Abstract
Simple Summary
An oral squamous cell carcinoma (OSCC) is a tumor of the oral cavity that has a five-year survival rate of only around 50%. As this rate has not increased in recent decades, despite improvements in diagnosis and therapy, novel, easily accessible biomarkers for prognosis assessment are still needed. In our study, we measured the growth factor protein progranulin/GP88 in the serum of OSCC patients and demonstrated that an increased serum GP88 level is associated with a better prognosis for the OSCC patients in our study group. Furthermore, serum GP88 levels were not significantly associated with age, sex, or the tumor’s histological features, indicating that serum GP88 levels may be an independent predictor of an individual OSCC patient’s prognosis. These findings may help to improve therapy management of an OSCC in personalized medicine.
Abstract
Progranulin (PGRN)/GP88 is a growth factor that is expressed in a wide range of tumor tissues. The secreted form is involved in various biological processes including proliferation and inflammation. In several tumor types, the serum GP88 level is associated with a patient’s prognosis; however, data for oral squamous cell carcinomas (OSCCs) have not yet been reported. We measured the serum GP88 levels in 96 OSCC patients by an enzyme immunosorbent assay (EIA) and correlated these data with clinicopathological parameters and patient outcomes. The GP88 levels in the serum of OSCC patients and healthy volunteers were comparable. In OSCC patients, the levels did not correlate with age, sex, or TNM status. In a Kaplan–Meier survival analysis, a serum GP88 level < 68 ng/mL was significantly associated with worsened survival (p = 0.0005, log-rank-test) as well as in uni- and multivariate Cox regression analyses (RR = 4.6 [1.6–12.9], p = 0.004 and RR = 4.2 [1.2–12.0], p = 0.008). This effect was predominant in OSCC patients older than 60.5 years (p = 0.027), while in younger patients no significant association between serum GP88 levels and prognosis could be observed. Altogether, lower serum GP88 levels are significantly associated with a worsened outcome for an OSCC and may be an interesting candidate for risk stratification during OSCC therapy.
Keywords: GP88, progranulin, serum, OSCC, prognosis
1. Introduction
An oral squamous cell carcinoma (OSCC), which mainly comprises cancer of the oral cavity and adjacent histological structures, is the fifteenth most-diagnosed cancer worldwide [1]. The standard therapy involves surgical excision of the tumor following radiotherapy or chemotherapy. For follow-up rehabilitation of functional defects. the grafting of bone material from different sources [2,3] and patient-specific implantation of prosthetics is practiced [4]. The application of stem cells to reverse bone degeneration or dental loss offers great hope for the future [5,6]. Nonetheless, the five-year survival rate of OSCC patients is only about 50% and has stagnated in recent decades [7]. Therefore, very early detection and prognosis stratification may be the main step for personalized risk management and subsequent therapy management for OSCC patients.
Liquid biopsies offer the advantage of low-invasive detection of a wide variety of metabolic products or molecular factors generated by the tumor. Given the applicability of glycoprotein 88 (GP88) to serum measurements in a wide variety of body fluids [8], soluble GP88/progranulin (PGRN) may be an interesting candidate for a biomarker in OSCC patients. Furthermore, because links already exist between serum GP88 levels and disease progression or prognosis in malignancies (e.g., breast cancer [9,10,11], non-small-cell lung cancer [12] and prostate cancer [13,14]) and in the genesis and progression of other diseases (e.g., frontotemporal lobar degeneration [15,16], obesity [17,18], systemic lupus erythematosus [19,20] and rheumatoid arthritis [21,22]), changes in serum GP88 levels seem to reflect a pathophysiological state in a wide variety of conditions.
Progranulin/GP88 is a member of the unique growth-factor family, expressed as a soluble 88 kDa glycoprotein and identified with others in the teratoma PC cell line [23]. It contributes to disease progression by stimulating proliferation and invasion in a multitude of different tumor entities [24,25,26,27,28] via the activation of several tumor-related pathways like ERK and TNFR2/Akt signaling [29,30,31,32] and PI3K [32] or Wnt [33] signaling. GP88 can promote angiogenesis via stimulation of VEGF in breast cancer and colorectal cancer cells [29,34]. An accumulation of GP88 in cancer stem cells of hepatocellular carcinoma or an association with cancer stemness in glioblastoma has been suggested [35,36]. GP88 expression has also been reported in relation to different cancer treatment resistance mechanisms such as letrozole and tamoxifen resistance in breast cancer cells [27,34], temozolomide resistance of glioblastoma [35], dexamethasone resistance in multiple melanoma [37], and chemoresistance to cisplatin in ovarian cancer cell lines [38]. Furthermore, GP88 is involved in inflammatory processes by, for instance, suppressing TNFα-induced IL-8 production in human epithelial cell lines [39] or human aortic smooth muscle cells [30]. However, GP88 action on inflammation is a double-edged sword, as the elastin-mediated processing of progranulin to lower molecular weight granulins results in pro-inflammatory activity of the cleaved factor by inducing, for instance, interleukin 8 (IL-8) secretion in epithelial cell lines, which attracts neutrophils [39]. Additionally, the macrophages of GP88-deficient mice were demonstrated to produce increased pro-inflammatory cytokines like monocyte chemoattractant protein-1 (MCP1), IL-6, IL-12 and tumor necrosis factor (TNF) in reaction to an acute infection, while the anti-inflammatory IL-10 production was largely suppressed [40]. Taken together, because GP88 acts at the crossing of several biological processes associated with the pathophysiology of malignancies, it is an interesting target for diagnostic and therapeutic applications.
The aim of this study was to measure GP88 levels in the serum of 96 OSCC patients and correlate these data with the demographic, clinicopathological and prognostic data of the patients to determine whether serum GP88 levels are associated with OSCC occurrence and progression.
2. Materials and Methods
2.1. Patients
Ninety-six patients suffering from an oral squamous cell carcinoma (OSCC) were included after a positive evaluation of the study by the local ethics committee of the Medical Faculty of the Martin Luther University Halle–Wittenberg (Ethical registry 210/19.08.09/10; approval date: 19.08.2009). The patients gave written informed consent. The median age of the patients was 60.5 years (range: 42–87), with 69 (71.9%) men and 27 (28.1%) women enrolled. Blood sampling was performed in all cases in this study on the day of the surgical excision of the tumor with no prior treatment. Twenty-six patients (27.1%) received radiotherapy subsequent to excision, 11 patients (11.5%) received chemotherapy with cisplatin, and one patient received taxol (1.0%). The patient group is part of the previously described cohort [41,42]. Demographic and clinicopathological data of the patients are summarized in Table 1. Healthy volunteers were blood donors with a median age of 64.0 years (23 males and 10 females).
Table 1.
Demographic and clinicopathological data of the OSCC patient cohort. Significant correlation with an increased serum GP88 level is marked in bold.
| Parameter | Subgroup | Serum GP88 < 68 ng/mL | Serum GP88 ≥ 68 ng/mL | n | p |
|---|---|---|---|---|---|
| age | <60.5 | 33 | 16 | 49 | 0.39 |
| ≥60.5 | 32 | 15 | 47 | ||
| sex | male | 46 | 23 | 69 | 0.73 |
| female | 19 | 8 | 27 | ||
| patient status | alive | 31 | 27 | 58 | <0.001 |
| deceased | 34 | 4 | 38 | ||
| T stage | T1 | 12 | 9 | 21 | 0.44 |
| T2 | 22 | 12 | 34 | ||
| T3 | 16 | 4 | 20 | ||
| T4 | 15 | 6 | 21 | ||
| N stage | N0 | 38 | 22 | 60 | 0.50 |
| N1 | 10 | 2 | 12 | ||
| N2 | 16 | 7 | 23 | ||
| N3 | 1 | 0 | 1 | ||
| M | M0 | 64 | 31 | 95 | 0.49 |
| M1 | 1 | 0 | 1 | ||
| Grading | 1 | 10 | 4 | 14 | 0.93 |
| 2 | 40 | 19 | 59 | ||
| 3 | 15 | 8 | 23 | ||
| radiotherapy | no | 43 | 27 | 70 | 0.03 |
| yes | 22 | 4 | 26 | ||
| chemotherapy | no | 54 | 30 | 84 | 0.06 |
| yes | 11 | 1 | 12 |
Significant correlation with an increase serum GP88 level is marked in bold.
2.2. Preanalytics
Ten milliliters of venous blood was drawn on the day of surgical excision of a patient’s tumor. Blood was immediately centrifuged at 400× g, and serum was then transferred to separate reaction tubes and subsequently stored at −80 °C. A serum aliquot was thawed directly before enzyme immunosorbent assay (EIA) measurement.
2.3. GP88 EIA
Serum GP88 levels were measured by a quantitative GP88 sandwich EIA developed and manufactured by A&G Pharmaceutical Inc. (Columbia, MD, USA) according to the manufacturer’s protocol (also described in [8]). Briefly, 96-well EIA plates (Corning, Kennebunk, ME, USA) were coated with the antihuman GP88 6B3 monoclonal antibody the day before incubation with 200 μL patients serum (1:10) each for 2 h. After washing, the wells were incubated with rabbit polyclonal 37 kDa antibody as a detection antibody for 1 h. EIA reaction was triggered by TMB substrate incubation for 5 to 15 min and measured by an absorbance readout at 620 nm on a GENios Microplate Reader (Tecan, Männedorf, Switzerland). Quantification was performed by a comparison of the absorption readouts with the control samples (human GP88 at levels from 0 to 20 ng/mL). Standard samples, patients’ samples, and healthy volunteers’ samples were measured in duplicate, and the mean value was applied for concentration calculations.
2.4. Statistics
Statistical analyses were performed using SPSS Statistics 25 (IBM, Ehningen, Germany). ROC curves were performed for the comparison of serum GP88 levels of healthy volunteers against OSCC patients and for the assessment of an optimized cut-off value through Youden index calculation. The distribution of serum GP88 levels in different groups (age, sex, T, N, G) were compared by a ChiSquare test and non-parametric tests (Mann–Whitney U-Test, Kruskal–Wallis test, Shapiro–Wilk test). Survival analyses were calculated by Kaplan–Meier analyses and uni-/multivariate Cox regression analyses. Overall survival (OS) was assessed from the date of serum collection to the last follow-up date or death of the patient.
3. Results
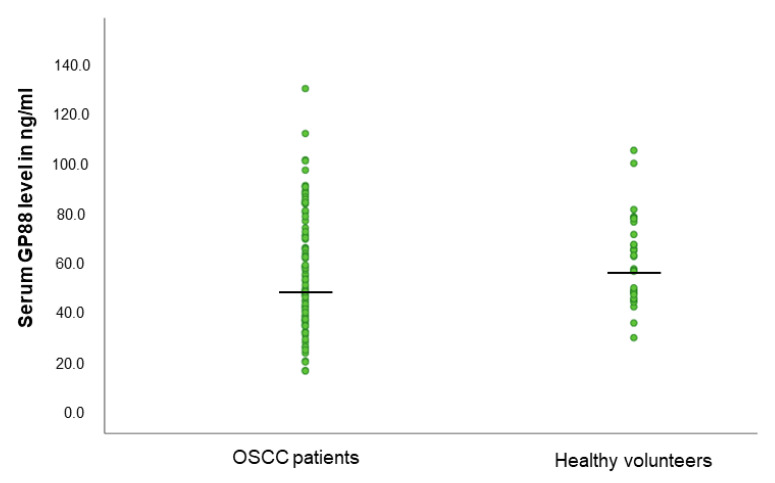
3.1. GP88 Levels Are Not Different in the Serum of OSCC Patients and Healthy Volunteers
We compared the levels of serum GP88 in OSCC patients to those assessed in healthy volunteers. The median age in both groups was not significantly different (OSCC patients: 60.5 years; healthy: 64.0 years; p = 0.10; unpaired Student’s t-test). Median serum GP88 levels did not significantly differ in healthy blood donors in comparison to age-matched OSCC patients (57.6 ng/mL vs. 52.1 ng/mL; p = 0.61, Student’s t-test; see Figure 1).
Figure 1.
Serum GP88 level distribution in OSCC patients and healthy volunteers.
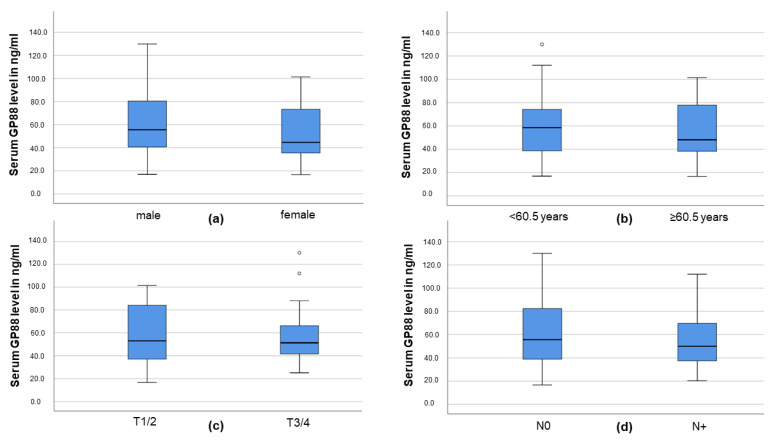
3.2. Serum GP88 Level and Demographic and Clinicopathological Parameters
We analyzed the GP88 serum levels of the OSCC patients according to sex, age, T and N stage. The levels were slightly lower in female OSCC patients compared those of males (median GP88 level 44.7 ng/mL vs. 55.6 ng/mL); however, this difference was not significant (p = 0.249; Mann–Whitney U-Test; see Figure 2a). Serum GP88 levels were also gradually lower in patients ≥60.5 years (median GP88 level 48.1 ng/mL vs. 58.5 ng/mL in younger patients); however, this difference also did not reach significance (p = 0.408; Mann–Whitney U-Test; see Figure 2b). Regarding the T stage of the tumor, median serum GP88 levels were almost equal in low-grade tumors (T1/2) compared with advanced tumors (T3/T4; 51.2 ng/mL vs. 52.9 ng/mL; p = 0.847; Mann–Whitney U-Test; see Figure 2c). Patients with no nodal metastases exhibited a gradually higher serum GP88 level (55.6 ng/mL vs. 49.9 ng/mL); however, this difference was also not significant (p = 0.421; Mann–Whitney U-Test; see Figure 2d). In summary, serum GP88 levels in OSCC patients did not seem to be correlated with age, sex, T or N stage.
Figure 2.
Distribution of serum GP88 levels according to (a) sex, (b) age median, (c) T stage or (d) nodal metastasis.
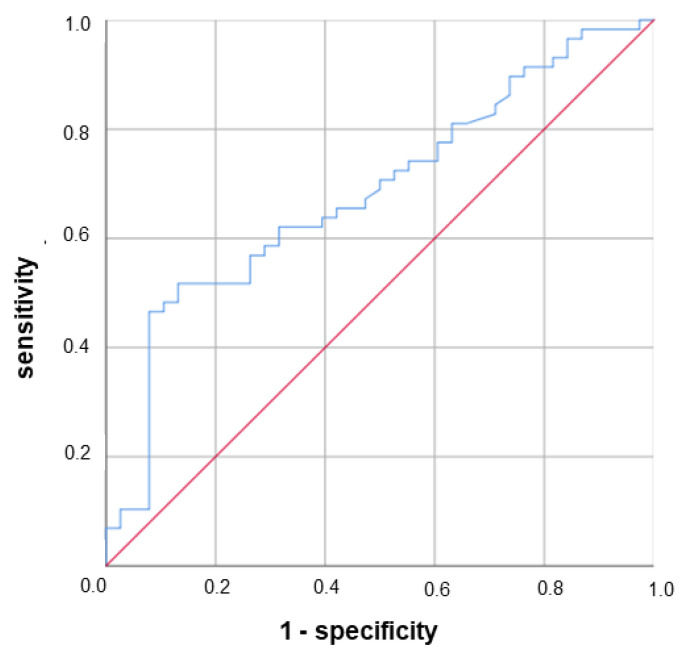
3.3. Lower Serum GP88 Levels Are Significantly Associated with Worsened Survival
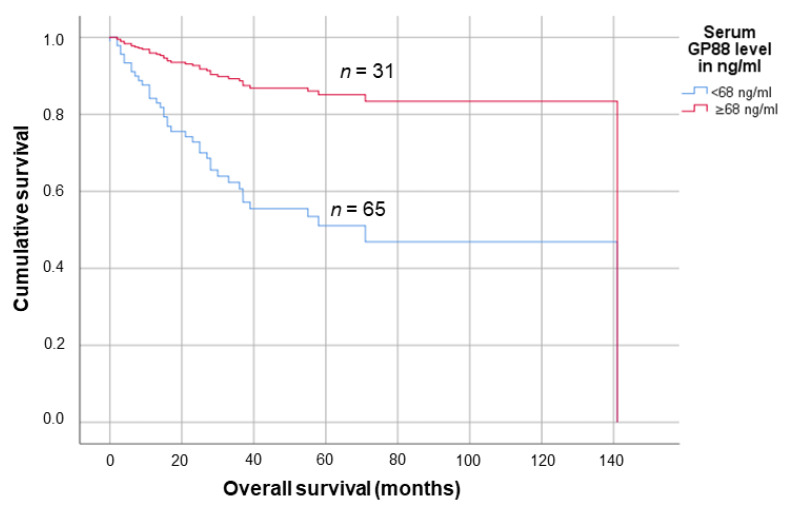
For subsequent survival analyses, an optimized cut-off according to the Youden index calculated from a ROC analysis (see Figure 3), with survival of the patient as the discriminative event, was applied.
Figure 3.
ROC analysis of serum GP88 levels according to overall survival of the OSCC patients used for Youden index calculation. AUC of the ROC curve was 0.684 (95% CI: 0.577–0.792), p = 0.002.
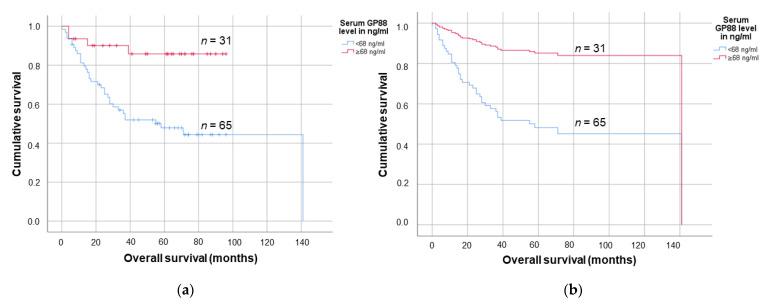
The cut-off value exhibiting the highest sensitivity and specificity in the ROC analysis was 68.0 ng/mL, with 65 patients (67.7%) exhibiting a lower serum GP88 level and 31 patients (32.3%) having a higher serum GP88 level. In the Kaplan–Meier survival analyses, a serum GP88 level below 68 ng/mL was significantly associated with shortened mean survival (75.8 months (95% CI: 60.2–91.4 months) vs. 84.8 months (95% CI: 74.6–95.1 months); p = 0.002, log-rank test (see Figure 4a).
Figure 4.
Survival analyses according to (a) Kaplan-Meier and (b) univariate Cox regression survival analyses estimating the influence of the serum GP88 level on the OSCC patients prognosis.
Furthermore, in an univariate Cox regression analysis, a lower serum GP88 level in the OSCC patients was associated with a 4.6-fold increased risk of death (95% CI: 1.6–12.9; p = 0.004; see Figure 4b). Concordantly, in multivariate Cox regression analyses (adjusted for tumor grade (G), tumor stage (T) and lymph node stage (N) of the tumor), lower serum GP88 levels were significantly associated with a 4.2-fold increased risk of death in the patient cohort (95% CI: 1.4–12.0; p = 0.008; see Figure 5; see also Table S1 and Figure S1). In TCGA analyses regarding the prognostic impact of the OSCC PGRN mRNA expression on the patients’ outcome, no association could be detected (see Figure S2). We hypothesized that the PGRN mRNA levels in the tumor tissue were not related to the corresponding PGRN serum levels; however, this matter warrants further studies.
Figure 5.
Multivariate Cox regression analysis modelling the survival of OSCC patients according to their serum GP88 levels.
3.4. Lower Serum GP88 Levels Are a Negative Prognostic Marker in Elderly OSCC Patients
Finally, we analyzed the association of serum GP88 levels with OSCC patient survival in younger (<60.5 years) and older (≥60.5 years) individuals. Age-adjusted cut-off values for both groups were calculated by Youden index optimization, which gave an unchanged cut-off value for the younger patients (68.0 ng/mL) while the cut-off for older patients was lower (65.0 ng/mL). Uni- and multivariate Cox regression analyses revealed that in the older patient group, the relative risk of death was significantly increased for those with lower serum GP88 levels (RR = 5.74 and 5.45, respectively, see Table 2), while in younger OSCC patients, serum GP88 levels had no significant impact on patient survival.
Table 2.
Uni- and multivariate Cox Regression analyses on the impact of serum GP88 levels in younger (<60.5 years) and elderly (≥60.5 years).
| OSCC Patients | GP88 Levels | Univariate Cox Regression Analysis | Multivariate Cox Regression Analysis | ||||
|---|---|---|---|---|---|---|---|
| p | RR (95% CI) | n | p | RR (95% CI) | n | ||
| OSCC patients < 60.5 years |
Serum GP88 level < 68.0 ng/mL | 0.118 | 3.26 (0.74–14.39) | 33 | 0.261 | 2.4 (0.52–11.24) | 33 |
| Serum GP88 level ≥ 68.0 ng/mL | reference | 16 | reference | 16 | |||
| OSCC patients ≥ 60.5 years |
Serum GP88 level < 65.0 ng/mL | 0.019 | 5.74 (1.33–24.72) | 32 | 0.027 | 5.45 (1.22–24.39) | 32 |
| Serum GP88 level ≥ 65.0 ng/mL | reference | 15 | reference | 15 | |||
Abbreviations: CI, confidence interval.
Additional analysis regarding the prognostic impact of GP88 in females vs males, T1/2 vs. T3/4, N0 vs. N+, and patients with vs. patients without radiotherapy are given in the Supplementary Tables S2–S5. Interestingly, lower GP88 serum levels were only a significant prognostic factor in males, while in female OSCC patients this connection was not significant, probably due to low total numbers (see Table S2). In an OSCC exhibiting T1/2 or N0, a lower GP88 serum level was also a significant factor for a worse outcome (see Table S3 and S4), while radiotherapy did not influence the predictive power of serum GP88 levels (see Table S5).
4. Discussion
In this study, we measured the serum GP88 level in patients with an oral squamous cell carcinoma (OSCC) and assessed its impact on their demographic, clinicopathological characteristics and prognosis. In our study, serum GP88 levels were not significantly different in patients with an OSCC (52.1 ng/mL) compared to those of healthy volunteers (57.6 ng/mL). Although limited information is available on GP88 serum levels for patients with an OSCC, compared those of healthy volunteers, this result is in contrast to the available literature on other tumors. Breast cancer patients showed increased GP88 serum levels having mean levels of 40.7 to 45.3 ng/mL compared to 28.7 ng/mL for age-matched healthy volunteers, with no significantly different expression due to age or ethnicity [9]. In non-small cell lung cancer patients, serum GP88 concentrations were higher (mean: 49.9 ng/mL) compared to those of healthy controls (mean: 28.4 ng/mL) [12]. Furthermore, lymphoid malignancies demonstrated higher serum GP88 levels (91.3 ng/mL) than were detected in control subjects (mean: 57.7 ng/mL) [43]. Yamamoto and colleagues also determined the mean serum GP88 level in a cohort of 417 healthy individuals to be 40.1 ng/mL, and observed no significant differences associated with age or sex [21]. However, patients with rheumatoid arthritis (RA) demonstrated higher levels of serum GP88 than were found in healthy volunteers [21]. In prostate carcinoma patients, a mean serum GP88 level of 48.7 ng/mL was determined [13]. In glioma patients, mean PGRN serum levels were higher (74.0 ng/mL) than in healthy controls (29.6 ng/mL) [44]. Concerning oral health, mean PGRN serum levels were also higher in patients with Sjögren’s syndrome in comparison to healthy controls [45]. In line with these findings, PGRN levels accompanied by soluble Oxford 40 ligand (sOX40L) levels were found to be increased in Sjögren’s syndrome patients [46].
We were able to demonstrate a significant association between a lower (< 68 ng/mL) serum GP88 level and worsened survival in OSCC patients. On the other hand, an elevated serum GP88 level at three months after surgery and chemotherapy was associated with worsened survival for ovarian cancer [47]. Therefore, it was suggested that GP88 is an independent prognostic factor for this tumor entity due to a missing correlation with age, stage and tumor grade [47]. Similar results were seen by Carlson and colleagues, who found that a higher serum GP88 level was an independent prognostic factor for ovarian cancer [48]. In hormone receptor-positive breast cancer, serum GP88 levels were positively associated with a risk of recurrence, while in hormone receptor-negative tumors no such correlation was demonstrated [11]. In metastatic breast cancer patients, a serum GP88 level >55 ng/mL was associated with a 4-fold decrease in survival [10]. In chronic lymphatic leukemia, increased serum GP88 levels were significantly correlated with worsened survival [49]. Interestingly, serum GP88 levels remained stable in non-progressing diseases over time, while it increased in patients with progressive CLL in a 20–50-month follow-up [49]. Furthermore, in a diffuse large B-cell lymphoma, a higher serum GP88 level predicted worsened survival [45]. In acute lymphoblastic leukemia, an elevated serum GP88 level was not associated with overall survival, but showed a correlation with disease-free survival [50]. Regarding non-malignancies, in community-acquired pneumonia a higher serum GP88 level was also associated with an earlier patient’s death [51]. Taken together, in all studied tumors except an OSCC, higher serum GP88 levels were associated with worsened survival. One explanation may be that GP88 is linked to metastasis [34,52] in several tumors, which is frequently associated with a higher aggressiveness of the respective tumor. Taken together, there was only one patient in our cohort who had distant metastases while 41 (38.7%) had nodal metastases. However, lymph node metastasis was not associated with patient survival in our cohort. Although it is a reliable and applicable predictor of prognosis in patients suffering from an OSCC [53,54], it might not predict prognosis accurately in all cases. After demonstrating that GP88 is an independent prognostic marker in our cohort, we propose it as a promising additive molecular factor for identifying aggressive OSCC subtypes including in the early stages. On a biological level, increased GP88 expression may have beneficial anti-inflammatory effects because it targets tumor necrosis factor receptors (TNFRs), thereby diminishing TNFα action [55,56] and resulting in decreased tumor aggressiveness. This is in agreement with reports showing that increased salivary TNFα and other cytokine levels are associated with an OSCC and higher disease stages [57,58]. In addition, GP88 was shown to play an anti-inflammatory role in an acute lung injury model at increasing regulatory T cells (Tregs) and interleukin- (IL-) 10 levels [59]. This finding further supports the general hypothesis that GP88 as a multifaceted immune-regulatory molecule is involved in acute and chronic inflammation [60]. Inflammation is one of the hallmarks of cancer [61]. As stated above, GP88 exerts an anti-inflammatory action by binding to TNFR1, which antagonizes the pro-inflammatory action of TNF-α [55], which affects, regulates and augments TGF-β1-induced EMT [62,63]. EMT is part of another hallmark of cancer: invasion and metastasis [61]. GP88 binding to TNFR1 also antagonizes the pro-inflammatory action of IL-1β [60]. Both TNF-α and IL-1β are also considered to be possible indicators of malignant transformation in oral disorders [64]. Furthermore, Liu et al. recently demonstrated, in a murine macrophage cell line, that progranulin (GP88) can significantly inhibit liposaccharide-induced NFkB/MAPK pathways by inhibiting the phosphorylation of NFκB and its nuclear translocation and the phosphorylation of ERK1 [65]. Both pathways are also characteristic of tumor development; however, the underlying crosstalk between tumor cell adaptions and metabolic or immunological pathways in an OSCC warrants further research. In our opinion, both metabolic rearrangement and immune-escape mechanisms, in combination with growth factors like GP88, may play pivotal roles in early oral carcinogenesis.
Additionally, we showed that a lower serum GP88 level is an indicator of a poor prognosis, especially in elderly (≥60.5 years) OSCC patients, but in younger patients the effect was less pronounced. Previously, we were able to demonstrate that lower serum GP88 levels were more frequently found in younger prostate cancer patients, while elevated levels were found in older patients [13]. However, in prostate carcinoma patients, elevated levels were only associated with worsened survival in younger patients [13]. However, there are still less data on the impact of serum GP88 levels on the genesis and progression of malignancies or systemic diseases in different age groups; therefore, further research is needed.
5. Conclusions
We assessed for the first time the serum levels of GP88 in patients with an oral squamous cell carcinoma. These patients did not exhibit significantly higher serum GP88 levels than found in healthy volunteers. While serum GP88 expression was not correlated to age, sex, or clinical T or N stage of the tumor, a decreased serum GP88 level was significantly associated with worsened OSCC patient survival. GP88 is a pleiotropic factor that has effects on tumorigenesis and metastasis and has an anti-inflammatory effect. Since the OSCC cases investigated here were either local or regional, it is possible that in this study the effect of GP88 was mainly the result of its inflammatory action. To sum up, we identified GP88 is an independent prognostic factor in an OSCC and as a promising biomarker in combination with both the TNM system and other prognostic markers. Measurement of serum GP88 levels, therefore, might be an interesting option for OSCC risk stratification and therapy management.
Acknowledgments
We acknowledge the financial support within the funding program Open Access Publishing by the German Research Foundation (DFG). We are grateful to Sven Wach (FA University Hospital Erlangen-Nürnberg) for his support with the statistics.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/biology10050400/s1, Figure S1: Kaplan-Meier (a;c) and multivariate Cox Regression (c;d) survival analyses of serum GP88 levels in OSCC patients with subgroups according to the Youden index optimized subgroups (a) and (b) and quartiles (c) and (d), Figure S2: Kaplan-Meier survival analyses of the PGRN transcript in head and neck squamous cell carcinoma including OSCC patients regarding the (a) overall survival, (b) the disease-specific survival or (c) the progression free interval using TGCA data, Table S1: Multivariate Cox Regression analyses regarding the impact of T stage, N status and Grading on patients survival in addition to serum GP88 levels (cut-off value: 68 ng/mL), Table S2: Uni- and multivariate Cox Regression analyses on the impact of serum GP88 levels in male and female OSCC patients, Table S3: Uni- and multivariate Cox Regression analyses on the impact of serum GP88 levels in patients with T1/2 or T3/4 tumors, Table S4: Uni- and multivariate Cox Regression analyses on the impact of serum GP88 levels in patients with N0 or N+ tumors, Table S5: Uni- and multivariate Cox Regression analyses on the impact of serum GP88 levels in patients with or without subsequent radiotherapy.
Author Contributions
Conceptualization, T.G., G.S. and H.T.; data curation, S.O., H.T., A.W.E. and M.K.; formal analysis, T.G., H.T., A.W.E. and M.K.; investigation, T.S.; methodology, G.S.; project administration, T.G.; resources, M.B., G.S., S.O., A.W.E. and M.K.; supervision, T.G., S.O. and A.W.E.; validation, T.G., A.W.E. and M.K.; writing—original draft, T.G., H.T. and M.K.; Writing—review & editing, T.G., T.S., M.B., G.S., S.O., H.T., A.W.E. and M.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the local ethics committee of the Medical Faculty of the Martin Luther University Halle-Wittenberg (Ethical registry 210/19.08.09/10).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data can be obtained from the authors on reasonable behalf.
Conflicts of Interest
GS is co-founder and CEO of A&G Pharmaceutical Inc., Columbia, Maryland, USA. The other authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fitzmaurice C., Allen C., Barber R.M., Barregard L., Bhutta Z.A., Brenner H., Dicker D.J., Chimed-Orchir O., Dandona R., Dandona L., et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3:524–548. doi: 10.1001/jamaoncol.2016.5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zizzari V.L., Zara S., Tetè G., Vinci R., Gherlone E., Cataldi A. Biologic and clinical aspects of integration of different bone substitutes in oral surgery: A literature review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016;122:392–402. doi: 10.1016/j.oooo.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Probst F.A., Fliefel R., Burian E., Probst M., Eddicks M., Cornelsen M., Riedl C., Seitz H., Aszódi A., Schieker M., et al. Bone regeneration of minipig mandibular defect by adipose derived mesenchymal stem cells seeded tri-calcium phosphate- poly(D,L-lactide-co-glycolide) scaffolds. Sci. Rep. 2020;10:2062. doi: 10.1038/s41598-020-59038-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gherlone E.F., Capparé P., Tecco S., Polizzi E., Pantaleo G., Gastaldi G., Grusovin M.G. Implant Prosthetic Rehabilitation in Controlled HIV-Positive Patients: A Prospective Longitudinal Study with 1-Year Follow-Up. Clin. Implant Dent. Relat. Res. 2016;18:725–734. doi: 10.1111/cid.12353. [DOI] [PubMed] [Google Scholar]
- 5.Fliefel R., Ehrenfeld M., Otto S. Induced pluripotent stem cells (iPSCs) as a new source of bone in reconstructive surgery: A systematic review and meta-analysis of preclinical studies. J. Tissue Eng. Regen. Med. 2018;12:1780–1797. doi: 10.1002/term.2697. [DOI] [PubMed] [Google Scholar]
- 6.Capparè P., Tetè G., Sberna M.T., Panina-Bordignon P. The Emerging Role of Stem Cells in Regenerative Dentistry. Curr. Gene Ther. 2020;20:259–268. doi: 10.2174/1566523220999200818115803. [DOI] [PubMed] [Google Scholar]
- 7.Eckert A.W., Wickenhauser C., Salins P.C., Kappler M., Bukur J., Seliger B. Clinical relevance of the tumor microenvironment and immune escape of oral squamous cell carcinoma. J. Transl. Med. 2016;14:85. doi: 10.1186/s12967-016-0828-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Serrero G., Hicks D. Measurement of Circulating Progranulin (PGRN/GP88/GEP) by Enzyme-Linked Immunosorbent Assay and Application in Human Diseases. Methods Mol. Biol. 2018;1806:95–105. doi: 10.1007/978-1-4939-8559-3_7. [DOI] [PubMed] [Google Scholar]
- 9.Tkaczuk K.R., Yue B., Zhan M., Tait N., Yarlagadda L., Dai H., Serrero G. Increased Circulating Level of the Survival Factor GP88 (Progranulin) in the Serum of Breast Cancer Patients When Compared to Healthy Subjects. Breast Cancer. 2011;5:155–162. doi: 10.4137/BCBCR.S7224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tkaczuk K.H.R., Hawkins D., Yue B., Hicks D., Tait N., Serrero G. Association of Serum Progranulin Levels with Disease Progression, Therapy Response and Survival in Patients with Metastatic Breast Cancer. Clin. Breast Cancer. 2020;20:220–227. doi: 10.1016/j.clbc.2019.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koo D.H., Park C.-Y., Lee E.S., Ro J., Oh S.W. Progranulin as a prognostic biomarker for breast cancer recurrence in patients who had hormone receptor-positive tumors: A cohort study. PLoS ONE. 2012;7:e39880. doi: 10.1371/journal.pone.0039880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Edelman M.J., Feliciano J., Yue B., Bejarano P., Ioffe O., Reisman D., Hawkins D., Gai Q., Hicks D., Serrero G. GP88 (progranulin): A novel tissue and circulating biomarker for non-small cell lung carcinoma. Hum. Pathol. 2014;45:1893–1899. doi: 10.1016/j.humpath.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greither T., Fischer K., Theil G., Marcou M., Holzhausen H.-J., Weigelt K., Serrero G., Hicks D., Yue B., Fornara P., et al. Expression of GP88 (progranulin) in serum of prostate cancer patients is associated with Gleason scores and overall survival. Cancer Manag. Res. 2018;10:4173–4180. doi: 10.2147/CMAR.S172069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pan C.-X., Kinch M.S., Kiener P.A., Langermann S., Serrero G., Le S., Corvera J., Sweeney C.J., Li L., Zhang S., et al. PC cell-derived growth factor expression in prostatic intraepithelial neoplasia and prostatic adenocarcinoma. Clin. Cancer Res. 2004;10:1333–1337. doi: 10.1158/1078-0432.CCR-1123-03. [DOI] [PubMed] [Google Scholar]
- 15.Sleegers K., Brouwers N., van Damme P., Engelborghs S., Gijselinck I., van der Zee J., Peeters K., Mattheijssens M., Cruts M., Vandenberghe R., et al. Serum biomarker for progranulin-associated frontotemporal lobar degeneration. Ann. Neurol. 2009;65:603–609. doi: 10.1002/ana.21621. [DOI] [PubMed] [Google Scholar]
- 16.Schofield E.C., Halliday G.M., Kwok J., Loy C., Double K.L., Hodges J.R. Low serum progranulin predicts the presence of mutations: A prospective study. J. Alzheimers Dis. 2010;22:981–984. doi: 10.3233/JAD-2010-101032. [DOI] [PubMed] [Google Scholar]
- 17.Youn B.-S., Bang S.-I., Klöting N., Park J.W., Lee N., Oh J.-E., Pi K.-B., Lee T.H., Ruschke K., Fasshauer M., et al. Serum progranulin concentrations may be associated with macrophage infiltration into omental adipose tissue. Diabetes. 2009;58:627–636. doi: 10.2337/db08-1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matsubara T., Mita A., Minami K., Hosooka T., Kitazawa S., Takahashi K., Tamori Y., Yokoi N., Watanabe M., Matsuo E.-I., et al. PGRN is a key adipokine mediating high fat diet-induced insulin resistance and obesity through IL-6 in adipose tissue. Cell Metab. 2012;15:38–50. doi: 10.1016/j.cmet.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Tanaka A., Tsukamoto H., Mitoma H., Kiyohara C., Ueda N., Ayano M., Ohta S.-i., Inoue Y., Arinobu Y., Niiro H., et al. Serum progranulin levels are elevated in patients with systemic lupus erythematosus, reflecting disease activity. Arthritis Res. Ther. 2012;14:R244. doi: 10.1186/ar4087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qiu F., Song L., Ding F., Liu H., Shu Q., Yang N., Liu W., Li X. Expression level of the growth factor progranulin is related with development of systemic lupus erythematosus. Diagn. Pathol. 2013;8:88. doi: 10.1186/1746-1596-8-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yamamoto Y., Takemura M., Serrero G., Hayashi J., Yue B., Tsuboi A., Kubo H., Mitsuhashi T., Mannami K., Sato M., et al. Increased serum GP88 (Progranulin) concentrations in rheumatoid arthritis. Inflammation. 2014;37:1806–1813. doi: 10.1007/s10753-014-9911-4. [DOI] [PubMed] [Google Scholar]
- 22.Cerezo L.A., Kuklová M., Hulejová H., Vernerová Z., Kaspříková N., Veigl D., Pavelka K., Vencovský J., Šenolt L. Progranulin Is Associated with Disease Activity in Patients with Rheumatoid Arthritis. Mediat. Inflamm. 2015;2015:740357. doi: 10.1155/2015/740357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou J., Gao G., Crabb J.W., Serrero G. Purification of an autocrine growth factor homologous with mouse epithelin precursor from a highly tumorigenic cell line. J. Biol. Chem. 1993;268:10863–10869. doi: 10.1016/S0021-9258(18)82064-6. [DOI] [PubMed] [Google Scholar]
- 24.He Z., Bateman A. Progranulin gene expression regulates epithelial cell growth and promotes tumor growth in vivo. Cancer Res. 1999;59:3222–3229. [PubMed] [Google Scholar]
- 25.Lu R., Serrero G. Inhibition of PC cell-derived growth factor (PCDGF, epithelin/granulin precursor) expression by antisense PCDGF cDNA transfection inhibits tumorigenicity of the human breast carcinoma cell line MDA-MB-468. Proc. Natl. Acad. Sci. USA. 2000;97:3993–3998. doi: 10.1073/pnas.97.8.3993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheung S.T., Wong S.Y., Leung K.L., Chen X., So S., Ng I.O., Fan S.T. Granulin-epithelin precursor overexpression promotes growth and invasion of hepatocellular carcinoma. Clin. Cancer Res. 2004;10:7629–7636. doi: 10.1158/1078-0432.CCR-04-0960. [DOI] [PubMed] [Google Scholar]
- 27.Abrhale T., Brodie A., Sabnis G., Macedo L., Tian C., Yue B., Serrero G. GP88 (PC-Cell Derived Growth Factor, progranulin) stimulates proliferation and confers letrozole resistance to aromatase overexpressing breast cancer cells. BMC Cancer. 2011;11:231. doi: 10.1186/1471-2407-11-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhao J., Li X., Liu J., Jiang W., Wen D., Xue H. Effect of Progranulin on Migration and Invasion of Human Colon Cancer Cells. J. Coll. Physicians Surg. Pak. 2018;28:607–611. doi: 10.29271/jcpsp.2018.08.607. [DOI] [PubMed] [Google Scholar]
- 29.Yang D., Wang L.-L., Dong T.-T., Shen Y.-H., Guo X.-S., Liu C.-Y., Liu J., Zhang P., Li J., Sun Y.-P. Progranulin promotes colorectal cancer proliferation and angiogenesis through TNFR2/Akt and ERK signaling pathways. Am. J. Cancer Res. 2015;5:3085–3097. [PMC free article] [PubMed] [Google Scholar]
- 30.Kojima Y., Ono K., Inoue K., Takagi Y., Kikuta K.-i., Nishimura M., Yoshida Y., Nakashima Y., Matsumae H., Furukawa Y., et al. Progranulin expression in advanced human atherosclerotic plaque. Atherosclerosis. 2009;206:102–108. doi: 10.1016/j.atherosclerosis.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 31.Yang D., Li R., Wang H., Wang J., Han L., Pan L., Li X., Kong Q., Wang G., Su X. Clinical implications of progranulin in gastric cancer and its regulation via a positive feedback loop involving AKT and ERK signaling pathways. Mol. Med. Rep. 2017;16:9685–9691. doi: 10.3892/mmr.2017.7796. [DOI] [PubMed] [Google Scholar]
- 32.Ong C.H.P., Bateman A. Progranulin (granulin-epithelin precursor, PC-cell derived growth factor, acrogranin) in proliferation and tumorigenesis. Histol. Histopathol. 2003;18:1275–1288. doi: 10.14670/HH-18.1275. [DOI] [PubMed] [Google Scholar]
- 33.Ding D., Li C., Zhao T., Li D., Yang L., Zhang B. LncRNA H19/miR-29b-3p/PGRN Axis Promoted Epithelial-Mesenchymal Transition of Colorectal Cancer Cells by Acting on Wnt Signaling. Mol. Cells. 2018;41:423–435. doi: 10.14348/molcells.2018.2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tangkeangsirisin W., Serrero G. PC cell-derived growth factor (PCDGF/GP88, progranulin) stimulates migration, invasiveness and VEGF expression in breast cancer cells. Carcinogenesis. 2004;25:1587–1592. doi: 10.1093/carcin/bgh171. [DOI] [PubMed] [Google Scholar]
- 35.Bandey I., Chiou S.-H., Huang A.-P., Tsai J.-C., Tu P.-H. Progranulin promotes Temozolomide resistance of glioblastoma by orchestrating DNA repair and tumor stemness. Oncogene. 2015;34:1853–1864. doi: 10.1038/onc.2014.92. [DOI] [PubMed] [Google Scholar]
- 36.Cheung P.F.Y., Cheng C.K.C., Wong N.C.L., Ho J.C.Y., Yip C.W., Lui V.C.H., Cheung A.N.Y., Fan S.T., Cheung S.T. Granulin-epithelin precursor is an oncofetal protein defining hepatic cancer stem cells. PLoS ONE. 2011;6:e28246. doi: 10.1371/journal.pone.0028246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang W., Hayashi J., Serrero G. PC cell-derived growth factor confers resistance to dexamethasone and promotes tumorigenesis in human multiple myeloma. Clin. Cancer Res. 2006;12:49–56. doi: 10.1158/1078-0432.CCR-05-0929. [DOI] [PubMed] [Google Scholar]
- 38.Pizarro G.O., Zhou X.C., Koch A., Gharib M., Raval S., Bible K., Jones M.B. Prosurvival function of the granulin-epithelin precursor is important in tumor progression and chemoresponse. Int. J. Cancer. 2007;120:2339–2343. doi: 10.1002/ijc.22559. [DOI] [PubMed] [Google Scholar]
- 39.Zhu J., Nathan C., Jin W., Sim D., Ashcroft G.S., Wahl S.M., Lacomis L., Erdjument-Bromage H., Tempst P., Wright C.D., et al. Conversion of proepithelin to epithelins: Roles of SLPI and elastase in host defense and wound repair. Cell. 2002;111:867–878. doi: 10.1016/S0092-8674(02)01141-8. [DOI] [PubMed] [Google Scholar]
- 40.Yin F., Banerjee R., Thomas B., Zhou P., Qian L., Jia T., Ma X., Ma Y., Iadecola C., Beal M.F., et al. Exaggerated inflammation, impaired host defense, and neuropathology in progranulin-deficient mice. J. Exp. Med. 2010;207:117–128. doi: 10.1084/jem.20091568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eckert A.W., Horter S., Bethmann D., Kotrba J., Kaune T., Rot S., Bache M., Bilkenroth U., Reich W., Greither T., et al. Investigation of the Prognostic Role of Carbonic Anhydrase 9 (CAIX) of the Cellular mRNA/Protein Level or Soluble CAIX Protein in Patients with Oral Squamous Cell Carcinoma. Int. J. Mol. Sci. 2019;20:375. doi: 10.3390/ijms20020375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rot S., Kaune T., Taubert H., Greither T., Kotrba J., Güttler A., Wichmann H., Bilkenroth U., Wienke A., Al-Nawas B., et al. Prognostic impact of mRNA levels of LGR5 transcript variants in OSCC patients. BMC Cancer. 2019;19:155. doi: 10.1186/s12885-019-5327-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yamamoto Y., Goto N., Takemura M., Yamasuge W., Yabe K., Takami T., Miyazaki T., Takeuchi T., Shiraki M., Shimizu M., et al. Association between increased serum GP88 (progranulin) concentrations and prognosis in patients with malignant lymphomas. Clin. Chim. Acta. 2017;473:139–146. doi: 10.1016/j.cca.2017.07.024. [DOI] [PubMed] [Google Scholar]
- 44.Wang M., Li G., Yin J., Lin T., Zhang J. Progranulin overexpression predicts overall survival in patients with glioblastoma. Med. Oncol. 2012;29:2423–2431. doi: 10.1007/s12032-011-0131-6. [DOI] [PubMed] [Google Scholar]
- 45.Zhang N., Yang N., Chen Q., Qiu F., Li X. Upregulated expression level of the growth factor, progranulin, is associated with the development of primary Sjögren’s syndrome. Exp. Ther. Med. 2014;8:1643–1647. doi: 10.3892/etm.2014.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Qi X., Guo H., Sun C., Tian Y., Ding M., Yang Y., Jin H. Clinical significance of progranulin correlated with serum soluble Oxford 40 ligand in primary Sjögren’s syndrome. Medicine. 2020;99:e19967. doi: 10.1097/MD.0000000000019967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Han J.J., Yu M., Houston N., Steinberg S.M., Kohn E.C. Progranulin is a potential prognostic biomarker in advanced epithelial ovarian cancers. Gynecol. Oncol. 2011;120:5–10. doi: 10.1016/j.ygyno.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carlson A.M., Maurer M.J., Goergen K.M., Kalli K.R., Erskine C.L., Behrens M.D., Knutson K.L., Block M.S. Utility of progranulin and serum leukocyte protease inhibitor as diagnostic and prognostic biomarkers in ovarian cancer. Cancer Epidemiol. Biomark. Prev. 2013;22:1730–1735. doi: 10.1158/1055-9965.EPI-12-1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Göbel M., Eisele L., Möllmann M., Hüttmann A., Johansson P., Scholtysik R., Bergmann M., Busch R., Döhner H., Hallek M., et al. Progranulin is a novel independent predictor of disease progression and overall survival in chronic lymphocytic leukemia. PLoS ONE. 2013;8:e72107. doi: 10.1371/journal.pone.0072107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.El-Ghammaz A.M.S., Azzazi M.O., Mostafa N., Hegab H.M., Mahmoud A.A. Prognostic significance of serum progranulin level in de novo adult acute lymphoblastic leukemia patients. Clin. Exp. Med. 2020;20:269–276. doi: 10.1007/s10238-020-00610-x. [DOI] [PubMed] [Google Scholar]
- 51.Luo Q., He X., Zheng Y., Ning P., Xu Y., Yang D., Shang Y., Gao Z. Elevated progranulin as a novel biomarker to predict poor prognosis in community-acquired pneumonia. J. Infect. 2020;80:167–173. doi: 10.1016/j.jinf.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 52.Li G., Dong T., Yang D., Gao A., Luo J., Yang H., Wang L. Progranulin promotes lymphangiogenesis through VEGF-C and is an independent risk factor in human esophageal cancers. Hum. Pathol. 2018;75:116–124. doi: 10.1016/j.humpath.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 53.Taghavi N., Yazdi I. Prognostic factors of survival rate in oral squamous cell carcinoma: Clinical, histologic, genetic and molecular concepts. Arch. Iran. Med. 2015;18:314–319. [PubMed] [Google Scholar]
- 54.Ong W., Zhao R., Lui B., Tan W., Ebrahimi A., Clark J.R., Soo K.-C., Tan N.-C., Tan H.-K., Iyer N.G. Prognostic significance of lymph node density in squamous cell carcinoma of the tongue. Head Neck. 2016;38(Suppl. 1):E859–E866. doi: 10.1002/hed.24113. [DOI] [PubMed] [Google Scholar]
- 55.Tang W., Lu Y., Tian Q.-Y., Zhang Y., Guo F.-J., Liu G.-Y., Syed N.M., Lai Y., Lin E.A., Kong L., et al. The growth factor progranulin binds to TNF receptors and is therapeutic against inflammatory arthritis in mice. Science. 2011;332:478–484. doi: 10.1126/science.1199214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li X., Zuo Z., Chen Q., Li J., Tang W., Yang P. Progranulin is highly expressed in patients with chronic periodontitis and protects against experimental periodontitis in rats. J. Periodontol. 2018;89:1418–1427. doi: 10.1002/JPER.18-0132. [DOI] [PubMed] [Google Scholar]
- 57.Lee L.T., Wong Y.K., Hsiao H.Y., Wang Y.W., Chan M.Y., Chang K.W. Evaluation of saliva and plasma cytokine biomarkers in patients with oral squamous cell carcinoma. Int. J. Oral Maxillofac. Surg. 2018;47:699–707. doi: 10.1016/j.ijom.2017.09.016. [DOI] [PubMed] [Google Scholar]
- 58.Deepthi G., Nandan S.R.K., Kulkarni P.G. Salivary Tumour Necrosis Factor-α as a Biomarker in Oral Leukoplakia and Oral Squamous Cell Carcinoma. Asian Pac. J. Cancer Prev. 2019;20:2087–2093. doi: 10.31557/APJCP.2019.20.7.2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen Y.-Q., Wang C.-J., Xie K., Lei M., Chai Y.-S., Xu F., Lin S.-H. Progranulin Improves Acute Lung Injury through Regulating the Differentiation of Regulatory T Cells and Interleukin-10 Immunomodulation to Promote Macrophage Polarization. Mediat. Inflamm. 2020;2020:9704327. doi: 10.1155/2020/9704327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jian J., Konopka J., Liu C. Insights into the role of progranulin in immunity, infection, and inflammation. J. Leukoc. Biol. 2013;93:199–208. doi: 10.1189/jlb.0812429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 62.Yan C., Grimm W.A., Garner W.L., Qin L., Travis T., Tan N., Han Y.-P. Epithelial to mesenchymal transition in human skin wound healing is induced by tumor necrosis factor-alpha through bone morphogenic protein-2. Am. J. Pathol. 2010;176:2247–2258. doi: 10.2353/ajpath.2010.090048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhou C., Liu J., Tang Y., Liang X. Inflammation linking EMT and cancer stem cells. Oral Oncol. 2012;48:1068–1075. doi: 10.1016/j.oraloncology.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 64.Dikova V.R., Principe S., Bagan J.V. Salivary inflammatory proteins in patients with oral potentially malignant disorders. J. Clin. Exp. Dent. 2019;11:e659–e664. doi: 10.4317/jced.55917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu L., Guo H., Song A., Huang J., Zhang Y., Jin S., Li S., Zhang L., Yang C., Yang P. Progranulin inhibits LPS-induced macrophage M1 polarization via NF-кB and MAPK pathways. BMC Immunol. 2020;21:32. doi: 10.1186/s12865-020-00355-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data can be obtained from the authors on reasonable behalf.