Abstract
Patients with severe COVID-19 often experience complications including coagulopathy and fatal thrombosis. COVID-19 pneumonia sometimes leads to acute respiratory distress syndrome, requiring extracorporeal membrane oxygenation (ECMO), during which thrombosis and bleeding are major causes of death. Anticoagulation such as heparin is essential for COVID-19 patients on ECMO; however, bleeding might be caused by not only heparin, but also acquired von Willebrand syndrome (AVWS). To date, no study has examined ECMO-related bleeding and AVWS in COVID-19 patients.
We report a COVID-19 patient who experienced bleeding from AVWS in addition to disseminated intravascular coagulation (DIC) during ECMO. The level of high–molecular weight VWF multimers decreased during ECMO therapy, and these findings promptly improved after discontinuation of ECMO. Plasma levels of VWF antigen were extremely high, probably due to endothelial cell damage caused by COVID-19. On the other hand, plasma levels of ADAMTS13 activity were moderately reduced, to 20–30% of normal. The patient was successfully treated with cryoprecipitate in bleeding during ECMO without a reduction in heparin, which might have induced thromboembolism. Bleeding found in this patient might be caused by AVWS and DIC.
Severe COVID-19 patients are in a thrombotic state and need to receive anticoagulant therapy. However, once they receive ECMO therapy, bleeding symptoms could be observed. In such cases, physicians should think of AVWS in addition to the side effect of heparin and DIC.
Keywords: COVID-19, Extracorporeal membrane oxygenation, Acquired von Willebrand syndrome, Bleeding, Anticoagulation
See correspondence vol. 28: 402–403
Introduction
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)1). Multiple studies have shown that coagulation abnormalities are related to mortality in patients with severe COVID-19 pneumonia2). In fact, the incidence of thrombotic complications such as pulmonary embolism and extremity venous thrombosis is very high in critically ill COVID-19 patients, even in those receiving thromboprophylaxis3–5). In addition, 71.4% of non-survivors are diagnosed with disseminated intravascular coagulation (DIC) according to the International Society on Thrombosis and Haemostasis (ISTH) diagnostic creiteria2).
Some patients with COVID-19 rapidly develop acute respiratory distress syndrome (ARDS), necessitating veno-venous extracorporeal membrane oxygenation (ECMO) support1, 6). ECMO is frequently complicated by hemorrhage and thrombosis7, 8). Anticoagulant to prevent thrombus is a common cause of bleeding during ECMO. In addition, acquired von Willebrand syndrome (AVWS) has been reported as a hemorrhagic side effect of ECMO9, 10).
von Willebrand factor (VWF), a large plasma glycoprotein that plays an important role in hemostasis and thrombosis, is exclusively produced in vascular endothelial cells. Reduced levels or defective function of VWF can cause the most common inherited bleeding disorder, von Willebrand disease11). Plasma VWF consists of heterogeneous multimers with molecular masses ranging from 500 to 20,000 kDa12). High–molecular weight VWF multimers (HMW-VWFMs) are more active in thrombosis and hemostasis. A VWF-cleaving protease, ADAMTS13, regulates the molecular size of VWF under high shear stress. Type 2A von Willebrand disease (VWD) is associated with a mutation in the VWF A2 domain, which contains the ADAMTS13 cleaving site. In patients with type 2A VWD, mutated VWF is easily cleaved by ADAMTS13. This type of VWD results in reduced levels of HMW-VWFMs and a strong tendency to bleed. VWF dysfunction in patients with various underlying diseases is referred to as AVWS. Patients with cardiovascular diseases associated with AVWS, such as Heyde syndrome13), have been reported with increasing frequency over the past few decades. In these types of AVWS, non-physiologically high shear stress in blood results in excessive cleavage of VWF by ADAMTS13, resulting in AVWS with reduced levels of HMW-VWFMs as observed in type 2A VWD. ECMO-related AVWS is caused by the extraordinarily high shear stress inside the pump9).
In patients with severe COVID-19, thrombotic complications should be noted, and anticoagulation therapy prescribed as appropriate. To date, however, no study has examined ECMO-related bleeding and AVWS in COVID-19 patients in a thrombotic state. In this report, we describe the successful management of ECMO-related AVWS in a COVID-19 patient with elevated D-dimer.
Case Presentation
A 57-year-old man visited our hospital with cough and a high-grade fever (> 39°C) for 5 days. He had a history of contact with a COVID-19 patient 12 days prior. COVID-19 infection was confirmed by PCR, and he was admitted to our hospital the next day (day 1). The patient had been on medication for hypertension and hyperlipidemia, and had smoked until 4 years ago. On admission, pulse was 103 beat/minute, temperature 39.5°C, blood pressure 118/62 mmHg, respiratory rate 28/minute, and oxygen saturation 91% on room air. Blood examination revealed fibrin/fibrinogen degradation products (FDP) 10.6 µg/mL (normal, < 10 µg/mL), D-dimer 2.7 µg/mL (normal, < 0.5 µg/mL); platelets 142×109/L; fibrinogen, 10.6 g/L (normal, 20–40 mg/dL); prothrombin time, 12.6 seconds (normal, 11–13 seconds); thrombin-antithrombin complex (TAT) 3.7ng/mL (normal, 3.75 ng/mL); and plasmin-α2-plasmin inhibitor complex (PIC) 5.4 µg/mL (normal, < 0.8 µg/mL). Chest computed tomography showed bilateral ground-glass opacities. After admission, oxygen therapy was started, but pneumonia rapidly worsened. On day 3 after admission, he was transferred to the intensive care unit (ICU), and mechanical ventilation and favipiravir for SARS-CoV-2 were initiated. On day 7, D-dimer rapidly increased, and continuous unfractionated heparin was administrated. (D-dimer 176.8 µg/mL; platelets 213×109/L; fibrinogen, 8.24 g/L; prothrombin time, 14.2 seconds). A time course of clinical data and therapeutic interventions is shown in Fig. 1.
Fig. 1.
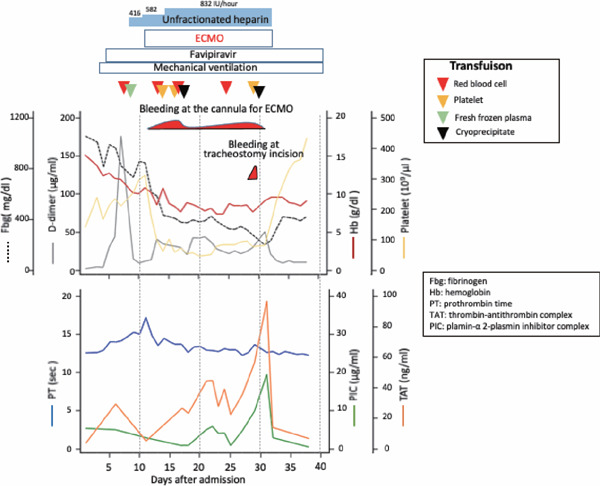
Time course of clinical data and therapeutic interventions
On admission, the patient had extremely high fibrinogen levels with normal platelet counts. Following the development of respiratory failure, D-dimer levels suddenly increased. Continuous administration of unfractionated heparin was initiated on day 7 after admission. ECMO support was provided between days 11 and 31. Cryoprecipitate was administrated on days 17 and 29, and was effective for bleeding. ECMO: veno-venous extracorporeal membrane oxygenation
On day 11, however, the patient was diagnosed with ARDS, and ECMO therapy was initiated. We used the right femoral vein (21 Fr cannula) for blood access and the right jugular vein (16.5 Fr cannula) for blood return. The volume of heparin was increased after ECMO began to prevent thrombosis in the circulation. Bleeding was observed at the cannula insertion point at the jugular vein. Platelet counts rapidly decreased after initiation of ECMO, probably because of the ECMO therapy. After initiation of ECMO, TAT and PIC gradually increased. In fact, this patient was diagnosed with DIC during ECMO treatment, based on the DIC score according to ISTH diagnostic guidelines. Platelets were transfused twice, but were not effective against bleeding.
Therefore, we performed VWF multimer analysis and observed decreased HMW-VWFMs after initiation of ECMO (Fig. 2). Hence, the patient was diagnosed with AVWS caused by ECMO. Loss of HMW-VWFMs can be induced by the degree of shear stress in ECMO and inserted pumps. Shear stress depends on the velocity and viscosity of blood and the diameter of vessels. However, we could not reduce the rotation rate of the ECMO pump or cannula size because of the severe respiratory condition. Therefore, cryoprecipitate made from 1,440 mL of fresh frozen plasma (FFP) was administrated to replenish VWF on day 17. Severe bleeding was temporarily stopped, but minor bleeding continued. In addition, oozing at the anus was observed between day 19 and 23. We performed surgical tracheostomy on day 29 due to the long period of intubation in the mouth. Bleeding from tracheal incision continued despite platelet transfusion. The patient received cryoprecipitate made from 1,440 mL of FFP again, and bleeding subsided. ARDS gradually improved, and ECMO was discontinued on day 31. Platelet counts quickly recovered, and D-dimer, PIC, and TAT decreased promptly. In addition, bleeding symptoms completely disappeared after discontinuation of ECMO therapy.
Fig. 2.
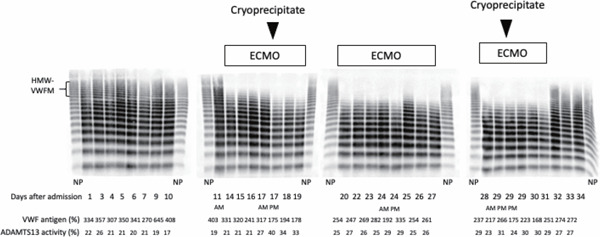
VWF multimer analysis and plasma levels of VWF antigen and ADAMTS13 activity
VWF multimer analysis using SDS-1.0% agarose electrophoresis revealed a reduction in the level of high-molecular weight VWF multimers (HMW-VWFMs) during ECMO support. VWF multimers were classified as HMW-VWFMs if they corresponded to bands > 10 in the VWF multimer analysis. Plasma levels of VWF antigen were extremely high, and ADAMTS13 activity was moderately reduced during the hospitalization. Values of 100% were defined as the amounts of VWF antigen, and ADAMTS13 activity in pooled plasma from normal healthy volunteers.
NP: normal human plasma, ECMO: veno-venous extracorporeal membrane oxygenation
Fig. 2 shows the results of VWF multimer analysis, with plasma levels of VWF antigen and ADAMTS13 activity. The level of HMW-VWFMs dramatically decreased during ECMO therapy between day 14 and day 31. Notably, these findings promptly improved after ECMO discontinuation. Plasma levels of VWF antigen were extremely high, probably due to endothelial cell damage caused by COVID-19. On the other hand, plasma levels of ADAMTS13 activity were moderately reduced, to 20–30% of normal.
Plasma levels of VWF antigen were measured by sandwich ELISA using rabbit anti-VWF polyclonal antibodies (Dako Cytomation, Copenhagen, Denmark) 14). VWF multimers were classified as HMW-VWFMs if they corresponded to bands > 10 in the VWF multimer analysis as shown in Fig. 215). Plasma values of ADAMTS13 activity were measured by chromogenic ADAMTS13-act-ELISA16). VWF multimer analysis was performed according to the method of Ruggeri and Zimmerman17) with some modifications18). Values of 100% were defined as the amounts of VWF antigen and ADAMTS13 activity in pooled plasma from normal healthy volunteers. This study was conducted with the approval of the ethics committee of Nara Medical University. Written informed consent was obtained from the patient.
Discussion
Currently, the pathophysiology and clinical course of COVID-19 patients are not well understood. However, two serious complications have been reported in patients with severe COVID-19: ARDS and coagulopathy with thromboembolism. For the latter, anticoagulant therapy such as low–molecular weight heparin (LMWH) is associated with better prognosis in COVID-19 patients with markedly elevated D-dimer level19). The coagulation abnormalities found in COVID-19 patients suggest activation of blood coagulation with fibrinolysis. This type of coagulopathy is observed in DIC patients with enhanced fibrinolysis, which often tend to experience bleeding. However, bleeding is a rare complication in patients with COVID-19. ISTH interim guidance recommends that LMWH should be considered in all patients who require hospital admission for COVID-19 20). If these patients exhibit bleeding, physicians are often reluctant to administer LMWH.
ARDS is the most common reason for ICU management in patients with severe COVID-19, and 2.9–4.9% of hospitalized patients require ECMO support6, 21, 22). Bleeding, which is often caused by anticoagulant and AVWS, is a frequent complication of ECMO23, 24). However, it is difficult to diagnose and treat patients with AVWS caused by excessive cleavage of VWF by ADAMTS13. The definitive therapy for this type of AVWS is to stop mechanical circulation of blood, but that is impossible in patients with severe respiratory failure, as in this patient. FFP and plasma-derived (PD) VWF products can be used to replenish VWF, but are effective only for short periods. Bleeding symptoms during ECMO are often misunderstood as a side effect of anticoagulant. Therefore, physicians often stop or decrease the volume of anticoagulant such as heparin. However, almost all patients with severe COVID-19 have coagulopathy; consequently, reduction of anticoagulant therapy is dangerous and might lead to severe thrombotic events.
In addition, DIC could not be excluded even during ECMO. In fact, our patient met the DIC score by ISTH diagnostic guidelines during ECMO. Because heparin might be effective for patients with DIC, it should be continued during ECMO even if the patient tends to bleed. In this patient, TAT was analyzed for activation of the coagulation pathway and PIC for activation of the fibrinolytic pathway. Before initiation of ECMO, PIC levels were constantly elevated. On the other hands, TAT levels sharply increased with elevated D-dimer. Activation of the coagulation pathway due to COVID-19 might have contributed to the pulmonary vascular microthrombosis25) in this patient, resulting in respiratory failure. After initiation of ECMO, both levels of TAT and PIC increased while going up and down, and decreased sharply after ECMO discontinuation. Contact activation of the coagulation cascade, thrombin generation, and fibrin deposition occur on the artificial surfaces in ECMO26). Thrombin generation also evokes the fibrinolytic system. Therefore, it is difficult to assess the coagulation precisely. However, we speculate that DIC-like coagulopathy existed in this patient even during ECMO.
In the case described here, unfractionated heparin was continued, and cryoprecipitate was administrated for bleeding. Thrombocytopenia was observed during ECMO, but platelet transfusion was not effective for treatment of bleeding. Thrombocytopenia is common in ECMO patients27). Combes et al.28) reported that thrombocytopenia (≦50 × 109/L) was found in 40% of patients with ECMO and severe thrombocytopenia (≦200 × 109/L) was found in 27 %. The underlying mechanisms of thrombocytopenia during ECMO are multifactorial, including primary disease, toxic drug effects, anticoagulation and the ECMO system used27). Therefore, it is difficult to speculate about the cause of thrombocytopenia. We considered that DIC due to ECMO and COVID-19 infection and contact with foreign surfaces in the ECMO system are major causes of thrombocytopenia.
In order to stop the bleeding caused by VWF deficiency, it is necessary to increase the plasma level of HMW-VWFMs over the threshold. PD-VWF product (Confact F®) and cryoprecipitate contain a higher concentration of VWF and a lower concentration of ADAMTS13 relative to FFP29). PD-VWF product and cryoprecipitate can supply HMW-VWFMs faster than FFP. In addition, cryoprecipitate contains α2 anti-plasmin, which can inactivate plasmin and suppress fibrinolysis30). Bleeding found in this patient might be mainly caused by AVWS and DIC. We believe that cryoprecipitate is the most effective treatment for ECMO-related AVWS in COVID-19 patients with DIC.
Patients with severe COVID-19 are in a thrombotic state and need to receive anticoagulant therapy such as LMWH. However, once they receive ECMO therapy, bleeding symptoms could be observed. In such cases, physicians should think of AVWS and initiate appropriate therapy while maintaining LMWH.
Acknowledgements
This work was supported by research grants from the Japan Agency for Medical Research and Development and from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Conflict of Interests
The authors have no conflict of interest.
Author Contributions
Contribution: M.H analyzed the data, and performed experiments; K.T., K.K. and H.F collected the data and performed patient care; M.K. performed experiments; M. M. designed the study, and wrote the manuscript.
References
- 1). Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS and China Medical Treatment Expert Group for C: Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med, 2020; 382: 1708-1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2). Tang N, Li D, Wang X and Sun Z: Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost, 2020; 18: 844-847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3). Poissy J, Goutay J, Caplan M, Parmentier E, Duburcq T, Lassalle F, Jeanpierre E, Rauch A, Labreuche J, Susen S and Lille ICUHC-g: Pulmonary Embolism in COVID-19 Patients: Awareness of an Increased Prevalence. Circulation, 2020; [DOI] [PubMed] [Google Scholar]
- 4). Cui S, Chen S, Li X, Liu S and Wang F: Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost, 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV and Endeman H: Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res, 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X and Peng Z: Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA, 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7). Koeckerling D, Pan D, Mudalige NL, Oyefeso O and Barker J: Blood transfusion strategies and ECMO during the COVID-19 pandemic. Lancet Respir Med, 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8). Thiagarajan RR, Barbaro RP, Rycus PT, McMullan DM, Conrad SA, Fortenberry JD, Paden ML and centers Em: Extracorporeal Life Support Organization Registry International Report 2016. ASAIO J, 2017; 63: 60-67 [DOI] [PubMed] [Google Scholar]
- 9). Kalbhenn J, Schmidt R, Nakamura L, Schelling J, Rosenfelder S and Zieger B: Early diagnosis of acquired von Willebrand Syndrome (AVWS) is elementary for clinical practice in patients treated with ECMO therapy. J Atheroscler Thromb, 2015; 22: 265-271 [DOI] [PubMed] [Google Scholar]
- 10). Tamura T, Horiuchi H, Obayashi Y, Fuki M, Imanaka M, Kuroda M, Nishimura S, Amano M, Sakamoto J, Tamaki Y, Enomoto S, Miyake M, Kondo H, Izumi C and Nakagawa Y: Acquired von Willebrand syndrome in patients treated with veno-arterial extracorporeal membrane oxygenation. Cardiovasc Interv Ther, 2019; 34: 358-363 [DOI] [PubMed] [Google Scholar]
- 11). Sadler JE, Budde U, Eikenboom JC, Favaloro EJ, Hill FG, Holmberg L, Ingerslev J, Lee CA, Lillicrap D, Mannucci PM, Mazurier C, Meyer D, Nichols WL, Nishino M, Peake IR, Rodeghiero F, Schneppenheim R, Ruggeri ZM, Srivastava A, Montgomery RR, Federici AB and Working Party on von Willebrand Disease C: Update on the pathophysiology and classification of von Willebrand disease: a report of the Subcommittee on von Willebrand Factor. J Thromb Haemost, 2006; 4: 2103-2114 [DOI] [PubMed] [Google Scholar]
- 12). Ruggeri ZM and Zimmerman TS: The complex multimeric composition of factor VIII/von Willebrand factor. Blood, 1981; 57: 1140-1143 [PubMed] [Google Scholar]
- 13). Vincentelli A, Susen S, Le Tourneau T, Six I, Fabre O, Juthier F, Bauters A, Decoene C, Goudemand J, Prat A and Jude B: Acquired von Willebrand syndrome in aortic stenosis. N Engl J Med, 2003; 349: 343-349 [DOI] [PubMed] [Google Scholar]
- 14). Bartlett A, Dormandy KM, Hawkey CM, Stableforth P and Voller A: Factor-VIII-related antigen: measurement by enzyme immunoassay. Br Med J, 1976; 1: 994-996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15). Budde U, Drewke E, Mainusch K and Schneppenheim R: Laboratory diagnosis of congenital von Willebrand disease. Semin Thromb Hemost, 2002; 28: 173-190 [DOI] [PubMed] [Google Scholar]
- 16). Kato S, Matsumoto M, Matsuyama T, Isonishi A, Hiura H and Fujimura Y: Novel monoclonal antibody-based enzyme immunoassay for determining plasma levels of ADAMTS13 activity. Transfusion, 2006; 46: 1444-1452 [DOI] [PubMed] [Google Scholar]
- 17). Ruggeri ZM and Zimmerman TS: Variant von Willebrand's disease: characterization of two subtypes by analysis of multimeric composition of factor VIII/von Willebrand factor in plasma and platelets. J Clin Invest, 1980; 65: 1318-1325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18). Budde U, Schneppenheim R, Plendl H, Dent J, Ruggeri ZM and Zimmerman TS: Luminographic detection of von Willebrand factor multimers in agarose gels and on nitrocellulose membranes. Thromb Haemost, 1990; 63: 312-315 [PubMed] [Google Scholar]
- 19). Tang N, Bai H, Chen X, Gong J, Li D and Sun Z: Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost, 2020; 18: 1094-1099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20). Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, Clark C and Iba T: ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost, 2020; 18: 1023-1026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21). Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X and Zhang L: Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet, 2020; 395: 507-513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22). Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J and Cao B: Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet, 2020; 395: 497-506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23). Kalbhenn J, Schlagenhauf A, Rosenfelder S, Schmutz A and Zieger B: Acquired von Willebrand syndrome and impaired platelet function during venovenous extracorpo real membrane oxygenation: Rapid onset and fast recovery. J Heart Lung Transplant, 2018; 37: 985-991 [DOI] [PubMed] [Google Scholar]
- 24). Horiuchi H, Doman T, Kokame K, Saiki Y and Matsumoto M: Acquired von Willebrand Syndrome Associated with Cardiovascular Diseases. J Atheroscler Thromb, 2019; 26: 303-314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25). Marongiu F, Grandone E and Barcellona D: Pulmonary thrombosis in 2019-nCoV pneumonia? J Thromb Haemost, 2020; 18: 1511-1513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26). Yusuff H, Zochios V and Brodie D: Thrombosis and coagulopathy in COVID-19 patients requiring extracorporeal membrane oxygenation. ASAIO J, 2020: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27). Jiritano F, Serraino GF, Ten Cate H, Fina D, Matteucci M, Mastroroberto P and Lorusso R: Platelets and extracorporeal membrane oxygenation in adult patients: a systematic review and meta-analysis. Intensive Care Med, 2020; 46: 1154-1169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28). Combes A, Hajage D, Capellier G, Demoule A, Lavoue S, Guervilly C, Da Silva D, Zafrani L, Tirot P, Veber B, Maury E, Levy B, Cohen Y, Richard C, Kalfon P, Bouadma L, Mehdaoui H, Beduneau G, Lebreton G, Brochard L, Ferguson ND, Fan E, Slutsky AS, Brodie D, Mercat A, Eolia Trial Group R and Ecmonet: Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome. N Engl J Med, 2018; 378: 1965-1975 [DOI] [PubMed] [Google Scholar]
- 29). Hori Y, Hayakawa M, Isonishi A, Soejima K, Matsumoto M and Fujimura Y: ADAMTS13 unbound to larger von Willebrand factor multimers in cryosupernatant: implications for selection of plasma preparations for thrombotic thrombocytopenic purpura treatment. Transfusion, 2013; 53: 3192-3202 [DOI] [PubMed] [Google Scholar]
- 30). McRoyan DK, McRoyan CJ, Sauter KL, Liu PI and Daniel SJ: Antithrombin III, plasminogen, plasmin, and alpha-2-antiplasmin in donor blood and plasma components. Ann Clin Lab Sci, 1985; 15: 165-170 [PubMed] [Google Scholar]


