Universities have long been involved in the creation and evaluation of pharmaceutical products. In its best form, academic participation in drug-related science both spurs innovation and, through the disinterest and skepticism that are hallmarks of the academic mission, provides a check on the premature enthusiasms of industry. In this commentary we examine the logic and behaviour of the pharmaceutical industry in pursuit of its interests and propose rules to govern university–industry partnerships that reflect the public interest.
The duty of universities is to seek truth. The duty of pharmaceutical companies is to make money for their shareholders. Drug companies that fail to do so go out of business. Universities that subordinate the disinterested search for truth to other ends lose credibility and their claim to a privileged status in society. If either abandons its fundamental mission, it ultimately fails. At times, institutional imperatives are bound to conflict.1,2
Research can either serve or subvert the public interest. Its findings may advance knowledge and support useful innovation, or be filtered and twisted to support prejudices or gain commercial advantage. The capacities and integrity of researchers, and their universities, can be enhanced or corrupted in the process. Some partnerships are united by an open-minded quest for discovery; others are unholy alliances whereby researchers and universities become handmaidens of industry. Whatever ethical bed we make, we lie in.
There is abundant evidence that many such partnerships place industry imperatives above both the public interest and the fundamental ethos of the university. The evidence includes major variation in disclosure requirements,3 insufficient protection of the right to publish in a timely fashion4 and researchers having financial interests in companies potentially affected by the outcomes of their research.5 The creation of the Canadian Institutes of Health Research (CIHR) and its renewed commitment to excellence and expanded capacity for innovation and discovery have created unprecedented health research opportunities in Canada. With what ethical compass will Canada chart its health research course?
The outcome will depend on 3 key players: the federal government and its agencies, the universities, and industry. The recent history of government policy is a 3-part drama. In the late 1980s the federal government concluded that increased drug research and development by the private sector in Canada would contribute to the economy. Second, multinational drug companies indicated that their expansion of research and development activities in their Canadian branches would be contingent on favourable patent protection legislation. Third, in return for extending patent protection, the government exacted a commitment from industry to invest 10% of sales in Canadian-based research.
The Medical Research Council of Canada6 (MRC, the forerunner of the CIHR) and many faculty members and universities supported these measures. The MRC budget declined for 3 consecutive years beginning in 1995/96 and was essentially frozen during most of the decade.6 Elsewhere, spending on health research rose significantly, most notably in the United States, where federal funding alone doubled in real terms during the 1990s.7 Science became more complex, expensive and competitive. To offset the severe restraints imposed on public funding of universities as part of the war on government deficits in Canada during the 1990s, researchers and universities had to look elsewhere for funding. Enter industry.
In 2000, “business enterprise,” which was almost exclusively the pharmaceutical industry (although Statistics Canada does not break down the figures), accounted for about 43% of gross domestic expenditures on research and development in the health field (the amount includes $350 million from foreign sources spent on business enterprises in Canada, which we assume to be industry dollars).8 Universities and teaching hospitals received $161 million from industry, which was more than the amount from provincial governments combined and over half the amount received from federal sources (largely the MRC–CIHR). Aside from being a major player on campus, industry exerts considerable influence on public policy by virtue of the $900 million it spends in-house on research and development.
What does industry expect for its $161 million invested in universities and teaching hospitals? Drug companies have a fiduciary duty to exploit the intellectual talent and ethical credibility of universities to advance their interests. The proximate goal is the publication of positive results of trials of new drugs, or evaluations that show that certain drugs are better than their competitors' products. The ultimate goal is sales. Negative findings often, and predictably, create an unhappy industry partner. Common sense suggests that universities must be vigilant about protecting their own, fundamentally different culture and orientation.
To date, they have not been. The new money and activity exploded onto the scene with inadequate oversight and no standardization of rules or mechanisms to resolve disputes. The results: some highly publicized aggressions,9 tarnished institutional reputations, one-sided marriages of convenience, and who knows how much unhelpful drug therapy and increased cost.
Unsettling incidents of this nature have occurred throughout the world.10 These are not impersonal and civil corporate disagreements; they often involve intimidating tactics by industry that profoundly affect researchers' lives and careers. Canadian cases, the details of which we do not recount for reasons of space, include the Bristol–Myers Squibb lawsuit against the Canadian Coordinating Office on Health Technology Assessment (CCOHTA) to suppress its statin report,11 and the AstraZeneca legal threat against McMaster University researcher Anne Holbrook for her review of medications for stomach disorders (personal communication 2001). Regardless of the outcome of these cases, industry harassment consumes time and energy (and in the CCOHTA case, 13% of its budget, for legal fees) and creates unease; these are of course the intended effects.
In other cases, the financial clout of industry may influence academic behaviour more subtly, or at least appear to do so. Witness the withdrawal of an offer of employment to Dr. David Healy by the Centre for Addictions and Mental Health (CAMH) in Toronto shortly after he made a speech critical of Prozac, whose manufacturer, Eli Lilly, donated $1.55 million to the CAMH in 2000.12,13,14 There is no evidence of direct involvement by Eli Lilly in this decision, but the company did withdraw corporate funding of The Hastings Centre after its journal published a series of articles critical of antidepressant prescribing practices.15
Such cases demonstrate yet again that, when public and private interests conflict, at least some companies will fiercely protect their shareholders' interests. If the drugs they hoped would be breakthroughs turn out to be “me-toos,” they must market them at the highest possible price in order to recoup the development costs, which can exceed US$100 million. If one company's drug is the therapeutic equivalent of other companies' drugs, it is obliged to try to persuade doctors, pharmacists and the public that its drug is actually better. In this, they are identical to car manufacturers and brewers of beer.
These inevitabilities demand prudent engagement. The warrant for prudence is not that something will go wrong; it is simply that something may go wrong, and has gone wrong in several cases. The intimidation and lawsuits are only the tip of the iceberg. Far more prevalent and insidious is the correlation between industry funding and research that shows a positive therapeutic effect.16 In a landmark article researchers found that industry-sponsored studies of calcium-channel antagonists are more likely to be supportive of that therapy than independently funded research.17 Similar findings emerged from a review of economic analyses of new oncology drugs.18 The positive skew is not dependent on such high-risk and brazen strategies as falsification of data; it is achievable by framing the questions and the design of studies to increase the probability of a positive result.
Industry funding creates an incentive to promote the positive and suppress the negative. When drug companies control publication of results or simply delay unwelcome findings, truth is partially disclosed and therefore compromised. And if researchers' laboratories and career prospects depend on renewed industry funding, their interests may begin to align with those of their paymasters. Unhappily, disinterested scholarly editorial practices often exacerbate rather than counteract this bias,19,20,21 reaffirming Francis Bacon's observation that “the human intellect ... is more moved and excited by affirmatives than negatives.”19
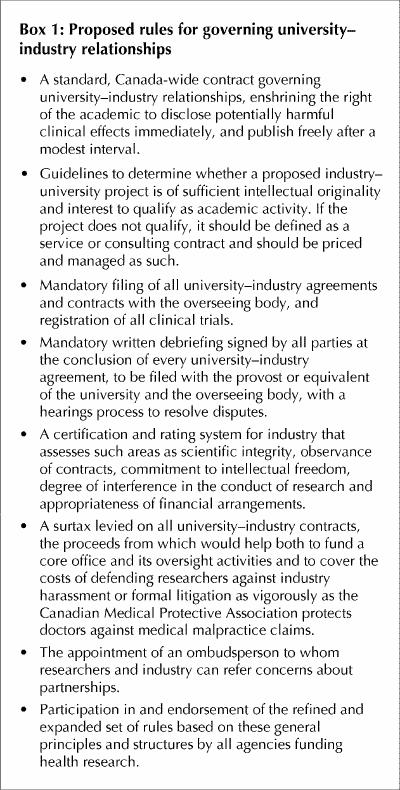
What is to be done? We propose the rules in Box 1 as a starting point for governing partnerships. The rules need an institutional home. One option would vest responsibility with the Association of Universities and Colleges of Canada. Health research is but a subset of all research, and the university, not its parts or affiliates, should be the institution of record. Any tendency for the health sciences to develop ethical standards in isolation must be resisted. “Academic separatism” flies in the face of the multidisciplinary and interdisciplinary collaboration that is heavily promoted as essential to the advancement of knowledge. Even more centrally, the university must not duck its responsibility to govern activities in its well-funded peripheries, including teaching hospitals.
Box 1.
Is a coordinated, national approach necessary? On the basis of the evidence to date, universities and researchers cannot be expected to protect their (and by extension the public's) interests with uniform sophistication and vigour.22 Some US commentators have proposed precisely our form of remedy.23 In May of this year the US National Bioethics Advisory Commission called for federal legislation to create the National Office for Human Research Oversight to oversee all research involving human subjects, including the definition, disclosure and management of conflict of interest.24
Not infrequently, universities encounter challenges, veiled in the language of increased accountability, to their freedom of inquiry and expression. The claim that proposed constraints would be fatal to the academic mission becomes hypocrisy if universities allow industry to define the nature of inquiry, dictate methods and shackle expression. An industry–university contract is a transaction, and our proposed rules are designed principally to protect the university's most precious commodity: intellectual integrity.
We are not asking academic researchers to forswear all interactions with industry. We are merely proposing rules for exercising due diligence to protect the essence of academic inquiry. A positive effect of the proposed rules would be voluntarily improved industry behaviour, with enlightened companies adopting honourable codes of conduct that in time may mitigate the wariness and cynicism that recent aggressions have doubtless engendered.
Some bargains are Faustian, and some horses are Trojan. Dance carefully with the porcupine, and know in advance the price of intimacy.
Footnotes
Acknowledgement: Dr. Ghali is supported by a Population Health Investigator Award from the Alberta Heritage Foundation for Medical Research and by a Government of Canada Research Chair in Health Services Research.
Competing interests: None declared.
Correspondence to: Mr. Steven Lewis, Access Consulting Ltd., 211–4th Ave. S, Saskatoon SK S7K 1N1; fax 306 343-1071; sj.lewis@home.com
References
- 1.Press E, Washburn J. The kept university. Atlantic Monthly 2000;285. Available: www.theatlantic.com/issues/2000/03/press.htm (accessed 2001 Aug 20).
- 2.Weatherall D. Academia and industry: increasingly uneasy bedfellows. Lancet 2000;355:1574. [DOI] [PubMed]
- 3.Van McCrary S, Anderson CB, Jakovljevic J, Khan T, McCullough LB, Wray NP, et al. A national survey of policies on disclosure of conflicts of interest in biomedical research. N Engl J Med 2000;343:1621-6. [DOI] [PubMed]
- 4.Cho MK, Shohara R, Schissel A, Rennie D. Policies on faculty conflicts of interest at US universities. JAMA 2000;284:2237-8. [DOI] [PubMed]
- 5.Lo B, Wolf LE, Berkeley A. Conflict-of-interest policies for investigators in clinical trials. N Engl J Med 2000;343:1616-20. [DOI] [PubMed]
- 6.Medical Research Council of Canada. Report of the president 1999–2000. Ottawa: Canadian Institutes of Health Research; 2000. Cat no MR1-2000. Available (in pdf format): www.cihr.ca/news/publications/publications/report9900_e.pdf (accessed 2001 Aug 20).
- 7.Meeks RL. Federal R&D funding by budget function: fiscal years 1999–2001, special report. Arlington (VA): National Science Foundation, Division of Science Resources Studies; 2001. Report no NSF 01-316.
- 8.Estimates of total expenditures on research and development in the health field in Canada, 1988 to 2000. Ottawa: Statistics Canada; 2001. Cat no. 88F0006XIE01006.
- 9.Hailey D. Scientific harassment by pharmaceutical companies: time to stop. CMAJ 2000;162(2):212-3. Available: www.cma.ca/cmaj/vol-162/issue-2/0212.htm [PMC free article] [PubMed]
- 10.Morgan S, Barer ML, Evans RG. Health economists meet the fourth tempter: drug dependency and scientific discourse. Health Econ 2000;9:659-67. [DOI] [PubMed]
- 11.Skolnick AA. Drug firm suit fails to halt publication of Canadian health technology report. JAMA 1998;280:683-4. [PubMed]
- 12.Boseley S. Bitter pill. Guardian Weekly 2001;164(22):23.
- 13.Hospital denies that withdrawal of MD's job offer was related to drug-company funding. CMAJ 2001;164(13):1879. Available: www.cma.ca/cmaj/vol-164/issue-13/1879a.asp
- 14.Lead donor Eli Lilly Canada launches education centre. In: Foundation progress report winter 2000. Toronto: Centre for Addiction and Mental Health; 2000. Available: www.camh.net/foundation/newsletters/foundation_news_winter2000.html (accessed 2001 Aug 20).
- 15.Kaebnick G. What about the report? Hastings Cent Rep 2001;31(2):16-7.11478088
- 16.Davidson RA. Source of funding and outcome of clinical trials. J Gen Intern Med 1986;1:155-8. [DOI] [PubMed]
- 17.Stelfox HT, Chua G, O'Rourke K, Detsky AS. Conflict of interest in the debate over calcium-channel antagonists. N Engl J Med 1998;332:101-6. [DOI] [PubMed]
- 18.Friedberg M, Saffran B, Stinson TJ, Nelson W, Bennett CL. Evaluation of conflict of interest in economic analyses of new drugs used in oncology. JAMA 1999;282:1453-7. [DOI] [PubMed]
- 19.Dickersin K. The existence of publication bias and risk factors for its occurrence. JAMA 1990;263:1385-9. [PubMed]
- 20.Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet 1991;337:867-72. [DOI] [PubMed]
- 21.Naylor CD. Meta-analysis and the meta-epidemiology of clinical research. BMJ 1997;315:617-9. [DOI] [PMC free article] [PubMed]
- 22.Boyd EA, Bero LA. Assessing faculty financial relationships with industry: a case study. JAMA 2000;284:2209-14. [DOI] [PubMed]
- 23.Hall ZA, Scott C. University–industry partnership. Science 2001;591:553. [DOI] [PubMed]
- 24.National Bioethics Advisory Commission. Ethical and policy issues in research involving human participants. Rockville (MD): The Commission; 2001 May 18. Recommendations available: http://bioethics.gov/press/finalrecomm5-18.html (accessed 2001 Aug 20).


