Abstract
Background:
Diagnosis, notification and timely initiation of treatment is an important cornerstone for the elimination of tuberculosis (TB). The referral and feedback mechanism under National Tuberculosis Programme of India has been changed from paper-based to web-based electronic system (Nikshay) since 2018. The current study was carried out to assess the effect of Nikshay in referral and receipt of feedback on treatment initiation and to understand the early implementation challenges.
Methods:
A mixed-methods study was conducted in a medical college referral unit (MCRU) of Delhi, India. The electronic TB notification data for July 2018–March 2019 were abstracted from Nikshay portal and analysed. Unadjusted and adjusted relative risk (aRR) was calculated to assess the factors associated with the receipt of feedback. Themes and subthemes were generated from qualitative data obtained through key-informant interviews of healthcare providers.
Results:
Of the total 4395 patients handled by MCRU during the study period, 3315 (75.4%) were referred out within and outside Delhi for treatment. Feedback was received among 797 (24.0%) of the patients who were referred out. Patients with extrapulmonary TB (aRR: 1.3, confidence interval (CI): 1.1–1.8), previously treated (aRR: 1.2, CI: 1.2–1.3) and registered for drug-resistant TB care (aRR: 1.4, CI: 1.1–1.8), had high chance of receiving feedback. Four broad themes emerged, namely, (a) awareness of programme and Nikshay; (b) tracking of patients; (c) user-friendly portal and (d) workload.
Conclusion:
The low feedback on treatment initiation of patients with TB needs further research after health system-level quality improvement interventions. Real-time tracking of patients is the need of the hour towards the path for TB elimination.
Keywords: Disease notification, feedback, Nikshay, referral, tuberculosis
Introduction
Tuberculosis (TB) is the most common infectious cause of mortality globally.[1] It was always in the developmental agenda as part of 'Stop TB strategy' under Millennium Development Goals and 'End TB Strategy' under Sustainable Development Goals. Providing integrated, patient-centred care for all patients with TB is one of the components of END TB Strategy.[2]
Globally, more than one-third of patients with TB missed notification as estimated in 2017.[3] India, one of the high TB burden countries, also missed the notification of nearly 30% cases, which amounts to 26% of global missed cases.[3,4] The country is tackling the TB burden through its Revised National TB Control Programme (RNTCP), which covered all the districts of the country. RNTCP planned to achieve 90% and 95% treatment initiation among notified patients by 2015 and 2020, respectively, as envisaged under the National Strategic Plan for TB elimination 2017–2025.[5] However, only 79% of patients notified in the public health facilities of India were initiated on treatment in 2017. This pretreatment loss to follow-up (LTFU) varied from 0% to 84% across districts of India.[4] Factors like male sex, migration, older individual and living in urban area are found to be associated with pretreatment LTFU.[6,7] This has been reported to be high among patients diagnosed at medical colleges or tertiary care hospitals.
Medical colleges share nearly 15% of the total TB cases notified in India.[8] However, most of the patients diagnosed with TB are referred to respective district TB centres (DTCs) for the initiation, follow-up and completion of treatment, as patients seek tertiary care services from different parts of the country (both inside and outside the district and outside the state). RNTCP has established a referral mechanism by sending a 'referral for treatment' form to DTC after confirmation of diagnosis from the medical college referral units (MCRUs).[9] The MCRU receives feedback in paper-based format, which is to be filled and sent by the DTC. The reported receipt of feedback was 54%, 74% and 75% in referral units of medical colleges situated in Puducherry, Hyderabad and Delhi, respectively.[8,9,10] Status of treatment initiation could not be verified in one-fourth to half of the referred TB patients due to wrong address, wrong phone number, the treatment being initiated outside RNTCP and migration.[8]
In May 2012, the Government of India had rolled out the case-based, web-based TB notification portal (Nikshay) for digitalizing and tracking the patients with TB. One of the key features of 'Nikshay' is the generation of a unique Nikshay ID for each TB patient at the site of diagnosis, which can help in tracking the patient from diagnosis till treatment outcome. Similarly, the programme has started using Nikshay to refer out the patients to other parts of the country from the place of diagnosis. Once referred from any designated microscopy centre (DMC) after diagnosis, the DTC to which the patient is referred will receive a message with patient details (name, age, sex, and phone number including village and tehsil) in the Nikshay inbox. Treatment is initiated after verification (either patient visit or healthcare worker's visit) and the DTC will send feedback along with the date of initiation of treatment via Nikshay.[11]
The Nikshay system has been implemented in National Capital Territory of Delhi (hereafter called as Delhi) to refer out the patients with TB since April 2018. This system is expected to facilitate smooth tracking and provide feedback on treatment initiation of the patients with TB referred out from the diagnosis site. Limited information is available for India whether Nikshay has smoothened the tracking of patients with TB and strengthened the feedback mechanism. With this background, we conducted this study to assess the referral feedback mechanism among patients with drug-sensitive TB diagnosed in Maulana Azad Medical College (MAMC) and associated hospitals (Lok Nayak hospital, Govind Pallabh Pant, and Guru Nanak eye hospitals) in Delhi and referred from RNTCP MCRU in 2018-19. We also explored the challenges faced by the healthcare providers in referring out and receiving feedback about patients with TB from RNTCP MCRU of Delhi.
Methods
Study design
This was a mixed-methods study with the quantitative part being a retrospective cohort study through record review of the routinely collected programmatic data from Nikshay portal and descriptive qualitative part (key-informant interview [KII]).
Study setting
Delhi is an union territory situated in the northern part of India, and administratively, Delhi is divided into 11 districts.[12] RNTCP has been implemented in all districts of Delhi. MAMC, and its associated hospitals, is a 2800-bedded tertiary care, teaching hospital located in the central district of Delhi. It is providing outpatient services to 7500 patients per day. All patients seeking healthcare services are screened for TB based on the clinical presentation and diagnosed using either sputum microscopy/Culture/GeneXpert. All patients diagnosed with TB are referred to RNTCP MCRU for treatment initiation or referral. Admitted patients with TB are initiated on treatment and referred to MCRU for continuation or transferring out the patients. The MCRU is manned with a medical officer in charge and other supporting staffs like Senior TB Treatment Supervisor (STS), Senior TB Laboratory Supervisor (STLS), TB Health Visitor (TB-HV) and Laboratory Technician. The flow of patients diagnosed, managed/referred via MCRU of MAMC and associated hospitals of Delhi after implementation of Nikshay is given in Figure 1.
Figure 1.

Diagnosis, referral and feedback flow of patients with tuberculosis at MAMC and associated hospitals of Delhi from April 2018. MAMC: Maulana Azad Medical College and its associated hospitals; RNTCP: Revised National TB Control Programme
Study population, period, sampling and sample size
All the patients referred from the MCRU of MAMC and associated hospitals from July 1, 2018, to March 31, 2019, for treatment initiation to the health facility near their residence, were included in the study. No sampling was done. District TB officer (DTO), STS, STLS and TBHV were selected through purposive sampling and interviewed telephonically for the qualitative part.
The operational definition for receipt of feedback
Availability of date of treatment initiation or reason for noninitiation of treatment was considered as receipt of feedback irrespective of the date of update. However, one month reference period was given to patients referred on March, 2019.
Data variables, sources of data and data collection procedure
The data were downloaded from Nikshay portal provided to MAMC and associated hospitals, Delhi. District and state of residence of the patient, type of health facility (DMC, Tuberculosis Unit, DTC or others), age, sex, type of TB (pulmonary, extrapulmonary), category of TB (new, previously treated), type of health facility sending feedback, date of diagnosis, date of referral and date of treatment initiation were imported from Nikshay portal.
In order to explore the challenges faced by the healthcare providers in referring out and receiving feedback about patients with TB from MCRU, we conducted KIIs over the telephone of DTO, STS, STLS and TBHV. One of the investigators (KS) of the study, who is a faculty member and trained in qualitative research, conducted the interviews. Interviews were conducted at the convenience of the participants after explaining the purpose of the study and verbal consent using a pretested interview guide. Verbatim notes were taken during the interview. Each interview lasted for 25–30 minutes. Participant's validation was ensured by reading back the summary at the end of the interview.
Data entry and data analysis
The downloaded quantitative data in excel form were exported to Stata version 12 (Stata Corp., Texas, USA). Key analytic outputs were the number and proportion of patients referred, gender, type and category of TB, state or district (if within Delhi) of residence and type of health facility referred to and feedback received was calculated. Similarly, mean and standard deviation (median and interquartile range [IQR] if skewed) were calculated for age and interval between the date of diagnosis, referral and treatment initiation. Quantum GIS V2.18.15 was used to plot the data in India state and Delhi district maps. Factors with P < 0.2 in univariate analysis were included for generalized linear model–Poisson regression (cluster adjusted) analysis for calculation of adjusted relative risk (aRR) with a 95% confidence interval for receipt of feedback. A p value <0.05 was considered statistically significant.
Transcripts were made immediately after the key informant interviews. The transcripts obtained were compiled by KS. KS and SK read the transcripts to become familiar with the data. KS did the descriptive content analysis manually, and SK reviewed the same to reduce bias and ensure interpreter credibility.[13,14] Following standard procedures and in consensus, the coding rules and theme generation were decided.[15] Both inductive and deductive codes were generated. Themes were created, combining similar codes.[13] The codes/themes were related back to the original data to ensure real reflection.[16] The findings were reported using 'Consolidated Criteria for Reporting Qualitative Research (COREQ Guidelines)'.[17]
Ethics approval
Ethics approval was obtained from MAMC Hospital, Delhi, and Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France. Informed consent was waived for the quantitative part of the study since it is record-based. Verbal informed consent was obtained for the KIIs. Administrative approval for the study was obtained from the State TB Office, Delhi.
Results
A total of 4395 patients reached the MCRU from July 2018 to March 2019 for registration with Nikshay and/or for initiation of treatment. Of them, 3315 (75.4%) patients were referred out to their nearby peripheral health institutes (PHIs) for treatment initiation after the creation of Nikshay ID [Table 1].
Table 1.
Demographic, clinical and feedback characteristics of patients with tuberculosis referred through Nikshay portal from a medical college referral unit of Delhi, July 2018-March 2019
| Characteristics | Total | Referred out | p | ||
|---|---|---|---|---|---|
| n | (%)a | n | (%)b | ||
| Total | 4395 | 3315 | (75.4%) | ||
| Age group (in years) | |||||
| <14 | 521 | (11.9) | 408 | (12.3) | 0.396 |
| 14-44 | 2948 | (67.1) | 2209 | (66.7) | |
| 45-64 | 739 | (16.8) | 559 | (16.9) | |
| ≥65 | 184 | (4.2) | 136 | (3.1) | |
| Not recorded | 3 | (<0.1) | 3 | (0.1) | |
| Gender | |||||
| Male | 2165 | (49.3) | 1615 | (48.7) | 0.213 |
| Female | 2224 | (50.6) | 1695 | (51.1) | |
| Others | 6 | (0.1) | 5 | (0.2) | |
| HIV status | |||||
| Reactive | 27 | (0.6) | 10 | (0.3) | <0.001 |
| Nonreactive | 980 | (22.3) | 393 | (11.9) | |
| Unknown | 2865 | (65.2) | 2574 | (77.6) | |
| Not recorded | 523 | (11.9) | 338 | (10.2) | |
| Site of tuberculosis | |||||
| Pulmonary | 1208 | (27.5) | 646 | (19.5) | 0.818 |
| Extra pulmonary | 761 | (17.3) | 411 | (12.4) | |
| Not recorded | 2426 | (55.2) | 2258 | (68.1) | |
| Type of tuberculosis | |||||
| New | 3282 | (74.7) | 2383 | (71.9) | <0.001 |
| Previously treated | 326 | (8.7) | 189 | (7.1) | |
| Failure | 4 | (0.1) | 0 | (0) | |
| Lost to follow-up | 8 | (0.2) | 4 | (0.1) | |
| Relapse | 96 | (2.2) | 20 | (0.6) | |
| Others | 218 | (5.0) | 165 | (5.0) | |
| PMDTc | 128 | (2.9) | 89 | (2.7) | |
| Not recorded | 659 | (15.0) | 654 | (19.7) | |
| Drug resistance | |||||
| Resistant | 242 | (5.5) | 188 | (77.7) | <0.001 |
| Sensitive | 976 | (22.2) | 787 | (80.6) | |
| Unknown | 3134 | (71.3) | 2339 | (74.6) | |
| Not recorded | 43 | (1.0) | 1 | (2.3) | |
| Feedback receipt | |||||
| Yes | 1710 | (38.9) | 797 | (24) | <0.001 |
| No | 2685 | (61.1) | 2518 | (76) | |
| Median duration (days) pretreatment delay (interquartile range)d | 4 | (1, 10) | 7 | (3, 14) | <0.001 |
aColumn percentage; brow percentage; cprogrammatic management of drug resistant TB; damong feedback received, treatment was not initiated among 52 and 40 patients in all patients and those who were referred out, respectively. For median duration calculation, valid dates were available for 1563 and 754 patients in all cases and among referred out cases, respectively
Characteristics of patients referred out
Of the patients with TB who were referred out, 2209 (66.7%) were in the age group of 14–44 years; 1695 (51.1%) were females; 2574 (77.6%) patient's HIV status was not known; 646 (19.5%) had pulmonary TB; 2383 (71.9%) were categorized under 'New treatment' category. There was a significant difference (P < 0.05) observed between those who were referred out and treatment initiated in terms of HIV status, type of TB and drug resistance [Table 1]. Feedback was received for 795 (24%) of the 3315 patients with TB who were referred out. Median (IQR) pretreatment delay was 7 (3,14) days among those patients who were referred out. The same for patients referred within the central district of Delhi, outside the central district but within Delhi and outside Delhi was 6 (0,12), 6 (2,13) and 10 (5,18) days, respectively (data not tabulated).
Treatment was not initiated among 40 (5%) patients referred out for treatment due to following reasons, namely, migrated from the current address (14), duplicate record (11), wrong address (10), death (3), and refusal for treatment initiation(2).
Characteristics of patients whose feedback was received
The receipt of feedback was higher among (a) female (24.4%) compared to male (23.5%), (b) HIV negative (85%) compared to HIV positive (50%), (c) patients with extrapulmonary TB (100%) compared to pulmonary TB (53.3%) and (d) previously treated (46.0%) and patients registered under Programmatic Management of Drug-Resistant Tuberculosis (PMDT) (100%) compared to new patients (25.6%) [Table 2]. On adjusted analysis, the receipt of feedback was significantly high among (a) patients with extrapulmonary TB (aRR: 1.3; 95% confidence interval (95% CI) 1.1–1.8) compared to patients with pulmonary TB and (b) previously treated (aRR: 1.2; 95% CI: 1.2–1.3) and patients registered under programmatic management of drug-resistant TB-PMDT (aRR: 1.4; 95% CI: 1.1–1.8).
Table 2.
Demographic and clinical factors associated with receipt of feedback about patients with tuberculosis referred out through Nikshay portal from a RNTCP medical college referral unit of Delhi, July 2018-March 2019
| Characteristics | Total referred | Received feedback | Unadjusted RR (95% CI) | Adjusted RRc (95% CI) | ||
|---|---|---|---|---|---|---|
| n | (%)a | n | (%)b | |||
| Total | 3315 | 797 | (24) | |||
| Age group (in years) | ||||||
| <14 | 408 | (12.3) | 101 | (24.8) | 0.9 (0.8-1.0) | Not included |
| 14-44 | 2209 | (66.7) | 533 | (24.1) | Ref. | |
| 45-64 | 559 | (16.9) | 137 | (24.5) | 1.0 (0.9-1.1) | |
| ≥65 | 139 | (4.1) | 26 | (19.1) | 0.9 (0.7-1.1) | |
| Gender | ||||||
| Male | 1615 | (48.7) | 380 | (23.5) | Ref. | Not included |
| Female | 1695 | (51.1) | 414 | (24.4) | 1.0 (0.9-1.0) | |
| Others | 5 | (0.2) | 3 | (60.0) | ||
| Place of treatment facility | ||||||
| Within central district of Delhi | 343 | (10.3) | 92 | (26.8) | 1.2 (1.0-1.5) | Not included |
| Other districts of Delhi | 2028 | (61.2) | 445 | (21.9) | Ref. | |
| Other states | 944 | (28.5) | 260 | (27.5) | 1.3 (1.1-1.4) | |
| HIV status | ||||||
| Reactive | 10 | (0.3) | 5 | (50.0) | Ref. | Ref. |
| Nonreactive | 393 | (11.9) | 334 | (85.0) | 1.2 (1.0-1.4) | 1.1 (0.9-1.2) |
| Unknown | 2574 | (77.6) | 156 | (6.1) | 0.1 (0.1-0.2) | 0.6 (0.5-0.7) |
| Not recorded | 338 | (10.2) | 302 | (89.3) | ||
| Site of tuberculosis | ||||||
| Pulmonary | 646 | (19.5) | 344 | (53.3) | Ref. | Ref. |
| Extrapulmonary | 411 | (12.4) | 411 | (100) | 1.4 (1.4-1.5) | 1.3 (1.1-1.8) |
| Not recorded | 2258 | (68.1) | 42 | (1.9) | ||
| Type of tuberculosis | ||||||
| New | 2383 | (71.9) | 609 | (25.6) | Ref | Ref |
| Previously treated | 189 | (5.7) | 87 | (46.0) | 2.5 (2.4-2.6) | 1.2 (1.2-1.3) |
| Lost to follow-up | 4 | (0.1) | 4 | (100) | ||
| Relapse | 20 | (0.6) | 20 | (100) | ||
| Others | 165 | (5.0) | 63 | (38.2) | ||
| PMDT | 89 | (2.7) | 89 | (100) | 2.5 (2.4-2.6) | 1.4 (1.1-1.8) |
| Not recorded | 654 | (19.7) | 12 | (1.8) | ||
| Drug resistance | ||||||
| Sensitive | 787 | (23.7) | 126 | (16.0) | Ref. | Ref. |
| Resistant | 188 | (5.7) | 106 | (56.4) | 2.4 (2.1-2.8) | 1.0 (0.9-1.2) |
| Unknown | 2339 | (70.6) | 564 | (4.1) | 1.6 (1.4-1.7) | 0.8 (0.8-0.9) |
| Not recorded | 1 | (<0.1) | 1 | (100) | ||
aColumn percentage; brow percentage; c1198 cases included for adjusted analysis; dplace of treatment facility is not included in the adjusted analysis as the total number reduced to 537 from 1198
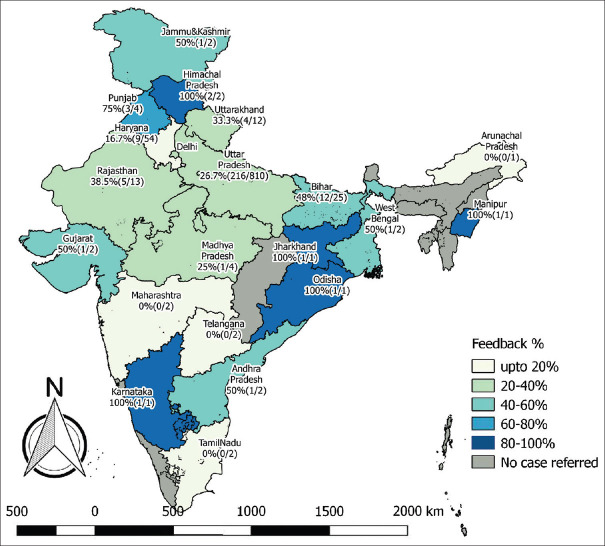
Receipt of feedback for patients referred out to other states, outside the central district of Delhi and within the central district of Delhi was 27.5%, 21.9% and 26.8%, respectively. The state-wise status of patients referred out from the MCRU and receipt of feedback has been depicted in Figure 2. The district-wise distribution of the same within Delhi is given in Figure 3.
Figure 2.
Status of receipt of feedback about patients with tuberculosis referred out through Nikshay portal from a medical college referral unit of Delhi to other states of India from July 2018 to March 2019
Figure 3.

Status of receipt of feedback about patients with tuberculosis referred out through Nikshay portal from a medical college referral unit in central district to within and outside districts of Delhi, July 2018–March 2019
Challenges faced by the healthcare providers in referring out and receiving feedback and suggested solutions for improvement
In-depth interviews were conducted to explore the perception and challenges faced by the healthcare providers in referring out and receiving feedback through Nikshay among five senior and middle-level managers of the MCRU involved in treatment initiation or referral of patients. As per their response, the patient load for the MCRU was 400–500 per month. Of them, 70% of the diagnosed patients were referred out for treatment, while feedback was obtained for 80% of those who were referred to as perceived by a senior programme manager. The emerged broad themes were (a) awareness of the programme and Nikshay, (b) tracking of patients, (c) user-friendly portal and (d) workload. The subthemes and the respective verbatims are given in Table 3.
Table 3.
Challenges perceived by healthcare providers in referring out and receiving feedback through Nikshay portal about patients with TB at a medical college referral unit of Delhi, India
| Themes | Codes | Verbatim |
|---|---|---|
| Awareness of programme and Nikshay | Low awareness about the programme | “As this is a medical college hospital, the patient load is very high. In addition, the doctors are also changing frequently due to which some patients are directly asked to visit their nearby health facility as they are not aware or forget due to high load of patients. But Nikshay ID has been created with us and we refer them without patients presence” |
| “The information written in the treatment card is minimal for entering in our system and referring out. We sometimes go back to the doctor and fill the complete details though we are also busy with our own responsibility” | ||
| Low awareness about the portal | “Initially, we were also confused what and where to enter in case of wrong address in the portal” | |
| “Though we were trained on Nikshay, the refresher training on the new portal is pending due to which we don’t know all the options available in the portal” | ||
| “Sometimes, we are afraid to operate the technology” | ||
| “No one teaches how to use the downloaded notification data” | ||
| Tracking of patients | Ascertain correct address and referral | “Patient provide local address of their relatives or wrong address. Confirmation of their address is a big task and it is consuming lot of time of ours” |
| “Sometimes due to high load, we don’t reconfirm the address from the patient. We just take the address from the treatment card” | ||
| “We see a lot of migrant population and it is quite difficult to ascertain their address and track them” | ||
| “Through this (Nikshay) almost 90% of the referral feedback was received. Ten percent problem in getting feedback was due to wrong address being given by the patients” | ||
| Duplication and hospital shopping | “Second time diagnosis of TB is not accepted by patients and mostly patients from nearby states visit here for diagnosis” | |
| “The STS of the referred out centre sometimes don’t provide feedback as the patient may be already diagnosed there and provided Nikshay” | ||
| “Patients are getting diagnosed for TB from various departments both at inpatients and outpatients. Sometimes same patient is diagnosed for TB at different departments and started on treatment simultaneously” | ||
| User-friendly portal | Complicated and non-user-friendly portal | “Not able to operate in our tablet” |
| “I have to fill the notification and treatment details which has to be filled by the STS” | ||
| “We used to wait for hours to just open the portal in initial days. Now that issue has been sorted out” | ||
| Multimodal use | “Can it be used in our mobile phone?” | |
| “It should be made more simpler to make me understand” | ||
| Adoption of new technology | “Initially we used to get feedback through post or phone call. No one is taking feedback (now). At personal level, no one is doing this. Otherwise it will take time for full use of Niksahy” | |
| Instant intimation of new patient | “We get immediate message when we transfer money via internet banking. Why can’t we get a message like this” | |
| “Currently no message/information comes if patient is initiated on treatment; only the name gets deleted. There should be a message or mail sent which says that 8/10 of your patients have been received and started on treatment” | ||
| “In the earlier version, a blinking message used to come everytime we open the portal which is not there in the current version” | ||
| Workload | Number of new initiatives | “There are lot of new initiatives like daily regimen, DBT, 99 DOTS, DST for all in recent days due to which we are getting less time for field” |
| Reducing the backlog | “Nikshay is going good. Only thing is the backlog should be cleared” | |
| “Don’t burden us with the backlog and start all new initiatives from effective dates” |
Discussion
The current study assessed the Nikshay, the case-based, web-based electronic system in referral and obtaining feedback on treatment initiation of patients with TB across the states of India. Nearly three-fourths of the patients were referred out from the MCRU for treatment initiation to other peripheral health institutes. However, the feedback on treatment initiation was updated only for one-fourth of the referred patients. Receipt of feedback was significantly high among patients with extrapulmonary TB compared to pulmonary TB, and previously treated and patients registered under PMDT compared to New TB. Though Nikshay is being used for notification and referring outpatients for the past one year, there are human and technology-related issues in identification and referral of patients and updating the referral feedback in the study setting.
The study had the following strengths. This is the first study which assessed the Nikshay for referral feedback mechanism, a government-owned electronic portal. Nikshay has been rolled out in all districts of the country with the aim of reaching the notification target of 3.5 million TB patients annually. The current study provided a number of important insights for policy and practice change, especially linking (back referral) the tertiary and primary healthcare system. The programmatic nature of the data reflects the field reality. The study included all the referred patients in the study period and assessed the factors related to receipt of feedback. The mixed-methods study design is an important strength of the study which explored the challenges and suggested solutions from the users qualitatively.
Feedback on treatment initiation was received for one-fourth of the referred patients. This percentage was lower than the reported referral linkage from medical colleges situated in Hyderabad (74%), Delhi (72.6%) and Puducherry (42.3%), respectively.[89,10] This could be due to fear of use and early stage of the implementation of the technology-based feedback system in our study compared to conventional feedback mechanisms like telephone, postcard and referral for treatment card and use of more than one conventional feedback mechanisms in other studies. Similar assessment done in Yemen, Indonesia, Cambodia and Pakistan reported 88.8%, 81.2%, 64.4% and 45% feedback rate, respectively.[18,19,20,21] Interestingly, low feedback rate reported from Pakistan could be linked with the use of new electronic TB referral/transfer register, which is similar to our study in the uptake of any new health systems intervention.[21]
The telephone was the main mode of feedback in Cambodia (97%), Delhi (78.1%) and Pakistan (69%).[9,20,21] However, the patient data updating is done separately in case of telephone or any other conventional feedback mechanism. In our case, the feedback is updated directly in the integrated electronic database for each patient. Further, it provides all the information about a patient comprehensively and instantly. There is a need to train and orient the users appropriately and adequately for efficient use since there are several changes in the Nikshay and the programme recently. The suggested solutions (from our study) to improve the feedback are, namely, (a) receipt of a message to the STS whenever a patient is referred to his area, (b) retaining some good features of Nikshay version 1 (colour-tagged blinking message on referred-in patients) and (c) permission to use in different devices.
The assumption of good feedback rate (~80%) by the senior programme manager cannot be criticized as it remained high using the conventional system as reported from another MCRU in Delhi.[9] However, it reflected the complete trust on the team and established feedback mechanism which should be reviewed periodically at least once in a month at MCRU level. The qualitative results also highlight the technical and operational issues of the shift from 'Hard copies to software', 'lack of familiarity with the software', 'technological issues' and 'increased workload of managing both the soft as well as hard copies'.[22]
As per the RNTCP guidelines, the treatment should be started within seven days of diagnosis.[8] We found that the median (IQR) duration for treatment initiation was 7 (3, 14) days for all referred patients in our study. The median pretreatment delay was higher among patients referred outside Delhi though 86% of patients were referred to Uttar Pradesh which is an adjoining state to Delhi. Further, the feedback should be updated to referral unit within seven days in case of the same district and within one month if referred outside the district or state. However, we were not able to assess the date of receipt of feedback as there is no variable available in Nikshay and due to retrospective record review design of the study.
The interpretation of the study results should be made with caution considering the following limitations. We did not verify the treatment status of the patients for whom the feedback was not received. However, the programme staff (STS or TBHV) of the respective referred centres were supposed to reach out to the patients, initiate the treatment and update Nikshay. Programme staff of respective PHI or patients can be contacted to verify the linkage and initiation of treatment as part of future operational research to validate the of referrals made through Nikshay.
The proportion of missing data in this study for the site of TB, type of TB and HIV status was 55.2%, 15% and 11.9%, which may affect the interpretation of the adjusted analysis. We did not carry out any advanced analysis to adjust for the missing data as the programme managers will not carry out such analysis in day-to-day practice for policy/practice change. It is important to report the programmatic data as it is available for assessment of completeness and timeliness, which reflects the early implementation challenges. It is also useful to understand and decide on the necessary enhancements needed in the Nikshay portal.
The referral of patients in the public health system of India always remained unidirectional, that is from primary to secondary or tertiary care hospitals. The Nikshay referral system is one of the important examples of back referral to the primary healthcare system after diagnosis or initial management at a higher level centre.[23] Though healthcare providers are accountable for tracking and initiating the treatment of the referred patients, the role of primary care physicians is not defined. The knowledge and skills of primary care physicians on the management of TB will improve directly or indirectly through the back referral of the cases. Further, forward referral for advanced diagnostics can be made from the primary care level to a higher level using the Nikshay system.
The study found low-level feedback on treatment initiation for patients referred within and outside states. The low feedback among pulmonary TB needs further research and immediate action. A relook in the standard operating procedures and periodic review of patients referred between institutes is the need of the hour. Considering the early stage of implementation of Niksay, the programme needs a series of health system-level quality improvement interventions. The user-friendliness of the Niksay interface can be improved by ensuring the suggested enhancements in the current study.
Financial support and sponsorship
The training course under which this research was conducted, and open-access publication charges was funded by, The Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM). No funding was obtained to conduct the study. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
This research was conducted as a part of the 'National Operational Research Training Course 2018–19' organized by Project Axshya, funded by The Global Fund and implemented by The International Union Against Tuberculosis and Lung Diseases (The Union), South-East Asia Regional Office, New Delhi, India. The training course was conducted in collaboration with RNTCP, Ministry of Health and Family Welfare, Government of India and National Institute for TB and Respiratory Diseases, New Delhi, India.
The training is based on “The Union/Medécins sans Frontières (MSF)” model OR course and has been acknowledged/accredited by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR) under SORT IT (Structured Operational Research and Training Initiative). Mentorship and facilitation for this course were provided through The Union South-East Asia Office, New Delhi; the Centre for Operational Research, The Union, Paris, France; Baroda Medical College, Vadodara; AIIMS, Nagpur; Médecins Sans Frontières, New Delhi; ESIC Medical College and PGIMSR, Bengaluru; Hindurao Hospital and Medical College, New Delhi; GMERS Medical College, Vadodara; Postgraduate Institute of Medical Education and Research, Chandigarh, India; Yenapoya Medical College, Mangalore.
References
- 1.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators T. Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211–59. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Global strategy and targets for tuberculosis prevention, care and control after 2015-Report by the Secretariat [Internet] 2013. [[cited 2018 Aug 25]]. p. 23. Available from: http://apps.who.int/gb/ebwha/pdf_files/EB134/B134_12-en.pdf .
- 3.World Health Organization. Global Tuberculosis Report 2018 [Internet]. WHO. World Health Organization. 2018. [[cited 2018 Aug 24]]. p. 277. Available from: https://www.who.int/tb/publications/global_report/en/
- 4.Ministry of Health and Family Welfare Government of India. TB India Report 2018 Revised National Tuberculosis Control Programme Annual Status Report [Internet] New Delhi: 2018. [[cited 2018 Aug 24]]. p. 176. Available from: https://tbcindia.gov.in/showfile.php?lid=3314 . [Google Scholar]
- 5.Purty AJ. Detect-treat-prevent-build: Strategy for TB elimination in India by 2025. Indian J Community Med. 2018;43:1–4. doi: 10.4103/ijcm.IJCM_321_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.MacPherson P, Houben RM, Glynn JR, Corbett EL, Kranzer K. Pre-treatment loss to follow-up in tuberculosis patients in low- and lower-middle-income countries and high-burden countries: A systematic review and meta-analysis. Bull World Health Organ. 2014;92:126–38. doi: 10.2471/BLT.13.124800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas BE, Subbaraman R, Sellappan S, Suresh C, Lavanya J, Lincy S, et al. Pretreatment loss to follow-up of tuberculosis patients in Chennai, India: A cohort study with implications for health systems strengthening. BMC Infect Dis. 2018;18:142. doi: 10.1186/s12879-018-3039-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chauhan RC, Purty AJ, Singh Z. Notified or missed cases.An assessment of successful linkage for referred tuberculosis patients in South India? Community Acquir Infect. 2015;2:137–41. [Google Scholar]
- 9.Khandekar J, Acharya AS, R TH, Sharma A. Do patients with tuberculosis referred from a tertiary care referral centre reach their peripheral health institution? Natl Med J India. 2013;26:332–4. [PubMed] [Google Scholar]
- 10.Kondapaka KK, Prasad SV, Satyanarayana S, Kandi S, Zachariah R, Harries AD, et al. Are tuberculosis patients in a tertiary care hospital in Hyderabad, India being managed according to national guidelines? PLoS One. 2012;7:e30281. doi: 10.1371/journal.pone.0030281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Revised National Tuberculosis Control Programme Ministry of Health and Family Welfare Government of India. NIKSHAY- A web based solution for monitoring of TB patients [Internet] [[cited 2018 Aug 24]]. Available from: https://nikshay.gov.in/AboutNikshay.htm .
- 12.Delhi Govt Portal: Home [Internet] [[cited 2018 Aug 24]]. Available from: http://delhi.gov.in/wps/wcm/connect/doit/Delhi+Govt/Delhi+Home .
- 13.Creswell J, Plano Clark V. Designing and Conducting Mixed Methods Research. London (United Kingdom): Sage Publications Ltd. 2007:142–5. [Google Scholar]
- 14.Kvale S. Doing Interviews. London (United Kingdom): SAGE Publications; 2007. [Google Scholar]
- 15.Saldana J. The Coding Manual for Qualitative Research. Los Angeles, CA, USA: SAGE Publications; 2010. [Google Scholar]
- 16.Lincoln YS, Guba EG. Naturalistic Inquiry. New York, NY, USA: SAGE Publications, Inc; 1985. p. 416. [Google Scholar]
- 17.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 18.Al-Hammady A, Ohkado A, Masui T, Al-Absi A. A survey on the referral of tuberculosis patients at the National Tuberculosis Institute, Yemen. Int J Tuberc Lung Dis. 2007;11:928–30. [PubMed] [Google Scholar]
- 19.Irawati SR, Basri C, Arias MS, Prihatini S, Rintiswati N, Voskens J, et al. Hospital DOTS linkage in Indonesia: A model for DOTS expansion into government and private hospitals. Int J Tuberc Lung Dis. 2007;11:33–9. [PubMed] [Google Scholar]
- 20.Choun K, Achanta S, Naik B, Tripathy JP, Thai S, Lorent N, et al. Using mobile phones to ensure that referred tuberculosis patients reach their treatment facilities: A call that makes a difference. BMC Health Serv Res. 2017;17:575. doi: 10.1186/s12913-017-2511-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Badar D, Ohkado A, Naeem M, Khurshid-Ul-Zaman S, Tsukamoto M. Strengthening tuberculosis patient referral mechanisms among health facilities in Punjab, Pakistan. Int J Tuberc Lung Dis. 2011;15:1362–6. doi: 10.5588/ijtld.10.0620. [DOI] [PubMed] [Google Scholar]
- 22.Dey S, Rao AP, Kumar A, Narayanan P. Awareness & utilization of NIKSHAY and perceived barriers for tuberculosis case notification among the private practitioners in Udupi district, Karnataka. Indian J Tuberc. 2020;67:15–9. doi: 10.1016/j.ijtb.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 23.Odayar J, Myer L. Transfer of primary care patients receiving chronic care: The next step in the continuum of care. Int Health. 2019;11:432–9. doi: 10.1093/inthealth/ihz014. [DOI] [PMC free article] [PubMed] [Google Scholar]