Abstract
Background
Decision-making related to coronary artery bypass grafting (CABG) in elderly patients is hampered by inadequate outcome data. We compared the clinical outcomes of octogenarians with those of septuagenarians who underwent CABG. Our secondary objective was to compare the costs associated with CABG in these groups.
Methods
We conducted a retrospective database review of patients 70 years of age and older who had undergone CABG at a regional cardiac surgical centre in Hamilton, Ont., between July 1, 1997, and Apr. 30, 2000. A total of 1034 patients were divided into 3 age groups: young septuagenarians (aged 70–74 years), old septuagenarians (aged 75–79) and those 80 and older. Costs were determined in a subset of 773 patients with the use of a case-costing system for cardiac surgery developed at our institution.
Results
The 3 groups were similar with respect to sex distribution and preoperative risk factors. Urgency scores at referral differed significantly between the groups, with the young septuagenarians demonstrating the lowest risk (mean score [and standard deviation] 4.48 [1.3] in that group, 4.28 [1.4] in the old septuagenarian group and 4.11 [1.2] in the octogenarian group). The rates of all complications combined were similar between the 3 groups (27.1%, 28.1% and 29.6% in the young and old septuagenarian groups and the octogenarian group respectively). There were no significant differences between the 3 groups in the mean number of grafts per patient (3.0, 3.1 and 3.0 respectively), the rate of postoperative death (3.3%, 5.7% and 4.2%), the mean length of stay (11.7, 13.4 and 12.6 days) or the incidence of postoperative myocardial infarction (4.5%, 3.4% and 4.2%). The total cost of CABG per patient did not differ significantly between the 3 groups.
Interpretation
Given that patients who are accepted for CABG represent a selected population, our findings suggest that, with careful triage, CABG in octogenarians is as safe as, and no more costly than, CABG in septuagenarians.
Cardiac surgery in octogenarians is a relatively new phenomenon in Canada and has arisen because of advancements in medical and holistic strategies for cardiovascular disease prevention and the growth of the elderly population.1,2 In 1999 Statistics Canada reported that about 12% of Canadians were 65 years of age and older, with those 85 years and older representing the fastest growing segment of the senior population.2 With rapid growth of the elderly segment of the Canadian population, the number of octogenarians being referred for cardiac interventions is expected to increase.3,4,5,6,7,8 This trend has both clinical implications for health care professionals directing the care of patients and economic implications for the Canadian health care system. Despite this trend, considerable debate remains with respect to cardiac surgery in patients 80 years and older. Up to the age of 79, there is little hesitation to operate on patients presenting for coronary artery bypass grafting (CABG). However, there appears to be a “psychological barrier” to surgery for both older patients and their clinicians. This may be due in part to the relative dearth of information regarding the outcomes of CABG in octogenarians, making it difficult for patients and clinicians to make a completely informed decision.
The Hamilton Health Sciences Corporation (HHSC) — General Site, a tertiary care teaching hospital in Hamilton, Ont., completes about 1300 cardiac surgeries each year, about 60% of which are isolated CABG procedures. Over the past 5 years, the proportion of older patients undergoing CABG at our institution has increased. Currently, people 70–74 years old form the largest 5-year age cohort of patients and those 70 and older account for 45% of all patients undergoing isolated CABG at our institution.
Observational studies have reported in-hospital death rates of 8% to 24% following CABG in octogenarians.3,4,5,6,7,8,9,10 However, octogenarians referred for elective isolated CABG have death rates that approach those among patients under 80.4,7,8 Rates of complications, on the other hand, are significantly higher among octogenarians than among younger patients.5,6,7,8,9,10 Although CABG in octogenarians is associated with increased morbidity, evidence suggests that the 3-year survival rate is significantly greater among octogenarians who have surgery than among those who are managed medically.1
The cost of CABG in octogenarians has been the focus of 2 US studies. Peterson and associates11 found that costs were significantly higher among octogenarians than among younger patients. Sollano and collaborators1 reported that CABG in octogenarians, although significantly more costly than CABG in younger patients, is highly cost-effective.
We conducted a retrospective cohort study to establish whether CABG can be performed in octogenarians with acceptable risk and costs comparable to those associated with CABG in younger elderly patients. Our primary objective was to compare clinical outcomes in octogenarians and septuagenarians who underwent isolated CABG at the HHSC. Determination of the costs associated with CABG in these age groups was our secondary objective.
Methods
Information on all adult patients undergoing cardiac surgery at the HHSC is routinely entered into a database as part of an ongoing collaboration between the HHSC and McMaster University in order to track patient outcomes following CABG. We retrospectively searched the database for patients aged 70 years and older who underwent isolated CABG at the HHSC — General Site between July 1, 1997, and Apr. 30, 2000. A total of 1034 patients met these criteria; their mean age was 74.3 (standard deviation [SD] 3.3) years. Patients were separated into 3 age cohorts: young septuagenarians (aged 70–74 years, n = 579 [56.0%]), old septuagenarians (aged 75–79, n = 384 [37.1%]) and octogenarians (aged 80 years and over, n = 71 [6.9%]). The Research Ethics Board of the HHSC and McMaster University approved the study design.
The following data were included for analysis: age, sex, preoperative status (Cardiac Care Network of Ontario [CCNO] urgency rating score,12 cardiac and medical history, location of coronary disease, disease severity, left ventricular ejection fraction, ischemic risk, expected procedural morbidity [rated as high or low with respect to existing comorbidities before surgery], previous CABG or sternotomy, myocardial infarction within 4 weeks preceding surgery and risk acuity [elective, semi-urgent, urgent or emergent] at surgery), cardiac risk factors (e.g., history of smoking, angina, congestive heart failure, myocardial infarction, cerebrovascular accident, diabetes mellitus, obesity and hyperlipidemia), perioperative data (e.g., number of grafts, use of left and right internal mammary arteries and saphenous vein grafts, cardiac and all-cause morbidity, intraoperative death, duration of intubation, and length of hospital stay before and after surgery [assessed per ward, intensive care unit (ICU), cardiac care unit (CCU) and step-down unit]). Preoperative risk factors, defined according to the CCNO provincial guidelines12 and standard care at our institution, were collected by the regional coordinator of the CCNO throughout the study period.
Detailed cost data were collected routinely after July 1998 and were therefore available for only a subset of 773 patients (422 young septuagenarians, 294 old septuagenarians and 57 octogenarians). Costs were determined using a modular case-costing system for cardiac surgery developed at our institution, where health care consumption per patient is meticulously recorded and calculated. Total costs represent the pre- and postoperative unit cost per location (ward, ICU, CCU and step-down unit) per day for each patient, the cost of the surgery, professional fees (surgeon, anesthetist and medical assistants) and the cost of all blood work, radiology tests, nuclear medicine investigations and medications. Overhead costs were calculated and allocated. Capital costs were not calculated. Our costing system correlates well with that for CABG in Ontario developed by the Ontario Case Cost Project.13 All reported costs are in 1998 Canadian dollars and are specifically related to those costs incurred at the HHSC.
Statistical analyses were performed by univariate analysis of variance with a post-hoc Scheffé test for specific differences between groups for continuous variables and by the χ2 test (Fisher's exact test if n < 5) for categorical variables. Categorical data are represented as frequency distributions and simple percentages. Values of continuous variables are expressed as means and SDs. All variables that were statistically significant preoperatively (p ≤ 0.05) were controlled for in an analysis of postoperative outcomes.
Results
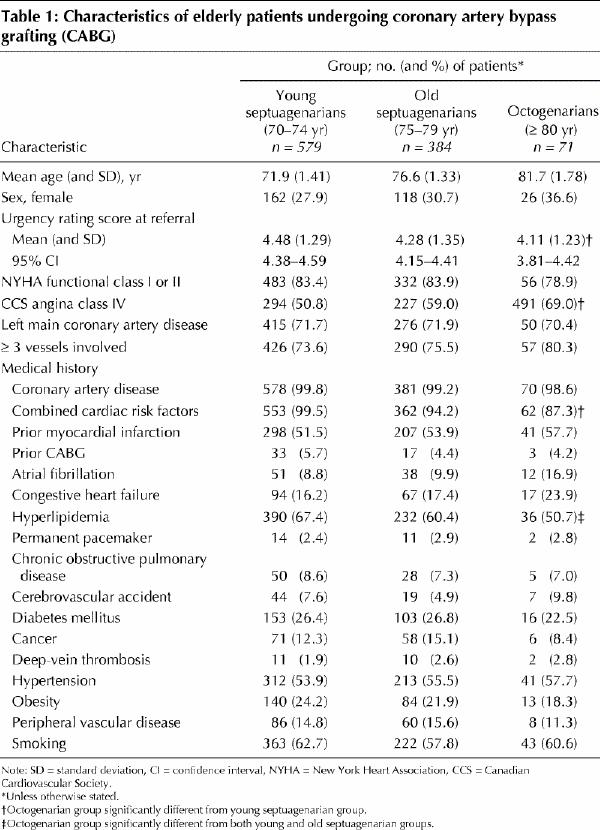
The 3 groups were similar with respect to sex distribution and most preoperative risk factors (Table 1). The mean urgency rating scores at referral differed significantly between the groups: the young septuagenarians were at significantly lower risk than the old septuagenarians (p = 0.02) and the octogenarians (p = 0.02); there were no significant differences between the old septuagenarians and the octogenarians (p = 0.32). Only 1 patient (a young septuagenarian) had Alzheimer's disease (0.2%). The 3 groups differed significantly with regard to combined cardiac risk factors (p = 0.02) and history of hyperlipidemia (p = 0.006). Differences in preoperative atrial fibrillation approached significance (p = 0.09). More of the octogenarians than of the young septuagenarians had severe angina (69.0% v. 50.8%, p = 0.02). The urgency rating score, angina class, combined cardiac risk factors and history of hyperlipidemia were used as covariates in all subsequent analyses of covariance.
Table 1
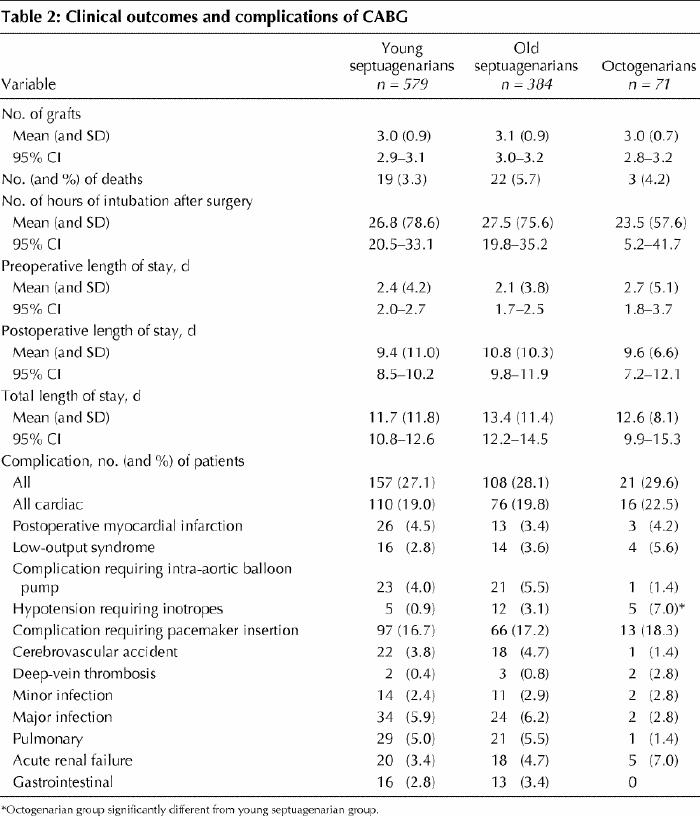
Clinical outcomes and complications are detailed in Table 2. There were no significant differences between the 3 groups in terms of the number of grafts, the number of intraoperative deaths, the duration of intubation following surgery, and the length of stay before and after CABG. The frequency of postoperative complications did not differ significantly between the groups except that more of the octogenarians than of either the young or old septuagenarians received inotropes to support blood pressure intraoperatively (p = 0.002), but the numbers of patients were small. Although not significant, the octogenarian group had the lowest incidence of stroke (p = 0.06) and the highest incidence of deep-vein thrombosis (p = 0.06). Age was significantly correlated with the total and postoperative length of stay after adjustment for the significant preoperative covariates (r = 0.068 and 0.077 respectively, p = 0.05).
Table 2
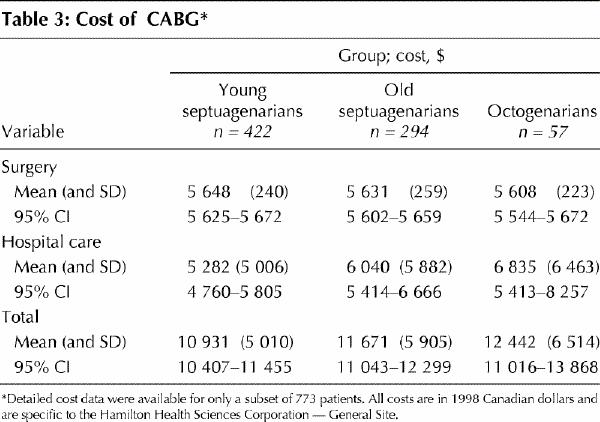
The costs per group are reported in Table 3. There were no significant differences between the 3 groups with respect to the total cost of CABG, with or without professional fees included. A trend was observed toward higher hospital costs in the octogenarian group than in the 2 septuagenarian groups, but the difference failed to reach statistical significance (p = 0.08). The cost of CABG (without professional fees) was significantly correlated with the total (r = 0.131) and postoperative (r = 0.131) length of stay, the number of grafts (r = 0.078) and age (r = 0.113) after adjustment for the significant preoperative covariates.
Table 3
Interpretation
The octogenarians in our study had death and complication rates and lengths of hospital stay similar to those of the septuagenarians. The incidence of neurological complications following CABG is reported to be 2% to 14% among elderly patients.4,5,11,14 All 3 groups in our study had low to moderate rates of cerebrovascular accident postoperatively (range 1.4% to 4.7%). These results compare well with the overall rate of stroke and transient ischemic attack at our institution (2.8%, 1999 data) and are well within the range of values for postoperative cerebrovascular accident reported among octogenarians in the literature.1,3,4,5,6,9
In a Canadian study reported by Fruitman and colleagues,5 octogenarians had a median postoperative length of stay of 10 days (range 8–13), which was significantly longer than that for patients under 80. In our study, the mean length of stay in the oldest group was 9.6 days; however, this did not differ significantly from the mean lengths of stay in the younger groups (9.4 and 10.8 in the young and old septuagenarian groups respectively). This similarity may be explained by the relative comparability of the groups (all elderly); the difference might have been greater had we included all CABG patients.
The rate of early death (in hospital and within 30 days after cardiac surgery) among octogenarians has been reported to range from 8% to 24%.1,3,4,5,6,7,8,9 However, when patients who had isolated CABG are examined separately, the rate is similar to that among patients under 80.7,8 Our findings support this observation: the rate of early death among the octogenarians in our study was much lower than that previously reported, and it approached the rate for all patients undergoing isolated CABG in our institution in 1999 (octogenarian group 4.2%, all patients 3.2%). In addition, the death rate among the octogenarians did not differ significantly from the rate among the younger and older septuagenarians (3.3% and 5.7% respectively). Data from the United States indicate a higher death rate among octogenarians (8.1%) than we have reported;4 however, it is difficult to interpret this difference because of systemic issues concerning patient selection, referral and waiting times for CABG that may differ between the United States and Canada.
Although our data are limited to a single institution, they represent the cost per case of isolated CABG. Two other Canadian studies of the cost of CABG included only 815 and 12016 patients over 70 years of age. Naglie and collaborators16 reported costs of CABG per patient over 70 of $16 400 to $35 800. The mean total cost of CABG per patient in our study was $12 937. Differences in sample size, costing methods, advances in both medical and surgical therapies as well as a trend toward shorter lengths of hospital stay are factors that may account for the cost differences reported in the Canadian literature. Two US studies of the cost of isolated CABG in octogenarians have been reported.1,11 These studies, although interesting, have limited applicability to the present investigation because of the costing methodology used and the differences in our health care systems.
There are several limitations to our study. We included patients from a single institution, which may reduce generalizability of the results. Our institution is a university- affiliated hospital that performs about 1300 cardiac procedures each year. It is well established that surgical outcomes improve with patient volume and affiliation with an educational institution.17,18,19 The retrospective and observational design of our study and the relatively small sample of octogenarians are other limitations. However, studies involving octogenarians will continue to be hampered by sample size issues because there are as yet small numbers of such patients undergoing CABG. A strength of our study is the thorough and complete nature of data collected in our database.
In summary, CABG in octogenarians appears to be as safe as, and no more costly than, CABG in septuagenarians. Considerable controversy remains as to whether the health care resources expended on CABG in elderly patients represents the most cost-effective method for preserving quality of life and independent living. In the absence of randomized trials, our data support prospective exploration into outcomes of surgery not easily determined, such as health-related quality of life after cardiac surgical interventions in this age group. In our experience, the risk of death and complications may not be the determining factors in a patient's decision to undergo surgery. Long-term follow-up of elderly patients undergoing CABG is necessary to determine survivability, health services utilization and economic implications in order to depict the impact of this intervention on the health care system.
Footnotes
This article has been peer reviewed.
Acknowledgments: We thank the members of the Cardiac Surgical Group at the time of the study (Drs. Labib Abouzahr, Irene Cybulsky, John Gunstensen, André Lamy, Alfons Parisi, Lloyd Semelhago, Bernard Shragge and Kevin Teoh), Hamilton Health Sciences Corporation — General Division, for allowing us access to their patients' information and for their critical review of this manuscript. We also thank Ms. Donna Wright, Regional Coordinator of the Cardiac Care Network of Ontario — General Division, for her diligent data collection and attention to detail and Dr. J. Hedges for assistance in developing the database.
Dr. Arthur is supported by a Career Scientist Award from the Ontario Ministry of Health.
Competing interests: None declared.
Correspondence to: Dr. André Lamy, CADENCE Research Group, Hamilton Health Sciences Corporation — General Site, 237 Barton St. E, Hamilton ON L8L 2X2; fax 905 577-1452; lamyand@hhsc.ca
References
- 1.Sollano JA, Rose EA, Williams DL, Thornton B, Quint E, Apfelbaum M, et al. Cost-effectiveness of coronary artery bypass surgery in octogenarians. Ann Surg 1998;228(3):297-306. [DOI] [PMC free article] [PubMed]
- 2.Statistical snapshots of Canada's seniors. No. 1: a growing population. Ottawa: Statistics Canada, for the Division of Aging and Seniors, Health Canada; 2000. Available: www.hc-sc.gc.ca/seniors-aines/pubs/factoids/en/no1.htm (accessed 2001 July 31).
- 3.Hirose H, Amano A, Yoshida S, Takahashi A, Nagano N, Kohmoto T. Coronary artery bypass grafting in the elderly. Chest 2000;117(5):1262-70. [DOI] [PubMed]
- 4.Alexander KP, Anstrom KJ, Muhlbaier LH, Grosswald RD, Smith PK, Jones RH, et al. Outcomes of cardiac surgery in patients age ≥ 80 years: results from the National Cardiovascular Network. J Am Coll Cardiol 2000;35:731-8. [DOI] [PubMed]
- 5.Fruitman DS, MacDougall CE, Ross DB. Cardiac surgery in octogenarians: Can elderly patients benefit? Quality of life after cardiac surgery. Ann Thorac Surg 1999;68:2129-35. [DOI] [PubMed]
- 6.Diewick M, Tandler R, Möllhoff T, Kerber S, Rökter J, Roeder N, et al. Heart surgery in patients aged eighty years and above: determinants of morbidity and mortality. Thorac Cardiovasc Surg 1997;45:119-26. [DOI] [PubMed]
- 7.Kirsch M, Guesnier L, Le Besnerais P, Hillion M, Debauchez M, Seguin J, et al. Cardiac operations in octogenarians: perioperative risk factors for death and impaired autonomy. Ann Thorac Surg 1998;66:60-7. [DOI] [PubMed]
- 8.Diegeler A, Autschbach R, Falk V, Walther T, Gummert J, Mohr RW, et al. Open heart surgery in the octogenarians — a study of long-term survival and quality of life. Thorac Cardiovasc Surg 1995;43:265-70. [DOI] [PubMed]
- 9.Naunheim KS, Kern MJ, McBride LR, Pennington DG, Barner HB, Kanter KR, et al. Coronary artery bypass surgery in patients aged 80 years or older. Am J Cardiol 1987;59:804-7. [DOI] [PubMed]
- 10.Craver JM, Puskas JD, Weintraub WW, Shen Y, Guyton RA, Gott JP, et al. 601 octogenarians undergoing cardiac surgery: outcome and comparison with younger age groups. Ann Thorac Surg 1999;67:1104-10. [DOI] [PubMed]
- 11.Peterson ED, Cowper PA, Jollis JG, Bebchuk JD, DeLong ER, Muhlbaier LH, et al. Outcomes of coronary artery bypass graft surgery in 24,461 patients aged 80 years or older. Circulation 1995;92(Suppl 9):II85-91. [DOI] [PubMed]
- 12.Naylor CD, Morgan CD, Levinton CM, Wheeler S, Hunter L, Klymciw K, et al. Waiting for coronary revascularization in Toronto: 2 years' experience with a regional referral office. CMAJ 1993;149(7):955-62. [PMC free article] [PubMed]
- 13.Ontario Case Cost Project. Ontario guide to case costing [version 1.1]. Toronto: Ontario Case Cost Project; 1995.
- 14.Fernandez J, Chen C, Anolik G, Brdlik OB, Laub GW, Anderson WA, et al. Perioperative risk factors affecting hospital stay and hospital costs in open heart surgery for patients >> or = 65 years old. Eur J CardiothoracSurg 1997; 11(6):1133-40. [DOI] [PubMed]
- 15.Krueger H, Goncalves JL, Caruth FM, Hayden RI. Coronary artery bypass grafting: How much does it cost? CMAJ 1992;146(2):163-8. [PMC free article] [PubMed]
- 16.Naglie G, Tansey C, Krahn MD, O'Rourke K, Detsky AS, Bolley H. Direct costs of coronary artery bypass grafting in patients aged 65 years or more and those under age 65. CMAJ 1999;160(6):805-11. Abstract available: www .cma .ca /cmaj/vol-160/issue-6/0805.htm [PMC free article] [PubMed]
- 17.Glower DD, Christopher TD, Milano CA, White WD, Smith LR, Jones RH, et al. Performance status and outcome after coronary artery bypass grafting in persons aged 80 to 93 years. Am J Cardiol 1992;70:567-71. [DOI] [PubMed]
- 18.Pliam MB, Zapolanski A, Ryan CJ, Shaw RE, Mengarelli LM. Recent improvements in results of coronary bypass surgery in octogenarians. J Invasive Cardiol 1999;11(5):281-9. [PubMed]
- 19.De Mol BA, Kallewaard M, Lewin F, van Gaalen GL, van den Brink RB. Single-institution effectiveness assessment of open-heart surgery in octogenarians. Eur J Cardiothorac Surg 1997; 12(2):285-90. [DOI] [PubMed]


