Abstract
Differentiated thyroid tumors (DTTs) are characterized by significant molecular variability in both spatial and temporal intra-tumoral heterogeneity (ITH), that could influence the therapeutic management. ITH phenomenon appears to have a relevant role in tumor growth, aggressive behavior and drug resistance. Accordingly, characteristics and consequences of ITH in DTTs should be better analyzed and understood in order to guide clinical practice, improving survival. Consequently, in the present review, we investigated morphological and molecular ITH of DTTs in benign, borderline neoplasms and in malignant entities, summarizing the most significant data. Molecular testing in DTTs documents a high risk for recurrence of cancer associated with BRAFV600E, RET/PTC 1/3, ALK and NTRK fusions, while the intermediate risk may be related to BRAFK601E, H/K/N RAS and PAX8/PPARγ. In addition, it may be suggested that tumor genotype is associated with peculiar phenotype.
Keywords: intratumoral heterogeneity, thyroid tumor, BRAF, RET/PTC rearrangements, RAS mutation
1. Introduction
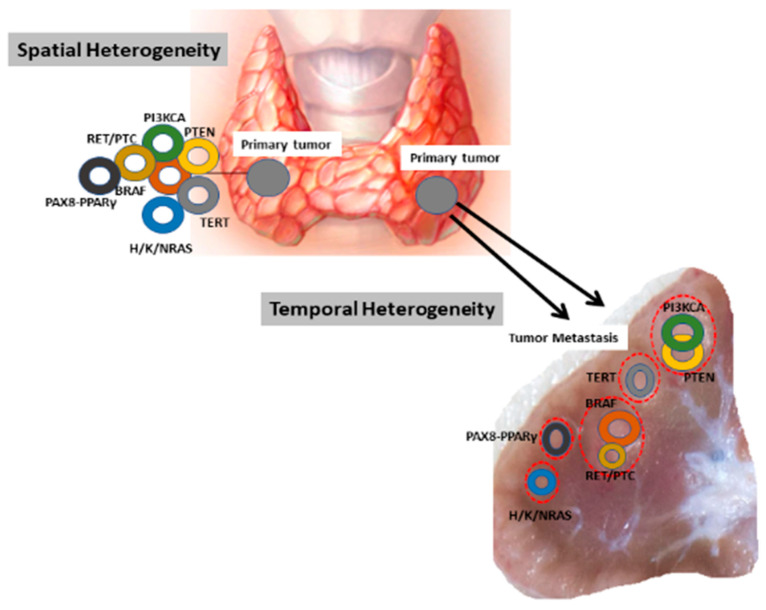
Intratumoral heterogeneity (ITH) represents a crucial determinant to explain the appearance of therapeutic resistance and treatment failure, resulting in poor prognosis and outcome. This intralesion mechanism is defined as diversity observed within a tumor since mosaics of different neoplastic clones are present in the same tumor at varying time [1]. ITH can exist either between geographical areas of the same tumor (spatial heterogeneity) or between different lesions that appear over time locally or distantly (temporal heterogeneity) (Figure 1) [1,2].
Figure 1.
Spatio-temporal heterogeneity in primary and corresponding lymph node metastasis in thyroid tumors.
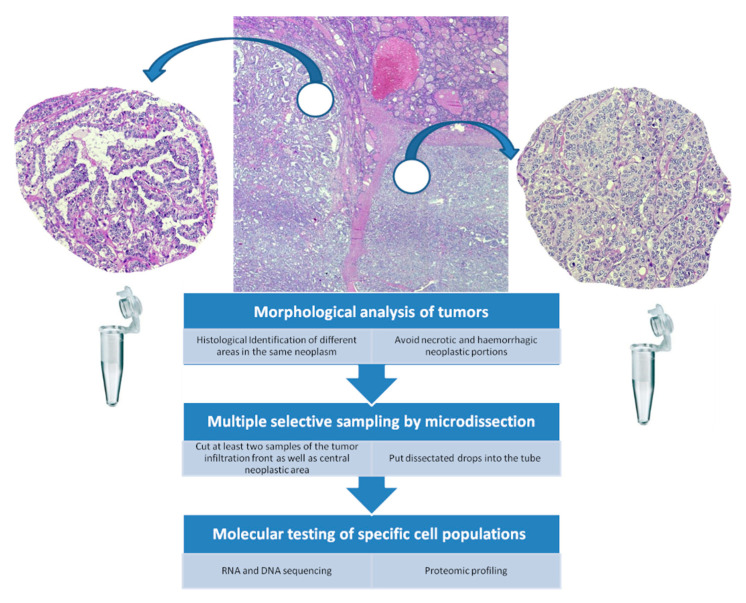
Temporal ITH leads to discordance between the primary tumor and the metastatic lesion, and it can stem from either two mutations in different clones in the primary tumor, one clone disseminating to the metastatic site or from a new mutation occurring in the metastatic lesion [3]. ITH may determine the development of different cell subpopulations which in turns may influence the response of a tumor to changes within the microenvironment [3,4]. In addition, this phenomenon may create a neoplastic diffusion throughout the body, realizing metastatic deposits or acquiring resistance to therapeutic agents. Therefore, ITH analysis can provide relevant information to define innovative and patient-tailored therapeutic strategies, based on detection of specific molecular alterations [2,4,5,6]. So far, ITH has been addressed at both morphological and molecular levels with different methods [7,8,9,10]. Specifically, microdissection is essential to define morphological heterogeneity, which includes histotype, tissue composition, inflammatory reaction, center and borders of tumors [6,8]. Indeed, at a microscopic level, pathologists can recognize different histological patterns in each tumor, with specific morphological characteristics, such as necrosis, apoptosis, fibrosis, hemorrhagic areas, stromal reaction and neo-angiogenesis. An operative workflow to analyze ITH in tumors should be based on morphology, requiring an examination of extensive neoplastic areas to identify the different histological portions of the tumor, analyzing at least two or more representative different portions obtained by microdissection procedure (Figure 2). However, the intratumoral differentiation (well-, moderately-, poorly-) is frequently focal, leading to morphofunctional differences. Furtherly, the choice of tissue specimens may depend on the location of the tumor infiltration front, with elements able to invade capsule and stroma, in contrast to central neoplastic section (Figure 2). Then, the dissected portions have to be passed in a tube for the RNA/DNA sequencing as well as proteomic profiling (Figure 2).
Figure 2.
A schematic proposed workflow to identify ITC and to perform molecular tests in DTC.
In addition to the inter-tumor heterogeneity, namely diversity between individuals having the same tumor type, ITH may result in different histological and cytological patterns in the same tumor, negatively impacting on the patient’s prognosis [11,12,13]. At the molecular level, genetic and epigenetic heterogeneity can be present [14]. Particularly, immunohistochemistry, in situ hybridization methods and next generation sequencing by detecting mutations of the driver genes secondary to genetic instability may help reveal clonal and/or non-clonal heterogeneity, which are associated to phenotypic alterations driving neoplastic progression and resistance to targeted therapy [6,15,16,17,18,19].
One of the most evident examples of ITH is encountered in thyroid carcinomas and adenomas. Although the majority of differentiated thyroid carcinomas (DTCs) show an indolent behavior with an excellent prognosis, as documented by a 10-years survival rate of 90%, approximately 10% of them are aggressive, tend to recur and lead the patient to death [20,21,22,23,24]. In this regard, a broad ITH is evident, with histotypes spanning from thyroid papillary microcarcinoma through anaplastic carcinoma, the latter representing the late and fatal stage of carcinogenesis [25,26,27,28,29].
The present paper should be considered as a review in order to furnish the “state of art” regarding ITH in differentiated thyroid tumors (DTCs). The major endpoint is to comparatively analyze morphological and molecular ITH of differentiated thyroid tumors (DTTs), either follicular adenoma (FA) either DTCs in order to evaluate their behavior, identifying markers for therapeutic approaches and making individualized their management. Regarding the novelty of the present review, probably there are not additional original data, but a relevant number for information concerning molecular variability in DTCs in relation to the corresponding morphological aspects as well as a precise definition of the operative workflow to reveal ITH.
2. Phenotypic and Molecular Heterogeneity in FA and Follicular-Patterned Borderline Lesions
To define morphological ITH in DTTs, we need to introduce the new classification of thyroid tumors, in which some changes were introduced [30,31,32,33,34]. In fact, together with follicular adenoma (FA), some borderline entities were added, such as tumors with uncertain malignant potential (UMP), noninvasive follicular thyroid neoplasms with papillary-like nuclear features (NIFTP) and hyalinizing trabecular tumor (HTT) [30,32] (Figure 3). FA were defined as benign, encapsulated and non-invasive neoplasm demonstrating evidence of thyroid follicular cell differentiation without nuclear features observed in papillary thyroid carcinoma (PTC) [30]. According to the 2017 WHO classification [35], the group of encapsulated follicular-patterned UMP tumors is divided into two entities: follicular tumors with uncertain malignant potential (FT-UMP) and well-differentiated tumors with uncertain malignant potential (WDT-UMP) (Figure 3A). FT-UMP is an encapsulated and/or well-circumscribed tumor with round nuclei that lack PTC-like features, whereas WDT-UMP presents a similar gross morphology but, well/partially developed nuclear changes of PTC and questionable capsular or vascular invasion [36,37].
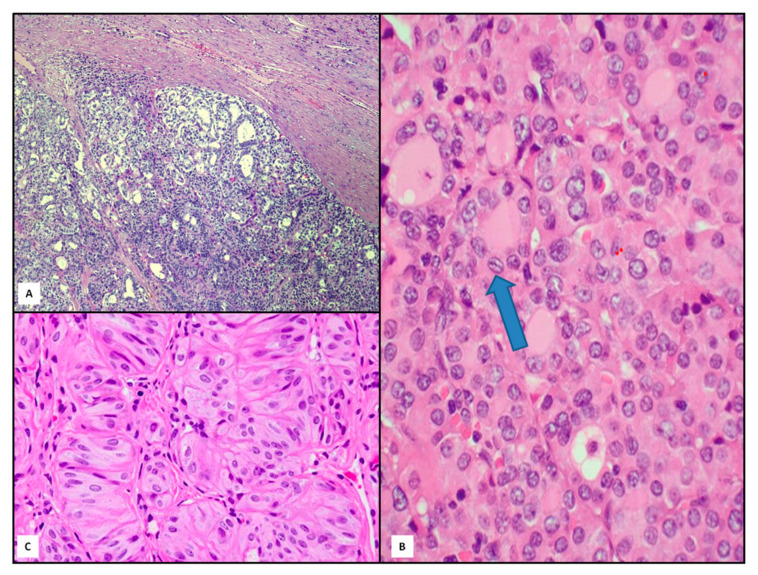
Figure 3.
Histological findings of follicular-patterned borderline lesions: tumor with uncertain malignant potential (UMP) ((A), hematoxylin and eosin, 80×), noninvasive follicular thyroid neoplasms with papillary-like nuclear features (NIFTP) ((B), hematoxylin and eosin, 400×) and hyalinizing trabecular tumor (HTT) ((C), hematoxylin and eosin, 200×). The arrow underlines the peculiar irregular nuclear membranes.
NIFTP is a solitary encapsulated nodule displaying the following features: a complete, frequently thick, fibrous capsule delimitating the tumor from adjacent tissue, follicular growth pattern and nuclear features of PTC [38] (Figure 3B). Papillae and capsular or vascular invasion are constantly absent [38,39]. Furthermore, NIFTP may be distinguished from both FA and hyperplastic nodule by the presence of the typical nuclear changes of PTC [40,41,42,43] (Figure 3B).
Another new interesting follicular-derived borderline lesion is represented by HTT, a well circumscribed solid neoplasm without capsular/vascular invasion or invasion of thyroid tissue adjacent to the tumor. Histologically, HTT is composed of trabeculae or sometimes nests of polygonal eosinophilic large cells intermingled with thin stromal bundles. This lesion maybe associated with chronic thyroiditis, nodular goiter or PTC [44,45,46] (Figure 3C).
Molecular profiles concerning classical FA and follicular-patterned borderline tumors are quite different (Table 1).
Table 1.
Histological and molecular heterogeneity in FA and follicular-patterned borderline lesions (H,K,N isoforms of RAS gene family).
| Mutations | |||||||
|---|---|---|---|---|---|---|---|
| PAX8-PPARγ | EIF1AX | EZH1 | GNAS | RAS | BRAF | RET/PTC | |
| FA | 5–20% | 5–10% | 3% | ~80% | HRAS 8%, KRAS 10%, NRAS 6% | - | - |
| NIFTP | 5% | - | - | - | H/N/KRAS (45%) | - | - |
| HTT | - | - | - | - | NRAS 0% | - | 47% |
| FT/WDT-UMP | <5% | - | - | - | HRAS 3–12%, KRAS 6–9%, NRAS 16–35% | - | - |
For instance, paired box gene 8 (PAX8)-peroxisome proliferator-activated receptor-γ (PPARγ) rearrangements are detected in about 5–20% of FA, but they are absent in non-pathological thyroid parenchyma surrounding FA or in the hyperplastic nodules [47,48,49]. Of the other somatic genetic alterations, Eukaryotic Translation Initiation Factor 1A X-Linked (EIF1AX) gene activating mutation is found in 5–10% of FA [50,51], while telomerase reverse transcriptase (TERT) promoter mutation are very rare in genuine FA and occasionally present in FA with atypical features [50,52]. Additionally, mutations concerning Enhancer of zeste 1 polycomb repressive complex 2 subunit (EZH1) gene are detected in 3% of the FA, frequently in association with the TSH-receptor (TSHR) and/or the guanine nucleotide binding protein, alpha stimulating (GNAS) mutations, and accounting for nearly 80% of cases in some series [33,47,53]. RAS mutations exhibit different rates in FA: mutations in HRAS are detected in 8%, in NRAS in 6% and in KRAS in 10%, respectively [51,54,55]. Interestingly, RAS mutations have a higher prevalence in FA of persons living in area of iodine deficiency [56]. In UMP tumors, HRAS mutation are present in 3–12% of cases at codon 61, similarly to KRAS mutations (6–9% of cases), but less frequently than NRAS mutations (16–35% of cases) [50,51,54,55]. However, H/N/K-RAS mutations are detected in 45% of NIFTP cases, while BRAFV600E mutation and Rearranged during transfection (RET) fusions are absent [51,55]. Finally, HTT lacks BRAF or NRAS mutations, but it has considerable frequency of RET/PTC rearrangements (47%) similar to that encountered in PTC [55,57].
3. Phenotypic and Molecular Heterogeneity in FTC
Follicular thyroid carcinomas (FTCs), which are well-known more aggressive cancer compared with PTCs, have a prevalent histologic presentation as microfollicular or trabecular patterns, and a less frequent architecture with follicular and colloid-rich morphology [58,59]. There are also morphological rarer subtypes that are predictive of a worse prognosis, including spindle cells, clear cells, signet-ring cells, rhabdoid and insular phenotypes [60,61]. Generally, regardless of histotype, FTCs present a thin or thick fibrous capsule that contains some small vessels; consequently, capsular invasion produces an incomplete delimitation of the tumor and becomes an indicator of vascular invasion. Based on the extent of capsular/vascular invasion, FTCs may be divided into two subgroups of prognostic significance, minimally invasive FTCs (Figure 4A) and widely invasive FTCs [60,61]. In 2015 the prognostic subgroups became four: minimally invasive with capsular invasion, minimally invasive with limited [<4 vessels) vascular invasion, minimally invasive with extensive [≥4 vessels) vascular invasion and widely invasive [59,62]. Recently, the last 2017 WHO classification suggested a 3-tiered risk groups: minimally invasive [capsular invasion only), encapsulated angio-invasive and widely invasive [59,60,61,62,63].
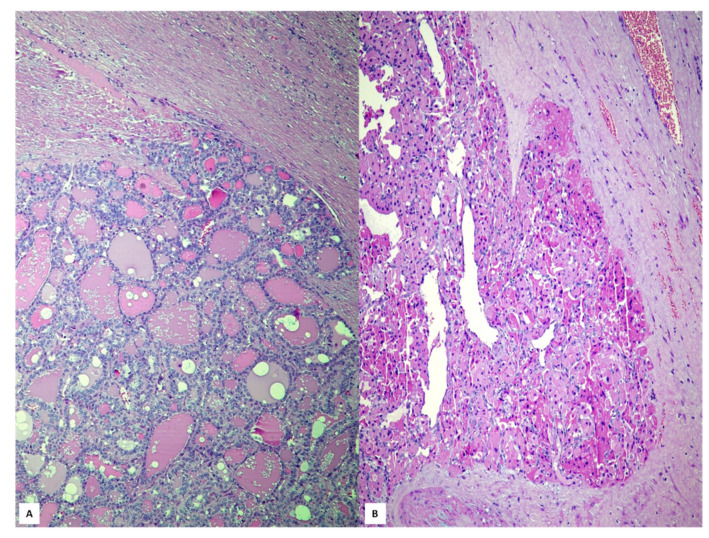
Figure 4.
The follicular thyroid carcinoma with minimally invasive capsular infiltration ((A), hematoxylin and eosin, 80×); malignant Hürthle cell tumor characterized by an evident capsular invasion ((B), hematoxylin and eosin, 100×).
From a molecular perspective, the major driving mutations of FTCs are those in the RAS family of genes; for this reason, these tumors are also known as RAS-like tumors [30,51,64,65] (Table 2).
Table 2.
Histological and molecular heterogeneity in FTC and HCT.
| Mutations | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| PIK3CA | EIF1AX | TP53 | PAX8-PPARγ | RAS | BRAF | TERTp | NF1 | MADCAM-1 | |
| FTC | 10% | 6% | 3% | 10–50% | HRAS 8%, KRAS 6%, NRAS 19% | 1% | 17–25% | - | - |
| Poorly differentiated FTC | 0–15% | - | 10–30% | <3% | H/N/KRAS (10–40%) | 5–30% | - | - | - |
| HCT | - | 11% | 7% | <5% | KRAS 11%NRAS 6% | - | 17% | 7% | 20% |
In detail, the three concurrent somatic H/N/K-RAS mutation were detected with different percentage, 8%, 19% and 6% respectively [51]. In addition, TERT promoter (TERTp) mutations have been revealed in 25% of FTCs, which are characterized by older age of patients, larger tumor size, advanced stage (III–IV), distant metastases and disease specific mortality [52]. Several other genes, which are generally involved in Phosphoinositide 3-kinases (PI3K)/Phosphatase and tensin homolog (PTEN)/AKT pathway have been found as mutated in FTCs [66,67]. PIK3CA copy gains are encountered in FTCs (10%) in comparison to BRAF mutations (1%) [67,68]. PTEN and PIK3CA mutations as well as PIK3CA copy gains rarely coexist in FTCs, while PI3K-PTEN-AKT pathway is common in poorly differentiated and anaplastic thyroid carcinomas, suggesting their important role in tumor progression [68,69]. Moreover, in FTCs EIF1AX mutation was identified in 6% of cases related with advanced disease [67,68]. ITH was also detected in FTCs with a range of histologic aspects, namely with follicular areas coexisting with poorly differentiated ones [67]. Interestingly, in poorly differentiated aggressive FTCs are characterized by frequent mutations in p53 (10–30%), RAS (10–40%), BRAF (5–30%) [69,70], but rare PAX8/PPARγ rearrangements (7–10%) have been reported [71,72]. Nevertheless, in FTCs PAX8/PPARγ rearrangements were revealed in female and younger patients with high cellularity and invasive aspects; this positively rearranged FTC documented a lower risk for distant metastasis [50].
Even if classified as follicular-patterned tumors, Hürthle cell tumors (HCTs) present peculiar microscopic characteristics consisting in large elements with abundant eosinophilic granular cytoplasm, centrally located nuclei and prominent nucleoli [73]. The new WHO classification distinguishes benign and malignant HCTs on the basis of capsular and vascular invasion (Figure 4B), similarly to FTCs [73]. Although believed to have a poorer prognosis compared to FTCs, it was demonstrated that Hürthle cell cancer has not higher rates of recurrence and does not concentrate less radioiodine [74,75,76]. Nevertheless, it has been reported that somatic genomic alterations in malignant HCTs are represented by Mucosal Vascular Address in Cell Adhesion Molecule 1 (MADCAM-1) (20%), EIF1AX (11%), DAXX, PT53 (7%) and Neurofibromatosis type 1 (NF1) (7%) mutations, while no BRAF mutations and a lower rate of NRAS (9%) mutation are encountered in comparison to FTC cases [77,78,79] (Table 2). In addition, TERTp and KRAS mutations have been identified in 17% and 11% respectively; NRAS occurred with a lower percentage (6%) [51].
4. Phenotypic and Molecular Heterogeneity in PTC and Its Variants
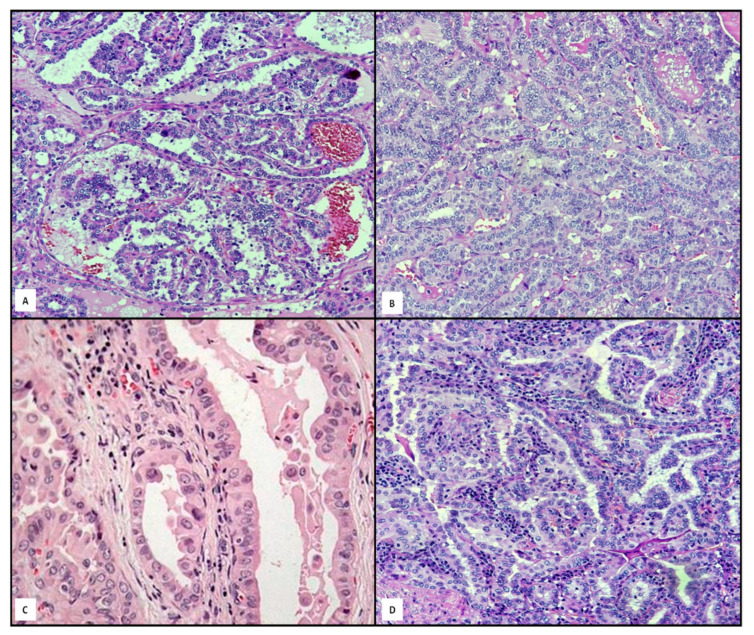
As well known, PTCs are not only the most common DTCs, but also the most common malignant entity, in that they account for over 70% of all thyroid neoplasms [80]. The classical variant presents typical microscopic features (Figure 5A), such as overlapping and clearing nuclei, irregularities of nuclear membrane in papillary architecture with fibrovascolar cores, psammoma bodies and sometimes aggregates of lymphocytes. Sixteen PTC variants with different behavior have been reported so far [81,82,83,84,85,86]. After the classic variant, the most common variants are the follicular one (Figure 5B), hobnail/micropapillary (Figure 5C), Whartin-like (Figure 5D) and solid one [81,82,83]. In spite of this morphological variability, molecular ITH is not constantly present, even in multifocal PTCs [84,85,86].
Figure 5.
A gallery of some relevant variants of PTC: classical ((A), hematoxylin and eosin, 120×); follicular ((B), hematoxylin and eosin, 120×); Whartin-like ((C), hematoxylin and eosin, 120×); micropapillary ((D), hematoxylin and eosin, 160×).
Genetic ITH of PTCs was scarcely addressed so far, partly due to the relatively low number of oncogenes involved in the early stages [87,88,89] (Table 3). BRAF mutations have been reported in 55% of the classical phenotype with a further significant increase in more aggressive and poorly differentiated PTCs [90,91], and in up to one third of cases of the columnar-cell variant [92,93]. In addition, BRAF mutations are frequently combined with TP53, TERTp, PIK3CA, catenin β-1 (CTNNB1), epidermal growth factor receptor (EGFR), v-akt murine thymoma viral oncogene homolog 1 (AKT1) and Notch homolog-1 (NOTCH1) mutations [83,94,95,96]. In the hobnail variant, the mutations detected concern BRAF (25%), TP53 (55%) and NOTCH1 (5%) [83,94,95,96]. It is well known that mutations in BRAF and RET genes (see below) may occur both in the initial steps of carcinogenesis and in the advanced ones [97,98]. However, different foci of the same PTC may differ for their BRAF status, and such difference may also exist between a primary PTC and any of its lymph node and/or distant metastases in up to one third of cases [97,98,99]. For instance, BRAFV600E mutation may occur either de novo in metastasized lymph nodes, or in metastasizing mutated cells could spread from non-analyzed PTC foci of the primary tumor [100,101,102]. ITH in BRAFV600E have been also demonstrated, since only less than 50% of neoplastic elements manifested BRAF mutation [103,104]. Although, the prognostic role of BRAFV600E mutation is still debatable, some studies showed an association with poor outcome, extra thyroid neoplastic extension and increased recurrence risk in PTCs [50,96,97,98]. By contrast, PTC with low risk clinicopathological features did not exhibit BRAFV600E mutations [101,102,103].
Table 3.
Histological and molecular heterogeneity in PTC.
| Mutations | ||||||||
|---|---|---|---|---|---|---|---|---|
| EIF1AX | TP53 | RAS | BRAF | TERT | RET | ALK | NOTCH1 | |
| Classical PTC | 0–5% | - | H/N/KRAS 6% | 55% | 5–15% | 5–25% | - | - |
| Clear cell/solid variant PTC | - | - | H/N/KRAS 30% | >55% | - | - | 5% | - |
| Columnar variant PTC | - | - | - | 33% | - | - | - | - |
| Tall cell variant PTC | - | - | - | 80–100% | - | - | - | - |
| Hobnail variant PTC | - | 55% | - | 25% | - | - | - | 5% |
Another common genetic alteration in PTCs is the RET/PTC rearrangement [105,106], which occurs in one third of cases of sporadic PTCs in adults, in half of cases of PTCs in children and young adults, mainly when lymph node metastasis and aggressive clinicopathological features were documented, similarly to NTRK rearranged PTC [107,108,109]. However, it has been shown that PTCs characterized by fusion oncogene (RET or NTRK) exhibited overlapping clinical behavior [109]. RET/PTC rearrangement has been also frequently observed in subjects exposed to radiation, either accidentally or therapeutically [110]. Moreover, this genetic alteration early occurs in thyroid carcinogenesis, being essentially restricted to PTCs and Hürthle cell tumors [111,112]. Finally, a low rate (1–5%) of PTCs documented ALK rearrangement in predominant follicular solid infiltrative pattern or in diffuse sclerosing variant, showing sometimes extrathyroidal extension as well as lymph node metastases [113].
As said at the beginning of this review, different methods of detection (immunohistochemistry, RT-PCR, RNA analysis after Laser Capture Microdissection) are able to detect RET/PTC rearrangements, the distribution of which may be influenced by intrinsic genetic [111]. Interestingly, Schopper et al. tested a panel of 8 cancer-related genes (BRAF, KRAS, HRAS, NRAS, EGFR, PIK3CA, KIT, and platelet-derived growth factor receptor α polypeptide [PDGFRA]) by using next-generation sequencing (NGS) in a single thyroid tumor presenting as a combination of conventional PTC with 4 variants (follicular, clear cell, columnar and poorly differentiated [112,113,114,115]. While conventional PTCs showed only a limited rate of H/N/KRAS mutation (6%), the clear cell and the follicular variants harbored KRAS mutations up to 5 times more frequently, viz. 30% and 20% respectively [114,115,116]. Finally, in PTCs the degree of DNA methylation is smaller than in follicular tumors (FA and FTC), and it varies according to BRAF and RAS status [117].
Despite a robust line of research, clinical implications of ITH in PTCs are questioned. Indeed, two studies demonstrated that allelic frequencies of mutated alleles are consistent with a monoclonal origin of PTCs, suggesting ITH in as many as ~10% of tumors [117,118].
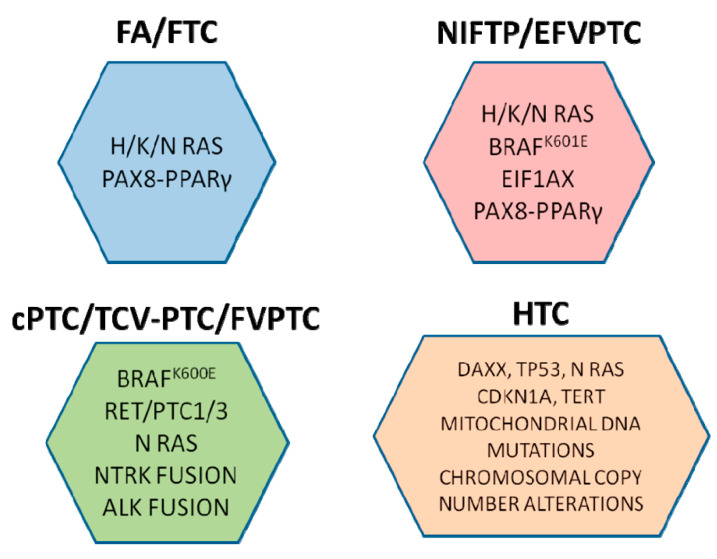
5. Conclusions
ITH influences tumor progression and response to treatment, as the appearance of resistant clones due to the selection pressure of treatment may worsen the patient’s prognosis. Therefore, ITH profiling can be useful to characterize thyroid cancer pathogenesis, together with the analysis of different genetic alterations associated with oncological risk. Nowadays, molecular testing in DTCs suggests a high risk for recurrence of cancer associated with BRAFV600E, RET/PTC 1/3, ALK and NTRK fusions, while the intermediate risk may be related to BRAFK601E, H/K/N RAS and PAX8/PPARγ (Figure 6).
Figure 6.
Synopsis showing the main biomolecular mutations in DTCs related to different histotypes.
Consequently, it may be suggested that tumor genotype is associated with peculiar phenotype; therefore, the identification of DTC morphology may be the driver to select different neoplastic portions in which molecular heterogeneity could be revealed. From this point of view, neoplastic sub-populations with different risk of recurrence or metastasis may be advantageously stratified, correctly treated and subjected to a shorter follow-up period. Recently, to measure ITH in cancer, an index has been proposed [119]; in detail, some neoplasms such as uterine carcinosarcoma, colorectal adenocarcinoma and ovarian cancer have been observed to be more heterogeneous than renal clear cell carcinoma and DTC [119].
Recent studies based on genetic analysis of thyroid tumors have brought several intriguing therapeutical personalized options for DTCs [120]. This innovative vision in which particularly targeted therapies based on specific diagnostic tests has been defined as “theranostics”, in order to provide a transition from conventional to a contemporary personalized medicine [121]. The first theranostic agent has been considered as the radioiodine treatment widely used for the management of DTC. Nevertheless, about 65% of the patients with advanced thyroid disease may became radioiodine-refractory related to the sodium/iodide symporter (NIS) [120,121]. Therefore, the targeted therapy of DTC should be connected to the genetic and epigenetic alterations and signaling pathways. In detail, PPARγ agonists, HDAC inhibitors, PI3K/AKT inhibitors and MEK/ERK inhibitors, have been recommended for NIS over-expression and have caused improved iodine uptake in thyroid cancers [121]. Moreover, it was shown that Dabrafenib represents the selective inhibitor of mutated forms of BRAF and it can realize the radioiodine uptake in metastatic PTC BRAFV600E-mutant iodine-refractory patients. Similarly, some molecular markers such as p53, PIK3CA, CTNNB1 and AKT1 may be considered indicators for an aggressive behavior of DTCs [121]. Furthermore, since fine needle aspiration cytology (FNAC) has been considered the commonly utilized morphological test, the molecular profiling may improve the diagnostic accuracy mainly in indeterminate or gray zone, furtherly supporting a personalized treatment for DTCs [122].
A better understanding of the molecular basis of thyroid cancers as well as development of more effective cancer therapies has revolutionized the treatment approach in patients with advanced thyroid cancer. Nevertheless, whether overall survival is improved with the use of these agents is still unclear. In fact, the major limitation in applying targeted therapies is their side-effects profile, as well as in the development of escape and resistance mechanisms by the tumors. Specifically, neoplastic cells may acquire resistance to the treatment by developing an escape mechanism against the targeting drugs. Consequently, most DTCs could develop resistance against targeted drugs by acquiring new mutations that result in over-activation of pathways or by induction of alternate pathways.
Nowadays, the cancer diagnosis should be assessed by a complex of information regarding to clinical, pathological, molecular and protein expression data of a specific neoplastic proliferation and its surrounding microenvironment; such an integrated system has been defined as “tissunomics” [123,124]. In full agreement with this approach, we contend that a systematic integration of morphology and molecular characteristics in DTC should be helpful in patient’s management.
Acknowledgments
The authors would like to thank Sandra De Dominici for her skilled technical assistance in reviewing the English style and grammar of the manuscript.
Abbreviations
| AKT1 | v-akt murine thymoma viral oncogene homolog 1 |
| DTC | differentiated thyroid carcinoma |
| DTT | differentiated thyroid tumor |
| EGFR | epidermal growth factor receptor |
| EIF1AX | Factor 1A X-Linked |
| EZH1 | zeste 1 polycomb repressive complex 2 subunit |
| FA | follicular adenoma |
| FTC | follicular thyroid carcinoma |
| GNAS | guanine nucleotide binding protein, alpha stimulating |
| HTT | hyalinizing trabecular tumor |
| ITH | intratumoral heterogeneity |
| MADCAM-1 | Mucosal Vascular Address in Cell Adhesion Molecule 1 |
| NF1 | Neurofibromatosis type 1 |
| NGS | next-generation sequencing |
| NIFTP | noninvasive follicular thyroid neoplasm with papillary-like nuclear features |
| NOTCH1 | Notch homolog-1 |
| PAX-8 | paired box gene 8 |
| PDGFRA | platelet-derived growth factor receptor α polypeptide |
| PI3K | Phosphoinositide 3-kinases |
| PPARγ | peroxisome proliferator-activated receptor-γ |
| PTC | papillary thyroid carcinoma |
| PTEN | Phosphatase and tensin homolog |
| RET | REarranged during Transfection |
| H,K,NRA | isoforms of RAS gene family |
| TERT | telomerase reverse transcriptase |
| TSHR | TSH-receptor |
| UMP | uncertain malignant potential tumor |
| WDT-UMP | well-differentiated tumors with uncertain malignant potential |
Author Contributions
Conceptualization, A.I. and G.T.; writing—original draft preparation, A.I., R.V., C.P., S.B. and G.T.; writing—review and editing, A.I., R.V., C.P., S.B. and G.T.; supervision, S.B. and G.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Messina University.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bedard P.L., Hansen A.R., Ratain M.J., Siu L.L. Tumour heterogeneity in the clinic. Nat. Cell Biol. 2013;501:355–364. doi: 10.1038/nature12627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fugazzola L., Muzza M., Pogliaghi G., Vitale M. Intratumoral Genetic Heterogeneity in Papillary Thyroid Cancer: Occurrence and Clinical Significance. Cancers. 2020;12:383. doi: 10.3390/cancers12020383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gandolfi G., Sancisi V., Torricelli F., Ragazzi M., Frasoldati A., Piana S., Ciarrocchi A. Allele Percentage of the BRAF V600E Mutation in Papillary Thyroid Carcinomas and Corresponding Lymph Node Metastases: No Evidence for a Role in Tumor Progression. J. Clin. Endocrinol. Metab. 2013;98:934–942. doi: 10.1210/jc.2012-3930. [DOI] [PubMed] [Google Scholar]
- 4.Schwaederle M., Kurzrock R. Actionability and precision oncology. Oncoscience. 2015;2:779–780. doi: 10.18632/oncoscience.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uzilov A.V., Ding W., Fink M.Y., Antipin Y., Brohl A.S., Davis C., Lau C.Y., Pandya C., Shah H., Kasai Y., et al. Development and clinical application of an integrative genomic approach to personalized cancer therapy. Genome Med. 2016;8:62. doi: 10.1186/s13073-016-0313-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stanta G., Bonin S. Overview on Clinical Relevance of Intra-Tumor Heterogeneity. Front. Med. 2018;5:85. doi: 10.3389/fmed.2018.00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stanta G. Tissue Heterogeneity as a Pre-analytical Source of Variability. Recent Results Cancer Res. 2015;199:35–43. doi: 10.1007/978-3-319-13957-9_4. [DOI] [PubMed] [Google Scholar]
- 8.Stanta G., Jahn S.W., Bonin S., Hoefler G. Tumour heterogeneity: Principles and practical consequences. Virchows Arch. Pathol. Anatom. Physiol. Klin. Med. 2016;469:371–384. doi: 10.1007/s00428-016-1987-9. [DOI] [PubMed] [Google Scholar]
- 9.Masoodi T., Siraj A.K., Siraj S., Azam S., Qadri Z., Albalawy W.N., Parvathareddy S.K., Al-Sobhi S.S., Al-Dayel F., Alkuraya F.S., et al. Whole-Exome Sequencing of Matched Primary and Metastatic PapillaryThyroid Cancer. Thyroid. 2020;30:42–56. doi: 10.1089/thy.2019.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nabi K., Le A. The Intratumoral Heterogeneity of Cancer Metabolism. Adv. Exp. Med. Biol. 2018;1063:131–145. doi: 10.1007/978-3-319-77736-8_10. [DOI] [PubMed] [Google Scholar]
- 11.Tong Y., Gao W.-Q., Liu Y. Metabolic heterogeneity in cancer: An overview and therapeutic implications. Biochim. Biophys. Acta Bioenerg. 2020;1874:188421. doi: 10.1016/j.bbcan.2020.188421. [DOI] [PubMed] [Google Scholar]
- 12.Marusyk A., Janiszewska M., Polyak K. Intratumor Heterogeneity: The Rosetta Stone of Therapy Resistance. Cancer Cell. 2020;37:471–484. doi: 10.1016/j.ccell.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hausser J., Alon U. Tumour heterogeneity and the evolutionary trade-offs of cancer. Nat. Rev. Cancer. 2020;20:247–257. doi: 10.1038/s41568-020-0241-6. [DOI] [PubMed] [Google Scholar]
- 14.González-Silva L., Quevedo L., Varela I. Tumor Functional Heterogeneity Unraveled by scRNA-seq Technologies. Trends Cancer. 2020;6:13–19. doi: 10.1016/j.trecan.2019.11.010. [DOI] [PubMed] [Google Scholar]
- 15.Marusyk A., Almendro V., Polyak K. Intra-tumour heterogeneity: A looking glass for cancer? Nat. Rev. Cancer. 2012;12:323–334. doi: 10.1038/nrc3261. [DOI] [PubMed] [Google Scholar]
- 16.Xu C., Cao H., Shi C., Feng J. The Role Of Circulating Tumor DNA In Therapeutic Resistance. Oncotargets Ther. 2019;12:9459–9471. doi: 10.2147/OTT.S226202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vessoni A.T., Filippi-Chiela E.C., Lenz G., Batista L.F.Z. Tumor propagating cells: Drivers of tumor plasticity, heterogeneity, and recurrence. Oncogene. 2020;39:2055–2068. doi: 10.1038/s41388-019-1128-4. [DOI] [PubMed] [Google Scholar]
- 18.Guo M., Peng Y., Gao A., Du C., Herman J.G. Epigenetic heterogeneity in cancer. Biomark. Res. 2019;7:1–19. doi: 10.1186/s40364-019-0174-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palacios J., Matías-Guiu X., Rodríguez-Peralto J.L., de Álava E., López J.I. Clinical challenges and implications of intratumor heterogeneity. Rev. Esp. Patol. 2019;52:234–241. doi: 10.1016/j.patol.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 20.Haugen B.R., Alexander E.K., Bible K.C., Doherty G.M., Mandel S.J., Nikiforov Y.E., Pacini F., Randolph G.W., Sawka A.M., Schlumberger M., et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26:1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Viola D., Valerio L., Molinaro E., Agate L., Bottici V., Biagini A., Lorusso L., Cappagli V., Pieruzzi L., Giani C., et al. Treatment of advanced thyroid cancer with targeted therapies: Ten years of experience. Endocr. Relat. Cancer. 2016;23:R185–R205. doi: 10.1530/ERC-15-0555. [DOI] [PubMed] [Google Scholar]
- 22.Ieni A., Barresi V., Cardia R., Licata L., Di Bari F., Benvenga S., Tuccari G. The micropapillary/hobnail variant of papillary thyroid carcinoma: A review of series described in the literature compared to a series from one southern Italy pathology institution. Rev. Endocr. Metab. Disord. 2016;17:521–527. doi: 10.1007/s11154-016-9398-4. [DOI] [PubMed] [Google Scholar]
- 23.Vita R., Ieni A., Tuccari G., Benvenga S. The increasing prevalence of chronic lymphocytic thyroiditis in papillary microcarcinoma. Rev. Endocr. Metab. Disord. 2018;19:301–309. doi: 10.1007/s11154-018-9474-z. [DOI] [PubMed] [Google Scholar]
- 24.Mattiuzzi C., Lippi G. Current Cancer Epidemiology. J. Epidemiol. Glob. Health. 2019;9:217–222. doi: 10.2991/jegh.k.191008.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jin S., Borkhuu O., Bao W., Yang Y.-T. Signaling Pathways in Thyroid Cancer and Their Therapeutic Implications. J. Clin. Med. Res. 2016;8:284–296. doi: 10.14740/jocmr2480w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fagin J.A., Wells S.A., Jr. Biologic and Clinical Perspectives on Thyroid Cancer. N. Engl. J. Med. 2016;375:1054–1067. doi: 10.1056/NEJMra1501993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ieni A., Vita R., Magliolo E., Santarpia M., Di Bari F., Benvenga S., Tuccari G. One-third of an Archivial Series of Papillary Thyroid Cancer (Years 2007–2015) Has Coexistent Chronic Lymphocytic Thyroiditis, Which Is Associated with a More Favorable Tumor-Node-Metastasis Staging. Front. Endocrinol. 2017;8:337. doi: 10.3389/fendo.2017.00337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haroon A., Rasheed M.R., Xu B. Molecular Alterations in Thyroid Carcinoma. Surg. Pathol. Clin. 2019;12:921–930. doi: 10.1016/j.path.2019.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tirrò E., Martorana F., Romano C., Vitale S.R., Motta G., Di Gregorio S., Massimino M., Pennisi M.S., Stella S., Puma A., et al. Molecular Alterations in Thyroid Cancer: From Bench to Clinical Practice. Genes. 2019;10:709. doi: 10.3390/genes10090709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kakudo K. How to handle borderline/precursor thyroid tumors in management of patients with thyroid nodules. Gland. Surg. 2018;7:S8–S18. doi: 10.21037/gs.2017.08.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lloyd R.V., McNicoll A. Annual review issue: An overview of 50 years of progress in endocrine pathology. Histopathology. 2018;72:4–5. doi: 10.1111/his.13289. [DOI] [PubMed] [Google Scholar]
- 32.Suster S. Controversies Regarding the Interpretation of Follicular Thyroid Nodules. Arch. Pathol. Lab. Med. 2019;143:1472–1476. doi: 10.5858/arpa.2019-0301-RA. [DOI] [PubMed] [Google Scholar]
- 33.Cameselle-Teijeiro J.M., Eloy C., Sobrinho-Simões M. Pitfalls in Challenging Thyroid Tumors: Emphasis on Differential Diagnosis and Ancillary Biomarkers. Endocr. Pathol. 2020;31:197–217. doi: 10.1007/s12022-020-09638-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baloch Z., Livolsi V.A. Fifty years of thyroid pathology: Concepts and developments. Hum. Pathol. 2020;95:46–54. doi: 10.1016/j.humpath.2019.09.008. [DOI] [PubMed] [Google Scholar]
- 35.Borda A., Zahan A.-E., Piciu D., Barbuș E., Berger N., Nechifor-Boilă A. A 15 year institutional experience of well-differentiated follicular cell-derived thyroid carcinomas; impact of the new 2017 TNM and WHO Classifications of Tumors of Endocrine Organs on the epidemiological trends and pathological characteristics. Endocrinology. 2020;67:630–642. doi: 10.1007/s12020-019-02158-7. [DOI] [PubMed] [Google Scholar]
- 36.Zhu Y., Li Y., Jung C.K., Song D.E., Hang J.-F., Liu Z., Jain D., Lai C.-R., Hirokawa M., Kakudo K., et al. Histopathologic Assessment of Capsular Invasion in Follicular Thyroid Neoplasms-an Observer Variation Study. Endoc. Pathol. 2020;31:132. doi: 10.1007/s12022-020-09620-7. [DOI] [PubMed] [Google Scholar]
- 37.Cracolici V., Ritterhouse L.L., Segal J.P., Puranik R., Wanjari P., Kadri S., Parilla M., Cipriani N.A. Follicular Thyroid Neoplasms: Comparison of Clinicopathologic and Molecular Features of Atypical Adenomas and Follicular Thyroid Carcinomas. Am. J. Surg. Pathol. 2020;44:881–892. doi: 10.1097/PAS.0000000000001489. [DOI] [PubMed] [Google Scholar]
- 38.Chu Y.-H., Sadow P.M. Noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP): Diagnostic updates and molecular advances. Semin. Diagn. Pathol. 2020;37:213–218. doi: 10.1053/j.semdp.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Livolsi V.A., Baloch Z. Noninvasive Follicular Tumor With Papillary-like Nuclear Features: A Practice Changer in Thyroid Pathology. Arch. Pathol. Lab. Med. 2020;30:1–5. doi: 10.5858/arpa.2019-0689-RA. [DOI] [PubMed] [Google Scholar]
- 40.Katsakhyan L., Song S., Lepe M., Shojaei H., Montone K.T., Livolsi V.A., Baloch Z.W. Practice Paradigms Before and After Introduction of the Diagnosis-Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features (NIFTP): An Institutional Experience. Endocr. Pathol. 2020;31:174–181. doi: 10.1007/s12022-020-09614-5. [DOI] [PubMed] [Google Scholar]
- 41.Xu B., Ghossein R.A. Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features (NIFTP): An Update. Head Neck Pathol. 2020;14:303–310. doi: 10.1007/s12105-019-01124-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nikiforov Y.E., Seethala R.R., Tallini G., Baloch Z.W., Basolo F. Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: A paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol. 2016;2:1023–1029. doi: 10.1001/jamaoncol.2016.0386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haugen B.R., Sawka A.M., Alexander E.K., Bible K.C., Caturegli P., Doherty G.M., Mandel S.J., Morris J.C., Nassar A., Pacini F., et al. American Thyroid Association Guidelines on the Management of Thyroid Nodules and Differentiated Thyroid Cancer Task Force Review and Recommendation on the Proposed Renaming of Encapsulated Follicular Variant Papillary Thyroid Carcinoma Without Invasion to Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features. Thyroid. 2017;27:481–483. doi: 10.1089/thy.2016.0628. [DOI] [PubMed] [Google Scholar]
- 44.Rossi E.D., Papotti M., Faquin W., LaRocca L.M., Pantanowitz L. The Diagnosis of Hyalinizing Trabecular Tumor: A Difficult and Controversial Thyroid Entity. Head Neck Pathol. 2020;14:778–784. doi: 10.1007/s12105-019-01083-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jones D.J., Kieliszak C.R., Patel S.S., Selinsky C.R. Hyalinizing trabecular tumor of the thyroid gland and its significant diagnostic issue. Thyroid Res. 2017;10:7. doi: 10.1186/s13044-017-0042-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Saglietti C., Piana S., La Rosa S., Bongiovanni M. Hyalinizing trabecular tumour of the thyroid: Fine-needle aspiration cytological diagnosis and correlation with histology. J. Clin. Pathol. 2017;70:641–647. doi: 10.1136/jclinpath-2017-204360. [DOI] [PubMed] [Google Scholar]
- 47.Jung C.K., Kim Y., Jeon S., Jo K., Lee S., Bae J.S. Clinical utility of EZH1 mutations in the diagnosis of follicular-patterned thyroid tumors. Hum. Pathol. 2018;81:9–17. doi: 10.1016/j.humpath.2018.04.018. [DOI] [PubMed] [Google Scholar]
- 48.Algeciras-Schimnich A., Milosevic D., McIver B., Flynn H., Reddi H.V., Eberhardt N.L., Grebe S.K. Evaluation of the PAX8/PPARG Translocation in Follicular Thyroid Cancer with a 4-Color Reverse-Transcription PCR Assay and Automated High-Resolution Fragment Analysis. Clin. Chem. 2010;56:391–398. doi: 10.1373/clinchem.2009.134015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Basili T., Dopeso H., Kim S.H., Ferrando L., Pareja F., Paula A.D.C., Da Silva E.M., Stylianou A., Maroldi A., Marchiò C., et al. Oncogenic properties and signaling basis of the PAX8-GLIS3 fusion gene. Int. J. Cancer. 2020;147:2253–2264. doi: 10.1002/ijc.33040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Acquaviva G., Visani M., Repaci A., Rhoden K.J., De Biase D., Pession A., Giovanni T. Molecular pathology of thyroid tumours of follicular cells: A review of genetic alterations and their clinicopathological relevance. Histopathology. 2017;72:6–31. doi: 10.1111/his.13380. [DOI] [PubMed] [Google Scholar]
- 51.Duan H., Liu X., Ren X., Zhang H., Wu H., Liang Z. Mutation profiles of follicular thyroid tumors by targeted sequencing. Diagn. Pathol. 2019;14:1–10. doi: 10.1186/s13000-019-0817-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boaventura P., Batista R., Pestana A., Reis M., Mendes A., Eloy C., Sobrinho-Simões M., Soares P. TERT promoter mutations: A genetic signature of benign and malignant thyroid tumours occurring in the context of tinea capitis irradiation. Eur. J. Endocrinol. 2017;176:49–55. doi: 10.1530/EJE-16-0740. [DOI] [PubMed] [Google Scholar]
- 53.Calebiro D., Grassi E.S., Eszlinger M., Ronchi C.L., Godbole A., Bathon K., Guizzardi F., De Filippis T., Krohn K., Jaeschke H. Recurrent EZH1 mutations are a second hit in autonomous thyroid adenomas. J. Clin. Investig. 2016;126:3383–3388. doi: 10.1172/JCI84894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nikiforov Y.E., Nikiforova M.N. Molecular genetics and diagnosis of thyroid cancer. Nat. Rev. Endocrinol. 2011;7:569–580. doi: 10.1038/nrendo.2011.142. [DOI] [PubMed] [Google Scholar]
- 55.Lorusso L., Cappagli V., Valerio L., Giani C., Viola D., Puleo L., Gambale C., Minaldi E., Campopiano M.C., Matrone A., et al. Thyroid Cancers: From Surgery to Current and Future Systemic Therapies through Their Molecular Identities. Int. J. Mol. Sci. 2021;22:3117. doi: 10.3390/ijms22063117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Führer D., Musholt T., Schmid K.W. Molecular Pathogenesis of Thyroid Nodules: Relevance for Clinical Care. Laryngorhinootologie. 2017;96:590–596. doi: 10.1055/s-0043-109180. [DOI] [PubMed] [Google Scholar]
- 57.Nikiforova M.N., Nikitski A.V., Panebianco F., Kaya C., Yip L., Williams M.D., Chiosea S.I., Seethala R.R., Roy S., Condello V., et al. GLIS Rearrangement is a Genomic Hallmark of Hyalinizing Trabecular Tumor of the Thyroid Gland. Thyroid. 2019;29:161–173. doi: 10.1089/thy.2018.0791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sobrinho-Simões M., Preto A., Rocha A.S., Castro P., Máximo V., Fonseca E., Soares P. Molecular pathology of well-differentiated thyroid carcinomas. Virchows Arch. 2005;447:787–793. doi: 10.1007/s00428-005-0065-5. [DOI] [PubMed] [Google Scholar]
- 59.Asa S.L. The Current Histologic Classification of Thyroid Cancer. Endocrinol. Metab. Clin. N. Am. 2019;48:1–22. doi: 10.1016/j.ecl.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 60.Xu B., Ghossein R. Evolution of the histologic classification of thyroid neoplasms and its impact on clinical management. Eur. J. Surg. Oncol. 2018;44:338–347. doi: 10.1016/j.ejso.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Xu B., A Ghossein R. Crucial parameters in thyroid carcinoma reporting—Challenges, controversies and clinical implications. Histopathology. 2018;72:32–39. doi: 10.1111/his.13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Asa S.L. The evolution of differentiated thyroid cancer. Pathology. 2017;49:229–237. doi: 10.1016/j.pathol.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 63.Kakudo K., Bai Y., Liu Z., Li Y., Ito Y., Ozaki T. Classification of thyroid follicular cell tumors: With special reference to borderline lesions [Review] Endocr. J. 2012;59:1–12. doi: 10.1507/endocrj.EJ11-0184. [DOI] [PubMed] [Google Scholar]
- 64.Angell T.E. RAS-positive thyroid nodules. Curr. Opin. Endocrinol. Diabetes Obes. 2017;24:372–376. doi: 10.1097/MED.0000000000000354. [DOI] [PubMed] [Google Scholar]
- 65.Nabhan F., Porter K., Lupo M.A., Randolph G.W., Patel K.N., Kloos R.T. Heterogeneity in Positive Predictive Value of RAS Mutations in Cytologically Indeterminate Thyroid Nodules. Thyroid. 2018;28:729–738. doi: 10.1089/thy.2017.0635. [DOI] [PubMed] [Google Scholar]
- 66.Yoo S.K., Lee S., Kim S.J., Jee H.G., Kim B.A., Cho H., Song Y.S., Cho S.W., Won J.K., Shin J.Y., et al. Comprehensive Analysis of the Transcriptional and Mutational Landscape of Follicular and Papillary Thyroid Cancers. PLoS Genet. 2016;12:e1006239. doi: 10.1371/journal.pgen.1006239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chmielik E., Rusinek D., Oczko-Wojciechowska M., Jarzab M., Krajewska J., Czarniecka A., Jarzab B. Heterogeneity of Thyroid Cancer. Pathobiology. 2018;85:117–129. doi: 10.1159/000486422. [DOI] [PubMed] [Google Scholar]
- 68.The AACR Project GENIE Consortium AACR Project GENIE: Powering precision medicine through an international consortium. Cancer Discov. 2017;7:818–831. doi: 10.1158/2159-8290.CD-17-0151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Xu B., Ghossein R. Poorly differentiated thyroid carcinoma. Semin. Diagn. Pathol. 2020;37:243–247. doi: 10.1053/j.semdp.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 70.Song Y.S., Park Y.J. Genomic Characterization of Differentiated Thyroid Carcinoma. Endocrinol. Metab. 2019;34:1–10. doi: 10.3803/EnM.2019.34.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yoo S.-K., Song Y.S., Park Y.J., Seo J.-S. Recent Improvements in Genomic and Transcriptomic Understanding of Anaplastic and Poorly Differentiated Thyroid Cancers. Endocrinol. Metab. 2020;35:44–54. doi: 10.3803/EnM.2020.35.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Volante M., Rapa I., Gandhi M., Bussolati G., Giachino D., Papotti M., Nikiforov Y.E. RAS Mutations Are the Predominant Molecular Alteration in Poorly Differentiated Thyroid Carcinomas and Bear Prognostic Impact. J. Clin. Endocrinol. Metab. 2009;94:4735–4741. doi: 10.1210/jc.2009-1233. [DOI] [PubMed] [Google Scholar]
- 73.Jalaly J.B., Baloch Z.W. Hürthle-cell neoplasms of the thyroid: An algorithmic approach to pathologic diagnosis in light of molecular advances. Semin. Diagn. Pathol. 2020;37:234–242. doi: 10.1053/j.semdp.2020.03.004. [DOI] [PubMed] [Google Scholar]
- 74.Sugino K., Kameyama K., Ito K., Nagahama M., Kitagawa W., Shibuya H., Ohkuwa K., Uruno T., Akaishi J., Suzuki A., et al. Does Hürthle Cell Carcinoma of the Thyroid Have a Poorer Prognosis than Ordinary Follicular Thyroid Carcinoma? Ann. Surg. Oncol. 2013;20:2944–2950. doi: 10.1245/s10434-013-2965-y. [DOI] [PubMed] [Google Scholar]
- 75.Kim S.K., Yun G.Y., Kim K.H., Park S.K., Choi H.Y., Ha S.K., Park H.C. Severe Hyponatremia Following Radioactive Iodine Therapy in Patients with Differentiated Thyroid Cancer. Thyroid. 2014;24:773–777. doi: 10.1089/thy.2013.0110. [DOI] [PubMed] [Google Scholar]
- 76.Zirilli G., Valenzise M., Dionigi G., Tuccari G., Romeo C., Campennì A., Corrias A., Tuli G., Ieni A., Pajno G.B., et al. Hurthle cell carcinoma in childhood: A retrospective analysis of five cases and review of pediatric literature. Pediatr Blood Cancer. 2020;67:e28300. doi: 10.1002/pbc.28300. [DOI] [PubMed] [Google Scholar]
- 77.Ganly I., Makarov V., Deraje S., Dong Y., Reznik E., Seshan V., Nanjangud G., Eng S., Bose P., Kuo F., et al. Integrated Genomic Analysis of Hürthle Cell Cancer Reveals Oncogenic Drivers, Recurrent Mitochondrial Mutations, and Unique Chromosomal Landscapes. Cancer Cell. 2018;34:256–270. doi: 10.1016/j.ccell.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gopal R.K., Kübler K., Calvo S.E., Polak P., Livitz D., Rosebrock D., Sadow P.M., Campbell B., Donovan S.E., Amin S., et al. Widespread Chromosomal Losses and Mitochondrial DNA Alterations as Genetic Drivers in Hürthle Cell Carcinoma. Cancer Cell. 2018;34:242–255. doi: 10.1016/j.ccell.2018.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kumari S., Adewale R., Klubo-Gwiezdzinska J. The Molecular Landscape of Hürthle Cell Thyroid Cancer Is Associated with Altered Mitochondrial Function—A Comprehensive Review. Cells. 2020;9:1570. doi: 10.3390/cells9071570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Olson E., Wintheiser G., Wolfe K.M., Droessler J., Silberstein P.T. Epidemiology of Thyroid Cancer: A Review of the National Cancer Database, 2000–2013. Cureus. 2019;11:e4127. doi: 10.7759/cureus.4127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hernandez-Prera J.C. The evolving concept of aggressive histological variants of differentiated thyroid cancer. Semin. Diagn. Pathol. 2020;37:228–233. doi: 10.1053/j.semdp.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 82.Póvoa A.A., Teixeira E., Bella-Cueto M.R., Melo M., Oliveira M.J., Sobrinho-Simões M., Maciel J., Soares P. Clinicopathological Features as Prognostic Predictors of Poor Outcome in Papillary Thyroid Carcinoma. Cancers. 2020;12:3186. doi: 10.3390/cancers12113186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nath M.C., Erickson L.A. Aggressive Variants of Papillary Thyroid Carcinoma: Hobnail, Tall Cell, Columnar, and Solid. Adv. Anat. Pathol. 2018;25:172–179. doi: 10.1097/PAP.0000000000000184. [DOI] [PubMed] [Google Scholar]
- 84.Hu J., Yuan I.J., Mirshahidi S., Simental A., Lee S.C., Yuan X. Thyroid Carcinoma: Phenotypic Features, Underlying Biology and Potential Relevance for Targeting Therapy. Int. J. Mol. Sci. 2021;22:1950. doi: 10.3390/ijms22041950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nagayama Y., Mishima H. Heterogenous nature of gene expression patterns in BRAF-like papillarythyroid carcinomas with BRAF(V600E) Endocrine. 2019;66:607–613. doi: 10.1007/s12020-019-02063-z. [DOI] [PubMed] [Google Scholar]
- 86.Colombo C., Muzza M., Proverbio M.C., Tosi D., Soranna D., Pesenti C., Rossi S., Cirello V., De Leo S., Fusco N., et al. Impact of Mutation Density and Heterogeneity on Papillary Thyroid Cancer Clinical Features and Remission Probability. Thyroid. 2019;29:237–251. doi: 10.1089/thy.2018.0339. [DOI] [PubMed] [Google Scholar]
- 87.Ieni A., Vita R., Cardia R., Giuffrè G., Benvenga S., Tuccari G. BRAF Status in Papillary Microcarcinomas of the Thyroid Gland: A Brief Review. Curr. Mol. Med. 2019;19:665–672. doi: 10.2174/1566524019666190717161359. [DOI] [PubMed] [Google Scholar]
- 88.Rangel-Pozzo A., Sisdelli L., Cordioli M.I.V., Vaisman F., Caria P., Mai S., Cerutti J.M. Genetic Landscape of Papillary Thyroid Carcinoma and Nuclear Architecture: An Overview Comparing Pediatric and Adult Populations. Cancers. 2020;12:3146. doi: 10.3390/cancers12113146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Li D.-D., Zhang Y.-F., Xu H.-X., Zhang X.-P. The role of BRAF in the pathogenesis of thyroid carcinoma. Front. Biosci. 2015;20:1068–1078. doi: 10.2741/4359. [DOI] [PubMed] [Google Scholar]
- 90.Zhao L., Wang L., Jia X., Hu X., Pang P., Zhao S., Wang Y., Wang J., Zhang Y., Lyu Z. The Coexistence of Genetic Mutations in Thyroid Carcinoma Predicts Histopathological Factors Associated With a Poor Prognosis: A Systematic Review and Network Meta-Analysis. Front. Oncol. 2020;10:10–540238. doi: 10.3389/fonc.2020.540238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kim K.J., Kim S.G., Tan J., Shen X., Viola D., Elisei R., Puxeddu E., Fugazzola L., Colombo C., Jarzab B., et al. BRAF V600E status may facilitate decision-making on active surveillance of low-risk papillary thyroid microcarcinoma. Eur. J. Cancer. 2020;124:161–169. doi: 10.1016/j.ejca.2019.10.017. [DOI] [PubMed] [Google Scholar]
- 92.Wong K.S., Higgins S.E., Marqusee E., Nehs M.A., Angell T., Barletta J.A. Tall Cell Variant of Papillary Thyroid Carcinoma: Impact of Change in WHO Definition and Molecular Analysis. Endocr. Pathol. 2018;30:43–48. doi: 10.1007/s12022-018-9561-4. [DOI] [PubMed] [Google Scholar]
- 93.Vuong H.G., Long N.P., Anh N.H., Nghi T.D., Hieu M.V., Hung L.P., Nakazawa T., Katoh R., Kondo T. Papillary thyroid carcinoma with tall cell features is as aggressive as tall cellvariant: A meta-analysis. Endocr. Connect. 2018;7:R286–R293. doi: 10.1530/EC-18-0333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Donaldson L.B., Yan F., Morgan P.F., Kaczmar J.M., Fernandes J.K., Nguyen S.A., Jester R.L., Day T.A. Hobnail variant of papillary thyroid carcinoma: A systematic review and meta-analysis. Endocrine. 2020:1–13. doi: 10.1007/s12020-020-02505-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Watutantrige-Fernando S., Vianello F., Barollo S., Bertazza L., Galuppini F., Cavedon E., Censi S., Benna C., Ide E.C., Parisi A., et al. The Hobnail Variant of Papillary Thyroid Carcinoma: Clinical/Molecular Characteristics of a Large Monocentric Series and Comparison with Conventional Histotypes. Thyroid. 2018;28:96–103. doi: 10.1089/thy.2017.0248. [DOI] [PubMed] [Google Scholar]
- 96.Ambrosi F., Righi A., Ricci C., Erickson L.A., Lloyd R.V., Asioli S. Hobnail Variant of Papillary Thyroid Carcinoma: A Literature Review. Endocr. Pathol. 2017;28:293–301. doi: 10.1007/s12022-017-9502-7. [DOI] [PubMed] [Google Scholar]
- 97.Walts A.E., Pao A., Sacks W., Bose S. BRAF genetic heterogeneity in papillary thyroid carcinoma and its metastasis. Hum. Pathol. 2014;45:935–941. doi: 10.1016/j.humpath.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 98.Le Pennec S., Konopka T., Gacquer D., Fimereli D., Tarabichi M., Tomás G., Savagner F., Decaussin-Petrucci M., Trésallet C., Andry G., et al. Intratumor heterogeneity and clonal evolution in an aggressive papillary thyroid cancer and matched metastases. Endocr. Relat. Cancer. 2015;22:205–216. doi: 10.1530/ERC-14-0351. [DOI] [PubMed] [Google Scholar]
- 99.Gawin M., Kurczyk A., Stobiecka E., Frątczak K., Polańska J., Pietrowska M., Widłak P. Molecular Heterogeneity of Papillary Thyroid Cancer: Comparison of Primary Tumors and Synchronous Metastases in Regional Lymph Nodes by Mass Spectrometry Imaging. Endocr. Pathol. 2019;30:250–261. doi: 10.1007/s12022-019-09593-2. [DOI] [PubMed] [Google Scholar]
- 100.Oler G., Ebina K.N., Michaluart P., Kimura E.T., Cerutti J. Investigation of BRAF mutation in a series of papillary thyroid carcinoma and matched-lymph node metastasis reveals a new mutation in metastasis. Clin. Endocrinol. 2005;62:509–511. doi: 10.1111/j.1365-2265.2005.02235.x. [DOI] [PubMed] [Google Scholar]
- 101.Vasko V., Hu S., Wu G., Xing J.C., Larin A., Savchenko V., Trink B., Xing M., Larin O. High Prevalence and Possible de Novo Formation of BRAF Mutation in Metastasized Papillary Thyroid Cancer in Lymph Nodes. J. Clin. Endocrinol. Metab. 2005;90:5265–5269. doi: 10.1210/jc.2004-2353. [DOI] [PubMed] [Google Scholar]
- 102.Chen P., Pan L., Huang W., Feng H., Ouyang W., Wu J., Wang J., Deng Y., Luo J., Chen Y. BRAF V600E and lymph node metastases in papillary thyroid cancer. Endocr. Connect. 2020;9:999–1008. doi: 10.1530/EC-20-0420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Guerra A., Fugazzola L., Marotta V., Cirillo M., Rossi S., Cirello V., Forno I., Moccia T., Budillon A., Vitale M. A High Percentage of BRAFV600E Alleles in Papillary Thyroid Carcinoma Predicts a Poorer Outcome. J. Clin. Endocrinol. Metab. 2012;97:2333–2340. doi: 10.1210/jc.2011-3106. [DOI] [PubMed] [Google Scholar]
- 104.Guerra A., Sapio M.R., Marotta V., Campanile E., Rossi S., Forno I., Fugazzola L., Budillon A., Moccia T., Fenzi G., et al. The primary occurrence of BRAF(V600E) is a rare clonal event in papillary thyroid carcinoma. J. Clin. Endocrinol. Metab. 2012;97:517–524. doi: 10.1210/jc.2011-0618. [DOI] [PubMed] [Google Scholar]
- 105.Khan M.S., Qadri Q., Makhdoomi M.J., A Wani M., A Malik A., Niyaz M., Masoodi S.R., I Andrabi K., Ahmad R., Mudassar S. RET/PTC Gene Rearrangements in Thyroid Carcinogenesis: Assessment and Clinico-Pathological Correlations. Pathol. Oncol. Res. 2020;26:507–513. doi: 10.1007/s12253-018-0540-3. [DOI] [PubMed] [Google Scholar]
- 106.Staubitz J.I., Schad A., Springer E., Rajalingam K., Lang H., Roth W., Hartmann N., Musholt T.J. Novel rearrangements involving the RET gene in papillary thyroid carcinoma. Cancer Genet. 2019;230:13–20. doi: 10.1016/j.cancergen.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 107.Yakushina V.D., Lerner L.V., Lavrov A.V. Gene Fusions in Thyroid Cancer. Thyroid. 2018:158–167. doi: 10.1089/thy.2017.0318. [DOI] [PubMed] [Google Scholar]
- 108.Cordioli M.I., Moraes L., Bastos A.U., Besson P., Alves M.T., Delcelo R., Monte O., Longui C., Cury A.N., Cerutti J.M. Fusion Oncogenes Are the Main Genetic Events Found in Sporadic PapillaryThyroid Carcinomas from Children. Thyroid. 2017;27:182–188. doi: 10.1089/thy.2016.0387. [DOI] [PubMed] [Google Scholar]
- 109.Prasad M.L., Vyas M., Horne M.J., Virk R.K., Morotti R., Liu Z., Tallini G., Nikiforova M.N., Christison-Lagay E.R., Udelsman R., et al. NTRK fusion oncogenes in pediatric papillary thyroid carcinoma in northeast United States. Cancer. 2016;122:1097–1107. doi: 10.1002/cncr.29887. [DOI] [PubMed] [Google Scholar]
- 110.Iglesias M.L., Schmidt A., Al Ghuzlan A., Lacroix L., De Vathaire F., Chevillard S., Schlumberger M. Radiation exposure and thyroid cancer: A review. Arch. Endocrinol. Metab. 2017;61:180–187. doi: 10.1590/2359-3997000000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ciampi R., Nikiforov Y.E. Alterations of the BRAF Gene in Thyroid Tumors. Endocr. Pathol. 2005;16:163–172. doi: 10.1385/EP:16:3:163. [DOI] [PubMed] [Google Scholar]
- 112.Nozaki Y., Yamamoto H., Iwasaki T., Sato M., Jiromaru R., Hongo T., Yasumatsu R., Oda Y. Clinicopathological features and immunohistochemical utility of NTRK-, ALK-, and ROS1-rearranged papillary thyroid carcinomas and anaplastic thyroid carcinomas. Hum. Pathol. 2020;106:82–92. doi: 10.1016/j.humpath.2020.09.004. [DOI] [PubMed] [Google Scholar]
- 113.Chou A., Fraser S., Toon C.W., Clarkson A., Sioson L., Farzin M., Cussigh C., Aniss A., O’Neill C., Watson N., et al. A Detailed Clinicopathologic Study of ALK-translocated Papillary Thyroid Carcinoma. Am. J. Surg. Pathol. 2015;39:652–659. doi: 10.1097/PAS.0000000000000368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Park J.Y., Kim W.Y., Hwang T.S., Lee S.S., Kim H., Han H.S., Lim S.D., Kim W.S., Yoo Y.B., Park K.S. BRAF and RAS Mutations in Follicular Variants of Papillary Thyroid Carcinoma. Endocr. Pathol. 2013;24:69–76. doi: 10.1007/s12022-013-9244-0. [DOI] [PubMed] [Google Scholar]
- 115.Schopper H.K., Stence A., Ma D., A Pagedar N., A Robinson R. Single thyroid tumour showing multiple differentiated morphological patterns and intramorphological molecular genetic heterogeneity. J. Clin. Pathol. 2016;70:116–119. doi: 10.1136/jclinpath-2016-203821. [DOI] [PubMed] [Google Scholar]
- 116.Cipriani N.A., Agarwal S., Dias-Santagata D., Faquin W.C., Sadow P.M. Clear Cell Change in Thyroid Carcinoma: A Clinicopathologic and Molecular Study with Identification of Variable Genetic Anomalies. Thyroid. 2017;27:819–824. doi: 10.1089/thy.2016.0631. [DOI] [PubMed] [Google Scholar]
- 117.Mancikova V., Buj R., Castelblanco E., Inglada-Pérez L., Diez A., De Cubas A.A., Curras-Freixes M., Maravall F.X., Mauricio D., Matias-Guiu X., et al. DNA methylation profiling of well-differentiated thyroid cancer uncovers markers of recurrence free survival. Int. J. Cancer. 2013;135:598–610. doi: 10.1002/ijc.28703. [DOI] [PubMed] [Google Scholar]
- 118.Carter S.L., Cibulskis K., Helman E., McKenna A., Shen H., Zack T., Laird P.W., Onofrio R.C., Winckler W., Weir B.A., et al. Absolute quantification of somatic DNA alterations in human cancer. Nat. Biotechnol. 2012;30:413–421. doi: 10.1038/nbt.2203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Oh B.Y., Shin H.-T., Yun J.W., Kim K.-T., Kim J., Bae J.S., Cho Y.B., Lee W.Y., Yun S.H., Park Y.A., et al. Intratumor heterogeneity inferred from targeted deep sequencing as a prognostic indicator. Sci. Rep. 2019;9:4542. doi: 10.1038/s41598-019-41098-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Khatami F., Larijani B., Nikfar S., Hasanzad M., Fendereski K., Tavangar S.M. Personalized treatment options for thyroid cancer: Current perspectives. Pharm. Pers. Med. 2019;12:235–245. doi: 10.2147/PGPM.S181520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Campennì A., Barbaro D., Guzzo M., Capoccetti F., Giovanella L. Personalized management of differentiated thyroid cancer in real life—practical guidance from a multidisciplinary panel of experts. Endocrines. 2020;70:280–291. doi: 10.1007/s12020-020-02418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Nishino M. Sustainable cytopathology in the precision medicine era: Exploring new sources for molecular testing in thyroid cytology specimens. Cancer Cytopathol. 2019;127:143–145. doi: 10.1002/cncy.22107. [DOI] [PubMed] [Google Scholar]
- 123.Ramón Y Cajal S., Hümmer S., Peg V., Guiu X.M., De Torres I., Castellvi J., Martinez-Saez E., Hernandez-Losa J. Integrating clinical, molecular, proteomic and histopathological data within the tissue context: Tissunomics. Histopathology. 2019;75:4–19. doi: 10.1111/his.13828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ramón Y Cajal S., Sesé M., Capdevila C., Aasen T., De Mattos-Arruda L., Diaz-Cano S.J., Hernández-Losa J., Castellví J. Clinical implications of intratumor heterogeneity: Challenges and opportunities. J. Mol. Med. 2020;98:161–177. doi: 10.1007/s00109-020-01874-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.