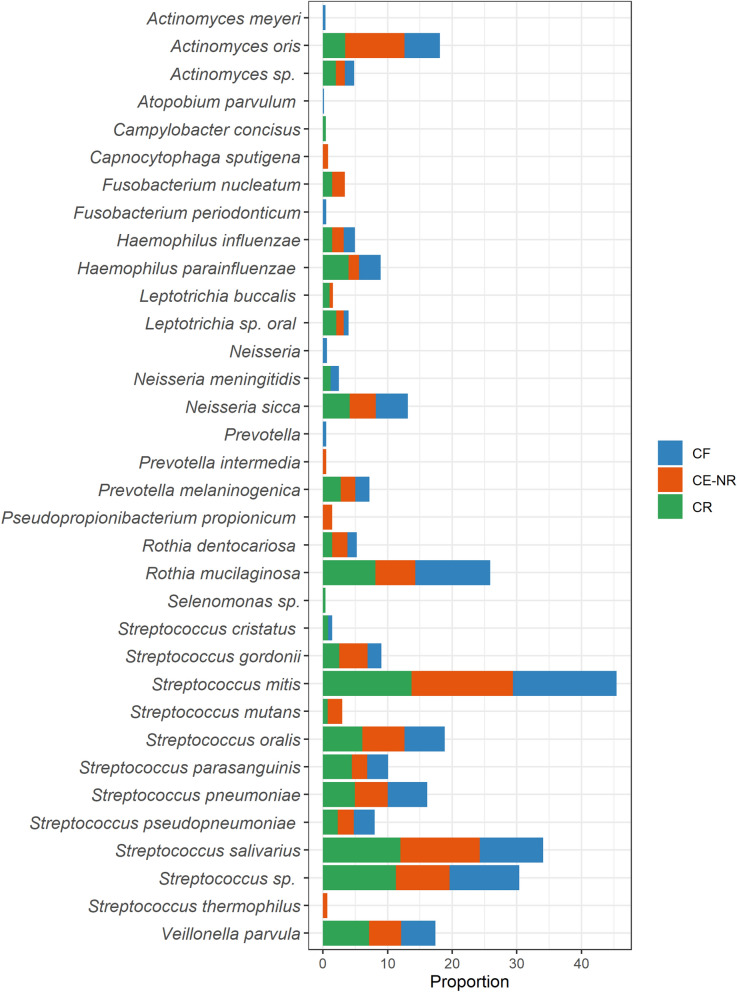
Salivary microbiome analysis revealed that Streptococcus parasanguinis is overrepresented in the CR group
We investigated the salivary microbiome using the Nanopore MinION platform to gain additional insight on the microbiota associated with ECC recurrence and whether other biomarkers of caries recurrence could be found. After filtering out H. sapiens sequences, which consisted of about 87% of all obtained sequences, and samples with coverage under 70%, the final dataset comprised of 53,953 long-read sequences distributed in 28 samples (CF: n = 10; CE-NR: n = 8; CR: n = 10) (Supplementary Table S1). The average number of sequences per sample was 1,926 and the median was 698 with a total of 703 bacterial species detected. Very low percentage of sequence readings belonging to fungi (0.7%), viruses (0.06%) or archaea (0.02%) were detected within this dataset. The alpha diversity mean of children with ECC recurrence was significantly greater as compared with caries free children (p = 0.011) but not with children in the CE-NR group (p = 0.57) (Fig. 3). The most abundant operational taxonomic units found in the three groups were Streptococcus mitis and Streptococcus salivarius (Fig. 4). Even though S. mutans was detected in higher abundance in the CE-NR subjects than in the other two groups, it comprised only a small proportion of the salivary microbiome (less than 5%) (Fig. 4), corroborating with our microbiological findings that showed that Mutans streptococci comprised of a small proportion of the total cultivable microbiota in saliva (Fig. 1). However, differential abundance analysis by the ALDEx2 ANOVA-like method revealed that Streptococcus parasanguinis was more abundant in CR than in CF subjects. The median centered log ratio (clr) value of this microorganism was 6.53 and 4.28 in CR and CF subjects, respectively, with an effect size of 0.62 and a substantial difference between them (p = 0.05). When CR and CE-NR groups were compared, a marginal difference was observed in which S. parasanguinis median clr value was 6.48 to CR and 4.72 to CE-NR with an effect of 0.58 (p = 0.06).
Figure 3.
Shannon alpha diversity and Beta diversity metrics of the salivary microbiome of children who were caries free (CF), caries experienced—no recurrence (CE-NR) and had active recurrent caries (CR). (A) Violin plot depicting Shannon alpha diversity measures for each sample category was analyzed by paired Kruskal–Wallis test. CR group has a significantly higher alpha diversity when compared to CF and CE-NR. (B) Beta diversity was compared by using Principal Coordinate Analysis and the strength of the differences were tested by Permutational Analysis of Variance. No differences were observed in Beta diversity among the groups.
Figure 4.
Distribution of the top 25 most abundant taxa across the caries free (CF), caries experienced—no recurrence (CE-NR) and active recurrent caries (CR) groups using rarefied taxon counts. The chart shows mean taxon counts for sample group. Means are shown as relative proportions.
The microbial communities from children of different caries statuses were compared by using multivariate PERMANOVA and Bray–Curtis distances, which showed no significant difference in beta diversity (R2 = 0.097; p = 0.189) (Fig. 3). Age (R2 = 0.047; p = 0.252), sex (R2 = 0.018; F = 0.488; p = 0.919) and caries status (R2 = 0.078; F Model = 1.043; p-value = 0.919) had no significant association with oral bacterial composition.
Discussion
Despite increased surveillance and better treatment approaches3, ECC continues to be a significant health problem2 that has a high recurrence rate. While the association of S. mutans and C. albicans in caries initiation and progression is well established19, much less is known about the characteristics of the microbiota associated with ECC recurrence. Therefore, new predictors of ECC recurrence with high prognostic value are still needed20. In the present study, we observed an association of co-infection with S. mutans, especially with Cbp+ strains, and C. albicans with caries recurrence in children that received restorative treatment for ECC and developed new dentin caries lesions within 6 months post-treatment.
Previously, our group showed that the expression of Cbps confers S. mutans with the ability to bind more avidly to collagen-rich tooth surfaces such as dentin and roots, as well as to invade oral epithelial cell lines11,21, which also contributes to S. mutans niche expansion beyond the tooth enamel22. Here, Cbp+ S. mutans strains were only found in children with caries recurrence and classified as S-ECC because they were younger than 3 years old. Based on the ability of Cbp+ strains to colonize oral epithelial cells11, it is possible that oral infection by Cbp+ S. mutans in these children occurred before tooth eruption, which would have allowed S. mutans to colonize the dental biofilm immediately upon tooth eruption. In an animal model of caries, Miller et al.11 demonstrated that infection with cnm+ S. mutans is associated with increased S. mutans load in dental plaque and with caries severity, suggesting a role for Cnm in the assembly of the cariogenic biofilm11. Furthermore, clinical studies have demonstrated that infection with cnm+ S. mutans is associated with increased caries risk in children9,10. We speculate that because Cbp+ S. mutans can colonize multiple niches in the oral cavity, possibly including soft tissues, these strains can rapidly recolonize oral surfaces after oral hygiene, prophylaxis and clinical intervention measures, ultimately resulting in recalcitrant infections.
In addition to S. mutans, the presence of Candida species in the oral cavity has been associated with dental caries, with C. albicans being the most prevalent species present in caries-active children15,23,24. In our cohort, CR subjects harbored highest levels of Candida spp. in plaque, especially in carious dentin plaque. Because collagen type I is the main organic component of dentin25 and C. albicans is highly aciduric and able to efficiently adhere to and degrade collagen, it is therefore not entirely unexpected that C. albicans is found in dentin carious lesions26–28. Also, in vitro studies showed that clinical isolates of C. albicans can promote tooth demineralization with consequent loss of hardness29, a finding that was supported by in vivo studies showing that rats infected with C. albicans developed carious lesions18,30. Notably, S. mutans and C. albicans have a synergistic interaction that promotes assembly of highly cariogenic biofilms resulting in the most aggressive forms of caries in children14–17 and in animals18. Moreover, S. mutans and C. albicans together are recalcitrant to surgical interventions (i.e. extensive dental treatment usually provided in hospital operating rooms) followed by prophylactic chlorhexidine treatments17 thereby contributing to increased risk of caries recurrence. In addition to synergistic interactions that promote biofilm accumulation18, C. albicans possesses several traits making it a desirable neighbor for S. mutans. More specifically, C. albicans utilizes lactic acid, a byproduct of S. mutans metabolism, as energy source, is highly acidogenic and aciduric, and reduces oxygen tension of the biofilm31. At the same time, S. mutans secretes glucosyltransferase B that binds to the surface of C. albicans making it a de facto glucan producer when sucrose is present, contributing to accumulation of biofilm matrix32. Strikingly, we observed that CR subjects infected with Cbp+ S. mutans had at least 13-fold more C. albicans and eightfold more Mutans streptococci counts in dentin than subjects infected with Cbp- S. mutans. Thus, it seems that co-infection with Cbp+ S. mutans and C. albicans results in even more potent synergistic cross-kingdom interactions. Studies investigating the contribution of Cbps to the establishment of S. mutans and C. albicans cariogenic biofilms are currently underway.
In accordance with previous studies7,33,34, our data demonstrated that serotype c is the most prevalent S. mutans serotype found in our cohort. Although most subjects of this study were infected with a single S. mutans serotype, co-infection with serotypes e and k was associated with caries recurrence, which is in alignment with studies showing that infection by more than one S. mutans serotype is associated to increased caries risk34. Even though Cbp+ strains have been commonly found in the less common serotypes e, f and k10,35, the majority of the Cbp+ S. mutans isolates identified in our study belonged to serotype c7. The differences observed in serotype prevalence of Cbp+ strains between previous studies and ours may relate to how little is known about the epidemiology of Cbp+ S. mutans in the United States, as most previous studies were done with European and Asian cohorts9,10,36.
Using the Nanopore MinION platform, we showed that the salivary microbiome of the CR group has greater alpha diversity than the CF group. This finding was unexpected as previous publications showed that in greater caries incidence, there is a reduction in diversity and an enrichment for aciduric and acidogenic species37–39. It should be noted that, to our knowledge, this is the first time that the Nanopore sequencing platform was used to study oral microbiome of caries recurrence. One possibility for this unexpected finding is that, when compared to the other sequencing platforms used in previous oral microbiome studies, Nanopore sequencing generates less bias as it does not require enrichment and amplification steps. Moreover, the Nanopore platform generates long reads allowing appropriate species-level assignments whereas for 16S-based sequencing platforms, species assignment is not always possible and often times bacterial identifications are made at genus level.
Similar to previous microbiome studies40,41, our salivary microbiome data could not identify specific taxa that could serve as biomarkers of health and disease. However, we found that S. parasanguinis was relatively more abundant in CR subjects than in the CF and CE-NR groups. Interestingly, studies comparing dental plaque from caries-active and caries-free subjects also observed that S. parasanguinis was over-represented in caries-active patients37,42. While the peroxigenic commensal Streptococcus parasanguinis is commonly seen as a beneficial microorganism that antagonizes S. mutans, future studies are warranted to address the role of S. parasanguinis in caries37.
Collectively, this study indicates that children colonized with Cbp+ S. mutans may be predisposed to recalcitrant caries infections that do not respond to clinical interventions, and that oral co-infection with Cbp+ S. mutans and C. albicans might be even harder to eradicate than S. mutans alone or Cbp- S. mutans and C. albicans. Even though the cross-sectional nature of this study is a limiting factor, the initial concept that ECC recurrence could be attributed to persistent co-infection with Cbp+ S. mutans and C. albicans is novel and warrants further investigation such as longitudinal studies to demonstrate cause and effect. If this relationship is confirmed, a paradigm shift can be made towards ECC prevention and treatment through the integration of this information into the assessment of caries risk. For example, simple tests involving oral swabs can be used to screen infants and toddlers for the presence of Cbp+ S. mutans and Candida species. Then, early interventions could be adopted to specifically target these microorganisms in children with ECC given the recalcitrant nature of this infection in this population.
Methods
Recruitment and enrollment
The human subject protocol was reviewed and approved by the Institutional Review Board of the University of Florida (IRB201600851). All methods were performed in accordance with STROBE guidelines and regulations. Children ranging from 6 to 72 months, in their primary dentition, were enrolled in the study between September 2016 through February 2020. All subjects were patients at the University of Florida College of Dentistry (UFCD) Department of Pediatric Dentistry. Written informed consent was obtained from at least one parent or legal guardian of the subjects before collection of the samples. Subjects that were in good general health and had not used antibiotics at least 1 month before their appointment were selected based on their overall baseline caries experience. Other exclusion criteria included: any medical conditions requiring pre-medication prior to dental treatment, immunosuppression or any type of compromised immune system, and orthodontic or intra-oral orthopedic appliances. These subjects were diagnosed by calibrated pediatric dentists then categorized into one of three groups based on the American Academy of Pediatric Dentistry (AAPD) criteria: (1) Caries Free group (CF; no visible caries), (2) Caries Experienced—No Recurrence group (CE-NR; prior ECC treatment with no visible caries 6-months post treatment), and (3) Caries Active—Recurrence group (CR; prior ECC treatment with visible dentin caries lesions within 3 to 6-months post treatment). Using AAPD criteria, subjects from the groups CE-NR and CR were also classified regarding ECC severity. Of note, the study team was recalibrated by the same pediatric dentist, Dr. Leda Mugayar, at least every six months or whenever a new member joined the study team.
Specimen collection
All enrolled subjects donated saliva and site-specific plaque samples from a healthy enamel surface (H), preferably from healthy teeth distal from the diseased one(s). If healthy teeth were not present, we collected from the largest intact enamel area of the least affected tooth. For CR patients, additional site-specific plaque sample from a white spot lesion (WS) on the edge of a carious lesion and from a cavitated lesion that visibly extends into the dentin (D) were collected. Approximately 1 ml of unstimulated saliva was obtained through a pediatric mucus trap attached to a vacuum pump43. All plaque samples were collected using a sterile dental micro-applicator brush, which was then deposited into a tube containing 1 ml sterile 0.1 M glycine buffer (pH 7) solution. Each patient received an alphanumeric code.
Microbiological analysis
Upon specimen collection, de-identified saliva and plaque samples were brought to lab within 3 h of collection and processed a blinded member of the study team. Samples were serially diluted in 1 ml of 0.1 M glycine buffer solution and plated on mitis-salivarius agar (Becton, Dickinson and Company BBL™, Franklin Lakes, NJ, USA) supplemented with 0.388 mg/ml bacitracin (MSB) for quantification and isolation of Mutans streptococci44,45. Saliva samples were also plated onto tryptic soy agar + 5% sheep blood agar (TSA II; Moltox, Boone, NC, USA) for quantification of total bacteria. MSB and TSA II plates were incubated at 37 °C in a 5% CO2 atmosphere for 48 h. The TSA II plates were transferred to an aerobic incubator for an additional 24 h to allow for growth of aerobes. Eight S. mutans-like colonies from each sample (saliva, H, WS and D) were picked from the MSB plates and patched onto tryptic soy agar (Becton, Dickinson and Company BBL™, Franklin Lakes, NJ, USA) plates for further analysis. Salivary counts of Mutans streptococci were normalized to total bacterial counts. Also, plaque counts of Mutans streptococci were normalized to total plaque protein content determined by bicinchoninic acid (BCA) protein assays. The identity of isolated S. mutans-like colonies was determined by PCR using S. mutans-specific primers46. Then, for the confirmed S. mutans colonies, the serotype and the presence of genes coding for the collagen and laminin binding proteins, cnm and cbm, were determined by PCR using serotype-specific primers33,34,47 and cnm and cbm-specific primers35,48 (Supplementary Table S2). UA159 (serotype c; cnm-), B14 (serotype e; cnm+), OMZ175 (serotype f; cnm+), and OM88X (serotype k; cbm+) were included as controls in the PCR reactions.
The prevalence of Candida spp. was determined by plating serial dilutions of saliva and plaque samples onto Sabouraud agar (Becton, Dickinson and Company BBL™, Franklin Lakes, NJ, USA) supplemented with 0.4 mg/ml chloramphenicol15. Salivary counts of Candida spp were normalized to total bacterial counts. Also, plaque counts of Candida spp were normalized to total plaque protein content determined by bicinchoninic acid (BCA) protein assays. Then, eight Candida spp. colonies from each sample (saliva, H, WS and D) were streaked onto HardyCHROM™ agar (Hardy Diagnostics, Santa Maria, CA, USA) for presumptive identification of the four main human-associated Candida species (C. albicans, C. tropicalis, C. glabrata, and C. krusei).
Salivary microbiome analysis
The salivary microbiome was investigated using the Nanopore MinION sequencing platform (Oxford Nanopore Technologies, Oxford, UK). Salivary DNA from each sample was extracted using the Quick-DNA™ Fungal/Bacterial Miniprep Kit following the manufacturer’s protocol (Zymo Research Corp, Irvine, CA, USA). Library preparation was performed using 400 ng of DNA from each sample and Rapid Barcoding Sequencing (SQK-RKB004, Oxford Nanopore Technologies, Oxford, UK) following manufacturer’s guidelines. Samples were pooled, cleaned and concentrated using AxyPrep FragmentSelect (Axygen, Union City, CA, USA). Next, 1 µl of rapid adapter was added to 10 µl of the pooled eluate and the library kept on ice until loaded onto the flow cell. Groups of 12 saliva samples were pooled to create one library. Shotgun metagenomic sequencing was carried out on a FLO-MIN 106D R9 MinION sequencer version. The Barcoding and WIMP workflows were employed using default Q-score ≥ 7. Each MinION cell was run for 48 h. The result files from the 3 workflows (12 patients in each workflow) were combined in order to compare the microbiota of all samples. The Raw sequences were deposited in the Sequence Read Archive (SRA) BioProject (accession number PRJNA679743).
Statistical analysis
The counts of Mutans streptococci and Candida spp. in the plaque and saliva among the three caries status groups were compared using general linear mixed modeling. To improve the normal distribution of the concentrations for regression modeling while also accounting for the presence of values of zero among the plaque and saliva assays, log transformations that included a constant in the form of, for example, log Mutans streptococci in plaque = log (Mutans streptococci counts in plaque + 0.000001) were used. Because there were age differences among the three groups, age in months was included as a covariate in the mixed models. Progression analyses were conducted using the MIXED procedure in the SAS statistical analysis package, version 9.4 (SAS Institute, Cary, NC, USA).
Microbial identification was carried out using WIMP analysis tool. The resulting table with the classification of each long Nanopore read was imported into the R environment. A contingency table was built and used for downstream analysis. The dataset was filtered by removing Homo sapiens DNA sequences and only samples with sequence coverage greater than 70% were kept. After rarefying the samples to the same number of sequences, Shannon diversity index estimator were calculated using the “phyloseq” package, and then plotted using the “ggpubr” package, both in the R environment. The alpha diversity measurements were tested for normality using the Shapiro–Wilk test, and differences among the categories were determined with the Kruskall–Wallis test.
Differences in microbial community structure were visualized by Principal Coordinate Analysis (PCoA) and the strength of the differences tested by Permutational Analysis of Variance (PERMANOVA). Briefly, the centered log ratio transformation was applied and the transformed dataset used to construct a dissimilarity matrix generated by euclidean distance. The matrix was ordinate by PCoA and the adonis function was used to calculate the PERMANOVA with the vegan package. The differential abundance analysis among groups was performed using ALDEx249.
Supplementary Information
Acknowledgements
We thank the pediatric dentistry residents Drs. Joshua Cline, Latoya Jones, Nikki Darbani, Max Rudie, Andrés Alvarez, Kiersten Pannel and Catherine Graham for excellent clinical assistance in collecting patient samples. We thank Dr. Jessica Kajfasz for critically revising the text. This work was supported by DE022559, 5R90DE022530-09 and Colgate-Palmolive CARE award.
Author contributions
B.A.G. and N.C.A., contributed to data acquisition, analysis, and interpretation; and drafted and critically revised the manuscript. S.L.T. and L.F.W.R., contributed to data analysis and interpretation; and critically revised the manuscript. L.R.F.M., contributed to conception, design, and critically revised the manuscript; J.A.L., contributed to conception and critically revised the manuscript; J.A., contributed to conception, design, data analysis and interpretation and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: B. A. Garcia and N. C. Acosta.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-90198-3.
References
- 1.American Academy of Pediatric Dentistry. Definition of early childhood caries (ECC). https://www.aapd.org/assets/1/7/d_ecc.pdf (2008).
- 2.Phantumvanit P, et al. WHO Global consultation on public health intervention against early childhood caries. Community Dent. Oral Epidemiol. 2018;46:280–287. doi: 10.1111/cdoe.12362. [DOI] [PubMed] [Google Scholar]
- 3.Berkowitz RJ, Amante A, Kopycka-Kedzierawski DT, Billings RJ, Feng C. Dental caries recurrence following clinical treatment for severe early childhood caries. Pediatr. Dent. 2011;33:510–514. [PubMed] [Google Scholar]
- 4.Pitts NB, et al. Dental caries. Nat. Rev. Dis. Prim. 2017;3:17030. doi: 10.1038/nrdp.2017.30. [DOI] [PubMed] [Google Scholar]
- 5.Hajishengallis E, Parsaei Y, Klein MI, Koo H. Advances in the microbial etiology and pathogenesis of early childhood caries. Mol. Oral Microbiol. 2017;32:24–34. doi: 10.1111/omi.12152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lemos JA, et al. The biology of Streptococcus mutans. Microbiol. Spectr. 2019;7:16–18. doi: 10.1128/microbiolspec.GPP3-0051-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Momeni SS, et al. Streptococcus mutans serotypes and collagen-binding proteins Cnm/Cbm in children with caries analysed by PCR. Mol. Oral Microbiol. 2019;34:64–73. doi: 10.1111/omi.12254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernando S, Tadakamadla SK, Bakr M, Scuffham PA, Johnson NW. Indicators of risk for dental caries in children: a holistic approach. JDR Clin. Transl. Res. 2019;4:333–341. doi: 10.1177/2380084419834236. [DOI] [PubMed] [Google Scholar]
- 9.Esberg A, et al. Streptococcus mutans adhesin biotypes that match and predict individual caries development. EBioMedicine. 2017;24:205–215. doi: 10.1016/j.ebiom.2017.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nomura R, et al. Molecular and clinical analyses of the gene encoding the collagen-binding adhesin of Streptococcus mutans. J. Med. Microbiol. 2009;58:469–475. doi: 10.1099/jmm.0.007559-0. [DOI] [PubMed] [Google Scholar]
- 11.Miller JH, et al. The collagen binding protein Cnm contributes to oral colonization and cariogenicity of Streptococcus mutans OMZ175. Infect. Immun. 2015;83:2001–2010. doi: 10.1128/IAI.03022-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Carvalho FG, Silva DS, Hebling J, Spolidorio LC, Spolidorio DMP. Presence of Mutans streptococci and Candida spp. in dental plaque/dentine of carious teeth and early childhood caries. Arch. Oral Biol. 2006;51:1024–1028. doi: 10.1016/j.archoralbio.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 13.Baraniya D, et al. Supragingival mycobiome and inter-kingdom interactions in dental caries. J. Oral Microbiol. 2020;12:1729305. doi: 10.1080/20002297.2020.1729305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xiao J, et al. Candida albicans carriage in children with severe early childhood caries (S-ECC) and maternal relatedness. PLoS ONE. 2016;11:e0164242. doi: 10.1371/journal.pone.0164242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raja M, Hannan A, Ali K. Association of oral candidal carriage with dental caries in children. Caries Res. 2010;44:272–276. doi: 10.1159/000314675. [DOI] [PubMed] [Google Scholar]
- 16.Fragkou S, et al. Streptococcus mutans, Streptococcus sobrinus and Candida albicans in oral samples from caries-free and caries-active children. Eur. Arch. Paediatr. Dent. 2016;17:367–375. doi: 10.1007/s40368-016-0239-7. [DOI] [PubMed] [Google Scholar]
- 17.Klinke T, et al. Changes in Candida spp., Mutans streptococci and lactobacilli following treatment of early childhood caries: A 1-year follow-up. Caries Res. 2014;48:24–31. doi: 10.1159/000351673. [DOI] [PubMed] [Google Scholar]
- 18.Falsetta ML, et al. Symbiotic relationship between Streptococcus mutans and Candida albicans synergizes virulence of plaque biofilms in vivo. Infect. Immun. 2014;82:1968–1981. doi: 10.1128/IAI.00087-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belstrøm D. The salivary microbiota in health and disease. J. Oral Microbiol. 2020;12:1723975. doi: 10.1080/20002297.2020.1723975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fontana M, Carrasco-Labra A, Spallek H, Eckert G, Katz B. Improving caries risk prediction modeling: a call for action. J. Dent. Res. 2020;99:1215–1220. doi: 10.1177/0022034520934808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abranches J, et al. The collagen-binding protein Cnm is required for Streptococcus mutans adherence to and intracellular invasion of human coronary artery endothelial cells. Infect. Immun. 2011;79:2277–2284. doi: 10.1128/IAI.00767-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Freires IA, et al. Heterologous expression of Streptococcus mutans Cnm in Lactococcus lactis promotes intracellular invasion, adhesion to human cardiac tissues and virulence. Virulence. 2017;8:18–29. doi: 10.1080/21505594.2016.1195538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koo H, Bowen WH. Candida albicans and Streptococcus mutans: A potential synergistic alliance to cause virulent tooth decay in children. Future Microbiol. 2014;9:1295–1297. doi: 10.2217/fmb.14.92. [DOI] [PubMed] [Google Scholar]
- 24.Udayalaxmi J, Shenoy N. Comparison between biofilm production, phospholipase and haemolytic activity of different species of candida isolated from dental caries lesions in children. J. Clin. Diagnos. Res. 2016;10:DC21–DC23. doi: 10.7860/JCDR/2016/17019.7643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goldberg M, Kulkarni AB, Young M, Boskey A. Dentin: structure, composition and mineralization. Front. Biosci. (Elite Ed) 2011;3:711–735. doi: 10.2741/e281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Connell LM, et al. Site-specific profiling of the dental mycobiome reveals strong taxonomic shifts during progression of early-childhood caries. Appl. Environ. Microbiol. 2020;86:e02825–e2919. doi: 10.1128/AEM.02825-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fakhruddin KS, et al. Candida biome of severe early childhood caries (S-ECC) and its cariogenic virulence traits. J. Oral Microbiol. 2020;12:1724484. doi: 10.1080/20002297.2020.1724484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pereira DFA, Seneviratne CJ, Koga-Ito CY, Samaranayake LP. Is the oral fungal pathogen Candida albicans a cariogen? Oral Dis. 2018;24:518–526. doi: 10.1111/odi.12691. [DOI] [PubMed] [Google Scholar]
- 29.Brandi TCA, et al. Demineralizing potential of dental biofilm added with Candida albicans and Candida parapsilosis isolated from preschool children with and without caries. Microb. Pathog. 2016;100:51–55. doi: 10.1016/j.micpath.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 30.Klinke T, Guggenheim B, Klimm W, Thurnheer T. Dental caries in rats associated with Candida albicans. Caries Res. 2011;45:100–106. doi: 10.1159/000324809. [DOI] [PubMed] [Google Scholar]
- 31.Metwalli KH, Khan SA, Krom BP, Jabra-Rizk MA. Streptococcus mutans, Candida albicans, and the human mouth: a sticky situation. PLoS Pathog. 2013;9:e1003616. doi: 10.1371/journal.ppat.1003616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ellepola K, Liu Y, Cao T, Koo H, Seneviratne CJ. Bacterial GtfB augments Candida albicans accumulation in cross-kingdom biofilms. J. Dent. Res. 2017;96:1129–1135. doi: 10.1177/0022034517714414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nakano K, et al. Serotype distribution of Streptococcus mutans a pathogen of dental caries in cardiovascular specimens from Japanese patients. J. Med. Microbiol. 2007;56:551–556. doi: 10.1099/jmm.0.47051-0. [DOI] [PubMed] [Google Scholar]
- 34.Shibata Y, et al. Analysis of loci required for determination of serotype antigenicity in Streptococcus mutans and its clinical utilization. J. Clin. Microbiol. 2003;41:4107–4112. doi: 10.1128/JCM.41.9.4107-4112.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nakano K, et al. Molecular characterization of Streptococcus mutans strains containing the cnm gene encoding a collagen-binding adhesin. Arch. Oral Biol. 2010;55:34–39. doi: 10.1016/j.archoralbio.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 36.Misaki T, et al. Presence of Streptococcus mutans strains harbouring the cnm gene correlates with dental caries status and IgA nephropathy conditions. Sci. Rep. 2016;6:36455. doi: 10.1038/srep36455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gross EL, et al. Beyond Streptococcus mutans: dental caries onset linked to multiple species by 16S rRNA community analysis. PLoS ONE. 2012;7:e47722. doi: 10.1371/journal.pone.0047722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hurley E, et al. Comparison of the salivary and dentinal microbiome of children with severe-early childhood caries to the salivary microbiome of caries-free children. BMC Oral Health. 2019;19:13. doi: 10.1186/s12903-018-0693-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kalpana B, et al. Bacterial diversity and functional analysis of severe early childhood caries and recurrence in India. Sci. Rep. 2020;10:21248. doi: 10.1038/s41598-020-78057-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ling Z, et al. Analysis of oral microbiota in children with dental caries by PCR-DGGE and barcoded pyrosequencing. Microb. Ecol. 2010;60:677–690. doi: 10.1007/s00248-010-9712-8. [DOI] [PubMed] [Google Scholar]
- 41.Simon-Soro A, et al. Combined analysis of the salivary microbiome and host defence peptides predicts dental disease. Sci. Rep. 2018;8:1484. doi: 10.1038/s41598-018-20085-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peterson SN, et al. The dental plaque microbiome in health and disease. PLoS ONE. 2013;8:e58487. doi: 10.1371/journal.pone.0058487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Morou-Bermudez E, et al. Urease activity as a risk factor for caries development in children during a three-year study period: A survival analysis approach. Arch. Oral Biol. 2011;56:1560–1568. doi: 10.1016/j.archoralbio.2011.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gold OG, Jordan HV, van Houte J. A selective medium for Streptococcus mutans. Arch. Oral Biol. 1973;18:1357–1364. doi: 10.1016/0003-9969(73)90109-X. [DOI] [PubMed] [Google Scholar]
- 45.Momeni SS, et al. Mutans streptococci enumeration and genotype selection using different bacitracin-containing media. J. Microbiol. Methods. 2014;103:53–57. doi: 10.1016/j.mimet.2014.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen Z, et al. Development of species-specific primers for detection of Streptococcus mutans in mixed bacterial samples. FEMS Microbiol. Lett. 2007;272:154–162. doi: 10.1111/j.1574-6968.2007.00756.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nakano K, Nomura R, Nakagawa I, Hamada S, Ooshima T. Demonstration of Streptococcus mutans with a cell wall polysaccharide specific to a new serotype, k, in the human oral cavity. J. Clin. Microbiol. 2004;42:198–202. doi: 10.1128/JCM.42.1.198-202.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nomura R, et al. Identification and characterization of a collagen-binding protein, Cbm, in Streptococcus mutans. Mol. Oral Microbiol. 2012;27:308–323. doi: 10.1111/j.2041-1014.2012.00649.x. [DOI] [PubMed] [Google Scholar]
- 49.Fernandes AD, Macklaim JM, Linn TG, Reid G, Gloor GB. ANOVA-like differential expression (ALDEx) analysis for mixed population RNA-Seq. PLoS ONE. 2013;8:67019. doi: 10.1371/journal.pone.0067019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.