Abstract
Aims and objectives:
Infection control is an essential part in dental practices. Potential disease transmission in the dental lab is well documented. Dental technicians should strictly adhere to the standard precautions in order to prevent potential risks of cross-contamination, thereby producing a safe environment for patients and staff. The aim of this study was to evaluate the knowledge, attitude, and practice among dental lab technicians toward infection control protocols at the dental laboratories of Riyadh.
Materials and methods:
A self-administered questionnaire will be distributed to dental lab technicians working at both private and governmental laboratories in Riyadh, Saudi Arabia. Data were collected from one hundred and twenty-one dental laboratory technicians.
Results:
According to the findings, only 42.9% had an infection control manual display in the dental lab, 43.8% had received infection control training courses as part of their orientation, 40.4% of the technicians had a valid hepatitis B vaccination. Dental technicians are exposed to high risk of injuries, 72.7% of respondents answered Yes, when they were asked about reporting sharp injuries to laboratory administration.
Conclusion:
There was poor compliance to infection control procedures, dental techniques are at increased risk of cross-contamination and infection, they have limited orientation and knowledge on the infection control guideline and policy.
Keywords: Dental laboratories, dental technicians, infection control
Introduction
Infection control in dental clinics and laboratories represents a main concern in recent years in relation to the perceived risk to which the professionals and patients from getting infected.[1] Before the 1970s, infection control was not performed in dental laboratories though there was a major concern on handling of items from “high-risk patients.” It was later realized that microorganisms could survive on saliva and blood and that any patient could be a source of infection.[2]
The transmission of diseases during treatment can occur if preventive measures are not taken. The risk of cross-contamination in dental clinics as well as transmission of microorganisms in prosthetic laboratories has been reported in various studies.[3]
The centers for disease control define standard precautions as “any standard of care designed to protect health care personnel and patients from pathogens that can be spread by blood or any other bodily fluid, excretion, or secretion.”[4] Standard precautions include respiratory hygiene with cough etiquette, hand washing, sharp safety, safe injection practices, sterile instruments and devices, clean and disinfected environmental surfaces, and the use of personal protective equipment (PPE).[5]
In the laboratory, infection can be transferred from cast to the dental technician/technologist by surface contact handpieces, burs, pumice, aerosols, and unwashed hands.[6]
A similar cross-sectional study[7] was conducted in Saudi Arabia-Jeddah had concluded that cross-contamination among dental team personals is a hazardous concern and that Strict compliance with infection control protocols is mandatory in the dental clinics, as well as, in dental laboratories.
Aim of the Study
The aim of this study was to evaluate the awareness, knowledge, and attitude of dental lab technicians toward infection control protocols in the dental laboratories of Riyadh.
Materials and Methods
An electronic literature search was accomplished to identify publications related to Infection Control and Dental techniques using the databases of Saudi Digital Library (SDL), PubMed, and Google Scholar for articles published in English within the past 10 years. The following terms were used as keywords: “infection control, dental laboratories, dental technicians.” Thirty-three articles were selected. After obtaining institutional review board (IRB) approval, a cross-sectional study was conducted to obtain information regarding the awareness toward the infection control in the Dental laboratories, Riyadh, Kingdom of Saudi Arabia.
Data were gathered from dental laboratory technicians in response to a questionnaire developed by the authors. A total of 121 dental technicians were participated in the questionnaire that was distributed as a hardcopy among the target population at a university-based, as well as, commercial dental laboratories, in the city of Riyadh, Saudi Arabia. The questionnaire consisted of eight sections: The First section included the demographic data, the second section was about the laboratory information, and the other sections of the questionnaire contained questions about knowledge assessment, attitude and practice toward infection control procedures.
Result
One hundred and twenty-one Dental Technicians had participated in the study (n = 121), 51.2% (n = 62) from governmental sector and 48.7% (n = 59) from private sector. The demographic characteristic of the participants included their professional years of experience [Figure 1], gender [Figure 2], and nationality [Figure 3] of the 121 technicians coming from 17 dental laboratories in the city of Riyadh.
Figure 1.

Years of experinces
Figure 2.

Gander of perticipation
Figure 3.

Nationality of participents
According to the laboratory information, only 42.9% (n = 52) from private and governmental sectors had an infection control manual display in the dental lab, 43.8% (n = 53) had technicians receive infection control training courses as part of their orientation, 32.2% (n = 39) had reported periodical onsite infection control training, 32.2% (n = 39)% reported the presence of infection control coordinator at the laboratory, and 25.6% (n = 31) of included technicians had reported that they are not acquainted of any infection control protocols in the laboratories.
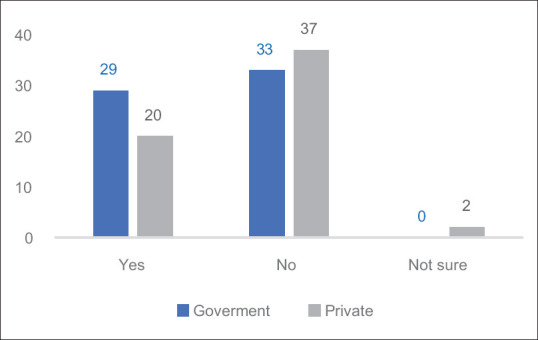
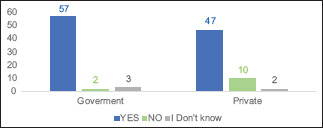
According to the findings from participant's information 40.4% (n = 49) of the laboratory's technicians had a valid hepatitis B vaccination [Figure 4]. Only 48.7% (n = 59) of the Dental laboratories had required employees to submit a valid hepatitis B vaccination record [Figure 5] 61.0% of the collected laboratory information had reported availability of Occupational hazards management policy and procedures, 57% had answered with Yes when they were asked if their technicians are aware of occupational hazards management policy and procedures.
Figure 4.
A valid hepatitis B vaccination
Figure 5.

A valid hepatitis B records
3.1 Knowledge Assessment Questions between the Government and Private Sector of the Laboratory Technicians Demonstrated the following:

1.1. Personal protective equipment is mandatory for all laboratory tasks?
1.2. Wearing face mask/ shield and eye protection is mandatory when operating rotatory equipment?

1.3. Maintaining infection control standard practices is essential to mitigate the risk for cross-infection?
1.4. Packing materials should be discarded to?

1.5. Delivery bags should be labeled with type of disinfectant and date of disinfection?

1.6. Alternative method for spraying?
5.2 Moving to the laboratory technicians attitude assessment toward infection control, result showed the following:
| Questions | |||
| 2.1. Personnel working at receiving area wear a clean uniform or laboratory coat, face mask, protective eyewear, and disposable gloves | Yes 65% (n=79) | No 13.2% (n=16) | Maybe 21.4% (n=26) |
| 2.2. Personnel working in the receiving area remove personal protective equipment before moving to an uncontaminated area of the lab | Yes 66.9% (n=81) | No 19% (n=23) | Maybe 14% (n=17) |
| 2.3. Incoming items that were not labeled as disinfected should be carefully unpacked in aseptic manner and which of the following: | 35.5% (n=43) should be washed under running water | 36.3% (n=44) should be immersed in sodium hypochlorite disinfecting solution | 28% (n=34) answers with (cleaned and disinfected with tuberculocidal disinfectant) |
| 2.4. New work or repair is performed at | 26.4% (n=32) answers with (Receiving area) | 72.7% (n=88) answers with (Production area) | 0.8% (n=1) answers with (Shipping area) |
| 2.5. Used plastic impression trays are | 78.5% (n=95) answers with (Discarded) | 16.5% (n=20) answers with (Disinfected) | 4.9% (n=6) answers with (Washed) |
| 2.6. Technicians report sharp injuries to laboratory administration | 72.7% (n=88) answers with Yes | 14% (n=17) answers with No | 13.2% (n=16) answers with Maybe |
| 2.7. Occupational health clinics are available to receive technicians exposed to injuries as result of handling lab work | 50.4% (n=61) answers with Yes | 15.7% (n=19) answers with No | 33.8% (n=41) answers with Maybe |
| 2.8. Impassions/casts are disinfected prior to CAD/CAM scanning | 54.5% (n=66) answers with Yes | 26.4% (n=32) answers with No | 19% (n=23) answers with Maybe |
5.3 Dental laboratory technicians Practice assessment had evaluated their Occupational Risks through the following questions:

5.3.1. When operating model trimmers personnel wear face mask/ shield and eye protection

5.3.2. When operating rotating equipment personnel wear face

5.3.3. Countertops and work surfaces at receiving area are:

5.3.4. Disinfected acrylic items stored and shipped in sealed plastic bag containing:

5.3.5. In order to reduce the risk of cross-infection, handling face bows and articulator are covered with:

5.3.6. Spray-wipe-spray method with phenolics or iodophors can be used for:
Discussion
Primary care physicians hold a strategic position in delivering preventive services. They must take the initiative and seek prevention rather than intervention methods. There is growing concern about the issue of cross-infection, but only a few studies carried out so far which had focused on the issues of controlling cross-infection in Dental laboratories. With enough research, primary care able to provide a trusting environment that forms a strong base for making optimal decisions to promote patient health.
The use of effective infection control procedures in the dental office and the dental laboratory will prevent cross-contamination that may extend to dentists, dental office staff, dental technicians, and patients.[8,9] Successful practice of infection control depends on the ability to understand the need for this dynamic concept with the proper implication of method and knowledge.[9]
For this purpose, the dental profession specifying Dental laboratories in Riyadh has been expected to meet traditional standards of cross-infection control, by following MOH guidelines.[8] To prevent the transmission of the infectious organism, and to have the best quality of work.
This is the first study conducted to assess the Knowledge attitude and practice of dental technicians working in dental laboratories for the government and private sectors in Riyadh. The response rate to the questionnaire in this study was high, this high rate is presumably due to the importance of the issue, infection in dental laboratories, and because technicians recognize that dental laboratories are as important as dental clinics in following infection control programs. All dental laboratories pose certain risks for cross-contamination of infectious diseases common to dentistry, the dental laboratory personnel (owners and employees) have the moral and legal responsibility to prevent cross-contamination via the dental laboratory.[10]
Technicians compliance to infection control could be a growing issue. A study conducted in Jeddah Saudi Arabia[7] highlighted several potential sources of cross-contamination in the dental laboratory, which were proven to be highly infectious, yet this study showed low compliance rate in these areas with infection control protocols recommended.[7] Similar study was conducted in Jorden.[11] Infection control in commercial laboratories in Jordan were investigated because these facilities often lack hazard risk instructions or occupational health policies that are more commonly available in Jorden universities and hospitals, thus suggesting that there is lack of compliance with infection control procedures of dental technicians working in commercial laboratories.[11] Another study conducted in Brazil[12] clearly showed that although most of dental technicians are aware that dental works may be potential sources of spreading pathogenic microorganisms, most laboratories do not adopt an infection control policy for working on prosthetic appliances and items related to them.[12]
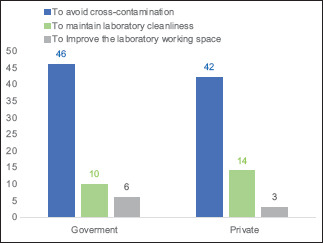
Given the result of this study, most of the technicians are aware of: wearing PPE being mandatory for all laboratory tasks, wearing face mask/shield and eye protection is mandatory when operating rotatory equipment to avoid injury and to minimize the potential for cross-contamination and disease transmission. Maintaining infection control standard practices is essential to mitigate the risk for cross-infection, and that all packing materials should be discarded As listed by MOH guidelines Laboratories Receiving area: Packing materials should be discarded to avoid cross-contamination.
Although we found that most technicians (90% of respondents) are aware of the existence of real contamination risk, 19% had responded with No when they were asked about removing PPE in the receiving area before moving to an uncontaminated area of the lab, and 47% are not aware of the barrier technique to cover instrument which poses obvious problems for sterilization such as face-bows and articulators.
According to MOH guidelines,[8] three methods are recommended to disinfect an impression, Spraying, Short-term Submersion, and Immersion Method. And as listed Short-term submersion is an alternative method to spraying. According to the knowledge assessment, most of the technicians (50% of respondents) had answered with the washing as an alternative method of spraying for disinfection. Washing is not sufficient to disinfect impression material as impression harbors infectious microorganisms the most. And they are the main sources that can potentially transfer the microorganisms from the patient's mouth to dental laboratory.[13]
On the best practice of infection control as followed by MOH Laboratories Incoming cases should be unpackaged carefully and handled in an aseptic manner. Unless the case was labeled as disinfected in the dental clinic, it should be cleaned and disinfected immediately on receipt with a MOH-registered tuberculocidal disinfectant. There was substantial nonconformity as 71.8% of respondents had chosen the other options over tuberculocidal disinfectant.
Dental technicians are exposed to a high risk of injuries; 72.7% of respondents had answers with YES, when they were asked about reporting sharp injuries to laboratory administration. Although more than half are aware of the reporting policy 33.8% are not aware of occupational health clinics to receive technicians who are exposed to injuries as result of handling lab work, and 15.7% are not provided with this service. This could be due to their limited orientations or limited resources provided.
Items that do not normally contact the mucous membranes but frequently become contaminated and cannot withstand heat-sterilization should be cleaned and disinfected between patients and according to the manufacturer's instructions. Spray-wipe spray method with phenolics or iodophors can be used for such items.[8] (62.8% of the respondent) had chosen spray-wipe spray for items that contact mucosal membrane, this could be to their misunderstanding by relating the question to impressions, or it could be due to their limited contact with the patients.
To ensure safe practice and environment for the technicians, valid hepatitis B record should be a standard policy for every technician. As Dental technicians, during their profession, contact several harmful factors.[14] According to the obtained data 40.4% (n = 49) of the participated laboratories technicians had a valid hepatitis B vaccination, and only 48.7% (n = 59) of the Dental laboratories had required employees to submit valid hepatitis B vaccination record. More than half of the participant do not have hepatitis B vaccination, Dental technician are at increased risk of accidental puncture and other types of injuries.[15] Which intern going to increase the risk of cross contamination and infection, as technicians are at risk of cross contamination.[6,9,15,16] Adding that almost half of the participated laboratories from both sectors did not require employees to submit a valid hepatitis B vaccination record, which the intern affects the quality of care provided to the employees. 1% to 62% is the risk of HBV transmission after a needle-stick, and it depends on the hepatitis B surface antigen (HBsAg) and hepatitis B e antigen status of the blood source from infected patient.[5] 1.8% is the average risk of HCV transmission.[5] For the HIV infection is only 0.3% risk after percutaneous exposure to HIV-infected blood.[5]
Supported by the Guidelines for Developing a Dental Laboratory Infection-Control Protocol by the International Journal of Prosthodontics in 1992,[10] All laboratory personnel who have not been previously vaccinated or have not had antibody testing revealing immunity should receive hepatitis B virus immunization. Additionally, immunized individuals should be tested 1 month after completing the vaccine because one person out of ten does not respond.[10] And by the Guidelines for infection control in dental health-care settings 2003,[15] Occupational Safety and Health Administration update on infection control in the dental laboratory.[17,18]
Although 61.0% of the collected laboratories information had reported availability of Occupational hazards management policy and procedures, only 57% had answered with Yes, when they were asked, if their technicians are aware of occupational hazards management policy and procedures. This emphasis on the importance of orientation to cover the aspect of care provided.
Conclusion/Recommendation
The results observed allowed the following conclusions: There was poor compliance to infection control procedures. Most participants did not have enough knowledge on proper guidelines and policies.
To sum up, all health care providers play a crucial role in prevention of the spread of cross-infection and maintain of the public health. Establishing formal and obligatory infection control courses and guidelines would mimics occupational risks. There should be a thorough inspection of the health care facilities its related laboratories.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Balcos C, Barlean M, Bobu L, Popescu E. Evaluation of infection control knowledge and attitude among dental technicians in IASI. Rom J Oral Rehabil. 2018;10:120–7. [Google Scholar]
- 2.Sammy K, Benjamin S. Infection control mechanisms employed by dental laboratories to prevent infection of their dental technicians/technologists. J Oral Health Craniofac Sci. 2016;1:1–11. [Google Scholar]
- 3.Agostinho AM, Miyoshi PR, Gnoatto N, Paranhos HF, Figueiredo LC, Salvador SL. Cross-contamination in the dental laboratory through the polishing procedure of complete dentures. Braz Dent J. 2004;15:138–43. doi: 10.1590/s0103-64402004000200010. [DOI] [PubMed] [Google Scholar]
- 4.Boyce R, Mull J. Complying with the occupational safety and health administration: Guidelines for the dental office. Dent Clin North Am. 2008;52:653–68. doi: 10.1016/j.cden.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Ajantha H, Kumar B. Infection control in the dental office-A review. Indian Journal of Dental Advancements. 2011;3(03):577–82. [Google Scholar]
- 6.Diaconu D, Vitalariu A, Tatarciuc M, Murariu A. The economic crisis effects on the cross-contamination control in dental laboratories. Rev Cercet Interv. 2014;47:105–16. [Google Scholar]
- 7.Ezzat A. Practice of cross-contamination prevention among dental laboratory technicians in the city of Jeddah in Saudi Arabia. EC Dent Sci. 2018;17:2227–38. [Google Scholar]
- 8.Moh.gov.sa. 2018. Manual of Infection Prevention & Control in Dental Settings [Google Scholar]
- 9.Nimonkar SV, Belkhode VM, Godbole SR, Nimonkar PV, Dahane T, Sathe S. Comparative evaluation of the effect of chemical disinfectants and ultraviolet disinfection on dimensional stability of the polyvinyl siloxane impressions. J Int Soc Prev Community Dent. 2019;9:152–8. doi: 10.4103/jispcd.JISPCD_406_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kimondollo PM. Guidelines for developing a dental laboratory infection-control protocol. Int J Prosthodont. 1992;5:452–6. [PubMed] [Google Scholar]
- 11.Al-Dwairi ZN. Infection control procedures in commercial dental laboratories in Jordan. J Dent Educ. 2007;71:1223–7. [PubMed] [Google Scholar]
- 12.Campanha N, Pavarina A, Vergani C, Machado A, Giampaolo E. Cross-infection control policy adopted by dental technicians. Rev Odontol UNESP. 2004;33:195–201. [Google Scholar]
- 13.Savabi O, Nejatidanesh F, Bagheri KP, Karimi L, Savabi G. Prevention of cross-contamination risk by disinfection of irreversible hydrocolloid impression materials with ozonated water. Int J Prev Med. 2018;9:37. doi: 10.4103/ijpvm.IJPVM_143_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diaconu D, Tatarciuc M, Vitalariu A. Quantitative analysis of bacterial contamination in dental laboratory air. Rom J Oral Rehabil. 2012;4:27–9. [Google Scholar]
- 15.Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, Malvitz DM Centers for Disease Control and Prevention (CDC) Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;52:1–61. [PubMed] [Google Scholar]
- 16.Salvia AC, Matilde FS, Rosa FC, Kimpara ET, Jorge AO, Balducci I, et al. Disinfection protocols to prevent cross-contamination between dental offices and prosthetic laboratories. J Infect Public Health. 2013;6:377–82. doi: 10.1016/j.jiph.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 17.Merchant V. An update on infection control in the dental laboratory. Quintessence Dent Technol. 1997;20:157–69. [Google Scholar]
- 18.Gupta, Sakshi, Rani, Sapna, Garg, Sandeep Infection control knowledge and practice: A cross-sectional survey on dental laboratories in dental institutes of North India. J Indian Prosthodont Soc. 2017;17:348–54. doi: 10.4103/jips.jips_5_17. [DOI] [PMC free article] [PubMed] [Google Scholar]


