Abstract
Severe acute respiratory syndrome coronavirus-2 (SARS CoV-2) infection causes the disease known as coronavirus disease that started in Wuhan (China) in December 2019, leading to the current COVID-19 pandemic. The common presenting symptoms include fever, dry cough, shortness-of-breath, while sore throat, diarrhea, and abdominal and chest pain are the least. The atypical presentation of SARS CoV-2 infection poses a challenge for family physicians to screen and manage such patients for COVID-19 and specifically those at high risk with underlying disease such a sickle cell disease. Herein, we report a case of SARS CoV-2 infection in a known patient of sickle cell disease (SCD) with an atypical presentation, in whom the course of the disease was mild to moderate, uncomplicated, and the patient had an uneventful recovery. Primary care physicians should be vigilant to screen and manage such patients with established protocols, especially in the ongoing COVID-19 pandemic.
Keywords: Acute chest syndrome, COVID-19, sickle cell disease, vaso-occlusive crisis
Introduction
Since the start of the current COVID-19 pandemic, that was caused by severe acute respiratory syndrome coronavirus-2 (SARS CoV-2), and as of October 26, 2020, over 43 million people affected globally[1] with a more vulnerable domain of individuals, aged with comorbid conditions such as diabetes, hypertension (HTN), obesity, cancer, HIV, and hepatic and renal disorders.[2,3] Sickle cell disease (SCD) patients that are thought to be vulnerable to complications if they get a viral illness, still it is controversial whether SCD patients are at an increased risk of complications if infected by COVID-19.
The common presenting symptoms in general include fever, dry cough, shortness-of- breath while sore throat, diarrhea, and abdominal and chest pain are the least as evident from the meta-analysis[4] while atypical presentation has been reported in SCD in many published case reports. Sickle cell disease (SCD), a genetic disorder caused by a single point mutation (Glu6Val), affects millions of people globally and in particular ancestors from sub-Saharan Africa, Saudi Arabia, India, and Mediterranean countries such as Italy, Greece, and Turkey. The prevalence of sickle cell trait Saudi Arabia is 5/1000 and 0.38/1000 for sickle cell disease, according to the Saudi premarital screening program report.[5]
Herein, we report a known patient of SCD with a laboratory-confirmed diagnosis of COVID-19 based on real-time polymerase chain reaction (RT-PCR) results. The course of the disease was mild-moderate, and the patient had an uneventful recovery.
Case Presentation
A 29-year-old male, a known patient of SCD, an HbSS/Sβ0, variant presented to the primary care center with a history of sore throat and three episodes of loose motions. There was no history of fever or cough. His past and family history is suggestive of splenectomy at the age of 13 and has a younger brother with SCD. Due to the current COVID-19 pandemic and nonspecific nature of symptoms related to this disease; the primary care physician requested a test for SARS CoV-2 with the advice of home isolation. A nasopharyngeal swab, taken for real-time polymerase chain reaction (RT-PCR) testing for SARS CoV-2 infection confirmed the diagnosis of COVID-19 the next day. The patient was admitted to the hospital for close observation and management.
On examination upon admission showed a well-looking afebrile patient with vitals as pulse 84/min, blood pressure (BP) 115/79 mmHg, and respiratory rate 22/min, SPO2 99% on room air with no other finding on clinical examination. Laboratory workup showed [Table 1]:
Table 1.
Laboratory Findings
| Blood Test | Result | Reference Range |
|---|---|---|
| WBC count | 11.26 | 3.6-11 103/µL |
| RBC | 3.96 | 4.5-5.5 103/µL |
| Hemoglobin | 10.7 | 13-17 g/dL |
| Neutrophils | 5.00 | 2-7 103/µL |
| Lymphocytes | 4.54 | 1.0-3.0 103/µL |
| Monocytes | 1.23 | 0-8 103/µL |
| Hematocrit | 31.2 | 40%-50% |
| Platelets | 459 | 150-410 103/µL |
| S. Urea | 2.56 | 2.50-9.20 mmol/L |
| S. Creatinine | 56.79 | 50.00-110.00 mmol/L |
| Na | 139 | 136-145 mmol/L |
| K | 4.5 | 3.3-4.8 mmol/L |
| Cl | 91 | 98-108 mmol/L |
| Alkaline phosphatase | 123 | 40-150 U/L |
| Prothrombin time | 28.4 | 9.7-11.4 s |
| INR (international normalized ratio) | 1.92 | 0.8-1.1 |
| APTT (activated partial thromboplastin time) | 65.3 | 27-40 s |
A plain radiograph of the chest [Figure 1] shows an old consolidation of the lung parenchyma.
Figure 1.
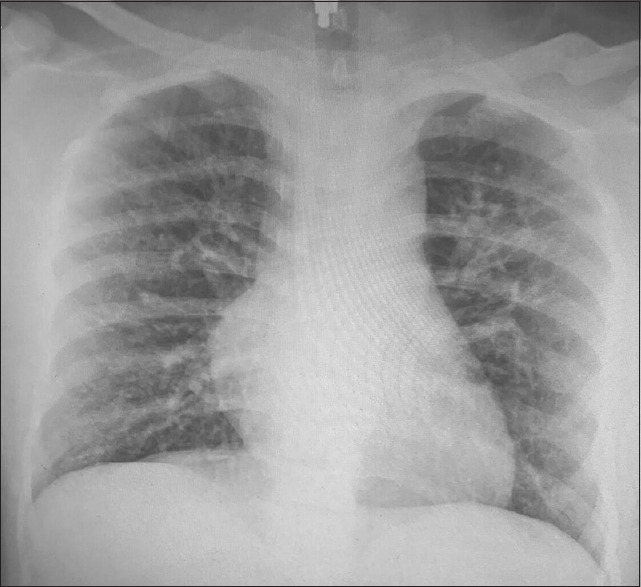
A plain radiograph of the chest showing an old consolidation
The patient was managed according to the national guidelines[6] for COVID-19. Given medication included Tab favipiravir 900 mg bid on the 1st day of admission, then 400 mg bid/day for 9 days. Tab. paracetamol 1000 mg SOS, Tab. vitamin-D 500/day, tab. calcium carbonate 500/day, and Cap. hydroxyurea 35 mg/kg/day as a patient's medication for SCD. Oxygen saturation was >95% at room air with no supplemental oxygen during his 1 week stay in hospital. The patient shifted to quarantine for a week-long, where he remained asymptomatic except for 2–3 motions on the 2nd day of quarantine. PCR test was repeated on the 14th day and was negative. The patient had an uneventful recovery.
Discussion
The current public health crisis of COVID-19, caused by severe acute respiratory syndrome corona virus-2 (SARS CoV-2) that started in the city of Wuhan (China) in late December 2019.[7] SARS CoV-2 infection severity varied greatly from asymptomatic to severe and even mortality. Despite the vulnerability of SCD patients due to their immunocompromised state and a high risk of thrombosis, a less severe course of SARS CoV-2 infection has been seen in the published literature so far. In a study conducted in Bahrain,[8] a neighboring country of Saudi Arabia that has a similar ethnic population, only six patients were SCD with concurrent SARS CoV-2 infection out of the total 378 SCD patients in the tested group. Of those confirmed cases, the disease course ranged from asymptomatic to mild. Abdulqader al-hebashi et al.[9] reported three patients of SCD with SARS CoV-2 infection from a single-family, a mother and two children. The mother remained asymptomatic while one child developed a vaso-occlusive crisis (VOC), the other got VOC and acute coronary syndrome (ACS), where all the patients showed full recovery. Another case series of four by Husain et al.[10] the common presenting symptoms were VOC, and no one had fever with no mortality seen.
The protective factors in SCD patients for SARS CoV-2 infection have yet to be determined once more evidence of the relationship between SCD and COVID-19 comes to the surface. The report of a patient with sickle cell disease with concurrent COVID-19 infection that may present with atypical symptoms will add valuable information to the family physicians and will help the family physicians to identify and manage them effectively.
Conclusion
In the current COVID-19 pandemic, primary care physicians should be aware of the atypical symptoms of SARS CoV-2 infection, especially in patients at high risk like sickle cell disease, and to follow the national guidelines and specific protocols to manage these patients in a much better way.
Key points
Sickle cell disease is a genetic disorder that affects millions worldwide.
The ongoing COVID-19 pandemic affects millions globally including patients with pre-existing conditions.
Patients with SARS CoV-2 infection may present with atypical symptoms.
Family physicians should be vigilant to screen patients with SARS CoV-2 infections, especially with chronic conditions like SCD.
Patient Consent
Written informed consent obtained from the patient for publication of the case and accompanying image.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that his names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Worldometer M. Coronavirus Update (live): 4,989,095 cases and 324, 970 deaths from COVID-19 virus pandemic – Worldometer. 2020. [[Last accessed on 2020 Oct 26]]. Available from: https://www.worldometers.info/coronavirus/#countries .
- 2.Ejaz H, Alsrhani A, Zafar A, Javed H, Junaid K, Abdalla AE, et al. COVID-19 and comorbidities: Deleterious impact on infected patients. J Infect Public Health. 2020;13:1833–9. doi: 10.1016/j.jiph.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanyaolu A, Okorie C, Marinkovic A, Patidar R, Younis K, Desai P, et al. Comorbidity and its impact on patients with COVID-19. SN Compr Clin Med. 2020;2:1069–76. doi: 10.1007/s42399-020-00363-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paudel SS. A meta-analysis of 2019 novel coronavirus patient clinical characteristics and comorbidities? Res Sq. 2020 doi: 10.21203/rs. 3.rs-21831/v1. (pre-print) [Google Scholar]
- 5.Alsaeed ES, Farhat GN, Assiri AM, Memish Z, Ahmed EM, Saeedi MY, et al. Distribution of hemoglobinopathy disorders in Saudi Arabia based on data from the Premarital Screening and Genetic Counseling Program, 20112015. J Epidemiol Glob Health. 2018;7(Suppl 1):S41–7. doi: 10.1016/j.jegh.2017.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saudi MoH protocol for patients suspected of/confirmed with COVID19 supportive care and antiviral treatment of suspected or confirmed COVID-19 infection (version 1.4), April 12th. Saudi Arabia: Ministry of Health; 2020. http://ghc.sa/ar-sa/Documents . [Google Scholar]
- 7.Liu W, Zhang Q, Chen J, Xiang R, Song H, Shu S, et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020;382:1370–1. doi: 10.1056/NEJMc2003717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.AbdulRahman A, AlAli S, Yaghi O, Shabaan M, Otoom S, Atkin SL, et al. COVID-19 and sickle cell disease in Bahrain. Int J Infect Dis. 2020;101:14–6. doi: 10.1016/j.ijid.2020.09.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Hebshi A, Zolaly M, Alshengeti A, Al Qurainees G, Yamani S, Hamdan N, et al. Pediatr Blood Cancer. 2020;67:e28547. doi: 10.1002/pbc.28547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hussain FA, Njoku FU, Saraf SL, Molokie RE, Gordeuk VR, Han J. COVID-19 infection in patients with sickle cell disease. Br J Haematol. 2020;189:851–2. doi: 10.1111/bjh.16734. [DOI] [PMC free article] [PubMed] [Google Scholar]


