Abstract
Background
The rate of completed suicide among Inuit in Canada has been alarmingly high in recent years, and the suicide rate among Inuit in northern Quebec has increased since 1982. Our objectives were to describe the characteristics of Inuit people who died by suicide in Nunavik between 1982 and 1996, and to identify the antecedents and correlates of completed suicide.
Methods
We carried out a case–control study of 71 people who died by suicide between 1982 and 1996 and 71 population-based living control subjects matched for sex, community of residence and age within 1 year. Comprehensive medical charts were reviewed for data on sociodemographic characteristics, medical and psychiatric history, childhood separations and family history, and use of health care services.
Results
Most of the case subjects were single males aged 15 to 24 years. The two principal means of suicide were hanging (in 39 cases [54.9%]) and gunshot (in 21 cases [29.6%]). About 33% had been in contact with medical personnel in the month before their death. The case subjects were significantly more likely than the control subjects to have received a lifetime psychiatric diagnosis (one or more of depression, personality disorder or conduct disorder) (odds ratio [OR] 4.3 [95% confidence interval (CI) 1.2–15.2]) and to have had a history of psychiatric symptoms, disorder (including solvent sniffing) or treatment (OR 3.5 [95% CI 1.4–8.7]). The case subjects had experienced more severe types of nonpsychiatric illnesses and injuries than the control subjects (p = 0.04). The case subjects had more lifetime contacts with health care services than the control subjects (p = 0.01) and were more likely than the control subjects to have had contact with health care services in the year before death of the case subject (p = 0.03), even when psychiatric diagnoses were controlled for in conditional regression analysis (OR 1.02 [95% CI 1.01–1.04] and 5.0 [95% CI 1.07–23.7] respectively).
Interpretation
Since case subjects had frequent contact with health care services, frontline medical personnel may be in a position to identify people at risk for suicide.
The rate of completed suicide among Inuit in Canada has been high in recent years.1,2,3,4 According to the Royal Commission on Aboriginal Peoples, the overall rate among Inuit from 1987 to 1991 was 3.9 times that in the general population in Canada.5 Among young people, the Inuit rate was 5.1 times that among non-Aboriginals.5 In the northern Quebec region of Nunavik, the suicide rate among Inuit in 1987–1994 was 6.5 times higher than that in the rest of Quebec; the rate was 20 times higher among those aged 15 to 24 years.6 The average rate rose from 32.3 per 100 000 in 1982–1986 to 87.9 per 100 000 in 1987–1991 and 77.7 per 100 000 in 1992–1996 (Nunavik Public Health Department: unpublished data). The most recent data show a further increase, to 121.5 per 100 000 for 1997–1999 (Nunavik Public Health Department: unpublished data).
Reasons offered to explain the higher rate of suicide among Inuit include rapid social and cultural change, poverty and geographic isolation, social and economic marginalization, cultural suppression and political disempowerment.7 Known or suspected risk factors for suicidal behaviour that have a higher prevalence in Inuit communities than in non-Aboriginal populations include childhood separation and loss, alcohol abuse and dependence, personal or family mental health problems and exposure to self-destructive behaviour by others.7,8,9,10,11
Although several studies have examined suicide among Inuit in Alaska, the Northwest Territories and Greenland,3,12,13,14,15,16,17,18 they had small samples14 or limited12 (or no3,13,15,16,17,18) control groups. Only Thorslund13 made brief reference to northern Quebec, noting a 15-fold increase in the suicide rate from 1944 to 1968. Our objectives in the present study were to describe the characteristics of Inuit people who died by suicide in Nunavik between 1982 and 1996, and to identify the antecedents and correlates of completed suicide. An underlying goal was to determine to what extent high risk for completed suicide could be detected by nonspecialist health care professionals. Because completed and attempted suicide may involve partly nonoverlapping groups of people,19 risk factors for attempted suicide were addressed by our group in separate studies of survey data.20,21
Methods
The Inuit of Nunavik live in 14 villages along the shores of Arctic northern Quebec. There is no road access to these communities; aircraft provide transport within Nunavik and to the South, at great expense. Most of the Inuit are lifetime residents of the region because there is little migration in and out of the area. The regional population increased from 5055 in 1982 to 8860 in 1996 (Nunavik Public Health Department: unpublished data). Two regional hospitals and community nursing stations are the only sources of health care within Nunavik. Psychiatrists from Montreal visit several times a year; patients requiring extended psychiatric care are referred to hospitals in southern Quebec. All health care services are delivered in the context of a unified medical chart reporting system: medical records provide comprehensive coverage of outpatient visits, community hospital stays and specialty services received out of the region. Abstraction of data from medical records is thus a powerful research tool in this setting.
Permission to conduct the study was obtained from the Nunavik Regional Board of Health and Social Services and the Council of Physicians, Dentists, Pharmacists and Midwives at Innuulitsivik Hospital. The Nunavik Public Health Department provided a list of deaths between 1982 and 1996; of these, 75 were classified as suicides by the coroner's report, the death certificate or physician's notes in the patient's medical record. Of the 75 cases, 73 were eligible for the study (2 cases were excluded because the people had spent their childhood and early adult life outside Nunavik). Two of the remaining 73 cases could not be reviewed for logistical reasons. A population-based control group of 71 living people was individually matched to the 71 case subjects for sex, community of residence and age within 1 year. The control subjects were chosen from the vaccination list at 1 regional hospital and from municipal population lists. The first person who matched a case subject for the 3 variables considered was selected as the control subject.
Medical chart review was conducted in the region in 2 stages: by a nurse-practitioner familiar with the local health care system, and by 3 medical students on public health rotations and 3 physicians (2 of whom were working in the region), under the supervision of a single research coordinator (L.J.B.). The research coordinator compiled a manual to standardize the review process, worked in liaison with 2 on-site supervisors and reviewed all data. All chart reviews were carried out with an identical, structured form containing categories adapted from those used in a study of attempted suicide20 and a case–control psychological autopsy study by Lesage and colleagues.22 The review period for each control subject was matched to the date of death of the corresponding case subject. When available, social services charts were consulted to obtain additional information (e.g., on substance use and family history) regarding the case subjects; for reasons of feasibility, these data were not obtained for the control subjects and thus were not used in comparisons.
Data extracted from the charts included sociodemographic characteristics, medical and psychiatric history, family history and childhood separations, history of substance use, and use of health care and social services. For the case subjects, we examined life events in the year before death and immediate precipitants in the 2 weeks before death. The most severe nonpsychiatric illness or injury was coded for each subject, based on the revised Seriousness of Illness Rating Scale.23 The lifetime number of contacts with health care services was determined, as was the lifetime number of unique health problems (including both somatic and psychological problems), as an index of burden of ill health. Hearing loss (secondary to chronic otitis media in early childhood and very common in the region6) was included because of its association with impaired language development and poor school performance,24,25 factors that may contribute to vulnerability to suicide.20 Some people had missing data because part of their charts had been destroyed, they had been living in an institution outside the region for a lengthy period, or they were older (chart recording did not start until about 1960).
We compared the case and control subjects with regard to medical history (including contact with health care services, hospital admissions, health problems and developmental history), psychiatric history, previous suicidal behaviour and adoption status. We tested differences in means and proportions using the paired t-test and the McNemar test respectively. The matched-pair odds ratio estimator was used in the bivariate comparison of proportions for case and control subjects. The χ2 test for trend was used for proportions over ordered time periods.26 We used conditional multivariate logistic regression (respecting the matched design, with case/control status as the dependent variable) to examine the relation of use of health care services and medical factors after controlling for lifetime psychiatric diagnoses. Also, we entered psychiatric, medical and developmental, and health care use variables stepwise and removed nonsignificant factors to determine the final reduced regression model.
Results
Fig. 1 shows the number of suicides (total 73) and suicide rate by year over the study period. There were 2 large peaks in the last half of the study period, in 1991 and 1993. The large fluctuations observed in Fig. 1 reflect the use of annual rates in a relatively small population. A regression line fitted to the annual rates showed that, on average, the rate of suicide per 100 000 increased about 5-fold (odds ratio 5.21; 95% confidence interval –0.01 to 10.43) over the study period. This increasing trend was of borderline statistical significance (p = 0.05).
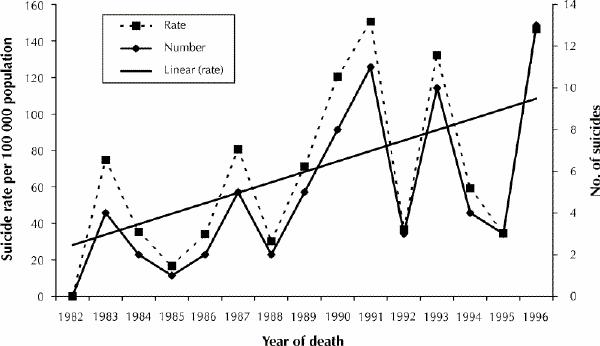
Fig. 1: Suicide rate and number of suicides by year from 1982 to 1996 among the Inuit in Nunavik, northern Quebec. Linear (rate) refers to the simple linear regression line showing trend in suicide rate.
Most of the 71 people included in the study who died by suicide were male (83.1% [59/71]), aged 15 to 24 years (70.4% [50/71]) and single (82.8% [48/58]); 12.1% (7/58) were married, and 5.2% (3/58) were separated or divorced. The age at death varied from about 12 years to over 50 years (mean 23.1 [standard deviation 8.6] years, median 20 years); 4 people (5.6%) were under 15 years of age, and 17 (23.9%) were 25 or older. The overall male:female ratio was about 5:1. Thirty-nine people (54.9%) died by hanging, 21 (29.6%) shot themselves, and 3 (4.2%) drowned themselves or had carbon monoxide poisoning; the method was unspecified for 8 (11.3%). The proportion of deaths by hanging increased by about 55% (95% confidence interval 42%–67%) from 1982–1986 to 1992–1996 (p value for trend < 0.01).
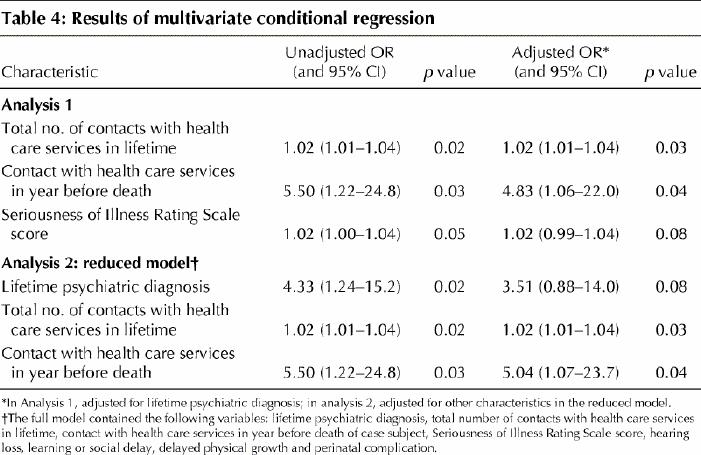
Tables 1, 2, 3 and 4 show the characteristics of the case subjects, comparisons between the case and control subjects, and the results of the multivariate conditional regression analysis. The case subjects were 3.5 times more likely than the control subjects to have had a psychiatric history and 4.3 times more likely to have had a psychiatric diagnosis. They had significantly more lifetime health care service contacts, an association that held when we controlled for lifetime psychiatric diagnoses in regression analysis (analysis 1; p = 0.03) (Table 4). Case subjects were 5.5 times more likely than control subjects to have had contact with health care services in the year before death of the case subject; the odds ratio when adjusted for psychiatric diagnoses was 4.8 (analysis 1; p = 0.04). The case subjects appeared to have experienced more severe medical illnesses and injuries on average in bivariate analysis, but this factor was not statistically significant when adjusted for psychiatric diagnoses. The reduced regression model (analysis 2, Table 4) showed that the number of lifetime contacts with health care services and the number of health care service contacts in the year before death of the case subject were independently associated with suicide.
Table 1
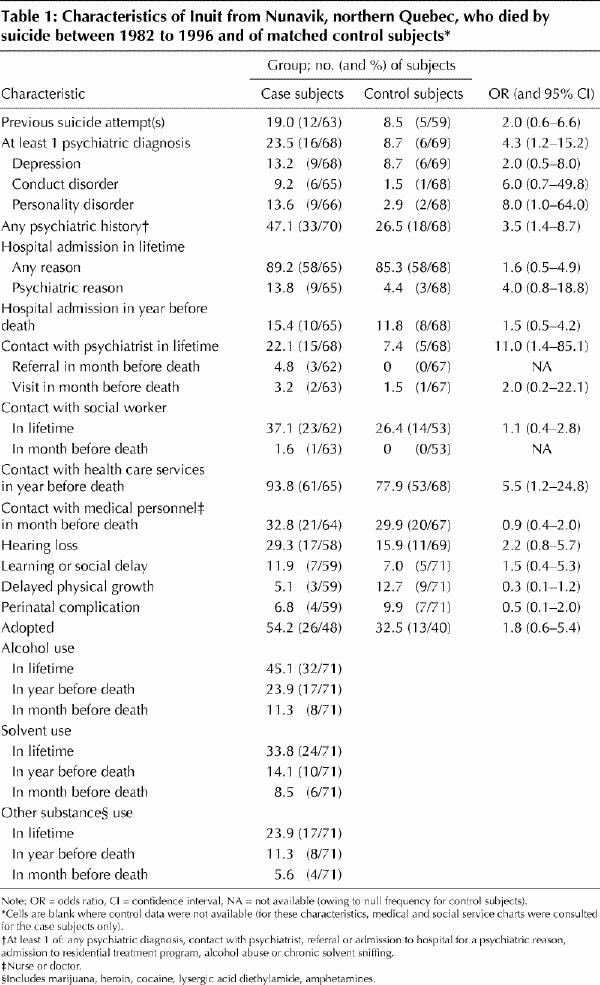
Table 2
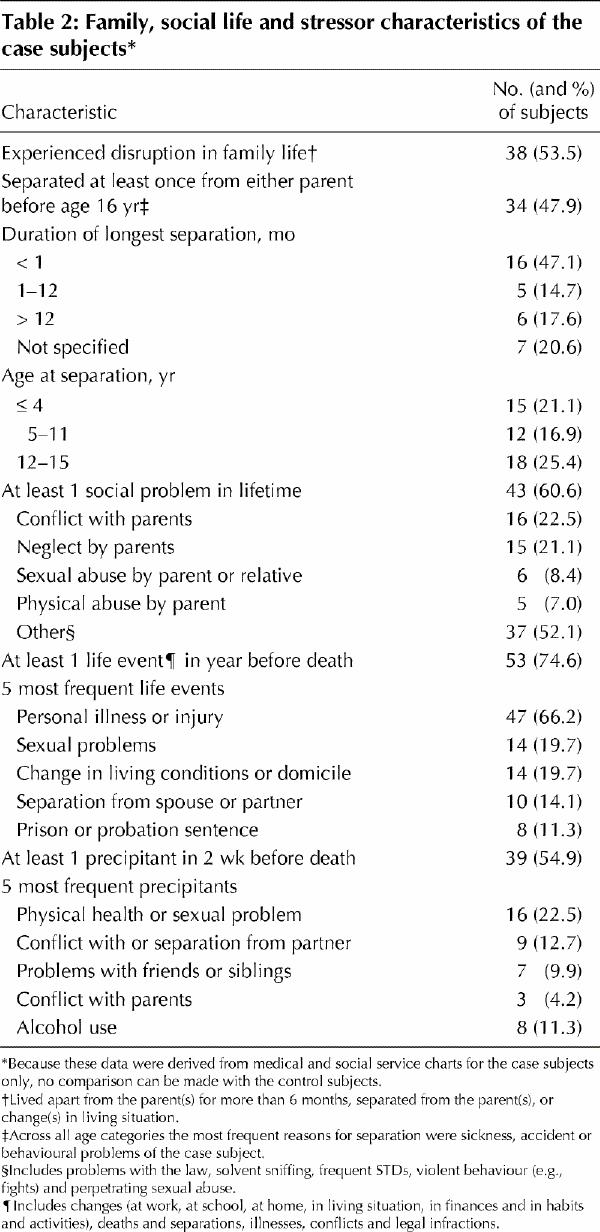
Table 3
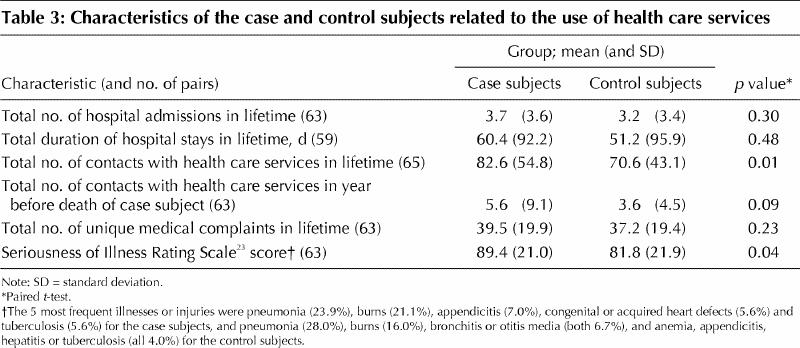
Table 4
Interpretation
We examined virtually all completed suicides among the Inuit in Nunavik in 1982–1996. In general, our results are comparable to those from other studies among Inuit in Alaska,14,16,17,18 the Northwest Territories3 and Greenland.12,13,15 Factors previously found to be frequent among people who died by suicide (or among a mixed group of 36 people who attempted suicide and 5 people who died by suicide12) have included recent precipitants (e.g., relationship breakdown),3,13 a history of emotional distress or depression,3 alcohol or drug abuse or intoxication at the time of death,3,12,13,14,15,17,18 previous help-seeking for social or mental health problems3 and criminal behaviour.3,12
The suicide rate among the Inuit in Nunavik increased over the study period, and public health data indicate that the rate has continued to climb since 1996. The demographic group most at risk for suicide is single males aged 15 to 24. This is consistent with recent reports on suicide among Aboriginal groups in the Northwest Territories,3 and in Alaska,17 British Columbia28 and Manitoba.27 The increase was most pronounced among those aged 15 to 24. Kettl and Bixler14 reported a similar finding in their case-control analysis of a subset of 33 Alaskan natives who died by suicide between 1979 and 1984.
The male:female ratio in our study was 5:1 overall and in the age group 15 to 24 years; most of the females who died by suicide were in this age group. Similar sex ratios have been reported among Aboriginal people on Manitoba reserves from 1973 to 1982,29 among Greenland-born Inuit from 1977 to 198613 and among Aboriginal people in Alaska from 1979 to 1994.17 The report on Aboriginal suicides in British Columbia also showed a male:female ratio of 5:1 among those aged 25 to 44, but a ratio of 1:1 among those aged 15 to 24.28
In Nunavik the predominant suicide methods were hanging and gunshot. Firearms are present in almost all Inuit households in the region. Use of firearms has consistently been reported to be the most common method of suicide among Aboriginal people in Alaska.16,17,18 Hanging has been shown to be a primary means in the Northwest Territories3 and among Aboriginal groups in Manitoba27 and British Columbia.28 In our study, the proportion of suicides by hanging increased significantly over the study period. The increase in this method may reflect the influence of social modelling on suicide, which, in this population, often occurs in clusters, with young people emulating their peers.4 Similarly, Isaacs and associates3 showed that the rate of suicide by hanging more than doubled from 1982–1986 to 1992–1996 in Nunavut (eastern Northwest Territories, predominantly Inuit population).
Kettl and Bixler14 found that Alaskan Aboriginals who killed themselves were more likely than control subjects to have a history of prior suicide attempts and alcohol abuse. A total of 40% of 403 Greenland Inuit who died by suicide13 and 56% of 78 people (87% Inuit) in the Northwest Territories who died by suicide3 were noted to have made a previous warning of suicidal intent. In our study, a greater proportion of case subjects than control subjects had made at least 1 previous suicide attempt, but the difference was not statistically significant. Use of alcohol was common among the case subjects; however, since this type of information was not collected routinely in the medical charts, we could not make comparisons with the control subjects.
Case–control studies in general populations in Canada, the United States, Taiwan, Finland and other countries using the method of psychological autopsy have consistently shown that psychiatric conditions underlie a large proportion of completed suicides.22,30,31,32,33,34,35 In our study, the case subjects were more likely than the control subjects to have a psychiatric diagnosis in their lifetime, the 2 most common being depression and personality disorder. We also found that a lifetime psychiatric diagnosis together with a history of substance use was common among the people who died by suicide, but we could not make this comparison with the control subjects. Unfortunately, there are no reliable data on the prevalence of psychiatric disorders in the region.6 A recent study in a Nunavut community showed that 26.5% of survey respondents had depression in the previous week, 19% had anxiety, and 30.6% had lifetime alcohol abuse or dependence.36
Prior contact with medical services among those who die by suicide has been found to be common — and more likely than among control subjects — in several general population studies.34,37,38,39,40 We found that the case subjects in our study had a greater number of contacts with health care services in their lifetime and were more likely to have had contact in the year before death than did the control subjects; these findings were not simply accounted for by a greater frequency of psychiatric diagnoses. Almost all of the case subjects had had contact with health care services at least once in the year before death, and about one-third saw medical personnel in the month before death.
Our study has several important limitations. Chart reviewers could not be blind to the status of the subject (either case or control). We did not include “accidental” deaths in the region, a number of which may have actually been suicides.14,41 We used a retrospective review of medical charts rather than a psychological autopsy because of the invasiveness of the latter procedure in small communities and because the time span of the review might have rendered family members' recollections unreliable. However, the medical charts were exceptionally comprehensive, owing to the ready availability of health care at nursing stations, centralized record keeping, and the isolation and stability of the population base.
Our results indicate that frontline medical personnel in Nunavik are in a position to detect people at high risk for suicide. Although a large proportion of the people who died by suicide had used health care services before death, the presenting problem in these visits was not necessarily a serious illness or psychiatric condition. Health care providers must therefore be alert to psychosocial problems in youths and assess suicide risk. Detection of high risk requires rapport and systematic inquiry into specific factors42,43 and could form part of a periodic health examination. After a program in which general practitioners were trained to recognize and treat depression on the island of Gotland, Sweden, there was evidence of a decrease in the overall suicide rate and in the number of suicides specifically related to depression.44 It is hoped that our study will help inform prevention initiatives by the Nunavik Regional Board of Health and Social Services, with which our team is collaborating.
Once identified, people at high risk must be referred to culturally appropriate crisis intervention or prevention programs. Such programs are likely to be most effective if initiated by and based in the community.45 For example, a rural New Mexico program in an American Indian community incorporates suicide risk screening, community education, family outreach and youths working as “natural helpers” or peer counsellors to provide services to young people at high risk in the schools.46 A decrease in the suicide rate among those aged 15 to 19 was sustained for the 5 years following initiation of the program.46
Given the limited sensitivity and specificity of risk factors for suicide, prevention directed exclusively at youths at high risk will miss many vulnerable people and incorrectly identify others. The high rates of exposure to suicide and of attempted suicide in Nunavik20,21 point to the need for a sustainable population- or community-based approach aimed at the broad spectrum of mental illness.47 Mental health must be promoted through fostering coping skills for interpersonal crises, conflict resolution and a positive collective identity.45,48 A community-based approach to suicide prevention must not focus exclusively on youths at high risk but must also include parents and extended families, who have also suffered from the effects of rapid culture change and marginalization.
Footnotes
This article has been peer reviewed.
Acknowledgements: We thank Michelle Delage, Eric Jarvis, Paul Farand, Marie-Noëlle Pépin, Tasnime Akbaraly, Carl Bromwich, Anne-Marie Uhlir and Luc Larrivée for performing the chart review and on-site supervision. We acknowledge Brian Schnarch, Carl Bromwich and Anne-Marie Uhlir for logistical support. We thank the staff at the nursing stations and regional hospitals (Innuulitsivik and Ungava Tulattavik) for assisting with the chart review.
This study was supported by grant 980991 from the Fonds de la recherche en santé du Québec and grant SR-3893 from the Conseil québécois de la recherche sociale.
Competing interests: None declared.
Correspondence to: Dr. Laurence J. Kirmayer, Institute of Community and Family Psychiatry, 4333 Côte Ste. Catherine Rd., Montreal QC H3T 1E4; fax 514 340-7503; laurence.kirmayer@mcgill.ca
References
- 1.Petawabano B, Gourdeau E, Jourdain F, Palliser-Tulugak A, Cossette J. Mental health and Aboriginal people of Québec. Montreal: Gaëtan Morin Éditeur; 1994. p. 23-70.
- 2.Young TK. The health of Native Americans: toward a biocultural epidemiology. New York: Oxford University Press; 1994. p. 176-215.
- 3.Isaacs S, Keogh S, Menard C, Hockin J. Suicide in the Northwest Territories: a descriptive review. Chronic Dis Can 1998;19(4):152-6. [PubMed]
- 4.Kirmayer LJ, Fletcher C, Boothroyd L. Suicide among the Inuit. In: Leenaars AA, Wenckstern S, Sakinofsky I, Dyck RJ, Kral MJ, Bland RC, editors. Suicide in Canada. Toronto: University of Toronto Press; 1998. p. 189-211.
- 5.Royal Commission on Aboriginal Peoples. Choosing life: a special report on suicide among Aboriginal people. Ottawa: The Commission; 1995. Cat no Z1-1991/1-41-4E.
- 6.Hodgins S. Health and well-being challenges in Nunavik: health conditions, determinants, and lines of action. Kuujjuaq (QC): Department of Public Health, Nunavik Regional Board of Health and Social Services; 1996.
- 7.Kirmayer LJ. Suicide among Canadian Aboriginal peoples. Transcult Psychiatr Res Rev 1994;31(1):3-58.
- 8.Bachman R. Death and violence on the reservation: homicide, family violence, and suicide in American Indian populations. New York: Auburn House; 1992.
- 9.Earls F, Escobar JI, Manson SM. Suicide in minority groups: epidemiologic and cultural perspectives. In: Blumenthal SJ, Kupfer DJ, editors. Suicide over the life cycle. Washington: American Psychiatric Press; 1991. p. 571-98.
- 10.Grossman DC, Milligan BC, Deyo RA. Risk factors for suicide attempts among Navajo adolescents. Am J Public Health 1991;81(7):870-4. [DOI] [PMC free article] [PubMed]
- 11.Health Canada. Suicide in Canada: update of the report of the Task Force on Suicide in Canada. Ottawa: Minister of National Health and Welfare; 1994. Cat no H39-107/1995E.
- 12.Grove O, Lynge J. Suicide and attempted suicide in Greenland. Acta Psychiatr Scand 1979;60:375-91. [DOI] [PubMed]
- 13.Thorslund J. Inuit suicides in Greenland. Arctic Med Res 1990;49:25-34. [PubMed]
- 14.Kettl PA, Bixler EO. Suicide in Alaska natives, 1979–1984. Psychiatry 1991;54: 55-63. [DOI] [PubMed]
- 15.Thorslund J. Suicide among Inuit youth in Greenland 1974–86. In: Postl BD, Gilbert P, Goodwill J, Moffatt MEK, O'Neil JD, Sarsfield PA, et al, editors. Circumpolar health '90. Winnipeg: University of Manitoba Press; 1991. p. 299-302.
- 16.Gessner BD. Temporal trends and geographic patterns of teen suicide in Alaska, 1979–1993. Suicide Life Threat Behav 1997;27(3):264-73. [PubMed]
- 17.Marshall D, Soule S. Accidental deaths and suicides among Alaska Natives, 1979–1994. Int J Circumpolar Health 1998;57(Suppl 1):497-502. [PubMed]
- 18.Hlady WG, Middaugh JP. Suicides in Alaska: firearms and alcohol. Am J Public Health 1988;78:179-80. [DOI] [PMC free article] [PubMed]
- 19.Hawton K. Suicide and attempted suicide among children and adolescents. Newbury Park (CA): Sage; 1986.
- 20.Kirmayer LJ, Malus M, Boothroyd LJ. Suicide attempts among Inuit youth: a community survey of prevalence and risk factors. Acta Psychiatr Scand 1996; 94:8-17. [DOI] [PubMed]
- 21.Kirmayer LJ, Boothroyd LJ, Hodgins S. Attempted suicide among Inuit youth: psychosocial correlates and implications for prevention. Can J Psychiatry 1998;43:816-22. [DOI] [PubMed]
- 22.Lesage AD, Boyer R, Grunberg F, Vanier C, Morissette R, Ménard-Buteau C, et al. Suicide and mental disorders: a case–control study of young men. Am J Psychiatry 1994;151:1063-8. [DOI] [PubMed]
- 23.Rosenberg SJ, Hayes JR, Peterson RA. Revising the Seriousness of Illness Rating Scale: modernization and re-standardization. Int J Psychiatry Med 1987;17:85-92. [DOI] [PubMed]
- 24.Julien G, Baxter JD, Crago M, Ilecki HJ, Thérien F. Chronic otitis media and hearing deficit among Native children of Kuujjuaraapik (northern Quebec): a pilot project. Can J Public Health 1987;78:57-61. [PubMed]
- 25.Tremblay C. Prevalence of hearing loss in northern Quebec: a medical and statistical challenge. Arctic Med Res 1991;Suppl:S653-4. [PubMed]
- 26.Armitage P, Berry G. Statistical methods in medical research. Oxford: Blackwell Scientific Publications; 1994. p. 402-7.
- 27.Malchy B, Enns MW, Young TK, Cox BJ. Suicide among Manitoba's aboriginal people, 1988 to 1994. CMAJ 1997;156(8):1133-8. Abstract available: www.cma.ca/cmaj/vol-156/issue-8/1133.htm [PMC free article] [PubMed]
- 28.Data report on the psychosocial characteristics of completed suicides in British Columbia. Vancouver: BC Suicide Prevention Program at Cooperative University–Provincial Psychiatric Liaison, University of British Columbia; 1997.
- 29.Garro LC. Suicides by status Indians in Manitoba. Arctic Med Res 1988;47 (Suppl 1):590-2. [PubMed]
- 30.Henriksson MM, Aro HM, Marttunen MJ, Heikkinen ME, Isometsä ET, Kuoppasalmi KI, et al. Mental disorders and comorbidity in suicide. Am J Psychiatry 1993;150:935-40. [DOI] [PubMed]
- 31.Cheng ATA. Mental illness and suicide: a case-control study in east Taiwan. Arch Gen Psychiatry 1995;52:594-603. [DOI] [PubMed]
- 32.Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry 1996;153:1001-8. [DOI] [PubMed]
- 33.Shaffer D, Gould MS, Fisher P, Trautman P, Moreau D, Kleinman M, et al. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry 1996;53:339-48. [DOI] [PubMed]
- 34.Appleby L, Cooper J, Amos T, Faragher B. Psychological autopsy study of suicides by people aged under 35. Br J Psychiatry 1999;75:168-74. [DOI] [PubMed]
- 35.Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age- and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry 1999; 38(12):1497-504. [DOI] [PubMed]
- 36.Haggarty J, Cernovsky Z, Kermeen P, Merskey H. Psychiatric disorders in an Arctic community. Can J Psychiatry 2000;45:357-62. [DOI] [PubMed]
- 37.Power K, Davies C, Swanson V, Gordon D, Carter H. Case-control study of GP attendance rates by suicide cases with or without a psychiatric history. Br J Gen Pract 1997;47:211-5. [PMC free article] [PubMed]
- 38.Haste F, Charlton J, Jenkins R. Potential for suicide prevention in primary care? An analysis of factors associated with suicide. Br J Gen Pract 1998;48: 1759-63. [PMC free article] [PubMed]
- 39.Pirkis J, Burgess P. Suicide and recency of health care contacts. Br J Psychiatry 1998;173:462-74. [DOI] [PubMed]
- 40.Boardman AP, Grimbaldeston AH, Handley C, Jones PW, Willmott S. The North Staffordshire Suicide Study: a case-control study of suicide in one health district. Psychol Med 1999;29:27-33. [DOI] [PubMed]
- 41.Barss P, Smith GS, Baker SP, Mohan D. Intentional injuries: homicide, suicide, and other violence. New York: Oxford University Press; 1998. p. 264-76.
- 42.Feightner JW, Worrall G. Early detection of depression by primary care physicians. CMAJ 1990;142(11):1215-20. [PMC free article] [PubMed]
- 43.Shaffer D, Craft L. Methods of adolescent suicide prevention. J Clin Psychiatry 1999;60(Suppl 2):70-4. [PubMed]
- 44.Rihmer Z, Rutz W, Pihlgren H. Depression and suicide on Gotland. An intensive study of all suicides before and after a depression-training programme for general practitioners. J Affective Disord 1995;35(4):147-52. [DOI] [PubMed]
- 45.Kirmayer LJ, Boothroyd LJ, Laliberté A, Laronde Simpson B. Suicide prevention and mental health promotion in Native communities. Montreal: Culture and Mental Health Research Unit, Institute of Community and Family Psychiatry, Sir Mortimer B. Davis–Jewish General Hospital; 1999. Report no 9.
- 46.Centers for Disease Control and Prevention. Suicide prevention evaluation in a Western Athabaskan American Indian tribe: New Mexico, 1988–1997. MMWR Morb Mortal Wkly Rep 1998;47(13):257-61. [PubMed]
- 47.Mortensen PB, Agerbo E, Erikson T, Qin P, Westergaard-Nielsen N. Psychiatric illness and risk factors for suicide in Denmark. Lancet 2000;355:9-12. [DOI] [PubMed]
- 48.Dryfoos JG. Adolescents at risk: prevalence and prevention. New York: Oxford University Press; 1990.


