Abstract
β-Lactam antibiotics target penicillin-binding proteins and inhibit the synthesis of peptidoglycan, a crucial step in cell wall biosynthesis. Staphylococcus aureus acquires resistance against β-lactam antibiotics by producing a penicillin-binding protein 2a (PBP2a), encoded by the mecA gene. PBP2a participates in peptidoglycan biosynthesis and exhibits a poor affinity towards β-lactam antibiotics. The current study was performed to determine the diversity and the role of missense mutations of PBP2a in the antibiotic resistance mechanism. The methicillin-resistant Staphylococcus aureus (MRSA) isolates from clinical samples were identified using phenotypic and genotypic techniques. The highest frequency (60%, 18 out of 30) of MRSA was observed in wound specimens. Sequence variation analysis of the mecA gene showed four amino acid substitutions (i.e., E239K, E239R, G246E, and E447K). The E239R mutation was found to be novel. The protein-ligand docking results showed that the E239R mutation in the allosteric site of PBP2a induces conformational changes in the active site and, thus, hinders its interaction with cefoxitin. Therefore, the present report indicates that mutation in the allosteric site of PBP2a provides a more closed active site conformation than wide-type PBP2a and then causes the high-level resistance to cefoxitin.
Keywords: mutation, mecA, methicillin-resistant Staphylococcus aureus, allosteric site, PBP2a
1. Introduction
Infections by methicillin-resistant Staphylococcus aureus (MRSA) are considered a pivotal global health issue. The MRSA isolate first emerged in the United Kingdom in 1961 and quickly spread globally [1]. MRSA is able to spread both in hospitals and within the community [2,3]. S. aureus infects skin glands, intact skin, nasal cavity, and intestinal mucosa, which can lead to bacteremia, pneumonia, or wound and bone infections [3,4,5]. MRSA acquires resistance against β-lactam antibiotics via a penicillin-binding protein 2a (PBP2a) [6]. PBP2a (a monofunctional transpeptidase) has a low affinity for β-lactam antibiotics and thus cannot be inhibited by these antibiotics [6]. MRSA clinical isolates become resistant to a number of antibiotic classes (e.g., fluoroquinolones, macrolides, aminoglycosides, and clindamycin) and β-lactam antibiotics [3]. These additional resistance mechanisms are due to mutations and acquired resistance determinants, along with the formation of biofilm. Therefore, the MRSA isolates are multidrug-resistant (MDR) pathogens, which is a major cause of mortality and morbidity globally [3]. In MRSA, PBP2a shows catalytic activity in peptidoglycan biosynthesis (eventually, biosynthesis of the MRSA cell wall) in cooperation with the transglycosylase activity of other PBPs, such as PBP2 [1,7,8]. The peptidoglycan polymer consists of glycan strands comprised of a repeating disaccharide unit (N-acetylglucosamine (GlcNAc) and N-acetylmuramylpentapeptide (MurNAc pentapeptide): GlcNAc–MurNAc pentapeptide) [1]. The adjacent glycan strands are cross-linked by the transpeptidase activity of PBP2a using peptide stems present on each MurNAc saccharide. The cell wall encases the entire MRSA in a single molecule, and its integrity is essential to the survival of MRSA. The PBP2a is encoded by the mecA gene carried by a mobile genetic element, and the staphylococcal cassette chromosome mec (SCCmec) is present on the chromosomes of MRSA strains [9]. Currently, thirteen allotypes of SCCmec (namely type I–XIII) have been defined. Among the thirteen SCCmec allotypes, the only rare allotype (type XI) contains the mecC gene instead of the mecA gene [3]. Furthermore, PBP2x shows cefuroxime resistance in Streptococcus pneumoniae [10]. Generally, the mecA gene is considered an essential genotypic characteristic of MRSA and the target gene for rapid diagnosis of MRSA infections [11] while the nuc gene (S. aureus-specific chromosomal gene encoding thermonuclease) is used for the rapid detection of overall S. aureus (both MSSA (methicillin-sensitive S. aureus) and MRSA) from clinical samples [12].
Point mutations in the mecA gene likely affect the function of the mecA-encoded PBP2a, leading to a change in the methicillin resistance activity [10]. Different previous studies have reported mutations in mecI and mecA, but few data were able to establish the correlation between mutations in such genes and resistance to β-lactam antibiotics [13]. Ceftaroline, a recently introduced anti-MRSA β-lactam antibiotic, binds noncovalently to the allosteric site of PBP2a, which creates a conformational change to allow for opening of the active site. Then, a second ceftaroline binds to the now opened active site, thus inhibiting the transpeptidase function of PBP2a [1,14]. However, mutations in the allosteric site disrupts the allosteric opening and may play a vital role in creating resistance against ceftaroline. Previously, mutations in the allosteric site (N146K, E150K, and E239K) of PBP2a have been shown to have low-level resistance against ceftaroline [14,15]. Another study reported the N146K-N204K-G246E triple mutant having high rates of resistance to anti-MRSA β-lactam antibiotics such as ceftaroline and ceftobiprole [16]. A high-level of resistance to ceftaroline was observed in the MRSA isolates carrying the Y446N-E447K double mutation in the active site region of PBP2a [17].
There is very limited data available on the mecA genetic polymorphisms, particularly, in the allosteric site of the PBP2a in clinical MRSA isolates showing high-level resistance to cefoxitin. In the current study, we investigated the genetic polymorphism of the mecA gene in clinical MRSA isolates from different specimens of district Lahore, Pakistan. We further determined the probable role of the observed novel mutation in the allosteric site of PBP2a in antibiotic resistance by protein modeling and protein-ligand docking.
2. Results
2.1. Characteristics of S. aureus Isolates
In the current study, 33 S. aureus were phenotypically isolated from clinical samples (blood, nasal swab, wound, etc.) from Lahore (isolation sites: Main Boulevard, Zarar Shaheed Road, Lahore Road, and Link Road), Pakistan. These 33 isolates were nuc-positive and were further confirmed as S. aureus through 16 s ribotyping.
2.2. Characteristics of MRSA Isolates
Of the 33 S. aureus, 30 isolates were found to be resistant to cefoxitin (Table 1) and to be mecA-positive. Therefore, these 30 isolates are MRSAs because polymerase chain reaction (PCR) amplification of the mecA gene and cefoxitin resistance determined by disk diffusion tests are considered a gold standard method for the rapid detection of MRSA infections [18,19]. Of the 30 MRSA, three isolates (MR-13, -14, and -33) demonstrated high-level cefoxitin resistance with inhibition zone diameters ranging from 3 mm to 4 mm (Table 1) and high minimum inhibitory concentrations (MICs) (≥64 mg/L) (Table 2). The remaining seventeen MRSA isolates revealed low-level cefoxitin resistance with inhibition zone diameters ranging from 13 mm to 20 mm (Table 1).
Table 1.
The antimicrobial disk susceptibility tests with cefoxitin 30 µg disks.
| Staphylococcus aureus Isolate | Zone Diameter (mm) | Interpretive Category a |
|---|---|---|
| MR-1 | 13 | R |
| MR-2 | 20 | R |
| MR-3 | 13 | R |
| MR-4 | 13 | R |
| MR-5 | 16 | R |
| MR-6 | 13 | R |
| MR-7 | 13 | R |
| MR-8 | 17 | R |
| MR-9 | 16 | R |
| MR-10 | 15 | R |
| MR-11 | 20 | R |
| MR-12 | 19 | R |
| MR-13 | 4 | R |
| MR-14 | 4 | R |
| MR-15 | 34 | S |
| MR-16 | 13 | R |
| MR-17 | 16 | R |
| MR-18 | 13 | R |
| MR-19 | 14 | R |
| MR-20 | 23 | S |
| MR-21 | 17 | R |
| MR-22 | 17 | R |
| MR-23 | 18 | R |
| MR-24 | 16 | R |
| MR-25 | 15 | R |
| MR-26 | 14 | R |
| MR-27 | 18 | R |
| MR-28 | 29 | S |
| MR-29 | 17 | R |
| MR-30 | 14 | R |
| MR-31 | 16 | R |
| MR-32 | 17 | R |
| MR-33 | 3 | R |
a The inhibition zone diameters were interpreted using the Clinical Laboratory Standards Institute (CLSI) breakpoints [20].
Table 2.
The missense mutations of PBP2a associated with the resistance to cefoxitin.
| Site/Source | B | N | W |
|---|---|---|---|
| MRSA isolate | MR-13 | MR-14 | MR-33 |
| Amino acid change(s) of PBP2a | E239K | G246E |
E239R E447K |
| Cefoxitin MIC (mg/L) | 64 | 64 | 128 |
B, blood; N, nasal swab; W, wound sample. MRSA, methicillin-resistant Staphylococcus aureus; PBP2a, penicillin-binding protein 2a; MIC, minimum inhibitory concentration. E239R is the novel mutation of PBP2a.
The prevalence of MRSA from the different clinical samples was different. The highest frequency (60%, 18 out of 30) of MRSA was observed in wound specimens. Furthermore, the frequencies of MRSA from blood specimens, nasal swabs, and ear swabs were 23% (n = 7), 10% (n = 3), and 7% (n = 2).
2.3. Genetic Polymorphism of mecA Gene
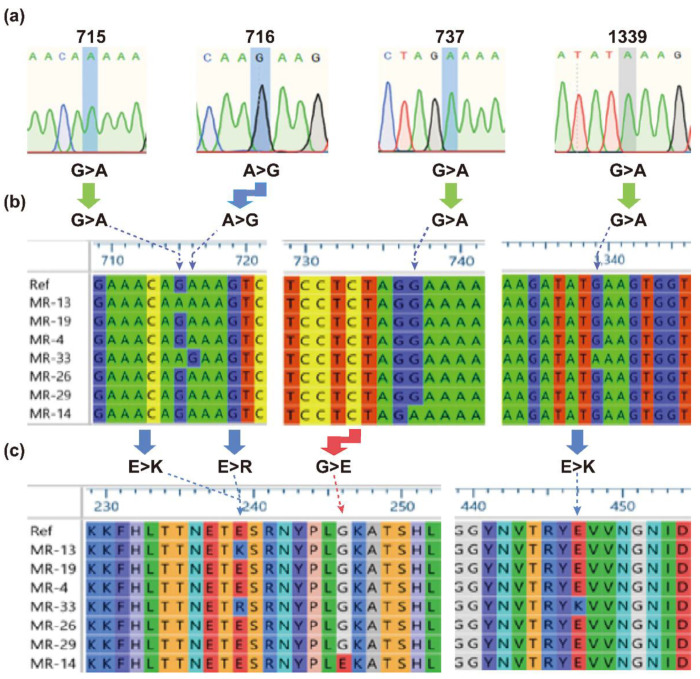
To find genetic polymorphism in the mecA gene, the mecA coding sequences of the MRSA isolates were subjected to alignment with a reference sequence from MRSA strain N315. The multiple DNA sequence alignment (Figure 1a,b) showed nucleotide substitutions at five different positions (i.e., 75, 715, 716, 737, and 1339). All of the mutations were responsible for the amino acid substitutions except for a silent mutation at position 75 (Figure 1).
Figure 1.
The detected variations in the mecA gene in the MRSA isolates (MR-13, -19, -4, -33, -26, -29, and -14). (a) Chromatograms showing nucleotide substitutions at different locations. (b) Multiple DNA sequence alignment. (c) Multiple protein sequence alignment. The sign “>” represents a substitution mutation. The left “E>K”, “E>R”, “G>E”, and the right “E>K” refer to E239K, E239R, G246E, and E447K, as shown by the dashed arrows. The left “G>A”, “A>G”, and “G>A”, and the right “G>A” refer to G715A, A716G, G737A, and G1339A. “Ref” represents the reference sequence (GenBank accession no. NC_002745). The MRSA isolates (MR-13, -14, and -33) show amino acid substitution(s) in PBP2a.
The amino acid substitutions (E239K, E239R, and G246K) took place at the active site of PBP2a and the fourth amino acid (E447K) was replaced at the allosteric site. The mutations (E239K, G246K, and E447K) from the three MRSA isolates (MR-13, -14, and 33) showing cefoxitin resistance with high MICs (≥64 mg/L) (Table 2) were reported to be involved in mediating the resistance to ceftaroline [15,16,17]. However, the E239R mutation (with additional E447K) demonstrating high-level resistance to cefoxitin (Table 2) is reported for the first time in this study. Therefore, the structural features of E239R in mediating the high-level resistance were investigated.
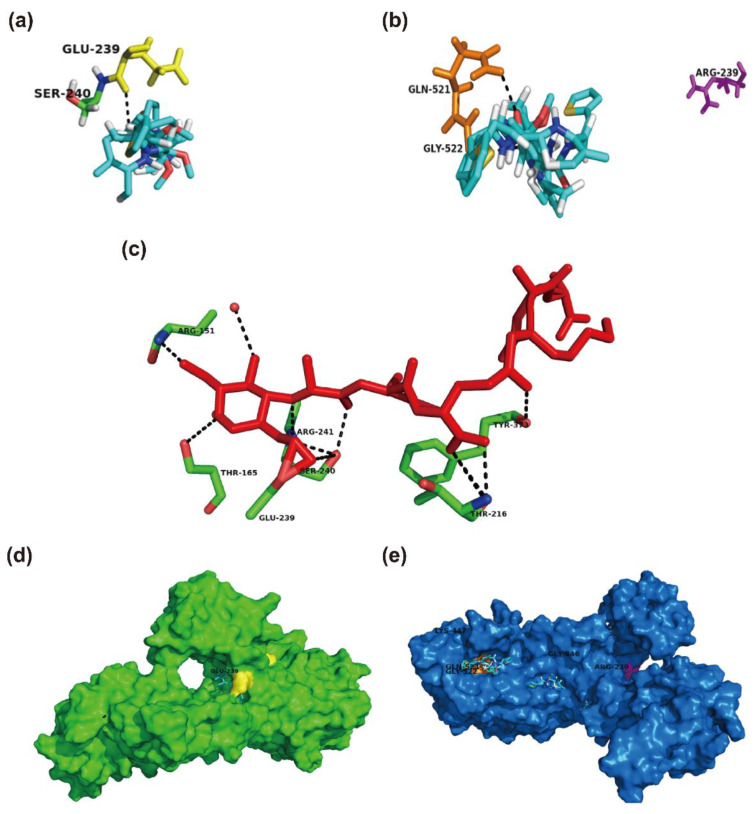
2.4. Structural Perspective of PBP2a with E239R Mutation on Cefoxitin Resistance
In order to assess the role of missense mutations in the structure and function (cefoxitin resistance) of PBP2a, we performed protein-ligand docking. The amino acid substitutions at positions 239 and 246 lie in the allosteric site of the non-penicillin-binding domain (allosteric domain), while E447K mutation exits from the active site of the transpeptidase domain of PBP2a [14]. Y446 and E447 lie within the active site of PBP2a [21]. Therefore, the Y446N and E447K mutants mediate resistance to ceftaroline [14,17]. However, the structural role of the mutation at E239 located in the allosteric site of PBP2a has not been clearly explained. The protein-ligand docking results showed that cefoxitin interacts directly with E239 at the allosteric site of wide-type PBP2a (Figure 2a). Furthermore, E239 is shown to be directly involved in the interaction with peptidoglycan (Figure 2c). However, the mutant PBP2a with E239R mutation has not shown any binding interactions with cefoxitin, as shown in Figure 2b. Furthermore, a ligand such as cefoxitin is positioned at E239 in the wild-type PBP2a (Figure 2d), while it is positioned away from R239 in the mutant PBP2a (Figure 2e). The mutation of glutamate at position 239 into arginine results in changing negatively charged side chains into positively charged R-groups. These results suggest that E239R mutation decreases the binding affinity of cefoxitin for arginine at the corresponding position and thus confers resistance to cefoxitin. The docking results showed that the binding affinity (−4.1 kcal/mol, the free energy of binding) of cefoxitin for the E239R mutant is lower than the binding affinity (−5.4 kcal/mol) of cefoxitin for the wild-type PBP2a, which indicates that cefoxitin has a lower affinity for the mutant PBP2a.
Figure 2.
The protein-ligand docking of cefoxitin with the wild-type PBP2a and E239R-mutant PBP2a of MRSA. (a) Cefoxitin (shown in capped sticks with carbon in cyan, oxygen in red, nitrogen in blue, and sulfur in yellow) interacts with the Glu-239 (E239, yellow) of the wild-type PBP2a. The docked ligand trajectory shows that cefoxitin is located in close proximity to E239. (b) Cefoxitin interacts with Gln-521 (orange) and Gly-522 (orange) instead of Arg-239 (R239, pink) in the E239R-mutant PBP2a. (c) Peptidoglycan (red, GlcNAc-MurNAc pentapeptide) interacts with E239 and other residues of the wild-type PBP2a. (d) Surface representation of the wild-type PBP2a (green) showing that the ligand (shown in caped sticks) is positioned at the allosteric site (yellow). (e) The ligand (shown in capped sticks) is pointed away from the allosteric site (pink) in the E239R-mutant PBP2a. All of the interactions are shown as black dashed lines. Glu, glutamic acid; Ser, serine; Gln, glutamine; Gly, glycine; Arg, arginine; Thr, threonine; Tyr, tyrosine; Lys, lysine.
3. Discussion
All 33 S. aureus clinical isolates demonstrated successful amplification of the nuc gene and were further confirmed as S. aureus through 16s ribotyping, which indicates high specificity for the rapid PCR detection of S. aureus through amplifying the nuc gene. The other reports were in accordance with our observations of the high specificity of the nuc gene in S. aureus for identification purposes [12,22]. In addition, all 30 mecA-positive MRSA isolates were found to be resistant to cefoxitin. These data suggest that the cefoxitin disk-diffusion (CFD) method is a sensitive phenotypic testing used for the identification of MRSA, as previously reported [18]. This CDF method is able to avoid misdiagnosis that could be the significant factor for the emergence of infections with MRSA [23] and could lead to the development of resistance against other important available antibiotics. A study from Pakistan reported that 22% of the clinical isolates were misdiagnosed as MRSA [24]. Many factors influence the accuracy of the MRSA diagnosis: symptomology, type of laboratory test used, and the effectiveness of the utilized tests [25]. Such a misdiagnosis emphasizes the use of specific, rapid, and sensitive techniques for epidemiological and therapeutic studies.
The highest frequency of MRSA was observed in wound specimens. Similar studies from Pakistan and India have reported the highest prevalence of MRSA from wound specimens [26,27]. The highest frequency of MRSA from wounds could be due to its presence on the skin as normal flora. The frequency of MRSA from blood specimens was 23% (n = 7), which is greater than the previously reported study showing that 12% MRSA are found in blood specimens, followed by at the wound source (26%) [28]. The frequency of MRSA from nasal swabs was 10% (n = 3), which is in good agreement with the previously reported data from Pakistan [29]. The frequency of MRSA from ear swabs was 7% (n = 2), which is lower than the frequencies (27–41%) that were reported previously [29,30]. However, the sample size was so small that we were not able to draw a clear epidemiological aspect of MRSA showing the resistance to cefoxitin in Pakistan.
In our study, four different missense mutations were detected within PBP2a in MRSA MR-13, MR-14, and MR-33 clinical isolates. Three of the four missense mutations have been described as a contributor of antibiotic resistance in other countries: E239K (Spain [15], Thailand [15], and the United States [17]), G246E (Africa [16], Greece [15], and Switzerland [31]), and E447K (the United States [17]). As far as we know, the E239R missense mutation has not been reported yet, but seems to be present in Pakistan. Our data showed that the E239R-E447K double mutant rendered MRSA MR-33 highly resistant to cefoxitin (MIC of 128 mg/L). The MRSA isolates harboring the Y446N-E447K double mutation at the active site region of PBP2a showed high-level resistance (MIC > 32 mg/L) to ceftaroline [17]. It was suggested that the Y446N mutation in the Y446N-E447K double mutant PBP2a is the main contributor of the high-level resistance [17], which agrees with the previous structural studies that implicated Y446N as the gatekeeper to the active site of the transpeptidase domain [14]. Furthermore, the E447K mutation may be a minor contributor stabilizing the Y446N-E447K double mutant (or facilitating the transpeptidation reaction) [17]. According to these results, the most likely cause of the high-level resistance to cefoxitin may be the E239R mutation in the E239R-E447K double mutant PBP2a, although isogenic mutants were not tested to confirm this suggestion.
It has been shown that the PBP2a-mediated β-lactam resistance in MRSA is imparted by the weaker binding of β-lactam antibiotics to the closed PBP2a transpeptidase (TP) pocket (the closed active site) in the TP domain [14,15]. Therefore, PBP2a allows MRSA to maintain TP activity in the presence of β-lactam antibiotics. The closed active site is why 17 MRSA clinical isolates showed low-level cefoxitin resistance with inhibition zone diameters ranging from 13 mm to 20 mm. However, PBP2a relies on PBP2 for the transglycosylase (TG) activity because it does not have any TG activity [15]. The experimental evidence demonstrated that cooperative functions between PBP2a and PBP2 exist in MRSA peptidoglycan biosynthesis and that these cooperative functions are achieved through a direct protein–protein interaction between PBP2a and PBP2 [15]. The structural studies identified an allosteric site 60 Å away from the active site of PBP2a [14]. Ceftaroline (or peptidoglycan) binds to the allosteric site, which is consistent with the structural data of S. pneumoniae PBP2x [10]. When the allosteric site of PBP2a is bound by the ligand such as ceftaroline (or peptidoglycan), a conformational change allows for opening of the active site (allosteric opening), which permits ligand (ceftaroline) entry, facilitates ceftaroline binding at the active site, and eventually inhibits TP activity [14,17].
The missense mutations at the allosteric site of PBP2a impart three traits on the mutant PBP2a in MRSA clinical isolates showing resistance to ceftaroline [1,14]: (1) these mutations not only created new salt-bridges (not present in the wild-type PBP2a) around the mutated residues but also established a new salt-bridge network among many residues 35 Å away from the mutated positions (but the salt-bridge observed in the wild-type PBP2a is not detected in the mutant PBP2a); (2) missense mutations change the electrostatic potential in the allosteric site, showing a marked basic character extending beyond the immediate position of the mutated residues; and (3) these mutations decrease the second-order rate constant for the acylation in the active site, which indicates that the acylation event becomes more unfavorable. Due to these structural traits (alterations), the missense mutations at the allosteric site of PBP2a disrupt the allosteric opening and these mutations create a more closed active site conformation, which may play a vital role in creating high-level resistance to cefoxitin and ceftaroline. Furthermore, this antibiotic resistance mechanism is consistent with the protein-ligand docking data of the E239R mutant in MRSA isolates, which shows high-level resistance to cefoxitin.
In conclusion, the CDF method along with PCR amplification of the mecA gene may be a sensitive technique for the detection of MRSA infections. The E239R mutation at the allosteric site of PBP2a results in the unfavorable positioning of the amino acid R-group for binding to cefoxitin at the corresponding position. Therefore, the E239R mutation provides the favorable conformation of PBP2a for the interaction with peptidoglycan even in the presence of cefoxitin with a lower affinity for the mutant PBP2a. Overall, a missense mutation at the allosteric site of PBP2a plays a vital role in providing antibiotic resistance to MRSA. These results can be useful both in the understanding of the development of antibiotic resistance and the design of new anti-MRSA antibiotics.
4. Materials and Methods
4.1. Bacterial Isolates
A total of 33 S. aureus isolates were isolated from the clinical samples of the Citi Lab and Research Centre (Medical Laboratory, Lahore, Pakistan) in 2019. The confirmed MRSA isolates were stored at −80 °C in 20% glycerol. The MRSA isolates were cultivated on nutrient agar (Oxoid, Hampshire, UK) and mannitol salt agar (Oxoid, Hampshire, UK).
4.2. Identification of S. aureus from Clinical Samples
S. aureus was isolated phenotypically from the clinical samples using a previously reported method [32,33]. Furthermore, the molecular detection of S. aureus was performed by PCR amplification of the nuc gene with Fnuc and Rnuc primers (Table 3) [34]. The expected PCR product of 270 bp was verified by agarose gel electrophoresis (Figure S1). S. aureus harboring the nuc gene was subjected to PCR amplification of the 16Sr DNA fragment using 16sF and 16sR primers (Table 3). The amplified PCR products were sequenced using a previously reported method [35]. The DNA sequence analysis was carried out through MEGA-X (www.megasoftware.net; accessed on 29 April 2021) and BLAST (https://blast.ncbi.nlm.nih.gov/Blast.cgi; accessed on 29 April 2021).
Table 3.
The primers used for PCR amplification and DNA sequencing.
| Primer Name | Primer Sequence (5′→3′) | Reference |
|---|---|---|
| Fnuc | GCGATTGATGGTGATACGGTT | This study |
| Rnuc | AGCCAAGCCTTGACGAACTAAAGC | This study |
| 16sF | AGAGTTTGATCCTTGGCTAG | This study |
| 16sR | GCYTACCTTGTTACGACTT | This study |
| mecA_DF | AAAATCGATGGTAAAGGTTGGC | This study |
| mecA_DR | AGTTCTGCAGTACCGGATTTGC | This study |
| MF | AACCGAAGAAGTCGTGTCAG | This study |
| MR | CATCGTTACGGATTGCTTCG | |
| MecAR4 | GATACATTCTTTGGAACGATG | [36] |
| MecAF5 | ACAAGATGATACCTTCGTTCCACTT | |
| MecAF3 | GAAGATGGCTATCGTGTCAC | |
| MecAF4 | GGTAATATCGACTTAAAACAAG |
4.3. Antimicrobial Susceptibility Testing
The antimicrobial susceptibility was tested by the Clinical Laboratory Standards Institute (CLSI) disk-diffusion method [20] on Müeller–Hinton agar with cefoxitin 30 µg disks (Oxoid). The plates were incubated for 24 h at 35 °C before measuring the inhibition zone diameters. S. aureus ATCC 25923 was included as a control strain. The inhibition zone diameters were interpreted using the CLSI criteria [20]. In the disk-diffusion method performed using a 30 µg cefoxitin disc, an inhibition zone diameter is considered methicillin resistant when ≤21 mm and is reported as methicillin sensitive when ≥22 mm. All MRSA isolates that demonstrated resistance to cefoxitin (Table 1) were further characterized as indicated below. Furthermore, MIC was determined by the broth microdilution method [37] for three MRSA isolates containing amino acid substitutions in PBP2a (Table 2).
4.4. Molecular Detection of mecA Gene
All of the MRSA isolates were confirmed by mecA gene detection through PCR amplification using mecA_DF and mecA_DR primers (Table 3). These forward and reverse primers were designed to amplify a highly conserved fragment of the mecA gene. The DNA was extracted using the QIAamp DNA Mini Kit (QIAGEN, Valencia, CA, USA), in accordance with the manufacturer’s protocol. The PCR amplifications were carried out on a DNA thermal cycler (mod. 2400, Perkin–Elmer Cetus, Norwalk, CT, USA) as previously described [38]. The DNA isolated from the MRSA isolates was subjected to PCR using the following conditions: initial denaturation for 4 min at 94 °C, followed by 30 cycles of denaturation at 94 °C for 30 s, annealing at 55 °C for 30 s, and extension for 1 min at 72 °C. Final extension was performed for 15 min at 72 °C. The expected PCR product of 533 bp was verified by agarose gel electrophoresis (Figure S2).
4.5. Genetic Polymorphism of mecA Gene
In order to determine the genetic polymorphism in the mecA gene, the entire mecA region including the mecA coding sequence was amplified from the MRSA isolates using MF and MR primers (Table 3). The primers were designed to amplify the complete gene sequence of the mecA gene from the complete genome sequences of MRSA (GenBank accession numbers CP039164 and NC_002745). The PCR amplification was performed with an initial denaturation at 94 °C for 5 min and 30 cycles of denaturation at 94 °C for 30 s, annealing at 56 °C for 30 s, and extension at 72 °C for 2 min. The final extension was performed at 72 °C for 20 min. The amplicon (2368 bp, Figure S3) was sequenced using the previously reported primers [36] and the newly designed primers (Table 3). The sequences were analyzed through MEGA-X by using the mecA gene (GenBank accession no. NC_002745 of MRSA strain N315) as a reference sequence [16].
4.6. Protein Modeling and Protein-Ligand Docking
In order to determine the structural change in mutant PBP2a caused by missense mutations found in the mecA gene of the MR-33 isolate, three-dimensional modeling of the mutant PBP2a carrying missense mutations (E239R and E447K) was performed by an automated homology modeling approach using the wild-type PBP2a (Protein Data Bank identification number ((PDB ID), 5M18) as a template in the SWISS-MODEL program (https://swissmodel.expasy.org/interactive; accessed on 29 April 2021). FoldX (http://foldxsuite.crg.eu/products#foldx; accessed on 29 April 2021) was used to repair the missing loops in the mutant and the wild-type structures of PBP2a and to optimize two PBP2a structures for energy minimization and the removal of amino acid side chain clashes as previously described [39]. The optimized mutant and the wild-type structures of PBP2a were then used for protein-ligand docking using AutoDock Vina [40]. The ligand cefoxitin was extracted and obtained from the structure (PBD ID, 3MZE) of the complex of cefoxitin with penicillin-binding proteins. The cefoxitin was docked with the optimized structures of wild-type and mutant PBP2a. The protein-ligand docking grid boxes in two PBP2a structures were selected based on the binding residues reported previously [24]. The binding affinity of cefoxitin with PBP2a was performed using AutoDock Vina. In AutoDock Vina, the parameter of the binding free energy has been used to determine the binding affinity of ligand (cefoxitin) with protein (PBP2a) [41]. The lesser the binding free energy, the higher the binding affinity the ligand has for the protein. AutoDock Vina is a free open-source package (http://vina.scripps.edu/; accessed on 29 April 2021) that can accurately and rapidly determine the binding affinity. AutoDock Vina is widely used with more than 6000 citations during the last ten years. AutoDock Vina has been available since 2010. AutoDock Vina is completely empirical and is comprised of hydrogen bonds, repulsion, Gaussian steric interactions, and hydrophobic and torsion terms [40]. AutoDock Vina was designed with parallel computing capabilities and is easy to use [41]. It was indicated that AutoDock Vina is accurate when determining binding affinity based on the CASF-2013 benchmark [42].
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ph14050420/s1. Figure S1. The amplification of the nuc gene fragment (270 bp) through PCR from Staphylococcus aureus isolated phenotypically from clinical samples. Figure S2. The amplification of the mecA gene fragment (533 bp) through PCR from MRSA isolates. Figure S3. The amplification of the entire mecA gene region (2368 bp) through PCR from MRSA isolates.
Author Contributions
Conceptualization, T.A., S.u.R. and S.-H.L.; data collection, T.A., A.B., A.M.K., J.-H.L. and J.-H.J.; data analysis, T.A., A.B., A.M.K., J.-H.L. and J.-H.J.; writing—original draft preparation, T.A., A.B., A.M.K., J.-H.L., J.-H.J., S.u.R. and S.-H.L.; writing—review and editing, T.A., A.B., A.M.K., J.-H.L., J.-H.J., S.u.R. and S.-H.L.; supervision, S.u.R. and S.-H.L.; funding acquisition, S.-H.L. and S.u.R. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by research grants from the Bio and Medical Technology Development Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Science, Information and Communications Technology (MSIT; grant No. NRF-2017M3A9E4078014); and from the NRF funded by the MSIT (grant Nos. NRF-2021R1A2C3004826 and NRF-2019R1C1C1008615). The portion of work done in Pakistan was funded by Higher Education Commission of Pakistan (grant No. NRPU-4501).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data are contained within the article or supplementary material.
Conflicts of Interest
The authors declare no conflict of interest. The funding bodies played no role in the design of the study, collection, analysis, or interpretation of the data or in the writing of the manuscript.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fishovitz J., Rojas-Altuve A., Otero L.H., Dawley M., Carrasco-Lopez C., Chang M., Hermoso J.A., Mobashery S. Disruption of allosteric response as an unprecedented mechanism of resistance to antibiotics. J. Am. Chem. Soc. 2014;136:9814–9817. doi: 10.1021/ja5030657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lai C.C., Chen C.C., Lu Y.C., Chuang Y.C., Tang H.J. The clinical significance of silent mutations with respect to ciprofloxacin resistance in MRSA. Infect. Drug Resist. 2018;11:681–687. doi: 10.2147/IDR.S159455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gajdács M. The continuing threat of methicillin-resistant Staphylococcus aureus. Antibiotics. 2019;8:52. doi: 10.3390/antibiotics8020052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aswani S.A., Abdul-Aziz A. The characterization of mecA gene and SCCmec typing in clinical samples of MRSA. Sci. Lett. 2019;13:1–7. [Google Scholar]
- 5.Namvar A.E., Bastarahang S., Abbasi N., Ghehi G.S., Farhadbakhtiarian S., Arezi P., Hosseini M., Baravati S.Z., Jokar Z., Chermahin S.G. Clinical characteristics of Staphylococcus epidermidis: A systematic review. GMS Hyg. Infect. Control. 2014;9:Doc23. doi: 10.3205/dgkh000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makgotlho P.E., Kock M.M., Hoosen A., Lekalakala R., Omar S., Dove M., Ehlers M.M. Molecular identification and genotyping of MRSA isolates. FEMS Immunol. Med. Microbiol. 2009;57:104–115. doi: 10.1111/j.1574-695X.2009.00585.x. [DOI] [PubMed] [Google Scholar]
- 7.Pinho M.G., Filipe S.R., de Lencastre H., Tomasz A. Complementation of the essential peptidoglycan transpeptidase function of penicillin-binding protein 2 (PBP2) by the drug resistance protein PBP2A in Staphylococcus aureus. J. Bacteriol. 2001;183:6525–6531. doi: 10.1128/JB.183.22.6525-6531.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinho M.G., de Lencastre H., Tomasz A. An acquired and a native penicillin-binding protein cooperate in building the cell wall of drug-resistant staphylococci. Proc. Natl. Acad. Sci. USA. 2001;98:10886–10891. doi: 10.1073/pnas.191260798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sekizuka T., Niwa H., Kinoshita Y., Uchida-Fujii E., Inamine Y., Hashino M., Kuroda M. Identification of a mecA/mecC-positive MRSA ST1-t127 isolate from a racehorse in Japan. J. Antimicrob. Chemother. 2020;75:292–295. doi: 10.1093/jac/dkz459. [DOI] [PubMed] [Google Scholar]
- 10.Hiramatsu K. Molecular evolution of MRSA. Microbiol. Immunol. 1995;39:531–543. doi: 10.1111/j.1348-0421.1995.tb02239.x. [DOI] [PubMed] [Google Scholar]
- 11.Anand K.B., Agrawal P., Kumar S., Kapila K. Comparison of cefoxitin disc diffusion test, oxacillin screen agar, and PCR for mecA gene for detection of MRSA. Indian J. Med. Microbiol. 2009;27:27–29. [PubMed] [Google Scholar]
- 12.Chen C., Zhao Q., Guo J., Li Y., Chen Q. Identification of Methicillin-resistant Staphylococcus aureus (MRSA) using simultaneous detection of mecA, nuc, and femB by loop-mediated isothermal amplification (LAMP) Curr. Microbiol. 2017;74:965–971. doi: 10.1007/s00284-017-1274-2. [DOI] [PubMed] [Google Scholar]
- 13.Shukla S.K., Ramaswamy S.V., Conradt J., Stemper M.E., Reich R., Reed K.D., Graviss E.A. Novel polymorphisms in mec genes and a new mec complex type in methicillin-resistant Staphylococcus aureus isolates obtained in rural Wisconsin. Antimicrob. Agents Chemother. 2004;48:3080–3085. doi: 10.1128/AAC.48.8.3080-3085.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Otero L.H., Rojas-Altuve A., Llarrull L.I., Carrasco-Lopez C., Kumarasiri M., Lastochkin E., Fishovitz J., Dawley M., Hesek D., Lee M., et al. How allosteric control of Staphylococcus aureus penicillin binding protein 2a enables methicillin resistance and physiological function. Proc. Natl. Acad. Sci. USA. 2013;110:16808–16813. doi: 10.1073/pnas.1300118110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alm R.A., McLaughlin R.E., Kos V.N., Sader H.S., Iaconis J.P., Lahiri S.D. Analysis of Staphylococcus aureus clinical isolates with reduced susceptibility to ceftaroline: An epidemiological and structural perspective. J. Antimicrob. Chemother. 2014;69:2065–2075. doi: 10.1093/jac/dku114. [DOI] [PubMed] [Google Scholar]
- 16.Schaumburg F., Peters G., Alabi A., Becker K., Idelevich E.A. Missense mutations of PBP2a are associated with reduced susceptibility to ceftaroline and ceftobiprole in African MRSA. J. Antimicrob. Chemother. 2016;71:41–44. doi: 10.1093/jac/dkv325. [DOI] [PubMed] [Google Scholar]
- 17.Long S.W., Olsen R.J., Mehta S.C., Palzkill T., Cernoch P.L., Perez K.K., Musick W.L., Rosato A.E., Musser J.M. PBP2a mutations causing high-level ceftaroline resistance in clinical methicillin-resistant Staphylococcus aureus isolates. Antimicrob. Agents Chemother. 2014;58:6668–6674. doi: 10.1128/AAC.03622-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loganathan A., Manohar P., Eniyan K., Jayaraj R., Nachimuthu R. Evaluation of various phenotypic methods with genotypic screening for detection of methicillin-resistant Staphylococcus aureus. Asian Biomed. (Res. Rev. News) 2019;13:225–233. doi: 10.1515/abm-2019-0065. [DOI] [Google Scholar]
- 19.Cao Y., Hao Y., Yang D., Pang B., Wang L. Fluorescent PCR detection of mecA in drug resistant MRSA: A methodological study. Br. J. Biomed. Sci. 2017;74:152–155. doi: 10.1080/09674845.2017.1297214. [DOI] [PubMed] [Google Scholar]
- 20.Clinical Laboratory Standards Institute (CLSI) Performance Standards for Antimicrobial Disk Susceptibility Tests. 13th ed. CLSI; Wayne, PA, USA: 2018. CLSI Standard M02. [Google Scholar]
- 21.Mahasenan K.V., Molina R., Bouley R., Batuecas M.T., Fisher J.F., Hermoso J.A., Chang M., Mobashery S. Conformational dynamics in penicillin-binding protein 2a of methicillin-resistant Staphylococcus aureus, allosteric communication network and enablement of catalysis. J. Am. Chem. Soc. 2017;139:2102–2110. doi: 10.1021/jacs.6b12565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coppens J., Van Heirstraeten L., Ruzin A., Yu L., Timbermont L., Lammens C., Matheeussen V., McCarthy M., Jorens P., Ieven M., et al. Comparison of GeneXpert MRSA/SA ETA assay with semi-quantitative and quantitative cultures and nuc gene-based qPCR for detection of Staphylococcus aureus in endotracheal aspirate samples. Antimicrob. Resist. Infect. Control. 2019;8:4. doi: 10.1186/s13756-018-0460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aqib A.I., Ijaz M., Farooqi S.H., Ahmed R., Shoaib M., Ali M.M., Mehmood K., Zhang H. Emerging discrepancies in conventional and molecular epidemiology of methicillin resistant Staphylococcus aureus isolated from bovine milk. Microb. Pathog. 2018;116:38–43. doi: 10.1016/j.micpath.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 24.Romeeza T., Nadeem A., Nauman J., Afia A., Kunwal R. Discrepancies in the diagnosis of methicillin resistant Staphylococcus aureus among different hospitals in Lahore, Pakistan. Int. Med. J. 2009;8:7–10. [Google Scholar]
- 25.De Bonville D. The impact of incorrect MRSA diagnoses. MLO Med. Lab. Obs. 2012;44:26–27. [PubMed] [Google Scholar]
- 26.Sapkota J., Sharma M., Jha B., Bhatt C.P. Prevalence of Staphylococcus aureus isolated from clinical samples in a tertiary care hospital: A descriptive cross-sectional study. JNMA J. Nepal Med. Assoc. 2019;57:398–402. doi: 10.31729/jnma.4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hussain M.S., Naqvi A., Sharaz M. Methicillin resistant staphylococcus aureus (MRSA); prevalence and susceptibility pattern of (MRSA) isolated from pus in tertiary care of district hospital of Rahim Yar Khan. Professional Med. J. 2019;26:122–127. [Google Scholar]
- 28.Khanal L.K., Adhikari R.P., Guragain A. Prevalence of methicillin resistant Staphylococcus aureus and antibiotic susceptibility pattern in a tertiary hospital in Nepal. J. Nepal Health Res. Counc. 2018;16:172–174. doi: 10.3126/jnhrc.v16i2.20305. [DOI] [PubMed] [Google Scholar]
- 29.Perwaiz S., Barakzi Q., Farooqi B.J., Khursheed N., Sabir N. Antimicrobial susceptibility pattern of clinical isolates of methicillin resistant Staphylococcus aureus. J. Pak. Med. Assoc. 2007;57:2–4. [PubMed] [Google Scholar]
- 30.Ariom T.O., Iroha I.R., Moses I.B., Iroha C.S., Ude U.I., Kalu A.C. Detection and phenotypic characterization of methicillin-resistant Staphylococcus aureus from clinical and community samples in Abakaliki, Ebonyi State, Nigeria. Afr. Health Sci. 2019;19:2026–2035. doi: 10.4314/ahs.v19i2.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kelley W.L., Jousselin A., Barras C., Lelong E., Renzoni A. Missense mutations in PBP2A affecting ceftaroline susceptibility detected in epidemic hospital-acquired methicillin-resistant Staphylococcus aureus clonotypes ST228 and ST247 in Western Switzerland archived since 1998. Antimicrob. Agents Chemother. 2015;59:1922–1930. doi: 10.1128/AAC.04068-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Forbes B.A., Sahm D.F., Weissfeld A.S. Study Guide for Bailey & Scott’s Diagnostic Microbiology. Mosby; Maryland Heights, MO, USA: 2007. [Google Scholar]
- 33.Sarhan S.R., Hashim H.O., Al-Shuhaib M.B.S. The Gly152Val mutation possibly confers resistance to β-lactam antibiotics in ovine Staphylococcus aureus isolates. Open Vet. J. 2020;9:339–348. doi: 10.4314/ovj.v9i4.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brakstad O.G., Aasbakk K., Maeland J.A. Detection of Staphylococcus aureus by polymerase chain reaction amplification of the nuc gene. J. Clin. Microbiol. 1992;30:1654–1660. doi: 10.1128/JCM.30.7.1654-1660.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee S.H., Kim J.Y., Lee G.S., Cheon S.H., An Y.J., Jeong S.H., Lee K.J. Characterization of blaCMY-11, an AmpC-type plasmid-mediated β-lactamase gene in a Korean clinical isolate of Escherichia coli. J. Antimicrob. Chemother. 2002;49:269–273. doi: 10.1093/jac/49.2.269. [DOI] [PubMed] [Google Scholar]
- 36.Bressler A.M., Williams T., Culler E.E., Zhu W., Lonsway D., Patel J.B., Nolte F.S. Correlation of penicillin binding protein 2a detection with oxacillin resistance in Staphylococcus aureus and discovery of a novel penicillin binding protein 2a mutation. J. Clin. Microbiol. 2005;43:4541–4544. doi: 10.1128/JCM.43.9.4541-4544.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Clinical Laboratory Standards Institute (CLSI) Performance Standards for Antimicrobial Susceptibility Testing. CLSI; Wayne, PA, USA: 2019. Twenti-Nineth Informational Supplement M100-S29. [Google Scholar]
- 38.Murakami K., Minamide W., Wada K., Nakamura E., Teraoka H., Watanabe S. Identification of methicillin-resistant strains of staphylococci by polymerase chain reaction. J. Clin. Microbiol. 1991;29:2240–2244. doi: 10.1128/JCM.29.10.2240-2244.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schymkowitz J., Borg J., Stricher F., Nys R., Rousseau F., Serrano L. The FoldX web server: An online force field. Nucleic Acids Res. 2005;33:W382–W388. doi: 10.1093/nar/gki387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Trott O., Olson A.J. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 2010;31:455–461. doi: 10.1002/jcc.21334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nguyen N.T., Nguyen T.H., Pham T.N.H., Huy N.T., Bay M.V., Pham M.Q., Nam P.C., Vu V.V., Ngo S.T. AutoDock Vina adopts more accurate binding poses but AutoDock 4 forms better binding affinity. J. Chem. Inf. Model. 2020;60:204–211. doi: 10.1021/acs.jcim.9b00778. [DOI] [PubMed] [Google Scholar]
- 42.Gaillard T. Evaluation of AutoDock and AutoDock Vina on the CASF-2013 benchmark. J. Chem. Inf. Model. 2018;58:1697–1706. doi: 10.1021/acs.jcim.8b00312. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are contained within the article or supplementary material.