Abstract
The general population has increasingly become the key contributor to irrational antibiotic use in China, which fuels the emergence of antibiotic resistance. This study aimed to estimate the prevalence of the general population’s irrational use behaviors of antibiotics and identify the potential reasons behind them. A systematic review and meta-analysis were performed concerning four main behaviors relevant to easy access and irrational use of antibiotics and common misunderstandings among the population about antibiotics. Four databases were searched, and studies published before 28 February 2021 were retrieved. Medium and high-level quality studies were included. Random effects meta-analysis was performed to calculate the prevalence of the general population’s irrational behaviors and misunderstandings relevant to antibiotic use. A total of 8468 studies were retrieved and 78 met the criteria and were included. The synthesis showed the public can easily obtain unnecessary antibiotics, with an estimated 37% (95% CI: 29–46) of the population demanding antibiotics from physicians and 47% (95% CI: 38–57) purchasing non-prescription antibiotics from pharmacies. This situation is severe in the western area of China. People also commonly inappropriately use antibiotics by not following antibiotic prescriptions (pooled estimate: 48%, 95% CI: 41–55) and preventatively use antibiotics for non-indicated diseases (pooled estimate: 35%, 95% CI: 29–42). Misunderstanding of antibiotic use was also popular among people, including incorrect antibiotic recognition, wrong antibiotic use indication, inappropriate usage, and ignorance of potential adverse outcomes. Over-and inappropriate use of antibiotics is evident in China and a multifaceted antibiotic strategy targeted at the general population is urgently required.
Keywords: general population, non-prescription purchase, demand for antibiotics, non-adherence, prophylactic antibiotic use, misunderstanding of antibiotics
1. Introduction
In the past several decades, antibiotic resistance (AR) has been increasingly recognized as one of the biggest threats to public health and economic development worldwide, as it makes common infectious diseases difficult to treat and results in increased mortality and treatment cost [1,2,3]. It has been reported that around 700,000 people die from AR worldwide every year. Without effective countermeasures, this figure is estimated to reach 10 million by 2050, leading to USD 100 trillion economic losses worldwide [4]. In addition to the huge loss to society, patients with AR also require extra hospital stays, additional costs, and have an even greater risk of mortality compared to those without infections [5,6].
To address this issue, a call for whole society engagement from one health perspective is required, covering everyone from all sectors and disciplines who should be responsible for preserving the effectiveness of the antibiotic agents [1]. Among the various stakeholders, the widespread inappropriate and overuse of antibiotics in humans still fuel the emergence of AR [7,8,9]. Though antibiotics are commonly prescription-required medicine for infectious diseases, existing studies have shown that people’s behaviors also play a role contributing to overuse of antibiotics [10,11,12], such as non-prescription purchasing of antibiotics, self-medication of antibiotics, storing and sharing of antibiotics, etc. [13,14,15]. Furthermore, the public’s behaviors can also sway physician’s rational use of antibiotics via expectation and pressure for antibiotics, which has been criticized as one key factor contributing to the unnecessary use of antibiotics by physicians [16,17,18,19,20].
However, people’s irrational use behaviors relevant to antibiotics are prevalent around the world [12,21,22,23]. A systematic review showed that the prevalence of self-medication of antibiotics is around 50% in the southeast Asian region [24]. More than half of pharmacy’s customers purchased antibiotics without a prescription globally and the proportion is much higher in developing countries, such as Indonesia and Ethiopia [19,25]. Furthermore, a recent systematic review showed that around 43% of patients expected antibiotics for respiratory tract infections worldwide [26] and existing studies showed that almost all (96.5%) of these patients are estimated to receive antibiotics [27].
As one of the largest consumers of antibiotics worldwide, China has been long criticized for its over and irrational use. Due to introducing a series of restrictive policies in the past decade, physician’s overuse of antibiotics has been significantly reduced [28]. However, a recent study has shown that in the general population, the demand side of antibiotic misuse increasingly became the key contributors to irrational use of antibiotics [29]. For example, more than half of customers can get antibiotics without prescriptions [30]. More than two thirds of medical students kept a personal stock of antibiotics and nearly one fifth of them used antibiotics as prophylaxis and demanded antibiotics from doctors [10]. It is estimated that roughly 58% of irrational use of antibiotics is due to the general population’s irrational use of antibiotics, compared with physician’s irrational prescribing contributing to the other 42% [29].
To address this issue, it is important to understand to what extent people will behave irrationally when using antibiotics and the potential reasons behind them. In the past decade, increasing studies reported the prevalence of the general population’s irrational use of antibiotics as well as the potential factors contributing to it. Results from these studies showed high degrees of variability of findings, settings, participants, and other study characteristics. Though one recent study has qualitatively synthesized the factors influencing the general population’s irrational use of antibiotics [31], it is still unclear what the prevalence of the general population’s irrational use of antibiotic behaviors is, as well as the prevalence of potential factors contributing to it.
Therefore, this systematic review aimed to synthesize the prevalence of irrational use behaviors as well as potential reasons relevant to antibiotics in China.
2. Methods
2.1. Review Framework
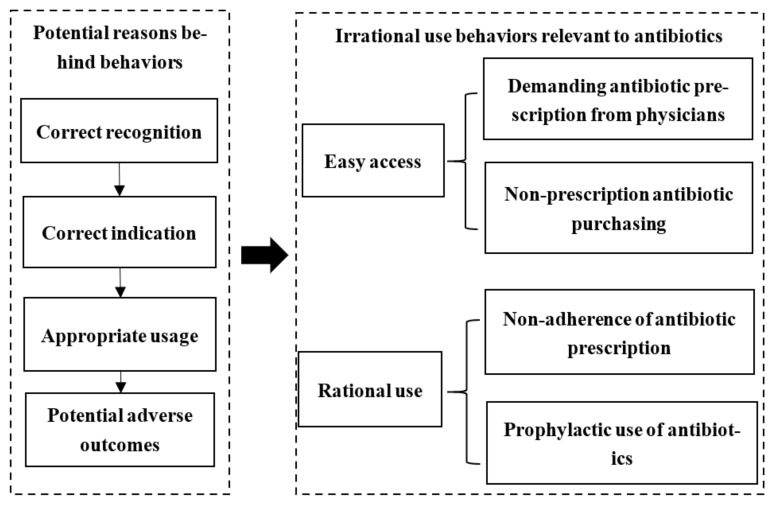
To understand the general population’s irrational use behaviors and potential reasons behind them, a review framework was developed (Figure 1), following the guidelines from the Joanna Briggs Institute (JBI) regarding the systematic reviews of prevalence and incidence [32]. The protocol of the current study has been registered in PROSPERO (No. CRD42021234432).
Figure 1.
Review framework.
Based on the World Health Organization [15], four kinds of behaviors were highlighted which are prevalent among general populations, including demanding antibiotic prescriptions from physicians, non-prescription antibiotic purchasing from pharmacies, non-adherence to antibiotic prescriptions, and prophylactic use of antibiotics. In the current study, these behaviors were classified into two aspects, namely, easy access to antibiotics and irrational use of antibiotics. In the current study, the general population refers to patients and people that are potential patients, for example, residents, the elderly, parents, etc. Prophylactic use of antibiotics refers to the behavior of people taking antibiotics to prevent common infectious diseases, such as the cold or flu, which are mainly non-indicated diseases [33].
In terms of potential reasons for behaviors, the definition of responsible antibiotic use was adopted [34]. To ensure a rational use of antibiotics, people are first required to correctly recognize the common antibiotics, understand the indications antibiotics may help, and, finally, know the appropriate usage and potential adverse outcomes. Thus, the general population’s correct recognition of antibiotics, correct indication of antibiotic use, correct usage of antibiotics, and potential adverse outcomes of antibiotics were treated as four potential reasons for people’s behaviors relevant to antibiotic use.
2.2. Search Strategy
Four databases were searched to identify relevant studies published before 28 February 2021, including the China National Knowledge Infrastructure (CNKI), VIP database, WANFANG database, and Chinese Biomedical Literature Service System (CBLSS). The development of search strategies followed participant, intervention, comparison, and outcome (PICOs) principles and search terms included “antibiotic”, “the general population”, “irrational use”, “behavior”, “factor” and their synonyms, combined with Boolean operators (for search examples, see Table 1). Details of search strategies can be found in Table S1.
Table 1.
Search strategy.
| # | Searches |
|---|---|
| 1 | (antibacterial * or antibiotics * or antimicrobial *).af. |
| 2 | (application * or management * or use * or storage * or non-prescri * or self-medication * or irrational * or abuse * or behavior * or status quo *).af. |
| 3 | (determinants * or knowledge * or attitude * or belief * or expectation * or medical advice * or compliance *).af. |
| 4 | (residents * or population * or general population * or public * or respiratory infection patients * or middle-aged and elderly * or students * or outpatients *).af. |
| 5 | 1 and 2 and 3 and 4 |
Note: * is a truncation operator, which refers to words with same stem and different endings to ensure full coverage of study topic.
2.3. Inclusion and Exclusion Criteria
According to the review framework (Figure 1), studies reporting at least one of the four identified general population behaviors regarding antibiotic use were included. We excluded studies concentrating on irrational antibiotic prescribing behavior of healthcare providers. Qualitative studies (no quantitative measures applied), reviews, conference reports, and unavailable full-text research were also excluded. Two reviewers (DL and LC) conducted the screening process independently with a Kappa agreement of 93.1%. Discrepancies were resolved through consensus.
2.4. Quality Assessment
Quality of all included studies were assessed on nine criteria based on the “Critical Appraisal Instrument for Studies Reporting Prevalence Data” from the JBI quality evaluation tool (Appendix A) [35]. These criteria concern appropriate sample frame, sample strategy, sample size, description of research settings, coverage of the sample, validity of measurement, data collection, statistical analysis methods, and generalizability of results. Each aspect was assessed by one item, which may be assessed as high quality (scored as 1), low quality, or unclear (scored as 0). The overall quality of each study was calculated, and studies were classified into poor level of quality (0–3), moderate level of quality (4–6), or high level of quality (7–9). Only studies with moderate or high level of quality were further included for meta-analysis. Assessment was conducted by two reviewers (DL and LC) and discrepancies were resolved through consensus.
2.5. Data Extraction
A standardized data extraction chart was developed according to JBI’s guidelines (Appendix B) [32]. Three kinds of information were extracted, including basic information of research (author, year of publication, aim of the study), characteristics of methodology (study setting, research type, sampling method, sample size, characteristics of participants), and prevalence of behaviors and potential reasons regarding the general population’s antibiotic use (proportion of the four kinds of irrational antibiotic use behaviors of the general population and proportion of incorrect understanding of the general population relevant to antibiotic use). Different publications that used the same data were extracted once.
2.6. Statistical Analysis
The proportion of people who showed irrational use behaviors of antibiotics or who hold misunderstandings towards antibiotic use was synthesized. The prevalence of people’s irrational use behaviors of antibiotics was assessed based on four indicators in the current study, namely, proportion of people who demand antibiotic prescriptions from physicians, proportion of people who purchase antibiotics without prescriptions, proportion of people who do not adherent to antibiotic prescriptions, and proportion of people who prophylactically use antibiotics to prevent the cold or other non-indicated diseases. The prevalence of people’s potential reasons of their irrational use behaviors was assessed based on four aspects, covering the proportion of people who can correctly recognize common antibiotics, the proportion of people who can correctly understand indication for antibiotic use, the proportion of people who can correctly use antibiotics, and the proportion of people who are aware of adverse outcomes of antibiotic use. Data synthesis was conducted using Freeman–Tukey transformed proportions and the pooled estimates were back transformed to ordinary proportions. The random effect meta-analysis with DerSimonian and Laird approach was adopted and the pooled proportions with 95% confidence intervals were calculated.
Subgroup analyses were conducted with respect to the geographical region (eastern, central, western China), study period, type of participant (rural residents, urban residents, students, pharmacy’s customer, parents, and others), quality level (moderate/high), and study size. Q test and I2 test were performed to determine the degree of heterogeneity across studies. A multivariable meta-regression analysis was conducted to explore the potential causes of the heterogeneity. The co-variates tested included geographical region, study size, characteristics of participants, study period, and quality of the research. Sensitivity analysis was performed by excluding each study in turn to examine the effect of outliers and confirm the robustness of our findings [36]. All statistical analysis was performed using Stata (version 14.0, Texas: StataCorp).
3. Results
3.1. Study Selection and Characteristics
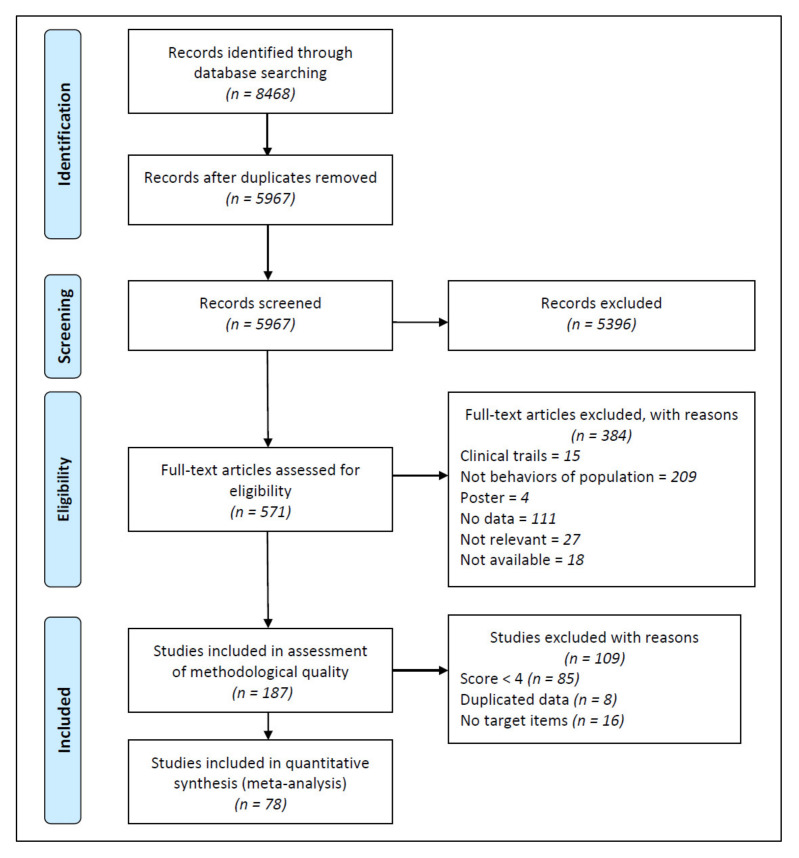
A total of 8468 articles were retrieved through the literature search, of which 187 met the inclusion criteria, and a total of 78 studies were included in the final meta-analysis (Figure 2). Almost all (71 out of 78) of the included studies applied cross-sectional design. These studies involved 79,165 participants from eastern (n = 39,181), central (n = 28,547), and western (n = 11,437) areas, covering 25 of the 34 provinces in China. The participants were rural residents (n = 11,810), urban residents (n = 18,785), rural and urban residents (n = 2946), students (n = 31,641), children’s parents (n = 7153), customers of pharmacies (n = 2168), and others (n = 4662) (Table 2).
Figure 2.
Flow diagram of study identification.
Table 2.
Characteristics of the included studies.
| First Author | Year | Region | Study Design | Type of Participants | Sample Size | Quality Assessment |
|---|---|---|---|---|---|---|
| Tian, X. [37] | 2006 | East | Cross-sectional | Students | 4980 | 4 |
| Su, D. [38] | 2006 | East | Quasi-experimental | Rural residents | 420 | 5 |
| Xie, J. [39] | 2006 | East | Quasi-experimental | Urban residents | 209 | 4 |
| Luo, J. [40] | 2008 | Central | Cross-sectional | Pharmacy customers | 1490 | 7 |
| Yin, T. [41] | 2008 | Central | Cross-sectional | Pharmacy customers | 396 | 7 |
| Hu, L. [42] | 2008 | East | Cross-sectional | Urban residents | 209 | 5 |
| Wang, Y. [43] | 2008 | East | Cross-sectional | Urban residents | 658 | 4 |
| Li, B. [44] | 2008 | Central | Cross-sectional | Children’s parents | 266 | 4 |
| Ye, L. [45] | 2009 | Central | Cross-sectional | Outpatients | 276 | 4 |
| Sun, L. [46] | 2010 | East | Cross-sectional | Students | 853 | 4 |
| Huang, W. [47] | 2011 | West | Cross-sectional | Outpatients | 956 | 5 |
| Huang, Y. [48] | 2011 | East | Cross-sectional | Urban residents | 298 | 4 |
| Ji, H. [49] | 2011 | West | Cross-sectional | Urban residents | 400 | 5 |
| Shan, H. [50] | 2011 | East | Cross-sectional | Outpatients | 1236 | 4 |
| Huang, C. [51] | 2012 | East | Cross-sectional | Rural residents | 400 | 5 |
| Cheng, S. [52] | 2012 | East | Cross-sectional | Urban residents | 164 | 5 |
| Zhao, L. [53] | 2012 | East | Cross-sectional | Rural residents | 1014 | 6 |
| Wu, Y. [54] | 2012 | West | Cross-sectional | Urban and rural residents | 1200 | 5 |
| Ma, X. [55] | 2012 | East | Cross-sectional | Urban residents | 4183 | 4 |
| Yu, M. [56] | 2012 | Central | Cross-sectional | Children’s parents | 854 | 5 |
| Liu, S. [57] | 2012 | East | Cross-sectional | Urban residents | 200 | 4 |
| Du, X. [58] | 2012 | Central | Cross-sectional | Students | 905 | 4 |
| Tao, G. [59] | 2013 | West | Quasi-experimental | Urban residents | 1000 | 6 |
| Li, Y. [60] | 2013 | East | Cross-sectional | Rural residents | 1589 | 5 |
| Jin, Y. [61] | 2013 | West | Cross-sectional | Urban residents | 2556 | 5 |
| Ye, W. [62] | 2013 | East | Cross-sectional | Rural residents | 800 | 4 |
| Tang, X. [63] | 2013 | East | Cross-sectional | Outpatients | 496 | 4 |
| Zhang, Y. [64] | 2013 | East | Cross-sectional | Students | 1180 | 4 |
| Xu, Y. [65] | 2013 | East | Cross-sectional | Urban residents | 106 | 5 |
| Liu, M. [66] | 2013 | East | Cross-sectional | Children’s parents | 1046 | 7 |
| Sun, W. [67] | 2014 | East | Quasi-experimental | Children’s parents | 593 | 6 |
| Ding, L. [68] | 2014 | East | Cross-sectional | Children’s parents | 722 | 5 |
| Tian, L. [69] | 2014 | East | Cross-sectional | Urban residents | 316 | 5 |
| Han, F. [70] | 2014 | Central | Cross-sectional | Students | 4462 | 5 |
| Yuan, J. [71] | 2014 | West | Cross-sectional | Rural residents | 435 | 6 |
| Bian, C. [72] | 2014 | Central | Cross-sectional | Outpatients | 1214 | 4 |
| Zhang, S. [73] | 2014 | Central | Cross-sectional | Urban residents | 500 | 5 |
| Xiong, X. [74] | 2014 | East | Cross-sectional | Urban residents | 354 | 4 |
| Lin, W. [75] | 2014 | East | Cross-sectional | Urban residents | 1784 | 5 |
| Sun, Y. [76] | 2014 | Central | Cross-sectional | Students | 388 | 4 |
| Liu, Y. [77] | 2015 | East | Quasi-experimental | Rural residents | 639 | 7 |
| Diao, M. [78] | 2015 | Central | Cross-sectional | Rural residents | 2047 | 5 |
| Chen, S. [79] | 2015 | East | Cross-sectional | Teachers | 84 | 8 |
| Wang, X. [80] | 2015 | Central | Cross-sectional | Students | 11,192 | 5 |
| Li, Y. [60] | 2015 | Central | Cross-sectional | Students | 692 | 5 |
| Cheng, J. [81] | 2015 | Central | Cross-sectional | Rural residents | 2611 | 6 |
| Zhang, Y. [82] | 2015 | East | Cross-sectional | Children’s parents | 250 | 6 |
| Song, Y. [83] | 2015 | East | Cross-sectional | Students | 812 | 4 |
| Cui, B. [84] | 2015 | East | Cross-sectional | Students | 528 | 4 |
| Ding, L. [85] | 2015 | East | Cross-sectional | Rural residents | 769 | 6 |
| Wang, G. [86] | 2015 | East | Cross-sectional | Urban residents | 1718 | 5 |
| Yu, Y. [87] | 2015 | East | Cross-sectional | Urban residents | 267 | 5 |
| Lei, Z. [88] | 2015 | Central | Cross-sectional | Pharmacy customers | 282 | 4 |
| Chen, C. [89] | 2016 | East | Cross-sectional | Civil servants | 400 | 5 |
| Tang, Z. [90] | 2016 | West | Cross-sectional | Children’s parents | 766 | 5 |
| Wang, Z. [91] | 2016 | East | Cross-sectional | Urban and rural residents | 438 | 5 |
| Jiang, H. [92] | 2016 | East | Cross-sectional | Urban residents | 449 | 6 |
| Wang, Q. [93] | 2016 | West | Cross-sectional | Students | 1584 | 4 |
| Jiang, Y. [94] | 2017 | East | Cross-sectional | Urban and rural residents | 651 | 4 |
| Luo, Y. [95] | 2017 | West | Cross-sectional | Students | 368 | 5 |
| Yang, Q. [96] | 2017 | East | Cross-sectional | Children’s parents | 713 | 4 |
| Wang, P. [97] | 2017 | East | Cross-sectional | Students | 1957 | 4 |
| Li, X. [98] | 2017 | East | Cross-sectional | Children’s parents | 658 | 4 |
| Piao, S. [99] | 2018 | East | Cross-sectional | Urban residents | 181 | 4 |
| Qin, Z. [100] | 2018 | West | Cross-sectional | Urban residents | 518 | 4 |
| Jiang, Y. [101] | 2019 | Central | Cross-sectional | Urban and rural residents | 657 | 6 |
| Cao, L. [102] | NA | East | Cross-sectional | Children’s parents | 1080 | 4 |
| Tan, Y. [103] | NA | West | Cross-sectional | Rural residents | 800 | 4 |
| Ye, L. [104] | NA | East | Cross-sectional | Students | 152 | 6 |
| Yao, X. [105] | NA | East | Cross-sectional | Students | 270 | 6 |
| Zhao, Y. [106] | NA | West | Cross-sectional | Students | 363 | 4 |
| Li, J. [107] | NA | West | Cross-sectional | Rural residents | 286 | 4 |
| Huang, C. [108] | NA | East | Quasi-experimental | Urban residents | 400 | 4 |
| Wu, C. [109] | NA | East | Quasi-experimental | Students | 337 | 4 |
| Wen, W. [110] | NA | Central | Cross-sectional | Urban residents | 315 | 4 |
| Lu, Z. [111] | NA | East | Cross-sectional | Students | 600 | 5 |
| Rong, J. [112] | NA | East | Cross-sectional | Urban residents | 2000 | 4 |
| Zhang, Y. [113] | NA | West | Cross-sectional | Children’s parents | 205 | 4 |
Among the four kinds of irrational use behaviors of people, demanding antibiotic prescription was surveyed by nearly half of the included studies (n = 30), followed by non-adherence to antibiotic prescriptions (n = 30), non-prescription purchasing (n = 29), and prophylactic use of antibiotics (n = 20). In terms of potential reasons of these behaviors, roughly half of the included studies surveyed the public’s incorrect recognition of antibiotics (n = 39), followed by people’s misconception of incorrect indication (antibiotic killing virus, n = 29; antibiotic cures the cold, n = 21), incorrect usage (antibiotic courses, n = 15; combination antibiotic use, n = 21), and potential adverse outcomes (antibiotic resistance, n = 36; adverse reaction, n = 11).
Studies included were deemed to be at a moderate or high level of quality (score >3). The most common source of bias was from sample coverage (71/78, 91.03%), for which most articles did not report a justification for whether they achieved a sufficient coverage of the identified sample.
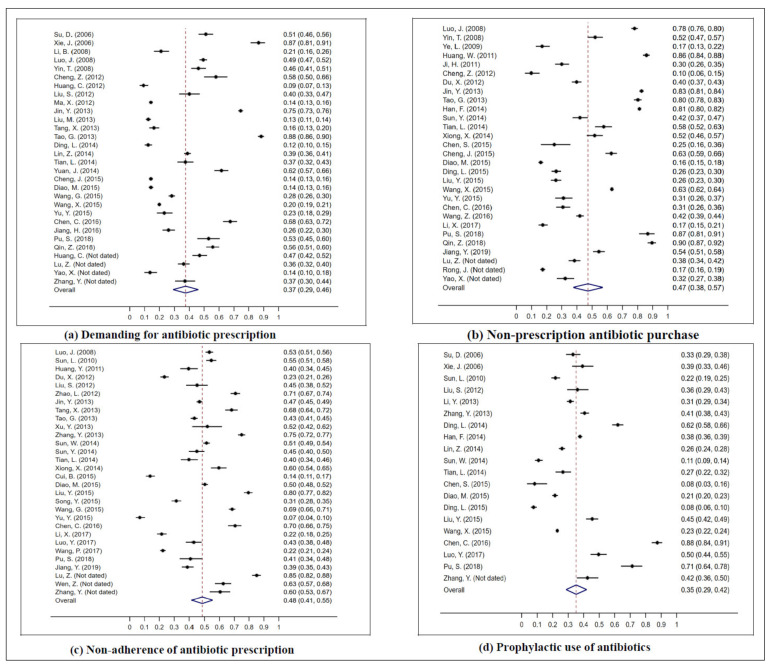
3.2. The Prevalence of Irrational Use Behaviors of the General Population
3.2.1. Demanding Antibiotic Prescription
The overall pooled estimate indicated over one third (37%, 95% CI: 29–46) of the general population have demanded antibiotic prescriptions from their physicians (Figure 3). Subgroup meta-analysis showed the pooled proportions were significantly different among studies from different regions (p < 0.001), different types of participants (p < 0.001), and different study sizes (p < 0.001). Studies from the western area of China reported the highest pooled proportions (65%, 95% CI: 50–78), followed by the eastern (34%, 95% CI: 26–43), and central areas (26%, 95% CI: 17–37). The highest proportion of behavior for demanding antibiotic prescriptions from physicians was observed in the customers of pharmacies (49%, 95% CI: 47–51), followed by urban residents (48%, 95% CI: 33–64), rural residents (28%, 95% CI: 13–45), students (23%, 95% CI: 13–34), and children’s parents (20%, 95% CI: 12–29) (Table 3).
Figure 3.
Meta-analysis of the pooled proportion of the general population’s irrational use behaviors regarding antibiotics. (a) Demanding for antibiotic prescription. (b) Non-prescription antibiotic purchase. (c) Non-adherence of antibiotic prescription. (d) Prophylactic use of antibiotics.
Table 3.
Subgroup analysis of the proportion of the general population’s irrational use behaviors regarding antibiotics (%, 95% CI).
| Subgroup | Demanding Antibiotic Prescription | Non-Prescription Antibiotic Purchasing | Non-Adherence to Antibiotic Prescription | Prophylactic Use of Antibiotics |
|---|---|---|---|---|
| Geographical region | ||||
| Eastern China | 34 (26–43) | 34 (25–44) | 49 (39–60) | 35 (25–46) |
| Central China | 26 (17–37) | 51 (36–65) | 45 (35–56) | 27 (18–37) |
| Western China | 65 (50–78) | 70 (51–86) | 47 (43–52) | 47 (43–51) |
| Study period | ||||
| <2010 | 51 (35–67) | 49 (15–83) | 53 (51–56) | 35 (31–39) |
| 2010–2015 | 37 (20–56) | 57 (43–70) | 51 (43–59)) | 32 (24–40) |
| ≥2015 | 32 (24–41) | 44 (31–58) | 40 (27–53) | 38 (24–53) |
| NA | 33 (20–47) | 29 (15–45) | 70 (51–86) | 42 (36–50) |
| Type of participant | ||||
| Rural residents | 28 (13–45) | 32 (15–52) | 67 (48–84) | 27 (16–39) |
| Urban residents | 48 (33–64) | 54 (32–76) | 45 (36–55) | 39 (26–54) |
| Students | 23 (13–34) | 49 (35–62) | 43 (27–61) | 34 (25–44) |
| Pharmacy’s customer | 49 (47–51) | 73 (71–75) | – | – |
| Children’s parents | 20 (12–29) | 17 (15–21) | 22 (18–25) | – |
| Urban and rural residents | – | 54 (51–58) | 39 (35–43) | – |
| Others | 38 (35–41) | 40 (7–80) | 61 (53–68) | 41 (12–74) |
| Quality score | ||||
| 4–6 | 38 (29–47) | 48 (37–58) | 47 (40–54) | 36 (29–43) |
| 7–9 | 35 (10–64) | 45 (18–75) | 63 (61–65) | 40 (3–44) |
| Study size | ||||
| <400 | 41 (28–55) | 40 (27–53) | 44 (34–55) | 38 (26–51) |
| 400–800 | 37 (24–51) | 42 (26–58) | 54 (31–76) | 40 (16–67) |
| 800–1200 | 88 (86–90) | 70 (41–93) | 51 (30–72) | 32 (30–34) |
| ≥1200 | 28 (16–42) | 54 (34–74) | 48 (37–58) | 28 (21–34) |
Substantial heterogeneity was observed among studies (χ2 = 7688.51, p < 0.001, I2 = 99.62%). The multivariable meta–regression yielded a significant multivariate model, explaining more than half of the heterogeneity (p = 0.0138, adjusted R2 = 55.45%, I2 = 93.70%), which indicated that study period (p = 0.016) and regions (p = 0.001–0.016) significantly influenced the pooled estimate of the general population’s behavior regarding demanding antibiotic prescriptions.
3.2.2. Non–Prescription Antibiotic Purchasing
The overall pooled estimate showed that 47% (95% CI: 38–57) of the general population have purchased antibiotics without prescriptions (Figure 3). A significant difference among the pooled proportions of studies from eastern, central, and western China was observed (p < 0.001), with estimates of 34% (95% CI: 25–444), 51% (95% CI: 36–65), and 70% (95% CI: 51–86), respectively. Different types of participants also showed significantly varied pooled proportions of non–prescription antibiotic purchasing behavior (p < 0.001), with the highest proportion observed in pharmacy customers (73%, 95% CI: 71–75), followed by urban residents (54%, 95% CI: 32–76), and students (49%, 95% CI: 35–62) (Table 3).
3.2.3. Non–Adherence to Antibiotic Prescription
The general population reported prevalent non–adherence to antibiotic prescriptions (Figure 3), the pooled proportion of this behavior was 48% (95% CI: 41–55). The subgroup meta–analysis showed that no significant difference was identified between studies from eastern (49%, 95% CI: 39–60), central (45%, 95% CI: 35–56), and western (47%, 95% CI: 43–52) China. A significant difference was found between different participants (p < 0.001), with the highest pooled proportion of this kind of behavior found in rural residents (67%, 95% CI: 48–84) while the lowest in children’s parents (22%, 95% CI: 18–25). In addition, different qualities of studies also reported different prevalence of non–adherence to antibiotic prescriptions of the public (p < 0.001), with high–quality studies reporting a pooled proportion of 63% (95% CI: 61–65) while moderate quality studies reported 50% (95% CI: 43–57) (Table 3).
3.2.4. Prophylactic Use of Antibiotics
The overall pooled estimate demonstrated that 35% (95% CI: 29–42) of the general population have prophylactically used antibiotics to prevent infections (Figure 3). The subgroup meta–analysis showed people from western China reported the highest pooled proportion (47%, 95% CI: 43–51), followed by those from eastern (35%, 95% CI: 25–46), and central China (27%, 95% CI: 18–37). In addition, urban residents reported the highest pooled proportion of prophylactic use of antibiotics, followed by students (34%, 95% CI: 25–44), and rural residents (27%, 95% CI: 16–39) (Table 3).
3.2.5. Sensitivity Analysis
The robustness of these pooled estimates was confirmed by sensitivity analysis. The previously obtained estimates were similar to the results from sensitivity analysis, with non–prescription antibiotic purchasing ranging from 45.86 to 48.64%, demanding antibiotic prescriptions from 36.48 to 39.30%, non–adherence to antibiotic prescriptions from 47.55 to 50.20%, and prophylactic use of antibiotics from 33.19 to 37.53%.
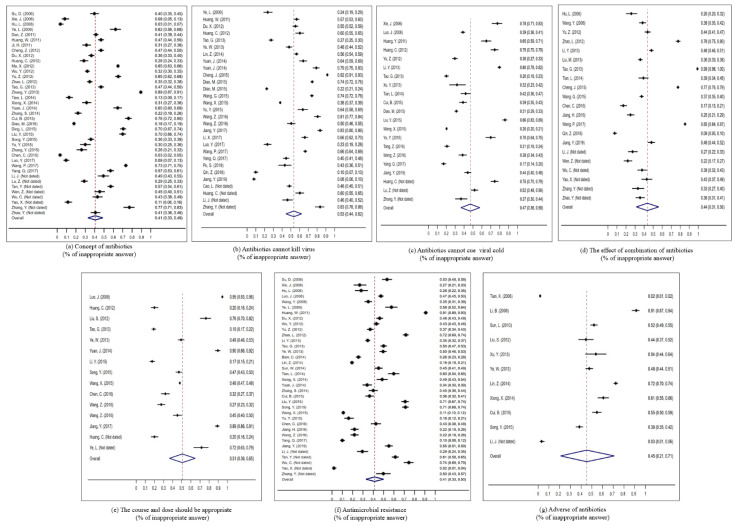
3.3. Prevalence of Potential Reasons of the General Population’s Irrational Use of Antibiotics
The proportion of people who showed different kinds of misconceptions of antibiotic use was extracted and their pooled proportions were synthesized, covering antibiotic recognition, correct indication, appropriate usage, and potential adverse outcomes.
The overall pooled proportion showed that nearly 41% (95% CI: 33–49) of the general population were unable to correctly recognize common antibiotics. People were also unable to correctly understand indications for antibiotic use, the pooled estimate of 53% (95% CI: 44–62) of participants believed that antibiotics can kill viruses and 47% (95% CI: 36–58) believed that most colds need antibiotics. People also commonly hold misconceptions about antibiotic usage, a pooled proportion of 44% (95% CI: 31–56) of the population thought that combined use of antibiotics was more effective than use of one antibiotic and 49% (95% CI: 35–64) believed that they should follow antibiotic prescriptions in dosing and duration. In terms of potential adverse outcomes of antibiotic use, the pooled estimates showed that 41% (95% CI: 33–50) of people did not understand that over and inappropriate use of antibiotics leads to antibiotic resistance and 45% (95% CI: 21–71) did not recognize that use of antibiotics may result in adverse reaction (Figure 4).
Figure 4.
Meta–analysis of the pooled proportion of the general population’s misconceptions regarding antibiotic use. (a) Concept of antibiotics (% of inappropriate answer). (b) Antibiotics cannot kill virus (% of inappropriate answer). (c) Antibiotics cannot cue viral cold (% of inappropriate answer). (d) The effect of combination of antibiotics (% of inappropriate answer). (e) The course and dose should be appropriate (% of inappropriate answer). (f) Antimicrobial resistance (% of inappropriate answer). (g) Adverse of antibiotics (% of inappropriate answer).
4. Discussion
4.1. Main Findings
The infections caused by antibiotic–resistance bacteria are increasingly difficult to treat and the consequences of AR, such as extra hospitalizations and deaths, are self–evident [5,6]. Based on data from 78 studies that included a total of 79,165 participants, this systematic review demonstrates that irrational use behaviors of antibiotics are common among the general population in China. On one hand, antibiotics are easily accessed by the general population. On the other hand, a considerable proportion of people cannot appropriately use antibiotics.
A huge variation of the public’s irrational use behaviors in different geographical regions was also identified based on subgroup analysis. People from western regions of China were more likely to show behaviors resulting in obtaining unnecessary antibiotics. Other than the fact that people reported less demanding of antibiotics from physicians over time, no significant declining trend was identified in people’s irrational use behaviors of antibiotics in the past decades.
The potential reasons for the prevalent over and irrational antibiotic use behaviors of the general population may lie on their misconception of antibiotics, which is also shown to be popular in the current study. It is estimated that roughly half of participants are unable to recognize common antibiotics, understand in what situation antibiotics are required, show sufficient knowledge of appropriate antibiotic usage, and understand adverse outcomes of antibiotics. These misunderstandings may lead to expectations of unnecessary antibiotics from the public and hinder people’s rational use of these medicines.
4.2. Strengths and Limitations
In the current study, a review framework was developed based on the WHO’s highlights of the general population’s irrational use behaviors of antibiotics. The definition of rational use of antibiotics was also referred to help identify potential reasons for the general population’s irrational use behaviors. Based on the review framework, a comprehensive search strategy was generated, covering four kinds of common inappropriate use behaviors and four aspects of misunderstanding of antibiotics among the general population in China. In addition, we carefully followed the guidelines of the systematic reviews of prevalence and incidence from JBI. Quality assessment was applied to ensure only studies with high and moderate quality were included. We also performed subgroup analysis and sensitivity analysis to ensure the robustness of the results.
There are also some limitations. First, the quality of the included studies may be underestimated due to the restrictions on the length of text in Chinese journals, causing details of methodology to possibly not be reported [114,115]. Second, only four main datasets were searched and we focused on synthesis of studies published in Chinese. Such strategy was adopted due to the aim of the current study and publication in English has been synthesized in existing reviews. However, the results of the current study seemed not to change even after inclusion of publications in English. Existing reviews synthesized English publications and narratively described prevalence of people’s irrational use behaviors of antibiotics, which is similar when compared with the results in the current study. Finally, there are limited studies on some indicators in the current study, such as the general population’s misconceptions of combination antibiotics use and adverse reaction. More studies are warranted to generate a more accurate and robust estimate.
4.3. Comparison with Existing Studies
The prevalence of irrational antibiotic use behaviors among the general population confirmed that they play a role in fueling overuse of antibiotics in China. The results of this study correspond with that from another study synthesizing data from publications in English [31], in which the proportion of people’s non–prescription purchasing behaviors ranged from 8.8 to 84.9% and demanding antibiotic prescriptions ranged from 1.8 to 74.5% in Mainland China. These figures are much higher than those from studies in the USA [20,116,117,118,119] and India [120], in which roughly one fifth of people had asked for antibiotics or obtained antibiotics without prescriptions. Considering only part of the expectation would translate to demanding behaviors, the desire for antibiotics is expected to be higher among the public [16].
It is worth noting that people were less likely to demand antibiotics from physicians over time in China, which was similar when compared with results from a survey in 14 countries that patient antibiotic expectation for respiratory tract infections decreased over time [26]. However, considering this trend was not identified in the public’s non–prescription purchasing behaviors, the decline is likely to be owed to the increasingly restricted regulations on healthcare providers. In past decades, a series of policies and national campaigns were introduced to improve healthcare’s rational use of antibiotics [121,122,123]. The recent national assessment showed that only 10.9% of outpatients end with antibiotic treatment and physicians over–prescribing antibiotics has dramatically decreased in the past 5 years in China [28]. Thus, people may adapt their behaviors and reduce their demanding behavior since it is less likely to result in an antibiotic prescription.
On the other hand, non–prescription purchasing from pharmacies is increasingly become an important outlet to fulfill peoples’ unnecessary demand for antibiotics [29]. This situation seemed stable based on the results from the current study. National simulated client studies showed that over 70% of patients with respiratory tract infections are able to easily obtain unnecessary antibiotics from either offline or online pharmacies in China [124,125]. In addition to high expectations of antibiotics from patients, loose regulation [30], economic incentives [126], fierce market competition, and a fragmentized healthcare system [30] also contributed to this situation. Though several policies have been introduced to enforce the regulation of irregular sales of non–prescription antibiotics after 2014 in China [124], the effect was limited and a comprehensive strategy is warranted [30].
In addition, the association between regional economic development and overuse of antibiotics has been established [127], which implies health inequalities across areas. In the current study, the variation between geographical areas of the public’s behaviors to obtain unnecessary antibiotics corresponds with the results from Scotland, in which the most deprived areas reported the highest antibiotic use. Two main aspects were highlighted contributing to high consumption of antibiotics within such kind of areas, namely, people’s susceptibility to infection [127] (due to poor living conditions, poor diet, etc.) and higher prevalence of misconceptions of antibiotics use [128].
In terms of rational use of antibiotics, the pooled proportion of people who do not follow antibiotic prescription is similar compared with the results in 2006 (44%) [129] and this figure is stable over decades and across regions. The prevalence of people’s non–adherence behavior is higher than results from Italy [130], France [131] and Portugal [132]. Previous studies have shown that adherence was associated with fewer concerns about treatment [133,134]. The traditional perspective to medicines among Chinese population, “as a medicine, it is more or less poisonous”, may contribute to the high proportion of medication non–adherence [135], which is also confirmed in patients with stroke, diabetes mellitus, and rheumatoid arthritis [134]. Prophylactic use of antibiotics is also prevalent among the general population in China, but it is not effective against common viral infections, such as the common cold and flu [29,136]. The results of our study are similar to previous reviews [31]. Studies have shown that preventative antibiotic use was associated with antibiotic storage at home. However, without a comprehensive surveillance system of outlets of antibiotics, antibiotics are commonly stored among families in China [29,137].
The general population’s misconception of antibiotic use is evident in China. In terms of knowledge of indication of antibiotic use, the results in the current study are similar compared with the estimates worldwide that around half of people are not able to correctly answer that antibiotics cannot cure colds and they should not be indicated for viral infection [138]. However, Chinese people seemed less knowledgeable of rational antibiotic usage [135] and are less aware that irrational antibiotic use can result in AR [138]. Though education of the general population is one core measure in China’s national action plan to contain bacterial resistance [139], limited information was available whether this campaign is effective.
4.4. Implications
To reduce irrational use of antibiotics, several national campaigns targeted at the public have been implemented worldwide. These interventions focused on educating people on the rational use of antibiotics via printed materials or mass media [140] and were deemed to help reduce antibiotic use in outpatients [140,141]. It has also been shown that multifaceted intervention, both involving physicians and patients, is more effective. To address the prevalent over and irrational use of antibiotics among the public in China, a comprehensive strategy is warranted and several implications may be drawn based on the current study.
First, a more comprehensive surveillance and tracking system of antibiotic prescriptions may be developed. The existing national surveillance system of antibiotic use in China concentrates on public hospitals. Information regarding primary healthcare and other facilities (village clinics, private clinics, etc.) are limited, despite irrational antibiotic being estimated to be more serious in these places. This system also needs to be further linked with pharmacy dispensing data, tracking the end of antibiotic prescriptions, to help irregular sales of antibiotics in both online and offline pharmacies. Through its effect on the general population’s behaviors, this kind of system has been initiated in Jinan, Shandong Province [142]. In addition to surveillance and tracking systems, implementation of a restriction policy of non–prescription sales of antibiotics is also significant. China has announced its national action plan to contain antimicrobial resistance in 2016 and aimed to achieve the goal that antibiotics will only be sold with a prescription in all pharmacies. However, limited supporting measures were identified to help achieve this goal despite non–prescription purchasing still being prevalent [139,143].
In addition, continuous training on antibiotic use and communication skills of physicians is required, especially for those in primary care, private clinics, and prescribing on the internet [30]. Such training programs have been proven to significantly reduce irrational use of antibiotics in children with upper respiratory tract infections in Guangxi Province. Physicians being accountable for prescriptions of antibiotics would reduce the public’s unnecessary access to antibiotics [30] and would further reduce their demand for antibiotics when they experienced similar symptoms the next time [144,145].
Finally, given the effectiveness of several national campaigns worldwide that significantly improve the general population’s awareness of rational antibiotic use [146,147], such interventions may also be introduced in China, particularly in remote regions with poor medical care.
5. Conclusions
Irrational use behaviors and misconceptions relevant to antibiotics among the general population is evident in China. People can easily obtain unnecessary antibiotics by demanding them from physicians or purchasing from pharmacies without prescriptions. They also showed popular behaviors of non–adherence to prescription or preventative use for non–indicated diseases, for example, the cold. Roughly half of people are unable to recognize common antibiotics, know the correct indication, understand rational usage, and realize the potential adverse outcomes. To address this issue, a comprehensive strategy is required, including construction of a systematic surveillance and tracking system of antibiotic prescriptions, a training program for physicians of rational use of antibiotics and communication skills, and a national campaign on the general population to improve their awareness.
Acknowledgments
We are thankful for all the support from our colleagues during the process.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/antibiotics10050497/s1, Table S1. Search Strategy.
Appendix A. JBI Critical Appraisal Checklist for Studies Reporting Prevalence Data
Reviewer ________________________ Date _____________
Author ____________________________ Year ____________ Record Number ______________________
| Heading | Yes | No | Unclear | Not Applicable |
| 1. Was the sample frame appropriate to address the target population? | ? | ? | ? | ? |
| 2. Were study participants sampled in an appropriate way? | ? | ? | ? | ? |
| 3. Was the sample size adequate? | ? | ? | ? | ? |
| 4. Were the study subjects and the setting described in detail? | ? | ? | ? | ? |
| 5. Was the data analysis conducted with sufficient coverage of the identified sample? | ? | ? | ? | ? |
| 6. Were valid methods used for the identification of the condition? | ? | ? | ? | ? |
| 7. Was the condition measured in a standard, reliable way for all participants? | ? | ? | ? | ? |
| 8. Was there appropriate statistical analysis? | ? | ? | ? | ? |
| 9. Was the response rate adequate, and if not, was the low response rate managed appropriately? | ? | ? | ? | ? |
Overall appraisal: Include: ? Exclude: ? Seek further info: ?
Comments (Including reason for exclusion)
Was the sample frame appropriate to address the target population? The sampling frame should match with the purpose of the study, and can obtain the target population of the study;
Were study participants sampled in an appropriate way? It is necessary to describe in detail what sampling method was used and how to gradually obtain our target population. For cluster and stratified sampling, you should describe the characteristics according to which participants are stratified and grouped. Non–probability sampling is not considered an appropriate survey research method;
Was the sample size adequate? In addition to a comprehensive census, a detailed and reasonable sample size calculation process is required for sample surveys;
Were the study subjects and the setting described in detail? The characteristics of the participants need to be described in detail, and demographic information, research time and research location need to be included at the same time;
Was the data analysis conducted with sufficient coverage of the identified sample? It is necessary to describe whether the samples can adequately cover the structure of each subgroup;
Were valid methods used for the identification of the condition? While using a self–made questionnaire as measurement tool, the reliability and validity test results of the questionnaire need to be provided; if a certain established standard or definition is applied in the research, its standard and source should be introduced in detail;
Was the condition measured in a standard, reliable way for all participants? Introduce whether the questionnaire surveyor has been uniformly trained, and introduce the content of the uniform training, or describe in detail the distribution and quality control process of the questionnaire in the data collection process;
Was there appropriate statistical analysis? The rate index should give the numerator, denominator, and rate with confidence interval;
Was the response rate adequate, and if not, was the low response rate managed appropriately? The response rate of the research needs to be given. Generally, the response rate is >70%. If the response rate is less than 70%, the response rate is too low. The research needs to provide solutions for the response rate.
Appendix B. Data Extraction Form for Prevalence Studies
Table A1.
Data extraction form for prevalence studies.
| Citation Details | ||||||
|---|---|---|---|---|---|---|
| Author | Title | Journal | Year | Issue | Volume | Pages |
| Generic Study Details | ||||||
| Study Design | Country | Setting/Context | Year/Timeframe for Data Collection | Participants Characteristic (Study Inclusion/Exclusion Information) | Condition and Measurement | Description of Main Result (n/N) |
Author Contributions
Conceptualization, C.L.; methodology, C.L., D.W., and L.D.; validation, C.L., L.D., and D.W.; formal analysis, L.D.; data curation, L.D.; writing—original draft preparation, L.D.; writing—review and editing, C.L.; visualization, L.D.; supervision, L.D.; funding acquisition, C.L. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the National Natural Science Foundation of China (grant no. 71,904,053). The funding body played no part in the study design, collection, analysis and interpretation of data, writing of the manuscript, or the decision to submit the manuscript for publication.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found through the search strategy.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Global Action Plan on Antimicrobial Resistance. World Health Organization; Geneva, Switzerland: 2016. [Google Scholar]
- 2.Watkins R.R., Bonomo R.A. Overview: Global and Local Impact of Antibiotic Resistance. Infect. Dis. Clin. N. Am. 2016;30:313–322. doi: 10.1016/j.idc.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . Antimicrobial Resistance Global Report on Surveillance: 2014 Summary. World Health Organization; Geneva, Switzerland: 2014. [Google Scholar]
- 4.O’neill J. Review on Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. HM Government; London, UK: 2016. [Google Scholar]
- 5.Zhen X., Lundborg C.S., Sun X., Hu X., Dong H. The Clinical and Economic Impact of Antibiotic Resistance in China: A Systematic Review and Meta–Analysis. Antibiotics. 2019;8:115. doi: 10.3390/antibiotics8030115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhen X., Stålsby Lundborg C., Sun X., Zhu N., Gu S., Dong H. Economic burden of antibiotic resistance in China: A national level estimate for inpatients. Antimicrob. Resist. Infect. Control. 2021;10:5. doi: 10.1186/s13756-020-00872-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Role of Antimicrobial Use in the Epidemiology of Resistant Pneumococci: A 10–Year Follow Up. Microb. Drug Resist. 2006;12:169–176. doi: 10.1089/mdr.2006.12.169. [DOI] [PubMed] [Google Scholar]
- 8.Bronzwaer S.L., Cars O., Buchholz U., Mölstad S., Goettsch W., Veldhuijzen I.K., Kool J.L., Sprenger M.J., Degener J.E. A European study on the relationship between antimicrobial use and antimicrobial resistance. Emerg. Infect. Dis. 2002;8:278–282. doi: 10.3201/eid0803.010192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goossens H., Ferech M., Vander Stichele R., Elseviers M. Outpatient antibiotic use in Europe and association with resistance: A cross–national database study. Lancet. 2005;365:579–587. doi: 10.1016/S0140-6736(05)17907-0. [DOI] [PubMed] [Google Scholar]
- 10.Hu Y., Wang X., Tucker J.D., Little P., Moore M., Fukuda K., Zhou X. Knowledge, Attitude, and Practice with Respect to Antibiotic Use among Chinese Medical Students: A Multicentre Cross–Sectional Study. Int. J. Environ. Res. Public Health. 2018;15:1165. doi: 10.3390/ijerph15061165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang X., Lin L., Xuan Z., Li L., Zhou X. Keeping Antibiotics at Home Promotes Self–Medication with Antibiotics among Chinese University Students. Int. J. Environ. Res. Public Health. 2018;15:687. doi: 10.3390/ijerph15040687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aljayyousi G.F., Abdel–Rahman M.E., El–Heneidy A., Kurdi R., Faisal E. Public practices on antibiotic use: A cross–sectional study among Qatar University students and their family members. PLoS ONE. 2019;14:e0225499. doi: 10.1371/journal.pone.0225499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grigoryan L., Burgerhof J.G., Haaijer–Ruskamp F.M., Degener J.E., Deschepper R., Monnet D.L., Di Matteo A., Scicluna E.A., Bara A.C., Lundborg C.S., et al. Is self–medication with antibiotics in Europe driven by prescribed use? J. Antimicrob. Chemother. 2007;59:152–156. doi: 10.1093/jac/dkl457. [DOI] [PubMed] [Google Scholar]
- 14.Lv B., Zhou Z., Xu G., Yang D., Wu L., Shen Q., Jiang M., Wang X., Zhao G., Yang S., et al. Knowledge, attitudes and practices concerning self–medication with antibiotics among university students in western China. Trop. Med. Int. Health Tm Ih. 2014;19:769–779. doi: 10.1111/tmi.12322. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization Antibiotic Resistance. [(accessed on 23 February 2021)]; Available online: https://www.who.int/news–room/fact–sheets/detail/antibiotic–resistance.
- 16.Macfarlane J., Holmes W., Macfarlane R., Britten N. Influence of patients’ expectations on antibiotic management of acute lower respiratory tract illness in general practice: Questionnaire study. BMJ. 1997;315:1211–1214. doi: 10.1136/bmj.315.7117.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scott J.G., Cohen D., DiCicco–Bloom B., Orzano A.J., Jaen C.R., Crabtree B.F. Antibiotic use in acute respiratory infections and the ways patients pressure physicians for a prescription. J. Fam. Pract. 2001;50:853–858. [PubMed] [Google Scholar]
- 18.Liu C., Liu C., Wang D., Deng Z., Tang Y., Zhang X. Determinants of antibiotic prescribing behaviors of primary care physicians in Hubei of China: A structural equation model based on the theory of planned behavior. Antimicrob. Resist. Infect. Control. 2019;8:23. doi: 10.1186/s13756-019-0478-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mangione–Smith R., McGlynn E.A., Elliott M.N., Krogstad P., Brook R.H. The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatrics. 1999;103:711–718. doi: 10.1542/peds.103.4.711. [DOI] [PubMed] [Google Scholar]
- 20.Francois Watkins L.K., Sanchez G.V., Albert A.P., Roberts R.M., Hicks L.A. Knowledge and Attitudes Regarding Antibiotic Use Among Adult Consumers, Adult Hispanic Consumers, and Health Care Providers—United States, 2012–2013. Morb. Mortal. Wkly. Rep. 2015;64:767–770. doi: 10.15585/mmwr.mm6428a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dyar O.J., Zhang T., Peng Y., Sun M., Sun C., Yin J., Ding L., Sun C., Wang Y., Sun Q., et al. Knowledge, attitudes and practices relating to antibiotic use and antibiotic resistance among backyard pig farmers in rural Shandong province, China. Prev. Vet. Med. 2020;175:104858. doi: 10.1016/j.prevetmed.2019.104858. [DOI] [PubMed] [Google Scholar]
- 22.Wang J., Sheng Y., Ni J., Zhu J., Zhou Z., Liu T., Zhang X., Zhao Q. Shanghai Parents’ Perception And Attitude Towards The Use Of Antibiotics On Children: A Cross–Sectional Study. Infect. Drug Resist. 2019;12:3259–3267. doi: 10.2147/IDR.S219287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang Z., Hu Y., Zou G., Lin M., Zeng J., Deng S., Zachariah R., Walley J., Tucker J.D., Wei X. Antibiotic prescribing for upper respiratory infections among children in rural China: A cross–sectional study of outpatient prescriptions. Glob. Health Action. 2017;10:1287334. doi: 10.1080/16549716.2017.1287334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nepal G., Bhatta S. Self–medication with Antibiotics in WHO Southeast Asian Region: A Systematic Review. Cureus. 2018;10:e2428. doi: 10.7759/cureus.2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Auta A., Hadi M.A., Oga E., Adewuyi E.O., Abdu–Aguye S.N., Adeloye D., Strickland–Hodge B., Morgan D.J. Global access to antibiotics without prescription in community pharmacies: A systematic review and meta–analysis. J. Infect. 2019;78:8–18. doi: 10.1016/j.jinf.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 26.Kianmehr H., Sabounchi N.S., Seyedzadeh Sabounchi S., Cosler L.E. Patient expectation trends on receiving antibiotic prescriptions for respiratory tract infections: A systematic review and meta–regression analysis. Int. J. Clin. Pract. 2019;73:e13360. doi: 10.1111/ijcp.13360. [DOI] [PubMed] [Google Scholar]
- 27.McNulty C.A., Nichols T., French D.P., Joshi P., Butler C.C. Expectations for consultations and antibiotics for respiratory tract infection in primary care: The RTI clinical iceberg. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 2013;63:e429–e436. doi: 10.3399/bjgp13X669149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhao H., Wei L., Li H., Zhang M., Cao B., Bian J., Zhan S. Appropriateness of antibiotic prescriptions in ambulatory care in China: A nationwide descriptive database study. Lancet Infect. Dis. 2021 doi: 10.1016/S1473-3099(20)30596-X. [DOI] [PubMed] [Google Scholar]
- 29.Wang X., Peng D., Wang W., Xu Y., Zhou X., Hesketh T. Massive misuse of antibiotics by university students in all regions of China: Implications for national policy. Int. J. Antimicrob. Agents. 2017;50:441–446. doi: 10.1016/j.ijantimicag.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 30.Wang X., Xuan Z., Storella T.H., Zhou X. Determinants of non–prescription antibiotic dispensing in Chinese community pharmacies from socio–ecological and health system perspectives. Soc. Sci. Med. 2020;256:113035. doi: 10.1016/j.socscimed.2020.113035. [DOI] [PubMed] [Google Scholar]
- 31.Lin L., Sun R., Yao T., Zhou X., Harbarth S. Factors influencing inappropriate use of antibiotics in outpatient and community settings in China: A mixed–methods systematic review. BMJ Glob. Health. 2020:5. doi: 10.1136/bmjgh-2020-003599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Systematic reviews of prevalence and incidence. Joanna Briggs Inst. Rev. Man. 2017;5:177–217. [Google Scholar]
- 33.Xu Y., Lu J., Sun C., Wang X., Hu Y.J., Zhou X. A cross–sectional study of antibiotic misuse among Chinese children in developed and less developed provinces. J. Infect. Dev. Ctries. 2020;14:129–137. doi: 10.3855/jidc.11938. [DOI] [PubMed] [Google Scholar]
- 34.Monnier A.A., Eisenstein B.I., Hulscher M.E., Gyssens I.C. Towards a global definition of responsible antibiotic use: Results of an international multidisciplinary consensus procedure. J. Antimicrob. Chemother. 2018;73:vi3–vi16. doi: 10.1093/jac/dky114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int. J. Evid. Based Healthc. 2015;13:147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 36.Behzadifar M., Heydarvand S., Behzadifar M., Bragazzi N.L. Prevalence of Hepatitis C Virus in Tuberculosis Patients: A Systematic Review and Meta–Analysis. Ethiop. J. Health Sci. 2019;29:945–956. doi: 10.4314/ejhs.v29i1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tian X., Tang X., Li J. Cognition status about side effect antibiotics among staff members and students in one college. Chin. Sch. Health. 2010;31:216–217. doi: 10.16835/j.cnki.1000-9817.2010.02.043. (In Chinese) [DOI] [Google Scholar]
- 38.Su D., Zhang X., Wang L. Evaluation of the pilot effect of health education on the control of antibiotic abuse in rural communities in Zhejiang. Chin. Rural Health Serv. Manag. 2010;30:296–298. (In Chinese) [Google Scholar]
- 39.Xie J., Yang T., He Y. Evaluation on the effectiveness of antimicrobial abuse publicity interventions among residents in Xiacheng District, Hangzhou. Zhejiang Prev. Med. 2009:3. doi: 10.19485/j.cnki.issn1007-0931.2009.03.040. (In Chinese) [DOI] [Google Scholar]
- 40.Luo J. Master’s Thesis. Central South University; Changsha, China: 2009. Study on self–medication behaviors and influencing factors of antimicrobial drugs among pharmacies customers. (In Chinese) [Google Scholar]
- 41.Yin T. Ph.D. Thesis. Central South University; Changsha, China: 2010. Social epidemiological study on the use of antibiotics among community residents in Changsha. (In Chinese) [Google Scholar]
- 42.Hu L. Study on anitbiotic use in urban population in Ningbo city. China Health Educ. 2010;26:127–128. doi: 10.16168/j.cnki.issn.1002-9982.2010.02.022. (In Chinese) [DOI] [Google Scholar]
- 43.Wang Y., Zou D. Analysis of cognitive behaviors of community residents toward the antimicrobial use. J. Pharmacoepidemiol. 2010;19:498–500. (In Chinese) [Google Scholar]
- 44.Li B., Wen Q., Deng L., Chen Z. Investigation and analysis of antibiotic–related knowledge of parents of children with children in the pediatric infusion room. J. Yangtze Univ. (Self Sci. Ed.) Med. Vol. 2009;6:323–325. doi: 10.3969/j.issn.1673-1409(R).2009.04.154. (In Chinese) [DOI] [Google Scholar]
- 45.Ye L., Hu Z. A survey of the cognition and use of antibiotics in patients in the Department of Infectious Diseases. Chin. J. Mod. Nurs. 2010;33:4028–4029. (In Chinese) [Google Scholar]
- 46.Sun L., Peng L., Cai F. Cognition of antibiotic and its intervention among staff and students in a vocational college. Chin. Sch. Dr. 2011;25:576–577. (In Chinese) [Google Scholar]
- 47.Huang W., Liao J., He J. A survey of Lanzhou uppperrespiratory tract infectious patients’ knoledge on antibiotics and its usage out hospital. Gansu Med. 2013;32:9–12. doi: 10.15975/j.cnki.gsyy.2013.01.023. (In Chinese) [DOI] [Google Scholar]
- 48.Huang Y., Zhang H., Qian K. Investigation on the awareness and use of antibiotics among community residents. Community Med. J. 2013;11:52–54. (In Chinese) [Google Scholar]
- 49.Ji H., Li D., Li P. Suevey on drug use related knowledge and behaviors among Xianyang City of Shaanxi Province in 2011. China Health Educ. 2014;30:694–697. doi: 10.16168/j.cnki.issn.1002-9982.2014.08.009. (In Chinese) [DOI] [Google Scholar]
- 50.Shan H., Fan M., Mao F. Investigation on the status quo of antibacterial drug use in outpatients. Pharm. Clin. Res. 2013;21:90–93. doi: 10.13664/j.cnki.pcr.2013.01.024. (In Chinese) [DOI] [Google Scholar]
- 51.Huang C., Jin Y. Survey of the knowledge and behavior for rational use of antibiotics in Huating Town, Jiading district, Shanhai. Shanghai Med. 2013;4:33–35. (In Chinese) [Google Scholar]
- 52.Cheng S., Shi L., Luo X. Investigation and analysis of rational use of antibiotics in the community residents of Beijing. China Pharm. 2013;24:3758–3760. doi: 10.6039/j.issn.1001-0408.2013.40.05. (In Chinese) [DOI] [Google Scholar]
- 53.Zhao L., Sun Q., Li C. Antibiotcs in rural Shandong province: User cognition and behavior. China Health Policy Res. 2013;6:43–47. doi: 10.3969/j.issn.1674-2982.2013.08.008. (In Chinese) [DOI] [Google Scholar]
- 54.Wu Y., Nan H., Tie Y. Analysis on rational use of drugs situation among urban and rural residents in Shaanxi Province. China Health Educ. 2015;31:289–292. doi: 10.16168/j.cnki.issn.1002-9982.2015.03.014. (In Chinese) [DOI] [Google Scholar]
- 55.Ma X., Yin W., Wei Y. Investigation and analysis of current situation of the cognition of residents and use of antibacterials in Shandong Province under National Essential Drug System. China Pharm. 2014;25:1066–1069. doi: 10.6039/j.issn.1001-0408.2014.12.04. (In Chinese) [DOI] [Google Scholar]
- 56.Yu M. Master’s Thesis. Fudan University; Shanghai, China: 2013. Utilization of Antibiotics and the Influencing Factors in Rural Areas of Jiangxi Province. (In Chinese) [Google Scholar]
- 57.Liu S., Gu W., Shen Q. The survey of the resident’s knowledge attitudes and practice for antimicrobial medicaiton in Minhang District of Shanghai. Community Med. J. 2016;14:7–10. (In Chinese) [Google Scholar]
- 58.Du X., Sun Y., Kang M. A survey of College Students’ awareness of antibacterial drugs. Chin. Prim. Med. 2014;21:650–652. (In Chinese) [Google Scholar]
- 59.Tao G. Investigation and analysis of effect of health education intervention on the knowledge–belief–behavior level of the rational use of antibiotics by community residents. China Pharm. 2015;26:3751–3754. doi: 10.6039/j.issn.1001-0408.2015.27.03. (In Chinese) [DOI] [Google Scholar]
- 60.Li Y. Investigation on cognition and judgment of present applicantion situation antibiotics in the medical students. J. Qiqihar Med. Coll. 2016;37:3944–3946. (In Chinese) [Google Scholar]
- 61.Jin Y., Lu Y., Lu P. Influence of demographic characteristics on antibiotics use among middle aged and elderly people. Chin. Public Health. 2014;30:1140–1143. doi: 10.11847/zgggws2014-30-09-10. (In Chinese) [DOI] [Google Scholar]
- 62.Ye W., Xuan R., Ye P. An empirical study on the assessment and influencing factors of the status quo of cognition and medication behavior of antibacterial drugs among residents in Dongguan. China Pract. Med. 2014;9:195–196. doi: 10.14163/j.cnki.11-5547/r.2014.09.004. (In Chinese) [DOI] [Google Scholar]
- 63.Tang X., Zhang Y. Investigation on the knowledge, belief and practice of the rational use of antibacterial drugs in outpatients. Jiangsu Prev. Med. 2015;26:122–123. doi: 10.13668/j.issn.1006-9070.2015.01.054. (In Chinese) [DOI] [Google Scholar]
- 64.Zhang Y., Pan Q. A survey on the cognition of antibacterial drugs among college students. Chin. J. Drug Abus. Prev. Treat. 2014;20:215–216. doi: 10.3969/j.issn.1006-902X.2014.04.010. (In Chinese) [DOI] [Google Scholar]
- 65.Xu Y., Lu S., Zou X. Investigation and analysis of the cognition and use of antibacterial drugs among residents in a certain community in Shanghai. Community Med. J. 2013;111:80–82. (In Chinese) [Google Scholar]
- 66.Liu M., Zhang X., Gao X. Investigation and analysis of 1046 children’s parents on antibacterial drugs–related cognition and behavior. China Healthc. Nutr. 2016;26:7–8. doi: 10.3969/j.issn.1004-7484.2016.23.006. (In Chinese) [DOI] [Google Scholar]
- 67.Sun W. Master’s Thesis. Shandong University; Jinan, China: 2015. The impact evaluation of health promotion on improving rational use of antibiotics among rural children caregiver. (In Chinese) [Google Scholar]
- 68.Ding L., Sun W., Li Y. Knowledge, attitude and practice about antibiotic use among caregivers of rural preschool children. Chin. Public Health. 2015;31:1109–1112. doi: 10.11847/zgggws2015-31-09-01. (In Chinese) [DOI] [Google Scholar]
- 69.Tian L., Peng L. Evaluation on the intervention effect of antibiotics in Dongli District of Tianjin. China Urban Rural Enterp. Health. 2017;32:13–15. doi: 10.16286/j.1003-5052.2017.04.005. (In Chinese) [DOI] [Google Scholar]
- 70.Han F. Master’s Thesis. Anhui Medical University; Hefei, China: 2015. Survey on the Present Knowledge and Use of Antibiotic of Suzhou Secondary Vocaitonal Students. (In Chinese) [Google Scholar]
- 71.Yuan J. Master’s Thesis. Kunming Medical University; Kunming, China: 2016. Knowledge, Attitude and Practice towards Antibiotcs Usage—A Cross Sectional Survey Amnog the Genernal Public in Luquan County, Yunnan Province. (In Chinese) [Google Scholar]
- 72.Bian C., Wang H., Wu J. Analysis of influencing factors on the awareness of antimicrobial resistance and preference in outpatients among second–tier hospitals in Anhui Province. Chin. J. Dis. Control. 2015;19:847–848. doi: 10.16462/j.cnki.zhjbkz.2015.08.023. (In Chinese) [DOI] [Google Scholar]
- 73.Zhang S., Shao C., Wu H. Investigation and analysis on the cognition and safe use of antibiotics among residents in Henan Province. Sci. Technol. Econ. Trib. 2015;16:125–126. (In Chinese) [Google Scholar]
- 74.Xiong X., Xiao X., Fan Y. Investigation of congnition and utilization situation of antibiotics among residents inWeifang. Community Med. J. 2015;13:1–4. (In Chinese) [Google Scholar]
- 75.Lin W., Jin H., Wu L. Cognition and attitude of community residents on anitbiotics and its usage status. Chin. Gen. Pract. 2015;18:3491–3495. doi: 10.3969/j.issn.1007-9572.2015.28.026. (In Chinese) [DOI] [Google Scholar]
- 76.Sun Y., Zhu X., Fang C. The cognition of college students on oral antibiotics. Front. Med. 2015;5:31–32. (In Chinese) [Google Scholar]
- 77.Liu Y. Master’s Thesis. Shandong University; Jinan, China: 2018. The research on the evauation about effect of intervention to promote the irrationla use of antibiotics of rural residents inShandong province. (In Chinese) [Google Scholar]
- 78.Diao M. Analysis of Antibacterial Drug Use by Rural Residents in Anhui Province. J. Nanjing Med Univ. (Soc. Sci. Ed.) 2017;17:462–466. doi: 10.7655/NYDXBSS20170606. (In Chinese) [DOI] [Google Scholar]
- 79.Chen S., Zhao G., Xia B. Investigation for the knowledge of drug use among and medication habits of teachers in a senior high school in Beijing. China Pharm. 2016;27:4187–4190. doi: 10.6039/j.issn.1001-0408.2016.30.04. (In Chinese) [DOI] [Google Scholar]
- 80.Wang X. Ph.D. Thesis. Zhejiang University; Hangzhou, China: 2018. Antibiotic related knowledge and behaviors:A cross–sectional study and Ron campaign among Chinese university students. (In Chinese) [Google Scholar]
- 81.Cheng J. Ph.D. Thesis. Anhui Medical University; Hefei, China: 2017. Antibiotics Use in Rural Areas and Piloting Intervention for Rational antibiotics use based on Plannede Behavior Theory. (In Chinese) [Google Scholar]
- 82.Zhang Y., Lin S., Li G. Congnition and usage of antibiotics in caregivers of 0–6 years old children in rural area of Weinan, 2015. Pract. Prev. Med. 2017;24:196–198. doi: 10.3969/j.issn.1006-3110.2017.02.019. (In Chinese) [DOI] [Google Scholar]
- 83.Song Y. Analysis of unreasonable use of antibacterial drugs for college students and countermeasures. J. Clin. Ration. Use Drugs. 2016;9:86–87. doi: 10.15887/j.cnki.13-1389/r.2016.17.055. [DOI] [Google Scholar]
- 84.Cui B. Investigation on congnition status of antibacterial agents among freshmen in a university. Chin. Sch. Dr. 2018;32:561–563. (In Chinese) [Google Scholar]
- 85.Ding L. Master’s Thesis. Shandong University; Jinan, China: 2016. A Study on Rural Residents’ baseline knowledge, attitudes, and practice of antibiotics–a case from a county in Shandong province. (In Chinese) [Google Scholar]
- 86.Wang G., Gao H., Yan J. Knowledge and behavior about antibiotics use in adult community residents in Tianjin between 20 and 69 years old. Chin. Public Health. 2017;33:407–411. doi: 10.11847/zgggws2017-33-03-17. (In Chinese) [DOI] [Google Scholar]
- 87.Yu Y., Zhao Y., Wang X. Cognition status quo of residents toward antibiotics in community in Tianjin city and analysis of its influencing factors. [(accessed on 22 April 2021)];Nurs. Res. 2016 30:3403–3406. doi: 10.3969/j.issn.1009-6493.2016.27.02. Available online: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2016&filename=SXHZ201627029&v=ufUEvZiz8f1%25mmd2BvxdnLEbH2R3UhcGlK7SWaFUfv02NvQsQ8tm5lZ5u2wcbZS%25mmd2FvpOSt. (In Chinese) [DOI] [Google Scholar]
- 88.Lei Z., Xu Y., Guo Q. An investigation of antibacterial medicine use in the communities of Changsha. Guangdong Chem. Ind. 2016;43:20–21. (In Chinese) [Google Scholar]
- 89.Chen C., Wang G., Gao H. Knowledge and behaviors of antibiotic and its influencing factors among civil servants in Tianjin (In Chinese) Occup. Health. 2018;34:622–626. doi: 10.13329/j.cnki.zyyjk.2018.0173. [DOI] [Google Scholar]
- 90.Tang Z., Tang J., Su Q. Investigation and Analysis on Cognition Degree of the Children Patients’ Parents on Common Cold and Its Medication Safety. China Pharm. 2018;27:78–81. doi: 10.3969/j.issn.1006-4931.2018.01.026. (In Chinese) [DOI] [Google Scholar]
- 91.Wang Z., Li Y., Huang X. Relationship between cognition on and attitudes towards antibiotic use among citizens in Hangzhou city. Chin. Public Health. 2018;34:882–886. doi: 10.11847/zgggws1114670. (In Chinese) [DOI] [Google Scholar]
- 92.Jiang H., Jin Y., Ye J. An analysis on knowledge, attitude and practice regarding antibiotics use among community residents in Hangzhou. Prev. Med. 2017;29:978–982. doi: 10.19485/j.cnki.issn1007-0931.2017.10.002. (In Chinese) [DOI] [Google Scholar]
- 93.Wang Q., Wang X., Kang C. Investigation on Use of Antibacterial Drugs among College Students in the City of Chengdu. Chin. Pharmacovigil. 2017;14:493–497. (In Chinese) [Google Scholar]
- 94.Jiang Y., Zhang F., Yan H. Congnition of antibiotics and its influence factors among residens in Xuzhou after the implementation of antimicrobial agents use. Prev. Med. Forum. 2018;24:483–486. doi: 10.16406/j.pmt.issn.1672-9153.2018.07.003. (In Chinese) [DOI] [Google Scholar]
- 95.Luo Y., Li H., Deng R. Antibiotic use knowledge, attitude and behavior of nursing students with different academic levels. Guangxi Med. 2019;41:141–145. doi: 10.11675/j.issn.0253-4304.2019.01.38. (In Chinese) [DOI] [Google Scholar]
- 96.Yang Q. Master’s Thesis. Zhejiang University; Hangzhou, China: 2018. A Study on the Rational Use of Antibiotics and Its Influential Factors in Children’s Parents in Xiacheng District. (In Chinese) [Google Scholar]
- 97.Wang P., Li Y., Bai J. Cognition, use and education demand of antibiotics among college students in 5 universities in China. Pract. Prev. Med. 2020;27:919–922. doi: 10.3969/j.issn.1006-3110.2020.08.007. (In Chinese) [DOI] [Google Scholar]
- 98.Li X., Wang Y., Song Y. Analysis of knowledge, belief and behavior regarding rational antibiotic use of some students in Dongcheng district, Beijing. China Health Educ. 2020;36:723–728. doi: 10.16168/kcnki.issn.1002-9982.2020.08.010. (In Chinese) [DOI] [Google Scholar]
- 99.Piao S. Investigation and analysis on the cognition and use of antibiotics among residents in a community in Dalian. China New Commun. 2019;21:221–222. (In Chinese) [Google Scholar]
- 100.Qin Z., Li H., Tian F. Investigation and analysis of drug behavior risk KAP of residents in Sichuan Province. J. Clin. Drug Ther. 2019;17:73–77. doi: 10.3969/j.issn.1672-3384.2019.04.017. (In Chinese) [DOI] [Google Scholar]
- 101.Jiang Y., Yang Y., Cheng J. Investigation of Cognition and Self–medication Behavior of Antibiotics among Urban and Rural Residents in Lu’an City. China Pharm. 2021;32:98–103. doi: 10.6039/j.issn.1001-0408.2021.01.18. (In Chinese) [DOI] [Google Scholar]
- 102.Cao L., Yuan Y., Sun Y. The effect of parental knowledge survey on preventing antibiotic abuse—An investigation on antibiotic knowledge of 1080 children’s parents. Chin. Med. J. 2004;2:35–37. (In Chinese) [Google Scholar]
- 103.Tan Y., Tang H., Zhang X. A survey on the cognition and use of antibiotics by residents in villages and towns in northeastern Sichuan. Beifang Pharm. 2014;11:126–127. (In Chinese) [Google Scholar]
- 104.Ye L. Evaluation of Health Education Effect on Undergraduates’ Antibiotic Application Cognition and Behavior. Chin. Sch. Health. 2004;2:196. (In Chinese) [Google Scholar]
- 105.Yao X., Liu S. Investigation on the cognition, usage habits and application attitude of antibacterial drugs among college students. Health Vocat. Educ. 2018;36:123–125. (In Chinese) [Google Scholar]
- 106.Zhao Y., Jiang Y., Wu Y. Investigation on Knowledge, Attitude and Practice on Antibiotics among Undergraduates of Sichuan University. China Pharm. Aff. 2017;31:1522–1526. doi: 10.16153/j.1002-7777.2017.12.025. (In Chinese) [DOI] [Google Scholar]
- 107.Li J., Li Y., Wei Y. Analysis on the Antibiotic Status of Rural Residents in Ethnic Autonomous Regions and Its Influencing Factors—Take Pingluo County for Example. China Health Ind. 2018;15:173–178. doi: 10.16659/j.cnki.1672-5654.2018.07.173. (In Chinese) [DOI] [Google Scholar]
- 108.Huang C., Jin Y. Effect Evaluation on Health Education Prevention for Reasonable Use of Antibiotics in Huating Town of Shanghai. Health Educ. Health Promot. 2014;9:439–441. doi: 10.16117/j.cnki.31-1974/r.2014.06.010. (In Chinese) [DOI] [Google Scholar]
- 109.Wu C., Guan S. Intervention effect evaluation antibiotics among boarding students in Wenzhou. Chin. Sch. Health. 2012;33:531–532. doi: 10.16835/j.cnki.1000-9817.2012.05.010. (In Chinese) [DOI] [Google Scholar]
- 110.Wen W. Investigation on Antibacterial Drug Knowledge and Drug Use Behavior of Residents in Yingze District. J. Shanxi Med. Coll. Staff Work. 2018;28:82–84. (In Chinese) [Google Scholar]
- 111.Lu T., Li X. Research on the Knowledge, Attitudes and Behaviors of Antibiotic Use among College Students from 5 Universities in Nanjing. J. Nanjing Med Univ. (Soc. Sci. Ed.) 2016;16:274–280. doi: 10.7655/NYDXBSS20160406. (In Chinese) [DOI] [Google Scholar]
- 112.Rong J., Gao J., Zhang L. Investigation and analysis on the cognitive situation of rational use of antibiotics in Shanghai. Health Educ. Health Promot. 2013;8:208–210. doi: 10.16117/j.cnki.31-1974/r.2013.03.030. (In Chinese) [DOI] [Google Scholar]
- 113.Zhang Y., Yu J., Li P. A survey of knowledge, attitude and practice about antibiotic use among caregivers and health knowledge among school–aged children; Proceedings of the Chinese Pharmaceutical Association Pharmaceutical Management Professional Committee Annual Meeting and Academic Symposium; Jinan, Shandong, China. 24 August 2018; (In Chinese) [Google Scholar]
- 114.The Medicine and Society Guide for Authors. [(accessed on 16 April 2021)]; Available online: http://yxysh.hust.edu.cn/info/1008/1036.htm.
- 115.The Chinese Health Service Management Guide for Authors. [(accessed on 16 April 2021)]; Available online: http://www.zgwssygl.cn/html/list–10–1.html.
- 116.Larson E., Lin S.X., Gomez–Duarte C. Antibiotic use in Hispanic households, New York city. Emerg. Infect. Dis. 2003;9:1096–1102. doi: 10.3201/eid0909.020371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Grigoryan L., Germanos G., Zoorob R., Juneja S., Raphael J.L., Paasche–Orlow M.K., Trautner B.W. Use of Antibiotics Without a Prescription in the U.S. Population: A Scoping Review. Ann. Intern. Med. 2019;171:257–263. doi: 10.7326/M19-0505. [DOI] [PubMed] [Google Scholar]
- 118.Mainous A.G., 3rd, Cheng A.Y., Garr R.C., Tilley B.C., Everett C.J., McKee M.D. Nonprescribed antimicrobial drugs in Latino community, South Carolina. Emerg. Infect. Dis. 2005;11:883–888. doi: 10.3201/EID1106.040960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zoorob R., Grigoryan L., Nash S., Trautner B.W. Nonprescription Antimicrobial Use in a Primary Care Population in the United States. Antimicrob. Agents Chemother. 2016;60:5527–5532. doi: 10.1128/AAC.00528-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Saradamma R.D., Higginbotham N., Nichter M. Social factors influencing the acquisition of antibiotics without prescription in Kerala State, south India. Social Sci. Med. 2000;50:891–903. doi: 10.1016/S0277-9536(99)00380-9. [DOI] [PubMed] [Google Scholar]
- 121.Measures for the Administration of Clinical Application of Antibacterial Drugs. [(accessed on 22 March 2021)]; Available online: http://www.nhc.gov.cn/fzs/s3576/201808/f5d983fb5b6e4f1ebdf0b7c32c37a368.shtml.
- 122.About the General Office of the State Council Opinions on Improving the National Essential Drug System. [(accessed on 22 March 2021)]; Available online: http://www.gov.cn/zhengce/content/2018–09/19/content_5323459.htm.
- 123.The 13th Five–Year Plan for Deepening the Reform of the Medical and Health System. [(accessed on 22 March 2021)]; Available online: http://www.gov.cn/zhengce/content/2017–01/09/content_5158053.htm.
- 124.Chang J., Xu S., Zhu S., Li Z., Yu J., Zhang Y., Zu J., Fang Y., Ross–Degnan D. Assessment of non–prescription antibiotic dispensing at community pharmacies in China with simulated clients: A mixed cross–sectional and longitudinal study. Lancet Infect. Dis. 2019;19:1345–1354. doi: 10.1016/S1473-3099(19)30324-X. [DOI] [PubMed] [Google Scholar]
- 125.Gong Y., Jiang N., Chen Z., Wang J., Zhang J., Feng J., Lu Z., Yin X. Over–the–counter antibiotic sales in community and online pharmacies, China. Bull. World Health Organ. 2020;98:449–457. doi: 10.2471/BLT.19.242370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kalungia A., Godman B. Implications of non–prescription antibiotic sales in China. Lancet Infect. Dis. 2019;19:1272–1273. doi: 10.1016/S1473-3099(19)30408-6. [DOI] [PubMed] [Google Scholar]
- 127.Covvey J.R., Johnson B.F., Elliott V., Malcolm W., Mullen A.B. An association between socioeconomic deprivation and primary care antibiotic prescribing in Scotland. J. Antimicrob. Chemother. 2014;69:835–841. doi: 10.1093/jac/dkt439. [DOI] [PubMed] [Google Scholar]
- 128.McNulty C.A., Boyle P., Nichols T., Clappison P., Davey P. Don’t wear me out––the public’s knowledge of and attitudes to antibiotic use. J. Antimicrob. Chemother. 2007;59:727–738. doi: 10.1093/jac/dkl558. [DOI] [PubMed] [Google Scholar]
- 129.Pechère J.C., Hughes D., Kardas P., Cornaglia G. Non–compliance with antibiotic therapy for acute community infections: A global survey. Int. J. Antimicrob. Agents. 2007;29:245–253. doi: 10.1016/j.ijantimicag.2006.09.026. [DOI] [PubMed] [Google Scholar]
- 130.Grosso G., Marventano S., Ferranti R., Mistretta A. Pattern of antibiotic use in the community: Νon–adherence and self–prescription rates in an Italian urban population. Mol. Med. Rep. 2012;5:1305–1310. doi: 10.3892/mmr.2012.818. [DOI] [PubMed] [Google Scholar]
- 131.Demoré B., Mangin L., Tebano G., Pulcini C., Thilly N. Public knowledge and behaviours concerning antibiotic use and resistance in France: A cross–sectional survey. Infection. 2017;45:513–520. doi: 10.1007/s15010-017-1015-2. [DOI] [PubMed] [Google Scholar]
- 132.Fernandes M., Leite A., Basto M., Nobre M.A., Vieira N., Fernandes R., Nogueira P., Nicola P.J. Non–adherence to antibiotic therapy in patients visiting community pharmacies. Int. J. Clin. Pharm. 2014;36:86–91. doi: 10.1007/s11096-013-9850-4. [DOI] [PubMed] [Google Scholar]
- 133.Horne R., Chapman S.C., Parham R., Freemantle N., Forbes A., Cooper V. Understanding patients’ adherence–related beliefs about medicines prescribed for long–term conditions: A meta–analytic review of the Necessity–Concerns Framework. PLoS ONE. 2013;8:e80633. doi: 10.1371/journal.pone.0080633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wei L., Champman S., Li X., Li X., Li S., Chen R., Bo N., Chater A., Horne R. Beliefs about medicines and non–adherence in patients with stroke, diabetes mellitus and rheumatoid arthritis: A cross–sectional study in China. BMJ Open. 2017;7:e017293. doi: 10.1136/bmjopen-2017-017293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.World Health Organization . Antibiotic Resistance: Multi–country Public Awareness Survey. World Health Organization; Geneva, Switzerland: 2015. [Google Scholar]
- 136.NHS UK Antibiotic Uses. [(accessed on 15 April 2021)]; Available online: https://www.nhs.uk/conditions/antibiotics/uses/
- 137.Sun C., Hu Y.J., Wang X., Lu J., Lin L., Zhou X. Influence of leftover antibiotics on self–medication with antibiotics for children: A cross–sectional study from three Chinese provinces. BMJ Open. 2019;9:e033679. doi: 10.1136/bmjopen-2019-033679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Gualano M.R., Gili R., Scaioli G., Bert F., Siliquini R. General population’s knowledge and attitudes about antibiotics: A systematic review and meta–analysis. Pharmacoepidemiol. Drug Saf. 2015;24:2–10. doi: 10.1002/pds.3716. [DOI] [PubMed] [Google Scholar]
- 139.National Action Plan for Containing Antimicrobial Resistance (2016–2020) Available online: https://www.who.int/publications/m/item/china–national–action–plan–to–contain–antimicrobial–resistance–(2016–2020)
- 140.Huttner B., Goossens H., Verheij T., Harbarth S. Characteristics and outcomes of public campaigns aimed at improving the use of antibiotics in outpatients in high–income countries. Lancet Infect. Dis. 2010;10:17–31. doi: 10.1016/S1473-3099(09)70305-6. [DOI] [PubMed] [Google Scholar]
- 141.Cross E.L., Tolfree R., Kipping R. Systematic review of public–targeted communication interventions to improve antibiotic use. J. Antimicrob. Chemother. 2017;72:975–987. doi: 10.1093/jac/dkw520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Make Prescription Medication No Longer Difficult! Trial Operation of the Province’s First Electronic Prescription Circulation Supervision Service Platform. [(accessed on 7 December 2020)]; Available online: https://baijiahao.baidu.com/s?id=1685403808329340175&wfr=spider&for=pc.
- 143.Chen J., Wang Y., Chen X., Hesketh T. Widespread illegal sales of antibiotics in Chinese pharmacies–a nationwide cross–sectional study. Antimicrob. Resist. Infect. Control. 2020;9:12. doi: 10.1186/s13756-019-0655-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kotwani A., Wattal C., Joshi P.C., Holloway K. Irrational use of antibiotics and role of the pharmacist: An insight from a qualitative study in New Delhi, India. J. Clin. Pharm. Ther. 2012;37:308–312. doi: 10.1111/j.1365-2710.2011.01293.x. [DOI] [PubMed] [Google Scholar]
- 145.Khan T.M., Ibrahim Y. A qualitative exploration of the non–prescription sale of drugs and incidence of adverse events in community pharmacy settings in the Eastern Province of the Kingdom of Saudi Arabia. Eur. J. Hosp. Pharm. Sci. Pract. 2013;20:26. doi: 10.1136/ejhpharm-2012-000161. [DOI] [Google Scholar]
- 146.Parsons S., Morrow S., Underwood M. Did local enhancement of a national campaign to reduce high antibiotic prescribing affect public attitudes and prescribing rates? Eur. J. Gen. Pract. 2004;10:18–23. doi: 10.3109/13814780409094222. [DOI] [PubMed] [Google Scholar]
- 147.Lim J.M., Singh S.R., Duong M.C., Legido–Quigley H., Hsu L.Y., Tam C.C. Impact of national interventions to promote responsible antibiotic use: A systematic review. J. Antimicrob. Chemother. 2020;75:14–29. doi: 10.1093/jac/dkz348. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found through the search strategy.