Abstract
Background
Anaemia associated with cancer and cancer therapy is an important clinical factor in the treatment of malignant diseases. Therapeutic alternatives are recombinant human erythropoiesis stimulating agents (ESAs) and red blood cell transfusions.
Objectives
To assess the effects of ESAs to either prevent or treat anaemia in cancer patients.
Search methods
This is an update of a Cochrane review first published in 2004. We searched the Central Register of Controlled Trials (CENTRAL), MEDLINE and EMBASE and other databases. Searches were done for the periods 01/1985 to 12/2001 for the first review, 1/2002 to 04/2005 for the first update and to November 2011 for the current update. We also contacted experts in the field and pharmaceutical companies.
Selection criteria
Randomised controlled trials on managing anaemia in cancer patients receiving or not receiving anti‐cancer therapy that compared the use of ESAs (plus transfusion if needed).
Data collection and analysis
Several review authors assessed trial quality and extracted data. One review author assessed quality assessment and extracted data, a second review author checked for correctness.
Main results
This update of the systematic review includes a total of 91 trials with 20,102 participants. Use of ESAs significantly reduced the relative risk of red blood cell transfusions (risk ratio (RR) 0.65; 95% confidence interval (CI) 0.62 to 0.68, 70 trials, N = 16,093). On average, participants in the ESAs group received one unit of blood less than the control group (mean difference (MD) ‐0.98; 95% CI ‐1.17 to ‐0.78, 19 trials, N = 4,715). Haematological response was observed more often in participants receiving ESAs (RR 3.93; 95% CI 3.10 to 3.71, 31 trials, N = 6,413). There was suggestive evidence that ESAs may improve Quality of Life (QoL). There was strong evidence that ESAs increase mortality during active study period (hazard ratio (HR) 1.17; 95% CI 1.06 to 1.29, 70 trials, N = 15,935) and some evidence that ESAs decrease overall survival (HR 1.05; 95% CI 1.00 to 1.11, 78 trials, N = 19,003). The risk ratio for thromboembolic complications was increased in patients receiving ESAs compared to controls (RR 1.52, 95% CI 1.34 to 1.74; 57 trials, N = 15,498). ESAs may also increase the risk for hypertension (fixed‐effect model: RR 1.30; 95% CI 1.08 to 1.56; random‐effects model: RR 1.12; 95% CI 0.94 to 1.33, 31 trials, N = 7,228) and thrombocytopenia/haemorrhage (RR 1.21; 95% CI 1.04 to 1.42; 21 trials, N = 4,507). There was insufficient evidence to support an effect of ESA on tumour response (fixed‐effect RR 1.02; 95% CI 0.98 to 1.06, 15 trials, N = 5,012).
Authors' conclusions
ESAs reduce the need for red blood cell transfusions but increase the risk for thromboembolic events and deaths. There is suggestive evidence that ESAs may improve QoL. Whether and how ESAs affects tumour control remains uncertain. The increased risk of death and thromboembolic events should be balanced against the potential benefits of ESA treatment taking into account each patient’s clinical circumstances and preferences. More data are needed for the effect of these drugs on quality of life and tumour progression. Further research is needed to clarify cellular and molecular mechanisms and pathways of the effects of ESAs on thrombogenesis and their potential effects on tumour growth.
Keywords: Humans, Anemia, Anemia/drug therapy, Anemia/etiology, Anemia/prevention & control, Cause of Death, Darbepoetin alfa, Erythrocyte Transfusion, Erythrocyte Transfusion/statistics & numerical data, Erythropoietin, Erythropoietin/adverse effects, Erythropoietin/analogs & derivatives, Erythropoietin/therapeutic use, Hypertension, Hypertension/chemically induced, Neoplasms, Neoplasms/blood, Neoplasms/complications, Quality of Life, Randomized Controlled Trials as Topic, Recombinant Proteins, Recombinant Proteins/adverse effects, Recombinant Proteins/therapeutic use, Thromboembolism, Thromboembolism/chemically induced
Plain language summary
Erythropoietin or darbepoetin for patients with cancer
Introduction
Researchers in The Cochrane Collaboration conducted a review of the effect of epoetin and darbepoetin for people with cancer. After searching for all relevant studies, they found 91 studies with up to 20,102 people. Their findings are summarized below:
What the research says:
In people with cancer‐related anaemia:
‐ Epoetin and darbepoetin decrease the need for red blood cell transfusions; however, they also increase the risk for hypertension, thromboembolic events and deaths
‐ It is not clear whether epoetin and darbepoetin improve quality of life, by making you feel less tired
When you have cancer, you often also have anaemia. Anemia means having lower than normal red blood cells in your blood. This might become even worse with cancer treatment such as chemotherapy and it is measured by the amount of haemoglobin in your red blood cells. As haemoglobin is responsible for carrying oxygen throughout your body, when you have anaemia you might experience symptoms such as extreme tiredness, shortness of breath, dizziness and chest pain. In order to treat anaemia, doctors often use red blood cell transfusions. Transfusions improve the symptoms of anaemia very quickly; however, they can have some infrequent complications like allergic reactions or transmission of infectious diseases.
Epoetin and darbepoetin belong to a group of medications called 'Erythropoiesis Stimulating Agents'. Erythropoietin is the name of a hormone produced mainly in the kidney, which takes part in the production of red blood cells. Epoetin and darbepoetin work in a similar way to this hormone to increase the number of red blood cells and treat anaemia. Epoetin and darbepoetin are not used as anti‐cancer therapy but as supportive treatment to treat anaemia caused by cancer or anticancer therapy. These drugs are marketed as Epogen®, Procrit®, (Eprex®), Recormon®, and Aranesp® and are given subcutaneously.
What happens to people with cancer related anaemia who take epoetin or darbepoetin:
‐ Twenty‐five out of 100 persons receiving epoetin or darbepoetin had to undergo red blood cell transfusions, compared to 39 out of 100 persons not receiving epoetin or darbepoetin.
‐ More people who received epoetin or darbepoetin died during and up to 30 days after the end of study compared with people who took placebo or underwent standard treatment. The increased risk for people taking epoetin or darbepoetin was 17%. One hundred and fourteen out of 1,000 persons receiving epoetin or darbepoetin died, compared with 98 out of 1,000 persons not receiving epoetin or darbepoetin. We could not identify particular characteristics of people or treatment strategies that increased or decreased the risk for dying.
‐ Concerning long‐term survival people taking epoetin or darbepoetin were 5% more at risk for dying than people taking placebo or receiving standard treatment.
‐ People receiving epoetin or darbepoetin rated their fatigue symptoms to be an average of 2.08 points improved on a scale of 0‐52 points after 3‐4 months, compared with people taking placebo or having standard treatment. This improvement, however, is less than the 3.0 point increase which is considered to be the minimum required for the patient to feel a difference in his experience of fatigue‐related symptoms using this scale.
‐ People taking epoetin or darbepoetin rated their fatigue and anaemia symptoms had to be an average of 6.14 points improved after three to four months, on a scale of 0‐80 points. This improvement is considered to reflect a positive change in the way patients experience their fatigue and anaemia related symptoms, as it is more than four to five points of increase which is the minimum required for this scale.
‐ Seven people out of 100 who took epoetin or darbepoetin suffered a thromboembolic event such as stroke and myocardial infarction compared with five people out of 100 who did not receive epoetin or darbepoetin.
‐ Six out of 100 people receiving epoetin or darbepoetin developed high blood pressure compared with four out of 100 people who took placebo or had standard care.
Summary of findings
Summary of findings for the main comparison. Erythropoietin or Darbepoetin for patients with cancer.
| Erythropoietin or Darbepoetin for patients with cancer | ||||||
| Patient or population: patients with cancer Settings: Intervention: Erythropoietin or Darbepoetin | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Erythropoietin or Darbepoetin | |||||
| Overall survival | Low | HR 1.05 (1 to 1.11) | 19003 (78 studies) | ⊕⊕⊕⊕ high | ||
| 50 per 1000 | 52 per 1000 (50 to 55) | |||||
| Moderate | ||||||
| 142 per 1000 | 149 per 1000 (142 to 156) | |||||
| High | ||||||
| 250 per 1000 | 261 per 1000 (250 to 273) | |||||
| On‐study mortality Death occurring up to 30 days after active study protocol | Low | HR 1.17 (1.06 to 1.29) | 15935 (70 studies) | ⊕⊕⊕⊕ high | ||
| 10 per 1000 | 12 per 1000 (11 to 13) | |||||
| Moderate | ||||||
| 59 per 1000 | 69 per 1000 (62 to 75) | |||||
| High | ||||||
| 98 per 1000 | 114 per 1000 (104 to 125) | |||||
| Thrombotic events | Low | RR 1.52 (1.33 to 1.73) | 15278 (57 studies) | ⊕⊕⊕⊝ moderate1 | ||
| 20 per 1000 | 30 per 1000 (27 to 35) | |||||
| Moderate | ||||||
| 46 per 1000 | 70 per 1000 (61 to 80) | |||||
| High | ||||||
| 100 per 1000 | 152 per 1000 (133 to 173) | |||||
| Quality of Life ‐ Change in FACT‐Fatigue (13 items) FACT‐F 13 sub‐scale | The mean quality of life ‐ change in fact‐fatigue (13 items) in the intervention groups was 2.08 higher (1.43 to 2.72 higher) | 4965 (18 studies) | ⊕⊕⊝⊝ low2,3 | |||
| Quality of Life ‐ Change in FACT‐Anaemia (20 items) FACT‐An 20 | The mean quality of life ‐ change in fact‐an (20 items) in the intervention groups was 6.14 higher (4.55 to 7.73 higher) | 1085 (6 studies) | ⊕⊕⊝⊝ low4,5 | |||
| Participants receiving red blood cell transfusions | Low | RR 0.65 (0.62 to 0.68) | 15877 (70 studies) | ⊕⊕⊕⊝ moderate6 | ||
| 300 per 1000 | 195 per 1000 (186 to 204) | |||||
| Moderate | ||||||
| 389 per 1000 | 253 per 1000 (241 to 265) | |||||
| High | ||||||
| 700 per 1000 | 455 per 1000 (434 to 476) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; HR: Hazard ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 A funnel plot analysis revealed a significant asymmetry, suggesting that negative results (in this case no thrombotic event) have been underreported 2 Only 18 out of a total of 91 studies assessing FACT‐13 reported this endpoint, which suggests some reporting bias, even if the funnel plot did not show an asymmetry. 13 more studies (i.e. studies that stated they either used FACT‐F or that they used FACT‐An 47 but do not report separately for FACT‐F or report it in a way that we cannot use. 3 Overall, it seems that there is an effect to fatigue‐related symptoms for patients treated with ESAs compared to controls; this effect, however, did not reach the threshold for a clinically important difference defined as 3.0. 4 Only 6 out of a total of 91 studies assessing FACT‐20 reported this endpoint, which suggests some reporting bias, even if the funnel plot did not show an asymmetry. Data from 19 studies addressing QoL can not used for review in cause of missing data (i.e.16 studies that stated they either used fact‐an or that they used fact‐an 47 but do not report separately for fact‐an). Out of these 4 studies which refer to “FACT‐An”/ to “fatigue sub‐scale”, were not useable because we cannot safely say to which instrument they are refer to. 5 Overall, the effects of ESAs to fatigue and anaemia related symptoms seem to be beneficial and the difference between groups reaches both statistical and clinical significance (clinically important difference defined as 4‐5). 6 A funnel plot analysis showed significant asymmetry between the studies, suggesting that negative results were under reported.
Background
Description of the condition
Anaemia, defined as a deficiency in the concentration of haemoglobin‐containing red blood cells, is a widely prevalent complication among cancer patients (Knight 2004). The prevalence of anaemia varies according to the type of neoplasia (Monnerat 1999). Patients with haematological malignancies frequently experience anaemia. At the time of diagnosis, 30% to 40% of patients with non‐Hodgkin's lymphoma (NHL) or Hodgkin's lymphoma (HD) and up to 70% of patients with multiple myeloma are anaemic; the figures are even higher in myelodysplastic syndromes (Garton 1995; Greenberg 1994). The extent of anaemia is also influenced by the type of cytostatic treatment. It is known that the proportion of anaemic patients with solid cancers rises up to 50% after chemotherapy or combined radiochemotherapy (Dalton 1998; Harrison 2001; Ludwig 1998; Reed 1994).
The National Cancer Institute and others have agreed to use the following classification for anaemia based on haemoglobin (Hb) values (Groopman 1999):
Grade 0, within normal limits, Hb values are 12.0 to 16.0 g/dL for women and 14.0 to 18.0 g/dL for men
Grade 1, mild (Hb 10 g/dL to normal limits)
Grade 2, moderate (Hb 8.0 to 10.0 g/dL)
Grade 3, serious/severe (Hb 6.5 to 7.9 g/dL)
Grade 4, life threatening (Hb less than 6.5 g/dL).
The pathophysiology of tumour anaemia is multi‐factorial (Mercadante 2000). In advanced stages of haematological malignancies, bone marrow involvement with malignant cells often leads to progressive anaemia. After exclusion of other causes, e.g. iron or vitamin deficiencies, occult bleeding, autoimmune haemolysis or pure red blood cell aplasia, anaemia can be related to "anaemia of chronic disorders". It is characterised by a close interaction between the tumour cell population and the immune system, leading to the activation of macrophages and increased expression of various cytokines, especially Interferon‐g, Interleukin‐1, Interleukin‐6 and tumour necrosis factor. This is followed by insufficient endogenous erythropoietin synthesis, suppressed differentiation of erythroid precursor cells in the bone marrow and alterations of iron metabolism (Johnson 1990; Ludwig 1998; Nowrousian 2002a; Spivak 1994a). For example, the elevation of interleukin 6 (Il‐6) leads to an up‐regulation of Hepcidin and a diminished erythropoietin‐synthesis. Hepcidin is one of the mediators that are released in inflammatory processes. It causes the destruction of another protein called ferroportin, which is important for the transport of Fe2+ from the enterocyte and the macrophage into the blood (Ganz 2011). The anaemia of chronic disorders, or chronic tumour anaemia is the most common type in patients with malignant disease, although it is often aggravated by chemo‐ or radiotherapy. In particular, platinum‐based chemotherapy regimens may diminish endogenous erythropoietin production by damaging renal tubular cells (Wood 1995).
Manifestation and severity of anaemia vary considerably among individual patients. Mild‐to‐moderate anaemia can cause typical symptoms including headache, palpitations, tachycardia and shortness of breath. Chronic anaemia may result in severe organ damage affecting the cardiovascular system, immune system, lungs, kidneys, muscles and the central nervous system (Ludwig 2001; Nissenson 1992). In addition to physical symptoms, the subjective impact of cancer‐related anaemia on quality of life (QoL), mental health and social activities may be substantial. Clinical studies have reported correlations between Hb levels and quality of life domains, for example mood, appetite (Leitgeb 1994), and the ability to work (Cella 1998; Thomas 1998).
Another aspect of anaemia in patients with malignant disease is the effect on the tumour itself. For malignant diseases such as Hodgkin's Disease (HD), chronic lymphocytic leukaemia (CLL), cervical carcinoma and cancer of the head and neck, anaemia has been reported to be an independent prognostic factor (Caro 2001; Hasenclever 1998; Nowrousian 2002b; Van Belle 2003). There is evidence that anaemia, with the consequence of increased tumour hypoxia, might result in a poorer response to radio‐ or chemotherapy (Hockel 1993; Nordsmark 1996; Van Belle 2003; Vaupel 1989; Vaupel 2000). Severe symptoms of anaemia may also necessitate dose reduction or delay of chemotherapy. All these factors may lead to a higher tumour burden and a decreased overall survival (Glaser 2001; Grau 2000; Knocke 1999). These observations have generated the hypothesis that strategies to diminish cancer‐related anaemia might alleviate not only anaemia‐related symptoms and improve quality of life, but also might improve tumour response and extend overall survival time. However, randomised controlled trials testing this hypothesis have generated conflicting evidence (Antonadou 2001; Henke 2003; Leyland‐Jones 2005).
Historically, blood transfusion was the conventional treatment of choice for severe cancer‐related anaemia. The literature reports a critical degree of anaemia as a Hb level below 8 g/dL, while mild‐to‐moderate anaemia (Hb level 8‐10 g/dL) usually has been left untreated (Carson 2012; Cella 1999; Glaspy 1997a; Henry 1992; Koeller 1998). Although homologous blood transfusion is the fastest method to alleviate symptoms, short‐ and long‐term risks exist (Engert 2000). Potential complications associated with blood transfusion are transmission of infectious diseases, transfusion reactions, allo‐immunisation, over‐transfusion and immune modulation with possible adverse effects on tumour growth (Landers 1996). The risk of severe infectious complications of blood transfusions are 1: 30.000 to 1:250.000 units of blood transfused for Hepatitis B, 1:30.000 to 1:150.000 for Hepatitis C and 1:250.000 to 1:1.000.000 for HIV (Goodnough 1999). Other complications such as allergic reactions and death due to major incompatibilities are infrequent but may be of concern (Williamson 1999). The development of intensified anti‐neoplastic therapies has increased the risk for blood transfusion, prompting oncologists to weigh the advantages and disadvantages of this treatment.
Description of the intervention
Recombinant human erythropoietin is a treatment option for cancer‐related anaemia. Human erythropoietin is an acidic glycoprotein hormone. Approximately 90% of the hormone is synthesised in the kidney and 10% in the liver (Koury 1988; Koury 1991). Basal production maintains a relatively constant plasma concentration of erythropoietin in individuals, within a range from 9 to 26 mU/mL. Tissue hypoxia is the most important trigger for increased synthesis. The effects of erythropoietin in the bone marrow are mediated by a specific surface receptor located mainly on erythroid progenitor and precursor cells (D´Andrea 1989; Spivak 1994b). Two major functions of erythropoietin are described: stimulating progenitor cell proliferation and maintaining their viability (Koury 1990).
Several short‐ and long‐lasting forms of recombinant human erythropoiesis‐stimulating agents (ESAs) are available, including Epoetin‐a and Epoetin‐ß and darbepoetin‐a (Darbepo) (Glaspy 2003; Halstenson 1991; Hedenus 2002; Joy 2002; Storring 1998; Vansteenkiste 2002). Recently, novel ESA molecules, such as continuous erythropoietin receptor activator (CERA) (Gascon 2010b), and biosimilars (epoetin theta, epoetin delta) have been developed (Jelkmann 2010). Clinical trials directly comparing Epo and Darbepo have been published and suggest that Epo and Darbepo are similarly effective with regard to Hb response and proportion of patients transfused (Alexopoulos 2004; Glaspy 2003; Schwartzberg 2004; Waltzman 2004). Based on these data, it seemed justified to combine both short‐ and long‐lasting erythropoietin formulations in one meta‐analysis.
How the intervention might work
Erythropoietin was first approved for the treatment of anaemia in chronic kidney failure. In 1990, erythropoietin was introduced in cancer therapy regimens for patients with multiple myeloma. A pilot study showed haematological response rates of 85% and an improved performance status (Ludwig 1990). Adverse effects such as hypertension, headaches and thrombotic events conclusively attributable to erythropoietin treatment were reported in very few patients (Beguin 1998). However, several randomised controlled trials reported increased incidences of thrombotic events, tumour progression and deaths (Hedenus 2003; Henke 2003; Leyland‐Jones 2005; Overgaard 2009; Smith 2008; Thomas 2008; Untch 2011_1; Wright 2007).
Why it is important to do this review
Since ESAs were licensed for the treatment of anaemia in cancer patients, more than 20 systematic reviews and meta‐analyses have been published. While there is clear evidence that ESAs reduce the need for red blood cell transfusions, increase Hb levels and also increase the risk for thromboembolic complications, there is ongoing debate on the effects of ESAs on QoL, tumour progression and mortality (Aapro 2006; Aapro 2008; Aapro 2009; Bennett 2008; Bottomley 2002; Cella 2004; Clark 2002; Devon 2009; Glaspy 2010; Hedenus 2005; Hellström‐L 1995; Jones 2004; Kimel 2008; Lambin 2009; Ludwig 2009; Minton 2008; Minton 2010; Quirt 2003; Quirt 2005; Ross 2003; Ross 2006; Ross 2007; Seidenfeld 2001b; Seidenfeld 2001a; Seidenfeld 2006; Tonelli 2009; Wilson 2007).
The first Cochrane review (published in 2004 in The Cochrane Library and 2005 as print publication) on this subject included 27 randomised controlled studies on erythropoietin with 3,287 adults, published between 1985 and April 2002 (Bohlius 2005) in collaboration with authors from a previous review conducted for AHRQ (Seidenfeld 2001a;Seidenfeld 2001b). For the first update, we included trials published between 2002 and 2005 in collaboration with an independent review team from the Department of Public Health and Epidemiology at the University of Birmingham and the support of the UK Department of Health (Bohlius 2006a). In 2009, we conducted a separate meta‐analysis based on individual patient data (IPD), which focused on on‐study mortality and overall survival in all cancer patients and in patients receiving chemotherapy (Bohlius 2009a; Bohlius 2009b).Given that this analysis was restricted to survival outcomes, we present here the second update of the Cochane Review, including all relevant outcomes and integrating results generated for the IPD analysis as well as recently published trials.
Objectives
To systematically review evidence on the outcomes of using recombinant human erythropoietin or darbepoetin to prevent or alleviate anaemia in patients with malignant disease, with respect to haematological response, red blood cell transfusion need, changes in quality of life, tumour response, on‐study mortality, overall survival and adverse events.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials using recombinant human erythropoietin or darbepoetin to treat or prevent anaemia in patients with malignant disease. Placebo control, as opposed to "no treatment", was not required for inclusion, but was considered in evaluating study quality. We excluded trials in which patients were allocated by a quasi‐random method, for example date of birth or day of month, as we considered this study design to be of poor quality leading to unreliable results. We included only trials with more than 10 documented participants in each study arm or relevant stratum. We excluded interim analyses of ongoing studies. We included studies that were stopped or suspended prematurely. The searches did not include language restrictions.
Types of participants
We included only participants diagnosed with malignant disease, using clinical and histological/cytological criteria, regardless of type or stage of the disease or previous therapy. All study participants had to be anaemic or at risk for anaemia from chemotherapy, radiotherapy or combination therapy, or the underlying malignant disease. Other causes of anaemia, such as haemolysis, iron deficiency and occult bleeding, had to have been excluded. We included studies with patients of every age. We excluded trials if more than 80% of participants were diagnosed with an acute leukaemia.
Types of interventions
We included studies evaluating the use of recombinant human erythropoiesis‐stimulating agents (ESAs) to prevent or reduce anaemia in cancer patients, given singly or concomitantly with chemotherapy, radiotherapy or combination therapy. ESAs could be administered subcutaneously or intravenously. In previous versions of this review, we required dosages of at least 300 U/kg body weight per week (epoetin‐a and beta) given for at least four weeks. For the current update we removed this criterion and we included studies or study arms with low dosages as well. We allowed dose adaptation of ESAs depending on haematological response. Concomitant supportive treatments, e.g. granulocyte colony‐stimulating factors (G‐CSF), had to be given equally in all study arms. In previous versions of this review, this criterion applied to iron supplementation as well. However, for the current update, we have changed this criterion and included trials using iron supplementation in the experimental but not in the control arm as well. We excluded trials on high‐dose myeloablative chemotherapy regimens followed by bone marrow or peripheral blood stem cell transplantation, as well as trials using erythropoietin for short‐term preoperative treatment to correct anaemia or to support collection of autologous blood prior to cancer surgery.
Included trials addressed one or more of the following comparisons of interest:
ESAs versus placebo or no treatment.
ESAs and red blood cell (RBC) transfusion as necessary versus observation and RBC transfusion as necessary, alone or with placebo.
ESAs plus conventional‐dose cancer therapy (non‐myeloablative chemotherapy and/or radiotherapy) versus identical therapy alone or with placebo.
ESAs and RBC transfusion as necessary plus conventional‐dose cancer therapy versus observation and RBC transfusion as necessary plus identical therapy, alone or with placebo.
Types of outcome measures
Primary outcomes
Haematological response
Measured as a binary outcome (proportion of patients with an increase in Hb level of 2 g/dL or more, or an increase in haematocrit of 6% points or more; measured as continuous data (change in Hb level from baseline until end of study). Of note, in the previous review we had restricted this outcome to studies with baseline Hb levels < 12 g/dL; in the current update we have removed this restriction.
Patients receiving RBC transfusions
Number of RBC units transfused per patient
Overall survival
On‐study mortality. Of note, we added on‐study mortality as a new outcome to the current update of the review.
Secondary outcomes
Tumour response (complete response)
Changes in quality of life including cancer‐related fatigue and anaemia symptoms, measured with the Functional Assessment of Cancer Therapy Anaemia (FACT‐An) Total scale (47 items), Anaemia sub‐scale (20 items), or Fatigue sub‐scale (13 items). We have chosen this instrument and its sub‐scales because they have been widely used in ESA trials and have good responsiveness to change and good convergent and discriminant validity (Cella 1997; Cella 2002; Cella 2007; Yellen 1997).
Adverse events (thromboembolic events, hypertension, haemorrhage/thrombocytopenia, rash/irritation/pruritus, seizures)
Search methods for identification of studies
We used the following sources to identify the studies for this updated review:
Previous Cochrane reviews on the effects of ESAs on cancer patients, mainly Bohlius 2006a and Bohlius 2009a; Bohlius 2009b.
Electronic search in bibliographic databases.
Conference Proceedings.
ODAC Documents 2004, 2007 and 2008 (see next section).
Reference lists of other systematic reviews and meta‐analyses.
Electronic searches Search strategies have been adapted from those suggested in the Cochrane Handbook for Systemtatic Reviews of Interventions (Lefebvre 2011). For detailed search strategies for each database, please refer to Appendix 1; Appendix 2; Appendix 3.For previous searches for this review see previous version of the review (Bohlius 2006a). For the current version, we identified relevant trials in any language through electronic searches of the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, and EMBASE. We conducted the initial search for the period 2004 to September 2009. We updated the search using the same search strategy in January 2011 and in November 2011. We did not use language restrictions. The full search strategy is on file.
Electronic searches
Search strategies have been adapted from those suggested in the Cochrane Handbook for Systemtatic Reviews of Interventions (Lefebvre 2011). For detailed search strategies for each database, please refer to Appendix 1; Appendix 2; Appendix 3.
For previous searches for this review, see previous version of the review (Bohlius 2006a). For the current version, we identified relevant trials in any language through electronic searches of the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, and EMBASE. We conducted the initial search for the period 2004 to September 2009. We updated the search using the same search strategy in January 2011 and in November 2011. We did not use language restrictions. The full search strategy is on file.
Searching other resources
Conference Proceedings
We searched conference proceedings of the American Society of Clinical Oncology, American Society of Hematology and European Society of Medical Oncology from January 1989 to December 2001 for the original Cochrane review; from January 2000 to December 2004 for the first update; and from January 2005 to November 2011 for the present update. We conducted searches of conference proceedings online, with CD‐ROMs or by handsearching.
Ongoing trials
For the previous versions of this review, we searched various sources for ongoing studies. For the current update we did not search specifically for ongoing trials in online registries.
Contact with authors
For previous versions of this review, we contacted groups or individuals as well as pharmaceutical companies who conducted randomised trials on recombinant human erythropoietin in cancer patients. For the current review, we contacted authors only to clarify eligibility of studies, if necessary.
Reference lists We checked reference lists of identified guidelines, systematic reviews and clinical trials for additional information.
Oncology Drug Advisory Committee Documents
For the current update, we evaluated documents presented at the Oncology Drug Advisory Committee (ODAC) hearing at the USA Food and Drug Administration (FDA), held in May 2004, May 2007 and March 2008. These documents include briefing documents plus additional power point presentations prepared by medical review authors of the FDA (FDA ODAC 2007; FDA ODAC 2008; Luksenburg 2004), as well as documents and additional power point presentations prepared by the companies Roche, Johnson & Johnson and Amgen (Amgen ODAC 2004; Amgen ODAC 2007; Amgen ODAC 2008; Johnson & Johnson ODAC 2004; Roche ODAC 2004). All of these documents are publicly available at FDA web pages.
Data collection and analysis
Selection of studies
Several review authors screened titles and abstracts of studies identified from the above sources according to the eligibility criteria stated previously. We did this step in duplicate. For the first Cochrane review this was undertaken by Simon Langensiepen and Julia Bohlius, for the first update this was undertaken by Jayne Wilson, Sunsan Brunskill, Julia Bohlius, Olaf Weingart and Sven Trelle. For the current update this was done by Annette Mettler, Julia Bohlius, Nadège Robert and Thomy Tonia. If eligibility could not be adequately assessed by screening the title and abstract, we obtained a full text version of the study for assessment. Studies that appeared to meet the inclusion criteria in the initial screening were further assessed for eligibility using a form containing the following questions.
Is the study described as randomised?
Did the participants in the study have a previously treated or untreated malignant disease?
Were the participants anaemic or at risk for anaemia from chemotherapy and/or radiotherapy or their malignant disease?
Was one group given Epoetin‐a or Epoetin‐ß or Darbepoetin‐alfa or any other ESA subcutaneously or intravenously?
Did the control group receive the same care (e.g. chemotherapy and supportive therapies) with or without placebo?
Did the study document relevant outcome measures?
To be eligible, studies had to meet all of the criteria stated above. If there was insufficient information to judge eligibility, we contacted the first author of the report for clarification. We resolved any disagreements between the review authors by discussion. We identified duplicate reports.
Data extraction and management
Data extraction was performed by one review author and facts were checked by a second review author. For the original Cochrane review this was done by Simon Langensiepen and Julia Bohlius. For the first update all publications until September 2004 were extracted by Julia Bohlius, Jayne Wilson and Susan Brunskill. For the current update, data were extracted by Julia Bohlius, Olaf Weingart, Annette Mettler, Nadège Robert and Thomy Tonia. For the previous version QoL data were extracted by Jayne Wilson, Susan Brunskill and Chris Hyde. For the current version, QoL data were extracted by Thomy Tonia, Annette Mettler, Nadège Robert and Julia Bohlius. For data extractions we used a standardised data extraction form. This form included the following items.
General information: title, authors, source, contact address of corresponding author, year of publication, any duplicate publications, trial setting, recruitment dates, funding.
Trial characteristics: design, method of randomisation, concealment of allocation, blinding of patients and clinicians.
Patients: sampling, inclusion and exclusion criteria, sample size, baseline characteristics, similarity of groups at baseline, diagnostic criteria, withdrawals, losses to follow‐up.
Interventions: placebo use, dose, dosing regimen, duration, route of administration, RBC transfusion trigger, co‐medications with dose, route and timing
Outcomes: outcomes as specified above.
We resolved disagreements arising at any stage by discussion and consensus.
Referencing of studies If we identified several publications for one study, we extracted the data from the most recent publication and amended this with information from other publications. We used the following suffixes to indicate the source of data.
We indicated data that were taken from either full text or abstract publication or based on personal communication with author name and year of publication
We cited data that were taken from the individual patient data meta‐analysis by Bohlius 2009a;Bohlius 2009b using the reference for the original study and adding the suffix “IPD”. For example, we cited survival data for the Hedenus 2003 which we had taken from the individual patient data meta‐analysis by Bohlius 2009a; Bohlius 2009b as "Hedenus 2003 IPD"
We assigned the following suffixes to data taken from an ODAC presentation:
J&J 2004 if we took the data from a J&J presentation for the ODAC 2004 hearing
J&J 2007 if we took the data from a J&J presentation for the ODAC 2007 hearing
Roche 2004 if we took the data from a Roche presentation for the ODAC 2004 hearing
FDA 2004 if we took the data from a FDA presentation for the ODAC 2004 hearing
FDA 2007 if we took the data from a FDA presentation for the ODAC 2007 hearing
Amgen 2007 if we took the data from an Amgen presentation for the ODAC 2007 hearing
For each unique study we assigned a five digit random number, entered for each reference in the "other" field. These numbers are identical to the numbers assigned to the studies in the IPD review by Bohlius 2009a; Bohlius 2009b. We assigned new five digit numbers for studies which we had not included in the IPD review.
For studies comparing more than one experimental arm to one control arm, we assigned a separate reference for each study arm. We labelled these study arms with the author and publication year of the main publication and added the suffixes a; b; c etc. For example, the study by Cazzola 1995 compared four different experimental study arms with one control group. The four different study arms are listed in the included studies and the data analyses as Cazzola 1995a; Cazzola 1995b; Cazzola 1995c and Cazzola 1995d.
Due to this referencing system a given study may appear more than once in the list of included studies. The total number of unique studies included is 91. For these 91 studies, a total of 198 study identifiers are listed in the sections Included studies and Characteristics of included studies.
Methods for QoL
In the previous review, we included any validated QoL instrument. For the current update, we restricted the analysis to studies meeting the inclusion criteria and also reporting QoL data using one of the following instruments.
a) FACT‐F 13: Functional Assessment of Cancer Therapy Fatigue sub‐scale, consisting of 13 fatigue‐specific questions
b) FACT‐An 20: Functional Assessment of Cancer Therapy Anaemia sub‐scale, consisting of 20 questions (13 from FACT‐F, plus 7 anaemia specific questions)
c) FACT‐An 47: Functional Assessment of Cancer Therapy Anaemia total score, consisting of 47 questions (20 from the FACT‐An sub‐scale plus 27 from the FACT‐General scale)
In the previous update, we excluded studies that did not clearly state the number of participants contributing to QoL data. For the current update, we decided to also include studies that did not report the exact number of participants contributing QoL data, in order to get as much information as possible. We included all studies reporting change between baseline and end of treatment per group. We limited the included QoL data to scores of the full instruments or sub‐scales that have been validated as stand‐alone instruments.
Rather than focusing on statistical significance, meaningful interpretation of QoL results emphasizes the degree to which differences between treatment and control arms exceed a Clinically Important Difference (CID) previously established for the QoL instruments utilized. For FACT‐Fatigue, this has been estimated to be three (Cella 2002) and for FACT‐An 20 four to five (Cella, personal communication, March 2010). For FACT‐An 47 a CID has not yet been established.
Assessment of risk of bias in included studies
Quality Assessment Two review authors independently assessed the full text articles of the eligible studies for quality. For the original Cochrane review this was undertaken by Simon Langensiepen and Julia Bohlius. For the first update this was done by Julia Bohlius and either Jayne Wilson or Susan Brunskill for the trials published until September 2004, and Julia Bohlius and Sven Trelle for trials published between September 2004 and April 2005. For the current update, this assessment was conducted by Annette Mettler, Nadège Robert and Thomy Tonia. For the original Cochrane review, we contacted all first authors or sponsoring pharmaceutical companies of the included trials in order to obtain detailed information on the study design. For the previous and current update (years 2002 to November 2011) this was not undertaken due to time limitations. However, for the IPD review (Bohlius 2009a; Bohlius 2009b) we had access to the clinical study reports of the included studies and used these to assess the quality of studies. We integrated these assessments in the current review update. For all other studies, we took this information from publications.
To assess the methodological quality and the risk of bias, we designed a quality assessment form specifically for the topic of this review, according to the recommendations in Chapter Eight of the Cochrane Handbook for Systematic Reviews ( Higgins 2011a). The sources we used for designing this form are: Alderson 2005; Jüni 2001; Moher 2001; Verhagen 1998) and the form contains the following questions.
Was allocation truly random?
Was the treatment allocation concealed?
Were study participants blinded (masked) to the treatment they received?
Were study clinicians blinded (masked) to the treatment received by individual study participants?
Did the analysis include an intention‐to‐treat (ITT) analysis?
We excluded studies from the analysis if they were not truly randomised or had inadequately concealed treatment allocation, e.g. if participants were assigned to treatments in alternate order, or according to their birth dates, or the day of the week they arrived at the treatment centre. We tested the effect of individual quality variables (allocation, blinding, ITT) in subgroup analyses. Because of the problematic use of quality summary scores, we did not use summary scores (Jüni 1999; Schulz 1995). We assessed baseline participant characteristics to see if the groups were balanced at baseline. We also assessed whether the number of patient withdrawals, dropouts and lost to follow‐up was reported for each study group; however, we did not use this information for the analyses.
For the present update we applied additional quality criteria to assess the quality of studies reporting data on tumour control. These criteria were as follows.
The study population had to be homogenous, i.e. all participants had to have the same tumour type and ‐ if relevant ‐ the same tumour stage. Alternatively, the study had to be stratified by tumour type or tumour stage.
The participants of the study had to receive a predefined, identical anticancer therapy. As above, we considered a study to meet this criterion if the study was stratified by treatment.
The study had to be designed to assess tumour response or tumour control prospectively or tumour control/response had to be the primary or secondary study outcome.
Dealing with missing data
Incomplete reporting of data
As suggested in Chapter 16 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b), we took the following steps in addressing missing data.
For studies that did not report the number of patients evaluated for a given outcome, we used the number of patients randomised per study arm as denominator. In studies where only the total number of population was reported (and not the number of patients per arm) and where the randomisation was 1:1, we assumed that randomisation was 1:1 for a given outcome as well, thus assuming that the outcome was calculated using ITT analysis.
Binary data: if only percentages but not absolute number of events were reported, we used percentages to calculate numerators.
Continous data: If estimates for mean and standard deviations (SD) were not reported, we used the methods published by Hozo et al to convert median and range estimates of outcomes such as Hb change into mean and SD (Hozo 2005). If mean change was not reported, we calculated this as the difference between end of treatment and baseline value. If SDs were not reported, we estimated them from standard errors, confidence intervals or ranges, whenever reported. If numerical data were not reported, we estimated means and/ or SDs from graphs or figures. If SDs and means were reported for subgroups only, we calculated a pooled SD by pooling the SDs of the two different subgroups. For some studies it was not clear whether the reported numbers were referring to SDs or SEs. To maximise the likelihood that our assumptions were valid, we assumed that the numbers were SDs and converted them to SEs and vice versa. We then assumed that the numbers were referring to SDs or SEs depending on which one seemed more likely for this outcome, as suggested in Deeks 1997. If mean change between baseline and end of treatment and corresponding SD was not reported, they were calculated by using a correlation coefficient. In addition, we used secondary sources to identify data that were not reported in the original publication. These secondary sources included ODAC briefing documents and other meta‐analyses. For example for QoL we retrieved data from secondary publications, that had attempted to retrieve missing information from authors (Minton 2008; Minton 2010) or imputed data (Tonelli 2009). To account for all these calculations, we conducted a subgroup analysis taking into account the source of data, as well as a sensitivity analysis differentiating between the studies for which we had to impute data in some way and those for which we did not impute any data.
Handling of discrepant data: If a study was published in several different publications, reports and presentations, we extracted the most recent or most comprehensive data. We compared the data of one study taken from different sources. If the data from different sources were discrepant, we applied the following rules to decide which data to use for analysis.
Most complete data set, e.g. where the sample size is largest OR data with consistent outcome definitions across trials were chosen for analysis.
If for one study outcome two different analyses were available (e.g. adjusted versus unadjusted analysis), we chose the unadjusted data for analysis.
Age: if age was not reported but the cancer was typical for adults, e.g. breast cancer or non‐small cell lung cancer (NSCLC), we classified the study as conducted in an “adult" population.
Assessment of heterogeneity
As suggested in Chapter 9 of the Cochrane Handbook of Systematic Reviews on Interventions (Deeks 2011), we explored potential causes of heterogeneity by performing sensitivity and subgroup analyses for primary and selected secondary outcome measures (see below). We used the P value of the homogeneity test and the I² statistic only to describe the extent of heterogeneity inherent in a meta‐analysis.
Assessment of reporting biases
In meta‐analyses with at least 10 trials, we generated a funnel plot and performed a linear regression test (Egger 1997) to examine the potential presence of bias. We considered a P value of less than 0.1 as significant for the linear regression test (Sterne 2011).
Data synthesis
We performed analyses according to the recommendations of Chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011).
We assumed a fixed‐effect model for all meta‐analyses. For binary data, we used the risk ratio as a measure of treatment effect and we used the Mantel‐Haenszel method for pooling. We used the estimated overall RR and a range of plausible values for the baseline‐risk to estimate numbers needed to benefit (NNTB) and numbers needed to harm (NNTH). For continuous data, we calculated the mean differences (MD) if the outcome was measured on the same scale in all trials. For QoL we combined only identical scales and sub‐scales in a given meta‐analysis. For time to event data, i.e. overall survival, we calculated hazard ratios (HR) based on individual patient data (IPD). If IPD were not available, we calculated the HR from published reports including secondary analyses (Bohlius 2009a; Bohlius 2009b), using methods described in Parmar et al (Parmar 1998) or binary mortality data. We performed all analyses using Review Manager (RevMan) 5.1; we used the statistical software package R (Ihaka 1996) for additional analyses that could not be done with RevMan 5.1.
In addition to subgroup analyses, we conducted random‐effects meta‐regression (see Section 9.6.4, Cochrane Handbook) for the following outcomes: Hb response, Hb change, participants receiving red blood cell transfusions, FACT‐Fatigue, FACT‐An 47 using R function rma.uni in R package metafor (Viechtbauer 2010). We used the DerSimonian‐Laird method to estimate the between‐study variance in meta‐regression. In model selection, we considered all covariates showing a significant effect (P < 0.05) in a univariate analysis. We restricted the analysis to studies providing information on all variables that were statistically significant in univariate analyses. For model selection, we used a back‐wise selection method; we removed consecutively the covariate with the largest P value as long as the P value was larger than 0.05.
In several studies different ESAs, dosages, and routes or schedules of administration were compared with one control group (Cazzola 1995; Henke 1999; Kotasek 2003; Kunikane 2001; Osterborg 1996; Smith 2003; Suzuki 2008; Ten Bokkel 1998; Thatcher 1999). For each multi‐arm study, we divided and randomly assigned control patients to the corresponding number of separate treatment groups for entry into RevMan (base model). As this might influence the weighting of the studies and thus the pooled results, we alternatively merged the two (or more) active arms of one study into one single experimental arm and compared it to the entire control group. We compared and described results for each outcome.
Subgroup analysis and investigation of heterogeneity
We conducted subgroup analyses using the following factors, if appropriate.·
Hb at study entry (Hb level < 10 g/dL versus 10 to 12 g/dL versus >12 g/dL versus unclear/not reported)
Solid tumours versus haematological malignancies (excluding myelodysplastic syndrome (MDS)) versus MDS versus mixed versus unclear versus not reported)
Age (children versus adults)
Age (only children versus adults > 18 years versus > 70% non‐elderly adults aged 18‐65 versus only non‐elderly adults versus > 70% elderly adults aged > 65 years versus only elderly adults aged > 65 years)
Type of treatment given (chemotherapy versus radiotherapy/radiochemotherapy versus no therapy versus other)
Type of treatment given (> 70% of patients receiving platinum‐based chemotherapy versus < 70% of patients receiving platinum‐based chemotherapy versus chemotherapy without platinum versus chemotherapy some (not quantified) patients receiving platinum versus chemotherapy no details given versus radiochemotherapy versus radiotherapy versus no therapy versus other). We categorised studies with less than 70% of patients receiving chemotherapy as “other” (P‐174 IPD; Rose 1994 IPD)
Short‐lasting ESA versus long‐lasting ESA
Duration of ESA medication (six to nine weeks versus 12 to 16 weeks versus more than 20 weeks)
Iron supplementation (fixed iron supplementation versus iron as necessary versus no explicit statement/no iron versus explicit NO iron versus iron handled differently in study arm)
Study quality parameters (concealment of allocation, masking, intention‐to‐treat analysis)
Source of data (full text publications versus abstract publications versus unreported data versus data reported at FDA/ODAC hearing versus other)
Compared to the previous version of this review, we added new subgroups to differentiate with more detail different age groups and different anti‐cancer therapy groups. For the subgroup “iron supplementation”, we added the categories “iron given differently in both study arms”, because of the change in the inclusion criteria described above and “explicitly stated NO iron”. However, no study was included in the latter subgroup. For the subgroup “publication”, we added the category “other", containing clinical trial results from sources that did not fit any other category. We dropped the following subgroup analyses as they did not seem to be relevant any longer or insufficient information was available: Number of drop outs documented; use of G‐CSF.
Sensitivity analysis
To test the robustness of the results, we conducted random‐effects meta‐analyses. We reported the estimates of the random‐effects only a) if they showed a difference to the fixed‐effect model or b) if they were necessary to allow for comparison with other meta‐analyses in the discussion section. We explored the influence of single large studies and the influence of different data sets, e.g. adjusted versus unadjusted data.
Results
Description of studies
Results of the search
Our initial literature search in March 2001 retrieved 1,592 references. For the first update of this review the Birmingham team identified and screened another 1,859 references. For the current update, we identified and screened a total of 2,207 references (999 at the first search on September 2009 and 1208 at the two searches conducted in 2011 (January and November)). For details, see the PRISMA flow diagram in Figure 1.
1.

Study flow diagram.
Included studies
The previous update of the Cochrane review (Bohlius 2006a) evaluated 57 studies with 9,353 participants. In the current update we include a total of 91 studies with 20,102 participants. All included trials were reported in English. Details are displayed in the Characteristics of included studies table. For those 91 studies, 198 references were included, see details as described in "Referencing of studies" in the Methods section.
Studies that were previously excluded and are now included
Four of the previously excluded studies are included in the current update, due to the change in the iron supplementation rule: for this update, studies are also included if they had different iron supplementation policies between the different study arms (Blohmer 2011; Moebus 2007; Rosen 2003; Sweeney 1998). We had previously excluded another study by mistake, we have now included this study (Gebbia 2003).
Studies that were previously included and are now excluded
We excluded two of the previously included studies (Henze 2002; Vadhan‐Raj 2004 ) because a substantial number of participants underwent major surgical procedures during ESA treatment.
Studies that were previously ongoing and are now included
We included four studies that were previously ongoing (Aapro 2008; Antonadou 2001; Charu 2007; Pronzato 2010).
Updated data for already included studies
If new publications supplemented or updated information from earlier sources, we added the new data and cited the new source as the study name. This led to the following changes: we replaced Coiffier 2001 with Boogaerts 2003, Janinis 2003 with Christodoulou 2009, EPO‐CAN‐15 with Goss 2005, N93 004 with Grote 2005, EPO‐GBR‐7 with Hoskin 2009, Machtay 2004 with Machtay 2007, Milroy 2003 with Milroy 2011, Savonije 2004 with Savonije 2005, GOG0109 with Thomas 2008, EPO‐CAN‐20 with Wright 2007, we amended Razzouk 2004 with Razzouk 2006, and Pronzato 2002 with Pronzato 2010.
Newly identified studies
Screening the references of other reviews on this subject, led to the identification and inclusion of three new studies (Gebbia 2003; ML17616 2006; ML17620 2006 ). We included three studies (EPO‐GER‐20 IPD; Kotasek 2002 IPD; OBE/EPO‐INT‐03 IPD) that were previously unpublished and retrieved for the IPD review (Bohlius 2009a; Bohlius 2009b). We identified 23 additional new studies that were published after the search for the previous review was conducted. We included these studies in the present update. From those, we had also included 11 in the IPD review (Aapro 2008; Debus 2006 J&J 2007; Gordon 2008; Hernandez 2009; Milroy 2011; Pirker 2008; Ray‐Coquard 2009; Smith 2008; Strauss 2008; Untch 2011_1; Wilkinson 2006) and we identified twelve from the literature search update (Engert 2010; Fujisaka 2011; Gupta 2009; Katakami 2008; Krzakowski 2008; Mystakidou 2005; Overgaard 2009; Suzuki 2008b; Tsuboi 2009; Tjulandin 2010; Tjulandin 2011; Winquist 2009).
Other changes
In the previous review (Bohlius 2006a), we had excluded studies and study arms with very low ESA dosages, in the current update we included all studies and study arms regardless of ESA dosage, for example see Cazzola 1995.
Study population
Hb level: We grouped studies by mean or median baseline Hb level at study entry. Thirty studies examined a study population with mean or median Hb below 10 g/dL at study entry, 38 had a baseline Hb between 10 and 12 g/dL and 18 studies sought to prevent anaemia, thus Hb at baseline was > 12 g/dL. Because of missing information, five studies could not be categorized Debus 2006 J&J 2004; EPO‐GER‐20 IPD; ML17620 2006; OBE/EPO‐INT‐03 IPD; P‐174 J&J 2004). Trials that directly compared the outcomes of initiating erythropoietin treatment at alternative Hb thresholds were not included in the present review.
Disease: Fifty‐nine studies analysed participants with solid tumours only, 12 studies included patients with haematological malignancies only, two trials included exclusively patients with MDS (Italian 1998; Thompson 2000) while 18 trials included patients with both solid tumours and haematological malignancies.
Treatment: The majority of participants received concomitant chemotherapy, which was given in 63 studies. In seven studies participants were treated with radiotherapy and in eight with radiochemotherapy. In nine trials no concomitant anticancer therapy was given. Finally, we categorized the type of anti‐cancer therapy administered as "unclear" in one study (Winquist 2009) and three studies with less than 70% of patients given chemotherapy as "other" (P‐174 J&J 2004; Rose 1994; Rosenzweig 2004).
Age: All studies but one (Razzouk 2006) evaluated adult participants.
Intervention: All trials compared erythropoiesis‐stimulating treatment initiated at study entry (plus RBC transfusion if necessary) with observation and transfusion of RBCs when the patient's Hb level fell below a defined threshold or at the discretion of the treating physician.
Study drug: Short‐lasting erythropoietins (including epoetin alpha, epoetin beta, epoetin theta) were administered in 76 studies and darbepoetin in 15 studies.
Duration: Duration of study medication was up to nine weeks in 17 studies, between 12 and 16 weeks in 50 studies and more than 17 weeks in 21 studies. In three studies the duration of study drug administration was unclear or not reported (EPO‐GER‐20 IPD; EPO‐INT‐1 J&J 2004; OBE/EPO‐INT‐03 IPD).
Route of administration: In all but three studies erythropoietin was administered subcutaneously. In two studies erythropoietin was given intravenously (Razzouk 2006; Wurnig 1996). Another study compared intravenous with subcutaneous administration (Henke 1999).
More details are provided in the table Characteristics of included studies.
Excluded studies
Overall, we excluded 227 trials, for reasons documented in the Characteristics of excluded studies. Thirty studies were excluded as ongoing trials (see next section) while one study was not retrievable.The largest group was excluded for not being randomised controlled trials (98 studies). We excluded 48 studies because participants of both study arms received ESAs, while we excluded 13 studies since they randomised less than 10 participants per study arm, our current threshold for inclusion. We excluded two previously included studies (Henze 2002; Vadhan‐Raj 2004) from this update, since most of their participants underwent surgery during the study; the same reason for exclusion was applied to another eight studies. Three studies were excluded due to the participants not having cancer, while three more due to the participants having acute leukaemia. Finally, 21 studies were excluded for other reasons, documented in the Characteristics of excluded studies.
Ongoing trials Overall, we identified 30 studies that are currently ongoing. For the previous Cochrane update, 29 trials were identified as ongoing. Since then, five were completed and are included in the present meta‐analysis (Aapro 2008; Antonadou 2001; Charu 2007; Pronzato 2010; Thomas 2008). We identified a mistake in the ongoing trials of the previous version: namely CDR0000068669 and EORTC 22996‐24002 were in fact the same study, now identified as Lambin 2006.Three of the previously ongoing trials are now excluded (Elsaid 2001; Miller 2004; Steensma 2011). Additionally, note that we were uncertain whether H Thomas 1997 and R Thomas 2002 are the same studies as the included Thomas 2002. We did not contact the authors and we, therefore, refer to these three documents as separate studies, with the first two still considered as ongoing trials. The remaining 20 trials are still ongoing.
We newly identified another 10 trials ongoing. We had excluded one (Gamucci 1993) in the previous Cochrane update and we identified another six (Boehrer 2010; Delarue 2009; Gascon 2010; Ghavamzadeh 2010; Liang 2009; Yousseff 2011) by the 2011 literature search. We identified the remaining three (Nitz 2008; Park 1996 and Rexer 2006) by other sources.
Risk of bias in included studies
For risk of bias table see Figure 2.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study. If for a given study more than one reference was included we reported our judgement only for the main reference and left the other references of the same study empty.
Allocation
Randomisation and concealment of allocation.
All included studies were described by the authors as randomised. For 27 studies we had some information on the methods used for randomisation, for 64 studies details were unavailable or the reporting was unclear. For 50 studies we judged the method for concealing allocation of treatment to be adequate. In 41 studies the method for allocation concealment could not be determined.
Blinding
Masking Forty‐six trials used a placebo control, 45 trials did not.
Incomplete outcome data
Most studies included intention‐to‐treat analyses in their reports, or excluded less than 10% of the patients randomised in the study from the analysis. However, the number of participants evaluated in a study varied between the outcomes assessed. Therefore, for each of the outcomes, we made an assessment as to whether or not the analysis was based on intention‐to‐treat or excluded less than 10% of the participants initially included. This information is displayed in the specific outcomes section in RevMan.
Selective reporting
For the first version of the Cochrane review, we contacted first authors to obtain unreported data on study design, participant characteristics and selected outcome data. For 19 of the 27 trials included in the first Cochrane review additional unpublished data were provided by the authors or pharmaceutical companies (Abels 1993; Cascinu 1994; Case 1993; Cazzola 1995; Boogaerts Coiffier 2001; Dammacco 2001; Del Mastro 1997; Henry 1995; Italian 1998; Kurz 1997; Littlewood 2001; Oberhoff 1998; Osterborg 1996; Osterborg 2002; Rose 1994; Ten Bokkel 1998; Thatcher 1999; Thompson 2000; Throuvalas 2000). For the update of the present review, authors of published reports were not contacted to obtain missing information.
Publication bias Funnel plot analyses were performed to investigate publication bias or other biases and are reported in the specific outcome sections.
Reporting bias No single outcome was reported consistently by all studies (N = 91) included in this systematic review. Some outcomes were estimated based on large proportions of the 91 studies and 20,102 participants included:
95% for overall survival (19,003/20,102), 79% for on‐study mortality (15,935/20,102), 80% for risk of transfusions (16,093/20,102), 77% for risk of thromboembolic events (15,498/20,102) and 58% for change in Hb (11,609/20,102). For other outcomes, fewer participants were included in the meta‐analyses: 36% (7,228/20,102) for hypertension, 32% (6,413/20,102) for haematologic response, 25% (5,012/20,102) for complete tumour response, 25% (5,012/20,102) for number of units transfused and 22% (4,507/20,102) for thrombocytopenia/haemorrhage.
For some outcomes only small proportions of participants could be evaluated, which questions the validity of the results achieved: 14% (2,890/20.102) for seizure, 12% (2,485/20,102) for rash.
Statistically significant differences between data taken from full text publications, abstract publications and unpublished data were found in the subgroups analyses for Hb response, Hb change, risk for transfusions and number of units transfused.
Other potential sources of bias
For some studies more than one source of data was available (e.g. unpublished data from the authors, FDA reports, IPD review). As for intention‐to‐treat mentioned above, we recorded the source of data separately for each outcome.
Effects of interventions
See: Table 1
Primary outcomes
(1) Haematological response
We defined this binary outcome as the proportion of participants with an increase in haemoglobin (Hb) level of 2 g/dL or more, or increase in haematocrit of six percentage points or more, unrelated to transfusion.
Overall, 31 trials including 6,413 participants were analysed. Of those studies, 22 trials including 4,307 participants were included in the previous Cochrane reviews (1985 to 2006). Nine trials (N= 2,106) were newly identified and added to the analysis (Aapro 2008; Charu 2007; Milroy 2011; ML17616 2006; ML17620 2006; Razzouk 2006; Suzuki 2008; Tjulandin 2010; Tjulandin 2011). As some of the trials (Cazzola 1995; Hedenus 2002; Kotasek 2003; Osterborg 1996; Smith 2003; Suzuki 2008; Tjulandin 2010) were split into subsets for analysis purposes, the number of trials displayed is 46.
We observed haematological response in 2,050 out of 3,710 participants in the erythropoietin and darbepoetin groups compared with 434 of 2,703 in the control groups, corresponding to a risk ratio (RR) for haematological response under the treatment with erythropoietin or darbepoetin of (RR 3.39; 95% confidence interval (CI) 3.10 to 3.71). There was significant statistical heterogeneity between the trials (I²= 53%), indicating that variation between trials in the magnitude of ESA effects on haematological response was larger than what would be expected from chance alone. However, all studies indicated a beneficial effect of ESAs with regard to haematological response. The funnel plot analysis was asymmetric (P = 0.0015), suggesting that beneficial effects were over reported.
In seven studies (Cazzola 1995; Hedenus 2002; Kotasek 2003; Osterborg 1996; Smith 2003; Suzuki 2008; Tjulandin 2010), two or more epoetin dosages or preparations were compared with one control group. Merging the active arms into one experimental arm for each of those four studies did not influence the overall result markedly (RR 3.42; 95% CI 3.12 to 3.74). Compared with the previous review (RR= 3.43 (95% CI 3.07 to 3.84, 22 trials, N = 4,307, Bohlius 2006a) neither the point estimate, nor the confidence interval have changed substantially.
To identify the source(s) of heterogeneity, subgroup analyses were performed. Univariate analyses identified significant differences (P < 0.05) between subgroups for baseline Hb level, age, type of anti‐cancer therapy, iron supplementation, duration of treatment, placebo control and type of publication. The backward selection resulted in a multivariate model containing the covariates Hb at baseline, age and iron supplementation. The final model is presented in Additional Table 2. For each combination of Hb at baseline, age and type of iron supplementation the risk ratio can be calculated from Table 2. For example, the logarithm of the risk ratio for a trial including adults with Hb between 10 and 12 g/dL at baseline and receiving iron as necessary is Intercept + adults + Hb 10‐12 g/dL + iron given as necessary = 0.81 + 0.62 + 0.35 = 1.78. Accordingly, the risk ratio is 5.93.
1. Haematologic response: results of meta‐regression analysis.
| Variable | log (effect size) | standard error | P value |
| Intercept | 0.81 | 0.1189 | <0.0001 |
| Hb baseline 10‐12 g/dL | 0.62 | 0.1430 | <0.0001 |
| Hb baseline > 12 g/dL | 0.85 | 0.4694 | 0.0688 |
| Children | ‐0.68 | 0.1653 | <0.0001 |
| Iron given differently in both study arms | ‐0.64 | 0.2348 | 0.0068 |
| Iron supplementation as necessary | 0.35 | 0.1315 | 0.0081 |
Hb: haemoglobin
We calculated numbers needed to benefit (NNTB) for several hypothetical baseline risks. In a population with an underlying risk [likelihood] of 6% to achieve haematological response, the NNTB would be 6.97 (95% CI 6.15 to 7.94); thus, about seven patients would need to be treated to achieve one additional Hb responder. In a population with an underlying risk of 16% the NNTB would be 2.62 (95% CI 2.31 to 2.98); thus, about three patients would need to be treated to achieve one additional Hb responder. In a population with a hypothetical baseline risk of 30% the NNTB would be 1.39 (95% CI 1.23 to 1.59); thus, one to two patients would need to be treated to achieve one additional Hb responder.
Overall, the analysis confirms prior evidence that ESAs yield haematological response in most but not all patients with malignant disease.
(2) Change in haemoglobin level from baseline until end of study
Fifty‐six studies including 11,609 participants reported the hb change from the start until the end of the study. Fifteen of those were included in the 2006 update (Bohlius 2006a). As some of the trials had multiple experimental arms (Cazzola 1995; Hedenus 2002; Henke 1999; Kotasek 2003; Krzakowski 2008; Kunikane 2001; Osterborg 1996; Smith 2003; Ten Bokkel 1998; Tjulandin 2010), the number of trials displayed in MetaView is 75. For this update, we included not only studies that reported the mean Hb change from baseline, but also studies that reported baseline and end of treatment (EOT) Hb values only, see Methods section.
The meta‐analysis showed that the mean difference was 1.57 (95% CI 1.51 to 1.62), showing a statistically significant difference in favour of treatment. There was, however, substantial heterogeneity between the trials (test for heterogeneity I² = 87%), although all but one study indicated a beneficial effect of ESAs with regard to Hb change. Funnel plot analysis did show some evidence for significant asymmetry (P = 0.037), suggesting that beneficial findings were over reported. Merging each multi‐arm trial into a single data set (i.e. a two‐arm trial) did not change the results (mean difference (MD) 1.56, 95% CI 1.51 to 1.62).
Examining the single studies, most of them reported a statistically significant change in Hb level for participants treated with erythropoietin or darbepoetin. A few studies, however, did not report a significant effect on Hb change (Cazzola 1995; Leyland‐Jones 2005; Razzouk 2006). Overall, the MD ranged from (MD ‐0.06; 95% CI ‐1.77 to 1.65, Cazzola 1995a) to (MD 3.30; 95% CI 1.13 to 5.47, Henke 1999c).
To identify the source(s) of heterogeneity, we performed subgroup analyses. Univariate analyses identified significant differences between subgroups for baseline Hb level, different malignancies, age, type of anti‐cancer therapy, short‐lasting versus long‐lasting ESA, duration of ESA treatment, iron supplementation, masking, intention‐to‐treat and type of publication. The backward selection resulted in a multivariate model containing the covariates type of ESA and age. The final model is presented in Additional Table 3 For each combination of type of ESA and age (adults or children) the mean difference can be calculated from Table 3. For example, the mean differences for a trial in adult patients receiving short‐lasting ESA is = Intercept + short lasting ESA = 1.15 + 0.56 = 1.71.
2. Hb change: results of meta‐regression analysis.
| Variable | mean difference | standard error | P value |
| Intercept | 1.15 | 0.1792 | <0.0001 |
| Children | ‐1.41 | 0.6911 | 0.0414 |
| Short acting ESA | 0.56 | 0.2041 | 0.0060 |
ESA: erythropoiesis stimulating agent
Overall, there is a statistically significant effect of ESAs on Hb change; compared with controls patients receiving ESAs achieve on average an increase of Hb levels of 1.57 g/dL from baseline to end of treatment (between 1.51 and 1.62 g/dL in 95% of patients).
(3) Patients receiving RBC transfusions
Overall, the updated analysis included 70 trials with 16,093 participants. Of those, 42 trials with 6,510 participants were included in the previous Cochrane review (Bohlius 2006a). Thirty trials were newly identified and added to the analysis. (Aapro 2008; Blohmer 2011; Charu 2007; Engert 2010; EPO‐INT‐3 J&J 2004; Fujisaka 2011; Gebbia 2003; Gordon 2008; Goss 2005; Grote 2005; Gupta 2009; Hernandez 2009; Katakami 2008; Krzakowski 2008; Leyland‐Jones 2005; Milroy 2011; Moebus 2007; O'Shaughnessy 2005; Pronzato 2010; Pirker 2008; Ray‐Coquard 2009; Rosen 2003; Smith 2008; Strauss 2008; Tjulandin 2010; Tjulandin 2011; Tsuboi 2009; Untch 2011_1; Wilkinson 2006; Wright 2007). Two studies that were included in the previous review (Henze 2002; Vadhan‐Raj 2004 ) were excluded from the current version because study participants received major surgery during ESA treatment. As some trials with multiple experimental arms were split into subsets (Cazzola 1995; Hedenus 2002; Kotasek 2003; Krzakowski 2008; Kunikane 2001; Osterborg 1996; Smith 2003;Ten Bokkel 1998; Thatcher 1999; Tjulandin 2010) the number of trials displayed is 88.
The risk ratio to receive red blood cell transfusions was statistically significantly reduced in the study groups receiving ESAs by 35% (RR 0.65, 95% CI 0.62 to 0.68). There was statistically significant heterogeneity between the trials (I² = 60%) indicating that variation in the effect of ESAs between trials was larger than would have resulted from chance alone. However, the majority of studies indicated a beneficial effect of ESAs with regard to the need of red blood cell transfusions. A funnel plot analysis showed significant asymmetry between the studies (P < 0.00001), suggesting that beneficial findings were over reported. Ten studies compared two or more ESA dosages/formulations with one control group. Merging the active arms of each study into a single experimental arm and comparing it to the study's entire control group did not substantially change the overall result (RR 0.65; 95% CI 0.62 to 0.68). Compared with the previous version of this review, the results did not change markedly (Bohlius 2006a: RR 0.64, 95% CI 0.60 to 0.68, 42 trials, N = 6,510).
To identify the source(s) of heterogeneity, we performed subgroup analyses. Univariate analyses identified significant differences (P < 0.05) between subgroups for baseline Hb level, different malignancies, age, type of anti‐cancer therapy, iron supplementation, concealment of allocation, placebo control, intention‐to‐treat analysis and type of publication. The backward selection resulted in a multivariate model containing the covariates Hb at baseline and underlying malignancy. The final model is presented in Additional Table 4. For each combination of Hb level and type of malignancy, the risk ratio can be calculated from Table 4. For example, the logarithm of the risk ratio for a trial in patients with solid tumours and baseline Hb level 10‐12 g/dL is = Intercept + solid + Hb 10 to 12 g/dL = ‐0.22 + ‐0.39 + ‐0.15 = ‐0.76. Accordingly, the risk ratio is 0.47.
3. Participants receiving RBC transfusions: results of meta‐regression analysis.
| Variable | log(effect size) | Standard error | P value |
| Intercept | ‐0.22 | 0.0506 | <0.0001 |
| Hb 10 ‐ 12 g/dL | ‐0.15 | 0.0650 | 0.0254 |
| Hb > 12 g/dL | 0.07 | 0.0601 | 0.2774 |
| MDS | 0.01 | 0.1004 | 0.8967 |
| Solid and haematological tumours | ‐0.03 | 0.0648 | 0.6726 |
| Solid tumours | ‐0.39 | 0.0637 | <0.0001 |
MDS: myelodysplastic syndrome RBC: red blood cell
To estimate the absolute effectiveness of erythropoietin, we applied the overall risk ratio of (RR 0.65; 95% CI 0.62 to 0.68) to a range of plausible values for the baseline‐risk. In a hypothesised population with an estimated risk of 30% to require RBC transfusions the NNTB is 9.52 (95% CI 8.77 to 10.42): about nine to 10 patients would need to receive ESAs to spare one patient from RBC transfusion. In a hypothesised population with an estimated risk of 50% to require RBC transfusions, the NNTB is 5.71 (95% CI 5.26 to 6.25): about five to six patients would need to receive erythropoietin to spare one patient from RBC transfusion. In a hypothesised population with an estimated risk of 70% to require RBC transfusions the NNTB is 4.08 (95% CI 3.76 to 4.46). In this setting about four patients would need to receive erythropoietin to spare one patient from RBC transfusion.
Overall, the data confirm results from prior analyses that ESAs reduce the risk ratio to receive RBC transfusions in patients with malignant disease. The effect size might be influenced by the underlying disease.
(4) Number of red blood cell units transfused
Overall, 19 studies evaluating a total of 4,715 patients are included in this update. Of those, 14 studies with 2,353 patients were included in the previous review (Bohlius 2006a). Five trials with 2,362 participants were newly identified and added to the analysis (Engert 2009; Grote 2005; Hernandez 2009; Savonije 2005; Thatcher 1999). As four multi‐arm studies were split into subsets (Ten Bokkel 1998; Thatcher 1999; Osterborg 1996; Cazzola 1995), the number of studies displayed in Meta‐View is 25.
The overall mean difference showed a statistically significant benefit for participants receiving ESAs (MD ‐0.98; 95% CI ‐1.17 to ‐0.78): the ESA group received on average 0.98 units of blood less per participant than the control group, who received an average of 3.65 units. Overall, there was moderate statistical heterogeneity between the trials (I² = 30%). All but one study indicated a reduced need of red blood cell units in patients receiving ESAs compared to controls. A funnel plot analysis did not show statistically significant asymmetry (P = 0.558). In four studies, two or more different ESA dosages were compared with one control group (Cazzola 1995; Osterborg 1996; Ten Bokkel 1998; Thatcher 1999). Merging the active arms of each study into a single experimental arm and comparing each to that study's entire control group did not substantially change the overall result (MD ‐0.98; 95% CI ‐1.17 to ‐0.78). Compared with the previous review (Bohlius 2006a: MD ‐1.05; 95% CI ‐1.32 to ‐0.78, 14 trials, N = 2,353), the overall result did not change markedly.
Subgroup analyses were conducted for all the comparisons and were found to be statistically significant for different age groups (test between subgroups P = 0.02), duration of ESA therapy (test between subgroups P = 0.03) and type of publication (test between subgroups P = 0.04). However, the absolute differences between subgroups were small.
Overall, the analysis suggests that ESAs modestly but statistically significantly reduces the number of RBC units transfused per patient.
(5) Overall survival
We defined overall survival as longest follow‐up available. Overall survival data were available from a total of 78 trials including 19,003 participants. Of those, 42 trials including 8,167 participants were included in the 2006 Cochrane review (Bohlius 2006a). Of these, we excluded one study which we had included in the previous review Vadhan‐Raj 2004 from the current version because study participants received major surgery during ESA treatment. For 30 previously included studies data were updated with newly available information from the individual patient meta‐analysis (Bohlius 2009a; Bohlius 2009b). Thirty‐seven trials were newly identified and added to the analysis Aapro 2008; Antonadou 2001; Blohmer 2011; Charu 2007 IPD; Christodoulou 2009; Debus 2006 IPD; Engert 2010; EPO‐GER‐20 IPD; Fujisaka 2011; Gordon 2008 IPD; Gupta 2009; Hernandez 2009; Huddart 2002 IPD; Kotasek 2002 IPD; Krzakowski 2008; Milroy 2003 IPD; ML17616 2006; ML17620 2006; Moebus 2007 IPD; Mystakidou 2005; OBE/EPO‐INT‐03 IPD; Overgaard 2009; Pirker 2008 IPD; Pronzato 2010 IPD; Quirt 1996 IPD; Ray‐Coquard 2009 IPD; Rosen 2003; Strauss 2008 IPD; Strauss 2008 IPD; Sweeney 1998; Thomas 2002 IPD; Tjulandin 2010; Tjulandin 2011; Tsuboi 2009; Untch 2011_2; Wilkinson 2006 IPD; Winquist 2009. Two studies (Krzakowski 2008; Tjulandin 2010) were split into subsets and four studies (Cascinu 1994; Hedenus 2002; Kurz 1997; Sweeney 1998) reported zero events; as a result the overall number of studies displayed in Meta‐View is 80.
The overall estimate is a hazard ratio (HR) of 1.05 (95% CI 1.00 to 1.11) in favour of placebo/no treatment. The heterogeneity between the trials was low, with an I² of 21%. Funnel plot analysis did not suggest asymmetry (P = 0.92).
In two studies (Krzakowski 2008; Tjulandin 2010), two different ESA dosages or formulations were compared with one control group. Merging the active arms into one single experimental arm compared with the entire control group did not influence the overall result (HR 1.05; 95% CI 1.00 to 1.11).
Although no statistically significant heterogeneity was apparent, we conducted subgroup analysis to explore the underlying clinical heterogeneity to assess the influence of clinical differences between the studies. Tests for heterogeneity between subgroups showed statistically significant differences for the analyses of baseline Hb levels (P = 0.02), iron supplementation (P = 0.005) and intention‐to‐treat analysis (P = 0.02). However, when excluding studies with unclear values for the subgroup analyses conducted, none of the analyses remained statistically significant. Statistically significant differences were not detected for any of the other subgroup analyses conducted.
We further investigated how single large studies influenced the overall results. There was no single study that contributed more than 10% weight to the overall analysis. There were four studies which each contributed more than 5% weight to the analysis (Aapro 2008 IPD; Debus 2006 IPD; Pirker 2008 IPD; Smith 2008 IPD). Taken together these four studies contributed 27% weight to the overall analysis. Of those, two suggested a negative impact on survival (Aapro 2008 IPD; Smith 2008 IPD) and two suggested a beneficial impact on overall survival (Debus 2006 IPD; Pirker 2008 IPD). Exclusion of the two unfavourable studies resulted in an HR of 1.04 (95% CI 0.98 to 1.10). Exclusion of the two favourable studies resulted in an HR of 1.08 (95% CI 1.02 to 1.14). We also investigated the effects of adjusted and unadjusted data where different results were reported (Henke 2003; Littlewood 2001). Using adjusted instead of unadjusted data for the Henke 2003 and Littlewood 2001 studies did not change the overall result (HR 1.05, 95% CI 1.00 to 1.11; adjusted data).
In summary, there is no evidence that erythropoietin or darbepoetin improves overall survival. Based on the data available it was not possible to clearly identify a subgroup of participants that was at higher or lower risk to experience detrimental effects from ESAs.
(6) On‐study mortality
We defined on‐study mortality as deaths occurring up to 30 days after the active study period. Such data were available for 78 studies including 15,935 patients. Two studies (Krzakowski 2008; Tjulandin 2010) were split into subsets and eight studies (Cascinu 1994; Del Mastro 1997; Hedenus 2002; Kurz 1997; Moebus 2007 IPD; Strauss 2008 IPD; Sweeney 1998; Untch 2008 IPD) reported zero events; as a result, the overall number of studies displayed in Meta‐View is 72.
The overall estimate showed an HR of 1.17 (HR 1.17; 95% CI 1.06 to 1.29) in favour of control. There was no heterogeneity between the studies (I² = 0%). A funnel plot analysis did not show evidence for significant asymmetry (P = 0.693).
Although there was no evidence for any statistical heterogeneity between the studies (I² = 0%), we conducted predefined subgroup analyses. Univariate analysis identified statistically significant differences only for intention‐to‐treat analyses (P = 0.04). No robust statistically significant differences were identified for any of the other subgroups of interest (i.e. baseline Hb level, type of malignancy, duration of treatment, type of anti‐cancer therapy, age, iron supplementation, type of publication, epoetin versus darbepoetin, type of data, concealment of allocation and masking).
We conducted a sensitivity analysis including eight additional studies. For seven of those (Antonadou 2001; Blohmer 2011; Christodoulou 2009; Engert 2009; Gupta 2009; Overgaard 2009; Winquist 2009), we calculated on‐study mortality from Kaplan Meier curves for overall survival and for the remaining study (Tsuboi 2009), we used long‐term mortality data. This sensitivity analysis yielded similar results; with an HR of 1.16 (95% CI 1.05 to 1.27, 78 trials, N=19,018).
We further investigated how single large studies influenced the overall results. There were two studies (Leyland‐Jones 2005 IPD; Smith 2008 IPD) which each contributed more than 10% weight to the analysis. Taken together these four studies contributed 28% weight to the overall analysis. Both studies suggested a negative impact on mortality. Exclusion of these two unfavourable studies resulted in an HR of 1.09 (95% CI 0.97 to 1.23).
Overall, there is evidence that ESA treatment increases mortality in cancer patients during active study period compared with controls.
Secondary outcomes
(7) Tumour response (complete response)
Tumour response (complete response) data were available from a total of 15 trials including 5,012 participants. Of these, 11 trials were included in the previous Cochrane review (Bohlius 2006a). Two previously included studies (Bamias 2003; Vadhan‐Raj 2004) were excluded from the current update since they did not explicitly state that they evaluated complete tumour response. We replaced previous data with updated study results where available (Grote 2005; Hoskin 2009; Machtay 2007). We included four additional studies published since 2006 (Engert 2009; Strauss 2008; Untch 2011_1; Wilkinson 2006). Since two multi‐arm trials were split into subsets (Cazzola 1995; Ten Bokkel 1998) the number of trials displayed in MetaView is 19.
The overall estimate shows a risk ratio of 1.02 (RR 1.02; 95% CI 0.98 to 1.06) that was not statistically significant. There was no significant heterogeneity between the trials (I² = 0%). Funnel plot analysis did not show strong evidence for asymmetry (P = 0.149). Merging the multi‐arm trial into one data set did not change the overall result (RR 1.02; 95% CI 0.98 to 1.06, 15 trials). Compared to the previous report (RR fixed‐effect: 1.12; 95% CI 1.01 to 1.23, random‐effect: 1.09, 95% CI 0.94 to 1.26, 13 trials , N = 2833), the updated review shows more conservative results. Only five of the included studies (Engert 2009; Hoskin 2009 GBR‐7 FDA 04; Machtay 2007; Strauss 2008; Untch 2011_1) met our specific quality criteria for assessment of tumour response (see Methods section). For the five studies meeting these criteria, the risk ratio was 0.99 (95% CI 0.95 to 1.02, five studies, N=2,476). For the remaining 10 studies with low quality the point estimate for RR suggested there might be a benefit for patients receiving ESAs, but the confidence interval did not reach statistical significance (RR 1.15, 95% CI 0.98 to 1.36, 10 trials, N = 2,536), with some evidence for a difference between subgroups tested (P = 0.07).
In conclusion, the data available suggest that ESAs do not have a beneficial effect on tumour control. The data are insufficient to exclude detrimental effects.
(8) Changes of health‐related quality of life
Twenty‐three studies including 5,584 patients reported results on QoL, as measured with FACT‐F, FACT‐An 20 or FACT‐An 47. In order to perform a meta‐analysis for the FACT measures, we had to extract means and SDs. In cases where no numerical data were given, we calculated means and/ or SDs from graphs or figures (Boogaerts 2003; Charu 2007; Gordon 2008; Hedenus 2003). In one trial (Christodoulou 2009) where SDs were reported separately for platinum and non platinum chemotherapy, we calculated a pooled SD by pooling the SDs of the two different subgroups. For the same study we also imputed the mean and the SD for changes between baseline and end of treatment, by using a correlation coefficient. For one study with missing SDs (Littlewood 2001) and no other way of imputing them, we used the SDs that have been already published by another meta‐analysis (Tonelli 2009). According to the authors of this meta‐analysis, the SDs were calculated as follows: for FACT‐fatigue they imputed the SD using the baseline SD reported in another publication for the same study (Fairclough 2003) and for the FACT‐An the SD was imputed using the average of the SDs from other studies who reported a SD for FACT‐An (personal communication with Dr. Lloyd, February 2010). For two further studies (Kotasek 2003; Vansteenkiste 2002), we used the mean and SDs reported in a meta‐analysis by Minton and colleagues (Minton 2008). These data were not available in the publications and were obtained by the authors of the meta‐analysis from the authors of the original studies or the pharmaceutical companies (personal communication with Dr. Minton, February 2010). To account for all these calculations, we conducted a sensitivity analysis, differentiating between the studies for which we had to impute data in some way and those for which we did not impute any data. One study (Christodoulou 2009) reported results separately for participants treated with platinum‐based chemotherapy and those treated with non‐platinum‐based chemotherapy. It is therefore included in both the platinum and non‐platinum chemotherapy subgroups for all the QoL outcomes below.
a) FACT‐F 13 sub‐scale
A total of 18 studies (4,965 patients) reported data for this outcome. The MD was 2.08 (95% CI 1.43 to 2.72). Heterogeneity between the included studies was moderate (I² = 53%). A funnel plot analysis showed significant asymmetry (P = 0.02772) with over reporting of studies that showed beneficial effects of ESAs.
The beneficial effect of ESAs on QoL measured with FACT‐F 13 was significantly larger in patients receiving chemotherapy than in those receiving radiotherapy or no anticancer therapy (P < 0.0001). Patients with Hb levels below 12 g/dL also had significantly (P = 0.0025) larger effects compared to patients with baseline Hb level > 12 g/dL, however, only one trial using radiotherapy had Hb levels > 12 g/dL at baseline (Hoskin 2009). The effect of epoetin was significantly (P < 0.0004) different from darbepoetin, however, the association is potentially confounded by three darbepoetin trials without anticancer therapy (Charu 2007; Gordon 2008; Smith 2008). The observed effect was larger in unblinded trials (MD 3.76, 955 CI 2.60 to 4.92) compared with double‐blind trials (MD 1.33, 95% CI 0.56 to 2.10, P = 0.0006). Significant differences were also observed for age group (adults versus >70% non‐elderly adults, P = 0.008). The backward selection resulted in a model containing the covariate type of ESA formulation, see Table 5. The MD for a trial in patients receiving short‐lasting ESAs is = Intercept + short lasting ESA = 1.09 + 2.20 = 3.29. However, in these analyses single studies were compared to groups of studies and thus results are not readily interpretable.
4. FACT‐F 13: results of meta‐regression analysis.
| Variable | mean difference | standard error | P value |
| Intercept | 1.09 | 0.6158 | 0.0779 |
| Short acting ESA | 2.20 | 0.8346 | 0.0083 |
ESA: erythropoiesis stimulating agent
One trial (Tsuboi 2009) reported two different sets of scores for the control group: in one set they substituted the missing data of two patients by the maximum decrease in score for all patients. The other set of results did not include data for these two patients. We used the scores without the substitution for the main analysis and we conducted a sensitivity analysis using the scores with the substituted data. The results did not change much, with the MD being 2.10 (95% CI 1.46 to 2.75, 18 studies, N = 4,967) and remained statistically significant (P < 0.00001).
Overall, it appears that there is an effect on fatigue‐related symptoms for patients treated with erythropoietin or darbepoetin compared with controls; this effect, however, did not reach the threshold for a clinically important difference defined as 3.0 (Cella 2002).
b) FACT‐An 20
Six studies were included for this outcome (Chang 2005; Christodoulou 2009; Littlewood 2001; O'Shaughnessy 2005; Savonije 2005; Wright 2007). The estimated MD is 6.14 (95% CI 4.55 to 7.73, N = 1,085). There was no evidence for statistical heterogeneity between the studies (I² = 0%). A funnel plot analysis was not done, because less than 10 studies were included in this analysis.
Subgroup analyses did not identify any significant differences in the magnitude of effect between the different subgroups. Of note, FACT‐An 20 improvements were seen across all Hb baseline subgroups (Hb < 10, 10 to 12 and > 12 g/dL).
Overall, the effects of ESAs on fatigue‐ and anaemia‐related symptoms appear to be beneficial and the difference between groups reaches both statistical and clinical significance (clinically important difference defined as four to five), however only six studies were included in this analysis.
c) FACT‐An Total 47
Nine studies, including 1,815 participants, reported data for this outcome. The estimated MD is 6.92 (95% CI 4.59 to 9.25). As one multi‐arm study (Krzakowski 2008) reported results separately for each arm, the number of studies appearing in Metaview is 10.Heterogeneity between the studies was quite high (I² = 85%). A funnel plot analysis was not done, because less than 10 trials were included in this analysis. Merging the two arms of the multi‐arm study mentioned above in one data set did not change the results (MD 6.92; 95% CI 4.59 to 9.25, nine studies, N = 1,815) or heterogeneity markedly (I² = 87%).
One study (Mystakidou 2005) reported an unusually high change for the treatment group (a mean change of 43.3 when the average mean change from all the other studies is 5.14). We, therefore, conducted a sensitivity analysis in which we excluded this study. The results are indeed different than the original analysis with a MD of 3.46 (95% CI 0.96 to 5.96, eight studies, N = 1,715). The statistical heterogeneity between the studies almost disappeared (I² = 0%). The results, however, remained statistically significant (P = 0.007).
We conducted sub‐group analysis that revealed the following subgroups as having significantly different magnitudes of ESA effect between each other: imputed versus non‐imputed data (P = 0.005), baseline Hb level (P < 0.0001), type of anti‐cancer therapy (P < 0.0001), duration of ESA treatment (P < 0.0001) and ITT analysis (P = 0.01). The backward selection resulted in a model containing the covariate type of anticancer therapy, see Additional Table 6. However, differences can also be explained by the study conducted by Mystakidou 2005 (see paragraph above), when removing this study no significant differences between subgroups were evident (data not shown).
5. FACT‐An 47: results of meta‐regression analysis.
| Variable | mean difference | Standard error | P value |
| Intercept | 6.10 | 2.3783 | 0.0103 |
| Chemotherapy, < 70% of participants receiving platinum‐based chemotherapy | ‐5.82 | 3.1929 | 0.0683 |
| Chemotherapy, > 70% of participants receiving platinum‐based chemotherapy | 0.81 | 3.7926 | 0.8303 |
| No anticancer therapy | 23.80 | 4.0571 | <0.0001 |
| Radiotherapy | ‐4.20 | 3.9147 | 0.2836 |
Overall, there is a statistically significant difference between patients treated with ESAs and controls when combining QoL parameters and fatigue‐ and anaemia‐related symptoms, which is however, most likely not clinically important.
(9) Adverse events
(9.1) Thromboembolic events
Data from thromboembolic complications were available from a total of 57 trials, including 15,498 participants. As three multi‐arm trials (Osterborg 1996; Ten Bokkel 1998; Thatcher 1999) were split into subsets and four studies reported zero events (Cascinu 1994; Gupta 2009; P‐174 J&J 2004; Thatcher 1999a), the number of studies displayed is 60. Thirty‐five studies including 6,769 participants were included in the 2006 update of the Cochrane review (Bohlius 2006a), results for 23 studies were newly identified (Aapro 2008; Blohmer 2011; Charu 2007 Amgen 2007; Debus 2006 J&J 2007; Engert 2009; Fujisaka 2011; Gordon 2008; Gupta 2009; Hedenus 2003 FDA 2007; Hernandez 2009; Milroy 2011; Moebus 2007 J&J 2007; Overgaard 2009; Pirker 2008; Pronzato 2010; Ray‐Coquard 2009; Smith 2008; Strauss 2008; Tjulandin 2011; Tsuboi 2009; Untch 2011_1; Wilkinson 2006; Winquist 2009). We removed one study from the analysis because a substantial number of participants underwent major surgical procedures during ESA treatment (Vadhan‐Raj 2004).
The overall risk ratio to suffer thromboembolic complications was increased by 52% for patients receiving ESAs (RR 1.52; 95% CI 1.34 to 1.74). There was no significant statistical heterogeneity between the trials (I² = 0%). A funnel plot analysis revealed a significant asymmetry (P = 0.02137), suggesting that harmful events (in this case thrombotic event) have been over reported. Merging the multi‐arm trials into one data set, did not change the results (RR 1.53; 95% CI 1.34 to 1.74). Compared with the results from the previous Cochrane review (RR 1.67; 95% CI 1.35 to 2.06, 35 trials, N = 6,769, Bohlius 2006a), results are similar. Subgroup analyses for predefined variables did not show robust evidence for statistically significant differences in magnitude or direction of the ESA effect between any of the subgroups tested (e.g. baseline Hb level, type of malignancy, duration of treatment, type of anti‐cancer therapy, age, iron supplementation, type of publication, epoetin versus darbepoetin, type of data, concealment of allocation and masking).
We calculated numbers needed to harm (NNTH) for several hypothetical baseline risks. In a population with an underlying risk of 2% the NNTH would be 96 (95% CI 68 to 147), thus one thromboembolic complication would occur for about every 96 patients treated. In a population with an underlying risk of 5% the NNTH would be 38 (95% CI 27 to 59), thus for every 38 patients treated with ESAs one additional thromboembolic complication might happen. In a population with a hypothetical baseline risk of 10% the NNTH would be 19 (95% CI 14 to 29), thus for every 19 patients treated one additional thromboembolic complication may happen.
In conclusion, the data available for the present analysis confirm and strengthen conclusions from the prior versions of this review that treatment with ESAs increases the risk of thrombosis or related complications.
(9.2) Hypertension
Hypertension data were available from a total of 31 trials including 7,228 participants. Of these trials, 16 including 2,263 randomised participants were included in the updated Cochrane review of 2006 (Bohlius 2006a), for 15 studies Fujisaka 2011; Gordon 2008; Hernandez 2009; Hoskin 2009; Krzakowski 2008; Milroy 2011; Osterborg 2002; Pirker 2008; Razzouk 2006; Savonije 2005; Smith 2008; Tjulandin 2010; Tjulandin 2011; Tsuboi 2009; Wilkinson 2006 data were newly identified. As six of the trials were split into subsets (Krzakowski 2008; Kunikane 2001; Osterborg 1996; Ten Bokkel 1998; Thatcher 1999; Tjulandin 2010) and two trials reported zero events (Cascinu 1994; Iconomou 2003) the number of trials displayed in MetaView is 37.
The risk ratio to develop hypertension for erythropoietin‐treated participants was increased by 30% (fixed‐effect model RR 1.30; 95% CI 1.08 to 1.56), reaching statistical significance (P = 0.006). Using the random‐effects model, however, the result was not statistically significant (RR 1.12, 95% CI 0.94 to 1.33). There was no statistical heterogeneity between the trials (I² = 0%). A funnel plot analysis revealed significant asymmetry (P value < 0.001), suggesting that harmful events (in this case hypertension) have been over reported. Merging the different arms of the multi‐arm trials did not change the overall result (RR 1.31, 95% CI 1.09 to 1.58). The updated results are similar to the previous Cochrane review (RR 1.24; 95% CI 1.00 to 1.54, 16 trials, N = 2,263 Bohlius 2006a).
One single study (Rose 1994) contributed 40% weight to this analysis. Excluding this study, the effect of ESAs on hypertension increased: fixed‐effect: RR 1.52; 95% CI 1.18 to 1.97, random‐effects: RR 1.40; 95% CI 1.07 to 1.83. For another trial, both published and unpublished data were available (Dammacco 2001). In the published sources 3/69 participants in the erythropoietin group and 1/76 participants in the control group were reported to suffer from hypertension. In the unpublished study report 43/69 participants in the erythropoietin group and 36/76 in the control group had hypertension. Including these data instead of the published numbers did not change the overall results significantly, (fixed‐effect model: RR 1.29; 95% CI 1.10 to 1.52), random‐effects model: RR 1.16; 95% CI 1.00 to 1.35).
We calculated numbers needed to harm for several hypothetical baseline risks. In a population with an underlying risk of 2% the NNTH would be 167 (95% CI 89 to 625), thus one patient would be affected with hypertension for about every 167 patients treated. In a population with an underlying risk of 5% the NNTH would be 67 (95% CI 36 to 250), thus for every about 67 patients treated with ESAs one additional episode of hypertension might happen. In a population with a hypothetical baseline risk of 10% the NNTH would be 33 (95% CI 18 to 125), thus for every about 33 patients treated, one additional hypertension episode may happen.
Overall, the data available in this analysis provide suggestive but not robust evidence, that ESAs in the treatment of cancer patients may increase the risk ratio to suffer from hypertension.
(9.3) Haemorrhage/Thrombocytopenia
Haemorrhage/thrombocytopenia data were available from a total of 21 trials including 4,507 participants. Of these trials, 10 including 1,488 randomised participants were included in the update of the Cochrane review in 2006 (Bohlius 2006a). Eleven additional trials Fujisaka 2011; Gebbia 2003; Goss 2005; Gupta 2009; Milroy 2011; Pirker 2008; Savonije 2005; Strauss 2008; Tsuboi 2009; Untch 2011_1; Witzig 2005) including 3,019 participants were added for this update. As three of the trials were split into subsets (Kunikane 2001; Osterborg 1996; Thatcher 1999) and three trials report zero events (Cascinu 1994; Gupta 2009; Osterborg 1996b), the number of trials displayed in MetaView is 24.
The risk ratio to develop thrombocytopenia was increased for erythropoietin‐treated participants (RR 1.21; 95% CI 1.04 to 1.42), reaching statistical significance (P = 0.01). When using the random‐effects model, the results were also statistically significant (RR 1.18, 95% CI 1.02 to 1.36). There was no statistical heterogeneity between the trials (I² = 0%). The funnel plot analysis did not show a significant asymmetry (P = 0.698). Results are similar to the previous review (RR = 1.13, 95 % CI 0.08 to 1.60, 10 trials, N = 1,488 Bohlius 2006a), however, the larger number of included studies and patients increased statistical power and the updated result reached statistical significance. Merging the arms of the multi‐arm trials mentioned above in one data set did not substantially change the results (RR 1.21, 95% CI: 1.04 to 1.41). Subgroup analyses were not performed.
We calculated numbers needed to harm for several hypothetical baseline risks. In a population with an underlying risk of 2% the NNTH would be 238 (95% CI 122 to 1,250), thus one patient would develop thrombocytopenia or haemorrhage for about every 238 patients treated. In a population with an underlying risk of 5% the NNTH would be 95 (95% CI 49 to 500), thus for about every 95 patients treated with ESAs one additional case of thrombocytopenia or haemorrhage might happen. In a population with a hypothetical baseline risk of 10% the NNTH would be 48 (95% CI 24 to 250), thus for every 48 patients treated one additional case of thrombocytopenia or haemorrhage might occur.
Overall, there is some evidence, that ESAs may increase the risk for thrombocytopenia/haemorrhage.
(9.4) Rash, Irritation, Pruritus
Data were available from a total of 16 trials including 2,485 participants. Of those, eight trials with 675 participants were included in the 2006 update (Bohlius 2006a). Data from eight more trials including 1,810 participants were added for this update. As two of the trials were split into subsets (Osterborg 1996; Thatcher 1999) and two trials reported zero events (Gupta 2009; Kurz 1997) the number of trials in MetaView is 18.
Overall, 53 events of skin rash, irritation or pruritus were reported in the erythropoietin group (N = 1,359) and 27 cases in the control group (N = 1,126) , resulting in a risk ratio of 1.49 (95% CI 0.99 to 2.24). There was no significant heterogeneity between the studies (I² = 0%). Merging the different subsets of the multi‐arm trials into one did not change the results (RR1.50, 95% CI 1.00 to 2.27). The funnel plot analysis did not show a significant asymmetry (P = 0.745). Further sensitivity analyses were not done. Compared with the previous Cochrane review (Bohlius 2006a), results are similar (RR 1.17; 95% CI 0.63 to 2.18, eight trials, N = 675 Bohlius 2006a). Based on the data available there is insufficient evidence to conclude that erythropoietin increases the risk of skin reactions.
(9.5) Seizures
Data on seizures were available from eight trials including 2,890 participants (Cascinu 1994; Case 1993; Gordon 2008; Henry 1995; Hernandez 2009; Pirker 2008; Savonije 2005; Smith 2008). Three of those trials (Cascinu 1994; Case 1993; Henry 1995) including 389 participants were included in the 2006 version of the Cochrane review (Bohlius 2006a), data from five further trials including 2,501 participants have been added to this update (Gordon 2008; Hernandez 2009; Pirker 2008; Savonije 2005; Smith 2008. Overall, 19 events of seizure were reported in the erythropoietin group (N=1,583) and 21 events in the control group (N = 1,307), resulting in a risk ratio of 0.77 (95% CI 0.42 to 1.41). There was no significant statistical heterogeneity between the trials (I² = 3%). Overall, there was no evidence for significant differences between the treatment groups compared.
Discussion
Summary of main results
This systematic review analysed the effectiveness and safety of erythropoiesis‐stimulating agents (ESAs) for managing anaemia in cancer patients. The primary findings of this updated review are as follows: ESAs significantly reduce the need for red blood cell transfusions and increase haematological response in cancer patients. However, there is also strong evidence that ESAs increase mortality during study period and some evidence that ESAs reduce overall survival. In addition, there is strong evidence that ESAs increase the risk for thromboembolic complications and some evidence that ESAs increase the risk of hypertension and thrombocytopenia/haemorrhage. The available data are insufficient to evaluate the effect of ESAs on tumour response. Their effect on patients' quality of life (QoL) and specific anaemia‐ and fatigue‐related symptoms (FACT‐An) reaches statistical and clinical significance; however, while it reaches statistical significance, it fails to reach clinical significance for fatigue‐related symptoms only (FACT‐F).
Overall completeness and applicability of evidence
The main strength of the newly updated review is the large number of studies and patients included. All studies were systematically evaluated and outcomes from previous versions of this review updated.
Quality of the evidence
The main weakness of this review are reporting and publication biases. For the outcomes mortality during study period and overall survival this was less of a problem, since we used results that were generated in an individual patient data meta‐analysis (Bohlius 2009a; Bohlius 2009b), which had included the majority of studies in the field. However, besides survival and mortality, no other outcomes were assessed in that review and thus for the remaining outcomes we had to rely on the published evidence. For several of these outcomes only a few studies could be evaluated. For example, hypertension was reported in only 31 of 91 studies, thrombocytopenia in 21 and thromboembolic complications in 57 of 91 studies, haemoglobin (Hb) response in 31 and the number of red blood cell units transfused in 20 of 91 studies. Similarly, numerical QoL data for FACT‐An or FACT‐F were only reported in 23 out of 91 trials. For some but not all of these outcomes, the suspected publication bias was further supported by asymmetric funnel plots. The numbers indicated here underline the lack of complete outcome reporting for a major part of studies and outcomes. In the light of these apparent reporting biases, we estimate that both the beneficial (number of patients transfused, QoL (FACT‐F), Hb response, change in Hb) as well as the harmful effects of ESAs other than mortality (thromboembolic events, hypertension) have been overestimated in our present analysis.
Agreements and disagreements with other studies or reviews
This and previous analyses provide consistent evidence that ESAs reduce the risk for RBC transfusions by approximately 30% to 40%. The point estimated generated in the current update is in line with previous (Bohlius 2006a) and other systematic reviews and meta‐analyses (Tonelli 2009). fOur analysis also provides consistent evidence that ESAs reduce the average number of RBC units transfused. Participants on ESAs received on average one unit of RBCs less (mean difference (MD) ‐0.98, 95% confidence interval (CI) ‐1.17 to ‐0.78) compared with controls which is in line with a previous, independent meta‐analysis, reporting a weighted mean difference (WMD) of −0.80 units (95% CI −0.99 to −0.61) (Tonelli 2009 HTA).
Apart from improving physiologic parameters such as Hb and haematocrit, erythropoietin was also hypothesised to improve QoL and to alleviate fatigue. Improved QoL after ESA treatment was previously reported in community based, single‐arm studies (Demetri 1998; Gabrilove 2001; Glaspy 1997). However, these data were inconclusive because they lacked controls. Later, several randomised controlled studies were conducted to investigate this question. QoL trials require specific methodological standards, such as the use of validated instruments, double blinding, a prospective plan to minimise missing data, investigating the pattern of missing data, and addressing missing data in the analysis (Aaronson 1991; Brandberg 2000). Our updated analysis does not provide evidence for a clinically important improvement of fatigue in patients receiving ESAs compared to controls. This result is more conservative compared to previous meta‐analyses on the same topic (Minton 2010; Tonelli 2009). While previous analyses identified differences for FACT‐F just at (MD 3.00; 95% CI 1.36‐4.64; 10 RCTs, N = 3,169) (Tonelli 2009) or above (MD 3.72; 95% CI 2.38‐5.06; 12 RCTs, N = 2,671) (Minton 2010, personal communication) the threshold for a clinically important difference, our analysis showed a MD of 2.08 (95% CI 1.43‐2.72, 18 RCTs, N = 4,965) which is below the estimated threshold of 3.0 (Cella 2002) . For FACT‐An 20 there seems to be a clinically important improvement in patients receiving ESAs with a MD of 6.14 (95% CI 4.55 to 7.73, six studies, N = 1,085), which is above the CID for FACT‐An, defined as four to five (Cella, personal communication March 2010). However, only a small number of published RCTs on ESAs reported QoL outcomes and therefore more evidence is needed for definitive conclusions. For FACT‐An 47 there is no established CID; however, we expect it to be at least above five, as this is the threshold for FACT‐An 20, which includes less than half the questions of FACT‐An 47. In our analysis there was no robust evidence for a clinically important improvement of QoL measured with FACT‐An 47.
Besides the beneficial effects of ESAs indicated above, our review also identified harmful effects, including an increased risk for thromboembolic events, hypertension, thrombocytopenia, death during study period and potentially decreased overall survival. The increased risk for thromboembolic events in patients receiving ESAs has been observed and reported by single RCTs (Aapro 2008; Goss 2005 J&J 2004; Pirker 2008) and previous meta‐analyses on the same topic (Aapro 2008;Aapro 2009b; Bennett 2008; Bohlius 2006a; Glaspy 2010; Ludwig 2009; Ross 2006; Seidenfeld 2006; Tonelli 2009). The effect estimates generated are comparable across the different meta‐analyses reported. The impact of baseline Haemoglobin levels has not been clarified to date. While one individual patient data meta‐analysis restricted to studies using Darbepoetin for patients receiving chemotherapy suggested an increased risk for thromboembolic events with higher baseline haemoglobin levels (Ludwig 2009), this was not confirmed in a second IPD analysis restricted to RCTs comparing epoetin beta verus control (Aapro 2009b). In this analysis, the risk for thromboembolic events decreased with increasing baseline haemoglobin levels (Aapro 2009b). Besides, there are reports that ESAs are inherently thrombogenic irrespective of baseline or current Hb levels (Barbera 2010; Fuste 2002; Malyszko 1995; Stasko 2002; Stohlawetz 2000). Strategies to reduce the risk for thromboembolic events by using e.g. anti‐coagulating drugs have not yet been evaluated in randomised controlled trials (Aapro 2009a).
Patients receiving ESAs may also have an increased risk for hypertension. In patients with chronic renal failure, hypertension is a common adverse effect of ESAs (Palmer 2010). This increase in blood pressure can be partly explained by the elevated blood viscosity and the loss of hypoxia‐induced vasodilatation in association with the increased Hb level (Cirillo 1993). The present analysis shows some evidence that ESAs also increase the risk for hypertension in cancer patients by approximately 30%. However, the result was statistically significant only in the fixed‐effect model and not in the random‐effects model. In addition, only 31 of 91 studies reported for this outcome. A funnel plot analysis revealed a significant asymmetry (P value < 0.001), suggesting that negative results (in this case no hypertension) have been underreported. Thus, the effect of ESAs on hypertension might be overestimated in the present analysis. A previous meta‐analysis in cancer patients has also identified an increased risk (RR 1.41, 95% CI 0.94 to 2.12, 17 studies, 3,792 patients) which failed to reach conventional level of statistical significance (Tonelli 2009). We also found some evidence that ESAs increase the risk for thrombocytopenia and haemorrhage (RR 1.21, 95% CI, 1.04 to 1.42, 21 trials, 4,507 patients, no evidence for publication bias), which has not been reported before. While the increased risk for thromboembolic events has been established, hypertension and thrombocytopenia/haemorrhage require closer monitoring in future studies.
In the current update of the systematic review, we found no evidence for a beneficial effect of ESAs on tumour control. At the same time, uncertainties remain as important information on tumour grade, tumour stage, intensity of anti‐neoplastic treatment received, timing and method of tumour response assessment were not reported. Relevant studies such as the Henke 2003 or the Antonadou 2001 study could not be included in the meta‐analysis, as they did not report data for complete tumour response. Overall, the data were not sufficient either to exclude or to prove a tumour promoting effect of erythropoiesis‐stimulating factors.
Single randomised controlled trials and previous meta‐analyses based on individual patient data (Bohlius 2009a; Bohlius 2009b) have reported an increased risk for death during the active study period. In the current review we have differentiated the active study period, defined as mortality during ESA treatment plus a short follow‐up time of 30 days, versus overall survival defined as the longest follow‐up available. We integrated the data that were generated previously for the individual patient data meta‐analysis (Bohlius 2009a; Bohlius 2009b) as well as studies which were not included in the IPD review. The updated review confirms the previous IPD review (Bohlius 2009a; Bohlius 2009b) showing an increased risk for on‐study mortality including all cancer patients (HR present meta‐analysis: 1.17, 95% CI 1.06 to 1.29, 70 studies, 15,935 patients; HR IPD review: 1.17, 95% CI 1.06‐1.30, 53 studies, N = 13,933). These results are in line with other meta‐analyses of on‐study mortality regardless of underlying cancer therapy. Aapro 2009b reported an HR of 1.13 (95% CI 0.87 to 1.46, 12 studies, N = 2,297) in studies on epoetin beta and Ross 2006 reported an HR of 1.14 (95% CI 0.90 to 1.45, 17 studies). Both meta‐analyses failed to reach conventional levels of statistical significance which may be explained by the fact that fewer studies and patients were included in each of these analyses. There was some evidence that ESAs decreased overall survival defined as longest follow‐up available (HR 1.05, 95% CI 1.00 to 1.11). As in the previous review (Bohlius 2009a; Bohlius 2009b), the effect was small and of borderline statistical significance. It remains uncertain whether or not the risk is also increased in the subset of patients receiving chemotherapy while also receiving an ESA. In the current updated review the HR for on ‐study mortality in patients receiving chemotherapy is 1.10 (95% CI 0.98 to 1.24, 50 studies, 12,058 patients) which is identical to the HR reported in the previous IPD review (Bohlius 2009a; Bohlius 2009b). However, there were no statistically significant differences between this subgroup and the total patient sample in either the prior IPD meta‐analysis or the current update and an increased risk in cancer patients undergoing chemotherapy and receiving ESAs cannot be excluded. FDA (FDA 2010) has recommended restricting the use of ESAs to cancer patients receiving chemotherapy with palliative intent. ESAs should not be used in patients receiving radiotherapy or no antic‐cancer therapy. However, an increased risk for death in patients receiving chemotherapy cannot be excluded.
Several hypotheses have been proposed to explain the increased risk for death in patients receiving ESAs. One is that erythropoietin might directly influence tumour cell growth. In vitro studies have reported high levels of erythropoietin receptors in breast cancer cells and other malignancies (Acs 2001; Arcasoy 2002; Bennett 2010; Henke 2006; Jelkmann 2004; Jelkmann 2008; McKinney 2011;Yasuda 2003). Either endogenously produced or exogenously administered, erythropoietin may promote the proliferation and survival of cancer cells expressing erythropoietin receptor (Acs 2001; Acs 2002; Arcasoy 2002; Bennett 2010; Henke 2006; Jelkmann 2004; Jelkmann 2008; McKinney 2011; Yasuda 2003). However, conflicting evidence has been reported from pre‐clinical studies on the effects of rHu erythropoietin on cultured cell lines (Bennett 2010). Tumour stimulation through erythropoietin has been suggested in some studies, whereas other studies have not observed a relationship between rHuEPO and tumour cell growth (Bennett 2010; McKinney 2011). An alternative hypothesis suggests that the efficacy of malignancy treatments, both radiotherapy and oxygen‐dependent chemotherapy, can be enhanced by decreasing tumour hypoxia. Tumour tissue is often hypoxic and this hypoxia may increase if the patient is anaemic (Becker 2000; Henke 2000; Tatum 2006; Vaupel 2001; Vaupel 2008). This hypothesis suggests that tumour hypoxia diminishes the effectiveness of radiotherapy and oxygen‐dependent chemotherapy (Tatum 2006; Vaupel 2001; Vaupel 2008). Evidence for this hypothesis comes from reports that tumour control and overall survival are better in solid tumour patients with better tumour oxygenation (Hockel 1993; Knocke 1999). In addition, some authors have reported that the effectiveness of oxygen‐dependent radiotherapy is impaired in anaemic patients (Frommhold 1998; Grau 2000). Enhanced cytocidal efficacy in adequately oxygenated cells has been documented for a number of cytotoxic drugs, such as cyclophosphamide, carboplatin and doxorubicin (Teicher 1981; Teicher 1994). In animal models, cyclophosphamide (Thews 2001) and cisplatin (Silver 1999) have yielded better tumour control with improved tissue oxygenation. Given these observations, it seems plausible that increasing the Hb level with erythropoietin may improve tumour oxygenation and thus tumour control and eventually overall survival. This has been partly demonstrated in animal models (Kelleher 1998). However, other pre‐clinical studies have demonstrated that experimental tumour cells acclimatize rapidly to acute anaemia and return to normal radio sensitivity despite continuing anaemia (Hirst 1984). Chronic anaemia does not necessarily produce radio‐resistance of experimental tumours (Koong 1991) and the correction of anaemia by erythropoietin does not necessarily increase radio‐sensitivity (Joiner 1993).
Authors' conclusions
Implications for practice.
ESAs reduce the need for red blood cell transfusions but increase the risk for thromboembolic events and deaths. There is suggestive evidence that ESAs may improve QoL. Whether and how ESAs affects tumour control remains uncertain. The increased risk of death and thromboembolic events should be balanced against the potential benefits of ESA treatment taking into account each patient’s clinical circumstances and preferences.
Implications for research.
More data are needed for the effect of these drugs on quality of life, tumour progression and other adverse effects. Further research is needed to clarify cellular and molecular mechanisms and pathways of the effects of ESAs on thrombogenesis and their potential effects on tumour growth.
What's new
| Date | Event | Description |
|---|---|---|
| 11 May 2012 | New citation required and conclusions have changed | Authors changed (new authors: Tonia T, Mettler A, Robert N) Substantive update, in the previous review the outcome haematological response was restricted to studies with baseline Hb levels < 12 g/dL; in the current update this restriction was removed. On‐study mortality was added as a new outcome to the current update of the review. Studies using iron supplements in one study arm only were included, in the previous version these studies were excluded. Studies using any dose of ESAs were included, in the previous review studies using very low dosages had been excluded. Any type of ESA was included in the review. |
| 30 November 2011 | New search has been performed | New search |
History
Protocol first published: Issue 4, 2002 Review first published: Issue 3, 2004
| Date | Event | Description |
|---|---|---|
| 15 August 2008 | Amended | Converted to new review format. |
| 24 May 2006 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We thank all authors and co‐workers of primary studies, for which additional information and study data were provided: R. Abels, K. Aziz, J. Blohmer, D. Case, S. Cascinu, M. Cazzola, C. Coiffier, F. Dammacco, L. Del Mastro, D. Henry, Italian Cooperative Study Group, C. Kurz, T. Littlewood, V. Moebus, C. Oberhoff, A. Österborg, E. Rose, W. Ten Bokkel, N. Thatcher, JA. Thompson, NA. Throuvalas, A. Varan. We thank the pharmaceutical companies for providing us with data for various studies (Roche) and admitted additionally insight into their clinical study reports (OrthoBiotech). We also thank the pharmaceutical companies for being very helpful in answering our questions during the process of this previous versions of this review (Roche, Johnson & Johnson).
We would like to thank all previous co‐authors who contributed to previous versions of this review: Simon Langensiepen, Jayne Wilson, Margaret Piper; Sven Trelle, Susan Bayliss, Susan Brunskill, Josie Sandercock, Ben Djulbegovic, Charles Bennett.
Special thanks to Pia Raanani and Sue Richards (CHMG editors) as well as Maryann Napoli (Consumer) and Nicole Skoetz (CHMG editorial base) for critical advice and strong support of previous and current versions of this review.
The first and the second update of this review was supported by the UK Department of Health Cochrane Review Update Incentive Scheme.
Appendices
Appendix 1. EMBASE search strategy
Please note that the same search strategy was used for the other searches conducted on the dates mentioned in the main text.
| No. | Query |
| #70 | #68 AND [1‐8‐2009]/sd NOT [11‐1‐2011]/sd |
| #68 | #38 AND #67 |
| #67 | #63 NOT #66 |
| #66 | #64 NOT #65 |
| #65 | 'human'/exp OR human |
| #64 | 'animal'/exp OR animal |
| #63 | #58 NOT #62 |
| #62 | #59 OR #60 OR #61 |
| #61 | 'abstract report' OR letter |
| #60 | 'case report' |
| #59 | 'case study' |
| #58 | #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 |
| #57 | 'prospective study' |
| #56 | placebo* |
| #55 | 'triple' NEAR/5 'blind' |
| #54 | 'treble' NEAR/5 'blind' |
| #53 | double AND blind* |
| #52 | single AND blind* |
| #51 | 'allocated' NEAR/2 'random' |
| #50 | 'allocated randomly' |
| #49 | 'randomly allocated' |
| #48 | 'random allocation' |
| #47 | rct |
| #46 | randomi?ed AND controlled AND trial? |
| #45 | 'placebo'/exp OR placebo |
| #44 | 'crossover procedure'/exp OR 'crossover procedure' |
| #43 | 'double blind procedure'/exp OR 'double blind procedure' |
| #42 | 'single blind procedure'/exp OR 'single blind procedure' |
| #41 | 'randomization'/exp OR 'randomization' |
| #40 | 'randomized controlled trial'/exp OR 'randomized controlled trial' |
| #39 | 'clinical trial'/exp OR 'clinical trial' |
| #38 | #36 AND #37 |
| #37 | #21 AND #27 |
| #36 | #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 |
| #35 | carcinoma* |
| #34 | tumo?r* |
| #33 | chemotherapy |
| #32 | myelodysplas* |
| #31 | oncolog* |
| #30 | cancer* |
| #29 | malignan* |
| #28 | 'neoplasm'/exp OR neoplasm |
| #27 | #22 OR #23 OR #24 OR #25 OR #26 |
| #26 | anemi* |
| #25 | anaemi* |
| #24 | anemia |
| #23 | anaemia |
| #22 | 'anemia'/exp OR anemia |
| #21 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 |
| #20 | 'erythropoietin receptor'/exp OR 'erythropoietin receptor' |
| #19 | micer* |
| #18 | mircer* |
| #17 | methoxy AND polyethylene AND 'glycol epoetin' AND beta |
| #16 | continuous AND erythropo?es* AND ('receptor'/exp OR receptor) AND activator |
| #15 | cera* |
| #14 | darbepo?eti* |
| #13 | cepo* |
| #12 | procit* |
| #11 | aranesp* |
| #10 | neorecormon* |
| #9 | eprex* |
| #8 | haemopo*etin* |
| #7 | haematopo*etin* |
| #6 | hemopo*etin* |
| #5 | hematopo*etin* |
| #4 | epo* |
| #3 | eritropo* |
| #2 | eryt*ropo* |
| #1 | 'erythropoietin' OR 'recombinant erythropoietin'/exp |
Appendix 2. MEDLINE search strategy
Please note that the same search strategy was used for the other searches conducted on the dates mentioned in the main text.
MEDLINE /Ovid (February 2011 to November 2011)
| # | Searches |
| 1 | exp ERYTHROPOIETIN/ |
| 2 | exp ERYTHROPOIETIN, RECOMBINANT/ |
| 3 | erythropoietin.mp. |
| 4 | erythropoiesis.mp. |
| 5 | exp EPOETIN ALFA/ |
| 6 | epoetin.mp. |
| 7 | epo.mp. |
| 8 | epoetin alfa.mp. |
| 9 | epoetin beta.mp. |
| 10 | eprex.mp. |
| 11 | neorecormon.mp. |
| 12 | aranesp.mp. |
| 13 | procrit.mp. |
| 14 | recombinant erythropoietin.mp. |
| 15 | darbepoetin alfa.mp. |
| 16 | darbepoetin.mp. |
| 17 | RECEPTORS, ERYTHROPOIETIN/ |
| 18 | CERA.mp. |
| 19 | or/1‐18 |
| 20 | exp ANEMIA/dt, th [Drug Therapy, Therapy] |
| 21 | anaemia.mp. |
| 22 | anemia.mp. |
| 23 | (anemi$ adj3 cancer).mp. |
| 24 | (anaemi$ adj3 cancer).mp. |
| 25 | or/20‐24 |
| 26 | exp Neoplasms/ |
| 27 | malignan$.mp. |
| 28 | cancer$.mp. |
| 29 | oncolog$.tw. |
| 30 | myelodysplas$.tw. |
| 31 | chemotherapy.mp. |
| 32 | tumo?r$.mp. |
| 33 | carcinom$.mp. |
| 34 | or/26‐33 |
| 35 | 19 and 25 |
| 36 | 34 and 35 |
| 37 | randomized controlled trial.pt. |
| 38 | controlled clinical trial.pt. |
| 39 | randomized.ab. |
| 40 | placebo.ab. |
| 41 | drug therapy.fs. |
| 42 | randomly.ab. |
| 43 | trial.ab. |
| 44 | groups.ab. |
| 45 | or/37‐44 |
| 46 | humans.sh. |
| 47 | 45 and 46 |
| 48 | 36 and 47 |
| 49 | limit 48 to ed=20080101‐20081231 |
| 50 | randomized controlled trial.pt. |
| 51 | controlled clinical trial.pt. |
| 52 | randomized controlled trials as topic/ |
| 53 | random allocation/ |
| 54 | double blind method/ |
| 55 | single blind method/ |
| 56 | or/50‐55 |
| 57 | (ANIMALS not HUMANS).sh. |
| 58 | 56 not 57 |
| 59 | clinical trial.pt. |
| 60 | exp clinical trial as topic/ |
| 61 | (clin$ adj25 trial$).ti,ab. |
| 62 | ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab. |
| 63 | placebos/ |
| 64 | placebo$.ti,ab. |
| 65 | random$.ti,ab. |
| 66 | research design/ |
| 67 | or/59‐66 |
| 68 | 67 not 57 |
| 69 | 68 not 58 |
| 70 | comparative study/ |
| 71 | exp evaluation studies/ |
| 72 | follow up studies/ |
| 73 | prospective studies/ |
| 74 | (control$ or prospectiv$ or volunteer$).ti,ab. |
| 75 | or/70‐74 |
| 76 | 75 not 57 |
| 77 | 76 not (58 or 69) |
| 78 | 58 or 69 or 77 |
| 79 | 36 and 78 |
| 80 | 48 or 79 |
| 81 | limit 80 to ed=20090801‐20110201 |
| 82 | limit 80 to ed=20110201‐20111201 |
Appendix 3. CENTRAL search strategy
Please note that the same search strategy was used for the other searches conducted on the dates mentioned in the main text.
Cochrane Central Register of Controlled Trials (Cochrane Library 2011, Issue 3)
| ID | Search |
| #1 | (erythropoietin) |
| #2 | MeSH descriptor Erythropoietin explode all trees |
| #3 | epoetin |
| #4 | epo |
| #5 | (epoetin next alfa) |
| #6 | (epoetin next beta) |
| #7 | (darbepoetin next alfa) |
| #8 | eprex |
| #9 | neorecormon |
| #10 | aranesp |
| #11 | procrit |
| #12 | (recombinant near erythropoietin) |
| #13 | "continuous erythropoietin receptor activation" |
| #14 | "continuous erythropoietin receptor activator" |
| #15 | CERA |
| #16 | C.E.R.A. |
| #17 | erythropoiesis |
| #18 | darbepoetin |
| #19 | (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18) |
| #20 | anemia |
| #21 | anaemia |
| #22 | MeSH descriptor Anemia explode all trees |
| #23 | (anemi* near cancer) |
| #24 | (anaemi* near cancer) |
| #25 | (#20 OR #21 OR #22 OR #23 OR #24) |
| #26 | (#19 AND #25) |
| #27 | (#26), from 2007 to 2008 |
| #28 | (#26), from 2008 to 2009 |
| #29 | (#26), from 2009 |
| #30 | (#28 OR #29) |
| #31 | (#26), from 2009 to 2011 |
| #32 | (#26), in 2011 |
Data and analyses
Comparison 1. Haematologic response.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Haematological response ‐ overall | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 2 Haematologic response ‐ baseline Hb | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 2.1 Hb <= 10 g/dL | 36 | 4137 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.02 [2.72, 3.35] |
| 2.2 Hb 10 to 12 g/dL | 8 | 1775 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.60 [3.79, 5.58] |
| 2.3 Hb > 12 g/dL | 1 | 380 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.48 [3.00, 18.62] |
| 2.4 Hb category unclear | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.04 [1.20, 3.46] |
| 3 Haematologic response ‐ different malignancies | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 3.1 solid tumours | 18 | 3089 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.56 [3.12, 4.07] |
| 3.2 haematological malignancies | 15 | 1623 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.12 [2.64, 3.69] |
| 3.3 MDS | 2 | 151 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.27 [0.86, 21.19] |
| 3.4 mixed | 12 | 1550 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.38 [2.80, 4.08] |
| 3.5 not reported | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Haematological response‐ age | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 4.1 children | 1 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.62 [1.20, 2.18] |
| 4.2 adults | 45 | 6191 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.55 [3.23, 3.90] |
| 5 Haematological response‐ age differentiated | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 5.1 only children <18 years | 1 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.62 [1.20, 2.18] |
| 5.2 adults ≥18 years | 43 | 5623 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.34 [3.03, 3.68] |
| 5.3 >70% non‐elderly 18‐65 years | 2 | 568 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.26 [5.22, 13.06] |
| 5.4 only non‐elderly adults | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.5 >70% elderly >65 years | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.6 only elderly adults | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Haematologic response ‐ different therapies | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 6.1 chemotherapy | 38 | 5562 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.32 [3.02, 3.64] |
| 6.2 radiotherapy/radiochemotherapy | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 no therapy | 7 | 630 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.50 [3.25, 9.31] |
| 6.4 other | 1 | 221 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.87 [1.69, 4.85] |
| 7 Haematologic response ‐ different therapies differentiated | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 7.1 chemotherapy, >70% with platinum | 7 | 1301 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.12 [2.51, 3.87] |
| 7.2 chemotherapy, <70% platinum containing | 3 | 659 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.71 [2.16, 3.40] |
| 7.3 chemotherapy without platinum (all patients) | 17 | 2614 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.73 [3.26, 4.26] |
| 7.4 chemotherapy, platinum and non‐platinum containing, no numbers given | 8 | 643 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.05 [2.84, 5.77] |
| 7.5 chemotherapy no details given | 3 | 345 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.13 [1.59, 2.86] |
| 7.6 radiochemotherapy | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.7 radiotherapy | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.8 no therapy | 7 | 630 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.50 [3.25, 9.31] |
| 7.9 other | 1 | 221 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.87 [1.69, 4.85] |
| 8 Haematologic response ‐ epoetin versus darbepoetin | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 8.1 Epoetin | 30 | 5270 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.27 [2.97, 3.59] |
| 8.2 Darbepoetin | 16 | 1143 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.22 [3.22, 5.55] |
| 9 Haematologic response ‐ duration of ESA medication | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 9.1 6 to 9 weeks | 6 | 349 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.74 [1.94, 7.19] |
| 9.2 12 to 16 weeks | 34 | 4574 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.17 [2.87, 3.51] |
| 9.3 more than 17 weeks | 6 | 1490 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.41 [3.52, 5.52] |
| 10 Haematologic response ‐ iron supplementation | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 10.1 fixed iron supplementation | 2 | 441 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.43 [1.92, 3.07] |
| 10.2 iron supplementation as necessary | 36 | 5265 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.63 [3.27, 4.03] |
| 10.3 no explicit statement on iron supplementation or no iron given | 7 | 399 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.82 [2.64, 8.81] |
| 10.4 explicitly stated NO IRON | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.5 iron given differently in both study arms | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.22 [1.63, 3.01] |
| 11 Haematologic response ‐ allocation concealment | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 11.1 adequate | 30 | 4721 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.35 [3.02, 3.72] |
| 11.2 unclear | 16 | 1692 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.50 [2.92, 4.19] |
| 12 Haematologic response ‐ masking | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 12.1 double‐blind | 29 | 3430 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.02 [2.70, 3.37] |
| 12.2 unblinded | 17 | 2983 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.07 [3.49, 4.74] |
| 13 Haematologic response ‐ intention‐to treat | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 13.1 ITT or less than 10% of participants per study arm excluded | 41 | 5657 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.32 [3.03, 3.65] |
| 13.2 more than 10% of participants per study arm excluded | 2 | 512 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.85 [3.76, 12.48] |
| 13.3 unclear | 3 | 244 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.04 [1.92, 4.80] |
| 14 Haematologic response ‐ publication | 46 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.39 [3.10, 3.71] |
| 14.1 full text publication | 32 | 5229 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.44 [3.12, 3.80] |
| 14.2 abstract publication | 2 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.19 [2.23, 12.04] |
| 14.3 unpublished data | 10 | 880 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.44 [2.45, 4.82] |
| 14.4 FDA hearing | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.5 clinical trial result information | 2 | 181 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.98 [1.36, 2.89] |
| 15 Haematological response ‐ merged experimental arms | 31 | 6413 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.42 [3.12, 3.74] |
1.1. Analysis.

Comparison 1 Haematologic response, Outcome 1 Haematological response ‐ overall.
1.2. Analysis.

Comparison 1 Haematologic response, Outcome 2 Haematologic response ‐ baseline Hb.
1.3. Analysis.

Comparison 1 Haematologic response, Outcome 3 Haematologic response ‐ different malignancies.
1.4. Analysis.

Comparison 1 Haematologic response, Outcome 4 Haematological response‐ age.
1.5. Analysis.

Comparison 1 Haematologic response, Outcome 5 Haematological response‐ age differentiated.
1.6. Analysis.

Comparison 1 Haematologic response, Outcome 6 Haematologic response ‐ different therapies.
1.7. Analysis.

Comparison 1 Haematologic response, Outcome 7 Haematologic response ‐ different therapies differentiated.
1.8. Analysis.

Comparison 1 Haematologic response, Outcome 8 Haematologic response ‐ epoetin versus darbepoetin.
1.9. Analysis.

Comparison 1 Haematologic response, Outcome 9 Haematologic response ‐ duration of ESA medication.
1.10. Analysis.

Comparison 1 Haematologic response, Outcome 10 Haematologic response ‐ iron supplementation.
1.11. Analysis.

Comparison 1 Haematologic response, Outcome 11 Haematologic response ‐ allocation concealment.
1.12. Analysis.

Comparison 1 Haematologic response, Outcome 12 Haematologic response ‐ masking.
1.13. Analysis.

Comparison 1 Haematologic response, Outcome 13 Haematologic response ‐ intention‐to treat.
1.14. Analysis.

Comparison 1 Haematologic response, Outcome 14 Haematologic response ‐ publication.
1.15. Analysis.

Comparison 1 Haematologic response, Outcome 15 Haematological response ‐ merged experimental arms.
Comparison 2. Change of haemoglobin level.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in Hb values ‐ overall | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 2 Change in Hb values ‐ baseline Hb | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 2.1 Hb <=10g/dL | 41 | 5092 | Mean Difference (IV, Fixed, 95% CI) | 1.53 [1.43, 1.62] |
| 2.2 Hb 10 to 12 g/dL | 23 | 3572 | Mean Difference (IV, Fixed, 95% CI) | 1.79 [1.71, 1.88] |
| 2.3 Hb >12 g/dL | 10 | 2824 | Mean Difference (IV, Fixed, 95% CI) | 1.12 [0.99, 1.25] |
| 2.4 unclear | 1 | 121 | Mean Difference (IV, Fixed, 95% CI) | 1.53 [0.91, 2.15] |
| 3 Change in Hb values ‐ different malignancies | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 3.1 solid tumours | 45 | 6262 | Mean Difference (IV, Fixed, 95% CI) | 1.76 [1.68, 1.83] |
| 3.2 haematological malignancies | 14 | 2391 | Mean Difference (IV, Fixed, 95% CI) | 1.05 [0.90, 1.19] |
| 3.3 MDS | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | 1.87 [0.89, 2.85] |
| 3.4 mixed | 15 | 2928 | Mean Difference (IV, Fixed, 95% CI) | 1.35 [1.21, 1.48] |
| 3.5 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Change in Hb values ‐ age | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 4.1 children | 1 | 222 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.27, 0.87] |
| 4.2 adults | 74 | 11387 | Mean Difference (IV, Fixed, 95% CI) | 1.58 [1.52, 1.64] |
| 5 Change in Hb values ‐ age differentiated | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 5.1 only children <18 years | 1 | 222 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.27, 0.87] |
| 5.2 adults ≥18 years | 62 | 8214 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.49, 1.64] |
| 5.3 > 70% non‐elderly 18‐65 years | 9 | 1136 | Mean Difference (IV, Fixed, 95% CI) | 1.99 [1.88, 2.10] |
| 5.4 only non‐elderly adults | 2 | 1992 | Mean Difference (IV, Fixed, 95% CI) | 0.76 [0.60, 0.91] |
| 5.5 > 70% elderly >65 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.6 only elderly adults | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 2.70 [1.87, 3.53] |
| 6 Change in Hb values ‐ different therapies | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 6.1 chemotherapy | 58 | 8956 | Mean Difference (IV, Fixed, 95% CI) | 1.46 [1.39, 1.52] |
| 6.2 radiotherapy/radiochemotherapy | 8 | 974 | Mean Difference (IV, Fixed, 95% CI) | 2.41 [2.24, 2.58] |
| 6.3 no therapy | 9 | 1679 | Mean Difference (IV, Fixed, 95% CI) | 1.42 [1.25, 1.60] |
| 7 Change in Hb values ‐ different therapies differentiated | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 7.1 chemotherapy, >70% with platinum | 19 | 2126 | Mean Difference (IV, Fixed, 95% CI) | 1.68 [1.55, 1.82] |
| 7.2 chemotherapy, <70% platinum containing | 7 | 1315 | Mean Difference (IV, Fixed, 95% CI) | 1.84 [1.62, 2.05] |
| 7.3 chemotherapy without platinum | 22 | 4511 | Mean Difference (IV, Fixed, 95% CI) | 1.33 [1.25, 1.42] |
| 7.4 chemotherapy, platinum and non‐platinum containing, no numbers given | 9 | 782 | Mean Difference (IV, Fixed, 95% CI) | 1.37 [1.13, 1.61] |
| 7.5 chemotherapy, no details given | 1 | 222 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.27, 0.87] |
| 7.6 radiotherapy | 5 | 696 | Mean Difference (IV, Fixed, 95% CI) | 2.32 [2.01, 2.63] |
| 7.7 radiochemotherapy | 3 | 278 | Mean Difference (IV, Fixed, 95% CI) | 2.45 [2.25, 2.65] |
| 7.8 no therapy | 9 | 1679 | Mean Difference (IV, Fixed, 95% CI) | 1.42 [1.25, 1.60] |
| 8 Change in Hb values ‐ epoetin vs darbepoetin | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 8.1 Epoetin | 57 | 8304 | Mean Difference (IV, Fixed, 95% CI) | 1.69 [1.62, 1.75] |
| 8.2 Darbepoetin | 18 | 3305 | Mean Difference (IV, Fixed, 95% CI) | 1.13 [1.00, 1.25] |
| 9 Change in Hb values ‐ duration of ESA medication | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 9.1 6 to 9 weeks | 17 | 1235 | Mean Difference (IV, Fixed, 95% CI) | 2.30 [2.16, 2.44] |
| 9.2 12 to 16 weeks | 43 | 6393 | Mean Difference (IV, Fixed, 95% CI) | 1.62 [1.54, 1.70] |
| 9.3 more than 17 weeks | 15 | 3981 | Mean Difference (IV, Fixed, 95% CI) | 1.05 [0.95, 1.16] |
| 10 Change in Hb values ‐ iron supplementation | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 10.1 fixed iron supplementation | 14 | 2483 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [1.81, 2.07] |
| 10.2 iron supplementation as necessary | 53 | 8807 | Mean Difference (IV, Fixed, 95% CI) | 1.47 [1.40, 1.53] |
| 10.3 no explicit statement on iron supplementation or no iron given | 8 | 319 | Mean Difference (IV, Fixed, 95% CI) | 1.66 [1.34, 1.99] |
| 10.4 explicitly stated no iron new | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.5 iron given differently in both study arms new ongoing | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Change in Hb values ‐ allocation concealment | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 11.1 adequate | 45 | 6768 | Mean Difference (IV, Fixed, 95% CI) | 1.52 [1.45, 1.60] |
| 11.2 unclear | 30 | 4841 | Mean Difference (IV, Fixed, 95% CI) | 1.62 [1.53, 1.71] |
| 12 Change in Hb values ‐ masking | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 12.1 double‐blind | 42 | 7438 | Mean Difference (IV, Fixed, 95% CI) | 1.47 [1.40, 1.55] |
| 12.2 unblinded | 33 | 4171 | Mean Difference (IV, Fixed, 95% CI) | 1.67 [1.59, 1.75] |
| 13 Change in Hb values ‐ intention‐to‐treat | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 13.1 ITT or less than 10% of participants per study arm excluded | 57 | 9137 | Mean Difference (IV, Fixed, 95% CI) | 1.61 [1.55, 1.68] |
| 13.2 more than 10% of participants per study arm excluded | 18 | 2472 | Mean Difference (IV, Fixed, 95% CI) | 1.28 [1.13, 1.43] |
| 13.3 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Change in Hb values ‐ publication | 75 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.57 [1.51, 1.62] |
| 14.1 full text publication | 59 | 10026 | Mean Difference (IV, Fixed, 95% CI) | 1.54 [1.47, 1.60] |
| 14.2 abstract publication | 3 | 252 | Mean Difference (IV, Fixed, 95% CI) | 1.70 [1.30, 2.09] |
| 14.3 unpublished data | 10 | 804 | Mean Difference (IV, Fixed, 95% CI) | 1.56 [1.36, 1.76] |
| 14.4 ODAC documents | 1 | 346 | Mean Difference (IV, Fixed, 95% CI) | 2.5 [2.14, 2.86] |
| 14.5 Clinical trials results | 2 | 181 | Mean Difference (IV, Fixed, 95% CI) | 1.48 [0.94, 2.02] |
| 15 Change in Hb values ‐ experimental arms merged | 56 | 11609 | Mean Difference (IV, Fixed, 95% CI) | 1.56 [1.51, 1.62] |
| 16 Change in Hb values‐ sensitivity analysis | 65 | 8685 | Mean Difference (IV, Fixed, 95% CI) | 1.66 [1.59, 1.72] |
| 17 Change in Hb values ‐ publication sensitivity analysis excluding Henke 2003 | 74 | 11263 | Mean Difference (IV, Fixed, 95% CI) | 1.54 [1.48, 1.60] |
| 17.1 full text publication | 58 | 8723 | Mean Difference (IV, Fixed, 95% CI) | 1.63 [1.57, 1.70] |
| 17.2 abstract publication | 4 | 1555 | Mean Difference (IV, Fixed, 95% CI) | 0.87 [0.69, 1.04] |
| 17.3 unpublished data | 10 | 804 | Mean Difference (IV, Fixed, 95% CI) | 1.56 [1.36, 1.76] |
| 17.4 ODAC documents | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17.5 clinical study report | 2 | 181 | Mean Difference (IV, Fixed, 95% CI) | 1.48 [0.94, 2.02] |
2.1. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 1 Change in Hb values ‐ overall.
2.2. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 2 Change in Hb values ‐ baseline Hb.
2.3. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 3 Change in Hb values ‐ different malignancies.
2.4. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 4 Change in Hb values ‐ age.
2.5. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 5 Change in Hb values ‐ age differentiated.
2.6. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 6 Change in Hb values ‐ different therapies.
2.7. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 7 Change in Hb values ‐ different therapies differentiated.
2.8. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 8 Change in Hb values ‐ epoetin vs darbepoetin.
2.9. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 9 Change in Hb values ‐ duration of ESA medication.
2.10. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 10 Change in Hb values ‐ iron supplementation.
2.11. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 11 Change in Hb values ‐ allocation concealment.
2.12. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 12 Change in Hb values ‐ masking.
2.13. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 13 Change in Hb values ‐ intention‐to‐treat.
2.14. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 14 Change in Hb values ‐ publication.
2.15. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 15 Change in Hb values ‐ experimental arms merged.
2.16. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 16 Change in Hb values‐ sensitivity analysis.
2.17. Analysis.

Comparison 2 Change of haemoglobin level, Outcome 17 Change in Hb values ‐ publication sensitivity analysis excluding Henke 2003.
Comparison 3. Participants receiving red blood cell transfusions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants receiving red blood cell transfusions ‐ overall | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 2 Participants receiving red blood cell transfusions ‐ baseline Hb | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 2.1 Hb <=10 g/dL | 42 | 5605 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.67, 0.76] |
| 2.2 Hb 10 to 12 g/dL | 29 | 5669 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.46, 0.55] |
| 2.3 Hb > 12 g/dL | 17 | 4819 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.67, 0.78] |
| 2.4 unclear | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Participants receiving red blood cell transfusions ‐ different malignancies | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 3.1 solid tumours | 53 | 9305 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.46, 0.54] |
| 3.2 haematological malignancies | 15 | 2852 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.75, 0.86] |
| 3.3 MDS | 2 | 151 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.68, 0.96] |
| 3.4 mixed | 19 | 3785 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.68, 0.80] |
| 3.5 not reported | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Participants receiving red blood cell transfusions ‐ age | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 4.1 children | 1 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.71, 0.99] |
| 4.2 adults | 87 | 15871 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.62, 0.67] |
| 5 Participants receiving red blood cell transfusions ‐ age differentiated | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 5.1 only children <18 years | 1 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.71, 0.99] |
| 5.2 adults ≥18 years | 70 | 11556 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.59, 0.66] |
| 5.3 >68% non‐elderly 18‐65 years | 11 | 1343 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.41, 0.60] |
| 5.4 only non‐elderly adults | 5 | 2927 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.72, 0.84] |
| 5.5 >68% elderly >65 years | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.6 only elderly adults | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.17, 0.94] |
| 6 Participants receiving red blood cell transfusions ‐ different therapies | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 6.1 chemotherapy | 71 | 13405 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.61, 0.67] |
| 6.2 radio/radiochemotherapy | 6 | 693 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.34, 0.58] |
| 6.3 no therapy | 10 | 1774 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.72, 0.91] |
| 6.4 unclear/other | 1 | 221 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.60, 0.99] |
| 7 Participants receiving red blood cell transfusions ‐ different therapies differentiated | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 7.1 chemotherapy, > 70% with platinum | 26 | 3592 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.44, 0.54] |
| 7.2 chemotherapy, < 70% with platinum | 10 | 2043 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.55, 0.73] |
| 7.3 chemotherapy without platinum (all patients) | 23 | 6509 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.69, 0.78] |
| 7.4 chemotherapy, platinum and non‐platinum containing, no numbers given | 9 | 772 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.43, 0.65] |
| 7.5 chemotherapy no details given | 3 | 489 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.63, 0.86] |
| 7.6 radiochemotherapy | 6 | 693 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.34, 0.58] |
| 7.7 radiotherapy | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.8 no therapy | 10 | 1774 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.72, 0.91] |
| 7.9 unclear/other | 1 | 221 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.60, 0.99] |
| 8 Participants receiving red blood cell transfusions ‐ epoetin versus darbepoetin | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 8.1 Epoetin | 67 | 11786 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 8.2 Darbepoetin | 21 | 4307 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.60, 0.72] |
| 9 Participants receiving red blood cell transfusions ‐ duration of ESA medication | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 9.1 6 to 9 weeks | 13 | 815 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.49, 0.74] |
| 9.2 12 to 16 weeks | 52 | 8413 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.61, 0.69] |
| 9.3 more than 17 weeks | 23 | 6865 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.61, 0.70] |
| 10 Participants receiving red blood cell transfusions ‐ iron supplementation | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 10.1 fixed iron supplementation | 10 | 2104 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.49, 0.70] |
| 10.2 iron supplementation as necessary | 63 | 12060 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.65, 0.71] |
| 10.3 no explicit statement on iron supplementation or no iron given | 11 | 645 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.42, 0.65] |
| 10.4 explicitly stated NO IRON | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.5 iron given differently in both study arms new | 4 | 1284 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.43, 0.61] |
| 11 Participants receiving red blood cell transfusions ‐ allocation concealment | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 11.1 adequate | 55 | 10898 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.58, 0.65] |
| 11.2 unclear | 33 | 5195 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.67, 0.76] |
| 12 Participants receiving red blood cell transfusions ‐ masking | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 12.1 double‐blind | 50 | 9677 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.68, 0.75] |
| 12.2 unblinded | 38 | 6416 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.47, 0.56] |
| 13 Participants receiving red blood cell transfusions ‐ intention‐to treat | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 13.1 ITT or less than 10% of participants per study arm excluded | 73 | 13772 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.63, 0.69] |
| 13.2 more than 10% of participants per study arm excluded | 11 | 1035 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.36, 0.63] |
| 13.3 unclear | 4 | 1286 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.33, 0.62] |
| 14 Participants receiving red blood cell transfusions ‐ publication | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 14.1 fulltext publication | 65 | 12678 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.63, 0.70] |
| 14.2 abstract publication | 7 | 1242 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.32, 0.49] |
| 14.3 unpublished data | 14 | 1658 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.67, 0.80] |
| 14.4 FDA presented data | 1 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.47, 0.78] |
| 14.5 Other | 1 | 201 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.26, 0.73] |
| 15 Participants receiving red blood cell transfusions ‐ first 4 weeks are... | 88 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
| 15.1 included in the analysis | 32 | 5319 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.61, 0.70] |
| 15.2 excluded from the analysis | 23 | 3288 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.61, 0.75] |
| 15.3 unclear | 33 | 7486 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.60, 0.68] |
| 16 Participants receiving red blood cell transfusions ‐ experimental arms merged | 70 | 16093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.62, 0.68] |
3.1. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 1 Participants receiving red blood cell transfusions ‐ overall.
3.2. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 2 Participants receiving red blood cell transfusions ‐ baseline Hb.
3.3. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 3 Participants receiving red blood cell transfusions ‐ different malignancies.
3.4. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 4 Participants receiving red blood cell transfusions ‐ age.
3.5. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 5 Participants receiving red blood cell transfusions ‐ age differentiated.
3.6. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 6 Participants receiving red blood cell transfusions ‐ different therapies.
3.7. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 7 Participants receiving red blood cell transfusions ‐ different therapies differentiated.
3.8. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 8 Participants receiving red blood cell transfusions ‐ epoetin versus darbepoetin.
3.9. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 9 Participants receiving red blood cell transfusions ‐ duration of ESA medication.
3.10. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 10 Participants receiving red blood cell transfusions ‐ iron supplementation.
3.11. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 11 Participants receiving red blood cell transfusions ‐ allocation concealment.
3.12. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 12 Participants receiving red blood cell transfusions ‐ masking.
3.13. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 13 Participants receiving red blood cell transfusions ‐ intention‐to treat.
3.14. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 14 Participants receiving red blood cell transfusions ‐ publication.
3.15. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 15 Participants receiving red blood cell transfusions ‐ first 4 weeks are....
3.16. Analysis.

Comparison 3 Participants receiving red blood cell transfusions, Outcome 16 Participants receiving red blood cell transfusions ‐ experimental arms merged.
Comparison 4. Number of red blood cell units transfused per patient.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of RBC units transfused ‐ overall | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 2 Number of RBC units transfused ‐ baseline Hb | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 2.1 Hb < 10g/dL | 16 | 1996 | Mean Difference (IV, Fixed, 95% CI) | ‐1.02 [‐1.35, ‐0.68] |
| 2.2 Hb 10 to 12g/dL | 5 | 1096 | Mean Difference (IV, Fixed, 95% CI) | ‐0.95 [‐1.24, ‐0.65] |
| 2.3 Hb > 12g/dL | 4 | 1623 | Mean Difference (IV, Fixed, 95% CI) | ‐0.97 [‐1.41, ‐0.54] |
| 3 Number of RBC units transfused ‐ age differentiated | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 3.1 only children <18 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 adults ≥18 years | 21 | 3093 | Mean Difference (IV, Fixed, 95% CI) | ‐0.81 [‐1.04, ‐0.57] |
| 3.3 >68% non‐elderly 18‐65 years | 3 | 353 | Mean Difference (IV, Fixed, 95% CI) | ‐1.25 [‐1.72, ‐0.77] |
| 3.4 only non‐elderly adults | 1 | 1269 | Mean Difference (IV, Fixed, 95% CI) | ‐1.60 [‐2.18, ‐1.02] |
| 3.5 >68% elderly >65 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.6 only elderly > 65 J | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number of RBC units transfused ‐ age | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 4.1 adults | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 5 Number of RBC units transfused ‐ different malignancies | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 5.1 solid tumours | 10 | 1437 | Mean Difference (IV, Fixed, 95% CI) | ‐1.07 [‐1.34, ‐0.80] |
| 5.2 haematological malignancies | 10 | 2254 | Mean Difference (IV, Fixed, 95% CI) | ‐1.19 [‐1.63, ‐0.76] |
| 5.3 mixed | 5 | 1024 | Mean Difference (IV, Fixed, 95% CI) | ‐0.62 [‐1.01, ‐0.24] |
| 6 Number of RBC units transfused ‐ different therapies | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 6.1 chemotherapy | 23 | 4376 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.18, ‐0.78] |
| 6.2 radiotherapy/radiochemotherapy | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 no therapy | 1 | 118 | Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐1.81, 0.47] |
| 6.4 unclear/ other | 1 | 221 | Mean Difference (IV, Fixed, 95% CI) | ‐2.2 [‐6.44, 2.04] |
| 7 Number of RBC units transfused ‐ different therapies differentiated | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 7.1 chemotherapy > 70% with platinum | 10 | 1344 | Mean Difference (IV, Fixed, 95% CI) | ‐1.11 [‐1.40, ‐0.83] |
| 7.2 chemotherapy, <70% with platinum | 2 | 584 | Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐0.93, ‐0.12] |
| 7.3 chemotherapy without platinum | 9 | 2054 | Mean Difference (IV, Fixed, 95% CI) | ‐1.23 [‐1.69, ‐0.78] |
| 7.4 chemotherapy, platinum and non‐platinum containing, no numbers given | 2 | 394 | Mean Difference (IV, Fixed, 95% CI) | ‐1.01 [‐1.80, ‐0.21] |
| 7.5 chemotherapy no details given | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.6 radiochemotherapy | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.7 radiotherapy | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.8 no therapy | 1 | 118 | Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐1.81, 0.47] |
| 7.9 unclear/other | 1 | 221 | Mean Difference (IV, Fixed, 95% CI) | ‐2.2 [‐6.44, 2.04] |
| 8 Number of RBC units transfused ‐ epoetin versus darbepoetin | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 8.1 Epoetin | 23 | 4052 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐1.29, ‐0.82] |
| 8.2 Darbepoetin | 2 | 663 | Mean Difference (IV, Fixed, 95% CI) | ‐0.78 [‐1.15, ‐0.42] |
| 9 Number of RBC units transfused ‐ duration of ESA medication | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 9.1 6 to 9 weeks | 6 | 364 | Mean Difference (IV, Fixed, 95% CI) | ‐1.25 [‐1.75, ‐0.75] |
| 9.2 12 to 16 weeks | 12 | 2688 | Mean Difference (IV, Fixed, 95% CI) | ‐0.78 [‐1.03, ‐0.54] |
| 9.3 more than 17 weeks | 7 | 1663 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐1.84, ‐0.95] |
| 10 Number of RBC units transfused ‐ iron supplementation | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 10.1 fixed iron supplementation | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 iron supplementation as necessary | 24 | 4402 | Mean Difference (IV, Fixed, 95% CI) | ‐0.92 [‐1.13, ‐0.72] |
| 10.3 no explicit statement on iron supplementation or no iron given | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.4 explicitely stated NO IRON | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.5 iron given differently in both study arms | 1 | 313 | Mean Difference (IV, Fixed, 95% CI) | ‐1.6 [‐2.30, ‐0.90] |
| 11 Number of RBC units transfused ‐ allocation concealment | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 11.1 adequate | 15 | 2243 | Mean Difference (IV, Fixed, 95% CI) | ‐0.93 [‐1.19, ‐0.67] |
| 11.2 unclear | 10 | 2472 | Mean Difference (IV, Fixed, 95% CI) | ‐1.04 [‐1.35, ‐0.74] |
| 12 Number of RBC units transfused ‐ masking | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 12.1 double‐blind | 12 | 3382 | Mean Difference (IV, Fixed, 95% CI) | ‐0.91 [‐1.14, ‐0.69] |
| 12.2 unblinded | 13 | 1333 | Mean Difference (IV, Fixed, 95% CI) | ‐1.16 [‐1.55, ‐0.77] |
| 13 Number of RBC units transfused ‐ intention‐to‐treat | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 13.1 ITT or less than 10% of participants per study arm excluded | 24 | 4583 | Mean Difference (IV, Fixed, 95% CI) | ‐0.99 [‐1.19, ‐0.79] |
| 13.2 more than 10% of participants per study arm excluded | 1 | 132 | Mean Difference (IV, Fixed, 95% CI) | ‐0.69 [‐1.66, 0.28] |
| 14 Number of RBC units transfused ‐ publication | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 14.1 full text publication | 4 | 1200 | Mean Difference (IV, Fixed, 95% CI) | ‐0.77 [‐1.06, ‐0.48] |
| 14.2 abstract publication | 1 | 1269 | Mean Difference (IV, Fixed, 95% CI) | ‐1.60 [‐2.18, ‐1.02] |
| 14.3 unpublished data | 20 | 2246 | Mean Difference (IV, Fixed, 95% CI) | ‐1.03 [‐1.33, ‐0.73] |
| 14.4 FDA presented data | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Number of RBC units transfused ‐ first 4 weeks are... | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 15.1 included in the analysis | 18 | 2658 | Mean Difference (IV, Fixed, 95% CI) | ‐0.99 [‐1.23, ‐0.74] |
| 15.2 excluded from the analysis | 3 | 623 | Mean Difference (IV, Fixed, 95% CI) | ‐0.53 [‐0.94, ‐0.12] |
| 15.3 unclear | 4 | 1434 | Mean Difference (IV, Fixed, 95% CI) | ‐1.72 [‐2.27, ‐1.18] |
| 16 Number of RBC units transfused ‐ experimental arms merged | 19 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 17 Number of RBC units transfused ‐ age differentiated sensitivity analysis | 25 | 4715 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐1.17, ‐0.78] |
| 17.1 only children <18 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 adults ≥18 years | 21 | 3093 | Mean Difference (IV, Fixed, 95% CI) | ‐0.81 [‐1.04, ‐0.57] |
| 17.3 >68% non‐elderly 18‐65 years | 4 | 1622 | Mean Difference (IV, Fixed, 95% CI) | ‐1.39 [‐1.75, ‐1.02] |
| 17.4 only non‐elderly adults | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17.5 >68% elderly >65 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17.6 only elderly > 65 J | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
4.1. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 1 Number of RBC units transfused ‐ overall.
4.2. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 2 Number of RBC units transfused ‐ baseline Hb.
4.3. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 3 Number of RBC units transfused ‐ age differentiated.
4.4. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 4 Number of RBC units transfused ‐ age.
4.5. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 5 Number of RBC units transfused ‐ different malignancies.
4.6. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 6 Number of RBC units transfused ‐ different therapies.
4.7. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 7 Number of RBC units transfused ‐ different therapies differentiated.
4.8. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 8 Number of RBC units transfused ‐ epoetin versus darbepoetin.
4.9. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 9 Number of RBC units transfused ‐ duration of ESA medication.
4.10. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 10 Number of RBC units transfused ‐ iron supplementation.
4.11. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 11 Number of RBC units transfused ‐ allocation concealment.
4.12. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 12 Number of RBC units transfused ‐ masking.
4.13. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 13 Number of RBC units transfused ‐ intention‐to‐treat.
4.14. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 14 Number of RBC units transfused ‐ publication.
4.15. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 15 Number of RBC units transfused ‐ first 4 weeks are....
4.16. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 16 Number of RBC units transfused ‐ experimental arms merged.
4.17. Analysis.

Comparison 4 Number of red blood cell units transfused per patient, Outcome 17 Number of RBC units transfused ‐ age differentiated sensitivity analysis.
Comparison 5. Overall survival.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Overall survival ‐ overall | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 2 Overall survival updated review (adjusted results) | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 3 Overall survival ‐ baseline Hb | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 3.1 Hb < 10 g/dL | 29 | 6144 | Peto Odds Ratio (95% CI) | 1.06 [0.96, 1.17] |
| 3.2 Hb 10 to 12 g/dL | 31 | 6418 | Peto Odds Ratio (95% CI) | 1.01 [0.93, 1.10] |
| 3.3 Hb > 12 g/dL | 15 | 5725 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 3.4 unclear | 5 | 716 | Peto Odds Ratio (95% CI) | 0.83 [0.67, 1.03] |
| 4 Overall survival ‐ different malignancies | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 4.1 solid tumours | 50 | 11704 | Peto Odds Ratio (95% CI) | 1.06 [1.00, 1.13] |
| 4.2 haematological malignancies | 11 | 2901 | Peto Odds Ratio (95% CI) | 1.07 [0.90, 1.26] |
| 4.3 MDS | 1 | 66 | Peto Odds Ratio (95% CI) | 4.52 [0.38, 53.37] |
| 4.4 mixed | 18 | 4332 | Peto Odds Ratio (95% CI) | 1.02 [0.91, 1.15] |
| 4.5 not reported | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 5 Overall survival ‐ age | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 5.1 children | 1 | 222 | Peto Odds Ratio (95% CI) | 0.98 [0.14, 7.03] |
| 5.2 adults | 79 | 18781 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 6 Overall survival ‐ age differentiated | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 6.1 only children < 18 | 1 | 222 | Peto Odds Ratio (95% CI) | 0.98 [0.14, 7.03] |
| 6.2 adults >= 18 | 62 | 13975 | Peto Odds Ratio (95% CI) | 1.07 [1.01, 1.13] |
| 6.3 > 68% non elderly 18‐65 | 11 | 1611 | Peto Odds Ratio (95% CI) | 0.86 [0.67, 1.10] |
| 6.4 only non‐elderly adults | 4 | 2916 | Peto Odds Ratio (95% CI) | 1.02 [0.82, 1.26] |
| 6.5 > 68% elderly > 65 | 2 | 279 | Peto Odds Ratio (95% CI) | 0.77 [0.51, 1.17] |
| 6.6 only elderly > 65 | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 7 Overall survival ‐ different therapies | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 7.1 chemotherapy | 55 | 13800 | Peto Odds Ratio (95% CI) | 1.04 [0.98, 1.11] |
| 7.2 radiotherapy/radiochemotherapy | 14 | 2939 | Peto Odds Ratio (95% CI) | 1.03 [0.92, 1.15] |
| 7.3 no therapy | 8 | 1942 | Peto Odds Ratio (95% CI) | 1.23 [1.04, 1.45] |
| 7.4 unclear/other | 3 | 322 | Peto Odds Ratio (95% CI) | 0.79 [0.49, 1.27] |
| 8 Overall survival ‐ different therapies differentiated | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 8.1 chemotherapy, > 70% with platinum | 19 | 3622 | Peto Odds Ratio (95% CI) | 1.01 [0.91, 1.12] |
| 8.2 chemotherapy, < 70% with platinum | 7 | 1812 | Peto Odds Ratio (95% CI) | 1.14 [0.95, 1.36] |
| 8.3 chemotherapy without platinum (all patients) | 19 | 6706 | Peto Odds Ratio (95% CI) | 1.08 [0.98, 1.19] |
| 8.4 chemotherapy, platinum and non platinum containing, no numbers given | 5 | 910 | Peto Odds Ratio (95% CI) | 0.94 [0.65, 1.37] |
| 8.5 chemotherapy no details given | 5 | 750 | Peto Odds Ratio (95% CI) | 0.82 [0.61, 1.10] |
| 8.6 radiochemotherapy | 8 | 1193 | Peto Odds Ratio (95% CI) | 0.92 [0.78, 1.09] |
| 8.7 radiotherapy | 6 | 1746 | Peto Odds Ratio (95% CI) | 1.12 [0.97, 1.30] |
| 8.8 no therapy | 8 | 1942 | Peto Odds Ratio (95% CI) | 1.23 [1.04, 1.45] |
| 8.9 unclear/other | 3 | 322 | Peto Odds Ratio (95% CI) | 0.79 [0.49, 1.27] |
| 9 Overall survival ‐ epoetin vs darbepoetin | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 9.1 Epoetin | 67 | 14047 | Peto Odds Ratio (95% CI) | 1.04 [0.98, 1.10] |
| 9.2 Darbepoetin | 13 | 4956 | Peto Odds Ratio (95% CI) | 1.09 [0.99, 1.20] |
| 10 Overall survival ‐ duration of ESA medication | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 10.1 6 to 9 weeks | 13 | 2244 | Peto Odds Ratio (95% CI) | 1.10 [0.95, 1.27] |
| 10.2 12 to 16 weeks | 46 | 9385 | Peto Odds Ratio (95% CI) | 1.05 [0.98, 1.13] |
| 10.3 more than 17 weeks | 18 | 6963 | Peto Odds Ratio (95% CI) | 1.04 [0.95, 1.14] |
| 10.4 not reported | 3 | 411 | Peto Odds Ratio (95% CI) | 1.10 [0.58, 2.07] |
| 11 Overall survival ‐ iron supplementation | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 11.1 fixed iron supplementation | 10 | 2348 | Peto Odds Ratio (95% CI) | 1.15 [0.99, 1.33] |
| 11.2 iron supplementation as necessary | 56 | 13888 | Peto Odds Ratio (95% CI) | 1.07 [1.01, 1.14] |
| 11.3 iron handled differently in the study arms | 9 | 2050 | Peto Odds Ratio (95% CI) | 0.96 [0.84, 1.11] |
| 11.4 no explicit statement on iron supplementation or no iron given | 5 | 717 | Peto Odds Ratio (95% CI) | 0.56 [0.38, 0.83] |
| 11.5 explicitly stated NO IRON | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 12 Overall survival ‐ publication | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 12.1 full text publication | 20 | 4531 | Peto Odds Ratio (95% CI) | 1.07 [0.92, 1.24] |
| 12.2 abstract publication | 3 | 1020 | Peto Odds Ratio (95% CI) | 1.09 [0.87, 1.37] |
| 12.3 unpublished data | 5 | 318 | Peto Odds Ratio (95% CI) | 0.73 [0.17, 3.05] |
| 12.4 Data presented at FDA hearing | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 12.5 Data taken from IPD review (Bohlius 2009) | 50 | 13018 | Peto Odds Ratio (95% CI) | 1.06 [1.00, 1.12] |
| 12.6 clinical trial result information | 1 | 60 | Peto Odds Ratio (95% CI) | 7.39 [0.15, 372.38] |
| 12.7 other | 1 | 56 | Peto Odds Ratio (95% CI) | 0.58 [0.33, 1.03] |
| 13 Overall survival ‐ time‐to‐event or binary mortality data | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 13.1 binary mortality data at end of study | 19 | 1917 | Peto Odds Ratio (95% CI) | 1.02 [0.66, 1.60] |
| 13.2 Data from IPD review | 50 | 13018 | Peto Odds Ratio (95% CI) | 1.06 [1.00, 1.12] |
| 13.3 Cox regression analysis, Hazard ratio, log‐rank test, p‐value | 7 | 3141 | Peto Odds Ratio (95% CI) | 1.07 [0.92, 1.25] |
| 13.4 Survival curve and p‐value | 4 | 927 | Peto Odds Ratio (95% CI) | 0.99 [0.78, 1.24] |
| 14 Overall survival ‐ allocation concealment | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 14.1 adequate | 47 | 12424 | Peto Odds Ratio (95% CI) | 1.08 [1.02, 1.14] |
| 14.2 unclear | 33 | 6579 | Peto Odds Ratio (95% CI) | 0.97 [0.87, 1.09] |
| 15 Overall survival ‐ masking | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 15.1 double‐blind | 42 | 10525 | Peto Odds Ratio (95% CI) | 1.06 [0.99, 1.14] |
| 15.2 unblinded | 38 | 8478 | Peto Odds Ratio (95% CI) | 1.04 [0.96, 1.12] |
| 16 Overall survival ‐ intention‐to‐treat | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 16.1 ITT or less than 10% of participants per study arm excluded | 75 | 18052 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 16.2 more than 10% of participants per study arm excluded | 2 | 385 | Peto Odds Ratio (95% CI) | 1.25 [0.92, 1.71] |
| 16.3 Unclear | 3 | 566 | Peto Odds Ratio (95% CI) | 0.49 [0.27, 0.89] |
| 17 Overall survival ‐ follow up | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 17.1 follow up longer than on‐study mortality | 44 | 13224 | Peto Odds Ratio (95% CI) | 1.05 [0.99, 1.10] |
| 17.2 Short term follow up | 36 | 5779 | Peto Odds Ratio (95% CI) | 1.14 [0.95, 1.36] |
| 18 Overall survival ‐ follow up and design | 80 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 18.1 Long term follow up and designed for long term follow up | 25 | 9704 | Peto Odds Ratio (95% CI) | 1.06 [0.99, 1.12] |
| 18.2 Long term follow up but not designed for long term follow up | 11 | 2197 | Peto Odds Ratio (95% CI) | 1.02 [0.89, 1.18] |
| 18.3 Long term follow up and design unclear | 7 | 1142 | Peto Odds Ratio (95% CI) | 0.96 [0.79, 1.16] |
| 18.4 Short term follow up but designed for long term follow up | 3 | 1250 | Peto Odds Ratio (95% CI) | 1.32 [1.05, 1.66] |
| 18.5 Short term follow up and not designed for long term follow up | 34 | 4710 | Peto Odds Ratio (95% CI) | 0.97 [0.76, 1.23] |
| 18.6 short term follow up and design unclear | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 19 Overall survival‐ experimental arms merged | 78 | 19003 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 20 Overall survival‐ experimental arms merged sens pos | 76 | 17551 | Peto Odds Ratio (95% CI) | 1.04 [0.98, 1.10] |
| 21 Overall survival‐ experimental arms merged sens neg | 76 | 18018 | Peto Odds Ratio (95% CI) | 1.08 [1.02, 1.14] |
| 22 Overall survival ‐ sensitivity analysis baseline Hb | 75 | 18287 | Peto Odds Ratio (95% CI) | 1.07 [1.01, 1.13] |
| 22.1 Hb < 10 g/dL | 29 | 6144 | Peto Odds Ratio (95% CI) | 1.06 [0.96, 1.17] |
| 22.2 Hb 10 to 12 g/dL | 31 | 6418 | Peto Odds Ratio (95% CI) | 1.01 [0.93, 1.10] |
| 22.3 Hb > 12 g/dL | 15 | 5725 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 23 Overall survival ‐ sensitivity analysis iron supplementation | 75 | 18286 | Peto Odds Ratio (95% CI) | 1.07 [1.01, 1.12] |
| 23.1 fixed iron supplementation | 10 | 2348 | Peto Odds Ratio (95% CI) | 1.15 [0.99, 1.33] |
| 23.2 iron supplementation as necessary | 56 | 13888 | Peto Odds Ratio (95% CI) | 1.07 [1.01, 1.14] |
| 23.3 iron handled differently in the study arms | 9 | 2050 | Peto Odds Ratio (95% CI) | 0.96 [0.84, 1.11] |
| 23.4 explicitly stated NO IRON | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 24 Overall survival ‐ sensitivity analysis intention‐to‐treat | 77 | 18437 | Peto Odds Ratio (95% CI) | 1.06 [1.01, 1.12] |
| 24.1 ITT or less than 10% of participants per study arm excluded | 75 | 18052 | Peto Odds Ratio (95% CI) | 1.05 [1.00, 1.11] |
| 24.2 more than 10% of participants per study arm excluded | 2 | 385 | Peto Odds Ratio (95% CI) | 1.25 [0.92, 1.71] |
5.1. Analysis.

Comparison 5 Overall survival, Outcome 1 Overall survival ‐ overall.
5.2. Analysis.

Comparison 5 Overall survival, Outcome 2 Overall survival updated review (adjusted results).
5.3. Analysis.

Comparison 5 Overall survival, Outcome 3 Overall survival ‐ baseline Hb.
5.4. Analysis.

Comparison 5 Overall survival, Outcome 4 Overall survival ‐ different malignancies.
5.5. Analysis.

Comparison 5 Overall survival, Outcome 5 Overall survival ‐ age.
5.6. Analysis.

Comparison 5 Overall survival, Outcome 6 Overall survival ‐ age differentiated.
5.7. Analysis.

Comparison 5 Overall survival, Outcome 7 Overall survival ‐ different therapies.
5.8. Analysis.

Comparison 5 Overall survival, Outcome 8 Overall survival ‐ different therapies differentiated.
5.9. Analysis.

Comparison 5 Overall survival, Outcome 9 Overall survival ‐ epoetin vs darbepoetin.
5.10. Analysis.

Comparison 5 Overall survival, Outcome 10 Overall survival ‐ duration of ESA medication.
5.11. Analysis.

Comparison 5 Overall survival, Outcome 11 Overall survival ‐ iron supplementation.
5.12. Analysis.

Comparison 5 Overall survival, Outcome 12 Overall survival ‐ publication.
5.13. Analysis.

Comparison 5 Overall survival, Outcome 13 Overall survival ‐ time‐to‐event or binary mortality data.
5.14. Analysis.

Comparison 5 Overall survival, Outcome 14 Overall survival ‐ allocation concealment.
5.15. Analysis.

Comparison 5 Overall survival, Outcome 15 Overall survival ‐ masking.
5.16. Analysis.

Comparison 5 Overall survival, Outcome 16 Overall survival ‐ intention‐to‐treat.
5.17. Analysis.

Comparison 5 Overall survival, Outcome 17 Overall survival ‐ follow up.
5.18. Analysis.

Comparison 5 Overall survival, Outcome 18 Overall survival ‐ follow up and design.
5.19. Analysis.

Comparison 5 Overall survival, Outcome 19 Overall survival‐ experimental arms merged.
5.20. Analysis.

Comparison 5 Overall survival, Outcome 20 Overall survival‐ experimental arms merged sens pos.
5.21. Analysis.

Comparison 5 Overall survival, Outcome 21 Overall survival‐ experimental arms merged sens neg.
5.22. Analysis.

Comparison 5 Overall survival, Outcome 22 Overall survival ‐ sensitivity analysis baseline Hb.
5.23. Analysis.

Comparison 5 Overall survival, Outcome 23 Overall survival ‐ sensitivity analysis iron supplementation.
5.24. Analysis.

Comparison 5 Overall survival, Outcome 24 Overall survival ‐ sensitivity analysis intention‐to‐treat.
Comparison 6. On‐study mortality.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 On‐study mortality ‐ overall | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 2 On‐study mortality ‐ baseline Hb | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 2.1 Hb < 10 g/dL | 28 | 5759 | Peto Odds Ratio (95% CI) | 1.12 [0.96, 1.32] |
| 2.2 Hb 10 to 12 g/dL | 26 | 5537 | Peto Odds Ratio (95% CI) | 1.09 [0.91, 1.29] |
| 2.3 Hb > 12 g/dL | 13 | 3923 | Peto Odds Ratio (95% CI) | 1.37 [1.12, 1.68] |
| 2.4 unclear | 5 | 716 | Peto Odds Ratio (95% CI) | 1.20 [0.75, 1.93] |
| 3 On‐study mortality ‐ different malignancies | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 3.1 solid tumours | 44 | 10056 | Peto Odds Ratio (95% CI) | 1.21 [1.06, 1.37] |
| 3.2 haematological malignancies | 10 | 1598 | Peto Odds Ratio (95% CI) | 1.13 [0.80, 1.59] |
| 3.3 MDS | 1 | 66 | Peto Odds Ratio (95% CI) | 4.52 [0.38, 53.37] |
| 3.4 mixed | 17 | 4215 | Peto Odds Ratio (95% CI) | 1.10 [0.92, 1.31] |
| 3.5 not reported | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 4 On‐study mortality ‐ age | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 4.1 children | 1 | 222 | Peto Odds Ratio (95% CI) | 0.98 [0.14, 7.03] |
| 4.2 adults | 71 | 15713 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 5 On‐study mortality ‐ age differentiated | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 5.1 children | 1 | 222 | Peto Odds Ratio (95% CI) | 0.98 [0.14, 7.03] |
| 5.2 adults >= 18 | 59 | 13007 | Peto Odds Ratio (95% CI) | 1.18 [1.07, 1.31] |
| 5.3 > 68% non elderly, 18‐65 | 10 | 1334 | Peto Odds Ratio (95% CI) | 0.76 [0.42, 1.35] |
| 5.4 only non elderly adults | 2 | 1372 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 5.5 > 68% elderly > 65 years | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 5.6 only elderly | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 6 On‐study mortality ‐ different therapies | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 6.1 chemotherapy | 52 | 12058 | Peto Odds Ratio (95% CI) | 1.10 [0.98, 1.24] |
| 6.2 radiotherapy/radiochemotherapy | 10 | 1669 | Peto Odds Ratio (95% CI) | 1.48 [0.96, 2.27] |
| 6.3 no therapy | 8 | 1942 | Peto Odds Ratio (95% CI) | 1.34 [1.07, 1.66] |
| 6.4 unclear/other | 2 | 266 | Peto Odds Ratio (95% CI) | 1.48 [0.65, 3.37] |
| 7 On‐study mortality ‐ different therapies differentiated | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 7.1 chemotherapy, > 70% with platinum | 19 | 3622 | Peto Odds Ratio (95% CI) | 1.04 [0.85, 1.27] |
| 7.2 chemotherapy, <70% with platinum | 6 | 1475 | Peto Odds Ratio (95% CI) | 1.06 [0.76, 1.49] |
| 7.3 chemotherapy without platinum, all patients | 18 | 5418 | Peto Odds Ratio (95% CI) | 1.24 [1.04, 1.47] |
| 7.4 chemotherapy, platinum and non‐platinum containing, no numbers given | 4 | 793 | Peto Odds Ratio (95% CI) | 0.74 [0.40, 1.38] |
| 7.5 chemotherapy, no details reported | 5 | 750 | Peto Odds Ratio (95% CI) | 0.82 [0.50, 1.34] |
| 7.6 radiochemotherapy | 6 | 822 | Peto Odds Ratio (95% CI) | 1.46 [0.85, 2.51] |
| 7.7 radiotherapy | 4 | 847 | Peto Odds Ratio (95% CI) | 1.51 [0.75, 3.06] |
| 7.8 no therapy | 8 | 1942 | Peto Odds Ratio (95% CI) | 1.34 [1.07, 1.66] |
| 7.9 unclear/other | 2 | 266 | Peto Odds Ratio (95% CI) | 1.48 [0.65, 3.37] |
| 8 On‐study mortality ‐ duration of ESA medication | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 8.1 6 to 9 weeks | 9 | 1113 | Peto Odds Ratio (95% CI) | 0.95 [0.57, 1.59] |
| 8.2 12 to 16 weeks | 44 | 8992 | Peto Odds Ratio (95% CI) | 1.16 [1.02, 1.33] |
| 8.3 more than 17 weeks | 16 | 5419 | Peto Odds Ratio (95% CI) | 1.22 [1.04, 1.42] |
| 8.4 not reported | 3 | 411 | Peto Odds Ratio (95% CI) | 0.82 [0.38, 1.78] |
| 9 On‐study mortality ‐ epoetin vs darbepoetin | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 9.1 Epoetin | 60 | 11478 | Peto Odds Ratio (95% CI) | 1.16 [1.03, 1.30] |
| 9.2 Darbepoetin | 12 | 4457 | Peto Odds Ratio (95% CI) | 1.20 [1.00, 1.44] |
| 10 On‐study mortality ‐ iron supplementation | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 10.1 fixed iron supplementation | 8 | 1911 | Peto Odds Ratio (95% CI) | 1.20 [0.80, 1.81] |
| 10.2 iron supplementation as necessary | 53 | 11954 | Peto Odds Ratio (95% CI) | 1.17 [1.05, 1.30] |
| 10.3 no explicit statement on iron supplementation or no iron given | 3 | 276 | Peto Odds Ratio (95% CI) | 2.16 [0.72, 6.46] |
| 10.4 explicitly stated no iron | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 10.5 iron handled differently in the study arms | 8 | 1794 | Peto Odds Ratio (95% CI) | 1.09 [0.74, 1.60] |
| 11 On‐study mortality ‐ publication | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 11.1 full text publication | 14 | 1689 | Peto Odds Ratio (95% CI) | 0.97 [0.60, 1.57] |
| 11.2 abstract publication | 2 | 181 | Peto Odds Ratio (95% CI) | 7.64 [1.29, 45.03] |
| 11.3 unpublished data | 5 | 318 | Peto Odds Ratio (95% CI) | 1.65 [0.20, 13.32] |
| 11.4 Data presented at FDA hearing | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 11.5 IPD Bohlius 2009 | 51 | 13747 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 12 On‐study mortality ‐ time‐to‐event or binary mortality data | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 12.1 binary mortality data at end of study | 21 | 2188 | Peto Odds Ratio (95% CI) | 1.14 [0.73, 1.79] |
| 12.2 Results from IPD review | 51 | 13747 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 12.3 Cox regression analysis, Hazard ratio, log‐rank test, p‐value | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 12.4 Survival curve and p‐value | 0 | 0 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 13 On‐study mortality ‐ allocation concealment | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 13.1 adequate | 42 | 11144 | Peto Odds Ratio (95% CI) | 1.20 [1.08, 1.34] |
| 13.2 unclear | 30 | 4791 | Peto Odds Ratio (95% CI) | 1.03 [0.82, 1.30] |
| 14 On‐study mortality ‐ masking | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 14.1 double‐blind | 39 | 9049 | Peto Odds Ratio (95% CI) | 1.19 [1.06, 1.34] |
| 14.2 unblinded | 33 | 6886 | Peto Odds Ratio (95% CI) | 1.12 [0.94, 1.34] |
| 15 On‐study mortality ‐ intention‐to‐treat | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 15.1 ITT or less than 10% of participants per study arm excluded | 69 | 15706 | Peto Odds Ratio (95% CI) | 1.16 [1.05, 1.28] |
| 15.2 more than 10% of participants per study arm excluded | 1 | 48 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 15.3 Unclear | 2 | 181 | Peto Odds Ratio (95% CI) | 7.64 [1.29, 45.03] |
| 16 On‐study mortality ‐ sensitivity analysis ‐ follow‐up | 80 | 19018 | Peto Odds Ratio (95% CI) | 1.16 [1.05, 1.27] |
| 16.1 Short term follow subgroup | 72 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 16.2 Short term from Kaplan Meier curve | 7 | 2966 | Peto Odds Ratio (95% CI) | 1.06 [0.60, 1.86] |
| 16.3 Long term follow up | 1 | 117 | Peto Odds Ratio (95% CI) | 0.94 [0.57, 1.54] |
| 17 On‐study mortality ‐ sensitivity analysis experimental arms merged | 70 | 15935 | Peto Odds Ratio (95% CI) | 1.17 [1.06, 1.29] |
| 18 On‐study mortality ‐ sensitivity analysis intention‐to‐treat | 70 | 15754 | Peto Odds Ratio (95% CI) | 1.16 [1.05, 1.28] |
| 18.1 ITT or less than 10% of participants per study arm excluded | 69 | 15706 | Peto Odds Ratio (95% CI) | 1.16 [1.05, 1.28] |
| 18.2 more than 10% of participants per study arm excluded | 1 | 48 | Peto Odds Ratio (95% CI) | 0.0 [0.0, 0.0] |
| 19 On‐study mortality ‐ sensitivity analysis excluding Leyland and Smith | 70 | 14007 | Peto Odds Ratio (95% CI) | 1.09 [0.97, 1.23] |
6.1. Analysis.

Comparison 6 On‐study mortality, Outcome 1 On‐study mortality ‐ overall.
6.2. Analysis.

Comparison 6 On‐study mortality, Outcome 2 On‐study mortality ‐ baseline Hb.
6.3. Analysis.

Comparison 6 On‐study mortality, Outcome 3 On‐study mortality ‐ different malignancies.
6.4. Analysis.

Comparison 6 On‐study mortality, Outcome 4 On‐study mortality ‐ age.
6.5. Analysis.

Comparison 6 On‐study mortality, Outcome 5 On‐study mortality ‐ age differentiated.
6.6. Analysis.

Comparison 6 On‐study mortality, Outcome 6 On‐study mortality ‐ different therapies.
6.7. Analysis.

Comparison 6 On‐study mortality, Outcome 7 On‐study mortality ‐ different therapies differentiated.
6.8. Analysis.

Comparison 6 On‐study mortality, Outcome 8 On‐study mortality ‐ duration of ESA medication.
6.9. Analysis.

Comparison 6 On‐study mortality, Outcome 9 On‐study mortality ‐ epoetin vs darbepoetin.
6.10. Analysis.

Comparison 6 On‐study mortality, Outcome 10 On‐study mortality ‐ iron supplementation.
6.11. Analysis.

Comparison 6 On‐study mortality, Outcome 11 On‐study mortality ‐ publication.
6.12. Analysis.

Comparison 6 On‐study mortality, Outcome 12 On‐study mortality ‐ time‐to‐event or binary mortality data.
6.13. Analysis.

Comparison 6 On‐study mortality, Outcome 13 On‐study mortality ‐ allocation concealment.
6.14. Analysis.

Comparison 6 On‐study mortality, Outcome 14 On‐study mortality ‐ masking.
6.15. Analysis.

Comparison 6 On‐study mortality, Outcome 15 On‐study mortality ‐ intention‐to‐treat.
6.16. Analysis.

Comparison 6 On‐study mortality, Outcome 16 On‐study mortality ‐ sensitivity analysis ‐ follow‐up.
6.17. Analysis.

Comparison 6 On‐study mortality, Outcome 17 On‐study mortality ‐ sensitivity analysis experimental arms merged.
6.18. Analysis.

Comparison 6 On‐study mortality, Outcome 18 On‐study mortality ‐ sensitivity analysis intention‐to‐treat.
6.19. Analysis.

Comparison 6 On‐study mortality, Outcome 19 On‐study mortality ‐ sensitivity analysis excluding Leyland and Smith.
Comparison 7. Complete tumour response.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Complete tumour response | 19 | 5012 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.98, 1.06] |
| 2 Tumour‐response specific quality criteria | 19 | 5012 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.98, 1.06] |
| 2.1 high quality | 5 | 2476 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.95, 1.02] |
| 2.2 low quality | 14 | 2536 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.98, 1.36] |
| 3 Complete tumour response ‐ experimental study arms merged | 15 | 5012 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.98, 1.06] |
7.1. Analysis.

Comparison 7 Complete tumour response, Outcome 1 Complete tumour response.
7.2. Analysis.

Comparison 7 Complete tumour response, Outcome 2 Tumour‐response specific quality criteria.
7.3. Analysis.

Comparison 7 Complete tumour response, Outcome 3 Complete tumour response ‐ experimental study arms merged.
Comparison 8. Change in FACT‐Fatigue 13.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in FACT‐Fatigue (13 items) ‐ overall | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 2 Change in FACT‐Fatigue sensitivity analysis‐ Tsuboi | 18 | 4967 | Mean Difference (IV, Fixed, 95% CI) | 2.10 [1.46, 2.75] |
| 3 Change in FACT‐F 13 ‐ baseline Hb | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 3.1 Hb <= 10 g/dL | 8 | 2484 | Mean Difference (IV, Fixed, 95% CI) | 1.66 [0.76, 2.55] |
| 3.2 Hb 10 to 12 g/dL | 9 | 2181 | Mean Difference (IV, Fixed, 95% CI) | 2.87 [1.89, 3.85] |
| 3.3 Hb > 12 g/dL | 1 | 300 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐2.63, 2.63] |
| 3.4 Hb category unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Change in FACT‐F 13 ‐ different malignancies | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 4.1 solid tumours | 9 | 2459 | Mean Difference (IV, Fixed, 95% CI) | 2.29 [1.33, 3.25] |
| 4.2 haematological malignancies | 2 | 566 | Mean Difference (IV, Fixed, 95% CI) | 1.99 [0.28, 3.69] |
| 4.3 mixed | 7 | 1940 | Mean Difference (IV, Fixed, 95% CI) | 1.87 [0.87, 2.87] |
| 4.4 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Change in FACT‐F 13 ‐ age | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 5.1 only children < 18 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 adults >= 18 years | 17 | 4627 | Mean Difference (IV, Fixed, 95% CI) | 1.82 [1.16, 2.49] |
| 5.3 >70% non elderly 18‐65 years | 1 | 338 | Mean Difference (IV, Fixed, 95% CI) | 5.1 [2.79, 7.41] |
| 5.4 only non‐elderly adults | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.5 >70% elderly >65 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.6 only elderly > 65 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Change in FACT‐F 13 ‐ different therapies | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 6.1 chemotherapy | 14 | 3515 | Mean Difference (IV, Fixed, 95% CI) | 2.79 [2.03, 3.55] |
| 6.2 radiotherapy | 1 | 300 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐2.63, 2.63] |
| 6.3 no therapy | 3 | 1150 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [‐0.91, 1.76] |
| 6.4 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Change in FACT‐F 13 ‐ different therapies differentiated | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.07 [1.43, 2.72] |
| 7.1 chemotherapy, >70% with platinum | 4 | 1069 | Mean Difference (IV, Fixed, 95% CI) | 1.85 [0.41, 3.30] |
| 7.2 chemotherapy, <70% platinum containing | 2 | 411 | Mean Difference (IV, Fixed, 95% CI) | 2.53 [‐0.01, 5.07] |
| 7.3 chemotherapy without platinum (all patients) | 6 | 1468 | Mean Difference (IV, Fixed, 95% CI) | 3.22 [2.12, 4.32] |
| 7.4 chemotherapy, platinum and non‐platinum containing, no numbers given | 3 | 567 | Mean Difference (IV, Fixed, 95% CI) | 3.27 [1.30, 5.23] |
| 7.5 radiochemotherapy NEW | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.6 radiotherapy | 1 | 300 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐2.63, 2.63] |
| 7.7 no therapy | 3 | 1150 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [‐0.91, 1.76] |
| 7.8 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.9 chemotherapy no details given | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Change in FACT‐F 13 ‐ epoetin versus darbepoetin | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 8.1 Epoetin | 11 | 2475 | Mean Difference (IV, Fixed, 95% CI) | 3.25 [2.33, 4.16] |
| 8.2 Darbepoetin | 7 | 2490 | Mean Difference (IV, Fixed, 95% CI) | 0.94 [0.04, 1.84] |
| 9 Change in FACT‐F 13 ‐ duration of ESA medication | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 9.1 6 to 9 weeks | 1 | 115 | Mean Difference (IV, Fixed, 95% CI) | 3.10 [‐0.27, 6.47] |
| 9.2 12 to 16 weeks | 15 | 4076 | Mean Difference (IV, Fixed, 95% CI) | 1.99 [1.30, 2.69] |
| 9.3 more than 17 weeks | 2 | 774 | Mean Difference (IV, Fixed, 95% CI) | 2.35 [0.46, 4.25] |
| 9.4 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Change in FACT‐F 13 ‐ iron supplementation | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 10.1 fixed iron supplementation | 4 | 863 | Mean Difference (IV, Fixed, 95% CI) | 1.64 [‐0.01, 3.29] |
| 10.2 iron supplementation as necessary | 13 | 3881 | Mean Difference (IV, Fixed, 95% CI) | 2.03 [1.32, 2.74] |
| 10.3 no explicit statement on iron supplementation or no iron given | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.4 explicitly stated NO IRON | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.5 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.6 iron given differently in both study arms new | 1 | 221 | Mean Difference (IV, Fixed, 95% CI) | 5.15 [1.70, 8.60] |
| 11 Change in FACT‐F 13 ‐ allocation concealment | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 11.1 adequate | 16 | 4493 | Mean Difference (IV, Fixed, 95% CI) | 2.20 [1.51, 2.89] |
| 11.2 unclear | 2 | 472 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐0.61, 3.02] |
| 11.3 unclear wether adequate or unclear :) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Change in FACT‐F 13 ‐ masking | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 12.1 double‐blind | 11 | 3384 | Mean Difference (IV, Fixed, 95% CI) | 1.33 [0.56, 2.10] |
| 12.2 unblinded | 7 | 1581 | Mean Difference (IV, Fixed, 95% CI) | 3.76 [2.60, 4.92] |
| 13 Change in FACT‐F 13 ‐ intention‐to treat | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 13.1 ITT or less than 10% of participants per study arm excluded | 4 | 864 | Mean Difference (IV, Fixed, 95% CI) | 3.30 [1.89, 4.70] |
| 13.2 more than 10% of participants per study arm excluded | 12 | 3689 | Mean Difference (IV, Fixed, 95% CI) | 1.80 [1.04, 2.56] |
| 13.3 unclear | 2 | 412 | Mean Difference (IV, Fixed, 95% CI) | 1.34 [‐0.95, 3.63] |
| 14 Change in FACT‐F 13 ‐ publication | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 14.1 full text publication | 16 | 4412 | Mean Difference (IV, Fixed, 95% CI) | 2.17 [1.49, 2.85] |
| 14.2 abstract publication | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 unpublished data | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.4 FDA hearing | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.5 clinical trial result information | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.6 other source | 2 | 553 | Mean Difference (IV, Fixed, 95% CI) | 1.32 [‐0.63, 3.26] |
| 15 Change in FACT‐F 13 ‐ type of data | 18 | 4965 | Mean Difference (IV, Fixed, 95% CI) | 2.08 [1.43, 2.72] |
| 15.1 Not imputed data | 7 | 2298 | Mean Difference (IV, Fixed, 95% CI) | 1.88 [0.96, 2.80] |
| 15.2 Imputed data | 11 | 2667 | Mean Difference (IV, Fixed, 95% CI) | 2.26 [1.36, 3.15] |
8.1. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 1 Change in FACT‐Fatigue (13 items) ‐ overall.
8.2. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 2 Change in FACT‐Fatigue sensitivity analysis‐ Tsuboi.
8.3. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 3 Change in FACT‐F 13 ‐ baseline Hb.
8.4. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 4 Change in FACT‐F 13 ‐ different malignancies.
8.5. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 5 Change in FACT‐F 13 ‐ age.
8.6. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 6 Change in FACT‐F 13 ‐ different therapies.
8.7. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 7 Change in FACT‐F 13 ‐ different therapies differentiated.
8.8. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 8 Change in FACT‐F 13 ‐ epoetin versus darbepoetin.
8.9. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 9 Change in FACT‐F 13 ‐ duration of ESA medication.
8.10. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 10 Change in FACT‐F 13 ‐ iron supplementation.
8.11. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 11 Change in FACT‐F 13 ‐ allocation concealment.
8.12. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 12 Change in FACT‐F 13 ‐ masking.
8.13. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 13 Change in FACT‐F 13 ‐ intention‐to treat.
8.14. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 14 Change in FACT‐F 13 ‐ publication.
8.15. Analysis.

Comparison 8 Change in FACT‐Fatigue 13, Outcome 15 Change in FACT‐F 13 ‐ type of data.
Comparison 9. Change in FACT‐An 20.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in FACT‐An (20 items) ‐ overall | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 2 Change in FACT‐An 20 ‐ baseline Hb | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 2.1 Hb <= 10 g/dL | 1 | 290 | Mean Difference (IV, Fixed, 95% CI) | 6.6 [3.92, 9.28] |
| 2.2 Hb 10 to 12 g/dL | 4 | 713 | Mean Difference (IV, Fixed, 95% CI) | 5.82 [3.71, 7.93] |
| 2.3 Hb > 12 g/dL | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | 6.4 [0.83, 11.97] |
| 2.4 Hb category unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Change in FACT‐An 20 ‐ different malignancies | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 3.1 solid tumours | 5 | 795 | Mean Difference (IV, Fixed, 95% CI) | 5.90 [3.92, 7.87] |
| 3.2 haematological malignancies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 mixed | 1 | 290 | Mean Difference (IV, Fixed, 95% CI) | 6.6 [3.92, 9.28] |
| 3.4 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Change in FACT‐An 20 ‐ age | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 4.1 only children < 18 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 adults >= 18 years | 5 | 747 | Mean Difference (IV, Fixed, 95% CI) | 5.93 [4.00, 7.86] |
| 4.3 >70% non elderly 18‐65 years | 1 | 338 | Mean Difference (IV, Fixed, 95% CI) | 6.59 [3.79, 9.39] |
| 4.4 only non‐elderly adults | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.5 >70% elderly >65 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.6 only elderly > 65 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Change in FACT‐An 20 ‐ different therapies | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 5.1 chemotherapy | 5 | 1051 | Mean Difference (IV, Fixed, 95% CI) | 6.21 [4.60, 7.82] |
| 5.2 radiotherapy | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 no therapy | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 3.9 [‐5.75, 13.55] |
| 5.4 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Change in FACT‐An 20 ‐ different therapies differentiated | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 6.1 chemotherapy, >70% with platinum | 2 | 256 | Mean Difference (IV, Fixed, 95% CI) | 5.08 [1.12, 9.04] |
| 6.2 chemotherapy, <70% platinum containing | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 chemotherapy without platinum (all patients) | 4 | 795 | Mean Difference (IV, Fixed, 95% CI) | 6.43 [4.66, 8.19] |
| 6.4 chemotherapy, platinum and non‐platinum containing, no numbers given | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.5 radiochemotherapy NEW | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.6 radiotherapy | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.7 no therapy | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 3.9 [‐5.75, 13.55] |
| 6.8 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.9 chemotherapy no details given | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Change in FACT‐An 20 ‐ epoetin versus darbepoetin | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 7.1 Epoetin | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 7.2 Darbepoetin | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Change in FACT‐An 20 ‐ duration of ESA medication | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 8.1 6 to 9 weeks | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 12 to 16 weeks | 5 | 795 | Mean Difference (IV, Fixed, 95% CI) | 5.90 [3.92, 7.87] |
| 8.3 more than 17 weeks | 1 | 290 | Mean Difference (IV, Fixed, 95% CI) | 6.6 [3.92, 9.28] |
| 8.4 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Change in FACT‐An 20 ‐ iron supplementation | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 9.1 fixed iron supplementation | 1 | 126 | Mean Difference (IV, Fixed, 95% CI) | 3.53 [‐1.90, 8.96] |
| 9.2 iron supplementation as necessary | 4 | 744 | Mean Difference (IV, Fixed, 95% CI) | 6.48 [4.68, 8.28] |
| 9.3 no explicit statement on iron supplementation or no iron given | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.4 explicitly stated NO IRON | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.5 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.6 iron given differently in both study arms new | 1 | 215 | Mean Difference (IV, Fixed, 95% CI) | 5.84 [1.47, 10.21] |
| 10 Change in FACT‐An 20 ‐ allocation concealment | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 10.1 adequate | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 10.2 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.3 unclear wether adequate or unclear :) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Change in FACT‐An 20 ‐ masking | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 11.1 double‐blind | 3 | 406 | Mean Difference (IV, Fixed, 95% CI) | 6.41 [4.06, 8.75] |
| 11.2 unblinded | 3 | 679 | Mean Difference (IV, Fixed, 95% CI) | 5.92 [3.76, 8.08] |
| 12 Change in FACT‐An 20 ‐ intention‐to treat | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 12.1 ITT or less than 10% of participants per study arm excluded | 1 | 338 | Mean Difference (IV, Fixed, 95% CI) | 6.59 [3.79, 9.39] |
| 12.2 more than 10% of participants per study arm excluded | 5 | 747 | Mean Difference (IV, Fixed, 95% CI) | 5.93 [4.00, 7.86] |
| 12.3 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Change in FACT‐An 20 ‐ publication | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 13.1 full text publication | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 13.2 abstract publication | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.3 unpublished data | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.4 FDA hearing | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.5 clinical trial result information | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Change in FACT‐An 20 ‐ data type | 6 | 1085 | Mean Difference (IV, Fixed, 95% CI) | 6.14 [4.55, 7.73] |
| 14.1 Not imputed data | 3 | 635 | Mean Difference (IV, Fixed, 95% CI) | 6.38 [4.20, 8.55] |
| 14.2 Imputed data | 3 | 450 | Mean Difference (IV, Fixed, 95% CI) | 5.88 [3.54, 8.21] |
9.1. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 1 Change in FACT‐An (20 items) ‐ overall.
9.2. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 2 Change in FACT‐An 20 ‐ baseline Hb.
9.3. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 3 Change in FACT‐An 20 ‐ different malignancies.
9.4. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 4 Change in FACT‐An 20 ‐ age.
9.5. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 5 Change in FACT‐An 20 ‐ different therapies.
9.6. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 6 Change in FACT‐An 20 ‐ different therapies differentiated.
9.7. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 7 Change in FACT‐An 20 ‐ epoetin versus darbepoetin.
9.8. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 8 Change in FACT‐An 20 ‐ duration of ESA medication.
9.9. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 9 Change in FACT‐An 20 ‐ iron supplementation.
9.10. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 10 Change in FACT‐An 20 ‐ allocation concealment.
9.11. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 11 Change in FACT‐An 20 ‐ masking.
9.12. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 12 Change in FACT‐An 20 ‐ intention‐to treat.
9.13. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 13 Change in FACT‐An 20 ‐ publication.
9.14. Analysis.

Comparison 9 Change in FACT‐An 20, Outcome 14 Change in FACT‐An 20 ‐ data type.
Comparison 10. Change in FACT‐An Total 47.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in FACT‐An Total (47 items) ‐ overall | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 2 Change in FACT‐An Total 47‐ sensitivity analysis | 9 | 1715 | Mean Difference (IV, Fixed, 95% CI) | 3.46 [0.96, 5.96] |
| 3 Change in FACT‐An Total 47 ‐ baseline Hb | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 3.1 Hb <= 10 g/dL | 5 | 978 | Mean Difference (IV, Fixed, 95% CI) | 2.57 [‐0.63, 5.78] |
| 3.2 Hb 10 to 12 g/dL | 4 | 537 | Mean Difference (IV, Fixed, 95% CI) | 16.22 [12.14, 20.30] |
| 3.3 Hb > 12 g/dL | 1 | 300 | Mean Difference (IV, Fixed, 95% CI) | 1.90 [‐4.19, 7.99] |
| 3.4 Hb category unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Change in FACT‐An Total 47 ‐ different malignancies | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 4.1 solid tumours | 8 | 1437 | Mean Difference (IV, Fixed, 95% CI) | 7.21 [4.58, 9.84] |
| 4.2 haematological malignancies | 1 | 206 | Mean Difference (IV, Fixed, 95% CI) | 6.10 [‐1.67, 13.87] |
| 4.3 mixed | 1 | 172 | Mean Difference (IV, Fixed, 95% CI) | 5.7 [‐0.83, 12.23] |
| 4.4 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Change in FACT‐An Total 47 ‐ age | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 5.1 only children < 18 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 adults >= 18 years | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 5.3 >70% non elderly 18‐65 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.4 only non‐elderly adults | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.5 >70% elderly >65 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.6 only elderly > 65 years | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Change in FACT‐An Total 47 ‐ different therapies | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 6.1 chemotherapy | 8 | 1415 | Mean Difference (IV, Fixed, 95% CI) | 3.77 [1.03, 6.51] |
| 6.2 radiotherapy | 1 | 300 | Mean Difference (IV, Fixed, 95% CI) | 1.90 [‐4.19, 7.99] |
| 6.3 no therapy | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 29.90 [23.46, 36.34] |
| 6.4 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Change in FACT‐An Total 47 ‐ different therapies differentiated | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 7.1 chemotherapy, >70% with platinum | 3 | 352 | Mean Difference (IV, Fixed, 95% CI) | 6.91 [1.12, 12.70] |
| 7.2 chemotherapy, <70% platinum containing | 3 | 600 | Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐3.90, 4.45] |
| 7.3 chemotherapy without platinum (all patients) | 3 | 463 | Mean Difference (IV, Fixed, 95% CI) | 6.10 [1.44, 10.76] |
| 7.4 chemotherapy, platinum and non‐platinum containing, no numbers given | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.5 radiochemotherapy NEW | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.6 radiotherapy | 1 | 300 | Mean Difference (IV, Fixed, 95% CI) | 1.90 [‐4.19, 7.99] |
| 7.7 no therapy | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 29.90 [23.46, 36.34] |
| 7.8 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.9 chemotherapy no details given | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Change in FACT‐An Total 47 ‐ epoetin versus darbepoetin | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 8.1 Epoetin | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 8.2 Darbepoetin | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Change in FACT‐An Total 47 ‐ duration of ESA medication | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 9.1 6 to 9 weeks | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 12 to 16 weeks | 8 | 1625 | Mean Difference (IV, Fixed, 95% CI) | 3.39 [0.83, 5.96] |
| 9.3 more than 17 weeks | 2 | 190 | Mean Difference (IV, Fixed, 95% CI) | 23.64 [18.05, 29.22] |
| 9.4 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Change in FACT‐An Total 47 ‐ iron supplementation | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 10.1 fixed iron supplementation | 7 | 1217 | Mean Difference (IV, Fixed, 95% CI) | 7.14 [4.31, 9.96] |
| 10.2 iron supplementation as necessary | 2 | 378 | Mean Difference (IV, Fixed, 95% CI) | 5.87 [0.86, 10.87] |
| 10.3 no explicit statement on iron supplementation or no iron given | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.4 explicitly stated NO IRON | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.5 unclear | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.6 iron given differently in both study arms new | 1 | 220 | Mean Difference (IV, Fixed, 95% CI) | 7.67 [0.40, 14.94] |
| 11 Change in FACT‐An Total 47 ‐ allocation concealment | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 11.1 adequate | 4 | 840 | Mean Difference (IV, Fixed, 95% CI) | 4.69 [0.92, 8.45] |
| 11.2 unclear | 6 | 975 | Mean Difference (IV, Fixed, 95% CI) | 8.30 [5.33, 11.26] |
| 12 Change in FACT‐An Total 47 ‐ masking | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 12.1 double‐blind | 6 | 1078 | Mean Difference (IV, Fixed, 95% CI) | 8.00 [5.13, 10.87] |
| 12.2 unblinded | 4 | 737 | Mean Difference (IV, Fixed, 95% CI) | 4.83 [0.84, 8.82] |
| 13 Change in FACT‐An Total 47 ‐ intention‐to treat | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 13.1 ITT or less than 10% of participants per study arm excluded | 4 | 585 | Mean Difference (IV, Fixed, 95% CI) | 10.85 [7.29, 14.41] |
| 13.2 more than 10% of participants per study arm excluded | 4 | 840 | Mean Difference (IV, Fixed, 95% CI) | 4.69 [0.92, 8.45] |
| 13.3 unclear | 2 | 390 | Mean Difference (IV, Fixed, 95% CI) | 2.54 [‐2.81, 7.90] |
| 14 Change in FACT‐An Total 47 ‐ publication | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 14.1 full text publication | 9 | 1725 | Mean Difference (IV, Fixed, 95% CI) | 7.02 [4.63, 9.40] |
| 14.2 abstract publication | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | 4.71 [‐6.49, 15.91] |
| 14.3 unpublished data | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.4 FDA hearing | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.5 clinical trial result information | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Change in Fact‐An Total 47 ‐ data type | 10 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
| 15.1 Not imputed data | 7 | 1101 | Mean Difference (IV, Fixed, 95% CI) | 9.31 [6.45, 12.17] |
| 15.2 Imputed data | 3 | 714 | Mean Difference (IV, Fixed, 95% CI) | 2.19 [‐1.83, 6.20] |
| 16 FACT‐An Total 47 ‐ merged experimental study arms | 9 | 1815 | Mean Difference (IV, Fixed, 95% CI) | 6.92 [4.59, 9.25] |
10.1. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 1 Change in FACT‐An Total (47 items) ‐ overall.
10.2. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 2 Change in FACT‐An Total 47‐ sensitivity analysis.
10.3. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 3 Change in FACT‐An Total 47 ‐ baseline Hb.
10.4. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 4 Change in FACT‐An Total 47 ‐ different malignancies.
10.5. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 5 Change in FACT‐An Total 47 ‐ age.
10.6. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 6 Change in FACT‐An Total 47 ‐ different therapies.
10.7. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 7 Change in FACT‐An Total 47 ‐ different therapies differentiated.
10.8. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 8 Change in FACT‐An Total 47 ‐ epoetin versus darbepoetin.
10.9. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 9 Change in FACT‐An Total 47 ‐ duration of ESA medication.
10.10. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 10 Change in FACT‐An Total 47 ‐ iron supplementation.
10.11. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 11 Change in FACT‐An Total 47 ‐ allocation concealment.
10.12. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 12 Change in FACT‐An Total 47 ‐ masking.
10.13. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 13 Change in FACT‐An Total 47 ‐ intention‐to treat.
10.14. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 14 Change in FACT‐An Total 47 ‐ publication.
10.15. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 15 Change in Fact‐An Total 47 ‐ data type.
10.16. Analysis.

Comparison 10 Change in FACT‐An Total 47, Outcome 16 FACT‐An Total 47 ‐ merged experimental study arms.
Comparison 11. Thrombotic events.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Thrombotic events ‐ overall | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 2 Thrombotic events ‐ baseline Hb | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 2.1 Hb < 10 g/dL | 19 | 4231 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [1.06, 1.88] |
| 2.2 Hb 10 to 12 g/dL | 26 | 5491 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [1.33, 2.03] |
| 2.3 Hb > 12 g/dL | 13 | 5348 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [1.15, 1.80] |
| 2.4 Hb unclear | 2 | 428 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [1.02, 2.65] |
| 3 Thrombotic events ‐ different malignancies | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 3.1 solid tumours | 36 | 9121 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [1.41, 1.96] |
| 3.2 haematological malignancies | 8 | 2531 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.93, 1.90] |
| 3.3 mixed | 14 | 3693 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.98, 1.69] |
| 3.4 MDS | 2 | 153 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.08 [0.23, 18.84] |
| 3.5 not reported | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Thrombotic events ‐ age | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 4.1 children | 1 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.95 [0.61, 14.28] |
| 4.2 adults | 59 | 15276 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.33, 1.73] |
| 5 Thrombotic events ‐ age differentiated | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 5.1 children | 1 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.95 [0.61, 14.28] |
| 5.2 adults >= 18 | 46 | 11310 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [1.38, 1.86] |
| 5.3 > 68% non elderly, 18‐65 | 7 | 1028 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.71 [1.02, 2.86] |
| 5.4 only non elderly | 5 | 2882 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.86, 1.60] |
| 5.5 > 68% elderly > 65 years | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.01, 4.58] |
| 5.6 only elderly | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Thrombotic events ‐ different therapies | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 6.1 chemotherapy | 37 | 10844 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [1.27, 1.73] |
| 6.2 radiotherapy/radiochemotherapy | 11 | 2384 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [1.44, 2.83] |
| 6.3 no therapy | 8 | 1921 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.88, 1.78] |
| 6.4 unclear/other | 4 | 349 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.09 [0.74, 5.93] |
| 7 Thrombotic events ‐ different therapies differentiated | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 7.1 chemotherapy, > 70% with platinum | 16 | 3136 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [1.13, 1.89] |
| 7.2 chemotherapy, < 70% with platinum | 3 | 919 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.92, 2.88] |
| 7.3 chemotherapy, without platinum, all patients | 14 | 6085 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [1.14, 1.76] |
| 7.4 chemotherapy, platinum and non platinum containing, no numbers given | 2 | 265 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.56 [0.79, 26.20] |
| 7.5 chemotherapy no details given | 2 | 439 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.67, 4.76] |
| 7.6 radiochemotherapy | 7 | 1097 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.01 [1.37, 2.96] |
| 7.7 radiotherapy | 4 | 1287 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [1.02, 4.07] |
| 7.8 no therapy | 8 | 1921 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.88, 1.78] |
| 7.9 unclear/other | 4 | 349 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.09 [0.74, 5.93] |
| 8 Thrombotic events ‐ epoetin versus darbepoetin | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 8.1 Epoetin | 50 | 11055 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [1.33, 1.85] |
| 8.2 Darbepoetin | 10 | 4443 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [1.16, 1.79] |
| 9 Thrombotic events ‐ duration of ESA treatment | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 9.1 6 to 9 weeks | 10 | 1719 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.06 [1.17, 3.64] |
| 9.2 12 to 16 weeks | 30 | 7223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [1.20, 1.77] |
| 9.3 more than 17 weeks | 19 | 6312 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.53 [1.27, 1.84] |
| 9.4 not reported | 1 | 244 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.15, 13.85] |
| 10 Thrombotic events ‐ iron supplementation | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 10.1 fixed iron supplementation | 4 | 1445 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.53 [0.92, 2.54] |
| 10.2 iron supplementation as necessary | 47 | 12073 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.51 [1.31, 1.74] |
| 10.3 no explicit statement on iron supplementation or no iron given | 4 | 293 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.39, 4.06] |
| 10.4 iron handled differently in the study arms | 5 | 1687 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [1.12, 2.54] |
| 10.5 explicitly stated NO IRON | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Thrombotic events ‐ concealment of allocation | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 11.1 adequate | 38 | 10494 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [1.40, 1.92] |
| 11.2 unclear | 22 | 5004 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [1.04, 1.65] |
| 12 Thrombotic events ‐ masking | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 12.1 double‐blind | 32 | 9209 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [1.19, 1.64] |
| 12.2 unblinded | 28 | 6289 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.78 [1.43, 2.23] |
| 13 Thrombotic events ‐ intention‐to‐treat | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 13.1 ITT or less than 10% of participants per study arm excluded | 55 | 13182 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [1.30, 1.72] |
| 13.2 more than 10% of participants per study arm excluded | 3 | 1589 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.59 [0.95, 2.66] |
| 13.3 unclear | 2 | 727 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.82 [1.15, 2.89] |
| 14 Thrombotic events ‐ publication | 60 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.34, 1.74] |
| 14.1 full text publication | 35 | 8388 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [1.32, 1.87] |
| 14.2 abstract publication | 2 | 1343 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.70, 1.55] |
| 14.3 unpublished data | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.06, 33.82] |
| 14.4 data presented at ODAC hearing | 21 | 5645 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.66 [1.33, 2.08] |
| 14.5 other | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.01, 4.58] |
| 15 Thrombotic events ‐ experimental arms merged | 57 | 15498 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.53 [1.34, 1.74] |
11.1. Analysis.

Comparison 11 Thrombotic events, Outcome 1 Thrombotic events ‐ overall.
11.2. Analysis.

Comparison 11 Thrombotic events, Outcome 2 Thrombotic events ‐ baseline Hb.
11.3. Analysis.

Comparison 11 Thrombotic events, Outcome 3 Thrombotic events ‐ different malignancies.
11.4. Analysis.

Comparison 11 Thrombotic events, Outcome 4 Thrombotic events ‐ age.
11.5. Analysis.

Comparison 11 Thrombotic events, Outcome 5 Thrombotic events ‐ age differentiated.
11.6. Analysis.

Comparison 11 Thrombotic events, Outcome 6 Thrombotic events ‐ different therapies.
11.7. Analysis.

Comparison 11 Thrombotic events, Outcome 7 Thrombotic events ‐ different therapies differentiated.
11.8. Analysis.

Comparison 11 Thrombotic events, Outcome 8 Thrombotic events ‐ epoetin versus darbepoetin.
11.9. Analysis.

Comparison 11 Thrombotic events, Outcome 9 Thrombotic events ‐ duration of ESA treatment.
11.10. Analysis.

Comparison 11 Thrombotic events, Outcome 10 Thrombotic events ‐ iron supplementation.
11.11. Analysis.

Comparison 11 Thrombotic events, Outcome 11 Thrombotic events ‐ concealment of allocation.
11.12. Analysis.

Comparison 11 Thrombotic events, Outcome 12 Thrombotic events ‐ masking.
11.13. Analysis.

Comparison 11 Thrombotic events, Outcome 13 Thrombotic events ‐ intention‐to‐treat.
11.14. Analysis.

Comparison 11 Thrombotic events, Outcome 14 Thrombotic events ‐ publication.
11.15. Analysis.

Comparison 11 Thrombotic events, Outcome 15 Thrombotic events ‐ experimental arms merged.
Comparison 12. Hypertension.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hypertension ‐ overall | 37 | 7228 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [1.08, 1.56] |
| 2 Hypertension ‐ merged experimental study arms | 31 | 7228 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [1.09, 1.58] |
| 3 Hypertension ‐ sensitivity analysis Dammacco | 37 | 7228 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [1.10, 1.52] |
| 4 Hypertension ‐ sensitivity analysis random effects | 37 | 7228 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.94, 1.33] |
| 5 Hypertension ‐ sensitivity analysis without Rose | 36 | 7007 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.18, 1.97] |
12.1. Analysis.

Comparison 12 Hypertension, Outcome 1 Hypertension ‐ overall.
12.2. Analysis.

Comparison 12 Hypertension, Outcome 2 Hypertension ‐ merged experimental study arms.
12.3. Analysis.

Comparison 12 Hypertension, Outcome 3 Hypertension ‐ sensitivity analysis Dammacco.
12.4. Analysis.

Comparison 12 Hypertension, Outcome 4 Hypertension ‐ sensitivity analysis random effects.
12.5. Analysis.

Comparison 12 Hypertension, Outcome 5 Hypertension ‐ sensitivity analysis without Rose.
Comparison 13. Thrombocytopenia or haemorrhage.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Thrombocytopenia ‐ overall | 24 | 4507 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [1.04, 1.42] |
| 2 Thrombocytopenia ‐ merged experimental arms | 21 | 4507 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [1.04, 1.41] |
| 3 Thrombocytopenia ‐ sensitivity analysis random effects | 24 | 4507 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [1.02, 1.36] |
13.1. Analysis.

Comparison 13 Thrombocytopenia or haemorrhage, Outcome 1 Thrombocytopenia ‐ overall.
13.2. Analysis.

Comparison 13 Thrombocytopenia or haemorrhage, Outcome 2 Thrombocytopenia ‐ merged experimental arms.
13.3. Analysis.

Comparison 13 Thrombocytopenia or haemorrhage, Outcome 3 Thrombocytopenia ‐ sensitivity analysis random effects.
Comparison 14. Rash.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Rash ‐ overall | 18 | 2485 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.49 [0.99, 2.24] |
| 2 Rash ‐ merged experimental arms | 16 | 2485 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [1.00, 2.27] |
14.1. Analysis.
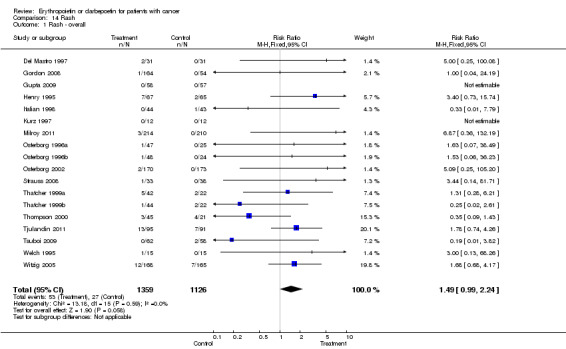
Comparison 14 Rash, Outcome 1 Rash ‐ overall.
14.2. Analysis.

Comparison 14 Rash, Outcome 2 Rash ‐ merged experimental arms.
Comparison 15. Seizure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Seizure ‐ overall | 8 | 2890 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.42, 1.41] |
15.1. Analysis.

Comparison 15 Seizure, Outcome 1 Seizure ‐ overall.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aapro 2008.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 463 randomised: ESA = 231; control = 232 disease: breast cancer (M1) treatment: chemotherapy mean/median baseline Hb: 11.4 g/dL |
|
| Interventions | drug: Epoetin beta dose: 30000 IU sc weekly Hb‐target: 13‐15 g/dL planned ESA duration: 24 weeks |
|
| Outcomes | primary: overall survival secondary: progression free survival, tumour response rate, QoL |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 97413) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Aapro 2008 IPD.
| Methods | see Aapro 2008 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Abels 1993.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 124 randomised: ESA = 65; control = 59 disease: hematological malignancies, genitourinary, gastrointestinal, and other cancer; except primary myeloid malignancy or acute leukaemia (category: mixed) treatment: none mean/median baseline Hb: 9.3 g/dL; |
|
| Interventions | drug: Epoetin alpha dose: 100 IU/kg tiw s.c. Hb‐target: not reported duration: 8 weeks |
|
| Outcomes | primary: transfusion, Hct secondary: QoL, safety |
|
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001) and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 98906) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ each patient was assigned a random identification number and was assigned to a treatment group by a computerised randomisation schedule |
Abels 1993 IPD.
| Methods | see Abels 1993 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Abels 1993 J&J 2004.
| Methods | see Abels 1993 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | Data presented by J&J at FDA/ODAC hearing in May 2004 | |
Antonadou 2001.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 385, randomised: ESA = 190, control = 195 disease: pelvic malignancies treatment: radiotherapy baseline Hb: 9.95 g/dL , ESA 9.8, control 10.1, , categorized as < 10g/dL |
|
| Interventions | drug: Epoetin dose: 10.000 U 5x/week s.c. Hb‐target: >= 13 g/dL duration: 5‐6 weeks |
|
| Outcomes | 4 years disease free survival, safety, Hb, tumour control, overall survival | |
| Notes | abstract, poster, study number = 10176 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | NR |
| Allocation concealment (selection bias) | Unclear risk | NR |
Aravantinos 2003.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 47 randomised: ESA = 24; control = 23 disease: ovarian, lung, stomach, other cancer (categorised as solid) treatment: platinum‐based chemotherapy Hb baseline: 9.6 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150 IU/kg tiw sc Hb target: 14 g/dL duration: NR, approx. >9‐12 weeks, categorized: 12‐16 weeks |
|
| Outcomes | primary: transfusion requirements (secondary: ?) Hct, Hb, RBC number | |
| Notes | full text publication, study number = 11595 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Bamias 2003.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 144 randomised: ESA = 72; control = 72 disease: ovarian, NSCLC, SCLC, other cancer (categorized: solid) treatment: platinum‐based chemotherapy Hb baseline: 11.5 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 10,000 IU tiw sc Hb target: 13 ‐ 15 g/dL duration: 21 to 24 weeks (duration of chemotherapy) |
|
| Outcomes | primary: transfusions secondary: Hb < 10 g/dL, predictors of response, optional: QoL |
|
| Notes | full text publication, study number = 16091 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Blohmer 2011.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 257, randomised: ESA = 128, control = 129 disease: cervical cancer treatment: platinum‐containing chemotherapy in all patients and radiotherapy (categorized as radiochemotherapy) baseline Hb: 11.9 g/dL , ESA 12.0 g/dL, control 11.8 g/dL, categorised as 10‐12 g/dL |
|
| Interventions | drug: Epoetin alfa dose: 10'000 IU sc. TIW Hb‐target: >14 g/dL duration: >20 weeks |
|
| Outcomes | primary: relapse free survival | |
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001), study number = 16218 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Yes ‐ computer random‐numbers generator |
| Allocation concealment (selection bias) | Low risk | Yes ‐ central registration of the patients for treatment allocation |
Boogaerts 2003.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 262 randomised: ESA = 133; control = 129 disease: multiple myeloma, Non‐Hodgkin lymphoma, chronic lymphocytic leukaemia, Hodgkin disease, ovarian, bone, gastrointestinal, respiratory, other cancer treatment: chemotherapy baseline Hb: 9.0 g/dL |
|
| Interventions | drug: Epoetin beta dose: 150 IU/kg sc TIW Hb‐target: 12‐14 g/dL planned ESA duration: 12 weeks |
|
| Outcomes | primary: QoL secondary: hematologic response, hematopoietic response, Hb change, transfusions, PS, Hct |
|
| Notes | full text publication of the study previously published as abstract Coiffier 2001, additional unpublished data were obtained for the first Cochrane review (1985‐2001) and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 36158) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Boogaerts 2003 IPD.
| Methods | see Boogaerts 2003 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Boogaerts Coiffier 2001.
| Methods | see Boogaerts 2003 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | Abstract | |
Carabantes 1999.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 35, randomised: ESA = 20, control = 15 disease: SCLC and ovarian carcinoma treatment: platinum‐containing chemotherapy baseline Hb: (at randomisation): 10.5 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150U/kg 3x/week s.c. Hb target: NR control: no treatment duration: 18‐24 weeks |
|
| Outcomes | haematologic response, transfusion requirements, QoL | |
| Notes | abstract publication, study number = 17026 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Unclear risk | unclear |
Cascinu 1994.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 100, randomised: ESA = 50; control = 50 disease: various solid tumours treatment: concomitant platinum‐based chemotherapy; some patients received G‐CSF (n = 27) mean/median baseline Hb: 8.7 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 100 U/kg 3x/week s.c. Hb target: 10 ‐ 12 g/dL duration: 9 weeks |
|
| Outcomes | haematologic response, change in Hb values, transfusion requirement, adverse events | |
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001), study number = 19548 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Yes ‐ computer random‐number generator |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ sealed envelopes |
Case 1993.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 157, randomised: ESA = 81; control = 76 disease: non myeloid hematological malignancies, breast, lung, gynaecological, gastrointestinal, other cancer treatment: non‐cisplatin chemotherapy mean/median baseline Hematocrit: 28.9% |
|
| Interventions | drug: Epoetin alpha dose: 150U/kg 3x/week s.c. Hb target: Hct 38%‐40% duration: 12 weeks |
|
| Outcomes | haematologic response, change in Hct, transfusion requirement, QoL, adverse events | |
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001) and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 34917) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ description is unclear |
Case 1993 IPD.
| Methods | see Case 1993 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 34917 | |
Case 1993 J&J 2004.
| Methods | see Case 1993 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Cazzola 1995.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 146, randomised: control = 29 (IPD: control:30, EPO: 116), evaluated EPO:114, control: 29 ESAa = 31; ESAb = 29; ESAc = 31; ESAd = 26; ESAtotal = 117 disease: multiple myeloma, Non‐Hodgkin´s Lymphoma treatment: chemotherapy, assumed without platinum because of hematological disease mean/median baseline Hb: 9.4 g/dL |
|
| Interventions | drug: Epoetin beta dosages: a: 1000 IU sc 7x/week; b: 2000 IU sc 7x/week; c: 5000 IU sc 7x/ week; d: 10000 IU sc 7x/week Hb‐target: 11‐13 g/dL (MM), 11‐15 g/dL (NHL) a: 1000 IU sc 7x/week, b: 2000 IU sc 7x/week; c: 5000 IU sc 7x/ week; d: 10000 IU sc 7x/week duration: 8 weeks |
|
| Outcomes | primary: haematologic response secondary: Hb, Hct, transfusions, reticulocytes, iron, ferritin, safety |
|
| Notes | full text publication, additional unpublished data obtained for first Cochrane Review and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 37653) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ randomisation list |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Cazzola 1995 IPD.
| Methods | seeCazzola 1995 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Cazzola 1995a.
| Methods | see Cazzola 1995 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Cazzola 1995b.
| Methods | see Cazzola 1995 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Cazzola 1995c.
| Methods | see Cazzola 1995 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Cazzola 1995d.
| Methods | see Cazzola 1995 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Chang 2005.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 354, randomised: ESA = 176; control = 178 disease: breast cancer, stage I‐IV treatment: chemotherapy baseline Hb: 11.3 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 40,000 IU qw sc Hb target: 14 g/dL duration: 16 weeks, max 28 weeks |
|
| Outcomes | primary: QoL secondary: maintain Hb above 12 g/dL, tumour response, overall survival |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 99137) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Chang 2005 IPD.
| Methods | see Chang 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 99137 | |
Charu 2007.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 287, randomised: ESA = 228, control = 59 disease: lymphoma, breast, lung, gastrointestinal, genitourinary, gynaecologic, other cancer treatment: none baseline Hb: 10.2 g/dL |
|
| Interventions | drug: Darbepoetin alpha dose: 3.0 µg/kg sc Q2W Hb‐target: 13‐14 g/dL (women), 13‐15 g/dL (men) duration: 12 weeks |
|
| Outcomes | primary: hospitalisation days secondary: costs, QoL, transfusion, Hb, safety |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 53081) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Charu 2007 Amgen 2007.
| Methods | see Charu 2007 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Charu 2007 IPD.
| Methods | see Charu 2007 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Christodoulou 2009.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 399, randomised: NR, evaluated: ESA 167, control = 170 disease: solid tumours treatment: chemotherapy, platinum and non‐platinum containing baseline Hb: 10.2 g/dL |
|
| Interventions | drug: Epoetin alfa dose: 10'000 IU TIW Hb‐target: 12 ‐ 14 g/dL duration: minimum anticipated duration 12 weeks. categorized 12‐16 weeks |
|
| Outcomes | primary: QoL secondary: transfusions, anaemia |
|
| Notes | full text publication, abstract in 2003 (Janinis), study number = 22108 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ block randomisation |
| Allocation concealment (selection bias) | Low risk | yes ‐ centrally randomised |
Dammacco 2001.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 145, randomised: ESA = 69; control = 76 disease: multiple myeloma treatment: chemotherapy mean/median baseline Hb: 9.5 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150U/kg 3x/week s.c. Hb target: 14 g/dL duration: 12 weeks |
|
| Outcomes | primary: transfusion secondary: haematologic response, Hb, Hct, reticulocytes, serum erythropoietin levels, QoL, adverse events |
|
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001) and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 11220) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ randomisation schedule prepared by RWJPRI |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ two randomisation lists (pat. prev. transfused or not), when patient enters the study the next number was to be assigned |
Dammacco 2001 IPD.
| Methods | see Dammacco 2001 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Dammacco 2001 J&J 2004.
| Methods | see Dammacco 2001 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | Data presented by J&J at FDA/ODAC hearing in May 2004 | |
Debus 2006 IPD.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 385, randomised: ESA = 195, control = 190 disease: NSCLC (stage III, primarily inoperable) treatment: radiochemotherapy baseline Hb: not reported, unclear |
|
| Interventions | drug: Epoetin alpha dose: 40'000 IU sc weekly Hb‐target: 12‐14 g/dL, in 11/2003 reduced to 12‐13 g/dL duration: assumed to be 12‐16 weeks |
|
| Outcomes | primary: 2‐year‐survival rate secondary: tumour response, QoL, tolerance to epoetin alpha, Hb change, transfusion, safety |
|
| Notes | only unpublished data available, were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 83322) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ randomisation code provided by OrthoBiotech |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ assigned envelopes, sequentially numbered, but it is unclear whether they were sealed and opaque |
Debus 2006 J&J 2004.
| Methods | see Debus 2006 IPD | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Debus 2006 J&J 2007.
| Methods | see Debus 2006 IPD | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Del Mastro 1997.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 62, randomised: ESA = 31, control = 31 disease: breast cancer treatment: non‐platinum based chemotherapy and G‐CSF 5µg/kg d4‐d11 s.c for all patients; radiotherapy and Tamoxifen fore the majority mean/median baseline Hb: 13.1 g/dL |
|
| Interventions | drug: Epoetin (?) dose: 150U/kg 3x/week s.c. Hb target: 13‐15 g/dL duration: 14 weeks |
|
| Outcomes | change in Hb values, transfusion requirement, QoL, adverse events | |
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001), study number = 24367 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Yes ‐ computer random‐number generator |
| Allocation concealment (selection bias) | Low risk | Yes ‐ central allocation |
Dunphy 1999.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 30, randomised: ESA = 15, control = 15 disease: head and neck cancer, NSCLC treatment: platinum‐based chemotherapy mean/median baseline Hb: 14.1 g/dL |
|
| Interventions | drug: Epoetin (?) dose: 150U/kg 3x/week s.c. Hb target: 16‐18 g/dL duration: 6 weeks |
|
| Outcomes | change in Hb values, transfusion requirement | |
| Notes | full text publication, study number = 25455 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Engert 2009.
| Methods | See Engert 2010 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Engert 2010.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 1,379, randomised ESA: 685, placebo: 694 disease: advanced stage Hodgkin Lymphoma treatment: chemotherapy without platinum baseline Hb: 12.5 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 40,000 IU /week Hb target: 12‐13 g/dL duration: > 20 weeks |
|
| Outcomes | primary: anaemia‐related fatigue secondary: other QoL, number of transfusions needed, Hb during and after treatment, safety, freedom from treatment failure, OS |
|
| Notes | full‐text publication, additional unpublished data, study number = 27258 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear, not reported |
| Allocation concealment (selection bias) | Unclear risk | unclear, not reported |
EPO‐GER‐20 IPD.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | n = 93, randomised: ESA = 45, control = 48 disease: SCLC (extensive stage) treatment: chemotherapy baseline Hb: not reported, unclear |
|
| Interventions | drug: Epoetin alpha dose: 10000 IU sc TIW Hb‐target: 12‐14 g/dL duration: during chemotherapy |
|
| Outcomes | primary: rate of patients with anaemia secondary: QoL, tolerability of ESA, transfusion, effectiveness of chemotherapy |
|
| Notes | only IPD data, study number = 31678 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ patients were assigned with a randomisation code provided by Janssen‐Cilag |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ assigned envelopes, sequentially numbered, but it is unclear whether they were sealed and opaque |
EPO‐INT‐1 IPD.
| Methods | see EPO‐INT‐1 J&J 2004 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
EPO‐INT‐1 J&J 2004.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 246, randomised: ESA = 165, control = 81 disease: ovarian cancer (stage I‐IV) treatment: chemotherapy baseline Hb: not reported, eligibility criterion Hb < 11 g/dL or Hb drop 1.5 g/dL, categorized as Hb 10‐12 g/dL |
|
| Interventions | drug: Epoetin alpha dose: a: 150, b: 300 IU/kg tiw sc Hb‐target: 14 g/dL duration: 1 month |
|
| Outcomes | primary: transfusion secondary: Hb change, Hct, QoL, survival |
|
| Notes | data presented by J&J at FDA/ODAC hearing in may 2004, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 53915) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ no description |
EPO‐INT‐3 IPD.
| Methods | see EPO‐INT‐3 J&J 2004 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
EPO‐INT‐3 J&J 2004.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 201, randomised: ESA = 136, control = 65 disease: breast, NHL, MM, ovarian, SCLC, other cancer treatment: chemotherapy, < 70% platinum containing baseline Hb: not reported, eligibility criterion Hb < 12 g/dL or Hb drop 1.5 g/dL, categorized as Hb 10‐12 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150‐300 IU/kg tiw sc Hb‐target: 14 g/dL for women and 16 g/dL for men duration: 12 weeks |
|
| Outcomes | primary: transfusions secondary: mortality, disease progression, tumour response, adverse events, Hb, QoL |
|
| Notes | Data presented by J&J at FDA/ODAC hearing in May 2004, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 36274), clinicaltrials.gov | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ according to randomisation schedule prepared by RWJPRI |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Fujisaka 2011.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | randomised N = 186, evaluated N = 181, ESA = 89, control = 92 disease: lung cancer, gynaecological cancer treatment: platinum‐based chemotherapy baseline Hb: 9.4 g/dL duration: 12 weeks |
|
| Interventions | drug: epoetin beta dose: 36,000 IU/week target Hb: 12.0g/dL duration: 12 weeks |
|
| Outcomes | primary: proportion of patients receiving RBCTs and/or Hb<8.0 g/dL secondary: need for transfusions, changes in Hb, QoL |
|
| Notes | full‐text publication, study id: 15478 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not reported |
| Allocation concealment (selection bias) | Low risk | central randomisation system |
Gebbia 2003.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 45, randomised ESA = 22, control = 23 disease: squamous cell carcinoma of the head an neck treatment: platinum‐containing chemotherapy baseline Hb: 12.1 g/dL |
|
| Interventions | drug: rhEpo dose: 10'000IU tiw Hb‐target: 12‐14 g/dL duration: NR |
|
| Outcomes | primary: NR secondary: transfusion, QoL, clinical outcome |
|
| Notes | full text publication, study number = 29327 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Unclear risk | unclear |
Gordon 2008.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 220, randomised: ESA = 164, control = 56 disease: non‐myeloid hematological malignancies, breast, gastrointestinal, genitourinary, lung, gynaecological, other cancer (stage I‐IV) therapy: none baseline Hb: 10.2 g/dL |
|
| Interventions | drug: Darbepoetin alpha dose: 6.75 µg/kg sc Q4W Hb‐target: 12‐13 g/dL duration: 16 weeks |
|
| Outcomes | primary: Hb response secondary: transfusion, Hb change, QoL, safety |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 65772) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ randomisation list will be centrally generated by Amgen |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Gordon 2008 IPD.
| Methods | see Gordon 2008 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Goss 2005.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 104, randomised: ESA = 52, control = 52 disease:SCLC (limited disease) treatment: radiochemotherapy baseline Hb: 13.5 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 40000 IU sc weekly Hb‐target: 14‐16 g/dL, in 10/2002 reduced to 12‐14 g/dL duration: during chemotherapy and radiotherapy |
|
| Outcomes | disease progression free survival, tumour response, overall survival, local disease progression, Hb, transfusion, QoL | |
| Notes | abstract publication, additional unpublished data obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 55703) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer‐generated |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Goss 2005 FDA 2004.
| Methods | see Goss 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Goss 2005 IPD.
| Methods | see Goss 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Goss 2005 J&J 2004.
| Methods | see Goss 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Grote 2005.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 224, randomised: ESA = 109, control = 115 disease: SCLC (limited and extensive disease) treatment: chemotherapy baseline Hb: 12.9 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150 IU/kg sc TIW Hb‐target: 14‐16 g/dL duration: NR, assumed to be 12 weeks (drug given during 3 x 3 weeks chemo plus 3 weeks) |
|
| Outcomes | primary: assess possible stimulatory effects of ESA on solid tumour growth, tumour response secondary: overall survival, Hb, transfusion, safety |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 73807) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ description is unclear |
Grote 2005 IPD.
| Methods | see Grote 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Grote 2005 J&J 2004.
| Methods | see Grote 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Gupta 2009.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 120, randomised: ESA = 60, control = 60 disease: cervical cancer treatment: platinum‐containing in all patients plus radiotherapy baseline Hb: 10.6 g/dL |
|
| Interventions | drug: Epoetin beta dose: 30'000 IU TIW Hb‐target: unclear duration: unclear |
|
| Outcomes | primary: Hb, energy level, QoL secondary: response rate, survival, toxicities, adverse events |
|
| Notes | full text publication, study number = 30057 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Unclear risk | unclear |
Hedenus 2002.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 66, randomised: ESA = 55, control = 11 disease: lymphoma: HD, NHL, MM treatment: NR, assumed to be chemotherapy without platinum baseline Hb: 9.6 g/dL |
|
| Interventions | drug: Darbepoetin alpha dosages: a: 1.0 µg/kg qw sc; b: 2.25 µg/kg qw sc; c:Darbepoetin 4.5 µg/kg qw sc Hb target: 13‐14 g/dL for women and 13‐15 g/dL for men duration: 12 weeks |
|
| Outcomes | primary: dose response relationship of darbepoetin in haemoglobin or haematopoietic response and overall survival secondary: transfusion |
|
| Notes | full text publication, study number = 32213 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Low risk | yes ‐ central computerized system |
Hedenus 2002a.
| Methods | see Hedenus 2002 | |
| Participants | ||
| Interventions | Darbepoetin 1.0 µg/kg qw sc | |
| Outcomes | ||
| Notes | ||
Hedenus 2002b.
| Methods | see Hedenus 2002 | |
| Participants | ||
| Interventions | Darbepoetin 2.25 µg/kg qw sc | |
| Outcomes | ||
| Notes | ||
Hedenus 2002c.
| Methods | see Hedenus 2002 | |
| Participants | ||
| Interventions | Darbepoetin 4.5 µg/kg qw sc | |
| Outcomes | ||
| Notes | ||
Hedenus 2003.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 349, randomised: ESA = 176, control = 173 disease: lymphoma: Hodgkin disease, NHL, MM, CLL, Waldenstrom´s disease treatment: NR, assumed to be chemotherapy without platinum Hb baseline: 9.5 g/dL |
|
| Interventions | drug: Darbepoetin alpha dose: 2.25 mg/kg qw sc Hb target: 13‐14 g/dL (women), 13‐15 g/dL (men) duration: 12 weeks |
|
| Outcomes | primary: Hb response secondary: transfusion, Hb change, QoL, safety |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 63455) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ based on a schedule specified by Amgen before the start of the study |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Hedenus 2003 FDA 2007.
| Methods | see Hedenus 2003 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Hedenus 2003 IPD.
| Methods | see Hedenus 2003 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | 63455 | |
Henke 1999.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 50, randomised: control = 11; ESAa = 19; ESAb = 14; ESAc = 6; ESAtotal = 39 disease: various solid tumours treatment: radiotherapy mean/median baseline Hb: 11.5 g/dL |
|
| Interventions | drug: Epoetin alpha or beta dose: ESAa: 150U/kg 3x/week i.v., ESAb: 300U/kg 3x/week i.v., ESAc: 150U/kg 3x/week s.c.; Hb target: 14 ‐ 16 g/dL (men) or 13 ‐ 15 g/dL (women) duration: 8 weeks |
|
| Outcomes | haematologic response, change in Hb values | |
| Notes | full text publication, study number = 39895 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Henke 1999a.
| Methods | see Henke 1999 | |
| Participants | n = 19 | |
| Interventions | Epoetin alpha or beta a: 150U/kg 3x/week i.v. | |
| Outcomes | ||
| Notes | ||
Henke 1999b.
| Methods | see Henke 1999 | |
| Participants | n = 14 | |
| Interventions | Epoetin alpha or beta b: 300U/kg 3x/week i.v.; | |
| Outcomes | ||
| Notes | ||
Henke 1999c.
| Methods | see Henke 1999 | |
| Participants | n= 6 | |
| Interventions | Epoetin alpha or beta c: 150U/kg 3x/week s.c. | |
| Outcomes | ||
| Notes | ||
Henke 2003.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 351, randomised: ESA = 180, control = 171 disease: advanced (stage III , IV) head and neck cancer treatment: radiotherapy baseline Hb: 11.8 g/dL |
|
| Interventions | drug: Epoetin beta dose: 300 IU/kg tiw sc Hb‐target: 12‐14 g/dL (women), 13‐15 g/dL (men) duration: 7‐9 weeks |
|
| Outcomes | primary: efficacy of radiotherapy, measured as local progression free survival secondary: survival, progression free survival, Hb, safety, tolerability |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 58106) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ each centre had numbered packages per stratum, once randomised the lowest number had to be assigned. There was a randomisation list only the statistics centre had access to. In addition, there were sealed envelopes for emergencies. |
| Allocation concealment (selection bias) | Low risk | yes ‐ coded drug packs of identical appearance |
Henke 2003 IPD.
| Methods | see Henke 2003 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Henke 2003 Roche 2004.
| Methods | See Henke 2003 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | Data presented by Roche at FDA/ODAC hearing in May 2004 | |
Henry 1995.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 132, randomised: ESA = 67, control = 65 disease: any type of cancer except primary myeloid malignancy or acute leukaemia treatment: platinum‐containing chemotherapy baseline Hb: 9.5 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150 IU/kg sc TIW Hb‐target: Hct 38%‐40% duration: 12 weeks |
|
| Outcomes | primary: Hct, transfusion, haematologic response secondary: correction of anaemia, response, QoL, safety |
|
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001) and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 70332) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer generated |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ medication boxes were used, but without identical appearance |
Henry 1995 IPD.
| Methods | see Henry 1995 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 70332 | |
Henry 1995 J&J 2004.
| Methods | see Henry 1995 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | Data presented by J&J at FDA/ODAC hearing in May 2004 | |
Hernandez 2009.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | n = 391, randomised: ESA = 196, control = 195 disease: non‐myeloid haematological malignancies, breast, lung, gastrointestinal, genitourinary, gynaecological, other cancer (stage I‐IV) treatment: chemotherapy, 36% receiving platinum baseline Hb:10.1 g/dL |
|
| Interventions | drug: Darbepoetin alpha dose: 300 µg sc Q3W Hb‐target: 12‐13 g/dL duration: 15 weeks |
|
| Outcomes | primary: transfusion secondary: Hb target achieved, number of transfusions, safety, QoL |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 37476, Taylor 2005) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Hernandez 2009 IPD.
| Methods | see Hernandez 2009 was Taylor 2005 in IPD meta‐analysis by Bohlius et al 2009 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 37476 | |
Hoskin 2009.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 300, randomised: ESA = 151, control = 149 disease: head and neck cancer (stage I‐IV) treatment: radiotherapy, no chemotherapy baseline Hb: 13.6 g/dL |
|
| Interventions | drug: Epoetin alpha dose: if Hb < 12.5 10000 IU sc TIW; if Hb > 12.5 4000 IU sc TIW Hb‐target: 14.5 to 15 g/dL duration: 12 weeks |
|
| Outcomes | primary: local disease free survival secondary: overall survival, QoL, safety |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 81645) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ central randomisation schedule stratified by the study site was generated by the sponsor |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ no description |
Hoskin 2009 GBR‐7 FDA 04.
| Methods | see Hoskin 2009 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | unpublished study, data obtained from FDA report for the FDA/ODAC in hearing May 2004 | |
Hoskin 2009 IPD.
| Methods | see Hoskin 2009 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 81645 | |
Hoskin 2009 J&J 2004.
| Methods | see Hoskin 2009 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Huddart 2002.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 95, randomised: ESA = 48, control = 47 disease: lung, gynaecological, genitourinary, other cancer treatment: platinum‐containing chemotherapy baseline Hb: not reported, eligibility criterion Hb < 10.5 g/dL, categorized as Hb 10‐12 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 10,000 IU tiw Hb‐target: 12‐14 g/dL duration: max 28 weeks |
|
| Outcomes | Hb response, reticulocyte, survival, QoL, safety | |
| Notes | abstract, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 88443) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ no description |
Huddart 2002 IPD.
| Methods | see Huddart 2002 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 88443 | |
Iconomou 2003.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 122, randomised: ESA = 57, control = 55 disease: lung, breast, colorectal, ovarian, unknown primary, kidney, stomach, other cancer treatment: chemotherapy, platinum & non platinum baseline Hb: 10.1 g/dL |
|
| Interventions | drug and dose: NR, assumed Epoetin alpha 10,000 IU tiw sc Hb target: NR duration: 12 weeks |
|
| Outcomes | primary: QoL secondary: Hb, transfusions |
|
| Notes | full text publication, study number = 40799 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Low risk | Randomisation was performed by a telephone call to the registry of the department of medicine |
Italian 1998.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 87, randomised: ESA = 44, control = 43 disease: Myelodysplastic Syndromes treatment: none mean/median baseline Hb: 8.2 g/dL; |
|
| Interventions | drug: Epoetin alpha dose: 150U/kg 3x/week s.c. Hb target: not reported duration: 8 weeks, thereafter Epo for all the patients |
|
| Outcomes | haematologic response, change in haemoglobin values, adverse events | |
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001), study number = 46703 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Yes ‐ computer random number generator |
| Allocation concealment (selection bias) | Low risk | Yes ‐ central registration by telephone before treatment assignment |
Katakami 2008.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 207, ESA = 103, control = 104 disease: lung and gynaecologic cancer treatment: platinum‐containing chemotherapy baseline Hb: not reported, eligibility criterion Hb <= 11 g/dL, categorized as Hb 10‐12 g/dL |
|
| Interventions | drug: darbepoetin alfa dose: 2.25 ug/kg once per week sc Hb target: 13.0 g/dL (amended to 12.0 g/dL) duration: 12 weeks |
|
| Outcomes | proportion of patients reaching transfusion trigger or receiving RBCT, haematologic endpoints, adverse events, survival |
|
| Notes | abstract publication (study id: 13567) additional study reporting exactly the same: Katsumata 2009 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear, not reported |
| Allocation concealment (selection bias) | Unclear risk | unclear, not reported |
Kotasek 2002.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 161, randomised: ESA = 129, control = 32 disease: lung, breast, gastrointestinal, genitourinary, gynaecological, other cancer (stage I‐IV) treatment: chemotherapy baseline Hb: not reported, eligibility criterion Hb <= 11 g/dL, categorized as Hb 10‐12 g/dL |
|
| Interventions | drug: Darbepoetin alpha dose: a: 9 µg/kg sc Q4W, b: 12 µg/kg sc Q4W, c: 15 µg/kg sc Q4W, d: 18 µg/kg sc Q4W Hb‐target: 13‐14 g/dL (women), 13‐15 g/dL (men) duration: 12 weeks |
|
| Outcomes | primary: safety secondary: determine effective dose, effect of ESA, QoL feasibility |
|
| Notes | additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 26117) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Kotasek 2002 IPD.
| Methods | see Kotasek 2002 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Kotasek 2003.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 259, randomised: ESA = 208, control = 51 disease: breast, gynaecological, gastrointestinal, lung, genitourinary, other cancer treatment: chemotherapy, not reported whether with or without platinum, interpreted as some patients receiving platinum baseline Hb: 9.9 g/dL |
|
| Interventions | drug = Darbepoetin alpha dose = a: 4.5 µg/kg sc Q3W, b: 6.75 µg/kg sc Q3W, c: 9 µg/kg sc Q3W, d: 12 µg/kg sc Q3W, e: 13.5 µg/kg sc Q3W, f: 15 µg/kg sc Q3W Hb‐target = 13‐14 g/dL (women), 13‐15 g/dL (men) duration = 12 weeks |
|
| Outcomes | primary: safety secondary: determine effective dose, effect of ESA, QoL feasibility |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 35466) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Kotasek 2003 IPD.
| Methods | see Kotasek 2003 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 35466 | |
Kotasek 2003a.
| Methods | see Kotasek 2003 | |
| Participants | N = 32 | |
| Interventions | Darbepoetin 4.5 µg/kg Q3W sc | |
| Outcomes | ||
| Notes | ||
Kotasek 2003b.
| Methods | see Kotasek 2003 | |
| Participants | N = 17 | |
| Interventions | Darbepoetin 6.75 µg/kg Q3W sc | |
| Outcomes | ||
| Notes | ||
Kotasek 2003c.
| Methods | see Kotasek 2003 | |
| Participants | N = 46 | |
| Interventions | Darbepoetin 9 µg/kg Q3W sc | |
| Outcomes | ||
| Notes | ||
Kotasek 2003d.
| Methods | see Kotasek 2003 | |
| Participants | N = 28 | |
| Interventions | Darbepoetin 12 µg/kg Q3W sc | |
| Outcomes | ||
| Notes | ||
Kotasek 2003e.
| Methods | see Kotasek 2003 | |
| Participants | N = 35 | |
| Interventions | Darbepeotin 13.5 µg/kg Q3W sc | |
| Outcomes | ||
| Notes | ||
Kotasek 2003f.
| Methods | see Kotasek 2003 | |
| Participants | N = 40 | |
| Interventions | Darbepoetin 15 µg/kg Q3W sc | |
| Outcomes | ||
| Notes | ||
Krzakowski 2008.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 313, randomised: ESA a = 104, ESA b = 105, control = 104 disease: lung cancer, gastrointestinal tumour, breast cancer, genitourinary, haematological and other cancer treatment: platinum and non‐platinum containing chemotherapy baseline Hb: 9.4 g/dL |
|
| Interventions | drug: Epoetin delta dose: a: 150 IU/kg tiw, b: 300 IU/kg tiw Hb‐target: 12 ‐ 14 g/dL duration: 12 weeks |
|
| Outcomes | primary: Hb, RBC, transfusions secondary: haematocrit, FACT‐An, subgroup analysis for type of cancer/ chemotherapy |
|
| Notes | full text publication, study number = 49839 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Unclear risk | unclear |
Krzakowski 2008a.
| Methods | see Krzakowski 2008 | |
| Participants | ESA a = 104 | |
| Interventions | dose: a: 150 IU/kg tiw | |
| Outcomes | ||
| Notes | ||
Krzakowski 2008b.
| Methods | see Krzakowski 2008 | |
| Participants | ESA b = 105 | |
| Interventions | dose: b: 300 IU/kg tiw | |
| Outcomes | ||
| Notes | ||
Kunikane 2001.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 72, evaluated: 53. randomisation is only given for those: Epoetin a = 16, Epoetin b = 18, control = 19 disease: NSCLC treatment: platinum based chemotherapy baseline Hb: 12.3 g/dL |
|
| Interventions | drug: Epoetin beta dose: 1: 100U/kg 3x/week s.c.; 2: 200U/kg 3x/week s.c. Hb‐target: 14 g/dL in women, 16 g/dL in men duration: 6 weeks |
|
| Outcomes | change in Hb values, transfusion requirement, adverse events | |
| Notes | full text publication, additional unpublished data obtained for first Cochrane Review, study number = 51164 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Low risk | yes ‐ central registration before treatment assignment |
Kunikane 2001a.
| Methods | see Kunikane 2001 | |
| Participants | Epoetin 1: n = 16 | |
| Interventions | Epoetin beta 1: 100U/kg 3x/week s.c. | |
| Outcomes | ||
| Notes | ||
Kunikane 2001b.
| Methods | see Kunikane 2001 | |
| Participants | ||
| Interventions | Epoetin beta 2: 200U/kg 3x/week s.c. | |
| Outcomes | ||
| Notes | ||
Kurz 1997.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 35, randomised: ESA = 23, control = 13 disease: gynaecologic tumours treatment: platinum based chemotherapy baseline Hb: 9.9 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150U/kg 3x/week s.c. Hb‐target: no upper target reported duration: 12 weeks |
|
| Outcomes | haematologic response, change in Haemoglobin values, transfusion requirement, Quality of Life, adverse events | |
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001), study number = 54819 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Yes ‐ random permuted blocks and a corresponding randomisation list at the randomisation office |
| Allocation concealment (selection bias) | Low risk | Yes ‐ registration of the patients with an institution seperate from the centre where patients were recruited before treatment assignment |
Leyland‐Jones 05 J&J 04.
| Methods | see Leyland‐Jones 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | Data presented by J&J at FDA/ODAC hearing in May 2004 | |
Leyland‐Jones 2005.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 939, randomised: ESA = 469, control = 470 disease: metastatic breast cancer (stage IV, M1) treatment: chemotherapy baseline Hb: 12.5 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 40,000 IU qw sc Hb‐target = 12‐14 g/dL duration: 52 weeks |
|
| Outcomes | primary: overall survival secondary: Hb, transfusion, tumour control, QoL, time to progression |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 17100) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer‐generated |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Leyland‐Jones 2005 IPD.
| Methods | see Leyland‐Jones 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 17100 | |
Littlewood 2001.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N=375, randomised: ESA = 251, control = 124 disease: NHL, MM, HD, CLL, gastrointestinal, other cancer treatment: chemotherapy without platinum baseline Hb: 9.8 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150 IU/kg sc TIW Hb‐target: 12‐15 g/dL duration: 28 weeks |
|
| Outcomes | primary: transfusion secondary: haematologic response, Hb, Hct, reticulocytes, predictors for response, QoL, adverse events, after protocol amendment also survival |
|
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001) and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 17123) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer‐generated randomisation schedule prepared by RWJPRI |
| Allocation concealment (selection bias) | Low risk | yes ‐ coded drug packs of identical appearance |
Littlewood 2001 IPD.
| Methods | see Littlewood 2001 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 17123 | |
Littlewood 2001 J&J 2004.
| Methods | SeeLittlewood 2001 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | Data presented by J&J at FDA/ODAC hearing in May 2004 | |
Machtay 2007.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 148, randomised: ESA = 77, control = 71 disease: head and neck cancer (stage I‐IV) treatment: radiotherapy, advanced stages received in addition platinum based chemotherapy baseline Hb: 12.1 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 40'000 IU sc weekly Hb‐target: 12.5‐14 g/dL (women), 13.5‐16 g/dL (men) duration: 8‐10 weeks |
|
| Outcomes | primary: local regional control tumour response secondary: overall survival, patterns of failure, local‐regional progression‐free survival, Hb, toxicity, QoL |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 87660), old publication was Machtay 2004 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Machtay 2007 IPD.
| Methods | see Machtay 2007 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 87660 | |
Milroy 2003 IPD.
| Methods | see Milroy 2011 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Milroy 2011.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 424, randomised: ESA = 214, control = 210 disease: NSCLC (stage IIIb or IV, advanced) treatment: platinum‐based chemotherapy baseline Hb: 12.7 g/dL |
|
| Interventions | drug: Epoetin alpha dose: if body weight > 45 kg 10000 IU sc TIW, if body weight < 45 kg 5000 IU sc TIW Hb‐target: 12.5‐14 g/dL (women), 13.5‐15 g/dL (men) duration = during chemotherapy |
|
| Outcomes | primary: QoL secondary: Hb, tumour response, survival, transfusion |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 67954) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
ML17616 2006.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 60 disease: MM, NHL and Cll treatment: chemotherapy, assumed to be without platinum because of hematological disease baseline Hb: not reported, eligibility criterion Hb <10 g/dL, categorized as Hb baseline < 10 g/dL |
|
| Interventions | drug: epoetin beta dose: 150 IU/kg TIW Hb‐target: NR duration: 12 weeks |
|
| Outcomes | primary: hematologic response secondary: Hb, transfusions, safety |
|
| Notes | clinical trial result information, study number = 99765 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Unclear risk | unclear |
ML17620 2006.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 121 disease: solid tumours treatment: platinum‐based chemotherapy baseline Hb: not reported, unclear |
|
| Interventions | drug: epoetin beta dose: 150 IU/kg TIW Hb‐target: NR duration: 12 weeks |
|
| Outcomes | primary: hematologic response secondary: Hb, transfusions, Hct, safety, blood pressure |
|
| Notes | clinical trial result information, study number = 10373 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Unclear risk | unclear |
Moebus 2007.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 643, randomised: ESA = 324, control = 319 disease: breast cancer (high risk, stage II/IIIA; M0) treatment: chemotherapy without platinum baseline Hb: 12.6 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150 IU/kg sc TIW Hb‐target: 13‐14 g/dL duration: 18 weeks |
|
| Outcomes | primary: transfusion, Hb secondary: recurrence free survival, overall survival, relapse, QoL |
|
| Notes | abstract publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001) and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 22515) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer random‐number generator |
| Allocation concealment (selection bias) | Low risk | yes ‐ central registration of patients before treatment allocation |
Moebus 2007 IPD.
| Methods | see Moebus 2007 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Moebus 2007 J&J 2007.
| Methods | see Moebus 2007 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Mystakidou 2005.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 100, randomised: ESA = 50, control = 50 disease: pancreatic, genital, colon and lung cancer treatment: none baseline Hb: 10.01 g/dL; for ESA group 9.87g/dL for control group 10.15, categorized as 10‐12 g/dL |
|
| Interventions | drug: Epoetin alfa dose: 40'000 weekly Hb‐target: 15 g/dL duration: 24 weeks |
|
| Outcomes | primary: Hb secondary: QoL, safety |
|
| Notes | full text publication, was excluded in the IPD Review, study number = 61315 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Unclear risk | unclear |
O'Shaughnessy 2005.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 100, randomised: ESA = 51, control = 49 disease: breast cancer, stages I‐IIIB treatment: chemotherapy baseline Hb: 12.9 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 40,000 IU qw sc Hb‐target: 13‐15 g/dL duration: 12 weeks |
|
| Outcomes | primary: cognitive function, fatigue secondary: QoL |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 40730) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer generated |
| Allocation concealment (selection bias) | Low risk | yes ‐ coded drug packs of identical appearance |
O'Shaugnessy 2005 IPD.
| Methods | see O'Shaughnessy 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 40730 | |
OBE/EPO‐INT‐03 IPD.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 72, randomised: ESA = 35, control = 37 disease: MM treatment: chemotherapy, assumed to be without platinum because of hematological disease baseline Hb: not reported, unclear |
|
| Interventions | drug: Epoetin alpha dose: 40'000 IU sc weekly Hb‐target: 12‐13 g/dL duration: during chemotherapy |
|
| Outcomes | primary: Hb change secondary: QoL, Hb response, transfusion, safety |
|
| Notes | unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 92503) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Oberhoff 1998.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 218, randomised: ESA = 114, control = 104 disease: ovarian, breast, lung, genitourinary, gastrointestinal, other cancer treatment: platinum containing chemotherapy baseline Hb: ESA arm 9.6 g/dL, control 10.3 g/dL, categorised as < 10 g/dL |
|
| Interventions | drug: Epoetin beta dose: 5000U daily s.c. Hb‐target: 14 g/dL duration: 12 weeks |
|
| Outcomes | primary: transfusion secondary: haematologic response, Hb response, safety |
|
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001) and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 45434) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Oberhoff 1998 IPD.
| Methods | see Oberhoff 1998 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 45434 | |
Osterborg 1996.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 144, randomised: ESA 1 = 47, ESA 2 = 48, control = 49 disease: MM, NHL, chronic lymphocytic lymphoma treatment: chemotherapy, non‐platinum containing baseline Hb: 8.8 g/dL |
|
| Interventions | drug: Epoetin beta dose: a: 10000 IU sc 7x/week, b: 2.000U daily s.c.; increased to 5.000U and 10.000U daily if no response Hb‐target: 12‐13 g/dL (women), 13‐14 g/dL (men) duration: 24 weeks |
|
| Outcomes | primary: transfusion secondary: safety, Hb, haematologic response |
|
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001) and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 43680) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Osterborg 1996 IPD.
| Methods | see Osterborg 1996 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 43680 | |
Osterborg 1996a.
| Methods | see Osterborg 1996 | |
| Participants | ||
| Interventions | dose a: 10'000 daily sc | |
| Outcomes | ||
| Notes | ||
Osterborg 1996b.
| Methods | see Osterborg 1996 | |
| Participants | ||
| Interventions | dose b: 2.000U daily s.c.; increased to 5.000U and 10.000U daily if no response | |
| Outcomes | ||
| Notes | ||
Osterborg 2002.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 349, randomised: ESA = 173, control = 176 disease: MM, NHL, CLL; treatment: chemotherapy, assumed without platinum because of hematological disease baseline Hb: 9.3 10g/dL |
|
| Interventions | drug: Epoetin beta dose: 150U/kg 3x/week s.c. Hb‐target = 13‐14 g/dL duration: 16 weeks |
|
| Outcomes | primary: transfusion free survival secondary: haematologic response, Hb change, time to response, number of blood transfusions, QoL, safety |
|
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 77914) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ randomisation program |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Osterborg 2002 IPD.
| Methods | see Osterborg 2002 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 77914 | |
Overgaard 2009.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 515, randomised: ESA = 255, control = 260 disease: head and neck cancer treatment: radiotherapy baseline Hb: approximately 13 g/dL |
|
| Interventions | drug: darbepoetin dose: 150 mg sc weekly Hb target: > 15.5 g/dL duration: 8 to 10 weeks |
|
| Outcomes | OS, DS, tumour control, adverse events | |
| Notes | abstract publication, study number = 62913 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not reported |
| Allocation concealment (selection bias) | Low risk | central allocation method |
P‐174 IPD.
| Methods | see P‐174 J&J 2004 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
P‐174 J&J 2004.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 45, randomised: ESA = 33, control = 12 disease: CLL (any stage) treatment: NR 'other' baseline Hb category: not reported, unclear |
|
| Interventions | drug: Epoetin alpha dose: 150 IU/kg tiw sc Hct‐target: 38% to 40% duration 12 weeks |
|
| Outcomes | primary: Hct secondary: Hb, transfusion, QoL, safety |
|
| Notes | data presented by J&J at FDA/ODAC hearing in May 2004, additional unpublished data were obtained for an individual patient data meta‐analysis (Bohlius et al, 2009 study number = 60584) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ no description |
Pirker 2008.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 600, randomised: ESA = 299, control = 301 disease: SCLC (untreated, extensive stage) treatment: platinum‐containing chemotherapy baseline Hb: 11.9 g/dL, ESA arm 12.03 g/dL, control 11.86 g/dL, categorised as 10‐12 g/dL |
|
| Interventions | drug: Darbepoetin alpha dose: 300 µg sc weekly for weeks 1‐4 then 300 µg Q3W starting week 5 onwards Hb‐target: 13‐14 g/dL duration: 19 weeks |
|
| Outcomes | primary: Hb change, survival secondary: QoL, progression‐free‐survival, tumour response, time to progression, transfusion |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 89335) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Pirker 2008 IPD.
| Methods | see Pirker 2008 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Pronzato 2010.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 223, randomised ESA=110, control =113 disease: breast cancer (stage I‐IV) treatment: chemotherapy baseline Hb: 10.7 g/dL |
|
| Interventions | drug: epoetin alpha dose: if body weight >45kg 10,000 IU sc TIW, if body weight <45kg 5,000 IU sc TIW Hb target: 12‐14 g/dL duration: categorized: >20 weeks |
|
| Outcomes | Primary: QoL (anaemia) Secondary: hematological response, other QoL, tumour response, OS, number of patients transfuse |
|
| Notes | Full‐text publication, unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 22233) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Pronzato 2010 IPD.
| Methods | see Pronzato 2010 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Quirt 1996.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 56, randomised: ESA = 28, control = 28 disease: lung, gynaecological, hematological malignancies, other cancer treatment: chemotherapy baseline Hb: 10.8 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150U/kg 3x/week s.c Hb‐target: 12.5‐14 g/dL duration: 16 weeks |
|
| Outcomes | primary: transfusion, Hb change secondary: QoL, costs from societal perspective, tumour response |
|
| Notes | abstract publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 80214) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ no description |
Quirt 1996 IPD.
| Methods | see Quirt 1996 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 80214 | |
Ray‐Coquard 2009.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 218, randomised: ESA = 110, control = 108 disease: breast, sarcoma, lung, ovarian, other solid cancer and hematological malignancies treatment: chemotherapy (IPD) full text: NR baseline Hb: 10.0 g/dL, categorised as 10‐12 g/dL |
|
| Interventions | drug: Epoetin alpha dose: if body weight < 45 kg 10000 IU sc 2x/week, if body weight 45 kg to < 89 kg 10000 IU sc TIW, if body weight > 89 kg 10000 IU sc 4x/week Hb‐target: 12‐14 g/dL planned ESA duration: 12 weeks |
|
| Outcomes | primary: transfusion dependent anaemia secondary: QoL, Hb response predictors, Hb, toxicity, survival, costs |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 37491) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes |
| Allocation concealment (selection bias) | Low risk | yes |
Ray‐Coquard 2009 IPD.
| Methods | see Ray‐Coquard 2009 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | abstract publication, IPD data | |
Razzouk 2004.
| Methods | see Razzouk 2006 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Razzouk 2006.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 224, randomised ESA: 112, Control: 112 disease: solid tumours, HD, NHL, ALL treatment: chemotherapy baseline Hb: 9.7 g/dL |
|
| Interventions | drug: epoetin alpha dose: 600 IU/kg iv weekly Hb target: 13‐15 g/dL (age >12 years), 13‐14 g/dL (age<12 years) duration: 16 weeks |
|
| Outcomes | primary: QoL secondary: Hb, transfusion |
|
| Notes | Full‐text publication, additional unpublished data were obtained for an Individual Patient Data meta‐analysis study (Bohlius et al 2009). Study number: 80515 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes‐ computer generated |
| Allocation concealment (selection bias) | Low risk | yes‐ central randomisation and coded drug packages of identical appearance |
Rose 1994.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 221, ESA = 142, control = 79 disease: CLL (stage III, IV) treatment: chemo‐ and radiotherapy, without platinum baseline Hb: 9.2 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150U/kg 3x/week s.c. Hb target: Hct 38%‐40% duration: 12 weeks |
|
| Outcomes | primary: Hct, haematologic response secondary: transfusion, safety, QoL |
|
| Notes | Abstract publication, additional unpublished data were obtained for the this Cochrane review and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 98358) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ no description |
Rose 1994 IPD.
| Methods | see Rose 1994 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 98358 | |
Rose 1994 J&J 2004.
| Methods | see Rose 1994 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | Data presented by J&J at FDA/ODAC hearing in May 2004 | |
Rosen 2003.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 90, randomised: ESA = 47, control = 43 disease: head and neck cancer treatment: radiation therapy and non platinum‐containing chemotherapy baseline Hb: 12.2 g/dL at baseline |
|
| Interventions | drug: Epo dose: 40'000 IU per week Hb‐target: NR duration: 14 weeks |
|
| Outcomes | primary: response rate, toxicity, disease free and overall survival secondary: response to Epo treatment |
|
| Notes | full text publication, was excluded in the IPD review: n = 90, study number = 72003 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Unclear risk | unclear |
Rosenzweig 2004.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 27, randomised: ESA = 14, control = 13 disease: metastatic breast cancer treatment: less than 50% of participants received chemotherapy, some received hormones, categorised as other baseline Hb: not reported, eligibility criterion Hb < 12 g/dL, categorised as Hb 10‐12 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 40,000 IU qw sc Hb target: NR duration: 12 weeks |
|
| Outcomes | primary: fatigue, QoL | |
| Notes | full text publication, study number = 76065 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Low risk | Yes ‐ using sequential, opaque, sealed envelopes with the order unknown to the investigators |
Savonije 2005.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 315, randomised: ESA = 211, control = 104 disease: NSCLC, gastrointestinal, gynaecological, colorectal, SCLC, other cancer treatment: platinum based chemotherapy baseline Hb: 10.7 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 10'000 IU sc TIW sc Hb‐target: 13‐14 g/dL duration: 14 weeks |
|
| Outcomes | primary: transfusion secondary: Hb, tumour response, QoL, survival |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 70724) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ randomisation centre generates a list of subject numbers and randomly allocate numbers to the two treatment groups using a block size of six |
| Allocation concealment (selection bias) | Low risk | Yes ‐ central randomisation |
Savonije 2005 IPD.
| Methods | see Savonije 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 70724 | |
Silvestris 1995.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 54, randomised: ESA = 30, control = 24 disease: MM treatment: chemotherapy without platinum baseline Hb: <=8 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150U/kg 3x/week s.c. Hb target: no target defined duration: 24 weeks |
|
| Outcomes | haematologic response, adverse events | |
| Notes | full text publication, study number = 76441 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Unclear risk | unclear |
Smith 2003.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 86, randomised: ESA = 64, control = 22 disease: genitourinary, breast, gastrointestinal, lymphoma: myeloma, CLL, NHL treatment: none baseline Hb: 9.995; <10 g/dL for two groups and 10‐12 g/dL for the other two, categorized as <10 g/dL |
|
| Interventions | drug: Darbepoetin alpha dose: see below Hb target: 13‐14 g/L (women), 13‐15 (men) g/dL duration: 12 weeks |
|
| Outcomes | primary: haematopoietic response secondary: time to response, Hb response, Hb change, transfusions, serum darbepoetin conc. in a subset of patients |
|
| Notes | full text publication, study number = 76561 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Unclear risk | unclear |
Smith 2003 Amgen 2007.
| Methods | see Smith 2003 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Smith 2003a.
| Methods | See Smith 2003 | |
| Participants | ||
| Interventions | dose a: 6.75 µg/kg Q3W sc | |
| Outcomes | ||
| Notes | ||
Smith 2003b.
| Methods | See Smith 2003 | |
| Participants | ||
| Interventions | dose b: 6.75 µg/kg Q4W sc | |
| Outcomes | ||
| Notes | ||
Smith 2003c.
| Methods | See Smith 2003 | |
| Participants | ||
| Interventions | dose c: 10 µg/kg Q4W sc | |
| Outcomes | ||
| Notes | ||
Smith 2008.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 989, randomised: ESA = 517, control = 472 disease: lung, hematological malignancies, breast, gastrointestinal, genitourinary, other cancer (stage III‐IV) treatment: none baseline Hb: 9.5 g/dL |
|
| Interventions | drug: Darbepoetin alpha dose: 6.75 µg/kg sc Q4W Hb‐target: 12‐13 g/dL duration: 16 weeks |
|
| Outcomes | primary: transfusion secondary: Hb, QoL, safety |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 81215) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Low risk | Yes, adequate |
Smith 2008 IPD.
| Methods | see Smith 2008 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Strauss 2008.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | n = 74, randomised: ESA = 34, control = 40 disease: cervical cancer (stage IIB‐IVA) treatment: radio‐ and platinum‐containing chemotherapy baseline Hb: 11.5 g/dL |
|
| Interventions | drug: Epoetin beta dose: 150 IU/kg sc TIW Hb‐target: 14‐15 g/dL duration: 12 weeks |
|
| Outcomes | primary: tumour control failures secondary: progression‐free survival, overall response rate, relapses/metastases, overall survival, Hb change, QoL, safety |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 70404) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ patient randomisation number were generated without reporting the method |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ patient randomisation numbers were to be allocated sequentially in the order in which the patients are enrolled |
Strauss 2008 IPD.
| Methods | see Strauss 2008 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Suzuki 2008.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N=123: ESA: 81, control=42 disease: lymphoma, breast cancer treatment: chemotherapy baseline Hb: not reported, eligibility criterion Hb <= 11 g/dL, after amendment <= 10 g/dL, categorized as Hb 10‐12 g/dL |
|
| Interventions | drug: darbepoetin alpha dose: a) 4.5 ug/kg sc Q3W or b) 6.75 ug/kg sc Q3W Hb target: <=13.0 g/dL, amended to <=12.0 g/dL duration: 12 weeks |
|
| Outcomes | Hb response, safety, QoL, survival | |
| Notes | abstract publication, study id: 14688 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear, not reported |
| Allocation concealment (selection bias) | Unclear risk | unclear, not reported |
Suzuki 2008a.
| Methods | see Suzuki 2008 | |
| Participants | darbepoetin: 40, placebo: 42 | |
| Interventions | darbepoetin 4.5 ug/kg sc Q3W vs placebo | |
| Outcomes | ||
| Notes | ||
Suzuki 2008b.
| Methods | see Suzuki 2008 | |
| Participants | darbepoetin: 41, placebo: 42 | |
| Interventions | darbepoetin 6.75 ug/kg sc Q3W vs placebo | |
| Outcomes | ||
| Notes | ||
Sweeney 1998.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 48, randomised: ESA = 24, control = 24 disease: breast, lung, prostate and cervix cancer treatment: chemotherapy for 5 patients, radiotherapy for probably all of the patients baseline Hb: ESA arm 12.07, control: 10.72 g/dL, categorized as 10‐12 g/dL |
|
| Interventions | drug: Epoetin alfa dose: 200 IU/kg/d Hb target: 14 g/dL for women and 15 g/dL for men duration: 7 weeks |
|
| Outcomes | Hb, total white blood cell count and platelets, QoL | |
| Notes | full text publication, excluded for IPD‐Review, study number = 77932 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated random numbers in blocks of 10 |
| Allocation concealment (selection bias) | Unclear risk | not reported, unclear |
Ten Bokkel 1998.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 122, randomised: ESA = 88, control = 34 disease: ovarian carcinoma (stage II‐IV) treatment: platinum‐based chemotherapy baseline Hb: 11.6 g/dL |
|
| Interventions | drug: Epoetin beta dose: a: 150 IU/kg sc TIW, b: 300 IU/kg sc TIW Hb‐target: 14‐15 g/dL duration = during chemotherapy, 24 weeks |
|
| Outcomes | primary: transfusion secondary: Hb, reticulocytes, Hct, safety, tumour response, adverse events |
|
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001) and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 47852) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Ten Bokkel 1998a.
| Methods | see Ten Bokkel 1998 | |
| Participants | Epoetin a: N = 45 | |
| Interventions | dose a: 150U/kg 3x/week s.c. | |
| Outcomes | ||
| Notes | ||
Ten Bokkel 1998b.
| Methods | see Ten Bokkel 1998 | |
| Participants | Epoetin 2: N = 42 | |
| Interventions | dose b: 300U/kg 3x/week s.c. | |
| Outcomes | ||
| Notes | ||
Ten Bokkel1998 IPD.
| Methods | see Ten Bokkel 1998 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 47852 | |
Thatcher 1999.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 130, randomised: ESA = 86, control = 44 disease: SCLC treatment: platinum based chemotherapy baseline Hb: 13.4 g/dL |
|
| Interventions | drug: Epoetin alpha dose: ESA a: 150 IU/kg sc TIW; ESAb: 300 IU/kg sc TIW Hb‐target: 13‐15 g/dL duration: 26 weeks |
|
| Outcomes | change in Hb values, transfusion requirement, QoL, adverse events | |
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001) and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 65529) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ upon study entry each patient was assigned a sequential identification number which had been randomly assigned to chemotherapy with or without ESA, blocks of 6, each investigator had to treat at least 6 patients, but preferably 12 patients. |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ see randomisation |
Thatcher 1999 IPD.
| Methods | see Thatcher 1999 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 65529 | |
Thatcher 1999a.
| Methods | See Thatcher 1999 | |
| Participants | Epoetin a: n = 42 | |
| Interventions | Epoetin alpha a: 150U/kg 3x/week s.c. | |
| Outcomes | ||
| Notes | ||
Thatcher 1999b.
| Methods | See Thatcher 1999 | |
| Participants | Epoetin b: N = 44 | |
| Interventions | Epoetin alpha b: 300U/kg 3x/week s.c. | |
| Outcomes | ||
| Notes | ||
Thomas 2002.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 130, randomised: ESA = 65, control = 65 disease: breast, gastrointestinal, gynaecological, other cancer treatment: chemotherapy baseline Hb: 10.6 g/dL |
|
| Interventions | drug: Epoetin alpha dose: if body weight > 45 kg 10000 IU sc TIW, if body weight < 45 kg 5000 IU sc TIW Hb‐target: 12‐14 g/dL duration: 12 weeks |
|
| Outcomes | Hb, QoL, transfusions | |
| Notes | abstract publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 84090) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Thomas 2002 IPD.
| Methods | see Thomas 2002 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 84090 | |
Thomas 2008.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 114 (from IPD), full‐text: accrued: 114, 5 found subsequently not eligible randomised: ESA = 57, control = 52; planned were 460, vs IPD, vs 2006 disease: cervical cancer (stage IIB ‐ IV A, M0) treatment: platinum‐based chemotherapy plus radiotherapy baseline Hb: 10.7 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 40000 IU sc weekly Hb‐target: 13‐14 g/dL duration: 8 weeks max, categorised as 6‐9 weeks |
|
| Outcomes | primary: progression‐free survival secondary: OS, local control, distant recurrences, thromboembolic events |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 21481) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description "eligible patients were randomised..." |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Thomas 2008 IPD.
| Methods | see Thomas 2008 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Thomas 2008 J&J 2004.
| Methods | see Thomas 2008 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Thompson 2000.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 66, randomised: ESA = 45, control = 21 disease: Myelodysplastic Syndromes treatment: no chemotherapy, GM‐CSF 0.3‐5.0 mg/kg daily in both groups mean/median baseline Hb: 9 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 150U/kg 3x/week s.c. + Hb target: 12 ‐ 13 g/dL duration: 12 weeks |
|
| Outcomes | haematologic response, change in Hb values, transfusion requirement, adverse events | |
| Notes | full text publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001), study number = 82687 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Yes ‐ computer random‐number generator |
| Allocation concealment (selection bias) | Low risk | Yes ‐ adequate |
Throuvalas 2000.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 55, randomised: ESA = 28, control = 27 disease: cervix and bladder carcinoma treatment: platinum‐based radiochemotherapy baseline Hb: 11.3 g/dL |
|
| Interventions | drug: Epoetin (?) dose: 10,000U 5x/week s.c. Hb target: NR duration: 6 weeks |
|
| Outcomes | change in Hb values, transfusion requirement, tumour response | |
| Notes | abstract publication, additional unpublished data were obtained for the first Cochrane review (1985‐2001), study number = 83700 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ random‐number generator |
| Allocation concealment (selection bias) | Low risk | yes ‐ central allocation |
Tjulandin 2010.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 223, randomised: Epo theta = 76, Epo beta = 73, control = 74 disease: ovarian cancer, gastric cancer, breast cancer, lung cancer. other solid cancers treatment: platinum‐based chemotherapy baseline Hb: 9.5 g/dL |
|
| Interventions | drug a): Epoetin theta, dose: 20'000 IU weekly drug b): Epoetin beta, dose: 150 IU/kg sc TIW Hb‐target: 13 g/dL duration: 12 weeks |
|
| Outcomes | primary: haematological response secondary: partial Hb response, RBCTs, number of bloods units transfused, safety, QoL |
|
| Notes | full‐text publication, study number = 19632 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated allocation schedule |
| Allocation concealment (selection bias) | Unclear risk | not reported |
Tjulandin 2010a.
| Methods | see Tjulandin 2010 | |
| Participants | ||
| Interventions | Epoetin theta, dose: 20'000 IU weekly | |
| Outcomes | ||
| Notes | ||
Tjulandin 2010b.
| Methods | see Tjulandin 2010 | |
| Participants | ||
| Interventions | Epoetin beta, dose: 150 IU/kg sc TIW | |
| Outcomes | ||
| Notes | ||
Tjulandin 2011.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 186, randomised: ESA = 95, control = 91 disease: hematological, breast and gastric cancer treatment: chemotherapy without platinum baseline Hb: 9.2 g/dL |
|
| Interventions | drug: Epoetin theta dose: 20'000 IU weekly Hb‐target: 13 g/dL duration: 12 weeks |
|
| Outcomes | primary: haematological response secondary: partial Hb response, RBCTs, number of bloods units transfused, safety, QoL |
|
| Notes | full‐text publication, study number = 18036 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | not reported |
Tsuboi 2009.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 122, randomised: ESA = 63, control = 59 disease: lung cancer, malignant lymphoma (HL and NHL) treatment: chemotherapy, both platinum and non‐platinum containing, no numbers given. baseline Hb: 10.2 g/dL |
|
| Interventions | drug: Epoetin beta dose: 36'000 IU sc weekly Hb target: >= 14 g/dL duration: 8 weeks |
|
| Outcomes | primary: Hb change secondary: hematological response, transfusions, Hb, QoL, (survival, cave: retrospective) |
|
| Notes | full text publication, abstract Watanabe 2006 was excluded for the IPD‐Review, study number = 92759 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation system |
Untch 2008 IPD.
| Methods | see Untch 2011_1 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Untch 2011_1.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 733, randomised: ESA = 356, control = 377 disease: breast cancer (M0) treatment: non platinum‐containing chemotherapy baseline Hb: 13.6 g/dL |
|
| Interventions | drug: Darbepoetin alpha dose: 4.5 µg/kg sc Q2W Hb‐target: 12.5‐13 g/dL duration: during chemotherapy, approximately > 20 weeks |
|
| Outcomes | primary: relapse free survival time, OS secondary: tumour control, safety and tolerability, transfusion, Hb level, QoL |
|
| Notes | two full text publications, in addition unpublished data were obtained for the individual patient data meta‐analysis study (Bohlius et al 2009, study number = 66960) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ no description |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ description is unclear |
Untch 2011_2.
| Methods | see Untch 2011_1 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Vansteenkiste 02 FDA 2004.
| Methods | see Vansteenkiste 2002 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Vansteenkiste 2002.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 320, randomised: ESA = 159, control = 161 disease: SCLC (limited and extensive), and NSCLC (stage I‐IV) treatment: platinum based chemotherapy baseline Hb: 10.1 g/dL |
|
| Interventions | drug: Darbepoetin alpha dose: 2.25 mg/kg sc weekly Hb‐target: 13‐14 g/dL (women), 13‐15 g/dL (men) duration: 12 weeks |
|
| Outcomes | primary: transfusion secondary: Hb response, Hb, transfusion timing and quantity, QoL |
|
| Notes | full text publication, additional unpublished data were obtained for and an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 49684) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ based on a schedule specified by Amgen before the start of the study |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Vansteenkiste 2002 IPD.
| Methods | see Vansteenkiste 2002 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | study number = 49684 | |
Welch 1995.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 30, randomised: ESA = 15, control = 15 disease: ovarian carcinoma treatment: platinum‐containing chemotherapy mean/median baseline Hb: 12.9 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 300U/kg 3x/week s.c. Hb ‐ target: 12‐15 g/dL duration: 24 weeks |
|
| Outcomes | change in Hb values, transfusion requirement, adverse events | |
| Notes | full text publication, study number = 97952 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear |
| Allocation concealment (selection bias) | Unclear risk | unclear |
Wilkinson 2006.
| Methods | randomised controlled trial, not placebo‐controlled | |
| Participants | N = 182, randomised: ESA = 121; control = 61 disease: ovarian cancer (stage I‐IV) treatment: chemotherapy baseline Hb: 10.7 g/dL |
|
| Interventions | drug: Epoetin alpha dose: if body weight > 45 kg 10000 IU sc TIW, if < 45 kg 5000 IU sc TIW Hb‐target: 12‐14 g/dL duration: max. 28 weeks |
|
| Outcomes | primary: Hb response secondary: QoL, transfusion, tumour response |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 75688) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | unclear ‐ a prospective randomisation procedure will be employed |
| Allocation concealment (selection bias) | Unclear risk | unclear ‐ assigned envelopes, but it is unclear whether they were opaque and sequentially numbered |
Wilkinson 2006 IPD.
| Methods | seeWilkinson 2006 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Winquist 2009.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 56, randomised ESA: 26, control = 30 disease: prostate cancer treatment: unclear Baseline Hb: 10.4 g/dL |
|
| Interventions | drug: epoetin alpha dose: 40,000 IU sc 3 times /week Hb target: 14.0 g/dL duration: 16 weeks |
|
| Outcomes | primary: QoL secondary: Hb level, RBCTs, adverse events, survival |
|
| Notes | letter publication, study number 13321 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not reported, unclear |
| Allocation concealment (selection bias) | Low risk | central telephone |
Witzig 2005.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 344, randomised: ESA = 174, control = 170 disease: lung, breast, other cancer (active incurable advanced stage) treatment: chemotherapy, platinum & non platinum Hb category: 9.5 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 40000 IU sc weekly Hb‐target: 13‐15 g/dL planned ESA duration: 16 weeks |
|
| Outcomes | primary: transfusions secondary: Hb change, Hb over time, predictors for response, incidence of nephrotoxicity, OS, tumour response, QoL |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 36512) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer‐generated |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation and coded drug packs of identical appearance |
Witzig 2005 IPD.
| Methods | see Witzig 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Witzig 2005 J&J 2004.
| Methods | see Witzig 2005 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | Data presented by J&J at FDA/ODAC hearing in May 2004 | |
Wright 2007.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 70, randomised: ESA = 33, control = 37 disease: NSCLC (advanced stage IIIA, B and IV, recurrent disease) treatment: no anticancer therapy baseline Hb: 10.3 g/dL |
|
| Interventions | drug: Epoetin alpha dose: 40'000 IU sc weekly Hb‐target: 12‐14 g/dL duration = 12 weeks |
|
| Outcomes | primary: QoL secondary: Hb, Hct, transfusion, safety |
|
| Notes | full text publication, additional unpublished data were obtained for an individual patient data meta‐analysis study (Bohlius et al 2009, study number = 53572) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | yes ‐ computer‐generated |
| Allocation concealment (selection bias) | Low risk | yes ‐ central randomisation |
Wright 2007 IPD.
| Methods | see Wright 2007 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Wurnig 1996.
| Methods | randomised controlled trial, placebo‐controlled | |
| Participants | N = 30, randomised: ESA = 16, control = 14 disease: Ewing's or osteosarcoma treatment: chemotherapy, some platinum‐based mean/median baseline Hb: 10.8 g/dL |
|
| Interventions | drug: Epoetin beta dose: 600U/kg 2x/week i.v. Hb‐target: 11‐13.5 g/dL duration: 20 weeks |
|
| Outcomes | change in Hb values, transfusion requirement, adverse events | |
| Notes | full text publication, no IPD data, study number = 97958 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Yes ‐ computer‐generated randomisation code |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
CLL: Chronic lymphatic leukaemia D: day ESA: erythropoiesis stimulating agent FDA: Food and Drug Administration, USA G‐CSF: Granulocyte colony‐stimulating factor Hb: Haemoglobin Hct: haematocrit HD: Hodgkin's Disease IPD: individual patient data i.v.: intravenous J&J: Johnson & Johnson Pharmaceuticals Ltd. MM: multiple myeloma NHL: non‐Hodgkin's lymphoma NSCLC: non‐small cell lung cancer NR: not reported ODAC: Oncology Drug Advisory Committee OS: overall survival QoL: Quality of Life qw: once per week Q3W: once every three weeks Q4W: once every four weeks RBC: red blood cell s.c.: subcutaneous SCLC: small cell lung cancer tiw: three times per week TR: Tumour response wk: week wks: weeks
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aagaard 2010 | nrct |
| Aapro 2009 | nrct |
| Abdelrazik 2007 | ineligible patient characteristics: ALL |
| Abraham 2011 | nrct |
| Adamson 2009 | no RCT |
| Alexopoulos 2004 | randomised comparison of epoetin alfa 10,000 IU tiw versus darbepoetin alfa 150 mcg qw, n = 50 |
| Anonymous 2007 | no RCT |
| Anthony 2011 | all arms ESAs |
| Arcasoy 2010 | nrct |
| Arslan 2004 | randomised comparison of different usage strategies |
| Auerbach 2004 | randomised comparison of different iron applications |
| Australian 2010 | nrct |
| Aziz 2001 | treatment allocation not concealed IPD: too small for inclusion |
| Barosi 1998 | nrct |
| Barosi 2011 | nrct |
| Beggs 2003 | randomised comparison of 40,000 IU epoetin alfa versus placebo, study too small for inclusion: n = 21 |
| Bell 2008 | no RCT |
| Bessho 1997 | ineligible patient characteristics: only patients with aplastic anaemia included, N = 131 |
| Bindi 2004 | unclear whether this a randomised controlled trial, authors have been unsuccesfully contacted IPD: too small for inclusion |
| Blayney 2003 | study stated to be randomised, experimental arms received darbepoetin alfa, treatment in the control group not documented, authors were contacted for clarification without success, n = 1173 |
| Boccia 2007 | no RCT |
| Borg 2008 | no RCT |
| Borget 2008 | no RCT |
| Bowen 2004 | G‐CSF only in one arm |
| Brower 2008 | nrct |
| Buchler 2011 | nrct |
| Buyukpamukcu 2002 | follow‐up study to Varan 1999, does not satisfy allocation concealment requirement |
| Cabanillas 2012 | acute leukaemia |
| Candelaria 2005 | no ESA was given |
| Canon 2006 | compared different ESA dosages |
| Canon 2011 | retrospective analysis of dose‐fidning study |
| Caravita 2009 | nrct |
| Casadevall 2004 | randomised controlled study in patients with MDS, comparing erythropoietin PLUS G‐CSF versus supportive care without erythropoietin and without G‐CSF |
| Cazzola 2003 | randomised comparison of once weekly 30,000 IU epoetin beta versus three times weekly 10,000 IU epoetin beta |
| Chan 1995 | very small trial, only 10 evaluable patients per study arm |
| Cheng 2009 | yixuesheng capsule with ESA vs ESA alone |
| Christodoulakis 2005 | ESAs were given in context with surgery |
| Coiffier 2006 | nrct |
| Coleman 2009 | not randomised for epo |
| Crawford 1997 | randomised‐controlled trial, placebo controlled, double‐blind, included 25 patients with SCLC, as no sufficient data were available the study was excluded |
| Crawford 2003 | randomised comparison of epootin alfa 40,000 IU per week versus control; patients in the control group received epoetin alfa when the Hb level decreased below 10g/dL, n = 216 |
| Crawford 2007 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Cremieux 2003 | nrct |
| Dahl 2008 | nrct |
| Daneryd 1998 | epoetin only given to the anaemic patients in the treatment arm |
| Dannemann 2004 | compared different ESA dosages |
| Demetri 1998 | community based, non randomised study including 2,370 patients with nonmyeloid malignancies |
| Dicato 2011 | nrct |
| Dronca 2008 | nrct |
| Dusenbery 1994 | mixed concurrent and historical controls |
| Elsaid 2001 | n too small |
| Fagnoni 2005 | retrospective study design |
| Ferrero 2009 | no RCT |
| Franchi 2008 | no RCT, dose comparing |
| Freeman 2006 | too small for inclusion, n = 14 |
| Fujisaka 2004 | single arm study, no RCT |
| Gabrilove 2001 | community based, nonrandomised study including 3,012 participants with nonmyeloid malignancies |
| Garton 1995 | very small trial, only 10 evaluable patrticipants per study arm |
| Gascon 2008 | nrct |
| Gebbia 1992 | n = 19, too small for inclusion |
| Glaser 1999 | no RCT, 37 participants with advanced oral squamous carcinoma receiving neoadjuvant radiochemotherapy |
| Glaser 2001 | no RCT, 191 patients with advanced oral squamous carcinoma receiving neoadjuvant radiochemotherapy |
| Glaspy 1997 | community study |
| Glaspy 2001 | dose finding study, not randomised |
| Glaspy 2002 | darbepoetin versus erythropoietin, related to Glaspy 2002b |
| Glaspy 2002b | darbepoetin versus erythropoietin, related to Glaspy 2002 |
| Glaspy 2003 | darbepoetin versus erythropoietin |
| Glaspy 2005 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Glaspy 2006 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Glaspy 2011 | nrct |
| Glimelius 1998 | randomised study with two different EPO groups: 2.000 U sc three times per week versus 10.000 U sc tree times per week |
| Glossmann 2003 | randomised controlled comparison in patietns with relapsed lymphoma undergoing stem‐cell supported high‐dose therapy with or without erythropoietin |
| Goldsmith 2011 | nrct |
| Granetto 2003 | randomised comparison of fixed versus weight‐based dosing of epoetin alfa |
| Gregory 2005 | nrct |
| Grigorescu 2006 | probably not randomised |
| Hadland 2009 | nrct |
| Han 2008 | randomised trial of amifostine vs epo |
| Harousseau 2005 | nrct |
| Hellström‐Lindberg 1998 | G‐CSF supplementation only in the control arm |
| Hellstörm‐Lindberg 2010 | nrct |
| Henry 2004 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Henry 2006 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Henry 2007 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Henze 2002 | surgery |
| Hesketh 2004 | comparison of different darbepo dosages |
| Hirsh 2007 | CERA |
| Huggett 2011 | not relevant (listed as "other reasons" in prisma") |
| Hyer 2011 | nrct |
| Itzykson 2009 | case report, no RCT |
| Jacubowski 2003 | comparisons of epo versus darbepo, ongoing |
| Jadersten 2008 | nrct |
| Jitnuyanont 2001 | randomised comparison of erythropoietin versus control in 24 anaemic cancer patients, study was split into three arms with 10 and less patients per study arm |
| Johansson 2001 | randomised comparison of epeotin beta 1,000 IU versus 5,000 IU three times per week |
| Jones 2011 | nrct |
| Juan 2006 | no RCT |
| Justice 2005 | compared different ESA products (sc vs iv) |
| Kara 2008 | nrct |
| Katodritou 2008 | nrct |
| Katodritou 2009 | nrct |
| Kettelhack 1998 | ESAs were given in context with surgery |
| Kim 2010 | no cancer |
| Kosmadakis 2003 | ESAs were given in context with surgery |
| Kotasek 2004 | compared different ESA dosages |
| Kotasek 2007 | compared different ESA dosages |
| Larsson 2008 | n = 18, too small for inclusion |
| Lastiri 2002 | nrct |
| Latagliata 2008 | nrct |
| Lavey 1993 | nrct |
| Lavey 2004 | nrct |
| Leitgeb 1994 | nrct |
| Leon 1998 | historical control group |
| Lichtin 2008 | nrct |
| Loibl 2006 | all patients received ESAs |
| Ludwig 1995 | nrct |
| Malik 1998 | nrct, N = 23 |
| Mangiameli 2002 | randomised controlled study with 5 patients per study arm |
| Mantovani 2000 | nrct |
| Marinaccio 2003 | randomised comparison of epoetin alfa versus control for patients with ovarian cancer undergoing surgery and chemotherapy, epoetin was administered BEFORE surgery, n = 22 |
| Markman 1993 | comparison of two non‐randomised trials |
| Mel 2008 | nrct |
| Merchionne 2009 | nrct |
| Merlano 2001 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| MF4266 | ineligible patient characteristics AML |
| Miller 2004 | unclear wether this is a randomised trial |
| Morishima 2006 | compared different ESA dosages |
| Morrow 2007 | nrct |
| Muravyov 2009 | single arm study without control group |
| Muravyov 2010 | nrct |
| Mustacchi 2006 | nrct |
| Nagel 2011 | too many patients in experimental arm did not receive ESAs |
| NCT00364845 2011 | no cancer |
| Nonoguchi 2009 | nrct |
| Oberhoff 2005 | nrct |
| Olsson 2002 | randomised comparison of epeotin beta 1,000 IU versus 5,000 IU three times per week |
| Opie 2011 | nrct |
| Ots 2008 | epoetin vs darbepoetin |
| Pat 2009 | nrct |
| Pierelli 1999 | randomised‐controlled trial, unblinded, not placebo controlled, 50 participants with ovarian carcinoma were included, as no sufficient data were available, the study was excluded |
| Poirier 2010 | nrct |
| Policarpo 2007 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Popescu 2010 | nrct |
| Porter 1996 | too small for inclusion |
| Puglisi 2009 | subgroup analysis |
| Rades 2009 | nrct |
| Rath 2010 | nrct |
| Rau 1998 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Rearden 2004 | randomised comparison of darbepoetin early and late initiating of treatment |
| Reed 2005 | compared different ESA products (epoetin versus darbepoetin) |
| Ribatti 2009 | nrct |
| Richardson 2011 | nrct |
| Rodgers 2008 | nrct |
| Sakai 2004 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Samper 2002 | randomised comparison of erythropoetin alfa 10,000 IU three times per week versus 30,000 IU once per week |
| Schwartzberg 2004 | darbepo versus epo |
| Schwartzberg 2005 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Schwartzberg 2007 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Scott 2002 | randomised comparison of erythropoietin versus placebo in head and neck cancer patients undergoing surgery |
| Senecal 2005 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Shasha 2003 | community study |
| Shi 2007 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Shord 2009 | nrct |
| Spaeth 2010 | nrct |
| Spicka 2004 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Steensma 2006 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Steensma 2011 | all patients EPO |
| Stein 1991 | very small study, fewer than 10 participants per treatment arm IPD: ineligible patient characteristics (e.g. with MDS or SAA) |
| Steinmetz 2011 | nrct |
| Stokoe 2009 | nrct |
| Stone 2008 | nrct |
| Straus 2002 | upfront epo compared to epo if Hb decreased below 9 g/dL |
| Straus 2006 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Stull 2010 | nrct |
| Suzuki 2008ex | single arm study |
| Tsukuda 1998 | very small study, fewer than 10 participants in the study arms |
| Tzekova 2009 | nrct |
| Uhl 2007 | nrct |
| Vadhan‐Raj 2003 | nrct |
| Vadhan‐Raj 2004 | surgery |
| Varan 1999 | treatment allocation not concealed IPD: too small for inclusion |
| Vekeman 2009 | nrct |
| Velilla Millan 2003 | randomised comparison of epeotin 10,000 IU tiw versus 40,000 IU qw |
| Vorvaud 2007 | nrct |
| Wagner 2004 | no usable data for any outcome |
| Walsh 2010 | nrct |
| Waltzman 2004 | comment to Glaspy 2003 study IPD: Darbepoetin compared to erythropoietin |
| Waltzman 2005 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Wauters 2006 | nrct |
| WHO 2011 | nrct |
| Yang 2008 | nrct |
| Yilmaz 2004 | application of different erythropoietin alfa dosages: 150 IU/kg tiw versus 250 IU/kg tiw in children with cancer |
| Yurut‐Caloglu 2008 | nrct |
| Zagari 2003 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Zaragoza 2004 | n = 17, too small for inclusion |
| Zhang 2003 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
| Zhou 2006 | ESAs were given in context with surgery, stem cell transplantation, compared different ESA dosages or ESA products (epoetin versus darbepoetin), or trials were not randomised |
ALL: acute lymphatic leukaemia AML: acute myeloid leukaemia CERA: continuous erythropoietin receptor activator ESAs: erythropoiesis stimulating agents G‐CSF: granulocyte colony‐stimulating factor Hb: haemoglobin IPD: individual patient data iv: intravenous MDS: myelodysplastic syndrome n: number nrct: not a randomised controlled trial RCT: randomised controlled trial SAA: serum amyloid A SCLC: small cell lung cancer sc: subcutaneous vs: versus
Characteristics of ongoing studies [ordered by study ID]
Blackstock.
| Trial name or title | 1CDR0000069148CCCWFU‐62299; NCI‐P01‐0200; CCCWFU‐BG01‐193 |
| Methods | |
| Participants | Solid ‐ NSCLC Chem + Rad |
| Interventions | Epo, unsure ‐ Epo dose unknown |
| Outcomes | Hb levels, disease progression, tumour response rate, overall survival, QoL, number of RBCT |
| Starting date | January 2002 |
| Contact information | AR Blackstock |
| Notes |
Boehrer 2010.
| Trial name or title | GFMAzaEpo‐2008‐1 trial, NCT01015352 |
| Methods | Randomised phase‐II trial |
| Participants | Lower Risk Myelodysplastic Syndrome (MDS) |
| Interventions | AZA vs AZA+Epoetin beta |
| Outcomes | Major erythroid responses (HI‐E major) after 6 courses, according to IWG 2000 criteria. Secondary endpoints included overall IWG 2000 HI‐E, including major and minor, after 4 and 6 courses, response duration, IPSS progression, survival and toxicity. |
| Starting date | NR |
| Contact information | |
| Notes | http://abstracts.hematologylibrary.org/cgi/content/abstract/ashmtg Unclear whether it should be included or not. |
Broadley.
| Trial name or title | Double‐blind randomised placebo controlled trial of the effect of epoetin alfa on symptomatic anaemia and fatigue in cancer patients receiving ongoing care without planned chemotherapy |
| Methods | |
| Participants | Disease: metastatic breast and prostate cancer; Treatment: none |
| Interventions | Epoetin alfa vs placebo |
| Outcomes | Change in HB values; QoL. |
| Starting date | October 1998 |
| Contact information | Dr K. Broadley Palliative Medicine The Royal Marsden NHS Trust Fulham Road Chelsea London SW3 6JJ UK |
| Notes |
Chapman 2004.
| Trial name or title | NRR 2004 Issue 2 Study ID numbers: N0123138194, REC 01/05/53.C |
| Methods | |
| Participants | Haem ‐ MM, Chemotherapy |
| Interventions | Epo alfa vs standard, epo dose unknown |
| Outcomes | Hb Respnse, QoL (FACT‐An) |
| Starting date | Jan 2002, Finish date: June 05 |
| Contact information | Chapman C |
| Notes |
Delarue 2009.
| Trial name or title | LNH03‐6B GELA Study |
| Methods | Multicentric prospective randomised phase III study |
| Participants | Elderly patients with DLBCL treated by immunochemotherapy |
| Interventions | Darbepoetin vs usual treatment |
| Outcomes | The efficacy of DA in association with chemotherapy (R‐CHOP) as measured by the EFS at 2 years, events being defined as death from any cause, relapse for complete responders and unconfirmed complete responders, progression during or after treatment and changes of therapy during allocated treatment. Secondary objectives were OS, PFS, DFS, response rate and analysis of toxicity. |
| Starting date | NR |
| Contact information | NR |
| Notes | Interim analysis |
EPO CAN 303.
| Trial name or title | EPO‐CAN‐303;NCT00083434R |
| Methods | |
| Participants | Not reported, no concomitant anticancer therapy |
| Interventions | Epo alfa? |
| Outcomes | NR |
| Starting date | NR |
| Contact information | NR |
| Notes |
Famoyin 2004.
| Trial name or title | A randomised phase II study of thalidomide with or without erythropoietin (EPO) in metastatic renal cell carcinoma (RCC) |
| Methods | Randomised phase II study |
| Participants | Metastatic renal cell carcinoma |
| Interventions | Thalidomide with or without EPO |
| Outcomes | Hb, QoL |
| Starting date | |
| Contact information | C. Famoyin, C. Byrnes, S. Roberts, J. Gollob, M. Atkins, J. Mier, Y.‐J. Ko, S. Gautam and D. McDemott Beth Israel Deaconess Medical Center, Boston, MA |
| Notes | Journal of Clinical Oncology, 2004 ASCO Annual Meeting Proceedings (Post‐Meeting Edition). Vol 22, No 14S (July 15 Supplement), 2004: 4747 |
Fisch.
| Trial name or title | CDR0000069409; MDA‐DM‐02331; MDA‐DM‐0038; NCI‐P02‐0225; NCI00052221MJ |
| Methods | |
| Participants | Solid tumours, no concomitant anti‐ malignancy treatment |
| Interventions | Epo alfa vs Placebo |
| Outcomes | Hb response, QoL, Fatigue |
| Starting date | Feb 03 |
| Contact information | Fisch S |
| Notes |
Gallagher.
| Trial name or title | The role of epoetin alpha in anaemia and fatigue in cancer patients |
| Methods | |
| Participants | Disease: ovarian and cervical cancer Treatment: concomitant cisplatin chemotherapy |
| Interventions | Epoetin alpha vs no treatment |
| Outcomes | Changes in HB values; QoL |
| Starting date | September 1998 |
| Contact information | Dr C Gallagher Medical Oncology Department St Bartholomew´s Hospital West Smithfield London EC1A 7BE UK |
| Notes |
Gamucci 1993.
| Trial name or title | Erythropoietin for the prevention of anaemia in neoplastic patients treated with cisplatin |
| Methods | Randomised controlled study |
| Participants | Patients with advanced tumours |
| Interventions | Epoetin alpha versus control |
| Outcomes | Hb, serum epoetin levels |
| Starting date | NR |
| Contact information | T. Gamucci, Department of Medical Oncology, 1, Regina Elena Institute for Cancer Research, Rome, Italy, |
| Notes | Gamucci T, Thorel MF, Frasca AM, Giannarell D, Calabresi F. Erythropoietin for the prevention of anaemia in neoplastic patients treated with cisplatin. Eur J Cancer. 1993;29A Suppl 2:S13‐4. PMID: 8398359 |
Gascon 2010.
| Trial name or title | Amgen 20070782; ClinicalTrials.gov NCT00858364 |
| Methods | Randomized, placebo‐controlled trial |
| Participants | Non‐small cell lung cancer (NSCLC) patients (pts) with anaemia concomitant with chemotherapy (ACC) |
| Interventions | Darbepoetin vs placebo |
| Outcomes | Noninferiority of ESA to placebo for overall survival (primary endpoint) and progression‐free survival (modified RECIST per investigator; secondary endpoint) will be examined when 2700 deaths occur. Other safety endpoints include tumour response and thromboembolic events. Transfusion rates are a key efficacy endpoint; Hb changes will also be reported. |
| Starting date | NR |
| Contact information | NR |
| Notes | No results yet; to follow up |
Ghavamzadeh 2010.
| Trial name or title | NR |
| Methods | Randomized, double blind, placebo‐controlled phase III study |
| Participants | Anaemic patients with lung or gynaecologic cancer receiving platinum‐containing chemotherapy |
| Interventions | Darbepoetin alpha |
| Outcomes | NR |
| Starting date | NR |
| Contact information | NR |
| Notes | Not retrievable from librarians. unclear whether it would be included or not |
H Thomas 1997.
| Trial name or title | Open label comparative evaluation of the effect of epoetin on quality of life and burden of illness in anaemic patients receiving platinum‐containing chemotherapy |
| Methods | |
| Participants | Disease: cancer; Treatment: concomitant platinum‐based chemotherapy |
| Interventions | |
| Outcomes | Changes in Hb values; QoL |
| Starting date | July 1997 |
| Contact information | Dr Hilary Thomas Department of Clinical Oncology Imperial College School of Medicine Hammersmith Hospital Du Cane Road London W12 0HS UK |
| Notes |
Howell.
| Trial name or title | A double blind, randomised, placebo‐controlled study to evaluate the impact of maintaining haemoglobin using epoetin alpha in stage IV breast cancer subjects receiving chemotherapy |
| Methods | |
| Participants | Disease: breast cancer; Treatment: concomitant chemotherapy |
| Interventions | Epoetin alfa vs placebo |
| Outcomes | Change in Hb values; Transfusion requirement; AE; OS; QoL. |
| Starting date | August 2000 |
| Contact information | Prof A. Howell Christie Hospital NHS Trust Wilmslow Road Withington Manchester M20 4BX UK |
| Notes |
Koelbl.
| Trial name or title | CDR 0000257189;AGOSG‐OVAR‐MO16375‐MARCH; EI20217; ROCHE‐MO16375; ROCH‐RO2053859 |
| Methods | |
| Participants | Solid cancers, Cervix ca, undergoing chemo ‐ plat + Rad |
| Interventions | Epo beta vs Standard care , epo dose unknown |
| Outcomes | Hb, AE, TR, Hb response, QoL |
| Starting date | |
| Contact information | H Koelbl |
| Notes |
Lambin 2006.
| Trial name or title | Lambin, was CDR0000068669 and EORTC 22996‐24002 |
| Methods | A phase III double‐blind, randomised, placebo‐controlled study of Erythropoietin when used as an adjuvant to radiation therapy in patients with head and neck squamous cell carcinoma |
| Participants | Head and neck squamous cell carcinoma; Radiation |
| Interventions | Epo once a week +RT +/‐chemotherapy versus placebo +RT +/‐chemotherapy |
| Outcomes | Loco‐regional control, overall survival, Hb levels during radiotherapy, adverse effects |
| Starting date | February 1999 designed for 762 patients |
| Contact information | Dr. P‐. Lambin, EORTC, Maastricht/Heerlen, The Netherlands Dr V. G. Budach Arbeitsgemeinschaft Radiologische Onkologie Dr J. Bernier EORTC Head and Neck Cancer Group Dr J.‐H. Bourhis Groupe d'Oncologie et Radiothérapie Tête et Cou Dr J. Denham Trans‐Tasman Radiation Oncological Group Incorporated |
| Notes |
Liang 2009.
| Trial name or title | The clinical study on recombinant human erythropoietin for chemotherapy ‐ related anaemia |
| Methods | Randomised controlled trial, not placebo‐controlled |
| Participants | N = 62 Disease: NR Treatment: chemotherapy Baseline Hb: NR |
| Interventions | Drug: Epo Dose: 12'000 IU tiw Hb‐target: NR Duration: 6 weeks |
| Outcomes | NR |
| Starting date | |
| Contact information | |
| Notes | Liang J, Qing B, Shen L, Cheng H. The clinical study on recombinant human erythropoietin for chemotherapy ‐ related anaemia. Clinical Research 2009;29(1):58‐60; full text in Chinese, English abstract, study number = 54993 |
Nitz 2008.
| Trial name or title | Adjuvant chemotherapy with or without darbepoetin in node‐positive breast cancer: a safety analysis from the phase III ARA plus trial |
| Methods | Randomised controlled trial |
| Participants | Breast cancer patients |
| Interventions | Darbepoetin versus control |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes | Nitz U, Oberhoff C, Reimer T, Schumacher C, Hackmann J, Warm M, Uleer C, Runde V, Gluz O, Zuna I West German Study Group, Moenchengladbach, Germany; Marienhospital, Essen, Germany; Klinikum Suedstadt, Rostock, Germany; St. Elisabeth KH, Koeln, Germany; Uni Koeln, Koeln, Germany; HZM Pharmaservice, Wiesbaden, Germany; Praxis Gyn. Onko., Hildesheim, Germany; Wilhelm‐Anton‐H., Goch, Germany. Adjuvant chemotherapy with or without darbepoetin in node‐positive breast cancer: a safety analysis from the phase III ARA plus trial. San Antonio Breast Cancer Symposium 2008:4100. |
O´Brien.
| Trial name or title | Open‐label randomised group‐comparative evaluation of the effect of epoetin on anaemia and fatigue in lung cancer patients receiving palliative platinum containing chemotherapy |
| Methods | |
| Participants | Disease: lung cancer Treatment: concomitant platinum containing chemotherapy |
| Interventions | Epoetin vs standardised intervention |
| Outcomes | Change in HB values; QoL; Response and tolerance to chemotherapy. |
| Starting date | August 1998 |
| Contact information | Dr Mary O´Brien Medicine Section The Royal Marsden NHS Trust Downs Road Sutton Surrey SM2 5PT UK |
| Notes |
O´Connell.
| Trial name or title | Phase III randomised study of epoetin alfa in anaemic patients with advanced cancer undergoing chemotherapy |
| Methods | |
| Participants | Disease: advanced cancer; Treatment: concomitant chemotherapy |
| Interventions | Epoetin alfa vs placebo |
| Outcomes | Change in Hb values; Transfusion requirement; QoL. |
| Starting date | December 1998 |
| Contact information | Dr M. J. O´Connell North Central Cancer Treatment Group USA |
| Notes |
Park 1996.
| Trial name or title | Clinical evaluation of recombinant human erythropoietin (Eprex) in anaemic cancer patients receiving chemotherapy |
| Methods | Randomised controlled trial |
| Participants | Anaemic cancer patients (lung cancer, stomach cancer, colon cancer) |
| Interventions | Epeotin alpha |
| Outcomes | Haematocrit, RBC transfusion |
| Starting date | NR |
| Contact information | NR |
| Notes | Park HS, Hong DS, Lee SJ, Chung TJ, Choi YM. Clinical evaluation of recombinant human erythropoietin(Eprex) in anaemic cancer patients receiving chemotherapy. Ann Oncol 1996;7(Suppl 5). |
Parliament.
| Trial name or title | Radiation therapy with or without Epoetin alfa in anaemic patients with head and neck cancer |
| Methods | |
| Participants | Disease: need and neck cancer; Treatment: concomitant radiotherapy |
| Interventions | Epoetin: Control: no treatment |
| Outcomes | Changes in Hb values; AEs; QoL; local tumour control rate; OS. |
| Starting date | |
| Contact information | Cross Canada Institute Edmonton, Alberta T6G 1Z2 Canada |
| Notes |
R Thomas 2002.
| Trial name or title | EPREX trial: Open‐label comparative‐group evaluation of the effect of epoetin alfa on quality of life and burden of illness in anaemic cancer patients receiving platinum containing chemotherapy |
| Methods | |
| Participants | Disease: various malignancies; Treatment: concomitant platinum‐based chemotherapy |
| Interventions | Epoetin alfa vs no treatment |
| Outcomes | QoL; Patient burden; Transfusion requirements; Change in Hb values. |
| Starting date | June 1997 |
| Contact information | Dr R. Thomas Primrose Oncology Unit Bedford South Wing Hospital Kempston Road Bedford MK42 9DJ UK |
| Notes |
Recasens 2003.
| Trial name or title | Randomised comparison of epoetin alfa versus control in patients with multiple myeloma, n=91, only interim analysis available so far, costs reported |
| Methods | Randomised controlled trial |
| Participants | Patients with multiple myeloma |
| Interventions | Epoetin alpha versus control |
| Outcomes | Costs |
| Starting date | |
| Contact information | pgiraldo@salud.aragon.es |
| Notes | Recasens V, Rubio‐Martinez A, Gomez‐Barrera M, Rubio‐Felix D, Giralt M, Giraldo P. A pharmacoeconomical analysis comparing Epoetin Alpha vs transfusion in patients with anaemia associated to multiple myeloma. Blood. 2003; Vol. 102, issue 11. |
Rexer 2006.
| Trial name or title | Prospektiv offene, randomisierte Phase III Studie zur Evaluation von Darbepoetin Alfa (Aranesp) als Supportivtherapie bei Paienten mit "good/intermediate prognosis" Keimzelltumoren: PEB versus PEB+ Darbepoetin alfa (Aranesp"), Leitung: Prof. Bokemeyer, University Hospital Eppendorf, Hamburg, Germany |
| Methods | Randomised controlled trial |
| Participants | Testicular cancer patients |
| Interventions | Darbepoetin versus control |
| Outcomes | Hb, RBC transfusion, QoL, disease progressions, OS. |
| Starting date | NR |
| Contact information | Ina Böhlke, i.boehlke@uke.uni‐hamburg.de |
| Notes | Rexer H [Darbepoetin alfa (Aranesp) as supportive therapy in patients with germ cell tumours]. Urologe A. 2006 Aug;45(8):1017‐8. MeckEvidence, Geschäftsstelle der AUO, Seestr. 11, 17252, Schwarz. AUO@MeckEvidence.de |
Rudd.
| Trial name or title | Evaluation of epoetin in lung cancer pts. receiving chemotherapy |
| Methods | |
| Participants | Disease: lung cancer; Treatment: concomitant platinum‐based chemotherapy |
| Interventions | Epoetin alpha vs no treatment |
| Outcomes | |
| Starting date | November 1998 |
| Contact information | Dr R. M. Rudd Medical Oncology Department St Bartholomew´s Hospital West Smithfield London EC1A 7BE UK |
| Notes |
Stewart.
| Trial name or title | Open randomised comparative group evaluation of the effect of epoetin alfa on local disease free survival and quality of life in head and neck cancer patients receiving radical radiotherapy |
| Methods | |
| Participants | Disease: head and neck cancer; Treatment: concomitant radiotherapy |
| Interventions | |
| Outcomes | Local tumour control; Disease‐free survival; QoL; OS. |
| Starting date | August 1999 |
| Contact information | Dr J. S. Stewart Department of Radiotherapy Charing Cross Hospital Fulham Palace Road London W6 8RF UK |
| Notes |
UKCCCR GN308.
| Trial name or title | A double‐blind, placebo controlled study to assess the effects of early intervention and/or treatment with Epoetin alfa on anaemia in cancer patients receiving non platinum containing chemotherapy |
| Methods | |
| Participants | Disease: cancer Treatment: concomitant chemotherapy |
| Interventions | Epoetin vs placebo |
| Outcomes | Transfusion requirement; QoL. |
| Starting date | |
| Contact information | UKCCCR Register Co‐ordinator MRC Clinical Trials Unit 222 Euston Road London NW1 2DA |
| Notes |
Yousseff 2011.
| Trial name or title | The Effectiveness of a Fixed Low Dose of Erythropoietin (EPO) in Anemic Solid Tumor Patients Receiving Concomitant Chemotherapy: A Prospective, Randomized, Controlled Study |
| Methods | Randomised controlled trial |
| Participants | Anemic solid tumour patients |
| Interventions | Low dose Epoetin versus control |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes | Youssef Lama A, Hussien Dilman Haj, Sulaiman Siham. The Effectiveness of a Fixed Low Dose of Erythropoietin (EPO) in Anemic Solid Tumor Patients Receiving Concomitant Chemotherapy: A Prospective, Randomized, Controlled Study. ASH Annual Meeting Abstracts 2011;118(21):2092 |
Ziras 2001.
| Trial name or title | Soluble transferrin receptor (sTFR) as a predictor of response to prophylactic epoetin alfa (EPO) treatment in non‐anaemic cancer patients (pts) under chemotherapy (CT). Preliminary results. |
| Methods | Randomised controlled trial |
| Participants | Non‐anaemic cancer patients |
| Interventions | Epoetin alpha |
| Outcomes | Hb |
| Starting date | NR |
| Contact information | Agii Anargiri Cancer Hospital Athens, Metaxa Cancer Hosptial, Piraeus, Greece |
| Notes | Proc Am Soc Clin Oncol 20:2001 (abstr 2987) |
AE: adverse event AZA: Azacitidine DLBCL: diffuse large B‐cell lymphoma. EPO: Erythropoietin ESA: erythropoiesis stimulating agent G‐CSF: granulocyte colony‐stimulating factors Hb: haemoglobin IPSS: International Prognostic Scoring System OS: overall survival PFS: progression‐free survival Pts.: patients QoL: quality of life RBCS: Red blood cells s.c.: subcutaneous vs.: versus NR: not reported RBCT: red blood cell transfusions RT: radiotherapy TR: tumour response
Differences between protocol and review
In previous versions of this review, we required dosages of at least 300 U/kg body weight per week (epoetin‐a and beta) given for at least four weeks. For the current update this criterion was removed and we included studies or study arms with low dosages as well. In previous versions of this review, iron supplementation had to be identical in the study arms of a given trial. For the current update, we changed this criterion and included trials using iron supplementation in the experimental but not in the control arm as well.
Contributions of authors
Thomy Tonia: Quality of Life analysis, searching for trials, eligibility and quality assessment, fact checking, data extraction and analysis, drafting of QoL and discussion, revision of review
Annette Mettler: Searching for trials, eligibility and quality assessment, data extraction and analysis
Nadège Robert: Searching for trials, eligibility and quality assessment, data extraction and analysis
Guido Schwarzer: Statistical and methodological advice, data analysis, content input
Olaf Weingart: eligibility and quality assessment, fact checking, creating summary of findings table
Jerome Seidenfeld: Clinical and scientific advice, content input, revision of draft review
Chris Hyde: Protocol development, searching for trials, eligibility and quality assessment, data extraction and analysis
Andreas Engert: Clinical and scientific advice, content input
Julia Bohlius: Protocol development, searching for trials, eligibility and quality assessment, data extraction and analysis, drafting and revision of review
Sources of support
Internal sources
Department of Internal Medicine I, University of Cologne, Germany.
Cochrane Haematological Malignancies Group (CHMG), Germany.
Institute of Social and Preventive Medicine, University of Bern, Switzerland.
External sources
Department of Health, UK.
Declarations of interest
Thomy Tonia, Annette Mettler, Nadège Robert, Olaf Weingart, Guido Schwarzer, Jerome Seidenfeld, Chris Hyde, Andreas Engert, Julia Bohlius: none known.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Aapro 2008 {published and unpublished data}
- Aapro M, Barnadas A, Leonard RC, Marangolo M, Untch M. Effects of epoetin beta treatment in patients with metastatic breast cancer receiving chemotherapy. Results of the BRAVE trial. Breast Cancer Research and Treatment 2006; Vol. 100:abstract 6095.
- Aapro M, Leonard RC, Barnadas A, Marangolo M, Untch M, Malamos N, et al. Effect of once‐weekly epoetin beta on survival in patients with metastatic breast cancer receiving anthracycline‐ and/or taxane‐based chemotherapy: Results of the Breast Cancer‐Anemia and the Value of Erythropoietin (BRAVE) Study. Journal of Clinical Oncology 2008;26(4):592‐8. [DOI] [PubMed] [Google Scholar]
- Leonard RC, Aapro M, Chan S, Dirix LY, Mayordomo J, Reichert D, et al. Once weekly epoetin beta in patients with metastatic breast cancer receiving anthracycline‐ or taxane‐based chemotherapy. Annals of Oncology 2004;Vol. 15(Suppl 3):iii.50 (Abstract 188p). [Google Scholar]
Aapro 2008 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Abels 1993 {published and unpublished data}
- Abels R. Erythropoietin for anemia in cancer patients. European Journal of Cancer 1993;29A(Suppl 2):2‐8. [DOI] [PubMed] [Google Scholar]
- Abels R. Recombinant human erythropoietin in the treatment of the anaemia of cancer. Acta Haematologica 1992;87 (Suppl 1):4‐11. [DOI] [PubMed] [Google Scholar]
- Abels RI, Larholt KM, Krantz KD, Bryant EC. Recombinant Human Erythropoietin (rHuEPO) for the treatment of the anemia of cancer. Oncologist 1996;1(3):140‐50. [PubMed] [Google Scholar]
Abels 1993 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Abels 1993 J&J 2004 {published data only}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Antonadou 2001 {published data only}
- Antonadou D, Cardamakis E, Puglisi M, Malamos N, Throuvalas N. Erythropoietin enhances radiation treatment efficacy in patients with pelvic malignancies. Final results of a randomized phase III study. Poster.
Aravantinos 2003 {published data only}
- Aravantinos G, Linardou H, Makridaki D, Laiou E, Zafiropoulos A, Janninis J, et al. Recombinant human erythropoietin for platinum‐based chemotherapy‐induced anaemia: A single‐centre randomised study. Journal of B U On 2003;8(2):127‐32. [MEDLINE: ] [PubMed] [Google Scholar]
Bamias 2003 {published data only}
- Bamias A, Aravantinos G, Kalofonos C, Timotheadou N, Siafaka V, Vlahou I, et al. Prevention of anemia in patients with solid tumors receiving platinum‐based chemotherapy by recombinant human Erythropoietin (rHuEpo): a prospective, open label, randomized trial by the Hellenic Cooperative Oncology Group. Oncology 2003;64(2):102‐10. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Blohmer 2011 {published and unpublished data}
- Blohmer JU, Paepke S, Sehouli J, Boehmer D, Kolben M, Würschmidt F, et al. Randomized phase III trial of sequential adjuvant chemoradiotherapy with or without erythropoietin alfa in patients with high‐risk cervical cancer: results of the NOGGO‐AGO intergroup study. Journal of Clinical Oncology 2011;29(28):3791‐7. [DOI] [PubMed] [Google Scholar]
- Blohmer JU, Wuerschmidt J, Petry K, Weise G, Sehouli J, Kimming R, et al. Results with sequential adjuvant chemo‐radiotherapy with vs. without epoetin alfa for patients with high‐risk cervical cancer: results of a prospective, randomized, open and controlled AGO and NOGGO‐intergroup study. Annals of Oncology. Vol. 15 Suppl 3. 2004.
Boogaerts 2003 {published and unpublished data}
- Neorecormon (epoetin beta). Briefing package or the FDA Oncologic Advisory Committee Meeting, May 4, 2004 Vol. RO 205‐3859.
- Boogaerts M, Coiffier B, Kainz C, Epoetin beta QOL Working Group. Impact of epoetin beta on quality of life in patients with malignant disease. British Journal of Cancer 2003;88(7):988‐95. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Boogaerts 2003 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Boogaerts Coiffier 2001 {published and unpublished data}
- Coiffier B, Boogaerts M, Kainz C. Impact of epoetin beta on quality of life in patients with malignant disease. 6th Congress of the European Haematology Association. 2001:Abstract #194.
Carabantes 1999 {published data only}
- Carabantes FJ, Benavides M, Trujillo R, Cobo M, Hebrero ML, Garcia S, et al. Epoetin alfa in the prevention of anemia in cancer patients undergoing platinum‐based chemotherapy (CT) (CT). A prospective randomized study. Proceedings of the American Society of Clinical Oncology 1999;18:596a. Abstract 2303. [Google Scholar]
Cascinu 1994 {published and unpublished data}
- Cascinu S, Fedeli A, Ferro E, Fedeli SL, Catalano G. Recombinant human erythropoietin treatment in cisplatin‐associated anemia: a randomized, double‐blind trial with placebo. Journal of Clinical Oncology 1994;12:1058‐62. [DOI] [PubMed] [Google Scholar]
Case 1993 {published and unpublished data}
- Abels RI, Larholt KM, Krantz KD, Bryant EC. Recombinant Human Erythropoietin (rHuEPO) for the treatment of the anemia of cancer. Oncologist 1996;1(3):140‐50. [PubMed] [Google Scholar]
- Case DC, Bukowski RM, Carey RW, Fishkin EH, Henry DH, Jacobson RJ, et al. Recombinant human erythropoietin therapy for anemic cancer patients on combination chemotherapy. Journal of the National Cancer Institute 1993;85(10):801‐6. [DOI] [PubMed] [Google Scholar]
Case 1993 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Case 1993 J&J 2004 {published data only}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Cazzola 1995 {published and unpublished data}
- Neorecormon (epoetin beta). Briefing package or the FDA Oncologic Advisory Committee Meeting, May 4, 2004 Vol. RO 205‐3859.
- Cazzola M, Messinger D, Battistel V, Bron D, Cimino R, Enller‐Ziegler L, et al. Recombinant human erythropoietin in the anemia associated with multiple myeloma or non‐Hodgkin's lymphoma: dose finding and identification of predictors of response. Blood 1995;86(12):4446‐53. [PubMed] [Google Scholar]
Cazzola 1995a {published and unpublished data}
- Cazzola M, Messinger D, Battistel V, Bron D, Cimino R, Enller‐Ziegler L, et al. Recombinant human erythropoietin in the anemia associated with multiple myeloma or non‐Hodgkin's lymphoma: dose finding and identification of predictors of response. Blood 1995;86(12):4446‐53. [PubMed] [Google Scholar]
Cazzola 1995b {published and unpublished data}
- Cazzola M, Messinger D, Battistel V, Bron D, Cimino R, Enller‐Ziegler L, et al. Recombinant human erythropoietin in the anemia associated with multiple myeloma or non‐Hodgkin's lymphoma: dose finding and identification of predictors of response. Blood 1995;86(12):4446‐53. [PubMed] [Google Scholar]
Cazzola 1995c {published and unpublished data}
- Cazzola M, Messinger D, Battistel V, Bron D, Cimino R, Enller‐Ziegler L, et al. Recombinant human erythropoietin in the anemia associated with multiple myeloma or non‐Hodgkin's lymphoma: dose finding and identification of predictors of response. Blood 1995;86(12):4446‐53. [PubMed] [Google Scholar]
Cazzola 1995d {published and unpublished data}
- Cazzola M, Messinger D, Battistel V, Bron D, Cimino R, Enller‐Ziegler L, et al. Recombinant human erythropoietin in the anemia associated with multiple myeloma or non‐Hodgkin's lymphoma: dose finding and identification of predictors of response. Blood 1995;86(12):4446‐53. [PubMed] [Google Scholar]
Cazzola 1995 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chang 2005 {published and unpublished data}
- Chang J, Couture F, Young S, McWatters KL, Lau CY. Once weekly epoetin alfa maintains hemoglobin, improves quality of life and reduces transfusion in breast cancer patients receiving chemotherapy. Journal of Clinical Oncology 2005;23(12):2597‐605. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Chang J, Couture FA, Young SD, Lau CY, Lee McWatters K. Weekly administration of epoetin alfa improves cognition and quality of life in patients with breast cancer receiving chemotherapy. Supportive Cancer Therapy 2004;2(1):52‐8. [DOI] [PubMed] [Google Scholar]
Chang 2005 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Charu 2007 {published and unpublished data}
- Charu V, Belani CP, Gill AN, Bhatt M, Ben‐Jacob A, Tomita D, et al. A controlled, randomized, open‐label study to evaluate the effect of every‐2‐week darbepoetin alfa for anemia of cancer. Annual Meeting Proceedings of the American Society of Clinical Oncology 2004:abstract 8084.
- Charu V, Belani CP, Gill AN, Bhatt M, Tomita D, Rossi G, et al. Efficacy and safety of every‐2‐week darbepoetin alfa in patients with anemia of cancer: a controlled, randomized, open‐label phase II trial. Oncologist 2007;12(6):727‐37. [DOI] [PubMed] [Google Scholar]
- Charu V, Saidman B, Ben‐Jacob A, Justice GR, Maniam AS, Rearden T, et al. Improvements in fatigue are associated with early treatment with darbepoetin alfa every 3 weeks in anemic patients receiving chemotherapy. The Journal of Supportive Oncology 2005;3(2 Suppl 1):14‐5. [Google Scholar]
Charu 2007 Amgen 2007 {published data only}
- Amgen Inc with contributions from Johnson & Johnson Pharmaceutical Research and Development, L.L.C. Safety of Erythropoiesis‐Stimulating Agents (ESAs) in Oncology). Background information for Oncologic Drugs Advisory Committee 10 May 2007.
Charu 2007 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Christodoulou 2009 {published data only}
- Christodoulou C, Dafni U, Aravantinos G, Koutras A, Samantas E, Karina M, et al. Effects of epoetin‐alpha on quality of life of cancer patients with solid tumors receiving chemotherapy. Anticancer Research 2009;29:693‐702. [PubMed] [Google Scholar]
- Janinis J, Dafni U, Aravantinos G, Kalofonos HP, Papakostas P, Tsavdaridis D, et al. Quality of life (QoL) outcome of epoietin‐alfa (EPO‐A) in anemic cancer patients undergoing platinum or non‐platinum‐based chemotherapy: a randomized study conducted by the Hellenic Cooperative Oncology Group. Proceedings of the American Society of Clinical Oncology. 2003; Vol. 22:789.
Dammacco 2001 {published and unpublished data}
- Dammacco F, Castoldi G, Rodjer S. Efficacy of epoetin alfa in the treatment of anaemia of multiple myeloma. British Journal of Haematology 2001;113(1):172‐9. [DOI] [PubMed] [Google Scholar]
- Dammacco F, Silvestris F, Castoldi GL, Grassi B, Bernasconi C, Nadali G, et al. The effectiveness and tolerability of epoetin alfa in patients with multiple myeloma refractory to chemotherapy. International Journal of Clinical and Laboratory Research 1998;28:127‐34. [DOI] [PubMed] [Google Scholar]
Dammacco 2001 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dammacco 2001 J&J 2004 {published data only}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Debus 2006 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Debus 2006 J&J 2004 {published and unpublished data}
- Debus J, Hindermann S, Morr H, Mezger J, Sebastian M, Angermund R, et al. Epoetin alfa (EPO) and survival in patients with non‐resectable NSCLC ‐ Interim results. Lung Cancer 2005; Vol. 49, issue Suppl 3:S57.
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Debus 2006 J&J 2007 {published data only}
- Debus J, Hindermann S, Morr H, Mezger J, Sebastian M, Angermund R, et al. Epoetin alfa (EPO) and survival in patients with non‐resectable NSCLC ‐ Interim results. Lung Cancer 2005; Vol. 49, issue Suppl 3:S57.
Del Mastro 1997 {published and unpublished data}
- Mastro L, Venturini M, Lionetto R, Garrone O, Melioli G, Pasquetti W, et al. Randomized phase III trial evaluating the role of erythropoietin in the prevention of chemotherapy‐induced anemia. Journal of Clinical Oncology 1997;15(7):2715‐21. [DOI] [PubMed] [Google Scholar]
Dunphy 1999 {published data only}
- Dunphy FR, Harrison BR, Dunleavy TL, Rodriguez JJ, Hilton JG, Boyd JH. Erythropoietin reduces anemia and transfusions. Cancer 1999;86:1362‐7. [DOI] [PubMed] [Google Scholar]
Engert 2009 {published data only}
- Engert A, Borchmann P, Fuchs M, Josting A, Haverkamp H, Diehl V. Prospetively randomized placebo‐controlled trial of epoetin‐alfa in patients with advanced‐stage Hodgking lymphoma: final analysis of the GHSG HD15‐EPO trial. Blood ASH Annual Meeting Abstracts 2008;112:2598. [Google Scholar]
Engert 2010 {published data only}
- Engert A, Josting A, Haverkamp H, Villalobos M, Lohri A, Sökler M, et al. Epoetin alfa in patients with advanced‐stage Hodgkin's lymphoma: results of the randomized placebo‐controlled GHSG HD15EPO trial. Journal of Clinical Oncology 2010;28(13):2239‐45. [DOI] [PubMed] [Google Scholar]
EPO‐GER‐20 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
EPO‐INT‐1 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
EPO‐INT‐1 J&J 2004 {published and unpublished data}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
- Luksenburg H, Weir A, Wager R. EPO‐INT‐1: Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen, Inc. and Procrit (epoetin alfa) Ortho Biotech, L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Oncologic Drugs Advisory Committee, Rockville (MD), USA, 2004; Vol. http://www.fda.gov/ohrms/dockets/ac/04/briefing/4037b2_04.pdf [date of last access March 27, 2009].
EPO‐INT‐3 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
EPO‐INT‐3 J&J 2004 {published and unpublished data}
- A placebo controlled study on the effect of r‐HeUPO in patients with malignancy receiving chemotherapy.Study: CR005923. Raritan, NJ: RW Johnson Pharmaceutical Research Institute 1998.
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
- Luksenburg H, Weir A, Wager R. EPO‐INT‐3: Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen, Inc. and Procrit (epoetin alfa) Ortho Biotech, L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Oncologic Drugs Advisory Committee Rockville (MD), USA, 2004; Vol. http://www.fda.gov/ohrms/dockets/ac/04/briefing/4037b2_04.pdf [date of last access March 27, 2009].
Fujisaka 2011 {published data only}
- Fujisaka Y, Sugiyama T, Saito H, Nagase S, Kudoh S, Endo M, et al. Randomised, phase III trial of epoetin‐B to treat chemotherapy‐induced anaemia according to the EU regulation. British Journal of Cancer 2011;105(9):1267‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshizaki A, Kumagai S, Sugiyama T, Goto I, Saito H, Ariyoshi Y, Saijo N, Ohashi Y. A phase III, randomized, double‐blind placebo‐controlled study of epoetin beta in lung and gynecological cancer receiving platinum‐based chemotherapy: Japan Erythropoietin Study Group. Annals of Oncology 2010;21(S8):viii385. [Google Scholar]
Gebbia 2003 {published data only}
- Gebbia V, Marco P, Citarrella P. Systemic chemotherapy in elderly patients with locally advanced and/or inoperable squamous cell carcinoma of the head and neck: impact of anemia and role of recombinant human erythropoietin. Critical Reviews in Oncology/Hematology 2003;48:49‐55. [DOI] [PubMed] [Google Scholar]
Gordon 2008 {published and unpublished data}
- Gordon D, Nichols G, Ben‐Jacob A, Tomita D, Lillie T, Miller C. Treating anemia of cancer with every‐4‐week darbepoetin alfa: Final efficacy and safety results from a phase II, randomized, double‐blind, placebo‐controlled study. Oncologist 2008;13(6):715‐24. [DOI] [PubMed] [Google Scholar]
- Gordon DH, Nichols G, Ben‐Jacob A, Lam H, Lillie T, Miller C. Treating anemia of cancer with darbepoetin alfa administered every 4 weeks: Final results from a phase 2, randomized, double‐Blind, placebo‐controlled study in cancer patients not receiving chemotherapy and/or radiotherapy. Blood 2006; Vol. 108, issue 11 Suppl:abstract 1304.
Gordon 2008 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Goss 2005 {published and unpublished data}
- Goss G, Feld R, Bezjak A, Perry G, Melosky B, Smith C, et al. Impact of maintaining Hb with epoetin alfa on time to progression (TTP), overall survival (OS), quality of life (QOL) and transfusion reduction in limited disease SCLC patients. Lung cancer 2005; Vol. 49, issue Suppl 2:S53.
Goss 2005 FDA 2004 {published data only}
- Luksenburg H, Weir A, Wager R. Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen, Inc. and Procrit (epoetin alfa) Ortho Biotech, L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. FDA Briefing Document May 4, 2004 Oncologic Drugs Advisory Committee.
Goss 2005 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Goss 2005 J&J 2004 {published and unpublished data}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD Report Date: 30 MARCH 2004.
Grote 2005 {published and unpublished data}
- Grote T, Yeilding AL, Castillo R, Butler D, Fishkin E, Henry DH, et al. Efficacy and safety analysis of epoetin alfa in patients with small‐cell lung cancer: a randomized, double‐blind, placebo‐controlled trial. Journal of Clinical Oncology 2005;23(36):9377‐86. [DOI] [PubMed] [Google Scholar]
- Luksenburg H, Weir A, Wager R. Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen, Inc. and Procrit(epoetin alfa) Ortho Biotech, L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. FDA Briefing Document May 4, 2004 Oncologic Drugs Advisory Committee.
Grote 2005 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grote 2005 J&J 2004 {published and unpublished data}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Gupta 2009 {published data only}
- Gupta S, Singh P, Bisht S, Bhatt M, Pant M, Gupta R, et al. Recombinant human erythropoietin in patients of advanced Cancer treated "by chemoradiotherapy". Landes Bioscience 2009;8(1):13‐7. [DOI] [PubMed] [Google Scholar]
Hedenus 2002 {published data only}
- Hedenus M, Hansen S, Taylor K, Arthur C, Emmerich B, Dewey C, et al. Randomized, dose‐finding study of darbepoetin alfa in anaemic patients with lymphoproliferative malignancies. British Journal of Haematology 2002;119(1):79‐86. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hedenus 2002a {published data only}
- Hedenus M, Hansen S, Taylor K, Arthur C, Emmerich B, Dewey C, et al. Randomized, dose‐finding study of darbepoetin alfa in anaemic patients with lymphoproliferative malignancies. British Journal of Haematology 2002;119(1):79‐86. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hedenus 2002b {published data only}
- Hedenus M, Hansen S, Taylor K, Arthur C, Emmerich B, Dewey C, et al. Randomized, dose‐finding study of darbepoetin alfa in anaemic patients with lymphoproliferative malignancies. British Journal of Haematology 2002;119(1):79‐86. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hedenus 2002c {published data only}
- Hedenus M, Hansen S, Taylor K, Arthur C, Emmerich B, Dewey C, et al. Randomized, dose‐finding study of darbepoetin alfa in anaemic patients with lymphoproliferative malignancies. British Journal of Haematology 2002;119(1):79‐86. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hedenus 2003 {published and unpublished data}
- Amgen Inc. Aranesp® (darbepoetin alfa) safety. Oncologic Drugs Advisory Committee, 4 May 2004.
- Hedenus M, Adriansson M, San Miguel J, Kramer MH, Schipperus MR, Juvonen E, et al. Efficacy and safety of darbepoetin alfa in anaemic patients with lymphoproliferative malignancies: a randomized, double‐blind, placebo‐controlled study. British Journal of Haematology 2003;122(3):394‐403. [DOI] [PubMed] [Google Scholar]
- Hedenus M, Brandberg Y, Molostova V, Iosova G, Abdulkadyrov K, Messinger D, et al. Efficacy of epoetin beta in treating the anaemia of cancer in patients with haematological malignancies. Proceedings of the 6th Congress of the European Haematology Association 2001:abstract 190.
Hedenus 2003 FDA 2007 {published and unpublished data}
- 20000161. Continuing reassessment of the risks of erythropoiesis‐stimulating agents (ESAs) administered for the treatment of anemia associated with cancer chemotherapy. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Oncologic Drugs Advisory Committee, Rockville (MD), USA, 2007; Vol. http://www.fda.gov/ohrms/dockets/ac/07/briefing/2007‐4301b2‐02‐ FDA.pdf.
Hedenus 2003 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Henke 1999 {published data only}
- Henke M, Guttenberger R, Barke A, Pajonk F, Potter R, Frommhold H. Erythropoietin for patients undergoing radiotherapy: a pilot study. Radiotherapy and Oncology 1999;50(2):185‐90. [DOI] [PubMed] [Google Scholar]
Henke 1999a {published data only}
- Henke M, Guttenberger R, Barke A, Pajonk F, Potter R, Frommhold H. Erythropoietin for patients undergoing radiotherapy: a pilot study. Radiotherapy and Oncology 1999;50(2):185‐90. [DOI] [PubMed] [Google Scholar]
Henke 1999b {published data only}
- Henke M, Guttenberger R, Barke A, Pajonk F, Potter R, Frommhold H. Erythropoietin for patients undergoing radiotherapy: a pilot study. Radiotherapy and Oncology 1999;50(2):185‐90. [DOI] [PubMed] [Google Scholar]
Henke 1999c {published data only}
- Henke M, Guttenberger R, Barke A, Pajonk F, Potter R, Frommhold H. Erythropoietin for patients undergoing radiotherapy: a pilot study. Radiotherapy and Oncology 1999;50(2):185‐90. [DOI] [PubMed] [Google Scholar]
Henke 2003 {published and unpublished data}
- Henke M, Laszig R, Ruebe C, Schaefer U, Haase KD, Schilcher B, et al. Erythropoietin to treat head and neck cancer patients with anaemia undergoing radiotherapy: randomised, double‐blind, placebo‐controlled trial. Lancet 2003;362:1255‐60. [DOI] [PubMed] [Google Scholar]
- Schipper J, Henke M. Erythropoietin in patients with head and neck carcinomas? [Erythropoetin bei Karzinomen im Kopf‐/Halsbereich?]. Laryngorhinootologie 2004;83(5):292‐7. [DOI] [PubMed] [Google Scholar]
Henke 2003 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Henke 2003 Roche 2004 {published data only}
- Neorecormon (epoetin beta). Briefing package or the FDA Oncologic Advisory Committee Meeting, May 4, 2004 Vol. RO 205‐3859.
Henry 1995 {published and unpublished data}
- Abels RI, Larholt KM, Krantz KD, Bryant EC. Recombinant Human Erythropoietin (rHuEPO) for the treatment of the anemia of cancer. Oncologist 1996;1(3):140‐50. [PubMed] [Google Scholar]
- Henry DH, Abels RI. Recombinant human erythropoietin in the treatment of cancer and chemotherapy‐induced anemia: results of double‐blind and open‐label follow‐up studies. Seminars in Oncology 1994;21(2 (Suppl 3)):21‐8. [PubMed] [Google Scholar]
- Henry DH, Brooks BJ, Case DC, Fishkin E, Jacobson R, Keller AM, et al. Recombinant human erythropoietin therapy for anemic cancer patients receiving cisplatin chemotherapy. Cancer Journal from Scientific American 1995;1:252‐60. [PubMed] [Google Scholar]
Henry 1995 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Henry 1995 J&J 2004 {published data only}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Hernandez 2009 {published and unpublished data}
- Hernandez. Randomized, double‐blind, placebo‐controlled trial of every‐3‐week darbepoetin alfa 300 micrograms for treatment of chemotherapy‐induced anemia. Current Medical Research and Opinion 2009;25(9):2109‐20. [DOI] [PubMed] [Google Scholar]
- Taylor K, Ganly P, Charu V, DiBenedetto J, Kracht K, Rossi G, et al. Randomized, double‐blind, placebo‐controlled study of darbepoetin alfa every 3 weeks for the treatment of chemotherapy‐induced anemia. Blood 2005; Vol. 106, issue 11:abstract 3556.
Hernandez 2009 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoskin 2009 {published data only}
- Hoskin P, Robinson M, Slevin N, Morgan D, Harrington K, Gaffney C. Effect of Epoetin Alfa on Survival and Cancer Treatment‐Related Anemia and Fatigue in Paatients Receiving Radical Radiotherapy With Curative Intent for Head and Neck Cancer. Journal of Clinical Oncology 2009;27(34):5751‐5756. [DOI] [PubMed] [Google Scholar]
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Hoskin 2009 GBR‐7 FDA 04 {published data only}
- Luksenburg H, Weir A, Wager R. EPO‐GBR‐7: Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen Inc. and Procrit (epoetin alfa) Ortho Biotech L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Oncologic Drugs Advisory Committee, Rockville (MD), USA, 2004; Vol. http://www.fda.gov/ohrms/dockets/ac/04/briefing/4037b2_04.pdf [date of last access March 27, 2009].
Hoskin 2009 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoskin 2009 J&J 2004 {published data only}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Huddart 2002 {published and unpublished data}
- Huddart RA, Welch RS, Chan S, Perren T, Atkinson R. A prospective randomised comparative‐group evaluation of epoetin alfa for the treatment of anaemia in UK cancer patients receiving platinum‐based chemotherapy. Annals of Oncology 2002;13 (Suppl 5):177. [MEDLINE: ] [Google Scholar]
Huddart 2002 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Iconomou 2003 {published data only}
- Iconomou G, Koutras A, Rigopoulos A, Vagenakis AG, Kalofonos HP. Effect of recombinant human erythropoietin on quality of life in cancer patients receiving chemotherapy: results of a randomized, controlled trial. Journal of Pain & Symptom Management 2003;25(6):512‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Italian 1998 {published and unpublished data}
- Italian Cooperative Study Group For rHuEpo In Myelodysplastic Syndromes. A randomized double‐blind placebo‐controlled study with subcutaneous recombinant human erythropoietin in patients with low‐risk myelodysplastic syndromes. British Journal of Haematology 1998;103:1070‐4. [DOI] [PubMed] [Google Scholar]
Katakami 2008 {published data only}
- Katakami N, Nishiwaki Y, Fujiwara Y, Tsuboi M, Takeda K, Nakanishi T, et al. Randomized, double‐blind, placebo‐controlled phase III study of weekly administration of darbepoetin alfa (DA) in anemic patients with lung or gynecologic cancer receiving platinum‐containing chemotherapy. Annals of Oncology 2008;19(S8):viii277‐viii278. [Google Scholar]
- Katsumata N, Fujiwara Y, Katakami N, Nishiwaki Y, Tsuboi M, Takeda K, et al. Randomized, double‐blind, placebo‐controlled phase III study of weekly administration of darbepoetin alfa in anemic patients with lung or gynecologic cancer receiving platinum‐containing chemotherapy. Vox Sanguinis 2009;97(S1):58. [Google Scholar]
Kotasek 2002 {published and unpublished data}
- Kotasek D, Albertsson M, Mackey J, Darbepoetin Alfa 980291 Study Group. Randomized, double‐blind, placebo‐controlled, dose‐finding study of darbepoetin alfa administered once every 3 (Q3W) or 4 (Q4W) weeks in patients with solid tumors. Proceedings of the American Society of Clinical Oncology 2002; Vol. 21:356a.
- Kotasek D, Albertsson M, Mackey J, Steger G, Rossi G, O'Byne J, et al. Once per cycle dosing of darbepoetin alfa is feasible in anemic cancer patients receiving chemotherapy. Annals of Oncology 2002; Vol. 13, issue Suppl 5:170.
Kotasek 2002 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kotasek 2003 {published and unpublished data}
- Kotasek D, Berg R, Poulsen E, Colowick A. Randomized, double‐blind, placebo controlled, phase I/II dose finding study of ARANESP (TM) administered once every three weeks in solid tumor patients. Blood 2000; Vol. 96, issue 11:abstract 1268.
- Kotasek D, Steger G, Faught W, Underhill C, Poulsen E, Colowick AB, et al. Darbepoetin alfa administered every 3 weeks alleviates anaemia in patients with solid tumours receiving chemotherapy; results of a double‐blind, placebo‐controlled, randomised study. European Journal of Cancer 2003;39(14):2026‐34. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kotasek 2003a {published and unpublished data}
- Kotasek D, Berg R, Poulsen E, Colowick A. Randomized, double‐blind, placebo controlled, phase I/II dose finding study of ARANESP (TM) administered once every three weeks in solid tumor patients. Blood 2000; Vol. 96, issue 11:abstract 1268.
- Kotasek D, Steger G, Faught W, Underhill C, Poulsen E, Colowick AB, et al. Darbepoetin alfa administered every 3 weeks alleviates anaemia in patients with solid tumours receiving chemotherapy; results of a double‐blind, placebo‐controlled, randomised study. European Journal of Cancer 2003;39(14):2026‐34. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kotasek 2003b {published and unpublished data}
- Kotasek D, Berg R, Poulsen E, Colowick A. Randomized, double‐blind, placebo controlled, phase I/II dose finding study of ARANESP (TM) administered once every three weeks in solid tumor patients. Blood 2000; Vol. 96, issue 11:abstract 1268.
- Kotasek D, Steger G, Faught W, Underhill C, Poulsen E, Colowick AB, et al. Darbepoetin alfa administered every 3 weeks alleviates anaemia in patients with solid tumours receiving chemotherapy; results of a double‐blind, placebo‐controlled, randomised study. European Journal of Cancer 2003;39(14):2026‐34. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kotasek 2003c {published and unpublished data}
- Kotasek D, Berg R, Poulsen E, Colowick A. Randomized, double‐blind, placebo controlled, phase I/II dose finding study of ARANESP (TM) administered once every three weeks in solid tumor patients. Blood 2000; Vol. 96, issue 11:abstract 1268.
- Kotasek D, Steger G, Faught W, Underhill C, Poulsen E, Colowick AB, et al. Darbepoetin alfa administered every 3 weeks alleviates anaemia in patients with solid tumours receiving chemotherapy; results of a double‐blind, placebo‐controlled, randomised study. European Journal of Cancer 2003;39(14):2026‐34. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kotasek 2003d {published and unpublished data}
- Kotasek D, Berg R, Poulsen E, Colowick A. Randomized, double‐blind, placebo controlled, phase I/II dose finding study of ARANESP (TM) administered once every three weeks in solid tumor patients. Blood 2000; Vol. 96, issue 11:abstract 1268.
- Kotasek D, Steger G, Faught W, Underhill C, Poulsen E, Colowick AB, et al. Darbepoetin alfa administered every 3 weeks alleviates anaemia in patients with solid tumours receiving chemotherapy; results of a double‐blind, placebo‐controlled, randomised study. European Journal of Cancer 2003;39(14):2026‐34. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kotasek 2003e {published and unpublished data}
- Kotasek D, Berg R, Poulsen E, Colowick A. Randomized, double‐blind, placebo controlled, phase I/II dose finding study of ARANESP (TM) administered once every three weeks in solid tumor patients. Blood 2000; Vol. 96, issue 11:abstract 1268.
- Kotasek D, Steger G, Faught W, Underhill C, Poulsen E, Colowick AB, et al. Darbepoetin alfa administered every 3 weeks alleviates anaemia in patients with solid tumours receiving chemotherapy; results of a double‐blind, placebo‐controlled, randomised study. European Journal of Cancer 2003;39(14):2026‐34. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kotasek 2003f {published and unpublished data}
- Kotasek D, Berg R, Poulsen E, Colowick A. Randomized, double‐blind, placebo controlled, phase I/II dose finding study of ARANESP (TM) administered once every three weeks in solid tumor patients. Blood 2000; Vol. 96, issue 11:abstract 1268.
- Kotasek D, Steger G, Faught W, Underhill C, Poulsen E, Colowick AB, et al. Darbepoetin alfa administered every 3 weeks alleviates anaemia in patients with solid tumours receiving chemotherapy; results of a double‐blind, placebo‐controlled, randomised study. European Journal of Cancer 2003;39(14):2026‐34. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kotasek 2003 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Krzakowski 2008 {published data only}
- Krzakowski M, DYNEPO Oncology Study Group. Epoetin delta: efficacy in the treatment of anaemia in cancer patients receiving chemotherapy. Clinical Oncology 2008;20:705‐13. [DOI] [PubMed] [Google Scholar]
Krzakowski 2008a {published data only}
- Krzakowski M, DYNEPO Oncology Study Group. Epoetin delta: efficacy in the treatment of anaemia in cancer patients receiving chemotherapy. Clinical Oncology 2008;20:705‐13. [DOI] [PubMed] [Google Scholar]
Krzakowski 2008b {published data only}
- Krzakowski M, DYNEPO Oncology Study Group. Epoetin delta: efficacy in the treatment of anaemia in cancer patients receiving chemotherapy. Clinical Oncology 2008;20:705‐13. [DOI] [PubMed] [Google Scholar]
Kunikane 2001 {published and unpublished data}
- Kunikane H, Watanabe K, Fukuoka M, Saijo N, Furuse K, Ikegami H, et al. Double‐blind randomized control trial of the effect of recombinant human erythropoietin on chemotherapy‐induced anemia in patients with non‐small cell lung cancer. International journal of clinical oncology 2001;6:296‐301. [DOI] [PubMed] [Google Scholar]
Kunikane 2001a {published and unpublished data}
- Kunikane H, Watanabe K, Fukuoka M, Saijo N, Furuse K, Ikegami H, et al. Double‐blind randomized control trial of the effect of recombinant human erythropoietin on chemotherapy‐induced anemia in patients with non‐small cell lung cancer. International journal of clinical oncology 2001;6:296‐301. [DOI] [PubMed] [Google Scholar]
Kunikane 2001b {published and unpublished data}
- Kunikane H, Watanabe K, Fukuoka M, Saijo N, Furuse K, Ikegami H, et al. Double‐blind randomized control trial of the effect of recombinant human erythropoietin on chemotherapy‐induced anemia in patients with non‐small cell lung cancer. International journal of clinical oncology 2001;6:296‐301. [DOI] [PubMed] [Google Scholar]
Kurz 1997 {published and unpublished data}
- Kurz C, Marth C, Windbichler G, Lahousen M, Medl M, Vavra N, et al. Erythropoietin treatment under polychemotherapy in patients with gynecologic malignancies: a prospective, randomized, double‐blind placebo‐controlled multicenter study. Gynecologic Oncology 1997;65(3):461‐6. [DOI] [PubMed] [Google Scholar]
Leyland‐Jones 05 J&J 04 {published data only}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Leyland‐Jones 2005 {published and unpublished data}
- Leyland‐Jones B. Breast cancer trial with erythropoietin terminated unexpectedly. Lancet Oncology 2003;4:459‐60. [DOI] [PubMed] [Google Scholar]
- Leyland‐Jones B, Semiglazov V, Pawlicki M, Pienkowski T, Tjulandin S, Manikhas G, et al. Maintaining normal hemoglobin levels with epoetin alfa in mainly nonanemic patients with metastatic breast cancer receiving first‐line chemotherapy: A survival study. Journal of Clinical Oncology 2005;23(25):5865‐8. [DOI] [PubMed] [Google Scholar]
- Luksenburg H, Weir A, Wager R. Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen, Inc. and Procrit (epoetin alfa) Ortho Biotech, L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. FDA Briefing Document May 4, 2004 Oncologic Drugs Advisory Committee.
Leyland‐Jones 2005 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Littlewood 2001 {published and unpublished data}
- Aapro MS, Cella D, Zagari M. Age, anemia, and fatigue. Seminars in Oncology 2002;29(3 Suppl 8):55‐9. [DOI] [PubMed] [Google Scholar]
- Fairclough DL, Gagnon DD, Zagari MJ, Marschner N, Dicato M. Evaluation of quality of life in a clinical trial with nonrandom dropout: the effect of epoetin alfa in anemic cancer patients. Quality of Life Research 2003;12(8):1013‐27. [DOI] [PubMed] [Google Scholar]
- Fallowfield L, Gagnon D, Zagari M, Cella D, Bresnahan B, Littlewood TJ, et al. Multivariate regression analyses of data from a randomised, double‐blind, placebo‐controlled study confirm quality of life benefit of epoetin alfa in patients receiving non‐platinum chemotherapy. British Journal of Cancer 2002;87(12):1341‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlewood TJ. Efficacy and quality of life outcomes of epoetin‐alpha in a double‐blind, placebo‐controlled, multicentre study of cancer patients receiving non‐platinum‐containing chemotherapy. Frontiers of Radiation Therapy and Oncology 2002;37:34‐7. [DOI] [PubMed] [Google Scholar]
- Littlewood TJ, Bajetta E, Nortier JW, Vercammen E, Rapoport B. Effects of epoetin alfa on hematologic parameters and quality of life in cancer patients receiving non‐platinum chemotherapy: Results of a randomized, double‐blind, placebo‐controlled trial. Journal of Clinical Oncology 2001;19(11):2865‐74. [DOI] [PubMed] [Google Scholar]
- Littlewood TJ, Cella D, Nortier JW. Erythropoietin improves quality of life. Lancet Oncology 2002;3(8):459‐60. [DOI] [PubMed] [Google Scholar]
- Littlewood TJ, Kallich JD, San Miguel J, Hendricks L, Hedenus M. Efficacy of darbepoetin alfa in alleviating fatigue and the effect of fatigue on quality of life in anemic patients with lymphoproliferative malignancies. Journal of Pain & Symptom Management 2006;31(4):317‐25. [DOI] [PubMed] [Google Scholar]
- Littlewood TJ, Nortier J, Rapoport B, Pawlicki M, Wasch G, Vercammen E, et al. Epoetin alfa corrects anemia and improves quality of life in patients with hematologic malignancies receiving non‐platinum chemotherapy. Hematological Oncology 2003;21(4):169‐80. [DOI] [PubMed] [Google Scholar]
- Martin SC, Gagnon DD, Zhang L, Bokemeyer C, Marwijk KM, Hout B. Cost‐utility analysis of survival with epoetin‐alfa versus placebo in stage IV breast cancer. Pharmacoeconomics 2003;21(16):1153‐69. [DOI] [PubMed] [Google Scholar]
Littlewood 2001 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Littlewood 2001 J&J 2004 {published data only}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD Report Date: 30 MARCH 2004.
Machtay 2007 {published and unpublished data}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
- Luksenburg H, Weir A, Wager R. Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen, Inc. and Procrit (epoetin alfa) Ortho Biotech, L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. FDA Briefing Document May 4, 2004 Oncologic Drugs Advisory Committee.
- Machtay M, Pajak T, Suntharalingam M, Hershock D, Stripp DC, Cmelak A, et al. Definitive radiotherpay +/‐ erythropoietin for squamous cell carcinoma of the head and neck: preliminary report of RTOG 99‐03. International Journal of Radiation Oncology, Biology, Physics. 2004; Vol. 60 (Suppl 1):S132.
- Machtay M, Pajak TF, Suntharalingam M, Shenouda G, Hershock D, Stripp DC, et al. Radiotherapy with or without erythropoietin for anemic patients with head and neck cancer: a randomized trial of the Radiation Therapy Oncology Group (RTOG 99‐03). International Journal of Radiation Oncology, Biology, Physics 2007;69(4):1008‐17. [DOI] [PubMed] [Google Scholar]
Machtay 2007 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Milroy 2003 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Milroy 2011 {published data only}
- Milroy R, Bajetta E, Berg PM, O'Brien MER, Perez‐Manga G, Georgoulias V, et al. Effects of epoetin alfa on anemia and patient‐reported outcomes in patients with non‐small cell lung cancer receiving chemotherapy: Results of a European, multicenter, randomized, controlled study. European Journal of Clinical and Medical Oncology 2011;3(2):49‐56. [Google Scholar]
ML17616 2006 {published data only}
- Multicenter, open label study of NeoRecormon treatment for anemia in adult patients with multiple myeloma, low grade non‐Hodgkin's lymphoma or chronic lymphocytic leukemia who have a relatively erythropoietin deficiency and are receiving anti‐tumor chemotherapy: ML17616 [Clinical Trial Result Information]. Shanghai, China:Shanghai Roche Pharmaceuticals Ltd; 2006 Vol. available: http://www.centerwatch.com/clinical‐trials/listings/studydetails.aspx?StudyID=97120; accessed: 30.09.09.
ML17620 2006 {published data only}
- Multicenter, open label study of NeoRecormon prevention and treatment for anemia in adult patients withsolid tumors and treated with platinum‐based chemotherapy prone to induce anemia. Study: ML17620 [Clinical Trial Result Information]. Shanghai, China:Shanghai Roche Pharmaceuticals Ltd; 2006 Vol. available: http://www.centerwatch.com/clinical‐trials/results/db/stur10331.html; accessed: 30.09.09.
Moebus 2007 {published and unpublished data}
- Moebus V, Bastert G, Kreienberg R, Eidtmann H, Cierna M, Untch M, et al. Epoetin Alpha Prevents Anemia and Transfusions of RBCS in Patients Receiving Dose‐Dense Sequential Chemotherapy. Proceedings of the American Society of Clinical Oncology 2001; Vol. 20:abstract 36.
- Moebus V, Lueck H, Thomssen C, Harbeck N, Nitz U, Kreienberg R, et al. The impact of epoetin‐alpha on anemia, red blood cell (RBC) transfusions, and survival in breast cancer patients (pts) treated with dose‐dense sequential chemotherapy: Mature results of an AGO phase III study (ETC trial). Journal of Clinical Oncology 2007; Vol. 25, issue 18 Suppl:569.
- Moebus V, Untch M, du Bois A, Lueck HJ, Thomssen C, Kuhn W, et al. Dose‐dense sequential chemotherapy with epirubicin(E), paclitaxel (T) and cyclophosphamide (C) (ETC) is superior to conventional dosed chemotherapy in high‐risk breast cancer patients (>= 4 +LN). First results of an AGO‐trial. Journal of Clinical Oncology 2004; Vol. 22, issue 14 Suppl:abstract 513.
- Untch M, Jackisch C, Lenhard MS, du Bois A, Lueck HJ, Thomssen C, et al. Epoetin‐alpha reduces red blood cell transfusions (RBC) in high‐risk breast cancer patients with adjuvant dose‐dense, sequential chemotherapy with epirubicin (E), paclitaxel (T) and cyclophosphamide (C) (ETC). Journal of Clinical Oncology 2005; Vol. 23, issue 16 Suppl:613.
Moebus 2007 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moebus 2007 J&J 2007 {published and unpublished data}
- Amgen Inc with contributions from Johnson & Johnson Pharmaceutical Research and Development, L.L.C. Safety of Erythropoiesis‐Stimulating Agents (ESAs) in Oncology). Background information for Oncologic Drugs Advisory Committee 10 May 2007.
Mystakidou 2005 {published data only}
- Mystakidou K, Kalaidopoulou O, Katsouda E, Parpa E, Kouskouni E, Chondros C, et al. Evaluation of epoetin supplemented with oral iron in patients with solid malignancies and chronic anemia not receiving anticancer treatment. Anticancer Research 2005;25(5):3495‐500. [PubMed] [Google Scholar]
O'Shaughnessy 2005 {published and unpublished data}
- O'Shaughnessy JA, Vukelja SJ, Holmes FA, Savin M, Jones M, Royall D, et al. Feasibility of quantifying the effects of epoetin alfa therapy on cognitive function in women with breast cancer undergoing adjuvant or neoadjuvant chemotherapy. Clinical Breast Cancer 2005;5(6):439‐46. [DOI] [PubMed] [Google Scholar]
- O'Shaugnessy J, Vukelja S, Savin M, Holmes FA, Jones M, Royall D, et al. Effects of epoetin alfa (Procrit) on cognitive function, mood, asthenia, and quality of life in women with breast cancer undergoing adjuvant or neoadjuvant chemotherapy: a double‐blind, randomized, placebo‐controlled trial. Proceedings of the American Society of Clinical Oncology 2002:abstract 1449.
O'Shaugnessy 2005 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
OBE/EPO‐INT‐03 IPD {published and unpublished data}
- Anonymous. A placebo‐controlled study on the effect of epoetin alfa in patients with malignancy receiving chemotherapy. Raritan (NJ): Johnson and Johhnson Pharmaceutical Research and Development. Available at www.clinicaltrials.gov/ct2/show/NCT00270166 2005..
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oberhoff 1998 {published and unpublished data}
- Neorecormon (epoetin beta). Briefing package or the FDA Oncologic Advisory Committee Meeting, May 4, 2004 Vol. RO 205‐3859.
- Ehmer B, Schrenk U, Franks W, Quardor O, Messinger D. Clinical efficacy of epoetin beta (EPO) in the correction of chemotherapy (CT) induced anemia in patients with solid cancer: a randomized controlled clinical trial. Annals of Oncololgy. 1996; Vol. 7 (Suppl 5):A2960.
- Oberhoff C, Krumeich B, Winkler UH, Hoffmann O, Schindler AE. Recombinant human erythropoietin (epoetin beta) in the treatment of chemotherapy ‐ associated anaemia: effects on blood coagulation and fibrinolysis in patients with gynecological malignancies. Annals of Hematology 2000; Vol. 79 Suppl 3:B16.
- Oberhoff C, Neri B, Amadori D, Petry KU, Gamucci T, Rebmann U, et al. Recombinant human erythropoietin in the treatment of chemotherapy‐ induced anemia and prevention of transfusion requirement associated with solid tumors: a randomized, controlled study. Annals of Oncology 1998;9(3):255‐60. [DOI] [PubMed] [Google Scholar]
- Oberhoff C, Stauch M, Wilhelm G, Musch E, Heinrich B, Neise M, et al. Prevention and therapy of anemia in tumor patients with Epoetin beta (NeoRecormon). Tumor Diagnostik und Therapie 2005;26(4):166‐71. [Google Scholar]
Oberhoff 1998 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Osterborg 1996 {published and unpublished data}
- Neorecormon (epoetin beta). Briefing package or the FDA Oncologic Advisory Committee Meeting, May 4, 2004 Vol. RO 205‐3859.
- Osterborg A, Boogaerts MA, Cimino R, Essers U, Holowiecki J, Juliusson G, et al. Recombinant human erythropoietin in transfusion‐dependent anemic patients with multiple myeloma and non‐Hodgkin's lymphoma‐‐a randomized multicenter study. Blood 1996;87(7):2675‐82. [PubMed] [Google Scholar]
Osterborg 1996a {published and unpublished data}
- Osterborg A, Boogaerts MA, Cimino R, Essers U, Holowiecki J, Juliusson G, et al. Recombinant human erythropoietin in transfusion‐dependent anemic patients with multiple myeloma and non‐Hodgkin's lymphoma‐‐a randomized multicenter study. Blood 1996;87(7):2675‐82. [PubMed] [Google Scholar]
Osterborg 1996b {published and unpublished data}
- Osterborg A, Boogaerts MA, Cimino R, Essers U, Holowiecki J, Juliusson G, et al. Recombinant human erythropoietin in transfusion‐dependent anemic patients with multiple myeloma and non‐Hodgkin's lymphoma‐‐a randomized multicenter study. Blood 1996;87(7):2675‐82. [PubMed] [Google Scholar]
Osterborg 1996 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Osterborg 2002 {published and unpublished data}
- Neorecormon (epoetin beta). Briefing package or the FDA Oncologic Advisory Committee Meeting, May 4, 2004 Vol. RO 205‐3859.
- Osterborg A, Brandberg Y, Hedenus M. Impact of epoetin‐ß on survival of patients with lymphoproliferative malignancies: long‐term follow up of a large randomized study. British Journal of Haematology 2005;129:206‐9. [DOI] [PubMed] [Google Scholar]
- Osterborg A, Brandberg Y, Hedenus M. Impact of epoetin‐ß on survival of patients with lymphoproliferative malignanices: long‐term follow up of a large randomized study. British Journal of Haematology 2005;129:206‐9. [DOI] [PubMed] [Google Scholar]
- Osterborg A, Brandberg Y, Molostova V, Iosava G, Abdulkadyrov K, Hedenus M, et al. Randomized, double‐blind, placebo‐controlled trial of recombinant human erythropoietin, epoetin Beta, in hematologic malignancies. Journal of Clinical Oncology 2002;20(10):2486‐94. [DOI] [PubMed] [Google Scholar]
Osterborg 2002 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Overgaard 2009 {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambin P, Ramaekers BLT, Mastrigt GAPG, Ende P, Jong J, Ruysscher DKM, et al. Erythropoietin as an adjuvant treatment with (chemo) radiation therapy for head and neck cancer. Cochrane Database of Systematic Reviews 2009, Issue 3, Art. No.: CD006158. [DOI: 10.1002/14651858.CD006158.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overgaard J. Interim Analysis of DAHANCA 10. http://www.dahanca.dk/get_media_file.php?mediaid=125 [accessed April 1, 2009] 2006, Dec 1.
- Overgaard J Sr, Hoff CM, Hansen HS, Specht L, Overgaard M, Grau C et al and Danish Head and Neck Cancer Group (DAHANCA). Randomized study of darbepoetin alfa as modifier of radiotherapy in patients with primary squamous cell carcinoma of the head and neck (HNSCC): Final outcome of the DAHANCA 10 trial. ASCO Meeting Abstracts 2009;27:6007. [Google Scholar]
- Overgaard J, Hoff C, Sand Hansen H, Specht L, Overgaard M, Grau C, et al. Randomized study of the importance of Novel Erythropoiesis Stimulating Protein (Aranesp®) for the effect of radiotherapy in patients with primary squamous cell carcinoma of the head and neck (HNSCC) ‐ the Danish Head and Neck Cancer Group DAHANCA 10 randomized trial. European Journal of Cancer Supplements 2007; Vol. 5:abstract 6LB.
P‐174 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
P‐174 J&J 2004 {published and unpublished data}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
- Luksenburg H, Weir A, Wager R. P‐174 in: Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen, Inc. and Procrit (epoetin alfa) Ortho Biotech, L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Oncologic Drugs Advisory Committee Rockville (MD), USA, 2004; Vol. http://www.fda.gov/ohrms/dockets/ac/04/briefing/4037b2_04.pdf [date of last access March 27, 2009].
- Pangalis GA, Poziopoulos C, Angelopoulou MK, Siakantaris MP, Panayiotidis P. Effective treatment of disease‐related anaemia in B‐chronic lymphocytic leukaemia patients with recombinant human erythropoietin. British Journal of Haematology 1995;89(3):627‐9. [DOI] [PubMed] [Google Scholar]
Pirker 2008 {published and unpublished data}
- Amgen. Aranesp(R) ``145 Study'' Shows No Difference in Survival in Patients with Small‐Cell Lung Cancer. Amgen Thousand Oaks, CA, 2007; Vol. http://wwwext.amgen.com/media/media_pr_detail.jsp?year=2007&releaseID=987476 [date of last access April 28, 2009].
- Pirker R, Ramlau RA, Schuette W, Zatloukal P, Ferreira I, Lillie T, et al. Safety and efficacy of darbepoetin alpha in previously untreated extensive‐stage small‐cell lung cancer treated with platinum plus etoposide. Journal of Clinical Oncology 2008;26(14):2342‐9. [DOI] [PubMed] [Google Scholar]
Pirker 2008 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pronzato 2010 {published data only}
- Pronzato P, Cortesi E, Rijt C, Moreno‐Nogueria A, Raimundo D, Ostler P, et al. Early intervention with epoetin alfa in breast cancer (BC) patients (pts) undergoing chemotherapy (CT): results of a randomized, multicenter, phase IIIb study (EPO‐INT‐47 Study Group). Annals of Oncology 2002; Vol. 13, issue Suppl 5:168.
- Pronzato P, Cortesi E, Rijt CC, Bols A, Moreno‐Nogueira JA, Oliveira CF, et al. Epoetin alfa improves anemia and anemia‐related, patient‐reported outcomes in patients with breast cancer receiving myelotoxic chemotherapy: results of a European, multicenter, randomized, controlled trial. Oncologist 2010;15(9):935‐43. [22233] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pronzato 2010 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Quirt 1996 {published and unpublished data}
- Quirt I, Micucci S, Moran LA, Pater J, Browman G. The role of recombinant human erythropoietin (EPO) in reducing red blood cell transfusions and maintaining quality of life (QOL) in patients with lymphoma and solid tumors receiving cytotoxic chemotherapy. Results of a randomized, double‐blind, placebo‐controlled clinical trial. Blood 1996;88(10 (Suppl 1)):347a. [Google Scholar]
Quirt 1996 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ray‐Coquard 2009 {published and unpublished data}
- Ray‐Coquard I, Dussart S, Goillot C, Mayeur D, Debourdeau P, Ghesquieres H, et al. A risk model for severe anemia to select cancer patients for primary prophylaxis with epoetin {alpha}: a prospective randomized controlled trial of the ELYPSE study group. Annals of Oncology 2009, issue doi:10.1093/annonc/mdn750. [DOI] [PubMed]
- Ray‐Coquard I, Perol D, Debourdeau P, Chabaud S, Chelghoum M, Mayeur D, et al. ELYPSE 4: A prospective randomized trial comparing Epo A in primary prophylaxis of severe anemia requiring red cells transfusion in high risk patients. Annals of Oncology 2006;17(Suppl 9):ix294. [Google Scholar]
Ray‐Coquard 2009 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Razzouk 2004 {published data only}
Razzouk 2006 {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds PS, Hockenberry M, Feusner J, Hord JD, Rackoff W, Rozzouk BI. Hemoglobin response and improvements in quality of life in anemic children with cancer receiving myelosuppressive chemotherapy. Journal of Supportive Oncology 2005;3(6 Suppl 4):10‐1. [PubMed] [Google Scholar]
- Razzouk BI, Hockenberry M, Hinds PS, Feusner J, Rackoff W, Hord JD. Influence of hemoglobin response to epoetin alfa on quality‐of‐life in anemic children with cancer receiving myelosuppressive chemotherapy. Blood 2004; Vol. 104, issue 11:abstract 221.
- Razzouk BI, Hord JD, Hockenberry M, Hinds PS, Feusner J, Williams D, et al. Double‐blind, placebo‐controlled study of quality of life, hematologic end points, and safety of weekly epoetin alfa in children with cancer receiving myelosuppressive chemotherapy. Journal of Clinical Oncology 2006;24(22):3583‐9. [DOI] [PubMed] [Google Scholar]
Rose 1994 {published and unpublished data}
- Rose E, Rai K, Revicki D. Clinical and health status assessments in anemic chronic lymphocytic leukemia (CLL) patients treated with epoetin alfa (EPO). Blood 1994;84(10 (Suppl 1)):526a. [Google Scholar]
Rose 1994 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rose 1994 J&J 2004 {published data only}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Rosen 2003 {published data only}
- Rosen FR, Haraf DJ, Kies MS, Stenson K, Portugal L, List MA, et al. Multicenter randomized Phase II study of paclitaxel (1‐hour infusion), fluorouracil, hydroxyurea, and concomitant twice daily radiation with or without erythropoietin for advanced head and neck cancer. Clinical Cancer Research 2003;9(5):1689‐97. [MEDLINE: ] [PubMed] [Google Scholar]
Rosenzweig 2004 {published data only}
- Rosenzweig MQ, Bender CM, Lucke JP, Yasko JM, Brufsky AM. The decision to prematurely terminate a trial of R‐HuEPO due to thrombotic events. Journal of Pain & Symptom Management 2004;27(2):185‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Savonije 2005 {published data only}
- Savonije J, Groeningen C, Bochove A, Pinedo H, Giaccone G. Early intervention with epoetin‐alfa during platinum‐based chemotherapy. Journal of Clinical Oncology. 2004; Vol. 22, issue 14S:#8111.
- Savonije JH, Groeningen CJ, Bochove A, Honkoop AH, Felius CL, Wormhoudt LW, et al. Effects of early intervention with epoetin alfa on transfusion requirement, hemoglobin level and survival during platinum‐based chemotherapy: Results of a multicenter randomised controlled trial. European Journal of Cancer 2005;41(11):1560‐9. [DOI] [PubMed] [Google Scholar]
- Savonije JH, Groeningen CJ, Wormhoudt LW, Giaccone G. Early Intervention with epoetin alfa during platinum‐based chemotherapy: an analysis of quality‐of‐life results of a multicenter, randomized, controlled trial compared with population normative data. The oncologist 2006;11(2):197‐205. [DOI] [PubMed] [Google Scholar]
Savonije 2005 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Silvestris 1995 {published data only}
- Silvestris F, Romito A, Fanelli P, Vacca A, Dammacco F. Long‐term therapy with recombinant human erythropoietin (rHu‐EPO) in progressing multiple myeloma. Annals of Hematology 1995;70:313‐8. [DOI] [PubMed] [Google Scholar]
Smith 2003 {published data only}
- Smith RE, Tchekmedyian NS, Chan D, Meza LA, Northfelt DW, Patel R, et al. A dose‐ and schedule‐finding study of darbepoetin alpha for the treatment of chronic anaemia of cancer. British Journal of Cancer 2003;88(12):1851‐8. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2003a {published data only}
- Smith RE, Tchekmedyian NS, Chan D, Meza LA, Northfelt DW, Patel R, et al. A dose‐ and schedule‐finding study of darbepoetin alpha for the treatment of chronic anaemia of cancer. British Journal of Cancer 2003;88(12):1851‐8. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2003 Amgen 2007 {published data only}
- Amgen Inc with contributions from Johnson & Johnson Pharmaceutical Research and Development, L.L.C. Safety of Erythropoiesis‐Stimulating Agents (ESAs) in Oncology). Background information for Oncologic Drugs Advisory Committee 10 May 2007.
Smith 2003b {published data only}
- Smith RE, Tchekmedyian NS, Chan D, Meza LA, Northfelt DW, Patel R, et al. A dose‐ and schedule‐finding study of darbepoetin alpha for the treatment of chronic anaemia of cancer. British Journal of Cancer 2003;88(12):1851‐8. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2003c {published data only}
- Smith RE, Tchekmedyian NS, Chan D, Meza LA, Northfelt DW, Patel R, et al. A dose‐ and schedule‐finding study of darbepoetin alpha for the treatment of chronic anaemia of cancer. British Journal of Cancer 2003;88(12):1851‐8. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2008 {published and unpublished data}
- 20010103. Continuing reassessment of the risks of erythropoiesis‐stimulating agents (ESAs) administered for the treatment of anemia associated with cancer chemotherapy. Department of Health and Human Services, Food and Drugs Administration, Center for Drug Evaluation and Research, Oncologic Drugs Advisory Committee, Rockville (MD), USA, 2007; Vol. http://www.fda.gov/ohrms/dockets/ac/07/briefing/2007‐4301b2‐02‐ FDA.pdf.
- Glaspy J, Smith RE, Aapro M, Ludwig H, Pinter T, Smakal M, et al. Results from a phase 3 randomized, double blind, placebo controlled study of darbepoetin alfa for the treatment of anemia in cancer patients not receiving chemotherapy or radiotherapy. Haematologica 2007; Vol. 92, issue Suppl 1:136. [DOI] [PubMed]
- Smith RE, Aapro MS, Ludwig H, Pinter T, Smakal M, Ciuleanu TE, et al. Darbepoetin alpha for the treatment of anemia in patients with active cancer not receiving chemotherapy or radiotherapy: results of a phase III, multicenter, randomized, double‐blind, placebo‐controlled study. Journal of Clinical Oncology 2008;26(7):1040‐50. [DOI] [PubMed] [Google Scholar]
Smith 2008 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Strauss 2008 {published and unpublished data}
- Strauss H, Haendgen G, Dunst.J, Koelbl H. Effects of anaemia correction with epoetin beta in patients with advanced cervical cancer. Proceedings of the American Society of Clinical Oncology 2003:abstract 5121.
- Strauss HG, Haendgen G, Dunst J, Haywrad CRW, Burger HU, Scherhag A, et al. Effects of anemia correction with epoetin beta in patients receiving radiochemotherapy for advanced cervical cancer. International Journal of Gynecological Cancer 2008;18(Suppl 3):515‐24. [DOI] [PubMed] [Google Scholar]
Strauss 2008 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Suzuki 2008 {published data only}
- Suzuki Y, Tokuda Y, Okamoto R, Nakagawa K, Ando K, Iwata H, et al. Randomized, placebo‐controlled phase II study of darbepoetin alfa (DA) administered every three weeks (Q3W) in patients with chemotherapy‐induced anemia (CIA). Annals of Oncology 2008;19(S8):viii277. [Google Scholar]
Suzuki 2008a {published data only}
- Suzuki Y, Tokuda Y, Okamoto R, Nakagawa K, Ando K, Iwata H, et al. Randomized, placebo‐controlled phase II study of darbepoetin alfa (DA) administered every three weeks (Q3W) in patients with chemotherapy‐induced anemia (CIA). Annals of Oncology 2008;19(S8):viii277. [Google Scholar]
Suzuki 2008b {published data only}
- Suzuki Y, Tokuda Y, Okamoto R, Nakagawa K, Ando K, Iwata H, et al. Randomized, placebo‐controlled phase II study of darbepoetin alfa (DA) administered every three weeks (Q3W) in patients with chemotherapy‐induced anemia (CIA). Annals of Oncology 2008;19(S8):viii277. [Google Scholar]
Sweeney 1998 {published data only}
- Sweeney PJ, Nicolae D, Ignacio L, Chen L, Roach M, Wara W, et al. Effect of subcutaneous recombinant human erythropoietin in cancer patients receiving radiotherapy: final report of a randomized, open‐ labelled, phase II trial. British Journal of Cancer 1998;77(11):1996‐2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayakumar S, Roach M, Wara W, Chan SK, Ewing C, Rubin S. Effect of subcutaneous recombinant human erythropoietin in cancer patients receiving radiotherapy: preliminary results of a randomized, open‐labeled, phase II trial. International Journal of Radiation Oncology, Biology and Physics 1993;26:721‐9. [DOI] [PubMed] [Google Scholar]
Ten Bokkel 1998 {published and unpublished data}
- Neorecormon (epoetin beta). Briefing package or the FDA Oncologic Advisory Committee Meeting, May 4, 2004 Vol. RO 205‐3859.
- Reed N, Rhan S, Hayward C, Burger H, Bokkel Huinink W. Impact of epoetin beta on the survival of anemic patients with ovarian cancer receiving platinum‐based chemotherapy. Proceedings of the American Society of Clinical Oncology 2003; Vol. 23, issue 16s:abstract 5102.
- Bokkel Huinink WW, Swart CAM, Toorn DW, et al. Controlled multicentre study of the influence of subcutaneous recombinant human erythropoietin on anaemia and transfusion dependency in patients with ovarian carcinoma treated with platinum‐based chemotherapy. Medical Oncology 1998;15(3):174‐82. [DOI] [PubMed] [Google Scholar]
Ten Bokkel 1998a {published and unpublished data}
- Bokkel Huinink WW, Swart CAM, Toorn DW, et al. Controlled multicentre study of the influence of subcutaneous recombinant human erythropoietin on anaemia and transfusion dependency in patients with ovarian carcinoma treated with platinum‐based chemotherapy. Medical Oncology 1998;15(3):174‐82. [DOI] [PubMed] [Google Scholar]
Ten Bokkel 1998b {published and unpublished data}
- Bokkel Huinink WW, Swart CAM, Toorn DW, et al. Controlled multicentre study of the influence of subcutaneous recombinant human erythropoietin on anaemia and transfusion dependency in patients with ovarian carcinoma treated with platinum‐based chemotherapy. Medical Oncology 1998;15(3):174‐82. [DOI] [PubMed] [Google Scholar]
Ten Bokkel1998 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thatcher 1999 {published and unpublished data}
- Campos E, Radford J, Steward, Milroy R, Dougal M, Swindell R, et al. Clinical and and in vitro effects of recombinant human erythropoietin in patients receiving intensive chemotherapy for small‐cell lung cancer. Journal of Clinical Oncology 1995;13(7):1623‐31. [DOI] [PubMed] [Google Scholar]
- Thatcher N, Campos ES, Bell DR, Steward WP, Varghese G, Morant R, et al. Epoetin alpha prevents anaemia and reduces transfusion requirements in patients undergoing primarily platinum‐based chemotherapy for small cell lung cancer. British Journal of Cancer 1999;80(3‐4):396‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thatcher 1999a {published and unpublished data}
- Thatcher N, Campos ES, Bell DR, Steward WP, Varghese G, Morant Ret al. Epoetin alpha prevents anaemia and reduces transfusion requirements in patients undergoing primarily platinum‐based chemotherapy for small cell lung cancer. British Journal of Cancer 1999;80(3‐4):396‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thatcher 1999b {published and unpublished data}
- Thatcher N, Campos ES, Bell DR, Steward WP, Varghese G, Morant R, et al. Epoetin alpha prevents anaemia and reduces transfusion requirements in patients undergoing primarily platinum‐based chemotherapy for small cell lung cancer. British Journal of Cancer 1999;80(3‐4):396‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thatcher 1999 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2002 {published and unpublished data}
- Thomas H, McAdam KF, Thomas RJ, Joffe JK, Sugden EM, Awwad ST, et al. Early intervention with epoetin alfa for treatment of anaemia and improvement of quality of life in cancer patients undergoing myelotoxic chemotherapy. Annals of Oncology. 2002; Vol. 13 (Suppl 5):177, #653P.
Thomas 2002 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2008 {published and unpublished data}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
- Luksenburg H, Weir A, Wager R. GOG‐191: Safety concerns associated with Aranesp (darbepoetin alfa) Amgen Inc. and Procrit (epoetin alfa) Ortho Biotech L.P., for the treatment of Anemia Associated with Cancer Chemotherapy. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Oncologic Drugs Advisory Committee, Rockville (MD), USA, 2004; Vol. http://www.fda.gov/ohrms/dockets/ac/04/briefing/4037b2_04.pdf [date of last access March 27, 2009].
- Thomas G, Ali S, Hoebers FJP, Darcy KM, Rodgers WH Patel M, et al. Phase III trial to evaluate the efficacy of maintaining hemoglobin levels above 12.0 g/dL with erythropoietin vs above 10.0 g/dL without erythropoietin in anemic patients receiving concurrent radiation and cisplatin for cervical cancer. Gynecologic Oncology 2008;108(2):317‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2008 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2008 J&J 2004 {published and unpublished data}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Thompson 2000 {published and unpublished data}
- Thompson JA, Gilliland DG, Prchal JT, Bennett JM, Larholt K, Nelson RA, et al. Effect of recombinant human erythropoietin combined with granulocyte/macrophage colony‐stimulating factor in the treatment of patients with myelodysplastic syndrome. Blood 2000;95:1175‐9. [PubMed] [Google Scholar]
Throuvalas 2000 {published and unpublished data}
- Throuvalas NA, Antonadou D, Boufi M, Lavey R Malamos N. Erythropoietin decreases transfusion requirements during radiochemotherapy. Proceedings of the American Society of Clinical Oncologists 2000;19:Abstract 1558. [Google Scholar]
Tjulandin 2010 {published data only}
- Tjulandin SA, Bias P, Elsässer R, Gertz B, Kohler E, Buchner A. Epoetin theat in anaemic cancer patients receiving platinum‐based chemotherapy: a randomised controlled trial.. Archives of Drug Information 2010;3:45‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tjulandin 2010a {published data only}
- Tjulandin SA, Bias P, Elsässer R, Gertz B, Kohler E, Buchner A. Epoetin theat in anaemic cancer patients receiving platinum‐based chemotherapy: a randomised controlled trial.. Archives of Drug Information 2010;3:45‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tjulandin 2010b {published data only}
- Tjulandin SA, Bias P, Elsässer R, Gertz B, Kohler E, Buchner A. Epoetin theat in anaemic cancer patients receiving platinum‐based chemotherapy: a randomised controlled trial.. Archives of Drug Information 2010;3:45‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tjulandin 2011 {published data only}
- Buchner A, Bias P. Epoetin theta shows efficacy and safety in a placebo controlled, randomized phase III study in cancer patients receiving non‐platinum chemotherapy. Onkologie 2009;32(Supplement 4):88, Abstract V348. [Google Scholar]
- Tjulandin SA, Bias P, Elsässer R, Gertz B, Kohler E, Buchner A. Epoetin theta with a new dosing schedule in anaemic cancer patients receiving nonplatinum‐based chemotherapy: a randomised controlled trial. Archives of Drug Information 2011;4(3):33‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsuboi 2009 {published data only}
- Tsuboi M, Ezaki K, Tobinai K, Ohashi Y, Saijo N. Weekly administration of epoetin beta for chemotherapy‐induced anemia in cancer patients: results of a multicenter, Phase III, randomized, double‐blind, placebo‐controlled study. Japanese Journal of Clinical Oncology 2009;39(3):163‐8. [DOI] [PubMed] [Google Scholar]
- Watanabe M, Ezaki K, Tobinai K, Tsuboi M, Ohashi Y, Hirashima K, et al. A multicenter phase III randomized, double‐blind placebo‐controlled study of Epoetin beta administered once‐weekly for chemotherapy induced anemia (CIA) in cancer patients: Japan Erythropoietin Study Group. Annals of Oncology 2006; Vol. 17, issue Suppl 9:294.
Untch 2008 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Untch 2011_1 {published data only}
- Untch M, Fasching PA, Konecny GE, Koch F, Conrad U, Fett W, Kurzeder C, et al. PREPARE trial: A randomized phase III trial comparing preoperative, dose‐dense, dose‐intensified chemotherapy with epirubicin, paclitaxel and CMF versus a standard‐dosed epirubicin/cyclophosphamide followed by paclitaxel (plus or minus) darbepoetin alfa in primary breast cancer‐results at the time of surgery. Annals of Oncology 2011;22(9):1988‐98. [DOI] [PubMed] [Google Scholar]
- Untch M, Fascing PA, Bauernfeind I, Conrad U, Camara O, Fett W, et al. PREPARE trial. A randomized phase III trial comparing preoperative, dose‐dense, dose‐intensified chemotherapy with epirubicin, paclitaxel and CMF with a standard dosed epirubicin/cyclophosphamide followed by paclitaxel +/‐ darbepoetin alfa in primary breast cancer: A preplanned interim analysis of efficacy at surgery. Journal of Clinical Oncology 2008; Vol. 26, issue Suppl:abstract 517.
Untch 2011_2 {published data only}
- Untch M, Fascing PA, Bauernfeind I, Conrad U, Camara O, Fett W, et al. PREPARE trial. A randomized phase III trial comparing preoperative, dose‐dense, dose‐intensified chemotherapy with epirubicin, paclitaxel and CMF with a standard dosed epirubicin/cyclophosphamide followed by paclitaxel +/‐ darbepoetin alfa in primary breast cancer: A preplanned interim analysis of efficacy at surgery. Journal of Clinical Oncology 2008; Vol. 26, issue Suppl:abstract 517.
- Untch M, Minckwitz G, Konecny GE, Conrad U, Fett W, Kurzeder C, et al. PREPARE trial: A randomized phase III trial comparing preoperative, dose‐dense, dose‐intensified chemotherapy with epirubicin, paclitaxel and CMF versus a standard‐dosed epirubicin/cyclophosphamide followed by paclitaxel with or without darbepoetin alfa in primary breast cancer‐outcome on prognosis. Annals of Oncology 2011;22(9):1999‐2006. [69960] [DOI] [PubMed] [Google Scholar]
Vansteenkiste 02 FDA 2004 {published and unpublished data}
- Luksenburg H, Weir A, Wager R. Safety Concerns Associated with Aranesp(darbepoetin alfa) Amgen, Inc. and Procrit(epoetin alfa) Ortho Biotech, L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. FDA Briefing Document May 4, 2004 Oncologic Drugs Advisory Committee.
Vansteenkiste 2002 {published and unpublished data}
- Amgen Inc. Aranesp® (darbepoetin alfa) safety. Oncologic Drugs Advisory Committee, 4 May 2004.
- Kallich JD, Tchekmedyian NS, Damiano AM, Shi J, Black JT, Erder MH. Psychological outcomes associated with anemia‐related fatigue in cancer patients. Oncology (Huntingt) 2002;16(9 Suppl 10):117‐24. [PubMed] [Google Scholar]
- Pirker R, Vansteenkiste J, Gateley J, Yates P, Colowick A, Musil J. A phase 3, double‐blind, placebo‐controlled, randomized study of novel erythropoiesis stimulating protein (NESP) in patients undergoing platinum treatment for lung cancer. Proceedings of the American Society of Clinical Oncology 2001; Vol. 20:abstract 1572.
- Tchekmedyian NS, Kallich J, McDermott A, Fayers P, Erder MH. The relationship between psychologic distress and cancer‐related fatigue. Cancer 2003;98(1):198‐203. [DOI] [PubMed] [Google Scholar]
- Tchekmedyian S, Glaspy J, Colowick A, Tomita D, Rossi G. Effect of darbepoetin alfa and recombinant human erythropoietin (rHuEPO) on early hemoglobin (Hb) changes in anemic cancer patients (pts). Annals of Oncology 2002; Vol. 13, issue Suppl 5:184.
- Vansteenkiste J, Pirker R, Massuti B, Barata F, Font A, Fiegl M, et al. Double‐blind, placebo‐controlled, randomized phase III trial of darbepoetin alfa in lung cancer patients receiving chemotherapy.[see comment]. Journal of the National Cancer Institute 2002;94(16):1211‐20. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Vansteenkiste J, Poulsen E, Rossi G, Glaspy J. Darbepoetin alfa: impact on treatment for chemotherapy‐induced anemia and considerations in special populations. Oncology (Huntingt) 2002;16(10 Suppl 11):45‐55. [PubMed] [Google Scholar]
- Vansteenkiste J, Tomita D, Rossi G, Pirker R. Darbepoetin alfa in lung cancer patients on chemotherapy: a retrospective comparison of outcomes in patients with mild versus moderate‐to‐severe anaemia at baseline. Supportive Care in Cancer 2004;12(4):253‐62. [DOI] [PubMed] [Google Scholar]
Vansteenkiste 2002 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Welch 1995 {published data only}
- James RD, Wilkinson PM, Belli F, Welch R, Cowan R. Recombinant human erythropoietin in patients with ovarian carcinoma and anaemia secondary to cisplatin and carboplatin chemotherapy: preliminary results. Acta Haematologica 1992;87 (Suppl 1):12‐5. [DOI] [PubMed] [Google Scholar]
- Welch RS, James RD, Wilkinson PM, et al. Recombinant human erythropoietin and platinum‐based chemotherapy in advanced ovarian cancer. Cancer Journal of the Scientific American 1995;1(4):261. [PubMed] [Google Scholar]
Wilkinson 2006 {published and unpublished data}
- Wilkinson PM, Antonopoulos M, Lahousen M, Lind M, Kosmidis P, Epo INT. Epoetin alfa in platinum‐treated ovarian cancer patients: results of a multinational, multicentre, randomised trial. British Journal of Cancer 2006;94(7):947‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilkinson 2006 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Winquist 2009 {published data only}
- Winquist E, Julian JA, Moore MJ, Nabid A, Sathya J, Wood L, et al. Randomized, double‐blind, placebo‐controlled trial of epoetin alfa in men with castration‐resistant prostate cancer and anemia. Journal of Clinical Oncology 2009;27(4):644‐6. [DOI] [PubMed] [Google Scholar]
Witzig 2005 {published and unpublished data}
- Dicato M, Vercammen E, Liu KL, Xiu LX, Bowers P. Relationship of body weight to efficacy of a fixed‐dose regimen of epoetin alfa vs placebo in anemic cancer patients. Haematologica 2005; Vol. 90, issue Suppl 2:abstract 0077.
- Witzig TE, Silberstein PT, Loprinzi CL, Sloan JA, Novotny PJ, Mailliard JA, et al. Phase III, randomized, double‐blind study of epoetin alfa versus placebo in anemic patients with cancer undergoing chemotherapy. Journal of Clinical Oncoogy 2005;23(12):2606‐17. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Witzig 2005 IPD {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Witzig 2005 J&J 2004 {published data only}
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients with Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
Wright 2007 {published and unpublished data}
- Luksenburg H, Weir A, Wager R. EPO‐CAN‐20: Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen Inc and Procrit (epoetin alfa) Ortho Biotech L.P. for the Treatment of Anemia Associated with Cancer Chemotherapy. Oncologic Drugs Advisory Committee, Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Rockville (MD), USA, 2004; Vol. http://www.fda.gov/ohrms/dockets/ac/04/briefing/4037b2_04.pdf [date of last access March 27, 2009].
- Wright JR, Ung YC, Julian JA, Pritchard KI, Whelan TJ, Smith C, et al. Randomized, double‐blind, placebo‐controlled trial of erythropoietin in non‐small‐cell lung cancer with disease‐related anemia. Journal of Clinical Oncology 2007;25(9):1027‐32. [DOI] [PubMed] [Google Scholar]
Wright 2007 IPD {published data only}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wurnig 1996 {published data only}
- Wurnig C, Windhager R, Schwameis E, Kotz R, Zoubek A, Stockenhuber F, et al. Prevention of chemotherapy‐induced anemia by the use of erythropoietin in patients with primary malignant bone tumors (a double‐blind, randomized, phase III study). Transfusion 1996;36(2):155‐9. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Aagaard 2010 {published data only}
- Aagaard AW, Purdy S, Philpott S. Review, Approval, and Marketingof Biosimilars in the United StatesPart 1: Safety and Regulatory Issues. BioProcess International 2010;8(11):12‐20. [Google Scholar]
Aapro 2009 {published data only}
- Aapro M, Osterwalder B, Scherhag A, Burger HU. Epoetin‐beta treatment in patients with cancer chemotherapy‐induced anaemia: the impact of initial haemoglobin and target haemoglobin levels on survival, tumour progression and thromboembolic events. British Journal of Cancer 2009;101(12):1961‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Abdelrazik 2007 {published data only}
- Abdelrazik N, Fouda M. Once weekly recombinant human erythropoietin treatment for cancer‐induced anemia in children with acute lymphoblastic leukemia receiving maintenance chemotherapy: A randomized case‐controlled study. Hematology 2007;12(6):533‐41. [DOI] [PubMed] [Google Scholar]
Abraham 2011 {published data only}
- Abraham J. Eribulin in patients with metastatic breast cancer previously treated with an anthracycline and a taxane. Community Oncology 2011;8(1):15‐7. [Google Scholar]
Adamson 2009 {published data only}
- Adamson JW. Erythropoietic‐stimulating agents: the cancer progression controversy and collateral damage to the blood supply.[comment]. Transfusion 2009;49(5):824‐6. [DOI] [PubMed] [Google Scholar]
Alexopoulos 2004 {published data only}
- Alexopoulos C, Kotsori A. A randomized comparison of rHuEPO with darbepoetin for cancer related anemia. Annals of Oncology 2004;15 Suppl 3:abstract 832P. [Google Scholar]
- Alexopoulos CG KA. A randomized comparison of rHuEPO with darbepoetin for cancer related anemia. Annals of Oncology. 2004; Vol. 15 Suppl 3.
Anonymous 2007 {published data only}
- Anonymous. Erythropoiesis‐stimulating agents: Continued challenges. Journal of Oncology Practice 2007;3(5):248‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Anthony 2011 {published data only}
- Anthony LB, Gabrail NY, Ghazal H, Woytowitz DV, Flam MS, Drelichman A, et al. IV iron sucrose for cancer and/or chemotherapy‐induced anemia in patients treated with erythropoiesisstimulating agents. Community Oncology 2011;8(6):270‐8. [Google Scholar]
Arcasoy 2010 {published data only}
- Arcasoy MO. Non‐erythroid effects of erythropoietin. Haematologica 2010;95(11):1803‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arslan 2004 {published data only}
- Arslan M, Evrensel T, Kurt E, Demiray M, Gonullu G, Kanat O, et al. Comparison of clinical outcomes of different erythropoietin usage strategies. Tumori 2004;90(4):394‐8. [DOI] [PubMed] [Google Scholar]
Auerbach 2004 {published data only}
- Auerbach M, Ballard H, Trout JR, McIlwain M, Ackerman A, Bahrain H, et al. Intravenous iron optimizes the response to recombinant human erythropoietin in cancer patients with chemotherapy‐related anemia: a multicenter, open‐label, randomized trial. Journal of Clinical Oncology 2004;22(7):1301‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Australian 2010 {published data only}
- Australian. Erythropoiesis‐stimulating agents increase mortality in cancer patients. Australian Journal of Pharmacy 2010;91(1076):62. [Google Scholar]
Aziz 2001 {published data only (unpublished sought but not used)}
- Aziz K, Hashem T, Mobarek N, Bary N, Ghoneimy I, Haddad S. Does recombinant human erythropoietin improve the outcome of radiation therapy in head and neck cancer Patients. Proceedings of ASTRO. 2001; Vol. Abstract #2274.
Barosi 1998 {published data only}
- Barosi G, Marchetti M, Liberato NL. Cost‐effectiveness of recombinant human erythropoietin in the prevention of chemotherapy‐induced anaemia. British Journal of Cancer 1998;78(0007‐0920 (Print), 0007‐0920 (Linking), 6):781‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barosi 2011 {published data only}
- Barosi G, Bosi A, Abbracchio MP, Danesi R, Genazzani A, Corradini P, Pane F, Tura S. Key concepts and critical issues on epoetin and filgrastim biosimilars: A position paper from the Italian Society of Hematology, Italian Society of Experimental Hematology, and Italian Group for Bone Marrow Transplantation. Haematologica 2011;96(7):937‐942. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beggs 2003 {published data only}
- Beggs VL, Disalvo WM, Meyer LP, Gragnev KH, Gibson JJ, Hoopes PJ, et al. Fatigue and plasma cytokines in a randomized double‐blind placebo‐controlled trial of epoetin alfa in patients undergoing combined modality therapy for unreseactable non‐small cell lung cancer (NSCLC). Proceedings of the American Society of Clincal Oncology. 2003; Vol. 22:733.
Bell 2008 {published data only}
- Bell D, Grimes D, Gurney H, Dalley D, Blackwell T, Fox R, et al. Outcomes and predicting response in anaemic chemotherapy patients treated with epoetin alfa. A multicentre, 4‐month, open‐label study in Australia and New Zealand. Internal Medicine Journal 2008;38(10):751‐7. [DOI] [PubMed] [Google Scholar]
Bessho 1997 {published data only}
- Bessho M, Hirashima K, Asano S, Ikeda Y, Ogawa N, Tomonaga M, et al. Treatment of the anemia of aplastic anemia patients with recombinant human erythropoietin in combination with granulocyte colony‐stimulating factor: a multicenter randomized controlled study. Multicenter Study Group. European Journal of Haematology 1997;58(4):265‐72. [DOI] [PubMed] [Google Scholar]
Bindi 2004 {published data only}
- Bindi M, Montemaggi M, Sabatino M, Paolelli LPR, Morelli R, Piazza D, et al. Reticulocytes can represent an early indicator of te erythropoietic response to darbepoetin alfa in the anemia by chemotherapy. Journal of Clinical Oncology. 2004; Vol. 22, issue 14S:#8245.
Blayney 2003 {published data only}
- Blayney D, Fesen M, Mirtsching BC, Katz D, Tomita D. Every‐2‐Week Darbepoetin Alfa improves hemoglobin in anemic patients with cancer undergoing chemotherapy: A stratified analysis by tumor type. Blood 2003; Vol. 102 (11):abstract 3779.
Boccia 2007 {published data only}
- Boccia R, Lillie T, Tomita D, Balducci L. The effectiveness of darbepoetin alfa administered every 3 weeks on hematologic outcomes and quality of life in older patients with chemotherapy‐induced anemia. Oncologist. 2007;12(1083‐7159 (Print), 1083‐7159 (Linking), 5):584‐93. [DOI] [PubMed] [Google Scholar]
Borg 2008 {published data only}
- Borg S, Glenngard AH, Osterborg A, Persson U. The cost‐effectiveness of treatment with erythropoietin compared to red blood cell transfusions for patients with chemotherapy induced anaemia: a Markov model. Acta Oncologica 2008;47(6):1009‐17. [DOI] [PubMed] [Google Scholar]
Borget 2008 {published data only}
- Borget I, Chouaid C, Demarteau N, Annemans L, Pujol JL. [Cost‐effectiveness of darbepoetin alpha in an every‐3‐weeks schedule]. [French]. Bulletin du Cancer 2008;95(4):465‐73. [DOI] [PubMed] [Google Scholar]
Bowen 2004 {published data only}
- Bowen D, Hyslop A, Keenan N, Groves M, Culligan D, Johnson P, et al. Prediction of response to recombinant erythropoietin plus granulocyte‐colony stimulating factor following a single subcutaneous bolus in patients with myelodysplastic syndromes; a randomised placebo controlled study. ASH Annual Meeting Abstracts 2004;104(11):1435. [Google Scholar]
Brower 2008 {published data only}
- Brower V. ESAs further restricted, but debate continues. Journal of the National Cancer Institute 2008;100(19):1344‐51. [DOI] [PubMed] [Google Scholar]
Buchler 2011 {published data only}
- Buchler T. [Therapeutic equivalence and effectiveness of Binocrit (HX575) in patients with anemia caused by chemotherapy]. [Czech]. Klinicka Onkologie 2011;24(2):147‐148. [PubMed] [Google Scholar]
Buyukpamukcu 2002 {published data only}
- Buyukpamukcu M, Varan A, Kutluk T, Akyuz C. Is epoetin alfa a treatment option for chemotherapy‐related anemia in children?. Medical and Pediatric Oncology 2002;39(4):455‐8. [DOI] [PubMed] [Google Scholar]
Cabanillas 2012 {published data only}
- Cabanillas ME, Kantarjian H, Thomas DA, Mattiuzz GN, Rytting ME, Bruera E, et al. Epoetin alpha decreases the number of erythrocyte transfusions in patients with acute lymphoblastic leukemia, lymphoblastic lymphoma, and Burkitt leukemia/lymphoma: results of a randomized clinical trial. Cancer 2012;118(3):848‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Candelaria 2005 {published data only}
- Candelaria M, Cetina L, Duenas‐Gonzalez A. Anemia in cervical cancer patients: implications for iron supplementation therapy. Medical Oncology 2005;22(2):161‐8. [DOI] [PubMed] [Google Scholar]
Canon 2006 {published data only}
- Canon JL, Vansteenkiste J, Bodoky G, Mateos MV, Bastit L, Ferreira I, et al. Randomized, double‐blind, active‐controlled trial of every‐3‐week darbepoetin alfa for the treatment of chemotherapy‐induced anemia. Journal of the National Cancer Institute 2006;98(4):273‐84. [DOI] [PubMed] [Google Scholar]
- Canon JL, Vansteenkiste J, Bodoky G, Mateos MV, Bastit L, Ferreira I, et al. Results of a randomised, double‐blind, active‐controlled trial of darbepoetin alfa administered once every 3 weeks for the treatment of anaemia in patients receiving multicycle chemotherapy. Haematologica 2005; Vol. 90, issue Suppl 2:abstract 471.
Canon 2011 {published data only}
- Canon JL, Vansteenkiste J, Hedenus M, Gascon P, Bokemeyer C, Ludwig H, et al. Transfusion risk in cancer patients with chemotherapy‐induced anemia when initiating darbepoetin alfa therapy at a baseline hemoglobin level of <9 g/dL versus 9 to <10 g/dL versus (greater‐than or equal to)10 g/dL: an exploratory analysis of a phase 3 trial. Medical Oncology 2011;xx:1‐9. [DOI] [PubMed] [Google Scholar]
Caravita 2009 {published data only}
- Caravita T, Siniscalchi A, Montanaro M, Niscola P, Stasi R, Amadori S, et al. High‐dose epoetin alfa as induction treatment for severe anemia in multiple myeloma patients. International Journal of Hematology 2009;90(2):270‐2. [DOI] [PubMed] [Google Scholar]
Casadevall 2004 {published data only}
- Casadevall N, Durieux P, Dubois S, Hemery F, Lepage E, Quarre MC, et al. Health, economic, and quality‐of‐life effects of erythropoietin and granulocyte colony‐stimulating factor for the treatment of myelodysplastic syndromes: a randomized, controlled trial. Blood 2004;104(2):321‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Casadevall N, Lepage E, Durieux P, Dubois S, Dreyfus F, Quarre MC, et al. Erythropoietin (RHUEPO) plus G‐CSF in the treatment of anemia in myelodysplastic syndromes (MDS): results of a randomised trial with impact on quality of life and costs. The Hematology Journal 2001, issue Suppl 1:abstract 687.
Cazzola 2003 {published data only}
- Cazzola M, Beguin Y, Kloczko J, Spicka I, Coiffier B. Once‐weekly epoetin beta is highly effective in treating anaemic patients with lymphoproliferative malignancy and defective endogenous erythropoietin production. British Journal of Haematology 2003;122(3):386‐93. [DOI] [PubMed] [Google Scholar]
- Cazzola M, Coiffier B, Kloczko J, Spika I. Once weekly NeoRecormon® (epoetin beta) for the treatment of anemia associated with lymphoproliferative malignancies: results of the NOW (NeoRecormon® once weekly) study. Hematology Journal 2002, issue 3 Suppl 1:abstract 0182.
Chan 1995 {published data only}
- Chan AT, Leung WT, Lin J, Yeo W, Johnson PJ. Recombinant human erythropoietin for anaemia in Chinese cancer patients on chemotherapy. Clinical Oncology (Royal College of Radiologists) 1995;7(4):272. [DOI] [PubMed] [Google Scholar]
Cheng 2009 {published data only}
- Cheng Z, Wu JL, Chen JF. Clinical observation on the treatment of male neoplastic anemia with Yixuesheng capsule combined with recombination human erythropoietin. Chinese Journal of Integrative Medicine 2009;15(1):63‐5. [DOI] [PubMed] [Google Scholar]
Christodoulakis 2005 {published data only}
- Christodoulakis M, Tsiftsis DD, Hellenic Surgical Oncology Perioperative EPO Study Group. Preoperative epoetin alfa in colorectal surgery: a randomized, controlled study. Annals of Surgical Oncology 2005;12(9):718‐25. [DOI] [PubMed] [Google Scholar]
Coiffier 2006 {published data only}
- Coiffier B, Boogaerts M, Aapro M, Hayward C, Burger HU. Effect of treatment with epoetin Beta on thromboembolic events in anemic patients with cancer: a metaanalysis. Supportive Cancer Therapy 2006;4(1):49‐55. [DOI] [PubMed] [Google Scholar]
Coleman 2009 {published data only}
- Coleman EA, Anaissie EJ, Kennedy RL, Lockhart KD, Stewart CB, Bailey C. Predictors of deep vein thrombosis (DVT) in newly diagnosed multiple myeloma (MM) patients with and without prophylactic recombinant erythropoietin (EPO) therapy. Journal of Clinical Oncology 2009;27(15):9554. [Google Scholar]
Crawford 1997 {published data only}
- Crawford J, Blackwell S, Shoemaker D, Pupa MR, Sparrow T, Herndon J, et al. Prevention of chemotherapy‐related anemia by recombinant human erythropoietin (EPO) in patients with small cell lung cancer receiving cyclophosphamide, doxorubicin, and etoposide (CAE) chemotherapy with G‐CSF support. Lung Cancer 1997;18 Suppl 1:205. [Google Scholar]
Crawford 2003 {published data only}
- Crawford J, Robert F, Perry M, Belani CP, Sarokhan B. Epoetin alfa 40,000 u once weekly maintains hemoglobin in advanced non‐small‐cell lung cancer patients receiving first‐line chemotherapy. Proceedings of the American Society of Clinical Oncology. 2003; Vol. 22:628.
- Crawford J, Robert F, Perry M, Belani CP, Sarokhan B. Epoetin alfa 40,000 u once weekly maintains hemoglobin in advanced non‐small‐cell lung cancer patients receiving first‐line chemotherapy. Proceedings of the American Society of Clinical Oncology 2003;22:628, abstract 2527. [Google Scholar]
Crawford 2007 {published data only}
- Crawford J, Robert F, Perry MC, Belani C, Williams D, Anemia Prevention in NSCLC Group. A randomized trial comparing immediate versus delayed treatment of anemia with once‐weekly epoetin alfa in patients with non‐small cell lung cancer scheduled to receive first‐line chemotherapy. Journal of thoracic oncology : official publication of the International Association for the Study of Lung Cancer 2007;2(3):210‐20. [DOI] [PubMed] [Google Scholar]
Cremieux 2003 {published data only}
- Cremieux P, Greenberg P, Piech CT. Epoetin alfa is more effective and less costly relative to darbepoetin alfa in lung cancer patients receiving treatment for chemotherapy‐induced anemia [abstract no. 2248]. Proceedings of the American Society of Clinical Oncology. 2003; Vol. 22:2248.
Dahl 2008 {published data only}
- Dahl NV, Henry DH, Coyne DW. Thrombosis with erythropoietic stimulating agents‐does iron‐deficient erythropoiesis play a role?. Seminars in Dialysis 2008;21(3):210‐1. [DOI] [PubMed] [Google Scholar]
Daneryd 1998 {published data only}
- Daneryd P, Svanberg E, Körner U, Lindholm E, Sandström R, Brevinge H, et al. Protection of metabolic and exercise capacity in unselected weight‐losing cancer patients following treatment with recombinant erythropoietin: a randomized prospective study. Cancer Research 1998;58:5374‐9. [PubMed] [Google Scholar]
- Lindholm E, Daneryd P, Korner U, Hyltander A, Fouladiun M, Lundholm K. Effects of recombinant erythropoietin in palliative treatment of unselected cancer patients. Clinical Cancer Research 2004;10(20):6855‐64. [DOI] [PubMed] [Google Scholar]
- Lonnroth C, Svensson M, Wang W, Korner U, Daneryd P, Nilsson O, et al. Survival and erythropoietin receptor protein in tumours from patients randomly treated with rhEPO for palliative care. Medical Oncology 2008;25(1):22‐9. [DOI] [PubMed] [Google Scholar]
Dannemann 2004 {published data only}
- Dannemann B, Wacholtz M, Lau H, Cheung W. Pharmacokinetics (PK) and pharmacodynamics (PD) of epoetin alfa in cancer patients with anemia receiving cyclic chemotherapy. Journal of Clinical Oncology 2004; Vol. 22, issue 14s:775, abstract 8203.
Demetri 1998 {published data only}
- Demetri GD, Kris M, Wade J, Degos L, Cella D. Quality‐of‐life benefit in chemotherapy patients treated with epoetin alfa is independent of disease response or tumor type: Results from a prospective community oncology study. Journal of Clinical Oncology 1998;16:3412‐25. [DOI] [PubMed] [Google Scholar]
Dicato 2011 {published data only}
- Dicato M. Erythropoiesis‐stimulating agents: The present situation. Clinical and Translational Oncology 2011;13(5):287‐8. [DOI] [PubMed] [Google Scholar]
Dronca 2008 {published data only}
- Dronca RS, Steensma DP. VTE and mortality associated with erythropoiesis‐stimulating agents in cancer‐associated anemia.[comment]. Nature Clinical Practice Oncology 2008;5(9):504‐5. [DOI] [PubMed] [Google Scholar]
Dusenbery 1994 {published data only}
- Dusenbery KE, McGuire WA, Holt PJ, Carson LF, Fowler JM, Twiggs LB. Erythropoietin increases hemoglobin during radiation therapy for cervical cancer. International Journal of Radiation Oncology, Biology, Physics 1994;29(5):1079‐84. [DOI] [PubMed] [Google Scholar]
Elsaid 2001 {unpublished data only}
- Elsaid A, Farouk M. Significance of anemia and role of erythropoietin in radiation induced mucositis in head and neck cancer patients. International Journal of Radiation Oncology Biology Physics 2001; Vol. 51, issue 3 Suppl 1:368.
Fagnoni 2005 {published data only}
- Fagnoni P, Limat S, Chaigneau L, Guardiola E, Briaud S, Schmitt B, et al. Clinical and economic impact of epoetin in adjuvant‐chemotherapy for breast cancer. Support.Care Cancer 2006;14(0941‐4355 (Print), 0941‐4355 (Linking), 10):1030‐7. [DOI] [PubMed] [Google Scholar]
Ferrero 2009 {published data only}
- Ferrero D, Darbesio A, Giai V, Genuardi M, Dellacasa CM, Sorasio R, et al. Efficacy of a combination of human recombinant erythropoietin + 13‐cis‐retinoic acid and dihydroxylated vitamin D3 to improve moderate to severe anaemia in low/intermediate risk myelodysplastic syndromes. British Journal of Haematology 2009;144(3):342‐9. [DOI] [PubMed] [Google Scholar]
Franchi 2008 {published data only}
- Franchi F, Pastore C, Nigita G, Seminara P. Darbepoetin in the control of cancer‐related anaemia. Clinical & Experimental Medicine 2008;8(4):225‐7. [DOI] [PubMed] [Google Scholar]
Freeman 2006 {published data only}
- Freeman III BB, Hinds P, Iacono LC, Razzouk BI, Burghen E, Stewart CF. Pharmacokinetics and pharmacodynamics of intravenous epoetin alfa in children with cancer. Pediatric Blood & Cancer 2006;47(5):572‐9. [DOI] [PubMed] [Google Scholar]
Fujisaka 2004 {published data only}
- Fujisaka Y, Tamura T, Ohe Y, Kunitoh H, Sekine I, Yamamoto N, et al. Pharmacokinetics and pharmacodynamics of weekly epoetin beta in lung cancer patients. Japanese Journal of Clinical Oncology 2006;36(8):477. [DOI] [PubMed] [Google Scholar]
Gabrilove 2001 {published data only}
- Gabrilove JL, Cleeland CS, Livingston RB, Sarokhan B, Winer E, Einhorn LH. Clinical evaluation of once‐weekly dosing of epoetin alfa in chemotherapy patients: improvements in hemoglobin and quality of life are similar to three‐times‐weekly dosing. Journal of Clinical Oncology 2001;19(11):2875‐82. [DOI] [PubMed] [Google Scholar]
Garton 1995 {published data only}
- Garton JP, Gertz MA, Witzig TE, Greipp PR, Lust JA, Schroeder G, et al. Epoetin alfa for the treatment of the anemia of multiple myeloma. A prospective, randomized, placebo‐controlled, double‐blind trial. Archives of Internal Medicine 1995;155:2069‐74. [PubMed] [Google Scholar]
Gascon 2008 {published data only}
- Gascn P. Safety update on erythropoiesis‐stimulating agents: Trials within and outside the accepted indications. unknown AM 2008;13(SUPPL. 3):4‐10. [DOI] [PubMed] [Google Scholar]
Gebbia 1992 {published data only}
- Gebbia V, Gebbia N, Testa A, Valenza R, Borsellino N, Rausa L. Subcutaneous recombinant human erythropoietin prevents chemotherapy‐related anemia in patients with advanced cancer. International Journal of Oncology 1992;1:341‐5. [PubMed] [Google Scholar]
Glaser 1999 {published data only}
- Glaser C, Millesi W, Wanschitz F, Schull B, Lang S, Leitha T, et al. R‐HuErythropoietin treatment increases efficacy of neo‐adjuvant radiochemotherapy and improves cancer free survival of patient with oral squamous cell carcinoma: a 17 months follow‐up. ASCO 1999;Meeting Abstract:Abstract 1543. [Google Scholar]
Glaser 2001 {published data only}
- Glaser CM, Millesi W, Kornek GV, Lang S, Schull B, Watzinger F, et al. Impact of hemoglobin level and use of recombinant erythropoietin on efficacy of preoperative chemoradiation therapy for squamous cell carcinoma of the oral cavity and oropharynx. International Journal of Radiation Oncology, Biology, Physics 2001;50(3):705‐15. [DOI] [PubMed] [Google Scholar]
Glaspy 1997 {published data only}
- Glaspy J, Bukowski R, Steinberg D, Taylor C, Tchekmedyian S, Vadhan‐Raj S. Impact of therapy with epoetin alfa on clinical outcomes in patients with nonmyeloid malignancies during cancer chemotherapy in community oncology practice. Journal of Clinical Oncology 1997;15:1218‐34. [DOI] [PubMed] [Google Scholar]
Glaspy 2001 {published data only}
- Glaspy J, Jadeja JS, Justice G, Kessler J, Richards D, Schwartzberg L, et al. A dose‐finding and safety study of novel erythropoiesis stimulating protein (NESP) for the treatment of anaemia in patients receiving multicycle chemotherapy. British Journal of Cancer 2001;84 Suppl 1:17‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Glaspy 2002 {published data only}
- Glaspy JA, Jadeja JS, Justice G, Kessler J, Richards D, Schwartzberg L, et al. Darbepoetin alfa given every 1 or 2 weeks alleviates anaemia associated with cancer chemotherapy. British Journal of Cancer 2002;87(3):268‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Glaspy 2002b {published data only}
- Glaspy JA, Tchekmedyian NS. Darbepoetin alfa administered every 2 weeks alleviates anemia in cancer patients receiving chemotherapy. Oncology (Huntingt) 2002;16(10 Suppl 11):23‐9. [PubMed] [Google Scholar]
Glaspy 2003 {published data only}
- Glaspy JA, Jadeja JS, Justice G, Fleishman A, Rossi G, Colowick AB. A randomized, active‐control, pilot trial of front‐loaded dosing regimens of darbeopetin‐alfa for the treatment of patients with anemia during chemotherapy for malignant disease. Cancer 2003;97:1312‐20. [DOI] [PubMed] [Google Scholar]
Glaspy 2005 {published data only}
- Glaspy J, Henry D, Patel R, Tchekmedyian S, Applebaum S, Berdeaux D, et al. Effects of chemotherapy on endogenous erythropoietin levels and the pharmacokinetics and erythropoietic response of darbepoetin alfa: A randomised clinical trial of synchronous versus asynchronous dosing of darbepoetin alfa. European Journal of Cancer 2005;41(8):1140‐9. [DOI] [PubMed] [Google Scholar]
Glaspy 2006 {published data only}
- Glaspy J, Jadeja J, Justice G, Fleishman A, Rossi G, Colowick A. Optimizing the management of anemia in patients with cancer: a randomized, active‐controlled, study investigating the dosing of darbepoetin alfa. Hematology Journal 2002:abstract 0109.
- Glaspy J, Vadhan‐Raj S, Patel R, Bosserman L, Hu E, Lloyd RE, et al. Randomized comparison of every‐2‐week darbepoetin alfa and weekly epoetin alfa for the treatment of chemotherapy‐induced anemia: the 20030125 Study Group Trial. Journal of Clinical Oncology 2006;24(15):2290‐7. [DOI] [PubMed] [Google Scholar]
Glaspy 2011 {published data only}
- Glaspy JA. Darbepoetin Alfa controversies, from dosage issues to safety concerns: The larger lesson. Oncology 2011;25(5):423‐4. [PubMed] [Google Scholar]
Glimelius 1998 {published data only}
- Glimelius B, Linne T, Hoffman K, Larsson L, Svensson JH, Nasman P, et al. Epoetin beta in the treatment of anemia in patients with advanced gastrointestinal cancer. Journal of Clinical Oncology 1998;16(2):434‐40. [DOI] [PubMed] [Google Scholar]
Glossmann 2003 {published data only}
- Glossmann JP, Engert A, Wassmer G, Flechtner H, Ko Y, Rudolph C, et al. Recombinant human erythropoietin, epoetin beta, in patients with relapsed lymphoma treated with aggressive sequential salvage chemotherapy ‐ results of a randomized trial. Annals of Hematology 2003;82(8):469‐75. [DOI] [PubMed] [Google Scholar]
Goldsmith 2011 {published data only}
- Goldsmith DJ, Covic AC. Significant further evidence to bolster the link between epoetin and strokes in chronic kidney disease and cancer. Kidney International 2011;80(3):237‐9. [DOI] [PubMed] [Google Scholar]
Granetto 2003 {published data only}
- Granetto C, Ricci S, Martoni A, Pezzella G, Testore F, Mattioli R, et al. Comparing the efficacy and safety of fixed versus weight‐based dosing of epoetin alpha in anemic cancer patients receiving platinum‐based chemotherapy. Oncology Reports 2003;10(5):1289‐96. [PubMed] [Google Scholar]
Gregory 2005 {published data only}
- Gregory SA. Efficacy of darbepoetin alfa in the treatment of chemotherapy‐induced anemia in non‐Hodgkin's lymphoma. Supportive Cancer Therapy 2006;3(4):232‐9. [DOI] [PubMed] [Google Scholar]
Grigorescu 2006 {published data only}
- Grigorescu AC, Boldearu C. Platinum‐based chemotherapy for patients (PT) with non small cell lung cancer (NSCLC) with anemia treated with epoetin beta or blood transfusions, a pilot study. Annals of Oncology 2006;17(Supplement 9):ix295 Abstract 1022p. [Google Scholar]
Hadland 2009 {published data only}
- Hadland BK, Longmore GD. Erythroid‐stimulating agents in cancer therapy: potential dangers and biologic mechanisms. Journal of Clinical Oncology 2009;27(25):4217‐26. [DOI] [PubMed] [Google Scholar]
Han 2008 {published data only}
- Han HS, Han JY, Yu SY, Pyo HR, Kim HY, Cho KH, et al. Randomized phase 2 study of subcutaneous amifostine versus epoetin‐alpha given 3 times weekly during concurrent chemotherapy and hyperfractionated radiotherapy for limited‐disease small cell lung cancer. Cancer 2008;113(7):1623‐31. [DOI] [PubMed] [Google Scholar]
Harousseau 2005 {published data only}
- Harousseau JL, Fumoleau P, Lange W, Welslau M. Increasing hemoglobin levels with epoetin alfa in anemic hematologic cancer patients receiving chemotherapy correlates significantly with improved quality of life. Blood. 2005, The American Society of Hematology, 2004; Vol. 104, issue 11:2213.
Hellstörm‐Lindberg 2010 {published data only}
- Hellstrm‐Lindberg, E. Erythropoiesis‐stimulating agents in myelodysplastic syndromes. Leukemia and Lymphoma 2010;51(7):1155‐6. [DOI] [PubMed] [Google Scholar]
Hellström‐Lindberg 1998 {published data only}
- Hellström Lindberg E, Ahlgren T, Beguin Y, Carlsson M, Carneskog J, Dahl IM, et al. Treatment of anemia in myelodysplastic syndromes with granulocyte colony‐stimulating factor plus erythropoietin: results from a randomized phase II study and long‐term follow‐up of 71 patients. Blood 1998;92(1):68‐75. [PubMed] [Google Scholar]
Henry 2004 {published data only}
- Henry DH, Dahl NV, Auerbach M, Tchekmedyian S, Laufman LR. Intravenous ferric gluconate (FG) for increasing response to epoetin (EPO) in patients with anemia of cancer chemotherapy results of a multicenter, randomized trial. Blood 2004; Vol. 104, issue 11 Pt 2:10b, abstract 3696.
Henry 2006 {published data only}
- Henry DH, Gordan LN, Charu V, Wilhelm FE, Williams D, Xie J, et al. Randomized, open‐label comparison of epoetin alfa extended dosing (80 000 U Q2W) vs weekly dosing (40 000 U QW) in patients with chemotherapy‐induced anemia. Current Medical Research & Opinion 2006;22(7):1403‐13. [DOI] [PubMed] [Google Scholar]
- Henry DH, Williams D, Xie J, Wilhelm F. Randomized, open‐label comparison of epoetin alfa extended dosing (80,000 U every two weeks) versus weekly dosing (40,000 U weekly) in anemic patients with cancer receiving chemotherapy. Journal of Supportive Oncology 2007;5(4 Suppl 2):16‐7. [Google Scholar]
Henry 2007 {published data only}
- Henry DH, Dahl NV, Auerbach M. Is thromboembolism in cancer patients treated with erythropoietic stimulating agents related to thrombocytosis and iron restricted erythropoiesis?. Blood 2007; Vol. 110, issue 11:abstract 1625.
- Henry DH, Dahl NV, Auerbach M, Tchekmedyian S, Laufman LR. Intravenous ferric gluconate significantly improves response to epoetin alfa versus oral iron or no iron in anemic patients with cancer receiving chemotherapy. Oncologist 2007;12(2):231‐42. [DOI] [PubMed] [Google Scholar]
Henze 2002 {published data only}
- Henze G, Michon J, Morland B, Perek D, Rizzari C, Zoubek A, EPO INT51 Study Group. Phase III randomized study: efficacy of epoetin alfa in reducing blood transfusions in newly diagnosed pediatric cancer patients receiving chemotherapy. 2002 ASCO Annual Meeting. 2002.
Hesketh 2004 {published data only}
- Hesketh PJ, Arena F, Patel D, Austin M, D'Avirro P, Rossi G, et al. A randomized controlled trial of darbepoetin alfa administered as a fixed or weight‐based dose using a front‐loading schedule in patients with anemia who have nonmyeloid malignancies. Cancer 2004;100(4):859‐68. [DOI] [PubMed] [Google Scholar]
- Hesketh PJ, Arena F, Patel D, Poulsen E, D'Avirro P, Rossi G, et al. Front‐loaded darbepoetin alfa with Q3W maintenance administered as a fixed or weight‐based dose in anemic cancer patients results in similar efficacy profiles. Proceedings of the American Society of Clinical Oncology 2003:abstract 2941.
Hirsh 2007 {published data only}
- Hirsh V, Glaspy J, Mainwaring P, Manegold C, Ramlau R, Eid JE. Phase II study of two dose schedules of C.E.R.A. (Continuous Erythropoietin Receptor Activator) in anemic patients with advanced non‐small cell lung cancer (NSCLC) receiving chemotherapy. Trials 2007;8(1745‐6215 (Electronic)):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huggett 2011 {published data only}
- Huggett B, Hodgson J, Lahteenmki R. Public biotech 2010‐the numbers. Nature Biotechnology 2011;29(7):585‐91. [DOI] [PubMed] [Google Scholar]
Hyer 2011 {published data only}
- Hyer R. Serum hepcidin levels predict ESA and IV iron responses. Oncology Report 2011;July‐August:35. [Google Scholar]
Itzykson 2009 {published data only}
- Itzykson R, Ayari S, Vassilief D, Berger E, Slama B, Vey N, et al. Is there a role for all‐trans retinoic acid in combination with recombinant erythropoetin in myelodysplastic syndromes? A report on 59 cases. Leukemia 2009;23(4):673‐8. [DOI] [PubMed] [Google Scholar]
Jacubowski 2003 {published data only}
- Jacubowski AA, Hurria A, Williams D. Head‐to‐head comparison of epoetin alfa 40,000 QW vs darbepoetin alfa 200 mcg Q2W in anemic patients with cancer receiving chemotherapy: preliminary results. Blood. 2003; Vol. 102, issue 11:#4391.
Jadersten 2008 {published data only}
- Jadersten M, Malcovati L, Dybedal I, Della Porta MG, Invernizzi R, Montgomery SM, et al. Erythropoietin and granulocyte‐colony stimulating factor treatment associated with improved survival in myelodysplastic syndrome. Journal of Clinical Oncology 2008;26(21):3607‐13. [DOI] [PubMed] [Google Scholar]
Jitnuyanont 2001 {published data only}
- Jitnuyanont A. Impact of therapy with recombinant human erythropoietin (r‐HuEPO) and Quality‐of‐life in anemic cancer patients. Internal Medicine Journal of Thailand 2001;17(4):283‐90. [Google Scholar]
Johansson 2001 {published data only}
- Johansson JE, Wersall P, Brandberg Y, Andersson SO, Nordstrom L, EPO‐Study Group. Efficacy of epoetin beta on hemoglobin, quality of life, and transfusion needs in patients with anemia due to hormone‐refractory prostate cancer‐‐a randomized study. Scandinavian Journal of Urology & Nephrology 2001;35(4):288‐94. [DOI] [PubMed] [Google Scholar]
Jones 2011 {published data only}
- Jones CA, Elbert‐Avila K. Palliative care in advanced cancer in older adults: management of pain, fatigue, and gastrointestinal symptoms. Clinical Geriatrics 2011;19(11):23‐9. [Google Scholar]
Juan 2006 {published data only}
- Juan O, Munoz J, Albert A, Olmos S, Campos JM, Molins C, et al. Clinical benefit associated with early erythropoietic intervention in chemotherapy induced anemia. Annals of Oncology 2006;17(Supplement 9):ix293 Absrtact 1014P. [Google Scholar]
Justice 2005 {published data only}
- Justice G, Kessler JF, Jadeja J, Campos L, Weick, J, et al. A randomized, multicenter study of subcutaneous and intravenous darbepoetin alfa for the treatment of chemotherapy‐induced anemia. Annals of Oncology 2005;16:1192‐8. [DOI] [PubMed] [Google Scholar]
Kara 2008 {published data only}
- Kara O, Dizdar O, Altundag K. Erythropoiesis‐stimulating agents in the treatment of cancer‐associated anemia.[comment]. JAMA 2008;300(24):2855‐7. [DOI] [PubMed] [Google Scholar]
Katodritou 2008 {published data only}
- Katodritou E, Verrou E, Hadjiaggelidou C, Gastari V, Laschos K, Kontovinis L, et al. Erythropoiesis‐stimulating agents are associated with reduced survival in patients with multiple myeloma.[see comment]. American Journal of Hematology 2008;83(9):697‐701. [DOI] [PubMed] [Google Scholar]
Katodritou 2009 {published data only}
- Katodritou E, Terpos E, Kaloutsi V, Verrou E, Gastari V, Varthaliti M, et al. Correlation of erythropoietin stimulating agents (ESAs) with the post‐therapy micro‐vessel density (MVD) in newly diagnosed myeloma patients: a possible mechanism of ESAs association with reduced survival rates. Blood (ASH Annual Meeting Abstracts) 2009;114(22):4873. [Google Scholar]
Kettelhack 1998 {published data only}
- Kettelhack C, Hones C, Messinger D, Schlag PM. Randomized multicentre trial of the influence of recombinant human erythropoietin on intraoperative and postoperative transfusion need in anaemic patients undergoing right hemicolectomy for carcinoma. British Journal of Surgery 1998;85(1):63‐7. [DOI] [PubMed] [Google Scholar]
Kim 2010 {published data only}
- Kim TE, Kim KP, Kim BH, Shin SG, Jang IJ, Yu KS. Pharmacokinetic and pharmacodynamic comparison of two recombinant human erythropoietin formulations after single subcutaneous administration: an open‐label, sequence‐randomized, two‐treatment crossover study in healthy Korean male volunteers. Clinical Therapeutics 2010;32(11):1968‐76. [DOI] [PubMed] [Google Scholar]
Kosmadakis 2003 {published data only}
- Kosmadakis N, Messaris E, Maris A, Katsaragakis S, Leandros E, Konstadoulakis MM, et al. Perioperative erythropoietin administration in patients with gastrointestinal tract cancer: prospective randomized double‐blind study. Annals of Surgery 2003;237(3):417‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kotasek 2004 {published data only}
- Kotasek D, Canon JL, San Miguel J, Hedenus L, Hendricks G, Rossi K, et al. Correction/maintenance dosing (front loading) of darbepoetin alfa: final results from a randomized phase 3 active controlled trial. Blood 2004;104(11):abstract 1636. [Google Scholar]
- Kotasek D, Canon JL, San Miguel J, Hedenus M, Hendricks L, Rossi G, et al. Correction/maintenance dosing (front loading) of darbepoetin alfa: Final results from a randomized phase III active‐controlled trial. The Journal of Supportive Oncology 2005;3(2 SUPPL. 1):16‐7. [Google Scholar]
Kotasek 2007 {published data only}
- Kotasek D, Canon J‐L, Mateos MV, Hedenus M, Rossi G, Taylor K. A randomized, controlled trial comparing darbepoetin alfa correction/maintenance dosing with weekly dosing for treating chemotherapy‐induced anemia. Current Medical Research & Opinion 2007;23(6):1387‐401. [DOI] [PubMed] [Google Scholar]
Larsson 2008 {published data only}
- Larsson G, Janson ET. Anemia in patients with midgut carcinoid, treated with alpha interferon: effects by erythropoietin treatment on the perceived quality of life. European Journal of Cancer Care 2008;17(2):200‐4. [DOI] [PubMed] [Google Scholar]
Lastiri 2002 {published data only}
- Lastiri JM, Specterman SR, Rendo P, Pallotta MG, Varela MS, Goldstein S. [Predictive response variables to recombinant human erythropoietin treatment in patients with anemia and cancer]. Medicina (B Aires) 2002;62(0025‐7680 (Print), 0025‐7680 (Linking), 1):41‐7. [PubMed] [Google Scholar]
Latagliata 2008 {published data only}
- Latagliata R, Oliva EN, Volpicelli P, Carmosino I, Breccia M, Vincelli I, et al. Twice‐weekly high‐dose rHuEpo for the treatment of anemia in patients with low‐risk myelodysplastic syndromes. Acta Haematologica 2008;120(2):104‐7. [DOI] [PubMed] [Google Scholar]
Lavey 1993 {published data only}
- Lavey RS, Dempsey WH. Erythropoietin increases hemoglobin in cancer patients during radiation therapy. International Journal of Radiation Oncology, Biology, Physics 1993;27:1147‐52. [DOI] [PubMed] [Google Scholar]
Lavey 2004 {published data only}
- Lavey RS, Liu PY, Greer BE, Robinson WR, Chang PC, Wynn RB, et al. Recombinant human erythropoietin as an adjunct to radiation therapy and cisplatin for stage IIB‐IVA carcinoma of the cervix: a Southwest Oncology Group study. Gynecol Oncol 2004;95(1):145‐51. [DOI] [PubMed] [Google Scholar]
Leitgeb 1994 {published data only}
- Leitgeb C, Pecherstorfer M, Fritz E, Ludwig H. Quality of life in chronic anaemia of cancer during treatment with recombinant human erythropoietin. Cancer 1994;73:2535‐42. [DOI] [PubMed] [Google Scholar]
Leon 1998 {published data only}
- Leon P, Jimenez M, Barona P, Sierrasesumaga L. Recombinant human erythropoietin for the treatment of anemia in children with solid malignant tumors. Medical and Pediatric Oncology 1998;30(2):110‐6. [DOI] [PubMed] [Google Scholar]
Lichtin 2008 {published data only}
- Lichtin AE. How safe are erythropoiesis‐stimulating agents?[see comment]. Cleveland Clinic Journal of Medicine 2008;75(5):359‐60. [DOI] [PubMed] [Google Scholar]
Loibl 2006 {published data only}
- Loibl S, Kaufmann M, Maataoui V, Mehta KM, Hofmann K, Petrich S, et al. Darbepoetin alfa as primary prophylaxis of anemia in patients with breast cancer treated preoperatively with docetaxel/doxorubicin/cyclophosphamide. Supportive Cancer Therapy 2006;3(2):103‐9. [DOI] [PubMed] [Google Scholar]
Ludwig 1995 {published data only}
- Ludwig H, Sundal E, Pecherstorfer M, Leitgeb C, Bauernhofer T, Beinhauer A, et al. Recombinant human erythropoietin for the correction of cancer associated anemia with and without concomitant cytotoxic chemotherapy. Cancer 1995;76(11):2319‐29. [DOI] [PubMed] [Google Scholar]
Malik 1998 {published data only}
- Malik IA, Khan ZK, Hakimali A, Sabih M, Rehman G. The effect of subcutaneous recombinant human erythropoietin (r‐HuEPO) on anemia in cancer patients receiving platinum‐based chemotherapy. Journal of the Pakistan Medical Association 1998;48(5):127‐31. [PubMed] [Google Scholar]
Mangiameli 2002 {published data only}
- Mangiameli A, Spina S, Iannetti E, Catalano D, Spadaro D, Trovato GM. [Erythropoietin and cisplatin‐induced neuropathies in cancer patients]. [Italian]. Clinica Terapeutica 2002;153(3):177‐80. [PubMed] [Google Scholar]
Mantovani 2000 {published data only}
- Mantovani L, Lentini G, Hentschel B, Wickramanayake PD, Loeffler M, Diehl V, et al. Treatment of anaemia in myelodysplastic syndromes with prolonged administration of recombinant human granulocyte colony‐stimulating factor and erythropoietin. British Journal of Haematology 2000;109(2):367‐75. [DOI] [PubMed] [Google Scholar]
Marinaccio 2003 {published data only}
- Marinaccio M, Mele E, Giotta F, Cantinieri C, Cocca M. Pretreatment normalization of mild anemia with epoetin alfa: Impact on the outcome in epithelial ovarian cancer patients. Proceedings of the American Society of Clinical Oncology. 2003; Vol. 22:486.
Markman 1993 {published data only}
- Markman M, Reichman B, Hakes T, n S, Jones W, Lewis JL Jr, et al. The use of recombinant human erythropoietin to prevent carboplatin‐induced anemia. Gynecologic Oncology 1993;49(2):172‐6. [DOI] [PubMed] [Google Scholar]
Mel 2008 {published data only}
- Mel JR, Salar A, Rodriguez CA, Alegre A, Gonzalez A, Cassinello J, et al. A prospective observational study of the effectiveness, safety, and effect on fatigue of darbepoetin alfa for the treatment of chemotherapy‐induced anaemia. Current Medical Research & Opinion 2008;24(10):2931‐42. [DOI] [PubMed] [Google Scholar]
Merchionne 2009 {published data only}
- Merchionne F, Dammacco F. Biological functions and therapeutic use of erythropoiesis‐stimulating agents: perplexities and perspectives. British Journal of Haematology 2009;146(2):127‐41. [DOI] [PubMed] [Google Scholar]
Merlano 2001 {published data only}
- Merlano M, Ricci S, Martoni A. Comparing the efficacy of fixed vs. weight‐based dosing of epoetin alfa in anemic cancer patients receiving platinum‐based chemotherapy. European Journal of Cancer 2001; Vol. 37, issue Suppl 6:S346.
MF4266 {published data only}
- Luksenburg H, Weir A, Wager, R. MF4266 in: Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen, Inc. and Procrit (epoetin alfa) Ortho Biotech, L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research, Oncologic Drugs Advisory Committee, Rockville (MD), USA, 2004; Vol. http://www.fda.gov/ohrms/dockets/ac/04/briefing/4037b2_04.pdf [date of last access March 27, 2009].
Miller 2004 {published data only}
- Miller KB, Kim HT, Greenberg P, Jagt R, Bennett JM, Tallman MS, et al. Phase III prospective randomized trial of EPO with or without G‐CSF versus supportive therapy alone in the treatment of myelodysplastic syndromes (MDS): Results of the ECOG‐CLSG trial (E1996). Blood 2004; Vol. 104, issue 11:70.
Morishima 2006 {published data only}
- Morishima Y, Ogura M, Yoneda S, Sakai H, Tobinai K, Nishiwaki Y, et al. Once‐weekly epoetin‐beta improves hemoglobin levels in cancer patients with chemotherapy‐induced anemia: A randomized, double‐blind, dose‐finding study. Japanese Journal of Clinical Oncology 2006;36(10):655‐61. [DOI] [PubMed] [Google Scholar]
Morrow 2007 {published data only}
- Morrow GR. Cancer‐related fatigue: Causes, consequences, and management. The Oncologist 2007;12(SUPPL. 1):1‐3. [DOI] [PubMed] [Google Scholar]
Muravyov 2009 {published data only}
- Muravyov AV, Cheporov SV, Kislov NV, Volkova EL. Hemorheological changes in solid tumor patients after treatment with recombinant erythropoetin. Clinical Hemorheology & Microcirculation 2009;41(1):39‐47. [DOI] [PubMed] [Google Scholar]
Muravyov 2010 {published data only}
- Muravyov AV, Cheporov SV, Kislov NV, Bulaeva SV, Maimistova AA. Comparative efficiency and hemorheological consequences of hemotransfusion and epoetin therapy in anemic cancer patients. Clinical Hemorheology & Microcirculation 2010;44(2):115‐23. [DOI] [PubMed] [Google Scholar]
Mustacchi 2006 {published data only}
- Mustacchi G, Ceccherini R, Dellach C, Foladore S, Milani S, Leita M, et al. An induction dose of epoetin alpha of 40 000 IU daily for three consecutive days increases and maintains hemoglobin levels in anemic cancer patients undergoing chemotherapy. Annals of Oncology 2006;17(0923‐7534 (Print), 0923‐7534 (Linking), 11):1705‐8. [DOI] [PubMed] [Google Scholar]
Nagel 2011 {published data only}
- Nagel S, Kellner O, Engel‐Riedel W, Guetz S, Schumann C, Gieseler F, et al. Addition of darbepoetin alfa to dose‐dense chemotherapy: Results from a randomized phase II trial in small‐cell lung cancer patients receiving carboplatin plus etoposide. Clinical Lung Cancer 2011;12(1):62‐9. [DOI] [PubMed] [Google Scholar]
NCT00364845 2011 {published data only}
- NCT00364845. A randomised single‐blind study to improve health‐related quality of life as measured by the sf‐36 vitality score by correcting anemia with aranesp (darbepoetin alfa) in the elderly. clinicaltrials.gov./ct2./show/NCT00364845. 2011.
Nonoguchi 2009 {published data only}
- Nonoguchi H, Otaki Y, Tokuyama M, Yamamoto S, Nakanishi T. Epoetins and mortality in patients with cancer.[comment]. Lancet 2009;374(9686):287‐8. [DOI] [PubMed] [Google Scholar]
Oberhoff 2005 {published data only}
- Oberhoff C, Stauch M, Wilhelm G, Musch E, Heinrich B, Neise M, et al. Prevention and therapy of anemia in tumor patients with epoetin beta (NeoRecormon®) [Prävention und Therapie der Anämie bei Tumorpatienten mit Epoetin beta (NeoRecormon®)]. Tumordiagnostik & Therapie 2005;26:166‐71. [Google Scholar]
Olsson 2002 {published data only}
- Olsson AM, Svensson JH, Sundstrom J, Bergstrom S, Edekling T, Carlsson G, et al. Erythropoietin treatment in metastatic breast cancer‐‐effects on Hb, quality of life and need for transfusion. Acta Oncologica 2002;41(6):517‐24. [DOI] [PubMed] [Google Scholar]
Opie 2011 {published data only}
- Opie LH. Erythropoietin as a cardioprotective agent: Down but not out. Heart 2011;97(19):1537‐9. [DOI] [PubMed] [Google Scholar]
Ots 2008 {published data only}
- Ots PM, Carrizosa CL, Perez AR, Dios Saez Garrido J, Perez JM. Darbepoetin versus epoetin alfa for the correction of anemia in cancer patients receiving radiotherapy or chemoradiotherapy treatment. Clinical Medicine Oncology 2008;2:393‐399. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pat 2009 {published data only}
- Pat K, Anrys B, Verhulst D, Aelst F, Eygen K, Galdermans D, et al. Observational Aranesp Survey to Investigate the Q3W Schedule (OASIS): a prospective observational study of treatment of chemotherapy‐induced anaemia with every 3 weeks darbepoetin alfa. Supportive Care in Cancer 2009;17(2):211‐5. [DOI] [PubMed] [Google Scholar]
Pierelli 1999 {published data only}
- Pierelli L, Perillo A, Greggi S, Salerno G, Panici PB, Menichella, et al. Erythropoietin addition to granulocyte colony‐stimulating factor abrogates life‐threatening neutropenia and increases peripheral‐blood progenitor‐cell mobilization after epirubicin, paclitaxel, and cisplatin combination chemotherapy: results of a randomized comparison. Journal of Clinical Oncology 1999;17(4):1288‐95. [DOI] [PubMed] [Google Scholar]
Poirier 2010 {published data only}
- Poirier AL, Commer JM, Kwiatkowski F, Mercier M, Bonnetain F. [Oncology blood transfusion and quality of life: review]. Transfusion Clinique et Biologique 2010;17(5‐6):357‐61. [DOI] [PubMed] [Google Scholar]
Policarpo 2007 {published data only}
- Policarpo GD, Henry DH. Epoetin alfa for chemotherapy‐induced anemia: Assessment of two equivalent dosing regimens. Community Oncology 2007;4(3):129‐35. [Google Scholar]
Popescu 2010 {published data only}
- Popescu R, Rohr A, Piguet D, Irle C, Giger M, Brunner R, et al. Rapid anaemia control with epoetin: results of a Swiss survey on treatment of chemotherapy‐induced anaemia. Acta Haematologica 2010;123(2):129‐34. [DOI] [PubMed] [Google Scholar]
Porter 1996 {published data only}
- Porter JC, Leahey A, Polise K, Bunin G, Manno CS. Recombinant human erythropoietin reduces the need for erythrocyte and platelet transfusions in pediatric patients with sarcoma: A randomized, double‐blind, placebo‐controlled trial. Journal of Pediatrics 1996;129(5):656‐60. [DOI] [PubMed] [Google Scholar]
Puglisi 2009 {published data only}
- Puglisi F, Deroma L, Russo S, Carteni G, Sporchia A, Ucci G, et al. Effect of age on hemoglobin levels and quality of life following treatment with epoetin alfa in cancer patients. Critical Reviews in Oncology‐Hematology 2009;69(2):175‐82. [DOI] [PubMed] [Google Scholar]
Rades 2009 {published data only}
- Rades D. Erythropoietin administration during radiotherapy in anaemic head‐and‐neck cancer patients: Is it still a reasonable option or too dangerous?. Oral 2009;45(2):91‐3. [DOI] [PubMed] [Google Scholar]
Rath 2010 {published data only}
- Rath T. Iron and erythropoiesis‐stimulating agents in anaemia. European Journal of Oncology Pharmacy 2010;4(3):20‐1. [Google Scholar]
Rau 1998 {published data only}
- Rau B, Schlag PM, Willeke F, Herfarth C, Stephan P, Franke W. Increased autologous blood donation in rectal cancer by recombinant human erythropoietin (rhEPO). European Journal of Cancer 1998;34(7):992‐8. [DOI] [PubMed] [Google Scholar]
Rearden 2004 {published data only}
- Charu V, Saidman B, Ben‐Jacob A, Justice GR, Maniam AS, Rearden T, et al. Improvements in fatigue are associated with early treatment with darbepoetin alfa every 3 weeks (Q3W) Darbepoetin alfa (DA) treatment in anemic patients (pts) receiving chemotherapy. Blood 2004; Vol. 104:abstract 233.
- Rearden T, Charu V, Saidman B, Justice GR, Manaim AS. Results of a randomized study of every three‐week dosing (Q3W) of darbepoetin alfa for chemotherapy‐induced anemia (CIA). Blood 2003; Vol. 102, issue 11 Pt 2:abstract 3783.
- Rearden TP, Charu V, Saidman B, Ben‐Jacob A, Justice GR, Manaim AS, et al. Results of a randomized study of every three‐week dosing (Q3W) of darbepoetin alfa for chemotherapy‐induced anemia (CIA). Journal of Clinical Oncology 2004;22(14 Suppl):abstract 8064. [Google Scholar]
Reed 2005 {published data only}
- Reed SD, Radeva JI, Daniel DB, Fastenau JM, Williams D, Schulman KA. Early hemoglobin response and alternative metrics of efficacy with erythropoietic agents for chemotherapy‐related anemia. Current Medical Research & Opinion 2005;21(10):1527‐33. [DOI] [PubMed] [Google Scholar]
Ribatti 2009 {published data only}
- Ribatti D. Erythropoietin and cancer, a double‐edged sword. Leukemia Research 2009;33(1):1‐4. [DOI] [PubMed] [Google Scholar]
Richardson 2011 {published data only}
- Richardson PG, Schlag R, Khuageva N, Dimopoulos M, Shpilberg O, Kropff M, et al. Characterization of haematological parameters with bortezomib‐melphalan‐prednisone versus melphalan‐prednisone in newly diagnosed myeloma, with evaluation of long‐term outcomes and risk of thromboembolic events with use of erythropoiesis‐stimulating agents: Analysis of the VISTA trial. British Journal of Haematology 2011;153(2):212‐21. [DOI] [PubMed] [Google Scholar]
Rodgers 2008 {published data only}
- Rodgers GM III, Becker PS, Bennett CL, Cella D, Chanan‐Khan A, Chesney C, et al. Cancer‐ and chemotherapy‐induced anemia. Journal of the National Comprehensive Network 2008;6(6):536‐64. [DOI] [PubMed] [Google Scholar]
Sakai 2004 {published data only}
- Sakai H, Saijo N, Ohashi Y. Once‐weekly epoetin beta improves hemoglobin levels and quality of life in patients with chemotherapy‐induced anemia:A randomized, double blind, parallel group dose finding study. Annals of Oncology. 15 2004; Vol. 15, issue Suppl 3.
- Sakai H, Saijo N, Ohashi Y. Once‐weekly epoetin beta improves hemoglobin levels and quality of life in patients with chemotherapy‐induced anemia:A randomized, double blind, parallel group dose finding study. Journal of Clinical Oncology 2004;22(Suppl):abstract 8169. [DOI] [PubMed] [Google Scholar]
Samper 2002 {published data only}
- Samper OP, Rodriguez PA, Martin dM, Saez GJ, Delgado Perez JM. Treatment of anemia in patients under radiotherapy with subcutaneous epoetenium alpha 10,000 iu three times a week and 40,000 iu once a week. [Spanish]. Oncologia (Madrid) 2002;25(8):40‐6. [Google Scholar]
Schwartzberg 2004 {published data only}
- Schwartzberg LS, Yee LK, Senecal FM, Charu V, Tomita D, Wallace J, et al. A randomized comparison of every‐2‐week darbepoetin alfa and weekly epoetin alfa for the treatment of chemotherapy‐induced anemia in patients with breast, lung, or gynecologic cancer. The Oncologist 2004;9(6):696‐707. [DOI] [PubMed] [Google Scholar]
Schwartzberg 2005 {published data only}
- Schwartzberg L, Yee L, Charu V, Tomita D, Rossi G, Senecal F. Comparable efficacy and safety of darbepoetin alfa 200 mug every 2 weeks and epoetin alfa 40,000 U weekly in patients with breast cancer: Results of a randomized comparison. The Journal of Supportive Oncology 2005;3(2 Suppl 1):30‐1. [Google Scholar]
Schwartzberg 2007 {published data only}
- Schwartzberg L, Rearden T, Yee L, Mirtsching B, Charu V, Lam H, et al. A phase II, randomized, open‐label study to assess the efficacy of extended‐dose schedule administration of darbepoetin alfa in cancer patients with chemotherapy‐induced anemia. Journal of Supportive Oncology 2007;5(4 Suppl 2):22‐3. [Google Scholar]
Scott 2002 {published data only}
- Scott SN, Boeve TJ, McCulloch TM, Fitzpatrick KA, Karnell LH. The effects of epoetin alfa on transfusion requirements in head and neck cancer patients: a prospective, randomized, placebo‐controlled study. Laryngoscope 2002;112(7 Pt 1):1221‐9. [DOI] [PubMed] [Google Scholar]
Senecal 2005 {published data only}
- Senecal FM, Yee L, Gabrail N, Charu V, Tomita D, Rossi G, et al. Treatment of chemotherapy‐induced anemia in breast cancer: results of a randomized controlled trial of darbepoetin alfa 200 microg every 2 weeks versus epoetin alfa 40,000 U weekly. Clinical Breast Cancer 2005;6(5):446‐54. [DOI] [PubMed] [Google Scholar]
Shasha 2003 {published data only}
- Shasha D, George MJ, Harrison LB. Once‐weekly dosing of epoetin‐alpha increases hemoglobin and improves quality of life in anemic cancer patients receiving radiation therapy either concomitantly or sequentially with chemotherapy. Cancer 2003;98(5):1072‐9. [DOI] [PubMed] [Google Scholar]
Shi 2007 {published data only}
- Shi L, Hudges M, Yurgin N, Boye KS. Impact of dose frequency on compliance and health outcomes: A literature review (1966‐2006). Expert Review of Pharmacoeconomics and Outcomes Research 2007;7(2):187‐202. [DOI] [PubMed] [Google Scholar]
Shord 2009 {published data only}
- Shord SS, Auerbach M. Treating chemotherapy‐induced anemia following the revised labeling for ESAs. Community 2009;6(6):279‐82. [Google Scholar]
Spaeth 2010 {published data only}
- Spaeth 2010. [Epoetin beta for the treatment of chemotherapy‐induced anaemia in solid and haematological malignancies. Results of an open‐label, multicentric clinical trial]. Bulletin du cancer 2010;97(8):969‐78. [DOI] [PubMed] [Google Scholar]
Spicka 2004 {published data only}
- Spicka I, Beguin Y. Effect of anemia correction with epoetin beta (neorecormon) once weekly on performance status and disease response. Hematology Journal 2004, issue Suppl 2:abstract 553.
Steensma 2006 {published data only}
- Steensma DP, Molina R, Sloan JA, Nikcevich DA, Schaefer PL, Rowland KM, et al. Phase III study of two different dosing schedules of erythropoietin in anemic patients with cancer. Journal of Clinical Oncology 2006;24(7):1079‐89. [DOI] [PubMed] [Google Scholar]
- Steensma DP, Molina R, Sloan JA, Nikcevich DA, Schaefer Pl, Rowland KM, et al. A phase III randomized trial of two different dosing schedules of erythropoietin (EPO) in patients with cancer‐associated anemia: North Central Cancer Treatment Group (NCCTG) study N02C2. Journal of Clinical Oncology Vol. 23, issue 16s:abstract 8031.
Steensma 2011 {published data only}
- Steensma DP, Sloan JA, Dakhil SR, Dalton R, Kahanic SP, Prager DJ, et al. Phase III, randomized study of the effects of parenteral iron, oral iron, or no iron supplementation on the erythropoietic response to darbepoetin alfa for patients with chemotherapy‐associated anemia. Journal of Clinical Oncology 2011;29(1):97‐105. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stein 1991 {published data only}
- Stein RS, Abels RI, Krantz SB. Pharmacologic doses of recombinant human erythropoietin in the treatment of myelodysplastic syndromes. Blood 1991;78(7):1658‐63. [PubMed] [Google Scholar]
Steinmetz 2011 {published data only}
- Steinmetz HT, Tsamaloukas A, Schmitz S, Wiegand J, Rohrberg R, Eggert J, et al. A new concept for the differential diagnosis and therapy of anaemia in cancer patients. Supportive Care in Cancer 2011;19(2):261‐9. [DOI] [PubMed] [Google Scholar]
Stokoe 2009 {published data only}
- Stokoe, C. Adapting practice in the face of new data. Journal of Practice 2009;5(2):83‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stone 2008 {published data only}
- Stone PC, Minton O. Cancer‐related fatigue. European Journal of 2008;44(8):1097‐104. [DOI] [PubMed] [Google Scholar]
Straus 2002 {published data only}
- Straus DJ, Turner RR, Testa MA, Hayes JF, Sarokhan BJ. Epoetin Alfa treatment Improves Quality of Life and Increases Hemoglobin Levels during Chemotherapy for Lymphoma, Chronic Lymphocytic Leukemia (CLL)., and Multiple Myeloma (MM) Patients with Mild‐to‐Moderate Anemia. Blood, ASH Annual Meeting. 2002; Vol. ?, issue ?.
Straus 2006 {published data only}
- Straus DJ, Testa M, Riggs SA, Tulpule A, Sarokhan B. Early treatment with epoetin alfa improves anemia, quality of life, and productivity in patients with hematologic malignancies and mild anemia during chemotherapy. Blood 2003; Vol. 102:abstract 1811.
- Straus DJ, Testa MA, Sarokhan BJ, Czuczman MS, Tulpule A, Turner RR, et al. Quality‐of‐life and health benefits of early treatment of mild anemia: a randomized trial of epoetin alfa in patients receiving chemotherapy for hematologic malignancies. Cancer 2006;107(8):1909‐17. [DOI] [PubMed] [Google Scholar]
Stull 2010 {published data only}
- Stull DE, Vernon MK, Legg JC, Viswanathan HN, Fairclough D, Revicki DA. Use of latent growth curve models for assessing the effects of darbepoetin alfa on hemoglobin and fatigue. Contemporary Clinical Trials 2010;31(2):172‐9. [DOI] [PubMed] [Google Scholar]
Suzuki 2008ex {published data only}
- Suzuki Y, Tokuda Y, Fujiwara Y, Minami H, Ohashi Y, Saijo N. Weekly epoetin beta maintains haemoglobin levels and improves quality of life in patients with non‐myeloid malignancies receiving chemotherapy. Japanese Journal of Clinical Oncology 2008;38(3):214‐21. [DOI] [PubMed] [Google Scholar]
Tsukuda 1998 {published data only}
- Tsukuda M, Yuyama S, Kohno H, Itoh K, Kokatsu T, Kawai S. Effectiveness of weekly subcutaneous recombinant human erythropoietin administration for chemotherapy‐induced anemia. Biotherapy 1998;11:21‐5. [DOI] [PubMed] [Google Scholar]
Tzekova 2009 {published data only}
- Tzekova V, Mihaylov G, Elezovic I, Koytchev R, Epoetin Zeta Oncology Study Group. Therapeutic effects of epoetin zeta in the treatment of chemotherapy‐induced anaemia. Current Medical Research & Opinion 2009;25(7):1689‐97. [DOI] [PubMed] [Google Scholar]
Uhl 2007 {published data only}
- Uhl D. Cancer and chemotherapy associated anemia: Do erythropoietins worsen the prognosis?. Deutsche Apotheker Zeitung 2007;147(50):32‐3. [Google Scholar]
Vadhan‐Raj 2003 {published data only}
- Vadhan‐Raj S, Mirtsching B, Charu V, Terry D, Rossi G, Tomita D, et al. Assessment of hematologic effects and fatigue in cancer patients with chemotherapy‐induced anemia given darbepoetin alfa every two weeks. Journal of Supportive Oncology 2003;1(2):131‐8. [PubMed] [Google Scholar]
Vadhan‐Raj 2004 {published and unpublished data}
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Background information for Oncologic Drugs Advisory Committee Meeting, Safety of Erythropoietin Receptor Agonists (ERAs) in Patients With Cancer. Johnson and Johnson briefing document for FDA/ODAC hearing May 4, 2004; Gaithersburg, MD, Report Date: 30 MARCH 2004.
- Luksenburg H, Weir A, Wager R. EPO‐GBR‐7: Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen Inc. and Procrit (epoetin alfa) Ortho Biotech L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Oncologic Drugs Advisory Committee, Rockville (MD), USA, 2004; Vol. http://www.fda.gov/ohrms/dockets/ac/04/briefing/4037b2_04.pdf [date of last access March 27, 2009].
- Vadhan‐Raj S, Skibber JM, Crane C, Buesos‐Ramos CE, Rodriguez‐Bigas MA, Feig BW, et al. Randomized, double‐blind, placebo‐controlled trial of epoetin alfa (Procrit) in patients with rectal and gastric cancer undergoing chemo‐radiotherapy (CT/RT) followed by surgery: early termination of the trial due to increased incidence of thrombo‐embolic events (TEE). Blood. 2004; Vol. 104, issue 11:#2915.
Varan 1999 {published data only (unpublished sought but not used)}
- Buyukpamukcu M, Varan A, Kutluk T, Akyuz C. Is epoetin alfa a treatment option for chemotherapy‐related anemia in children?. Medical and Pediatric Oncology 2002;39(4):455‐8. [DOI] [PubMed] [Google Scholar]
- Varan A, Büyükpamukçu M, Kutluk T, Akyüz C. Recombinant human erythropoietin treatment for chemotherapy‐related anemia in children. Pediatrics 1999;103(2):E161‐4. [DOI] [PubMed] [Google Scholar]
Vekeman 2009 {published data only}
- Vekeman F, Bookhart BK, White J, McKenzie RS, Duh MS, Piech CT, et al. Impact of limiting erythropoiesis‐stimulating agent use for chemotherapy‐induced anemia on the United States blood supply margin.[see comment]. Transfusion 2009;49(5):895‐902. [DOI] [PubMed] [Google Scholar]
Velilla Millan 2003 {published data only}
- Velilla Millan C, Polo Jaime S, Lopez P, Navarrete Campos S, Valencia Julve J, Bascon Santolo N, et al. Effect of two administration schedules of erythropoietin upon hemoglobin in breast cancer patients treated with radiation therapy. [Spanish]. Oncologia (Madrid) 2003;26(8):45‐51. [Google Scholar]
Vorvaud 2007 {published data only}
- Voravud N, Sriuranpong V, Suwanrusme H. Antianemic effect of once weekly regimen of epoetin alfa 40,000 units in anemic cancer patients receiving chemotherapy. Journal of the Meical Association of Thailand 2007;90(0125‐2208 (Print), 0125‐2208 (Linking), 6):1082‐8. [PubMed] [Google Scholar]
Wagner 2004 {published data only}
- Wagner LM, Billups CA, Furman WL, Rao BN, Santana VM. Combined use of erythropoietin and granulocyte colony‐ stimulating factor does not decrease blood transfusion requirements during induction therapy for high‐risk neuroblastoma: A randomized controlled trial. Journal of Clinical Oncology 2004;22(10):1886‐93. [DOI] [PubMed] [Google Scholar]
Walsh 2010 {published data only}
- Walsh TS, Wyncoll DLA, Stanworth SJ. Managing anaemia in critically ill adults. BMJ 2010;341(7772):547‐51. [DOI] [PubMed] [Google Scholar]
Waltzman 2004 {published data only}
- Waltzman R WD. Head‐to‐head comparison of epoetin alfa (EPO) 40,000 QW vs darbepoetin alfa (DARB) 200 µg Q2W in anemic cancer patients receiving chemotherapy (CT): final results of a planned interim analysis (IA). Blood. 2004; Vol. 104, issue 11.
- Waltzman RJ. A randomized, active‐control, pilot trial of front‐loaded dosing regimens of darbepoetin‐alfa for the treatment of patients with anemia during chemotherapy for malignant disease. Cancer 2004;100(7):1545‐6. [DOI] [PubMed] [Google Scholar]
Waltzman 2005 {published data only}
- Waltzman R, Croot C, Justice GR, Fesen MR, Charu V, Williams D. Randomized comparison of epoetin alfa (40,000 U weekly) and darbepoetin alfa (200 microg every 2 weeks) in anemic patients with cancer receiving chemotherapy. The Oncologist 2005;10(8):642‐50. [DOI] [PubMed] [Google Scholar]
- Waltzman RJ, Croot C, Williams D. Final haematologic results: epoetin alfa (EPO) 40,000 U QW vs darbepoetin alfa (DARB) 200 µg Q2W in anemic cancer patients (pts) receiving chemotherapy (CT). Journal of Clinical Oncology 2005; Vol. 23, issue 16s:abstract 8030.
Wauters 2006 {published data only}
- Wauters I, Pat K, Vansteenkiste J. Flexible dosing with Darbepoetin alfa for the treatment of chemotherapy‐induced anemia. Therapeutics & Clinical Risk Management 2006;2(2):175‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2011 {published data only}
- WHO. Regulatory Action and News: Erythropoietin: withdrawal of marketing authorization application. WHO Drug Information 2011;25(2):125. [Google Scholar]
Yang 2008 {published data only}
- Yang S, Jun M, Hong‐Li Z, Jian‐Min W, Chun W, Lu‐Gui Q, et al. A multi‐center open‐labeled study of recombinant erythropoietin‐(beta) in the treatment of anemic patients with multiple myeloma, low‐grade non‐Hodgkin's lymphoma, or chronic lymphocytic leukemia in Chinese population. International Journal of Hematology 2008;88(2):139‐44. [DOI] [PubMed] [Google Scholar]
Yilmaz 2004 {published data only}
- Yilmaz D, Cetingul N, Kantar M, Oniz H, Kansoy S, Kavakli K. A single institutional experience: Is epoetin alpha effective in anemic children with cancer?. Pediatric Hematology & Oncology 2004;21(1):1‐8. [PubMed] [Google Scholar]
Yurut‐Caloglu 2008 {published data only}
- Yurut‐Caloglu V, Caloglu M. Treatment of anemia by recombinant human erythropoietin in cancer patients undergoing radiotherapy. Asia‐Pacific Journal of Clinical 2008;4(4):199‐207. [Google Scholar]
Zagari 2003 {published data only}
- Zagari M, Wacholz M, Xiu L. An open‐label, controlled, randomized, dose comparison study of epoetin alfa for the treatment of anemia in cancer patients receiving platinum‐containing chemotherapy. The Hematology Journal 2003;61(4 Suppl 2):abstract 0177. [Google Scholar]
Zaragoza 2004 {published data only}
- Queipo Zaragoza JA, Chicote Perez F, Beltran Meseguer JF, Borrell Palanca A, Giner Marco V, Esteve Claramunt J, Pastor Sempere F. Improvement of anemia and quality of life of patients with prostate cancer by treatment with human recombinant erythropoietin [Mejora de la anemia y calidad de vida en pacientes con cáncer de próstata mediante la administración de eritropoyetina humana recombinante]. Archivos españoles de urología 2004;57(1):35‐40. [PubMed] [Google Scholar]
Zhang 2003 {published data only}
- Zhang XF, Shi JG, Yang Y. Clinical observations on RHuEPO in the treatment of breast cancer chemotherapy related anemia. China Journal of Cancer Prevention and Treatment 2003;10(8):861‐2. [Google Scholar]
Zhou 2006 {published data only}
- Zhou L‐X, Wu W‐X, Li M, Yu W‐J. Clinical observation of recombinant human erythropoietin in treatment of preoperative anemia in patients with gastric cancer. Pharmaceutical Care & Research (Yaoxue Fuwu Yu Yanjiu) 2006;6(5):355‐7. [Google Scholar]
References to ongoing studies
Blackstock {unpublished data only}
- Blackstock AW. A phase III randomised trial evaluating the effect of eüpetin alfa (procrit) on local control in patietns undergoing cocnurrent chemotherapy and radiation therapy for non‐small cell lung cancer. NCT00028938. ClinicalTrials.gov last updated August 2009.
Boehrer 2010 {published data only}
- Boehrer S, Beyne‐Rauzy O, Prebet T, Park S, Guerci A, Stamatoulas A, et al. Interim Results of A Randomized Phase II Trial of Azacitidine (AZA) +/‐ Epo In Lower Risk Myelodysplastic Syndrome (MDS) Resistant to An Erythropoietic Stimulating Agent (ESA) Alone. Blood (ASH Annual Meeting Abstracts) 2010;116(21):1880. [Google Scholar]
Broadley {unpublished data only}
- Broadley K. Double blind randomised placebo controlled trial of the effect of epoetin alfa on symptomatic anaemia and fatigue in cancer patients receiving ongoing care without planned chemotherapy. N0258040123. National Research Register 2003.
Chapman 2004 {unpublished data only}
- Chapman CS. A randomised comparison of the effect of maintaining haemoglobin levels with weekly epoetin alfa or with conventional anaemia management in subjects with multiple myeloma undergoing chemotherapy (EMMY). N0123138194. NRR 2004.
Delarue 2009 {published data only}
- Delarue R, Haioun C, Broussais‐Guillaumot F, Sibon D, Fournier M, Mounier N, et al. Efficacy and safety of prophylactic use of darbepoetin alfa in patients with diffuse large B‐cell lymphoma (DLBCL) treated with immunochemotherapy: results of the interim analysis of the LNH03‐6B GELA Study. Blood 2009;114(22):Abstract 1701. [Google Scholar]
EPO CAN 303 {unpublished data only}
- EPO‐CAN‐303. Treatment of anaemic patients with cancer who are not receiving chemotherapy or radiotherapy. ClinicalTrials.gov Last updated 2007.
Famoyin 2004 {published data only}
- Famoyin C, Byrnes C, Roberts S, Gollob M, Atkins M, Mier J, et al. A randomized phase II study of thalidomide with or without erythropoietin (EPO) in metastatic renal cell carcinoma (RCC). Journal of Clinical Oncology. 22 2004; Vol. 22, issue 14S.
Fisch {unpublished data only}
- Fisch MJ. Epoetin Alfa in treating fatigue in patients with advanced solid tumors who are not receiving chemotherapy. NCT00052221. ClinicalTrials.gov Last updated 2009.
Gallagher {unpublished data only}
- Gallagher C. The role of epoetin alpha in anaemia and fatigue in cancer patients. N0205036683. National Research Register 2003.
Gamucci 1993 {published data only}
- Gamucci T, Thorel MF, Frasca AM, Giannarell D, Calabresi F. Erythropoietin for the prevention of anaemia in neoplastic patients treated with cisplatin. European Journal of Cancer 1993;29A Suppl 2:13‐4. [DOI] [PubMed] [Google Scholar]
Gascon 2010 {published data only}
- Gascon P, Henry DH, Fleishman A, Borenstein JE. Design of an ongoing randomized study on the long‐term safety and efficacy of darbepoetin alfa (DA) administered 500 mcg every three weeks (Q3W) to non‐small cell lung cancer (NSCLC) patients (pts) with anemia concomitant with chemotherapy (ACC). Journal of Clinical Oncology 2010;28(15):Abstract TPS325. [Google Scholar]
Ghavamzadeh 2010 {published data only}
- Ghavamzadeh A, Alimoghaddam K, Jahani M, Hamidieh AA, Mousavi SA, Khatami F, et al. Randomized, double blind, placebo‐controlled phase III study of weekly administration of darbepoetin alfa in anemic patients with lung or gynecologic cancer receiving platinum‐containing chemotherapy. ABMT 2010 Annual Meeting. 2010.
Howell {unpublished data only}
- Howell A. A double‐blind, randomised, placebo‐controlled study to evaluate the impact of maintaining haemoglobin using Epres R (epoetin alpha) in stage IV breast cancer sugjects receiving chemotherapy. N0063096721. National Research Register 2003.
H Thomas 1997 {unpublished data only}
- H Thomas. Open label comparative evaluation of the effect of epoetin on quality of life and burden of illness in anaemic patients receiving platinum‐containing chemotherapy. Cochrane Review 1997.
Koelbl {unpublished data only}
- Koelbl H. Epoetin beta in treating anemia in patients with cervical cancer. NCT00046969. ClinicalTrials.gov Last updated 2009.
Lambin 2006 {published data only}
- Lambin P. Radiation therapy with or without epoetin alfa in treating patients with head and neck cancer. NCT00017277. ClinicalTrials.gov Last updated 2009.
Liang 2009 {published data only}
- Liang J, Qing B, Shen L, Cheng H. The clinical study on recombinant human erythropoietin for chemotherapy ‐ related anaemia. Clinical Research 2009;29(1):58‐60. [Google Scholar]
Nitz 2008 {published data only}
- Nitz U, Oberhoff C, Reimer T, Schumacher C, Hackmann J, Warm M et al. West German Study Group, Moenchengladbach, Germany, Marienhospital, Essen, Germany, Klinikum Suedstadt, Rostock, Germany, St. Elisabeth KH, Koeln, Germany, Uni Koeln, Koeln, Germany, HZM Pharmaservice, Wiesbaden, Germany, Praxis Gyn. Onko, Hildesheim, Germany, Wilhelm‐Anton‐H, Goch, Germany. Adjuvant chemotherapy with or without darbepoetin in node‐positive breast cancer: a safety analysis from the phase III ARA plus trial.. San Antonio Breast Cancer Symposium 2008:4100.
O´Brien {unpublished data only}
- O'Brien. Open‐label randomised group‐comparative evaluation of the effect of epoetin on anaemia and fatigue in lung cancer patients receiving palliative platinumcontaining chemotherapy. Cochrane Review 1998.
O´Connell {unpublished data only}
- O'Connell MJ. Phase III Randomised study of epoetin alpha in anemic patients with advanced cancer undergoing chemotherapy.NCCTG‐979253/ NCT00003600. Cancer.gov, ClinicalTrials.gov Last updated 2009.
Park 1996 {published data only}
- Park HS, Hong DS, Lee SJ, Chung TJ, Choi YM. Clinical evaluation of recombinant human erythropoietin(Eprex r) in anemic cancer patients receiving chemotherapy. Annals of Oncology 1996;7(Suppl 5):63. [Google Scholar]
Parliament {unpublished data only}
- Parliament M. Phase III randomised study of radiotherapy with or without epoetin alfa in anemic patients with squamous cell carcinoma of the head and neck. ClinicalTrials.gov.
Recasens 2003 {published data only}
- Recasens V, Rubio‐Martinez A, Gomez‐Barrera M, Rubio‐Felix D, Giralt M, Giraldo P. A pharmacoeconomical analysis comparing Epoetin Alpha vs transfusion in patients with anemia associated to multiple myeloma. Blood. 2003; Vol. 102, issue 11.
- Rubio‐Martinez A, Recasens B, et al. Anemia associated to multiple myeloma: repsonse to epoetin alpha. Hematology Journal 2003;4(S1):S202. [Google Scholar]
Rexer 2006 {published data only}
R Thomas 2002 {unpublished data only}
- R Thomas. Open‐label comparative group evaluation of the effect of epoetin alfa on quality of life and burden of illness in anaemic cancer patients receiving platinum containing chemotherapy. N0040004850. Current cotrolled trials 2002.
Rudd {unpublished data only}
- Rudd M. Evaluation of epoetin alpha in lung cancer patients receiving chemotherapy. N0205036678. Current Controlled Trials 2002.
Stewart {unpublished data only}
- Stewart JSW. Open randomised comperative group evaluation of the effect of epoetin alfa on local disease free survival and quality of life in head and neck cancer patients receiving radical radiotherapy. N0016089950. Current Controolled Trials 2002.
UKCCCR GN308 {unpublished data only}
- UKCCCR GN308. A double‐blind, placebo‐controlled study to assess the effects of early intervention and/or treatment with epoetin alfa on anaemia in cancer patients receiving non‐platinum containing chemotherapy. ISRCTN Register 2009.
Yousseff 2011 {published data only}
- Youssef Lama A, Hussien Dilman Haj, Sulaiman Siham. The effectiveness of a fixed low dose of erythropoietin (EPO) in anemic solid tumor patients receiving concomitant chemotherapy: a prospective, randomized, controlled study. ASH Annual Meeting Abstracts 2011;118(21):2092. [Google Scholar]
Ziras 2001 {published data only}
- Ziras N, Rozakou AJ, Potamianou A, Kouloubinis A, Drakos S, Giannakakis T, et al. Soluble transferrin receptor (sTFR) as a predictor of response to prophylactic epoetin alfa (EPO) treatment in non‐anemic cancer patients (pts) under chemotherapy (CT). Preliminary results. Proceedings of the American Society of Clincal Oncology 2001;20:Abstract #2987. [Google Scholar]
Additional references
Aapro 2006
- Aapro M, Coiffier B, Dunst J, Osterborg A, Burger HU. Effect of treatment with epoetin beta on short‐term tumour progression and survival in anaemic patients with cancer: A meta‐analysis. British Journal of Cancer 2006;95(11):1467‐73. [PUBMED: 17117175] [DOI] [PMC free article] [PubMed] [Google Scholar]
Aapro 2009a
- Aapro M, Barnadas A, Leonard RC, Marangolo M, Untch M, Ukarma L, et al. What is the impact of antithrombotic therapy and risk factors on the frequency of thrombovascular events in patients with metastatic breast cancer receiving epoetin beta?. European Journal of Cancer (Oxford, England : 1990) 2009;45(17):2984‐91. [PUBMED: 19646862] [DOI] [PubMed] [Google Scholar]
Aapro 2009b
- Aapro M, Osterwalder B, Scherhag A, Burger HU. Epoetin‐beta treatment in patients with cancer chemotherapy‐induced anaemia: the impact of initial haemoglobin and target haemoglobin levels on survival, tumour progression and thromboembolic events. British Journal of Cancer 2009;101(12):1961‐71. [PUBMED: 19997109] [DOI] [PMC free article] [PubMed] [Google Scholar]
Aaronson 1991
- Aaronson NK. Methodologic issues in assessing the quality of life in cancer patients. Cancer 1991;67:844‐50. [DOI] [PubMed] [Google Scholar]
Acs 2001
- Acs G, Acs P, Beckwith SM, Pitts RL, Clements E, Wong K, et al. Erythropoietin and erythropietin receptor expression in human cancer. Cancer Research 2001;61:3561‐5. [PubMed] [Google Scholar]
Acs 2002
- Acs G, Zhang PJ, Rebbeck TR, Acs P, Verma A. Immunohistochemical expression of erythropoietin and erythropoietin receptor in breast carcinoma. Cancer 2002;95(5):969‐81. [DOI] [PubMed] [Google Scholar]
Alderson 2005
- Alderson P, Green S, Higgins JPT. Assessment of study quality. Cochrane Reviewers' Handbook 4.2.2 [updated March 2004]. Chichester, UK: John Wiley & Sons, Ltd., 2005. [Google Scholar]
Amgen ODAC 2004
- Amgen Inc. Aranesp (darbepoetin alfa) Safety. Oncologic Drugs Advisory Committee; 4 May 2004.
Amgen ODAC 2007
- Amgen Thousand Oaks. Safety of Erythropoiesis‐Stimulating Agents (ESAs) in Oncology. 2007 ODAC Meeting Information Package Darbepoetin alfa and Epoetin alfa; BACKGROUND INFORMATIONFORONCOLOGIC DRUGS ADVISORY COMMITTEE 10 May 2007.
Amgen ODAC 2008
- Amgen in collaboration with Johnson & Johnson. ODAC Meeting Briefing Document Epoetin alfa (Epogen®/PROCRIT®) and darbepoetin alfa (Aranesp®) [THE ONCOLOGIC DRUGS ADVISORY COMMITTEE (ODAC) MEETING 13 March 2008]. http://www.fda.gov/ohrms/dockets/ac/08/briefing/2008‐4345b2‐00‐FDA‐index.htm 13 March 2008.
Arcasoy 2002
- Arcasoy MO, Amin K, Karayal AF, Chou SC, Raleigh JA, Varia MA, et al. Functional significance of erythropoietin receptor expression in breast cancer. Laboratory Investigation 2002;82(7):911‐8. [DOI] [PubMed] [Google Scholar]
Barbera 2010
- Barbera L, Thomas G. Erythropoiesis stimulating agents, thrombosis and cancer. Radiotherapy and Oncology: Journal of the European Society for Therapeutic Radiology and Oncology 2010;95(3):269‐76. [PUBMED: 20219259] [DOI] [PubMed] [Google Scholar]
Becker 2000
- Becker A, Stadler P, Lavey RS, Hansgen G, Kuhnt T, Lautenschlager C, et al. Severe anemia is associated with poor tumor oxygenation in head and neck squamous cell carcinomas. International Journal of Radiation Oncology, Biology, Physics 2000;46(2):459‐66. [DOI] [PubMed] [Google Scholar]
Beguin 1998
- Beguin Y. A Risk‐benefit assessment of epoetin in the management of anaemia associated with cancer. Drug Safety 1998;19(4):269‐82. [DOI] [PubMed] [Google Scholar]
Bennett 2008
- Bennett CL, Silver SM, Djulbegovic B, Samaras AT, Blau CA, Gleason KJ, et al. Venous thromboembolism and mortality associated with recombinant erythropoietin and darbepoetin administration for the treatment of cancer‐associated anemia. JAMA 2008;299(8):914‐24. [PUBMED: 18314434] [DOI] [PubMed] [Google Scholar]
Bennett 2010
- Bennett CL, Lai SY, Henke M, Barnato SE, Armitage JO, Sartor O. Association between pharmaceutical support and basic science research on erythropoiesis‐stimulating agents. Archives of Internal Medicine 2010;170(16):1490‐8. [PUBMED: 20837837] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bohlius 2009a
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Erythropoietin or darbepoetin for patients with cancer ‐ meta‐analysis based on individual patient data. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007303.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bohlius 2009b
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, et al. Recombinant human erythropoiesis‐stimulating agents and mortality in patients with cancer: a meta‐analysis of randomised trials. Lancet 2009;373(9674):1532‐42. [DOI] [PubMed] [Google Scholar]
Bottomley 2002
- Bottomley A, Thomas R, Steen K, Flechtner H, Djulbegovic B. Human recombinant erythropoietin and quality of life: a wonder drug or something to wonder about?. Lancet Oncology 2002;3:145‐53. [DOI] [PubMed] [Google Scholar]
Brandberg 2000
- Brandberg Y. Assessing the impact of cancer‐related anaemia on quality of life and the role of rHuEPO. Medical Oncology 2000;17(Suppl. 1):S23‐S31. [PubMed] [Google Scholar]
Caro 2001
- Caro JJ, Salas M, Ward A, Goss G. Anemia as an independent prognostic factor for survival in patients with cancer: a systemic, quantitative review. Cancer 2001;91(12):2214‐21. [PUBMED: 11413508] [PubMed] [Google Scholar]
Carson 2012
- Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK et al: for the Clinical Transfusion Medicine Committee of the AABB. Red blood cell transfusion: a clinical practice guideline from the AABB. Annals of Internal Medicine 26 March 2012;Published online:N/A. [DOI] [PubMed] [Google Scholar]
Cella 1997
- Cella, D. The Functional Assessment of Cancer Therapy‐Anemia (FACT‐An) Scale: a new tool for the assessment of outcomes in cancer anemia and fatigue. Seminars in Hematology 1997;34(3 Suppl 2):13‐9. [PubMed] [Google Scholar]
Cella 1998
- Cella D. Factors influencing quality of life in cancer patients: anemia and fatigue. Seminars in Oncology 1998;25(3 Suppl 7):43‐6. [PubMed] [Google Scholar]
Cella 1999
- Cella D, Bron D. The effect of epoetin alfa on quality of life in anemic cancer patients. Cancer Practice 1999;7:177‐82. [DOI] [PubMed] [Google Scholar]
Cella 2002
- Cella D, Eton DT, Lai JS, Peterman AH, Merkel DE. Combining anchor and distribution‐based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. Journal of Pain and Symptom Mmanagement 2002;24:547‐61. [DOI] [PubMed] [Google Scholar]
Cella 2004
- Cella D, Kallich J, McDermott A, Xu X. The longitudinal relationship of hemoglobin, fatigue and quality of life in anemic cancer patients: results from five randomized clinical trials. Annals of Oncology : official journal of the European Society for Medical Oncology / ESMO 2004;15(6):979‐86. [PUBMED: 15151958] [DOI] [PubMed] [Google Scholar]
Cella 2007
- Cella D. The Functional Assessment of Chronic Illness Therapy‐Fatigue (FACIT‐F) Scale: Summary of development and validation. Elmhurst, IL, FACIT.org 2007.
Cirillo 1993
- Cirillo M, Capasso G, DeSanto NG. Relationship between hematocrit and blood pressure: implications for primary hypertension. Nephron 1993;65:505‐10. [DOI] [PubMed] [Google Scholar]
Clark 2002
- Clark O, Adams JR, Bennett CL, Djulbegovic B. Erythropoietin, uncertainty principle and cancer related anaemia. BMC Cancer 2002;2(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dalton 1998
- Dalton JD, Bailey NP, Barrett‐Lee PJ, O´Brien MER. Multicenter UK audit of anemia in patients receiving cytotoxic chemotherapy. American Society of Clinical Oncology. 1998:Abstract #1611.
Deeks 1997
- Deeks J. Are you sure that's a standard deviation?. Cochrane News 1997, issue 11:11‐2.
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta‐analyses.. Higgins JPT, Green S, editor(s). Cochrane Handbook of Systematic Reviews of Interventions, version 5.1.0 (updated March 2011) 2011.
Devon 2009
- Devon KM, McLeod RS. Pre and peri‐operative erythropoeitin for reducing allogeneic blood transfusions in colorectal cancer surgery. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD007148.pub2; PUBMED: 19160325] [DOI] [PubMed] [Google Scholar]
D´Andrea 1989
- D´Andrea AD, Lodish HF, Wong GG. Expression cloning of the murine erythropoietin receptor. Cell 1989;57:277‐85. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Engert 2000
- Engert A. Recombinant human erythropoietin as an alternative to blood transfusion in cancer‐related anaemia. Disease Management and Clinical Outcomes 2000;8(5):259‐72. [Google Scholar]
Fairclough 2003
- Fairclough DL, Gagnon DD, Zagari MJ, Marschner N, Dicato M. Evaluation of quality of life in a clinical trial with nonrandom dropout: the effect of epoetin alfa in anemic cancer patients. Quality of Life Research 2003;12(8):1013‐27. [DOI] [PubMed] [Google Scholar]
FDA 2010
- FDA Drug Safety Communication: Erythropoiesis‐Stimulating Agents (ESAs): Procrit, Epogen and Aranesp. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm200297.htm.
FDA ODAC 2007
- FDA. Continuing Reassessment of the Risks of Erythropoiesis‐Stimulating Agents (ESAs) Administered for the Treatment of Anemia associated with Cancer Chemotherapy. FDA BRIEFING DOCUMENT May 10, 2007 Oncologic Drugs Advisory Committee.
FDA ODAC 2008
- FDA BRIEFING DOCUMENT March 13, 2008, Oncologic Drugs Advisory Committee. http://www.fda.gov/ohrms/dockets/ac/08/briefing/2008‐4345b2‐00‐FDA‐index.htm March 13 2008.
Frommhold 1998
- Frommhold H, Guttenberger R, Henke M. The impact of blood hemoglobin content on the outcome of radiotherapy. The Freiburg experience. Strahlentherapie und Onkologie 1998;174(Suppl IV):31‐4. [PubMed] [Google Scholar]
Fuste 2002
- Fuste B, Serradell M, Escolar G, Cases A, Mazzara R, Castillo R, et al. Erythropoietin triggers a signaling pathway in endothelial cells and increases the thrombogenicity of their extracellular matrices in vitro. Thrombosis and haemostasis 2002;88(4):678‐85. [PUBMED: 12362243] [PubMed] [Google Scholar]
Ganz 2011
- Ganz T. Hepcidin and iron regulation, 10 years later. Blood 2011;117(17):4425‐33. [PUBMED: 21346250] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gascon 2010b
- Gascon P, Pirker R, Mastro L, Durrwell L. Effects of CERA (continuous erythropoietin receptor activator) in patients with advanced non‐small‐cell lung cancer (NSCLC) receiving chemotherapy: results of a phase II study. Annals of Oncology : official journal of the European Society for Medical Oncology / ESMO 2010;21(10):2029‐39. [PUBMED: 20335369] [DOI] [PubMed] [Google Scholar]
Glaspy 1997a
- Glaspy J. The impact of epoetin alfa on quality of life during cancer chemotherapy: a fresh look at an old problem. Seminars in Hematology 1997;34 Suppl 2:20‐6. [PubMed] [Google Scholar]
Glaspy 2010
- Glaspy J, Crawford J, Vansteenkiste J, Henry D, Rao S, Bowers P, et al. Erythropoiesis‐stimulating agents in oncology: a study‐level meta‐analysis of survival and other safety outcomes. British Journal of Cancer 2010;102(2):301‐15. [PUBMED: 20051958] [DOI] [PMC free article] [PubMed] [Google Scholar]
Goodnough 1999
- Goodnough LT, Brecher ME, Kanter MH, AuBuchon JP. Transfusion medicine ‐ blood transfusion ‐ second of two parts. New England Journal of Medicine 1999;340(7):525‐33. [DOI] [PubMed] [Google Scholar]
Grau 2000
- Grau C, Overgaard J. Significance of hemoglobin concentration for treatment outcome. In: Molls M, Vaupel P editor(s). Blood Perfusion and Microenvironment of Human Tumors. Berlin: Springer, 2000:101‐12. [Google Scholar]
Greenberg 1994
- Greenberg PL. The myelodysplastic syndromes. In: Hoffmann R, Benz E, Shattil S, Furie B, Cohen H editor(s). Hematology: Basic Principles and Practice. New York, NY: Churchill Livingstone, 1994:1098. [Google Scholar]
Groopman 1999
- Groopman JE, Itri LM. Chemotherapy‐Induced Anemia in Adults: Incidence and Treatment. Journal of the National Cancer Institute 1999;91(19):1616‐34. [DOI] [PubMed] [Google Scholar]
Halstenson 1991
- Halstenson CE, Macres M, Katz SA, Schnieders JR, Watanabe M, Sobota JT, et al. Comparative pharmacokinetics and pharmacodynamics of epoetin alfa and epoetin beta. Clinical Pharmacology and Therapeutics 1991;50:702‐12. [DOI] [PubMed] [Google Scholar]
Harrison 2001
- Harrison L, Shasha D, Shiaova L, White C, Ramdeen B, Portenoy R. Prevalence of anemia in cancer patients undergoing radiation therapy. Seminars in Oncology 2001;28(2 Suppl 8):54‐9. [DOI] [PubMed] [Google Scholar]
Hasenclever 1998
- Hasenclever D, Diehl V. A prognostic score for advanced Hodgkin's disease. International Prognostic Factors Project on Advanced Hodgkin's Disease. New England Journal of Medicine 1998;339:1506‐14. [DOI] [PubMed] [Google Scholar]
Hedenus 2005
- Hedenus M, Vansteenkiste J, Kotasek D, Austin M, Amado RG. Darbepoetin alfa for the treatment of chemotherapy‐induced anemia: disease progression and survival analysis from four randomized, double‐blind, placebo‐controlled trials. Journal of Clinical Oncology : official journal of the American Society of Clinical Oncology 2005;23(28):6941‐8. [PUBMED: 16192582] [DOI] [PubMed] [Google Scholar]
Hellström‐L 1995
- Hellström‐Lindberg E. Efficacy of erythropoietin in the myelodysplastic syndromes: a meta‐analysis of 205 patients from 17 studies. British Journal of Haematology 1995;89:67‐71. [DOI] [PubMed] [Google Scholar]
Henke 2000
- Henke M, Guttenberger R. Erythropoietin in radiation oncology ‐ a review. Oncology 2000;58:175‐82. [DOI] [PubMed] [Google Scholar]
Henke 2006
- Henke M, Mattern D, Pepe M, Bezay C, Weissenberger C, Werner M, et al. Do erythropoietin receptors on cancer cells explain unexpected clinical findings?. Journal of Clinical Oncology : official journal of the American Society of Clinical Oncology 2006;24(29):4708‐13. [PUBMED: 17028293] [DOI] [PubMed] [Google Scholar]
Henry 1992
- Henry DH. Changing patterns of care in the management of anemia. Seminars in Oncology 1992;19:3‐7. [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S. Chapter 8: Assessing risk of bias in included studies.. Higgins JPT, Green S, editor(s). Cochrane Handbook of Systematic Reviews of Interventions 5.1.0 (updated March 2011) 2011.
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG. Chapter 16: Special topics in statistics. Higgins JPT, Green S, editor(s). Cochrane Handbook of Systematic Reviews of Intervetions, Version 5.1.0 (updated March 2011) 2011.
Hirst 1984
- Hirst DG, Hazlehurst JL, Brown JM. The effect of alterations in haematocrit on tumour sensitivity to X‐rays. International Journal of Radiation Biology and Related Studies in Physics, Chemistry, and Medicine 1984;46(4):345‐54. [DOI] [PubMed] [Google Scholar]
Hockel 1993
- Hockel M, Knoop C, Schlenger K, Vorndran B, Baussmann E, Mitze M, et al. Intratumoral pO2 predicts survival in advanced cancer of the uterine cervix. Radiotherapy Oncology 1993;26:45‐50. [DOI] [PubMed] [Google Scholar]
Hozo 2005
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology 2005;5(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ihaka 1996
- Ihaka R, Gentleman R. R: A language for Data Analysis and Graphics. Journal of Computational and Graphical Statistics 1996;5(3):299‐314. [Google Scholar]
Jelkmann 2004
- Jelkmann W, Wagner K. Beneficial and ominous aspects of the pleiotropic action of erythropoietin. Annals of Hematolology 2004;83(11):673‐86. [DOI] [PubMed] [Google Scholar]
Jelkmann 2008
- Jelkmann W, Bohlius J, Hallek M, Sytkowski AJ. The erythropoietin receptor in normal and cancer tissues. Critical Reviews in Oncology/Hematology 2008;67(1):39‐61. [PUBMED: 18434185] [DOI] [PubMed] [Google Scholar]
Jelkmann 2010
- Jelkmann W. Biosimilar epoetins and other "follow‐on" biologics: update on the European experiences. American Journal of Hematology 2010;85(10):771‐80. [PUBMED: 20706990] [DOI] [PubMed] [Google Scholar]
Johnson & Johnson ODAC 2004
- Johnson & Johnson Pharmaceutical Research & Development, L.L.C. Safety of Erythropoietin Receptor Agonists (ERAs) in Patients With Cancer. Background Information For Oncologic Drugs Advisory Committee Meeting. May 4 2004.
Johnson 1990
- Johnson CS, Cook CA, Furmanski P. In vivo supression of erythropoiesis by tumor necrosis factor‐alpha (TNF‐alpha): Reversal with exogenous erythropoietin (EPO). Experimental Hematology 1990;18:109‐13. [PubMed] [Google Scholar]
Joiner 1993
- Joiner B, Hirst VK, McKeown SR, McAleer JJ, Hirst DG. The effect of recombinant human erythropoietin treatment on tumour radiosensitivity and cancer‐associated anaemia in the mouse. Brirish Joural of Cancer 1993;68(4):720‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2004
- Jones M, Schenkel B, Just J, Fallowfield L. Epoetin alfa improves quality of life in patients with cancer: results of metaanalysis. Cancer 2004;101(8):1720‐32. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Joy 2002
- Joy MS. Darbepoetin alfa: a novel erythropoiesis‐stimulating protein. Annals of Pharmacotherapy 2002;36:1183‐92. [DOI] [PubMed] [Google Scholar]
Jüni 1999
- Jüni P, Witschi A, Bloch R, Egger M. The hazards of scoring the quality of clinical trials for meta‐analysis. JAMA 1999;282:1054‐60. [DOI] [PubMed] [Google Scholar]
Jüni 2001
- Jüni P, Altman DG, Egger M. Assessing the quality of controlled clinical trials. BMJ 2001;323:42‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kelleher 1998
- Kelleher DK, Thews O, Vaupel P. Can erythropoietin improve tumor oxygenation?. Strahlentherapie und Onkologie 1998;174(Suppl IV):20‐3. [PubMed] [Google Scholar]
Kimel 2008
- Kimel M, Leidy NK, Mannix S, Dixon J. Does epoetin alfa improve health‐related quality of life in chronically ill patients with anemia? Summary of trials of cancer, HIV/AIDS, and chronic kidney disease. Value in Health : the journal of the International Society for Pharmacoeconomics and Outcomes Research 2008;11(1):57‐75. [PUBMED: 18237361] [DOI] [PubMed] [Google Scholar]
Knight 2004
- Knight K, Wade S, Balducci L. Prevalence and outcomes of anemia in cancer: a systematic review of the literature. The American Journal of Medicine 2004;116 Suppl 7A:11S‐26S. [PUBMED: 15050883] [DOI] [PubMed] [Google Scholar]
Knocke 1999
- Knocke TH, Weitmann HD, Feldmann HJ, Selzer E, Potter R. Intratumoral pO2‐measurements as predictive assay in the treatment of carcinoma of the uterine cervix. Radiotherapy and Oncology 1999;53(2):99‐104. [DOI] [PubMed] [Google Scholar]
Koeller 1998
- Koeller JM. Clinical guidelines for the treatment of cancer‐related anemia. Pharmacotherapy 1998;18:156‐69. [PubMed] [Google Scholar]
Koong 1991
- Koong AC, Hirst DG. The influence of chronic anaemia on the radiosensitivity of two mouse tumours. Brirish Journal of Cancer 1991;63(4):499‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koury 1988
- Koury ST, Bondurant MC, Koury MJ. Localization of erythropoietin synthesizing cells in murine kidneys by in situ hybridization. Blood 1988;71:524‐7. [PubMed] [Google Scholar]
Koury 1990
- Koury MJ, Bondurant MC. Control of red cell production: the roles of programmed cell death (apoptosis) and erythropoietin. Transfusion 1990;30:673‐4. [DOI] [PubMed] [Google Scholar]
Koury 1991
- Koury ST, Bondurant MC, Koury MJ. Localization of cells producing erythropoietin in murine liver by in situ hybridization. Blood 1991;77:2497‐503. [PubMed] [Google Scholar]
Lambin 2009
- Lambin P, Ramaekers BL, Mastrigt GA, Ende P, Jong J, Ruysscher DK, et al. Erythropoietin as an adjuvant treatment with (chemo) radiation therapy for head and neck cancer. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD006158.pub2; PUBMED: 19588382] [DOI] [PMC free article] [PubMed] [Google Scholar]
Landers 1996
- Landers DF, Hill GE, Wong KC, Fox IJ. Blood transfusion‐induced immunomodulation. Anesthesia and Analgesia 1996;82:187‐204. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies.. Higgins JPT Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (update March 2011). 2011.
Ludwig 1990
- Ludwig H, Fritz E, Kotzmann H, Hocker P, Gisslinger H, Barnas U. Erythropoietin treatment of anemia associated with multiple myeloma. New England Journal of Medicine 1990;322(24):1693‐9. [DOI] [PubMed] [Google Scholar]
Ludwig 1998
- Ludwig H, Fritz E. Anemia in cancer patients. Seminars in Oncology 1998;25(3 Suppl 7):2‐6. [PubMed] [Google Scholar]
Ludwig 2001
- Ludwig H, Strasser K. Symptomatology of anemia. Seminars in Oncology 2001;28(2, Suppl 8):7‐14. [DOI] [PubMed] [Google Scholar]
Ludwig 2009
- Ludwig H, Crawford J, Osterborg A, Vansteenkiste J, Henry DH, Fleishman A, et al. Pooled analysis of individual patient‐level data from all randomized, double‐blind, placebo‐controlled trials of darbepoetin alfa in the treatment of patients with chemotherapy‐induced anemia. Journal of Clinical Oncology : official journal of the American Society of Clinical Oncology 2009;27(17):2838‐47. [PUBMED: 19380447] [DOI] [PubMed] [Google Scholar]
Luksenburg 2004
- Luksenburg H, Weir A, Wager R. Safety Concerns Associated with Aranesp (darbepoetin alfa) Amgen, Inc. and Procrit (epoetin alfa) Ortho Biotech, L.P., for the Treatment of Anemia Associated with Cancer Chemotherapy. FDA Briefing Document May 4, 2004 Oncologic Drugs Advisory Committee 2004.
Malyszko 1995
- Malyszko J, Malyszko JS, Borawski J, Rydzewski A, Kalinowski M, Azzadin A, et al. A study of platelet functions, some hemostatic and fibrinolytic parameters in relation to serotonin in hemodialyzed patients under erythropoietin therapy. Thrombosis Research 1995;77(2):133‐43. [PUBMED: 7740505] [DOI] [PubMed] [Google Scholar]
McKinney 2011
- McKinney M, Arcasoy MO. Erythropoietin for oncology supportive care. Experimental Cell Research 2011;317(9):1246‐54. [PUBMED: 21396935] [DOI] [PubMed] [Google Scholar]
Mercadante 2000
- Mercadante S, Gebbia V, Marrazzo A, Filosto S. Anaemia in cancer: pathophysiology and treatment. Cancer Treatment Reviews 2000;26:303‐11. [DOI] [PubMed] [Google Scholar]
Minton 2008
- Minton O, Richardson A, Sharpe M, Hotopf M, Stone P. A systematic review and meta‐analysis of the pharmacological treatment of cancer‐related fatigue. Journal of the National Cancer Institute 2008;100(16):1155‐66. [DOI] [PubMed] [Google Scholar]
Minton 2010
- Minton O, Richardson A, Sharpe M, Hotopf M, Stone P. Drug therapy for the management of cancer‐related fatigue. Cochrane Database of Systematic Reviews 2010, Issue 7. [DOI: 10.1002/14651858.CD006704.pub3; PUBMED: 20614448] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2001
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomised trials. Lancet 2001;357(9263):1191‐4. [PubMed] [Google Scholar]
Monnerat 1999
- Monnerat C, Leyvraz S. Tumor anemia. Overview of the role of human recombinant erythropoietin (r‐hu‐EPO)in treatment of tumor anemia (in German). Schweizerische Rundschau für Medizin 1999;88:178‐88. [PubMed] [Google Scholar]
Nissenson 1992
- Nissenson AR. Epoetin and cognitive function. American Journal of Kidney Diseases 1992;20:21‐4. [PubMed] [Google Scholar]
Nordsmark 1996
- Nordsmark M, Overgaard M, Overgaard J. Pretreatment oxygenation predicts radiation response in advanced squamous cell carcinoma of the head and neck. Radiotherapy Oncology 1996;41:31‐9. [DOI] [PubMed] [Google Scholar]
Nowrousian 2002a
- Nowrousian MR. Pathophysiology of cancer‐related anemia. In: Nowrousian MR editor(s). Recombinant HumanErythropoietin (rhEPO) in Clinical Oncology. Wien, Austria: SpringerWienNewYork, 2002:39‐62. [Google Scholar]
Nowrousian 2002b
- Nowrousian MR. Prevalence, pathophysiology, predictive factors, and prognostic significance of anemia in cancer chemotherapy. In: Nowrousian MR editor(s). Recombinant Human Erythropoietin (rhEPO) in Clinical Oncology. Wien, Austria: SpringerWienNewYork, 2002:63‐100. [Google Scholar]
Palmer 2010
- Palmer SC, Navaneethan SD, Craig JC, Johnson DW, Tonelli M, Garg AX, et al. Meta‐analysis: erythropoiesis‐stimulating agents in patients with chronic kidney disease. Annals of Internal Medicine 2010;153(1):23‐33. [PUBMED: 20439566] [DOI] [PubMed] [Google Scholar]
Parmar 1998
- Parmar MKB, Torri V, Stewart L. Extracting summary statistics to perform meta‐analyses of the published literature for survival endpoints. Statistics in Medicine 1998;17:2815‐34. [DOI] [PubMed] [Google Scholar]
Quirt 2003
- Quirt I, Micucci S, Moran LA, Pater J, Browman G. The role of erythropoietin in the management of cancer patients with non‐hematologic malignancies receiving chemotherapy. Cancer Care Ontario Practice Guidelines Initiative March 1, 2003.
Quirt 2005
- Quirt I, Bramwell V, Charette M, Oliver T, and the Systemic Treatment Disease Site Group. The role of erythropoietin in the management of cancer patients with non‐hematologic malignancies receiving chemotherapy. Practice Guideline Report #12‐1. program in evidence‐based care; a cancer care ontario program 2005; Vol. #12‐1. [MEDLINE: ]
Reed 1994
- Reed WR, Hussey DH, DeGowin RL. Implications of the anemia of chronic disorders in patients anticipating radiotherapy. American Journal of the Medical Sciences 1994;308:9‐15. [DOI] [PubMed] [Google Scholar]
Roche ODAC 2004
- ROCHE. NEORECORMON (EPOETIN BETA). Briefing Package for the FDA Oncologic Drugs Advisory Committee Meeting May 4, 2004 Vol. RO 205‐3859.
Ross 2003
- Ross SD, Fahrbach K, Frame D, Scheye R, Connelly JE, Glaspy J. The effect of anemia treatment on selected health‐related quality‐of‐life domains: a systematic review. Clinical Therapeutics 2003;25(6):1786‐805. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ross 2006
- Ross SD, Allen IE, Henry DH, Seaman C, Sercus B, Goodnough LT. Clinical benefits and risks associated with epoetin and darbepoetin in patients with chemotherapy‐induced anemia: a systematic review of the literature. Clinical Therapeutics 2006;28(6):801‐31. [PUBMED: 16860166] [DOI] [PubMed] [Google Scholar]
Ross 2007
- Ross SD, Allen IE, Probst CA, Sercus B, Crean SM, Ranganathan G. Efficacy and safety of erythropoiesis‐stimulating proteins in myelodysplastic syndrome: a systematic review and meta‐analysis. The Oncologist 2007;12(10):1264‐73. [PUBMED: 17962620] [DOI] [PubMed] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman D. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408‐12. [DOI] [PubMed] [Google Scholar]
Seidenfeld 2001a
- Seidenfeld J, Piper M, Flamm C, Hasselblad V, Armitage JO, Bennett CL, et al. Epoetin treatment of anemia associated with cancer therapy: a systematic review and meta‐analysis of controlled clinical trials. Journal of the National Cancer Institute 2001;93(16):1204‐14. [DOI] [PubMed] [Google Scholar]
Seidenfeld 2001b
- Seidenfeld J, Aronson N, Piper MA, Flamm C, Hasselblad V, Ziegler KM. Uses of erythropoietin for anemia in oncology. Evidence report/technology assessment No. 30. Prepared by the Blue Cross and Blue Shield Association Evidence‐based Practice Center, 2001; Vol. Contract No. 290‐97‐0015. AHRQ Publ No. 01‐E009. Rockville (MD):Agency for Healthcare Research and Quality.
Seidenfeld 2006
- Seidenfeld J, Piper M, Bohlius J, Weingart O, Trelle S, Engert A, et al. Comparative effectiveness of epoetin and darbepoetin for managing anemia in patients undergoing cancer treatment. Agency for Healthcare Research and Quality 2006; Vol. Report No.: 3:N/A. [PubMed]
Silver 1999
- Silver DF, Piver MS. Effects of recombinant human erythropoietin on the antitumor effect of cisplatin in SCID mice bearing human ovarian cancer: A possible oxygen effect. Gynecologic Oncology 1999;73:280‐4. [DOI] [PubMed] [Google Scholar]
Spivak 1994a
- Spivak JL. Recombinant human erythropoietin and the anemia of cancer. Blood 1994;84:997‐1004. [PubMed] [Google Scholar]
Spivak 1994b
- Spivak JL. Cancer‐related anemia: its causes and characteristics. Seminars in Oncology 1994;21(2, Suppl 3):3‐8. [PubMed] [Google Scholar]
Stasko 2002
- Stasko J, Drouet L, Soria C, Mazoyer E, Caen J, Kubisz P. Erythropoietin and granulocyte colony‐stimulating factor increase plasminogen activator inhibitor‐1 release in HUVEC culture. Thrombosis Research 2002;105(2):161‐4. [PUBMED: 11958807] [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D. Chapter 10: Addressing reporting biases. Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 (updated March 2011) 2011.
Stohlawetz 2000
- Stohlawetz PJ, Dzirlo L, Hergovich N, Lackner E, Mensik C, Eichler HG, et al. Effects of erythropoietin on platelet reactivity and thrombopoiesis in humans. Blood 2000;95(9):2983‐9. [PUBMED: 10779449] [PubMed] [Google Scholar]
Storring 1998
- Storring PL, Tiplady RJ, Gaines Das RE, Stenning BE, Lamikanra A, Rafferty B. Epoetin alfa and beta differ in their erythropoietin isoform compositions and biological properties. British Journal of Haematology 1998;100:79‐89. [DOI] [PubMed] [Google Scholar]
Tatum 2006
- Tatum JL, Kelloff GJ, Gillies RJ, Arbeit JM, Brown JM, Chao KS, et al. Hypoxia: importance in tumor biology, noninvasive measurement by imaging, and value of its measurement in the management of cancer therapy. International Journal of Radiation Biology 2006;82(10):699‐757. [PUBMED: 17118889] [DOI] [PubMed] [Google Scholar]
Teicher 1981
- Teicher BA, Lazo JS, Sartorelli AC. Classification of antineoplastic agents by their selective toxicities toward oxygenated and hypoxic tumor cells. Cancer Research 1981;41:73‐81. [PubMed] [Google Scholar]
Teicher 1994
- Teicher BA. Hypoxia and drug resistance. Cancer Metastasis Reviews 1994;13:139‐68. [DOI] [PubMed] [Google Scholar]
Thews 2001
- Thews O, Kelleher DK, Vaupel P. Erythropoietin restores the anemia‐induced reduction in cyclophosphamide cytotoxicity in rat tumors. Cancer Research 2001;61:1358‐61. [PubMed] [Google Scholar]
Thomas 1998
- Thomas ML. Impact of anemia and fatigue on quality of life in cancer patients: a brief review. Medical Oncology 1998;15(Supp 1):3‐7. [PubMed] [Google Scholar]
Tonelli 2009
- Tonelli M, Hemmelgarn B, Reiman T, Manns B, Reaume MN, Lloyd A, et al. Benefits and harms of erythropoiesis‐stimulating agents for anemia related to cancer: a meta‐analysis. CMAJ 2009;180(11):E62‐E71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tonelli 2009 HTA
- Tonelli M, Lloyd A, Lee H, Wiebe N, Hemmelgarn B, Reiman T, et al. Erythropoiesis‐stimulating agents for anemia of cancer or of chemotherapy: systematic review and economic evaluation [Technology report number 119]. Ottawa: Canadian. Agency for Drugs and Technologies in Health; Ottawa: Canadian 2009; Vol. 119:N/A.
Van Belle 2003
- Belle SJ, Cocquyt V. Impact of haemoglobin levels on the outcome of cancers treated with chemotherapy. Critical Reviews in Oncology/Hematology 2003;47(1):1‐11. [PUBMED: 12853095] [DOI] [PubMed] [Google Scholar]
Vaupel 1989
- Vaupel P, Kallinowski F, Okunieff P. Blood flow, oxygen and nutrient supply, and metabolic microenvironment of human tumors: a review. Cancer Research 1989;49:6449‐65. [PubMed] [Google Scholar]
Vaupel 2000
- Vaupel P, Hockel M. Blood supply, oxygenation status and metabolic micromilieu of breast cancers: Characterization and therapeutic relevance. International Journal of Oncology 2000;17:869‐79. [DOI] [PubMed] [Google Scholar]
Vaupel 2001
- Vaupel P, Kelleher DK, Hockel M. Oxygen status of malignant tumors: Pathogenesis of hypoxia and significance for tumor therapy. Seminars in Oncology 2001;28(2):29‐35. [DOI] [PubMed] [Google Scholar]
Vaupel 2008
- Vaupel P. Hypoxia and aggressive tumor phenotype: implications for therapy and prognosis. The Oncologist 2008;13 Suppl 3:21‐6. [PUBMED: 18458121] [DOI] [PubMed] [Google Scholar]
Verhagen 1998
- Verhagen AP, DeVet HCW, DeBie RA, Kessels AGH, Boers M, et al. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. Journal of Clinical Epidemiology 1998;51(12):1235‐41. [DOI] [PubMed] [Google Scholar]
Viechtbauer 2010
- Viechtbauer W. Conducting meta‐analyses in R with Metafor package. Journal of Statistical Software 2010;36(3):1‐48. [Google Scholar]
Williamson 1999
- Williamson LM, Lowe S, Love EM, Cohen H, Soldan K, McClelland DB, et al. Serious hazards of transfusion (SHOT) initiative: analysis of the first two annual reports. BMJ 1999;319:16‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2007
- Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al. A systematic review and economic evaluation of epoetin alpha, epoetin beta and darbepoetin alpha in anaemia associated with cancer, especially that attributable to cancer treatment. Health technology assessment (Winchester, England) 2007;11(13):1‐202, iii‐iv. [PUBMED: 17408534] [DOI] [PubMed] [Google Scholar]
Wood 1995
- Wood PA, Hrushesky JM. Cisplatin‐associated anemia: an erythropoietin deficiency syndrome. Journal of Clinical Investigation 1995;95:1650‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yasuda 2003
- Yasuda Y, Fujita Y, Matsuo T, Koinuma S, Hara S, Tazaki A, et al. Erythropoietin regulates tumour growth of human malignancies. Carcinogenesis 2003;24:1021‐9. [DOI] [PubMed] [Google Scholar]
Yellen 1997
- Yellen SB, Cella DF, Webster K, et al. Measuring fatigue and other anemia‐related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. Journal of Pain and Symptom Management 1997;13:63‐74. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Bohlius 2005
- Bohlius J, Langensiepen S, Schwarzer G, Seidenfeld J, Piper M, Bennett C, et al. Recombinant human erythropoietin and overall survival in cancer patients: results of a comprehensive meta‐analysis. Journal of the National Cancer Institute 2005;97(7):489‐98. [DOI] [PubMed] [Google Scholar]
Bohlius 2006a
- Bohlius J, Wilson J, Seidenfeld, J, Piper M, Schwarzer G, Sandercock J, et al. Recombinant human erythropoietins and cancer patients: updated meta‐analysis of 57 studies including 9353 patients. Journal of the National Cancer Institute 2006;98:708‐14. [DOI] [PubMed] [Google Scholar]
Bohlius 2006b
- Bohlius J, Wilson J, Seidenfeld J, Piper M, Schwarzer G, Sandercock J, et al. Erythropoietin or Darbepoetin for patients with cancer. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD003407.pub4] [DOI] [PubMed] [Google Scholar]


