Abstract
BACKGROUND
Although mass vaccination against COVID-19 may prove to be the most efficacious end to this deadly pandemic, there remain concern and indecision among the public toward vaccination. Because pregnant and reproductive-aged women account for a large proportion of the population with particular concerns regarding vaccination against COVID-19, this survey aimed at investigating their current attitudes and beliefs within our own institution.
OBJECTIVE
This study aimed to understand vaccine acceptability among pregnant, nonpregnant, and breastfeeding respondents and elucidate factors associated with COVID-19 vaccine acceptance.
STUDY DESIGN
We administered an anonymous online survey to all women (including patients, providers, and staff) at our institution assessing rates of acceptance of COVID-19 vaccination. Respondents were contacted in 1 of 3 ways: by email, advertisement flyers, and distribution of quick response codes at virtual town halls regarding the COVID-19 vaccine. Based on their responses, respondents were divided into 3 mutually exclusive groups: (1) nonpregnant respondents, (2) pregnant respondents, and (3) breastfeeding respondents. The primary outcome was acceptance of vaccination. Prevalence ratios were calculated to ascertain the independent effects of multiple patient-level factors on vaccine acceptability.
RESULTS
The survey was administered from January 7, 2021, to January 29, 2021, with 1012 respondents of whom 466 (46.9%) identified as non-Hispanic White, 108 (10.9%) as non-Hispanic Black, 286 (28.8%) as Hispanic, and 82 (8.2%) as non-Hispanic Asian. The median age was 36 years (interquartile range, 25–47 years). Of all the respondents, 656 respondents (64.8%) were nonpregnant, 216 (21.3%) were pregnant, and 122 (12.1%) were breastfeeding. There was no difference in chronic comorbidities when evaluated as a composite variable (Table 1). A total of 390 respondents (39.2%) reported working in healthcare. Nonpregnant respondents were most likely to accept vaccination (457 respondents, 76.2%; P<.001) with breastfeeding respondents the second most likely (55.2%). Pregnant respondents had the lowest rate of vaccine acceptance (44.3%; P<.001). Prevalence ratios revealed all non-White races except for non-Hispanic Asian respondents, and Spanish-speaking respondents were less likely to accept vaccination (Table 3). Working in healthcare was not found to be associated with vaccine acceptance among our cohort.
CONCLUSION
In this survey study of only women at a single institution, pregnant respondents of non-White or non-Asian races were more likely to decline vaccination than nonpregnant and breastfeeding respondents. Working in healthcare was not associated with vaccine acceptance.
Key words: breastfeeding, COVID-19, risk reduction, vaccine
AJOG MFM at a Glance.
Why was this study conducted?
Although mass vaccination against COVID-19 may prove to be the most efficacious end to this deadly pandemic, there remain concern and indecision among pregnant and reproductive-aged women. This survey study aimed at investigating their current attitudes and beliefs.
Key findings
Pregnant respondents were more likely to decline vaccination than nonpregnant and breastfeeding respondents owing to a lack of sufficient research and fear of harming their fetus. Working in healthcare was not associated with vaccine acceptance.
What does this add to what is known?
Both pregnant and breastfeeding women were less likely to accept vaccination compared with nonpregnant women with no increased likelihood of acceptance among healthcare workers.
Introduction
Early in 2020, New York City became the epicenter of the COVID-19 pandemic in the United States. The morbidity and mortality from COVID-19 infection have reached historically tragic heights with significant racial and ethnic disparities in disease prevalence.1 Compared with nonpregnant women, pregnant women are at a higher risk of severe illness and complications from COVID-19. A report from the Centers for Disease Control and Prevention found that pregnant women were 3 times more likely to be admitted to the intensive care unit or require intubation and 1.5 times more likely to die from COVID-19 than nonpregnant women.2 Based on phase III randomized trials, vaccination against COVID-19 has been shown to be the most effective way thus far to prevent severe disease.3 Given this increased risk, it would follow that our patient population would welcome the introduction of a COVID-19 vaccine. Broad distribution and acceptance are required to achieve herd immunity and expedite the end of the pandemic. To this end, eligible patients declining vaccination could substantially delay or potentially preclude herd immunity leading to more morbidity and mortality from the disease. While we await further trails on the effects of the COVID-19 vaccine in pregnancy, understanding patient perception and barriers to vaccine acceptance is imperative in helping to end the pandemic.
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM), following the Emergency Use Authorization of both the Pfizer and Moderna vaccines by the Food and Drug Administration, allowed for autonomy of pregnant people in receipt of the vaccine after a shared decision-making discussion with their obstetrical providers.4 Since the recent publication of data on COVID-19 vaccination and its subsequent implementation, there have been no data on vaccine acceptance for pregnant women and those of reproductive age. In this study, we aimed to understand vaccine acceptability among pregnant women either receiving care or working within our department at the Columbia University Irving Medical Center at New York Presbyterian Hospital compared with nonpregnant women. In addition, we aimed to evaluate racial or ethnic disparities in vaccine acceptance in pregnant and nonpregnant individuals receiving care in our institution. Finally, we desired to elucidate factors associated with COVID-19 vaccine acceptance.
Methods
We administered an online survey from January 7, 2021, to January 29, 2021, to evaluate individual rates of acceptance of COVID-19 vaccination. The survey was targeted to all women (including patients, providers, and staff) at our institution. This study was approved by the Institutional Review Board (IRB) of Columbia University Irving Medical Center (protocol# AAAT5404). A web-based survey was created in REDCap, a secure web-based application designed to support data capture for research studies, and a URL link was created for respondents to complete the survey. Given the low likelihood of harm, informed consent was waived by our IRB. However, there was a written description at the beginning of the survey emphasizing its purpose and our support of the patient's decision toward vaccination. In addition, the names of the investigators were listed with contact information, and they were informed that the survey was optional and not mandatory.
Study population and data collection
Respondents were conveniently recruited through 3 primary sources with no restrictions to participation except that respondents were to be of the female sex. First, treating physicians of both privately and publicly insured patients within our institution were contacted for permission to approach their patients with our survey and encouraged to engage with patients about our survey. After permission was granted, all patient emails were obtained from the electronic medical record and respondents were sent email invitations (example provided in supplemental material) explaining the purpose of the survey with the link included. The second source came from advertisement flyers that were posted in the waiting rooms of participating physician offices and in the hospital informing women of the survey with a quick response (QR) code which linked to the survey online. The third source came from a “Virtual COVID-19 Vaccine Town Hall” targeted to women of reproductive age working in the Columbia University Irving Medical Center system. The QR code was posted at the beginning of the event with instructions to complete it before its start. The QR code was then removed once the event started. Given that the survey is anonymous and not unique, the URL could be shared among receivers.
Survey
A 23-question survey was created and piloted with a convenience sample in English and Spanish. At the start of the survey, respondents were informed that our department supports the personal decision of women regarding acceptance or declination of vaccination against COVID-19 and that the purpose of the survey was to better understand their thoughts and concerns regarding vaccination. Respondents were asked their age, pregnancy status, breastfeeding status, race, ethnicity, chronic medical conditions, employment, and their healthcare provider. Chronic comorbidities included asthma, chronic obstructive pulmonary disease, sickle cell disease, heart condition, diabetes mellitus, diabetes mellitus of pregnancy, chronic hypertension, immunocompromised state (HIV, cancer, etc), and tobacco use. On our ninth multiple choice question, respondents were asked if they planned on taking the vaccine once it was available to them. Respondents who responded “yes” or “I have already been vaccinated” were classified under vaccine acceptance. The remainder of their survey inquired about factors associated with vaccine acceptance. Those who responded “no” were classified under vaccine declination, and the remainder of their survey focused on factors associated with declination. Those who responded “unsure” were classified as undecided and answered all questions associated with vaccine acceptance and declination. All respondents were then queried on factors that would influence their decision to accept and decline the COVID-19 vaccine. Factors against vaccination included concerns of its effect on pregnancy, experiencing side effects, permanent injury, infertility, and risk of infection with COVID-19 from the vaccine. Factors in favor of vaccination included fear of severe COVID-19 infection, fear of infecting others with COVID-19, current available data from vaccine trials, healthcare workers acceptance of vaccination, current employment in healthcare, and fear of suffering severe illness because of their race and or ethnicity. The complete survey is found in Supplemental Table 1.
Once the links were opened by respondents, the survey had to be completed and could not be saved and returned to. The survey did not have required fields; therefore, respondents were not required to complete every question. Answer choices of “not applicable” or “not sure” were listed where appropriate. There was no incentive to complete the survey. None of the collected data had identifying information, so it could not be used to trace respondents’ answers to their patient charts. On the condition of grant of waiver for informed consent by the IRB, no unique identifiers (ie, cookies or IP addresses) could be used to determine unique respondents. Because the QR code linked to the survey was posted on flyers at the virtual events, we were unable to determine an absolute response rate.
Statistical analysis
Participants’ characteristics were summarized for the overall sample and by group of pregnancy status into 3 categories: (1) nonpregnant nonbreastfeeding respondents, (2) nonpregnant breastfeeding respondents, and (3) pregnant respondents. Medians with interquartile ranges (IQRs) were used to describe continuous variables and frequencies (percentages) for categorical variables. Group difference in baseline characteristics were compared using in Kruskal-Wallis test, chi-squared test, or Fisher exact test where appropriate. We used Poisson regression models to estimate the bivariate associations between multiple patient-level factors and vaccine acceptability. For the binary outcome of vaccine acceptability, prevalence ratios (PRs) were calculated. Omitted answers were not included in the analysis. All analyses were conducted using SAS (version 9.4; SAS Institute Inc, Cary, NC). Two-sided P≤.05 was considered statistically significant.
Results
In total, we had 1012 respondents. Of all the respondents who completed the survey, 466 (46.9%) were non-Hispanic White, 108 (10.9%) were non-Hispanic Black, 286 (28.8%) were Hispanic, 82 (8.2%) were non-Hispanic Asian, 52 (5.2%) classified as other, and 18 (1.8%) did not report any race or ethnicity. The median age was 36 years (IQR, 25–47 years); 390 (39.2%) were healthcare workers but only 5.8% were physicians. Of all respondents, 790 (79.6%) were employed with 317 (31.9%) reporting working from home either primarily or partially. A total of 656 respondents (64.8%) were pregnant, 216 (21.3%) were nonpregnant nonbreastfeeding, 122 (12.1%) were nonpregnant breastfeeding, and 18 respondents (1.8%) did not answer this question and were not included in the analysis. Of these, 390 respondents (39.2%) classified as working in healthcare; 106 (10.7%) specified their position in healthcare as “other,” 61 (6.1%) were nurses, 58 (5.8%) were doctors, and 57 (5.7%) were support staff (secretary, environmental services, patient educators, phlebotomist). The remainder of healthcare professions were represented in smaller numbers and included social workers, dieticians, physical therapists, medical and nurse assistants, nurse practitioners, nurse midwives, therapists, psychologist, physician assistants, and dentists (Supplemental Table 1). Among the 3 mutually exclusive groups, pregnant respondents tended to be younger, more likely to have had a conversation with a doctor regarding the vaccine, and more likely to be working from home. Nonpregnant respondents were more likely to have chronic hypertension at 11.1% than 3.2% and 6.6% among pregnant and breastfeeding respondents, respectively (P=.001), with the remainder of comorbidities the same among the 3 groups except for gestational diabetes (Table 1 ).
Table 1.
Baseline characteristics
| Variable | Nonpregnant (n=656, 64.8%) | Pregnant (n=216, 21.3%) | Breastfeeding (n=122, 12.1%) | P value |
|---|---|---|---|---|
| Age | 37.0 (16.0) | 34.0 (6.0) | 35.0 (7.0) | <.001 |
| Race or ethnicity | .04 | |||
| Non-Hispanic White | 311 (47.4) | 98 (45.4) | 57 (46.7) | |
| Non-Hispanic Black | 83 (12.7) | 13 (6.0) | 12 (9.8) | |
| Hispanics | 179 (27.3) | 74 (34.3) | 33 (27.0) | |
| Non-Hispanic Asian | 54 (8.2) | 20 (9.3) | 8 (6.6) | |
| Others | 29 (4.4) | 11 (5.1) | 12 (9.8) | |
| Language | <.001 | |||
| English | 612 (93.3) | 189 (87.5) | 99 (81.1) | |
| Spanish | 40 (6.1) | 27 (12.5) | 22 (18.0) | |
| Other | 4 (0.6) | 0 (0.0) | 1 (0.8) | |
| Healthcare provider | .018 | |||
| Midwife | 3 (0.5) | 4 (1.9) | 3 (2.5) | |
| Nurse practitioner | 38 (5.8) | 10 (4.6) | 8 (6.6) | |
| Other | 16 (2.4) | 3 (1.4) | 8 (6.6) | |
| Physician | 598 (91.2) | 199 (92.1) | 103 (84.4) | |
| Physician (healthcare provider) | <.001 | |||
| Family Medicine | 50 (7.6) | 27 (12.5) | 9 (7.4) | |
| Internal Medicine | 336 (51.2) | 80 (37.0) | 31 (25.4) | |
| Obstetrics and Gynecology | 185 (28.2) | 83 (38.4) | 61 (50.0) | |
| Other | 26 (4.0) | 8 (3.7) | 2 (1.6) | |
| Previous conversation with a healthcare provider regarding vaccination | .04 | |||
| Yes | 189 (31.6) | 79 (41.1) | 34 (29.8) | |
| No | 409 (68.4) | 113 (58.9) | 80 (70.2) | |
| Chronic conditions | ||||
| Composite comorbidity | 274 (41.8) | 80 (37.0) | 43 (35.2) | .248 |
| Asthma | 84 (12.8) | 29 (13.4) | 13 (10.7) | .75 |
| Chronic obstructive pulmonary disease | 3 (0.5) | 2 (0.9) | 0 (0.0) | .49 |
| Sickle cell disease | 1 (0.2) | 0 (0.0) | 2 (1.6) | .015 |
| Heart condition | 13 (2.0) | 2 (0.9) | 0 (0.0) | .19 |
| Diabetes mellitus before pregnancy | 13 (2.0) | 6 (2.8) | 3 (2.5) | .77 |
| Diabetes mellitus in pregnancy (pregnant only) | 15 (2.3) | 10 (4.6) | 14 (11.5) | <.001 |
| High blood pressure or chronic hypertension | 73 (11.1) | 7 (3.2) | 8 (6.6) | .001 |
| Immunocompromised (HIV, cancer, etc) | 20 (3.0) | 2 (0.9) | 2 (1.6) | .18 |
| Tobacco use | 5 (0.8) | 1 (0.5) | 1 (0.8) | .89 |
| Other | 69 (10.5) | 23 (10.6) | 6 (4.9) | .15 |
| Currently employed | 536 (81.8) | 174 (80.6) | 80 (65.6) | <.001 |
| Currently working from home? | ||||
| Yes | 165 (25.2) | 77 (35.6) | 34 (27.9) | .008 |
| No | 62 (9.5) | 21 (9.7) | 9 (7.4) | |
| Partially | 36 (5.5) | 2 (0.9) | 3 (2.5) | |
| Healthcare worker | 281 (42.8) | 74 (34.3) | 35 (28.7) | .016 |
| Role | .07 | |||
| Support staff (secretary, custodial staff, cleaning personnel, patient educators, phlebotomist) | 47 (7.2) | 7 (3.2) | 3 (2.5) | |
| Social worker | 9 (1.4) | 2 (0.9) | 3 (2.5) | |
| Dietician | 13 (2.0) | 1 (0.5) | 1 (0.8) | |
| Physical or occupational therapist | 8 (1.2) | 3 (1.4) | 1 (0.8) | |
| Medical or nurse assistant | 11 (1.7) | 1 (0.5) | 0 (0.0) | |
| Mental health counselor | 3 (0.5) | 0 (0.0) | 0 (0.0) | |
| Nurse | 47 (7.2) | 10 (4.6) | 4 (3.3) | |
| Nurse practitioner | 13 (2.0) | 4 (1.9) | 2 (1.6) | |
| Nurse midwife | 2 (0.3) | 0 (0.0) | 0 (0.0) | |
| Therapist | 3 (0.5) | 0 (0.0) | 0 (0.0) | |
| Psychologist | 10 (1.5) | 4 (1.9) | 0 (0.0) | |
| Physician's assistant | 6 (0.9) | 3 (1.4) | 2 (1.6) | |
| Doctor | 33 (5.0) | 20 (9.3) | 5 (4.1) | |
| Dentist | 0 (0.0) | 1 (0.5) | 1 (0.8) | |
| Other | 76 (11.6) | 18 (8.3) | 12 (9.8) | |
| Receipt of flu vaccine | .16 | |||
| Yes | 514 (88.3) | 175 (92.6) | 105 (92.1) | |
| No | 68 (11.7) | 14 (7.4) | 9 (7.9) | |
| Receipt of flu vaccine this year | .002 | |||
| Yes | 437 (66.6) | 159 (73.6) | 79 (64.8) | |
| No | 70 (10.7) | 16 (7.4) | 25 (20.5) |
The sum of row percentages does not equal 100% because missing observations were removed.
Sutton. COVID-19 vaccine acceptance among reproductive-aged women. Am J Obstet Gynecol MFM 2021.
Nonpregnant respondents were more likely to accept vaccination with an overall rate of 76.2%, with 370 (56.4%) respondents planning to take the vaccine and 87 (13.3%) having already received the vaccine (P<.001). Breastfeeding respondents were the second most likely to accept vaccination with an overall acceptance rate of 55.2%, with 60 (49.2%) reporting a plan to take the vaccine and 4 (3.3%) reporting already have received the vaccine. Pregnant respondents had the lowest percentage of responses indicating vaccine acceptance with an overall rate of 44.3%, with only 82 respondents (38.0%) planning to be vaccinated and 4 respondents (1.9%) who were already vaccinated (P<.001). In addition, pregnant respondents had the highest percentage of responses indicating vaccine declination with 59 (27.3%) stating they did not plan on getting the vaccine (P<.001). Breastfeeding respondents were the most likely to report indecision toward vaccination with 32 (26.2%) stating that they were “not sure” if they would accept or decline the vaccine compared with 49 pregnant respondents (22.7%) and 91 nonpregnant respondents (13.9%) (Table 2 ).
Table 2.
Vaccine responsiveness
| Response | Nonpregnant (n=656, 64.8%) | Pregnant (n=216, 21.3%) | Breastfeeding (n=122, 12.1%) |
|---|---|---|---|
| Accepted | 457 (76.2) | 86 (44.3) | 64 (55.2) |
| Plan to be vaccinated | 370 (56.4) | 82 (38.0) | 60 (49.2) |
| Already vaccinated | 87 (13.3) | 4 (1.9) | 4 (3.3) |
| Undecided | 91 (13.9) | 49 (22.7) | 32 (26.2) |
| Declined | 52 (8.7) | 59 (30.4) | 20 (17.2) |
Sutton. COVID-19 vaccine acceptance among reproductive-aged women. Am J Obstet Gynecol MFM 2021.
PRs were calculated for characteristics associated with vaccine acceptance. For race and ethnicity, PRs were calculated using non-Hispanic White respondents as reference. We found that all races were less likely to accept vaccination compared with White respondents except for non-Hispanic Asian respondents (Table 3 ). In addition, pregnancy and breastfeeding status were found to not be associated with vaccine acceptance. Using English language as the reference, Spanish-speaking respondents were less likely to accept vaccination compared with English-speaking respondents. Working in healthcare was not associated with vaccine acceptance (Table 3). When examined by individual profession using doctors as reference, nurses were no more or less likely to accept vaccination. When we analyzed 3 responses (acceptance, declination, undecided) between healthcare workers and nonhealthcare workers, we found no significant differences among the groups even when subdivided by type of healthcare worker (Supplemental Table 5). Having at least one chronic condition among those queried was not associated with vaccine acceptance. When analyzing chronic conditions separately, there were some marginal differences. Receipt of the flu vaccine was associated with vaccine acceptance (PR, 2.25; 95% confidence interval, 1.66–3.05).
Table 3.
Prevalence ratios for vaccine acceptance
| Variable | Prevalence ratio | 95% confidence interval | P value |
|---|---|---|---|
| Age, median (IQR) | <.0001 | ||
| Race or ethnicity | |||
| Non-Hispanic White | Reference | ||
| Non-Hispanic Black | 0.69 | 0.58–0.82 | |
| Hispanics | 0.64 | 0.56–0.73 | |
| Non-Hispanic Asian | 0.99 | 0.86–1.13 | |
| Others | 0.76 | 0.60–0.97 | |
| Language | |||
| English | Reference | ||
| Spanish | 0.75 | 0.61–0.93 | |
| Patient's healthcare provider | |||
| Physician | Reference | ||
| Obstetrics and Gynecology | Reference | ||
| Family medicine | 0.91 | 0.75–1.12 | |
| Internal medicine | 1.14 | 1.03–1.27 | |
| Other | 1.08 | 0.85–1.37 | |
| Midwife | 0.33 | 0.10–1.12 | |
| Nurse practitioner | 0.97 | 0.79–1.18 | |
| Other | 0.74 | 0.49–1.11 | |
| Previous conversation with a healthcare provider regarding vaccination | |||
| No | Reference | ||
| Yes | 1.04 | 0.95–1.15 | |
| Chronic conditions | |||
| No conditions | Reference | ||
| Composite condition | 0.96 | 0.88–1.06 | |
| Healthcare worker | |||
| No | Reference | ||
| Yes | 1.03 | 0.93–1.13 | |
| Doctor | Reference | ||
| Support staff (secretary, custodial staff, cleaning personnel, patient educators, phlebotomist) | 0.81 | 0.61–1.09 | |
| Social worker | 0.97 | 0.65–1.44 | |
| Dietician | 1.12 | 0.82–1.51 | |
| Physical or occupational therapist | 1.01 | 0.68–1.51 | |
| Medical or nurse assistant | 0.62 | 0.29–1.31 | |
| Mental health counselor | 1.39 | 1.18–1.65 | |
| Nurse | 0.96 | 0.74–1.23 | |
| Nurse practitioner | 0.95 | 0.67–1.35 | |
| Nurse midwife | 1.39 | 1.18–1.65 | |
| Therapist | 1.39 | 1.18–1.65 | |
| Psychologist | 0.86 | 0.54–1.36 | |
| Physician's assistant | 0.81 | 0.49–1.35 | |
| Dentist | 1.39 | 1.18–1.65 | |
| Other | 0.94 | 0.76–1.17 | |
| Previous positive COVID-19 test | |||
| No | Reference | ||
| Yes | 0.46 | 0.21–1.01 | |
| Current pregnant | |||
| No | Reference | ||
| Yes | 0.61 | 0.52–0.72 | |
| Currently breastfeeding | |||
| No | Reference | ||
| Yes | 0.73 | 0.61–0.86 | |
| Receipt of flu vaccine | |||
| No | Reference | ||
| Yes | 2.25 | 1.66–3.05 |
IQR, interquartile range.
Sutton. COVID-19 vaccine acceptance among reproductive-aged women. Am J Obstet Gynecol MFM 2021.
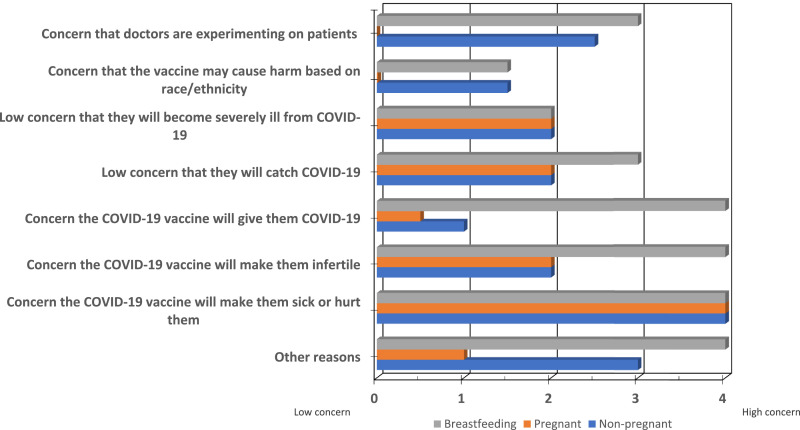
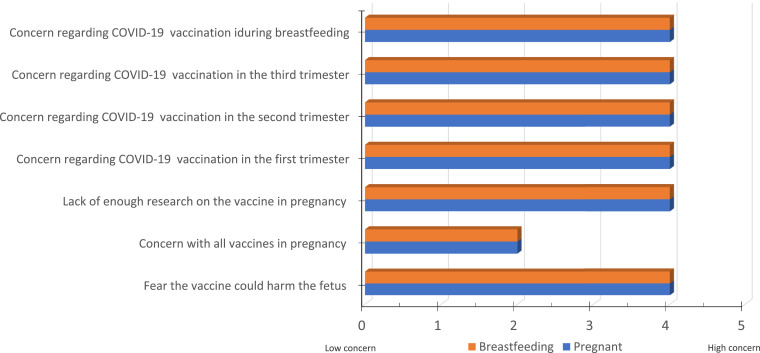
When queried regarding specific concerns about the vaccines, we found that those who declined vaccination were highly concerned that the vaccine would make them sick or harm them (Figure 1 , A). The next highest reported contributions to vaccine declination was the belief of having a low risk to contract and become severely ill from COVID-19 (median score, 2.0/5.0; IQR, 0.5–3.5). Among vaccine decliners, breastfeeding respondents shared similar concerns but were also concerned that the vaccine would cause them to become infertile (median score, 4.0/5.0; IQR, 2.5–5.0). Among pregnant vaccine decliners, there was a high concern of being vaccinated against COVID-19 in all trimesters. However, this was not uniformly shared toward all vaccines, such as vaccines against influenza or pertussis (Figure 1, B). There was additional concern regarding a lack of sufficient research on COVID-19 vaccination in pregnancy (median score, 4.0/5.0; IQR, 2.0–5.0) and fear that it could harm the fetus (median score, 4.0/5.0; IQR, 3.0–5.0).
Figure 1.
All respondents declining vaccination were questioned on specific reasons for declination
The bars represent the mean scores from 0 meaning “low or no concern” to 5 “highly concerned.”
Sutton. COVID-19 vaccine acceptance among reproductive-aged women. Am J Obstet Gynecol MFM 2021.
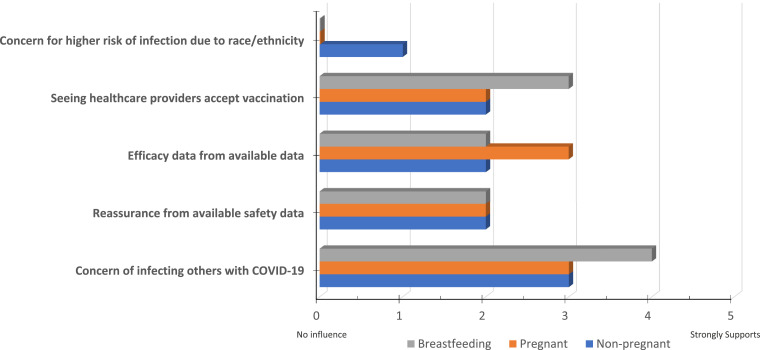
Among those who accept vaccination, influences that favored vaccination included efficacy data from available publications; reassurance from available safety data; concern that, if they became positive, they could infect others; and seeing healthcare providers vaccinated (Figure 2 , A). Most of our respondents had a very low concern of having a higher risk of infection because of their race or ethnicity (median score, 0.0/5/0; IQR, 0.0–2.0). When we examined the response to this question by race and ethnicity, we found that non-Hispanic White respondents consistently gave median scores of 0 for those questions whereas Hispanic and non-Hispanic Black respondents consistently chose scores that ranged from 1 to 3.5 of 5.0 among nonpregnant, pregnant, and breastfeeding respondents (Supplemental Tables 2 and 3).
Figure 2.
All pregnant respondents declining vaccination were questioned on pregnancy-related reasons for declination
The bars represent the mean scores from 0 meaning “low or no concern” to 5 “highly concerned.”
Sutton. COVID-19 vaccine acceptance among reproductive-aged women. Am J Obstet Gynecol MFM 2021.
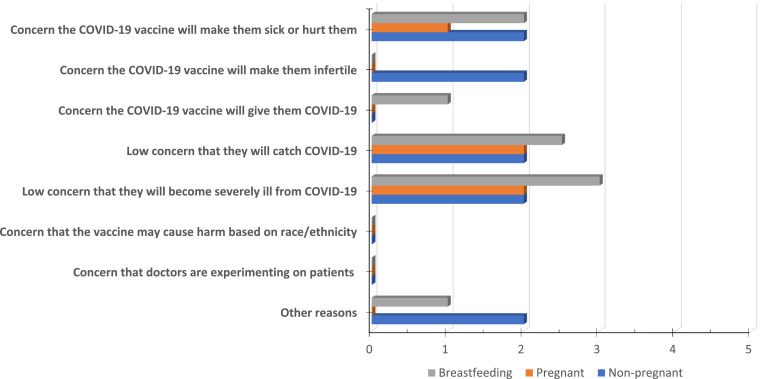
Among those who were undecided regarding vaccination, influences against vaccination included concern for the vaccine causing them harm and a belief that they themselves would not contract the virus or become severely ill from the virus (Figure 3 , A). Respondents were also invited to fill in their own personal reasons for accepting or declining vaccination which were aggregated under common categories (Supplemental Tables 6 and 7). The most common reasons for declining vaccination included concern for short- or long-term side effects, the speed of the development of the vaccine, fear of harming the pregnancy, previous allergy or anaphylaxis, lack of sufficient research, and potential interaction with other medical comorbidities. The most common reasons for desiring vaccination included having family or friends who were at a high risk of severe infection, personal immunity, presence of chronic comorbidities, protecting children, and contribution toward herd immunity.
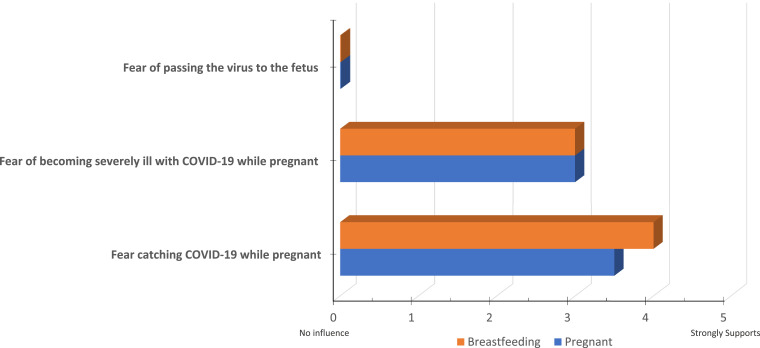
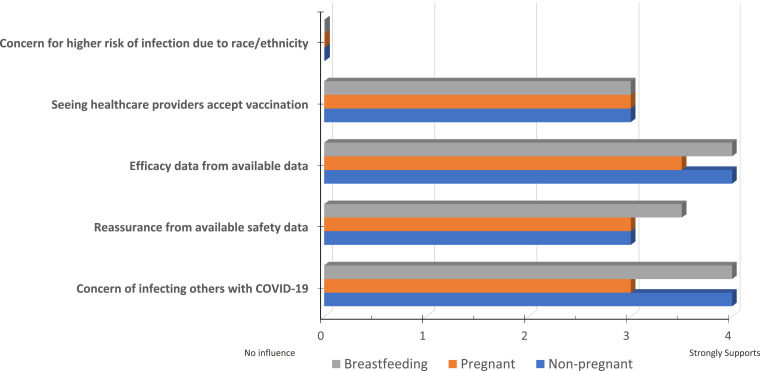
Figure 4.
All pregnant respondents accepting vaccination were questioned on pregnancy-related reasons for acceptance
The bars represent the mean scores from 0 meaning “little or no influence” to 5 “strongly supports.”
Sutton. COVID-19 vaccine acceptance among reproductive-aged women. Am J Obstet Gynecol MFM 2021.
Figure 5.
All hesitant respondents were questioned on reasons for declination
The bars represent the mean scores from 0 meaning “low or no concern” to 5 “highly concerned.”
Sutton. COVID-19 vaccine acceptance among reproductive-aged women. Am J Obstet Gynecol MFM 2021.
Figure 6.
All hesitant respondents were questioned on specific reasons for acceptance
The bars represent the mean scores from 0 meaning “little or no influence” to 5 “strongly supports.”
Sutton. COVID-19 vaccine acceptance among reproductive-aged women. Am J Obstet Gynecol MFM 2021.
Figure 3.
All respondents accepting vaccination were questioned on specific reasons for acceptance
The bars represent the mean scores from 0 meaning “little or no influence” to 5 “strongly supports.”
Sutton. COVID-19 vaccine acceptance among reproductive-aged women. Am J Obstet Gynecol MFM 2021.
Discussion
Clinical implications
Our study found that pregnant respondents were more likely to decline vaccination than nonpregnant and breastfeeding respondents. As a whole, healthcare workers were no more likely to be accepting of vaccines than nonhealthcare workers. When examined by individual healthcare profession, nurses were no more likely to accept vaccination than doctors. However, some professions had higher associations of vaccine acceptance, such as nurse midwives, therapists, mental health counselors, and dentists. Among pregnant respondents, specific reasons for declination typically related to concerns for the vaccine causing them or their fetus harm, causing infertility, and beliefs that they were at a low risk of contracting or becoming severely ill from COVID-19. We did not find varying levels of concern by trimester, and we did not see similar levels of concern with all vaccines in pregnancy. When we calculated PRs for vaccine acceptance, we found that non-White race and primarily non-English speaking respondents were more likely to decline vaccination. In all, our study is in line with findings from previously published surveys on vaccine acceptance.
A survey study conducted before the release of the vaccine by Schwarzinger et al5 of 1942 working-age adults found that 28.8% declined vaccination with declination significantly associated with female gender (34.5% vs 22.9%; p < 0.0001) and lower perceived severity of COVID-19 (OR 0.5, 95% CI 0.32-0.80; p=0.004). In the small pregnant portion of their majorly French cohort, they found that most pregnant respondents declined vaccination (14 of 23, 60.9%). A lack of research on the effects of the vaccine in pregnancy could affect the acceptance rate in pregnant women and women hoping to become pregnant in the near future. In another recently published survey study from our institution, women who were pregnant or seeking to conceive within the next 6 months were also found to be less likely to accept a messenger RNA COVID-19 vaccine (17.5% vs 47.3% for pregnant vs nonpregnant, P=.00001, and 41.3% vs 65.2% planning vs not planning to conceive, P=.0062) citing concern for unknown long-term health consequences on children and risk of pregnancy loss.6 One survey of 800 nurses in Hong Kong, China, found that there was a low level of COVID-19 vaccine acceptance and a high proportion of indecision because of concerns in pregnancy.7 We also found that healthcare workers were no more likely to accept vaccination. Although this should be interpreted with caution, other studies have published similar findings.
A large portion of our cohort worked in healthcare with a small minority serving as physicians. This was not surprising for 2 reasons. First, we distributed the survey at a virtual event for staff regarding COVID-19 vaccination. Second, a large portion of our staff uses the institution and our providers for healthcare. In our cohort, working in healthcare was not associated with vaccine acceptance. At first glance, this may seem discrepant in comparison with other studies. Gagneux-Brunon et al8 conducted a survey of healthcare workers on the frontline during the first wave of the pandemic in France and found high rates of vaccine acceptance at 76.9%. However, when they looked at the factors associated with vaccine acceptance, they found older age (respondents aged > 65 years had an OR 1.27, 95%CI 0.93-1.74 for vaccine acceptance in multivariable analysis using age < 30 years as the reference) and male gender (OR 1.88, 95%CI 1.38-2.56, P<0.001) as significant factors and found that nurses and assistant nurses were less inclined to getting the vaccine compared with doctors. Wang et al7 also surveyed nurses in Hong Kong, China, and found that only 40.0% accepted vaccination primarily because of the unknown effects of the vaccine on pregnancy. Another key distinction between these studies and ours is that our data were first to be collected and reported on after the release of the COVID-19 vaccine to general public with the currently available data from clinical trials.
Research implications
Our findings and those from previous studies further strengthen the stance of almost all major obstetrical professional societies including ACOG and SMFM that were uniformly disappointed in the lack of inclusion of pregnant women in clinical trials. Safeguarding pregnancy is vital for the propagation of our population. Pregnant women should be allowed to participate and take advantage of the safety measures built into IRB-approved modern clinical trials. This will allow their providers to take part in shared decision making with them using high-quality research in a patient population that is at a high risk of morbidity and mortality. Future research also needs to further evaluate vaccine declination and indecision among minority populations.
The survey by Fisher et al7 found that Black race was associated with vaccine declination and indecision with 39% of Black respondents willing to take the vaccine compared with 64% of White respondents. We found similar findings in our cohort when examining PRs comparing non-White with White respondents. Because there exists substantial racial disparity in morbidity and mortality from COVID-19, further investigation into reasoning behind vaccine indecision and declination among minority populations is vital.9 Although we don't yet have many comprehensive studies examining the reasons behind COVID-19 vaccine declination and indecision in Black and Hispanic women, past atrocities committed by scientific investigators have been written about in multiple media publications. Much of the distrust comes from historic injustices like the Tuskegee Syphilis study where curative treatment from syphilis was withheld from hundreds of Black men to study the natural progression of the disease. Current disparities among Black and Hispanic patients across all of medicine likely worsen distrust. Future research should focus on identifying sources of distrust and interventions geared at dismantling those barriers. In addition, we need continued reporting from clinical trials and education for all pregnant individuals, but especially for those in communities disproportionately affected by COVID-19. In our survey, respondents were able to fill in their own concerns which we aggregated under common themes in Supplemental Tables 5 and 6. Our respondents were specifically concerned about the short-term effects, long-term effects, overall safety, and the speed of vaccine development. Future research and education geared toward these themes may aid in decision making between respondents and their healthcare provider.
Strengths and limitations
Our study has several limitations. We are unable to report a response rate to our survey because of the nature of distribution. Although we know how many women received the survey by email, we are unable to differentiate them from those who received the survey by QR code from flyers that were posted in the hospital, at doctor's offices, and at several virtual town halls that were held for employees of our institution to discuss the COVID-19 vaccine. Survey studies with low response rates are at a higher risk of sampling bias. Although the QR code was removed from view before the discussion at the virtual town hall, it is possible that some of the respondents answered our survey after completion of the event. However, because of the lack of research in pregnancy, many of their questions regarding the safety and efficacy of the vaccine could not be answered definitely. Thus, we would expect that their responses to the survey would still be representative of the concerns of those within their cohort. This study also used a web-based survey which required respondents to have access to or ability to navigate the internet. The strengths of this study include its large number of respondents which was very diverse in self-reported race and ethnicity. This study focuses primarily on women with a large proportion within the reproductive age range. In addition, no other study has analyzed responses among pregnant, breastfeeding, and nonpregnant women.
Conclusions
As of the publication of this study, the COVID-19 pandemic has killed more than 500,000 Americans, and emerging data show that the vaccine may be the most efficacious way at limiting morbidity and mortality from the disease. Because reproductive-aged women make up a considerable portion of our population with unique concerns, studies that elucidate the said concerns are vital in ensuring that proper research outcomes are investigated and efficient outreach is performed to maximize vaccine uptake and hasten the end of this deadly pandemic.
Footnotes
M.D. has had a leadership role in the American College of Obstetricians and Gynecologists II's Safe Motherhood Initiative, which has received unrestricted funding from Merck for Mothers. C.G.B. disclosed receiving money paid to her institution from Society for Maternal-Fetal Medicine/AMAG. She also received funding from Sera Prognostics and various funds for medicolegal work. She also disclosed receiving National Institutes of Health grants. The other authors report no conflict of interest.
Cite this article as: Sutton D, D'Alton M, Zhang Y, et al. COVID-19 vaccine acceptance among pregnant, breastfeeding, and nonpregnant reproductive-aged women. Am J Obstet Gynecol MFM 2021;XX:x.ex–x.ex.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajogmf.2021.100403.
Appendix. Supplementary materials
References
- 1.Ogedegbe G, Ravenell J, Adhikari S, et al. Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York City. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.26881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zambrano LD, Ellington S, Strid P, et al. Update: characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status - United States, January 22-October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1641–1647. doi: 10.15585/mmwr.mm6944e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The American College of Obstetricians and Gynecologists; 2021. ACOG and SMFM joint statement on WHO recommendations Regarding COVID-19 vaccines and pregnant individuals.https://www.acog.org/news/news-releases/2021/01/acog-and-smfm-joint-statement-on-who-recommendations-regarding-covid-19-vaccines-and-pregnant-individuals Available at: Accessed February 16, 2021. [Google Scholar]
- 5.Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6:e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turocy J, Robles A, Reshef E, D'Alton M, Forman E, Williams Z. A survey of fertility patients’ attitudes towards the COVID-19 vaccine. Fertility & Sterility. 2021 https://www.fertstertdialog.com/posts/a-survey-of-fertility-patients-attitudes-towards-the-covid-19-vaccine Available at: Accessed February 21, 2021. [Google Scholar]
- 7.Wang K, Wong ELY, Ho KF, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine. 2020;38:7049–7056. doi: 10.1016/j.vaccine.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gagneux-Brunon A, Detoc M, Bruel S, et al. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect. 2021;108:168–173. doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muñoz-Price LS, Nattinger AB, Rivera F, et al. Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.21892. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.