The coronavirus disease of 2019 (COVID-19) has created unprecedented challenges to health care. In the spring of 2020, elective procedures were postponed for various specialties to decrease potential exposures and allow resource reallocation.1 As health systems resume elective procedures, we face a new challenge—patient fear. Two-fifths of US adults report avoiding or delaying medical care out of concern for COVID-19.2 Although current literature suggests that rates of hospital-acquired COVID-19 are low, little is known about the risk to patients undergoing same day or hospital-based procedures.3,4 In this study, we investigated the rate of postprocedural COVID-19, and we hypothesized that it would be low.
Methods
We conducted a retrospective cohort study of all adult cases of same day or hospital-based procedures at the University of Miami Hospital and Clinics from April 1 to September 23, 2020, who were negative by severe acute respiratory coronavirus virus 2 (SARS-CoV-2) polymerase chain reaction (PCR) swab testing within 72 hours before the procedure, had contact with our health system 5–14 days after the procedure, and were either screened for COVID-19 symptoms or were tested for SARS-CoV-2 during this contact. This 5–14-day time frame was selected because the median time to symptom onset after exposure is 5 days and 99% of people who exhibit symptoms are symptomatic by 14 days.5
Cases were identified from the electronic health record and included all procedures that were completed during the study period. Case-specific data, results of all tests, and answers to symptom screens (intended to be performed at each health system contact) were also obtained from the electronic health record. Standard summary statistics were used to describe cohort characteristics and postprocedural symptom screening and testing outcomes. Among cases who were both screened and tested, we evaluated the accuracy of symptom screening for test positivity. Finally, for those cases who had symptoms on screening but were never tested within our system, we performed a qualitative chart review to understand the circumstances. This study was approved by the University of Miami Institutional Review Board (no. 20200739).
Results
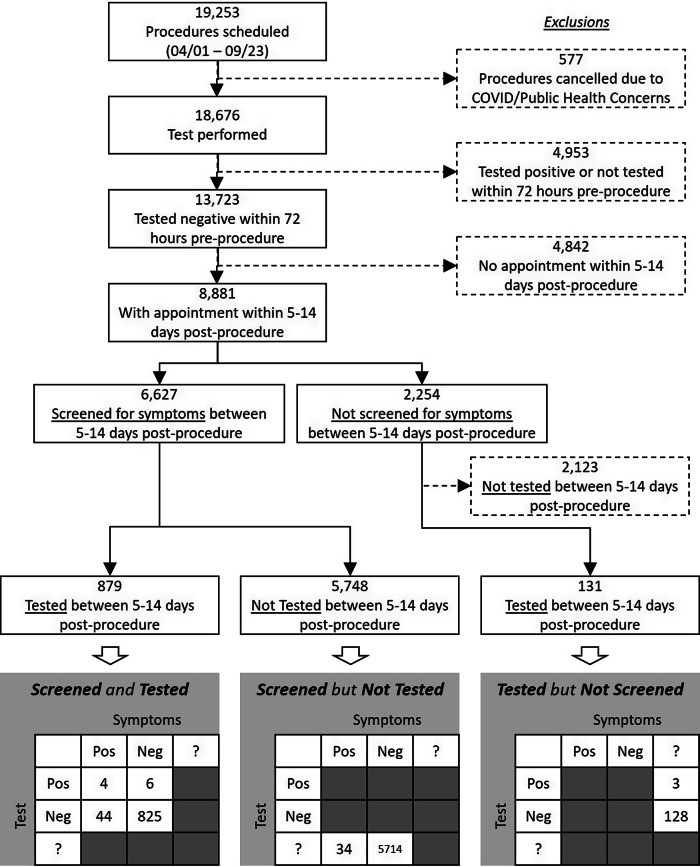
The cohort consisted of 8,881 preprocedure COVID-19–negative cases, of whom 879 (9.9%) were both screened for symptoms and tested for SARS-CoV-2 within 5–14 days after the procedure. Moreover, 5,748 (64.7%) were screened but not tested and 131 (1.5%) were tested but not screened (Fig. 1 and Supplementary Table 1 online).
Fig. 1.
Cohort flow diagram with symptom screen and testing results. Note. Neg, negative; Pos, positive; ?, unknown.
Overall, 82 postprocedure screens (1.2% of screens) revealed COVID-19–associated symptoms (including 48 cases who were tested and 34 who were not) and 13 tests (1.3% of tests) were positive. Furthermore, 91 (1.0% of all cases) had either symptoms or a test consistent with COVID-19. A positive symptom screen was only 40.0% sensitive but 94.9% specific for a positive SARS-CoV-2 test, with a negative predictive value of 99.3%.
Chart review of the 34 cases (0.4% of all cases) who screened positive for symptoms but were not tested revealed flaws in the screening process. Cases falsely screened positive by acknowledging prior SARS-CoV-2 testing (often preoperative, not symptom triggered) or, less frequently, reporting symptoms that were chronic (ie, not due to COVID-19).
Discussion
We found a rate of postprocedure COVID-19 acquisition of <1.5%, even lower than the daily test positivity rate for Florida during the same period of 2.3%–19.6%.6 Our health system has strict infection control practices: separate COVID-19 inpatient wards, individual rooms for all patients, droplet precautions even if SARS-CoV-2 swab negative, and adequate personal protective equipment. These practices likely minimized nosocomial SARS-CoV-2 transmission in addition to COVID-19 prevention education on discharge.
Our study was limited by its single-center design inclusive of a cohort heavily weighted toward ophthalmologic procedures, which may have affected the generalizability of our results. We also lacked access to test results performed outside our health system. Due to the inability to influence patient behavior in the initial 72 hours prior to and after the procedure, patients could potentially become infected in the community which may have influenced the results. Moreover, variation in community incidence rates over the course of our study may have affected postprocedure COVID-19 acquisition. An attempt to compare test positivity rates over time between cases and the regional population would necessarily be confounded by differences (eg, access to healthcare) between cohorts. Finally, only 9.9% of cases were screened and tested. Our inability to include 90.1% of cases may have introduced bias because, despite demographic and clinical similarities between included and excluded cases, service lines performing included and excluded cases differed.
Our results suggest that the risk of acquiring postprocedural COVID-19 is low in the setting of strict infection control practices. Further delay of procedures due to fear of contracting COVID-19 may not be warranted.
Acknowledgments
The University of Miami Hospital and Clinics had no role in any aspect of the work.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/ice.2021.191.
click here to view supplementary material
Financial support
The UHealth-DART Research Group is supported by the University of Miami Hospital and Clinics.
Conflicts of interest
All authors declare no conflicts of interest related to this article.
References
- 1. D’Antona L, Palasz J, Haq H, et al. Letter to the editor: risk of hospital-acquired coronavirus disease 2019 (COVID-19) infection during admission for semiurgent neurosurgical procedures. World Neurosurg 2020;140:486–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Czeisler MÉ, Marynak K, Clarke KE, et al. Delay or avoidance of medical care because of COVID-19–related concerns—United States, June 2020. Morbid Mortal Wkly Rep 2020;69:1250–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gu XX, Chen K, Yu H, Liang GY, Chen H, Shen Y. How to prevent in-hospital COVID-19 infection and reassure women about the safety of pregnancy: experience from an obstetric center in China. J Int Med Res 2020;48(7). doi: 10.1177/0300060520939337. [DOI] [PMC free article] [PubMed]
- 4. Rhee C, Baker M, Vaidya V, et al. Incidence of nosocomial COVID-19 in patients hospitalized at a large US academic medical center. JAMA Netw Open 2020;3(9):e2020498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med 2020;172:577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Daily state-by-state testing trends. Johns Hopkins Coronavirus Resource Center website. https://coronavirus.jhu.edu/testing/individual-states/florida. Accessed October 8, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/ice.2021.191.
click here to view supplementary material