Abstract
Objective: To describe the available knowledge on vulvo-perineal endometriosis including its diagnosis, clinical management and recurrence rate.
Methods: We followed the PRISMA guidelines for Systematic Reviews and our study was prospectively registered with PROSPERO (CRD42020202441). The terms “Endometriosis” and “Perineum” or “Vulva” were used as keywords. Cochrane Library, Medline/Pubmed, Embase and Clinicaltrials.gov were searched. Papers in English, Spanish, Portuguese, French or Italian from inception to July 30, 2020 were considered. Reference lists of included articles and other literature source such as Google Scholar were also manually scrutinized in order to identify other relevant studies. Two independent reviewers screened potentially eligible studies according to inclusion criteria.
Results: Out of 539 reports, 90 studies were eligible including a total of 283 patients. Their mean age was 32.7 ± 7.6 years. Two hundred sixty-three (95.3%) presenting with vulvo-perineal endometriosis have undergone either episiotomy, perineal trauma or vaginal injury or surgery. Only 13 patients (4.7%) developed vulvo-vaginal endometriosis spontaneously i.e., without any apparent condition favoring it. The reasons that motivated the patients to take medical advice were vulvo-perineal cyclical pain increasing during menstruations (98.2% of the patients, n = 278). Out of the 281 patients for whom a clinical examination was described, 274 patients (97.5%) showed a vulvo-perineal nodule, mass or swelling while six presented with bluish cutaneous lesions (2.1%) and 1 with bilateral polyps of the labia minora (0.4%). All but one patients underwent surgical excision of their lesions but only 88 patients (28.1%) received additional hormonal therapy. The recurrence rate was 10.2% (29 patients) considering a median follow-up period of 10 months (based on 61 studies).
Conclusion: In conclusion, vulvo-perineal endometriosis is a rare entity with approximately 300 cases reported in the literature since 1923. With the available knowledge shown in this systematic review, we encourage all practitioners to think about perineal endometriosis in case of perineal cyclical pain with or without previous perineal damage. Diagnosis should be done with clinical exam, perineal ultrasound and pelvic MRI when available. In case of anal sphincter involvement, perianal ultrasound should be performed. Surgical excision of the lesion should be realized in order to remove the lesion and to confirm the diagnosis histologically. Hormonal treatment could be proposed to attempt to decrease the size of a large lesion before surgery or to avoid recurrence of the lesion. As evidence-based approach to the diagnosis, treatment and recurrence rate of affected patients remains a challenge given its low prevalence, the variations in management found in the articles included and the limited quality of available studies, we suggest that a prospective database on vulvo-perineal endometriosis should be generated to increase knowledge but also awareness among healthcare professionals and optimize patients' care.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier: CRD42020202441.
Keywords: endometriosis, perineum, vulva, episiotomy, perineal pain, cyclical pain, perineal nodule, extrapelvic endometriosis
Introduction
Endometriosis is a complex benign disease characterized by an estrogen-dependent chronic inflammatory process and is defined as the presence of endometrial glands and stroma-like tissue outside the uterine cavity, most often located in the pelvis (1), although extrapelvic sites have been described, including the urinary and gastro-intestinal tracts, the nervous system, the thoracic cavity and diaphragm as well as some (sub-)cutaneous sites (2–5). It occurs in ~10% of women of reproductive-age and in 35–50% of women with infertility and chronic pelvic pain (6–8).
While extrapelvic endometriosis is a relatively uncommon condition, accounting for ~12% of all cases of endometriosis (9), perineal endometriosis is an even rarer entity. Cutaneous and subcutaneous endometriotic lesions have been observed in surgical scars following laparoscopy, laparotomy, vulvo-vaginal surgery, episiotomy and obstetrical lacerations whether surgically repaired or not (3). Perineal endometriosis may involve the skin and/or subcutaneous tissue of the vulva and perineum but also the perianal sphincteric muscular tissue (10). Following the first case of perineal endometriosis reported in 1923 (11), most of what is known of this commonly misdiagnosed entity comes from case reports published over the past 60–70 years.
Our study aims to identify all reported cases of vulvo-perineal endometriosis published in the literature in order to describe diagnostic processes, treatments and recurrence rates of this uncommon type of endometriosis and help practitioners to achieve prompt diagnosis and optimize patients' outcomes.
Methods
This study followed the principles of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement (12) and was prospectively registered within the International Prospective Register of Systematic Review (PROSPERO) on the 4th of August 2020 (number CRD42020202441).
The following search engines and electronic databases were searched on July 30, 2020 by one author (CM): Cochrane Library, Medline/Pubmed, Embase and Clinicaltrials.gov. The terms “Endometriosis” and “Perineum” or “Vulva” were used as keywords to recover all possible publications. Table 1 shows the queries and record numbers for the different databases used. No restrictions regarding language, type or date of publication were initially applied. Reference lists of included articles and other literature sources such as Google Scholar were also manually scrutinized in order to identify additional relevant studies. Articles in English, Spanish, Portuguese, French or Italian were considered. Review articles and studies describing exclusively lesions involving the abdominal wall or the inguinal area, or malignant transformation of endometriosis were excluded. Two reviewers (CM, ZCA) independently screened titles and abstracts of the search output to identify potentially eligible studies and cross-examined their results.
Table 1.
Description of queries in the different databases.
| Query | Results | |
|---|---|---|
| Pubmed/Medline | (“Endometriosis”[MeSH Terms] OR “Endometriosis”[All Fields]) AND (“perineum”[MeSH Terms] OR “perineum”[All Fields] OR “vulva” [MeSH Terms] OR “vulva”[All Fields]) | 171 |
| Embase | (“Endometriosis”/exp OR endometriosis) AND (“perineum”/exp OR perineum OR “vulva”/exp OR vulva) | 362 |
| Cochrane Library | (endometriosis):ti,ab,kw AND perineum):ti,ab,kw (Word variations have been searched) | 1 |
| (endometriosis):ti,ab,kw AND vulva):ti,ab,kw (Word variations have been searched) | 2 | |
| ClinicalTrials.gov | (“Endometriosis” AND “Perineum” OR “vulva”) | 3 |
| 539 |
Results
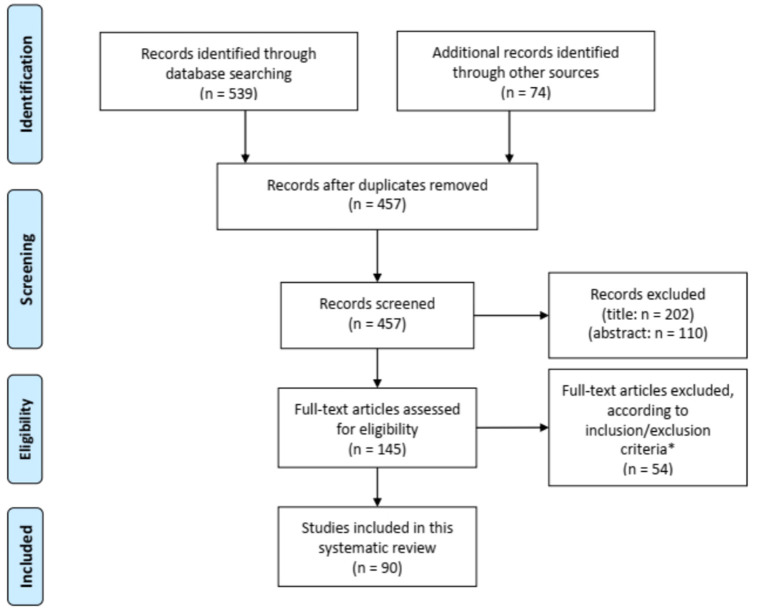
Figure 1 shows the flow chart of the literature search. Our search strategy yielded a total of 457 potentially eligible studies. Ninety articles published between 1956 and 2020 were eventually included in our review. Eighty-three articles were case reports or case series including one to eight patients (2, 9, 11, 13–90) and seven studies described retrospective cohorts of 14–36 patients (10, 91–96). The main results of the eight retrospectives studies can be found in Table 2.
Figure 1.
Flow diagram for study selection. *Seven articles could not be retrieved despite contacting the corresponding author.
Table 2.
Data of the literature about vulvo-perineal endometriosis describing more than 10 cases.
| Number of cases | Mean age (range) | Symptoms | Vulvo-perineal scar (n) | IAS | Work-up (n) | Duration of symptoms (range) (months) | Latent period (range) (months) | Treatment | Other endometriosis spots | Recurrence | Follow-up period (months) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Perineal nodule (%) | Progressive and cyclical pain (%) | Other (%) | Surgical | Medical | |||||||||||
| Paull et al. (91) | 15 | 28 (19-34) | 100 | 100 | NA | Episiotomy scar (15) | NA | NA | NA | 21 (1-60) | Excision | No | NA | 0 | 9: 12–48, 6: NA |
| Nominato et al. (92) | 21 | 30.8 (1-48) | 79 | 80 | NA | Episiotomy scar (19), perineoplasty (2), perineal surgery (1) | NA | NA | 44 | Excision | No | NA | 1 | NA | |
| Zhu et al. (93) | 36 | 30.67 (23-44) | 100 | 100 | Dysmenorrhea (13.9), dyspareunia (5.6) | Episiotomy (24), perineal tear (12) | 26 | CA 125 (30), color doppler perineal ultrasound (36) | NA | 42.8 (4-156) | Complete excision (28), uncomplete (7), hormonal (1) | GnRHa 3–6 months pre or post surgery (20 with IAS) | 3 | 7 (with incomplete excision) 1 with hormonal treatment alone | 0.5–168 |
| Chen et al. (10) | 31 | 33.4 (26-43) | 100 | 100 | NA | Episiotomy scar (20), perineal lacerations (11) | 31 | CA 125, pelvic U/s, perineal U/s (5) | NA | 36 (1-204) | Complete narrow excision (30), incomplete excision (1) | NE: 10 pre- and post-op 1–6 months (GnRHa, Nemestran, DMPA), 1 GnRHa 3 months preop-Mirena post-op, 9 GnRH a pre-op 3–5 months, 2 GnRHa 4 months post-op, 8 no treatment, IE: DPMA pre- and post-op 3–6 months | 2 (ovarian endometrioma) | 2 (NE with GnRHa 3 months, IE) | 18 (6-78) |
| Li et al. (94) | 17 | 34.35 (26-57) | 100 | 100 | NA | Episiotomy scar (17) | 6 | CA 125 (15), doppler U/s (8), pelvic U/s (17), MRI (2) | 37.82 (3-152) | 46.82 (2-204) | Excision | Post-op: 4 GnRHa (3 months), 2 mifepristone 1 month, 1 progesterone | 1 | 1 | 74.23 (5-151) |
| Matalliokis et al. (95) | 14 | 32.5 (±2.9) | 92.8 | 92.8 | NA | Episiotomy scar (14) | NA | U/s (3), CT (6), MRI (7) | NA | NA | Excision | NA | 3 | 2 | NA |
| Liu et al. (96) | 35 | 33.44 (25-48) | 100 | 100 | NA | Episiotomy scar (33), opposite side of episiotomy (1), mons pubis (1) | 10 | CA125 (11), perineal U/s (15), pelvic U/s (35) | NA | 42.44 (1-120) | Complete excision ± primary sphincteroplasty | preop (7) (5 GnRHa, 1 Marvelon, 1 mifepristone), post op (17) (2 mifepristone, 15 GnRHa) | 3 (18.75%) in non GnRHa group, 1 in the gnRHa group | 7–86 | |
U/s, ultrasound; CT-scan, computerized tomography; IAS, involved anal sphincter; CNE, complete narrow excision surgical margin: 0.3–0.5 cm; DMPA, depot pedroxyprogesterone acetate; GnRHa, gonadotropin-releasing hormone agonists; NE, narrow excision.
Two hundred and eighty-three patients, with a mean age of 32.7 ± 7.6 years and an age range from 14 to 69 years at diagnosis, were included. While 263 patients (95.3%) had undergone previous episiotomy, obstetrical lacerations, whether repaired or not, perineal trauma or vaginal surgery or injury, only 13 patients (4.6%) developed spontaneous vulvo-vaginal endometriosis i.e., in the absence of the most frequently associated conditions (Table 3). Among the latter, lesions developed in the Bartholin gland in 6 cases (21, 44, 48, 62, 70, 80). Previous history wasn't described for seven patients (40, 45, 47, 74).
Table 3.
Description of previous vulvo-perineal history.
| Vulvo-perineal endometriosis | Number of patients (/283) | % |
|---|---|---|
| Spontaneous | 13 | 4.6 |
| Previous vulvo-perineal lesion | 263 | 92.9 |
| Episiotomy or obstetrical laceration | 249 | 88 |
| Bartholin cystectomy | 4 | 1.4 |
| Laparotomy (for ovarian endometriosis) | 1 | 0.4 |
| Laparotomy (for ovarian endometriosis) with hernia repair | 1 | 0.4 |
| Laser vulvar surgery | 1 | 0.4 |
| Vaginal hysterectomy | 1 | 0.4 |
| Manchester surgery for prolapse | 1 | 0.4 |
| Mile's procedure for rectal cancer | 1 | 0.4 |
| Vulvar abrasion | 1 | 0.4 |
| Vulvar hematoma post trauma | 1 | 0.4 |
| Vulvar ulceration | 1 | 0.4 |
| Removal of Nuck canal remnant | 1 | 0.4 |
| Not specified | 7 | 2.5 |
The median latent period i.e., the time between perineal trauma or surgery and occurrence of symptoms was 2.5 years, ranging from 1 month to 14 years.
Incidence rates were reported in two studies, ranging between 0.01 and 0.06% after vaginal deliveries (84, 92). The incidence of anal sphincter involvement was reported only by Chen et al. who described a 0.37% incidence of perineal endometriosis among women treated surgically for endometriosis regardless of its location with 0.18% of patients presenting with anal sphincter involvement (10).
Main complaints were vulvar and/or perineal cyclical pain increasing during menstruations for 278 patients (98.2%). Five patients (1.8%) presented exclusively with other symptoms, e.g., painful bilateral polyps of the labia minora, cyclical bleeding, anal pruritus or infertility. Concurrent pelvic endometriosis occurred in 19 patients (6.1%). The median duration of symptoms before medical care was 12 months, ranging from 2 weeks to 20 years.
Out of the 281 patients for whom a clinical examination was described, 274 patients (97.5%) showed a vulvo-perineal nodule, mass or swelling, including one with vulvar ulceration, while 6 presented with bluish cutaneous lesions (2.1%) and one with bilateral polyps of the labia minora (0.4%).
The different workups conducted in the 283 patients are described in Table 4. The most common workup assessment was the serum level of cancer antigen 125 (CA125), measured in 105 patients (37.1%), followed by pelvic ultrasound (34.9%) and perineal ultrasound (27.%). Other workup examinations were performed in <10% of the cases. Slightly elevated serum levels of CA125 were found in 6.5–46.7% of patients with perineal endometriosis (10, 93, 94, 96). Pelvic ultrasound was mostly performed to exclude pelvic endometriosis. Perineal and endoanal ultrasound (50, 93, 94, 96), as well as magnetic resonance imaging (MRI) (94, 95) helped to describe precisely the size of the lesions and to diagnose and assess the extent of the anal sphincter involvement. Well-defined hypoechoic solid or cystic masses with hyperechoic spots or strands representing fibrosis within the scar tissue have been described (79, 97). Increased vascularity and spiculated borders with a single vessel entering the nodule from the periphery has also been observed (98). Fine needle aspiration cytology (FNAC) or biopsy of the lesions was reported in 19 patients (6.1%) and confirmed the diagnosis before surgical excision in 16 patients (84.2%) while it didn't confirm the presence of endometriosis in two patients [granulation tissue and old hemorrhage (22, 63)]. One biopsy result was not described (36).
Table 4.
Work-up for vulvo-perineal endometriosis.
| Number of patients (/283) | % | |
|---|---|---|
| Serum level of CA 125 | 105 | 37.1 |
| Pelvic Ultrasound | 99 | 34.9 |
| Perineal ultrasound | 78 | 27.6 |
| MRI | 19 | 6.7 |
| Biopsy | 17 | 6 |
| CT-scan | 9 | 3.2 |
| Endoanal ultrasound | 8 | 2.8 |
| Sigmoidoscopy | 7 | 2.5 |
| Anal Manometry | 4 | 1.4 |
| FNAC | 2 | 0.7 |
| Dermoscopy | 1 | 0.4 |
CA 125, cancer Antigen 125; MRI, magnetic resonance imaging; CT-scan, Computerized Tomography scan; FNAC, fine needle aspiration cytology.
All but one patients (282/283) underwent surgical excision of the perineal mass. In the patient where the perineal lesion was left, a total abdominal hysterectomy with bilateral salpingo-oophorectomy was performed to induce menopause and decrease pain-related symptoms (69). The detailed technique of the different surgical procedures was usually not described, except in two studies mentioning the following specifications i.e., narrow excision with deep surgical margins of 0.3–0.5 cm (10) or complete excision with a surgical margin of 0.5–1 cm (94). “Excision” or “surgical excision” without further details was mentioned for 148 patients (52.5%). Amongst the remainder, 73 had a “complete excision” (25.6%), 32 benefited from a “complete narrow excision” (11.3%) and 10 patients from a “wide excision” (3.5%). Eight surgeries were described as “incomplete” (2.8%). Histological findings confirmed endometriosis in all cases. Eighty-eight patients (28.1%) received hormonal therapy, either pre-or post-operatively for 3–6 months (Table 5).
Table 5.
Hormonal therapy.
| Année | Number of patients | Age | Rx Pre-surgery | Time (month) | Traitement | Rx Post-surgery | Time | Follow-up (months) | Récurrence |
|---|---|---|---|---|---|---|---|---|---|
| Shin et al. (67) | 1 | 33 | Danazol and GnRHa | 2 | Radical hysterectomy + bilateral oophorectomy with partial excision with cautherization of perineal lesions | local estrogens | NA | 6 | No |
| Liang et al. (2) | 1 | 30 | Danazol 800 mg | 1 | Excision | / | / | 12 | No |
| 1 | 33 | Danazol irregularly | NA | Excision | / | / | 12 | No | |
| Katz et al. (61) | 1 | 14 | Oral contraceptives | NA | Excision | / | / | 4 | No |
| Kang et al. (31) | 1 | 32 | GnRHa | 3 | Excision | / | / | NA | NA |
| Yogini et al. (35) | 1 | 34 | / | / | Drainage and excision | GnRHa | NA | NA | NA |
| Kahraman et al. (38) | 1 | 19 | / | / | Complete excision | Oral contraceptives | 3 | 3 | 1 |
| Zhu et al. (93) | 13 | 30.67 | GnRHa | 3–6 | Complete excision | GnRHa | 3–6 | 9–168 | No |
| 7 | GnRHa | 3– 6 | Incomplete excision | GnRHa | 3–6 | 4–12 | 7 | ||
| 1 | Contraceptives 17alpha-hydroxyprogesterone caproate 250 mg im/28 days and tamoxifen 10 mg twice a day | 15 | Complete excision | Contraceptives 17alpha-hydroxyprogesterone caproate 250 mg im/28 days and tamoxifen 10 mg twice a day | 8 | 84 | 1 | ||
| Hazard et al. (14) | 1 | 15 | / | / | Excision | Oral contraceptivew | NA | NA | No |
| Ngu et al. (63) | 1 | 30 | GnRha | 3 | Excision | / | / | NA | NA |
| Ruiz de Gauna et al. (20) | 1 | 32 | / | / | Wide excision | GnRHa | 3 | NA | No |
| Chen et al. (10) | 10 | 33.4 | GnRHa, Nemestran, DMPA | 1– 6 | Narrow excision | GnRHa, Nemestran, DMPA | 1–6 | NA | No |
| 1 | GnRHa | 3 | Narrow excision | IUD-LNG | NA | NA | No | ||
| 9 | GnRHa | 3–5 | Narrow excision | / | / | 12 | 1 | ||
| 2 | / | / | Narrow excision | GnRHa | 4 | NA | No | ||
| 1 | DMPA | 3–6 | Incomplete excision | DPMA | 3–6 | 72 | 1 | ||
| Hakimi et al. (80) | 1 | 28 | / | / | Excision (difficult) | LHRH | 6 | NA | NA |
| Grimstad et al. (24) | 1 | 29 | / | / | Excision | Oral contraceptives | 65 | 72 | 1 |
| Jeyaseelan et al. (83) | 1 | 38 | / | / | Excision | GnRHa | 3 | NA | NA |
| Li et al. (94) | 4 | 34.35 | / | / | Surgical excision | GnRHa | 3 | 12 | 1 |
| 2 | / | / | Surgical excision | Mifepristone | 1 | NA | No | ||
| 1 | / | / | Surgical excision | Progesterone | NA | NA | No | ||
| Sharp et al. (90) | 1 | 39 | / | / | Large biopsy | Dienogest 2 mg | 6 months | NA | NA |
| Baba et al. (55) | 1 | 35 | / | / | Complete excision | GnRH | NA | NA | NA |
| Sharm et al. (89) | 1 | 37 | / | / | Wide excision | GnRHa | 1 | 6 | No |
| Saloum et al. (58) | 1 | 34 | / | / | Excision | GnRHa | 3 | NA | No |
| Wallace et al. (17) | 1 | 42 | / | / | Excision | Oral contraceptives | 12 | 12 | No |
| Liu et al. (96) | 1 | 34 | Marvelon | NA | Complete excision | GnRHa | 3 | 85 | No |
| 12 | 31.8 | / | / | Complete excision | GnRHa | 3–6 | 45.5 | 1 (12 months) | |
| 1 | 37 | Mifepristone | 3 | Complete excision | Mifepristone | 3 | 75 | No | |
| 1 | 38 | GnRHa | 3 | Complete excision | Mifepristone | 3 | 62 | No | |
| 2 | 34.5 | GnRHa | 3 | Complete excision | GnRH | 3 | 46 | No | |
| 2 | 30.5 | GnRHa | 3 to 5 | Complete excision | / | / | 23.5 | No | |
| 88 |
A follow-up period was mentioned in 61 studies, with a median value of 10 months (range from 1 to 108 months). Recurrent lesions have been reported in 29 patients (10.2%) and are presented in Table 6. Out of these patients with recurrence, 13 benefited from hormonal treatment pre-or post-operatively (44.8%) (nine GnRHa, three oral contraceptives, and one DMPA) while 16 didn't receive any additional treatment.
Table 6.
Recurrences of perineal endometriosis after initial treatment.
| Number of patients | ASI | Initial treatment | Follow-up (months) | |||
|---|---|---|---|---|---|---|
| Surgical | Hormonal | Duration | ||||
| Prince et al. (41) | 1 | No | Excision | No | NA | 6 |
| Trampuz et al. (76) | 1 | yes | Excision | No | NA | 3 |
| Swerdlow et al. (69) | 1 | No | TAH + BSO | No | NA | 3 |
| Gordon et al. (22) | 1 | yes | Excision | No | NA | 5 |
| Liang et al. (2) | 1 | NA | Excision | No | NA | 12 |
| Kahraman et al. (38) | 1 | No | CE | Oral contraceptives | NA | 3 |
| Nominato et al. (92) | 1 | NA | Excision | No | NA | NA |
| Eyvazzadeh et al. (19) | 1 | No | Biopsy | No | NA | 60 |
| Iqbal et al. (28) | 1 | No | Incision and drainage | No | NA | 6 |
| Zhu et al. (93) | 7 | Yes | IE | GnRHa pre or post op | 3–6 months | 4–12 |
| 1 | NA | CE | Postop contraceptive pills 17alpha-hydroxyprogesterone caproate 250 mg intramuscular injection per 28 days and tamoxifen 10 mg twice a day for 8 months | 8 months | 84 | |
| Chen et al. (10) | 1 | Yes | NE | GnRHa Pre-op | 3 months | 12 |
| 1 | Yes | IE | DMPA pre- and post-op | 3–6 months | 72 | |
| Jain et al. (32) | 2 | No | Excision | No | NA | 3–7 |
| Grimstad et al. (24) | 1 | No (clitoris) | Excision | Oral contraceptives | NA | 72 |
| Li et al. (94) | 1 | NA | CE | GnRH | 3 | 12 |
| Matalliotakis et al. (95) | 2 | NA | Excision | NA | NA | NA |
| Liu et al. (96) | 3 | No | CE | No | NA | 12–36 |
| 1 | No | CE | GnRHa post-op | 3 months | 12 | |
| 29 | ||||||
IE, incomplete excision; CE, complete excision; NE, narrow excision; TAH + BSO, total abdominal hysterectomy + bilateral salpingo-oophorectomy; GnRHA, gonadotropin-releasing hormone analog; DMPA, Depot medoxyprogesterone acetate; NA, not available.
Discussion
While vulvo-perineal endometriosis presents mostly after perineal trauma, its exact etiology remains unclear, even if major progress has been achieved in the field over the last decades. Etiopathogenesis of endometriosis has generally been related to endometrial implantation, coelomic metaplasia, lymphatic dissemination and hematogenous spread (1) and the origin of extrapelvic endometriosis is not well-deciphered. As pelvic endometriosis can be considered as three separate entities (peritoneal, ovarian and recto-vaginal (deep) lesions) with different pathogeneses (99, 100), vulvo-perineal endometriosis could potentially also be separated between cystic and nodular lesions with distinct etiologies and treatment. Direct mechanical implantation seems to be the most plausible hypothesis for explaining scar endometriosis after obstetrical and gynecological procedures. According to this theory, mechanical dissemination during normal vaginal delivery, for example, allows transplantation of viable decidual endometrial cells into the episiotomy wound or perineal tear (2, 34, 53, 93, 101). We must note that scar endometriosis may as well-rarely be seen after a number of general surgical procedures like appendicectomy, inguinal hernial repair, laparoscopic cholecystectomy or even laparoscopic gastric by-pass (9). Nevertheless, perineal endometriosis has also been described in patients without any previous vulvo-vaginal trauma. In that respect, we found 13 cases of primary perineal endometriosis without vaginal birth, previous perineal injury in the literature. Different explanations of the pathogenesis of spontaneously developing perineal endometriotic lesions have been put forward with the most likely being lymphovascular dissemination (39, 53). However, the presence of endometriosis in the labia majora could also be explained by the direct spread of pelvic endometriosis along the round ligaments or Nuck canal's remnants while a solitary focus in the Bartholin's gland could theoretically be attributed to coelomic metaplasia (57). Eventually, other factors, such as immunological, genetic and familial factors, could be involved in the pathogenesis of this disease (94, 102).
Few studies have reported the incidence or prevalence of vulvo-perineal endometriosis. After vaginal delivery, the highest incidence rate of perineal endometriosis was reported by Nominato et al. representing 0.06% of patients, compared to 0.2% abdominal scar endometriosis after cesarean section (92), while perineal endometriosis only represents a proportion of 0.37% of women treated surgically for endometriosis (10).
Besides the rarity of vulvo-perineal endometriosis, its variability in clinical presentation makes this condition hardly recognized by some healthcare professionals leading to a delayed diagnosis. Misdiagnoses have also been reported such as herpes outbreak or perianal sepsis in the presence of vulvar pain with ulcerations or perianal swelling, respectively (14, 28). For instance, we showed a mean duration of symptoms of 12 months, ranging from 2 weeks to 20 years in our review meaning that half of them had to endure their pain for more than a year before being correctly diagnosed (94).
Early diagnosis and treatment are however recommended in order to prevent adverse complications such as long-term psychological distress, progressive involvement of the surrounding and adjacent tissues such as anal sphincter or rectum and potential malignant degeneration.
A detailed medical and surgical history associated with a thorough clinical exam are of great importance for accurate diagnosis. Good clinical vulvar and vaginal examination, including speculum and bimanual examination, are primordial to fully describe the perineal lesions. Rectal examination should be performed routinely in case of perineal lesions especially if suspicion of anal sphincter involvement (ASI). Clinically, endometriosis of the perineum and vulva presents as ill-defined papule or nodule, generally hard, usually located near a surgical scar, potentially skin-colored, dark-red, brown, or blue-black cystic (10, 103). It is mainly accompanied by cyclic pain and swelling, or periodic leakage of dark colored fluid during menses attributable to the fact that endometrial implants behave like normal endometrium. Some cases show neither discoloration of the perineal skin, nor local swelling nor intermittent leakage (32). Other symptoms can include dyspareunia. Interestingly, Zhu et al. described three criteria i.e., history of past perineal tear of episiotomy during vaginal delivery, presence of a tender nodule or mass at the perineal lesion on clinical exam and history of progressive and cyclic perineal pain which when all met provide a 100% positive predictive value (93). Concomitant pelvic endometriosis was found in 6.1% of patients in our systematic review. These results concord with the literature suggesting that scar endometriosis is not a risk factor for pelvic endometriosis (104, 105).
The differential diagnosis in such patients includes, but is not limited to, anal fistula, abscesses, suture granulomas, Bartholin cysts or bartholinitis, hernias, hematoma, sebaceous cyst, lipoma, herpes, neoplastic tissue or metastatic carcinoma, traumatic neuroma, desmoid tumor and anal melanoma (9, 28, 42, 45, 46). A perineal mass discovered in menopaused women should be considered as malignant until proven otherwise. Malignant degeneration occurs infrequently for cutaneous endometriosis representing 0.3–1% of endometriosis located in surgical scars (106). It is difficult to distinguish benign from malignant perineal endometriosis based on symptoms and clinical examination and a biopsy or surgical excision will always be necessary to confirm the diagnosis of malignant transformation (13). Histological observations are dominated by endometrioid carcinoma and sarcoma (107), but can also present as dermatosarcoma, clear cell carcinoma and serous papillary cystadenocarcinoma (87, 106, 108–116). As malignant transformation appears uncertain, unpredictable and may be very delayed, long-term follow-up is recommended.
The work-up appeared to be very variable depending on the medical team dealing with the patients. It was therefore difficult to evaluate the sensibility and specificity of each exam for perineal endometriosis as most of them have been realized in only a tiny proportion of the patients in this study. Levels of serum CA125 did not seem to be effective in diagnosing perineal endometriosis since it was usually normal or slightly increased. With regard to perineal ultrasonography, variable sonographic features were seen, as it is the case for abdominal wall endometriosis, which could make the diagnostic process more challenging but it remains useful to describe precisely the size of the lesions and to assess the extent of the ASI. Preoperative endoanal ultrasonography has also been described as a reliable technique for visualizing perianal endometriosis and diagnosing ASI, enabling the surgeon to determine the extent of an operative procedure and the possible need for a sphincteroplasty (46, 86). Ultrasonographic features of the lesion are usually similar to those observed with perineal ultrasonography with the advantage that it better reveals the involvement of the anal sphincter (10). Even if only 6.1% of the patients in this review benefited from this exam, magnetic resonance imaging (MRI) could become the modality of choice for perineal imaging (117, 118) as pelvic MRI has greater sensitivity (90–92%) and specificity (91–98%) for the diagnosis of endometriomas when compared to other non-invasive methods (119, 120). Vulvo-perineal localizations are easily identified on T1-weighted fat-suppressed images as hyper-intense spots within the perineum. Multilobular mass with inner hemorrhage, localized or diffuse vulvovaginal wall thickening, hemorrhagic or spiculated masses and distortion can also be observed (94, 117). MRI also helps in assessing the extent of the anal sphincter involvement (35). Depending on the availability in each center, we suggest that pelvic and perineal ultrasound as well as MRI should be performed in all patients and associated with endoanal ultrasound when there is a suspicion of ASI.
Histology is the hallmark of diagnosis which shows endometrial glands, stroma, and hemosiderin pigment. Generally, diagnosis is easy with a microscopic examination of a standard hematoxylin and eosin (H&E)-stained slide. Immunostaining for CD10 (neprilysin, a cell-surface metalloendopeptidase expressed in normal and ectopic endometrial stroma) increases the sensitivity compared to H&E staining (17, 19). Evidencing the estrogen receptor (ER) and progesteron receptor (PR) may help to identify endometrial glands (121). Furthermore, it is important to keep in mind that cutaneous endometriotic lesions show a broad spectrum of metaplastic changes and that all types of müllerian differentiation can be discovered (122) which make the diagnosis on FNAC or biopsy challenging for the unexperimented histologists.
Treatment of vulvo-perineal endometriosis includes usually surgical excision with or without hormonal suppression (GnRHa, oral contraceptives, progestins) (2, 10, 15, 123). It seems that complete excision should be the treatment of choice as it decreases the risk of recurrence (10, 93) and could reduce consequently the risk of malignant degeneration (109). Care must be applied to avoid rupturing the mass during surgery with its consecutive risk of re-implantation or leaving endometriotic remnants. To this end, excision of surrounding fibrous tissue has been suggested (94) although recommendations with respect to the surgical technique, e.g., surgical margins needed to decrease the risk of recurrence, are not available so far. Precise description of the surgical procedure including technique and margins is most often missing and awaited in future studies. When the anal sphincter is involved, complete narrow excision or wide excision of the endometrial tissue with a good healthy margin have been proposed with primary sphincteroplasty using the apposition or overlapping technique (10). Although symptomatic relief could be achieved with hormonal intervention, complete surgical excision still remains the best treatment for perineal endometriosis and often leads to permanent cure (71). As expected, large and deep lesions to the muscle or the fascia might be more difficult to excise completely. In large lesions, complete excision of the lesion may entail a synthetic mesh placement, tissue transfer for closure after resection (124) or combined surgery with gynecologic and plastic surgeons (125). It is however important to keep in mind that endometriosis remains a benign condition allowing conservative surgery and that decaying surgery is not recommended even in very large lesions. The type of resection should be based on the patient's age and desire for future pregnancy and the decision should be made only after possible outcomes of the different approaches have been discussed with the patient (86). Some authors have suggested that wide excision with primary sphincteroplasty could be optimal in younger patients, obviating the need for additional therapy, while narrow or incomplete excision with subsequent hormonal therapy could be advantageous in older patients closer to menopause to lessen the risk of incontinence due to sphincter resection (93). 28.1% of patients in this review received hormonal treatment pre-or post-operatively. As described in pelvic endometriosis, hormonal treatment could stabilize the size of cystic lesions and reduce pain as endometriosis is an estrogen-dependent process (126–129). Some authors suggested that massive lesions with anal sphincter involvement should be treated by hormonal therapy before surgery to reduce the size of the perineal mass (63). It should be noted that perineal endometriosis persists with medical treatment alone as it was always found on histology when hormonal treatment was followed by surgical excision. Various authors have reported the administration of a gonadotropin-releasing hormone analog to prevent recurrence (10, 31, 96). When complete wide excision, as reported by Zhu et al. (14), was performed, the recurrence rate was lower (3.3%) than the overall rate of 9.3% found in our review compiling all kinds of excisions, suggesting that recurrence was presumably due to incomplete removal of the lesions rather than to the absence of hormonal treatment (14). In addition, preoperative hormone therapy did not improve outcomes compared to surgery alone in patients with ASI (10). Results on hormonal therapy for abdominal wall or abdominal scar endometriosis are similar to those presented in this review showing a possible temporary relief of symptoms or potential slight reduction of the lesions' size easing the surgical resection but the bulk of evidence shows a low degree of efficacy. Currently, available data do not comment on best practices for the perioperative management of cutaneous endometriosis (104, 105, 130–134).
The limitations of this systematic review include the level of evidence due to the nature of the studies i.e., retrospective and case reports and the important variations in clinical management of vulvo-perineal endometriosis described in the available studies such as methods of diagnosis, surgery procedure's details and hormonal therapy. At present, there are no comparative studies to provide accurate and evidence-based guidelines regarding optimal diagnostic methods, treatment options and outcomes for endometriosis involving the perineum.
Although evidence-based guidelines cannot be retrieved from this systematic review due to the reasons mentioned above, Table 7 summarizes all the suggested recommendations based on our results and on the available literature. To improve our knowledge on this rare condition, we suggest developing a international database on vulvo-perineal endometriosis. Any future study regarding this type of endometriosis should include the data described in Table 8.
Table 7.
Summary of recommendations about vulvo-perineal endometriosis.
| Early diagnosis and treatment are recommended in order to prevent adverse complications. |
| A detailed medical and surgical history associated with a thorough clinical exam should be realized (vulvar and vaginal examination with rectal examination in case of suspicion of ASI). |
| Pelvic and perineal ultrasound as well as pelvic MRI should be performed in all patients and associated with endoanal ultrasound when there is a suspicion of ASI. |
| Histology is the hallmark of diagnosis. |
| Complete excision should be the treatment of choice as it decreases the risk of recurrence and could reduce consequently the risk of malignant degeneration. |
| Hormonal treatment could be proposed to attempt to decrease the size of a large lesion before surgery or to avoid recurrence of the lesion. |
| Long-term follow-up is recommended, as malignant transformation appears uncertain, unpredictable and may be very delayed. |
| Every case of vulvo-perineal endometriosis should be reported describing in details the previous history, the clinical management and the treatment received. |
Table 8.
Data to report in case of vulvo-perineal endometriosis.
| Patient |
| Age |
| BMI |
| Ethnicity |
| Obstetrical History |
| Gravidity - Parity |
| Type of delivery |
| Episiotomy - Perineal laceration - Perineal tear (degree) - Perineal repair |
| Timing of any history |
| Medical or surgical history |
| Previous vulvo-perineal lesion, surgery or trauma |
| Previous abdominal surgery |
| Timing of any history |
| Symptoms |
| Beginning |
| Duration |
| Type (pain, localization, cyclical or not, …) |
| Latent period since trauma |
| Other symptoms |
| Clinical exam |
| Presence of a perineal mass or nodule |
| Size |
| Tenderness |
| Color of the Skin color |
| Detailed localization |
| Speculum examination |
| Rectal examination |
| Anal Sphincter Involvment |
| Work-up |
| Perineal ultrasound |
| Pelvic ultrasound |
| Pelvic MRI |
| Perianal ultrasound |
| Biopsy or FNAC |
| Other |
| Association with pelvic endometriosis |
| Treatment |
| Surgery |
| Excision or biopsy |
| Detailed procedure |
| Margins |
| Spillage |
| Type of closure |
| Type of repair in case of ASI |
| Hormonal |
| Pre-or post-surgery |
| Type |
| Duration |
| Comparison of symptoms and clinical exam before and after treatment |
| Histology |
| Follow-up |
| Recurrence |
| Type |
| Timing after treatment |
| Malignant transformation |
In conclusion, vulvo-perineal endometriosis is a rare entity with ~300 cases reported in the literature since 1923. With the available knowledge shown in this systematic review, we encourage all practitioners to think about perineal endometriosis in case of perineal cyclical pain with or without previous perineal damage. Diagnosis should be done with clinical exam, perineal ultrasound and pelvic MRI when available. In case of anal sphincter involvement, perianal ultrasound should be performed. Surgical excision of the lesion should be realized in order to remove the lesion and to confirm the diagnosis histologically. Hormonal treatment could be proposed to attempt to decrease the size of a large lesion before surgery or to avoid recurrence of the lesion. As evidence-based approach to the diagnosis, treatment and recurrence rate of affected patients remains a challenge given its low prevalence, the variations in management found in the articles included and the limited quality of available studies, we suggest that a prospective database on vulvo-perineal endometriosis should be generated to increase knowledge but also awareness among healthcare professionals and optimize patients' care.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
CM: search strategy, screening of studies, data extraction, manuscript writing, and final revision. ZC: screening of studies. J-LS, ML, and PJ: final revision. VT: screening of studies and language revision. CW: search strategy, manuscript writing, and final revision. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Vercellini P, Viganò P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. (2014) 10:261–75. 10.1038/nrendo.2013.255 [DOI] [PubMed] [Google Scholar]
- 2.Liang CC, Tsai CC, Chen TC, Soong YK. Management of perineal endometriosis. Int J Gynecol Obstet. (1996) 53:261–5. 10.1016/0020-7292(95)02592-8 [DOI] [PubMed] [Google Scholar]
- 3.Davis AC, Goldberg JM. Extrapelvic endometriosis. Semin Reprod Med. (2017) 35:98–101. 10.1055/s-0036-1597122 [DOI] [PubMed] [Google Scholar]
- 4.Andres MP, Arcoverde FV, Souza CC, Fernandes LF, Simoes Abrao MS, Kho RM. Extrapelvic endometriosis: a systematic review. J Minim Invasive Gynecol. (2020) 27:373–89. 10.1016/j.jmig.2019.10.004 [DOI] [PubMed] [Google Scholar]
- 5.Jubanyik KJ, Comite F. Extrapelvic endometriosis. Obstet Gynecol Clin North Am. (1997) 24:411–40. 10.1016/S0889-8545(05)70311-9 [DOI] [PubMed] [Google Scholar]
- 6.Bulun SE. Endometriosis. N Engl J Med. (2009) 360:268–79. 10.1056/NEJMra0804690 [DOI] [PubMed] [Google Scholar]
- 7.Bulun SE, Yilmaz BD, Sison C, Miyazaki K, Bernardi L, Liu S, et al. Endometriosis. Endocr Rev. (2019) 40:1048–79. 10.1210/er.2018-00242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giudice LC. Clinical practice. Endometriosis. N Engl J Med. (2010) 362:2389–98. 10.1056/NEJMcp1000274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cinardi N, Franco S, Centonze D, Giannone G. Perineal scar endometriosis ten years after Miles' procedure for rectal cancer: case report and review of the literature. Int J Surg Case Rep. (2011) 2:150–3. 10.1016/j.ijscr.2011.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen N, Zhu L, Lang J, Liu Z, Sun D, Leng J, et al. The clinical features and management of perineal endometriosis with anal sphincter involvement: a clinical analysis of 31 cases. Hum Reprod. (2012) 27:1624–7. 10.1093/humrep/des067 [DOI] [PubMed] [Google Scholar]
- 11.Dougherty LS, Hull T. Perineal endometriosis with anal sphincter involvement: report of a case. Dis Colon Rectum. (2000) 43:1157–60. 10.1007/BF02236565 [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Catherwood AE, Cohen ES. Endometriosis with decidual reaction in episiotomy scar. Am J Obstet Gynecol. (1951) 62:1364–6. 10.1016/0002-9378(51)90068-3 [DOI] [PubMed] [Google Scholar]
- 14.Hazard DB, Harkins GJ. A case of cutaneous endometriosis following vulvar injury. J Endometr. (2011) 3:171–3. [Google Scholar]
- 15.Cheng DL, Heller DS, Oh C. Endometriosis of the perineum; report of two new cases and a review of literature. Eur J Obstet Gynecol Reprod Biol. (1991) 42:81–4. 10.1016/0028-2243(91)90165-H [DOI] [PubMed] [Google Scholar]
- 16.Demir M, Yildiz A, Ocal I, Yetimalar MH, Kilic D, Yavasi O. Endometriosis in episiotomy scar: a case report. J Cases Obstet Gynecol. (2014) 1:8–10. [Google Scholar]
- 17.Wallace E, Marin S, Elkattah R. Vulvar endometriosis in the setting of a traumatic neuroma. J Endometr Pelvic Pain Disord. (2019) 11:49–51. 10.1177/2284026519828909 [DOI] [Google Scholar]
- 18.Kirk EW. Endometrioma in the posterior half of the labium majus. J Obstet Gynaecol Br Emp. (1950) 57:237–9. 10.1111/j.1471-0528.1950.tb05233.x [DOI] [PubMed] [Google Scholar]
- 19.Eyvazzadeh AD, Smith YR, Lieberman R, Quint EH. A rare case of vulvar endometriosis in an adolescent girl. Fertil Steril. (2009) 91:929.e9–11. 10.1016/j.fertnstert.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 20.Ruiz de Gauna B, Rodriguez D, Cabré S, Callejo J. A case of endometriosis in episiotomy scar with anal sphincter involvement. Int J Clin Med. (2011) 2:624–6. 10.4236/ijcm.2011.251041855430 [DOI] [Google Scholar]
- 21.Gocmen A, Inaloz HS, Sari I, Inaloz SS. Endometriosis in the Bartholin gland. Eur J Obstet Gynecol Reprod Biol. (2004) 114:110–1. 10.1016/j.ejogrb.2003.07.004 [DOI] [PubMed] [Google Scholar]
- 22.Gordon PH, Schottler JL, Balcos EG, Goldberg SM. Perianal endometrioma: report of five cases. Dis Colon Rectum. (1976) 19:260–5. 10.1007/BF02590916 [DOI] [PubMed] [Google Scholar]
- 23.Gorkem U, Efeturk T, Guney G, Gungor T. A case of vulvar endometrioma mimicking a bartholin cyst. J Cases Obstet Gynecol. (2016) 3:57–60. 10.1093/jscr/rjv169 [DOI] [Google Scholar]
- 24.Grimstad FW, Carey E. Periclitoral endometriosis: the dilemma of a chronic disease invading a rare location. J Minim Invasive Gynecol. (2015) 22:684–6. 10.1016/j.jmig.2015.02.002 [DOI] [PubMed] [Google Scholar]
- 25.Healy JJ, Hills FH. Bilateral endometriosis of the vulva. Am J Obstet Gynecol. (1956) 72:1361–3. 10.1016/0002-9378(56)90801-8 [DOI] [PubMed] [Google Scholar]
- 26.Heller DS, Lespinasse P, Mirani N. Endometriosis of the perineum: a rare diagnosis usually associated with episiotomy. J Low Genit Tract Dis. (2016) 20:e48–9. 10.1097/LGT.0000000000000203 [DOI] [PubMed] [Google Scholar]
- 27.Gözükara I, Karapinar OS, HakverdiI AU. Endometriosis of episiotomy scar. J Turkish Ger Gynecol Assoc. (2016) 17:S166. [Google Scholar]
- 28.Iqbal M, Thumbe V, Dhange R, Chan SY, Bhalerao S. Perianal endometriosis mimicking recurrent perianal abscess. Case Rep Gastroenterol. (2009) 3:414–7. 10.1159/000250787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheleden J. Endometriosis of the perineum. Report of two cases. South Med J. (1968) 61:1313–4. 10.1097/00007611-196812000-00011 [DOI] [PubMed] [Google Scholar]
- 30.Kouach J, El Hassani M, Moussaoui DR, Mohamed D. Vulvar endometriosis. J Obstet Gynaecol Canada. (2008) 30:1095. 10.1016/S1701-2163(16)33014-6 [DOI] [PubMed] [Google Scholar]
- 31.Kang SK, Lee MW, Choi JH, Sung KJ, Moon KC, Koh JK. Cutaneous endometriosis: a combination of medical and surgical treatment. J Dermatolog Treat. (2002) 13:189–92. 10.1080/09546630212345677 [DOI] [PubMed] [Google Scholar]
- 32.Jain D. Perineal scar endometriosis: a comparison of two cases. BMJ Case Rep. (2013) 2013:bcr2013010051. 10.1136/bcr-2013-010051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.AbdullGaffar B, Keloth TR, Raman LG, Mahmood S, Almulla A, AlMarzouqi M, et al. Unusual benign polypoid and papular neoplasms and tumor-like lesions of the vulva. Ann Diagn Pathol. (2014) 18:63–70. 10.1016/j.anndiagpath.2013.11.005 [DOI] [PubMed] [Google Scholar]
- 34.Luterek K, Barcz E, Bablok L, Wierzbicki Z. Giant recurrent perineal endometriosis in an episiotomy scar - a case report. Ginekol Pol. (2013) 84:726–9. 10.17772/gp/1631 [DOI] [PubMed] [Google Scholar]
- 35.Yogini KD, Balasubramaniam D, Karunanithi S, Parthasarathi R. Perianal endometriosis: a rare presentation of extrapelvic endometriosis. J SAFOG. (2019) 11:138–9. 10.5005/jp-journals-10006-1659 [DOI] [Google Scholar]
- 36.Natale KE, Royer MC, Rush WL, Luption GP. Cutaneous deciduosis: a report of two cases of an unusual pseudomalignancy. J Cutan Pathol. (2012) 39:777–80. 10.1111/j.1600-0560.2012.01907.x [DOI] [PubMed] [Google Scholar]
- 37.Kanellos I, Kelpis T, Zaraboukas T, Betsis D. Perineal endometriosis in episiotomy scar with anal sphincter involvement. Tech Coloproctol. (2001) 5:107–8. 10.1007/s101510170009 [DOI] [PubMed] [Google Scholar]
- 38.Kahraman K, Sonmezer M, Gungor M. Recurrent vulvar-perineal endometriosis. Artemis. (2003) 4:77−9. [Google Scholar]
- 39.Zhu L, Lang J, Wong F, Guo L. Perineal endometriosis without perineal trauma: a case report. Chin Med J (Engl). (2003) 116:639–40. [PubMed] [Google Scholar]
- 40.Ferreira LA. Endometriosis as a differential diagnosis on vulvar lump: a case report. Int J Gynecol Obstet. (2018) 143:742. [Google Scholar]
- 41.Prince LN, Abrams J. Endometriosis of the perineum; review of the literature and case report. Am J Obstet Gynecol. (1957) 73:890–3. 10.1016/0002-9378(57)90402-7 [DOI] [PubMed] [Google Scholar]
- 42.Laadioui M, Alaoui F, Jayi S, Bouguern H, Chaara H, Melhouf MA. Deep perineal endometriosis on episiotomy scar: about a rare case. Pan Afr Med J. (2013) 16:112. 10.11604/pamj.2013.16.112.3415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maheswari L. Case report of epidiotomy scar endometriosis. Univ J Surg Surg Spec. (2017) 3. [Google Scholar]
- 44.Aydin Y, Atis A, Polat N. Bilateral endometrioma of Bartholin glands accompanying ovarian endometrioma. J Obstet Gynaecol. (2011) 31:187–9. 10.3109/01443615.2010.541303 [DOI] [PubMed] [Google Scholar]
- 45.Corazza M, Schettini N, Pedriali M, Toni G, Borhi A. Vulvar endometriosis. A clinical, histological and dermoscopic riddle. J Eur Acad Dermatology Venereol. (2020) 34:e321–2. 10.1111/jdv.16257 [DOI] [PubMed] [Google Scholar]
- 46.Watanabe M, Kamiyama G, Yamazaki K, Hiratsuka K, Takata M, Tsunoda A, et al. Anal endosonography in the diagnosis and management of perianal endometriosis: report of a case. Surg Today. (2003) 33:630–2. 10.1007/s00595-003-2545-z [DOI] [PubMed] [Google Scholar]
- 47.Marcos MF, Marchitelli C, Sluga C, Secco G, Gorgoza S, Martinez MM. Vulvar endometriosis: A series of 4 cases. J Low Genit Tract Dis. (2017) 21:S5–6. 10.1097/LGT.0000000000000269 [DOI] [Google Scholar]
- 48.Matseoane S, Harris T, Moscowitz E. Isolated endometriosis in a Bartholin gland. N Y State J Med. (1987) 87:575–6. [PubMed] [Google Scholar]
- 49.Mazzeo C, Gammeri E, Foti A, Rossitto M, Cucinotta E. Vulvar endometriosis and Nuck canal. Ann Ital Chir. (2014) 85:1–4. [PubMed] [Google Scholar]
- 50.Mişina A, Zaharia S, Harea P, Fuior-Bulhac L, Petrovici V, şor E, et al. Endometriosis of the vulva and perineum. Arta Medica. (2020) 1:4–8. 5889799 [Google Scholar]
- 51.Nussbaum W, Motyloff L. Endometriosis of the vulva during pregnancy. Am J Obstet Gynecol. (1957) 73:215–6. 10.1016/S0002-9378(16)37286-6 [DOI] [PubMed] [Google Scholar]
- 52.Mahmud N, Kusuda N, Ichinose S, Gyotoku Y, Nakajima H, Ishimaru T, et al. Needle aspiration biopsy of vulvar endometriosis: a case report. Acta Cytol. (1992) 36:514–6. [PubMed] [Google Scholar]
- 53.Nasu K, Okamoto M, Nishida M, Narahara H. Endometriosis of the perineum. J Obstet Gynaecol Res. (2013) 39:1095–7. 10.1111/jog.12003 [DOI] [PubMed] [Google Scholar]
- 54.Odobasic A, Pasic A, Iljazovic-Latifagic E, Arnautalic L, Odobasic Ad, Idrizovic E, et al. Perineal endometriosis: a case report and review of the literature. Tech Coloproctol. (2010) 14(Suppl. 1):S25–7. 10.1007/s10151-010-0642-8 [DOI] [PubMed] [Google Scholar]
- 55.Baba AA, Dar AM, Parray AA, Khan MA, Laway MA, Chowdri NA. Perineal scar endometriosis. Indian J Colo-Rectal Surg. (2018) 1:30. 10.4103/IJCS.IJCS_2_18 [DOI] [Google Scholar]
- 56.Brug P, Gueye N-A, Bachmann G. Vulvar endometriosis presenting with dyspareunia: a case report. J Reprod Med. (2012) 57:175–7. [PubMed] [Google Scholar]
- 57.Singh P, Bhutia K, Gudi MA, Chuan HH. Endometriotic foci in bartholin's cyst. J Gynecol Surg. (2017) 33:111–3. 10.1089/gyn.2016.0061 [DOI] [Google Scholar]
- 58.Saloum NM, Qureshi S, Ibrahim SA, Alrashid A. A rare case report of endometriosis in an episiotomy scar without anal sphincter involvement. EC Gynaecol. (2018) 12:466–70. [Google Scholar]
- 59.Kistner RW, Younge PA. Endometriosis occurring in a vaginoperineal fistula. Am J Obstet Gynecol. (1952) 63:455–7. 10.1016/S0002-9378(15)32847-7 [DOI] [PubMed] [Google Scholar]
- 60.Ramsey WH. Endometrioma involving the perianal tissues: report of a case. Dis Colon Rectum. (1971) 14:366–7. 10.1007/BF02553424 [DOI] [PubMed] [Google Scholar]
- 61.Katz Z, Goldchmit R, Blickstein I. Post-traumatic vulvar endometriosis. Eur J Pediatr Surg. (1996) 6:241–2. 10.1055/s-2008-1066519 [DOI] [PubMed] [Google Scholar]
- 62.Robotti G, Canepari E, Torresi M. Premenstrual inguinal swelling and pain caused by endometriosis in the Bartholin gland: a case report. J Ultrasound. (2015) 18:71–2. 10.1007/s40477-014-0076-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ngu SF, Cheung VY. Vulvar endometriosis. J Obstet Gynaecol Canada. (2011) 33:891. 10.1016/S1701-2163(16)35007-1 [DOI] [PubMed] [Google Scholar]
- 64.Sayfan J, Benosh L, Segal M, Orda R. Endometriosis in episiotomy scar with anal sphincter involvement - Report of a case. Dis Colon Rectum. (1991) 34:713–6. 10.1007/BF02050357 [DOI] [PubMed] [Google Scholar]
- 65.Shanmuga Jayanthan S, Shashikala G, Arathi N, S. Perineal scar endometriosis. Indian J Radiol Imaging. (2019) 29:457–61. 10.4103/ijri.IJRI_366_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Barisic GI, Krivokapic Z V, Jovanovic DR. Perineal endometriosis in episiotomy scar with anal sphincter involvement: report of two cases and review of the literature. Int Urogynecol J. (2006) 17:646–9. 10.1007/s00192-005-0022-5 [DOI] [PubMed] [Google Scholar]
- 67.Shin HC, Kim TH, Kim SW, Kim DS, Park CH, Huh CK. Perineal endometriosis. Ann Dermatol. (1994) 6:196–9. 10.5021/ad.1994.6.2.196 [DOI] [Google Scholar]
- 68.Sully L. Endometrioma of the perineum associated with episiotomy scars. Scott Med J. (1977) 22:307–9. 10.1177/003693307702200422 [DOI] [PubMed] [Google Scholar]
- 69.Swerdlow DB. Endometrioma masquerading as an anorectal abscess: report of a case. Dis Colon Rectum. (1975) 18:620–2. 10.1007/BF02587146 [DOI] [PubMed] [Google Scholar]
- 70.Heijink T, Bogers H, Steensma A. Endometriosis of the Bartholin gland: a case report and review of the literature. J Med Case Rep. (2020) 14:85. 10.1186/s13256-020-02424-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tam T, Huang S. Perineal endometriosis in an episiotomy scar: case report and review of literature. J Endometr. (2012) 4:93–6. 10.5301/JE.2012.941017300680 [DOI] [Google Scholar]
- 72.Tornqvist B. Endometriosis in vaginal, vulvar and perineal scars. Acta Obstet Gynecol Scand. (1949) 28:485–9. 10.3109/00016344909155706 [DOI] [PubMed] [Google Scholar]
- 73.Torres-Cepeda D, Reyna-Villasmil E, Santos-Bolívar J. Endometriosis vulvar. Reporte de Caso (Vulvar Endometriosis. Case Report). Av en Biomed. (2014) 3:38–41. [Google Scholar]
- 74.Ümit C, Kokanali MK, Erkilinç S, Doganay M. Spontanous vulvar endometriosis: report of a case. Gynecol Obs Reprod Med. (2014) 20:119–21. [Google Scholar]
- 75.Dadhwal V, Sharma A, Khoiwal K, Nakra T. Episiotomy scar endometriosis. Med J Armed Forces India. (2018) 74:297–9. 10.1016/j.mjafi.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Trampuz V. Endometriosis of the perineum. A report of 5 new cases. Am J Obstet Gynecol. (1962) 84:1522–5. 10.1016/S0002-9378(16)35801-X [DOI] [PubMed] [Google Scholar]
- 77.Buda A, Ferrari L, Marra C, Passoni P, Perego P, Milani R. Vulvar endometriosis in surgical scar after excision of the Bartholin gland: report of a case. Arch Gynecol Obstet. (2008) 277:255–6. 10.1007/s00404-007-0458-6 [DOI] [PubMed] [Google Scholar]
- 78.Turan V, Ergenoglu M, Yeniel O, Emiroglu G, Ulukus M, Zekioglu O. Vulvar endometrioma: a case report. J Nepal Med Assoc. (2011) 51:87–9. 10.31729/jnma.250 [DOI] [PubMed] [Google Scholar]
- 79.Gunes M, Kayikcioglu F, Ozturkoglu E, Haberal A. Incisional endometriosis after cesarean section, episiotomy and other gynecologic procedures. J Obstet Gynaecol Res. (2005) 31:471–5. 10.1111/j.1447-0756.2005.00322.x [DOI] [PubMed] [Google Scholar]
- 80.Hakimi I. Endometriosis in the Bartholin gland: a case report. J Gynecol Obstet. (2014) 2:75. 10.11648/j.jgo.20140205.1232605643 [DOI] [Google Scholar]
- 81.Hamdi A, Gharsa A, Jaziri D, Sfar E, Chelli D. Perineal endometriosis without perineal trauma: a case report. Chin Med J. (2015) 6:1–3. 10.4172/2155-9554.1000029312875740 [DOI] [Google Scholar]
- 82.Canlorbe G, Laas E, Cortez A, Daraï E. Spontaneous hymeneal endometriosis: a rare cause of dyspareunia. BMJ Case Rep. (2014) 2014:bcr2013202299. 10.1136/bcr-2013-202299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jeyaseelan S, Kwatra N. A rare case of episiotomy scar endometriosis. J Obstet Gynecol India. (2016) 66(Suppl. 2):654–5. 10.1007/s13224-015-0800-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Leite GKC, De Carvalho LFP, Korkes H, Guazzelli TF, Kenj G, Viana ADT. Scar endometrioma following obstetric surgical incisions: retrospective study on 33 cases and review of the literature. São Paulo Med J. (2009) 127:270–7. 10.1590/S1516-31802009000500005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rajesh Kamble V, Gawande MS. Preoperative magnetic resonance evaluation of perineal endometriosis in episiotomy scar with anal sphincter involvement. Panacea J Med Sci. (2016) 6:170. [Google Scholar]
- 86.Toyonaga T, Matsushima M, Tanaka Y, Nozawa M, Sogawa N, Kanyama H, et al. Endoanal ultrasonography in the diagnosis and operative management of perianal endometriosis: report of two cases. Tech Coloproctol. (2006) 10:357–60. 10.1007/s10151-006-0309-7 [DOI] [PubMed] [Google Scholar]
- 87.Xu S, Wang W, Sun LP. Comparison of clear cell carcinoma and benign endometriosis in episiotomy scar - two cases report and literature review. BMC Womens Health. (2020) 20:11. 10.1186/s12905-020-0880-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cai S-Q, Zheng M, Man X-Y. Perineal endometriosis: a case report. Int J Clin Exp Med. (2014) 7:2939–40. [PMC free article] [PubMed] [Google Scholar]
- 89.Sharma N, Khan DA, Jethani R, Baruah S, Dey B. Perineal endometriosis in an episiotomy scar: a case report and review of literature. Gynecol Obs Case Rep. (2018) 4:66. 10.21767/2471-8165.100006617300680 [DOI] [Google Scholar]
- 90.Sharp C, Kulkarni M, Rosamilia A, Tsaltas J. Vulval endometriosis following vaginal hysterectomy. J Minim Invasive Gynecol. (2020) 27:1453–4. 10.1016/j.jmig.2020.02.006 [DOI] [PubMed] [Google Scholar]
- 91.Paull T, Tedeschi LG. Perineal endometriosis at the site of episiotomy scar. Obstet Gynecol. (1972) 40:28–34. 10.1097/00006250-197207000-00006 [DOI] [PubMed] [Google Scholar]
- 92.Nominato NS, Victor Spyer Prates LF, Lauar I, Morais J, Maia L, Geber S. Endometriose de cicatriz cirúrgica: estudo retrospectivo de 72 casos Scar endometriosis: a retrospective study of 72 patients. Rev Bras Ginecol Obstet. (2007) 29:403–7. 10.1590/S0100-72032007000800007 [DOI] [Google Scholar]
- 93.Zhu L, Lang J, Wang H, Liu Z, Sun D, Leng J, et al. Presentation and management of perineal endometriosis. Int J Gynecol Obstet. (2009) 5:230–2. 10.1016/j.ijgo.2009.01.022 [DOI] [PubMed] [Google Scholar]
- 94.Li J, Shi Y, Zhou C, Lin J. Diagnosis and treatment of perineal endometriosis: review of 17 cases. Arch Gynecol Obstet. (2015) 292:1295–9. 10.1007/s00404-015-3756-4 [DOI] [PubMed] [Google Scholar]
- 95.Matalliotakis M, Matalliotaki C, Zervou MI, Krithinakis K, Goulielmos GN, Kalogiannidis I. Abdominal and perineal scar endometriosis: retrospective study on 40 cases. Eur J Obstet Gynecol Reprod Biol. (2020) 252:225–7. 10.1016/j.ejogrb.2020.06.054 [DOI] [PubMed] [Google Scholar]
- 96.Liu Y, Pi R, Luo H, Wang W, Zhao X, Qi X. Characteristics and long-term outcomes of perineal endometriosis: a retrospective study. Medicine. (2020) 99:e20638. 10.1097/MD.0000000000020638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Park SB, Kim JK, Cho KS. Sonography of endometriosis in infrequent sites. J Clin Ultrasound. (2008) 36:91–7. 10.1002/jcu.20431 [DOI] [PubMed] [Google Scholar]
- 98.Guerriero S, Conway F, Pascual MA, Graupera B, Ajossa S, Neri M, et al. Ultrasonography and atypical sites of endometriosis. Diagnostics. (2020) 10:345. 10.3390/diagnostics10060345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Donnez J, Nisolle M, Casanas-Roux F, Brion P, Da Costa Ferreira N. Stereometric evaluation of peritoneal endometriosis and endometriotic nodules of the rectovaginal septum. Hum Reprod. (1996) 11:224–8. 10.1093/oxfordjournals.humrep.a019024 [DOI] [PubMed] [Google Scholar]
- 100.Nisolle M, Donnez J. Peritoneal endometriosis, ovarian endometriosis, and adenomyotic nodules of the rectovaginal septum are three different entities. Fertil Steril. (1997) 68:585–96. 10.1016/S0015-0282(97)00191-X [DOI] [PubMed] [Google Scholar]
- 101.Steck WD, Helwig EB. Cutaneous endometriosis. JAMA. (1965) 191:167–70. 10.1001/jama.1965.03080030011002 [DOI] [PubMed] [Google Scholar]
- 102.Koninckx PR, Ussia A, Adamyan L, Wattiez A, Gomel V, Martin DC. Pathogenesis of endometriosis: the genetic/epigenetic theory. Fertil Steril. (2019) 111:327–40. 10.1016/j.fertnstert.2018.10.013 [DOI] [PubMed] [Google Scholar]
- 103.Haley JC, Mirowski GW, Hood AF. Benign vulvar tumors. Semin Cutan Med Surg. (1998) 17:196–204. 10.1016/S1085-5629(98)80014-X [DOI] [PubMed] [Google Scholar]
- 104.Tatli F, Gozeneli O, Uyanikoglu H, Uzunkoy A, Yalcin HC, Ozgonul A, et al. The clinical characteristics and surgical approach of scar endometriosis: a case series of 14 women. Bosn J Basic Med Sci. (2018) 18:275–8. 10.17305/bjbms.2018.2659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Horton JD, Dezee KJ, Ahnfeldt EP, Wagner M. Abdominal wall endometriosis: a surgeon's perspective and review of 445 cases. Am J Surg. (2008) 196:207–12. 10.1016/j.amjsurg.2007.07.035 [DOI] [PubMed] [Google Scholar]
- 106.Han L, Zheng A, Wang H. Clear cell carcinoma arising in previous episiotomy scar: a case report and review of the literature. J Ovarian Res. (2016) 9:1. 10.1186/s13048-016-0211-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Heaps JM, Nieberg RK, Berek JS. Malignant neoplasms arising in endometriosis. Obstet Gynecol. (1990) 75:1023–8. [PubMed] [Google Scholar]
- 108.Kwon YS, Nam JH, Choi G. Clear cell adenocarcinoma arising in endometriosis of a previous episiotomy site. Obstet Gynecol. (2008) 112 (2 Pt 2):475–7. 10.1097/AOG.0b013e318179475b [DOI] [PubMed] [Google Scholar]
- 109.Chene G, Darcha C, Dechelotte P, Mage G, Canis M. Malignant degeneration of perineal endometriosis in episiotomy scar, case report and review of the literature. Int J Gynecol Cancer. (2007) 17:709–14. 10.1111/j.1525-1438.2007.00822.x [DOI] [PubMed] [Google Scholar]
- 110.Hitti IF, Glasberg SS, Lubicz S. Clear cell carcinoma arising in extraovarian endometriosis: report of three cases and review of the literature. Gynecol Oncol. (1990) 39:314–20. 10.1016/0090-8258(90)90259-N [DOI] [PubMed] [Google Scholar]
- 111.Kholová I, Ryska A, Dedic K. Composite tumor consisting of dermatofibrosarcoma protuberans and giant cell fibroblastoma associated with intratumoral endometriosis. Pathol Res Pract. (2001) 197:263–7. 10.1078/0344-0338-00045 [DOI] [PubMed] [Google Scholar]
- 112.Kojima N, Yoshida H, Uehara T, Ushigusa T, Asami Y, Shiraishi K, et al. Primary clear cell adenocarcinoma of the vulva: a case study with mutation analysis and literature review. Int J Surg Pathol. (2019) 27:792–7. 10.1177/1066896919848823 [DOI] [PubMed] [Google Scholar]
- 113.Mesko JD, Gates H, McDonald TW, Youmans R, Lewis J. Clear cell ('Mesonephroid') adenocarcinoma of the vulva arising in endometriosis: a case report. Gynecol Oncol. (1988) 29:385–91. 10.1016/0090-8258(88)90241-7 [DOI] [PubMed] [Google Scholar]
- 114.Bolis GB, Maccio T. Clear cell adenocarcinoma of the vulva arising in endometriosis. A case report. Eur J Gynaecol Oncol. (2000) 21:416–7. [PubMed] [Google Scholar]
- 115.Todd RW, Kehoe S, Gearty J. A case of clear cell carcinoma arising in extragonadal endometriosis. Int J Gynecol Cancer. (2000) 10:170–2. 10.1046/j.1525-1438.2000.00024.x [DOI] [PubMed] [Google Scholar]
- 116.Buppasiri P, Kleebkaow P, Tharanon C, Aue-Aungkul A, Kietpeerakool C. Clear cell carcinoma arising in vulvar endometriosis. Case Rep Pathology. (2018) 2018:4263104. 10.1155/2018/4263104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ssi-Yan-Kai G, Thubert T, Rivain AL, Prevot S, Deffieux X, De Laveaucoupet J. Female perineal diseases: spectrum of imaging findings. Abdom Imaging. (2015) 40:2690–709. 10.1007/s00261-015-0427-7 [DOI] [PubMed] [Google Scholar]
- 118.Hosseinzadeh K, Heller MT, Houshmand G. Imaging of the female perineum in adults. Genitourinary Imaging. (2012) 32:E129–68. 10.1148/rg.324115134 [DOI] [PubMed] [Google Scholar]
- 119.Bazot M, Darai E, Hourani R, Thomassin I, Cortez A, Uzan S, et al. Deep pelvic endometriosis: MR imaging for diagnosis and prediction of extension of disease. Radiology. (2004) 232:379–89. 10.1148/radiol.2322030762 [DOI] [PubMed] [Google Scholar]
- 120.Kinkel K, Frei KA, Balleyguier C, Chapron C. Diagnosis of endometriosis with imaging: a review. Eur Radiol. (2006) 16:285–98. 10.1007/s00330-005-2882-y [DOI] [PubMed] [Google Scholar]
- 121.Cazacu E. Histological and immunohistochemical study of extragenital endometriosis. Virchows Arch. (2014) 465:S356. [Google Scholar]
- 122.Kazakov D V, Ondic O, Zamecnik M, Shelekhova K V, Mukensnabl P, Hes O, et al. Morphological variations of scar-related and spontaneous endometriosis of the skin and superficial soft tissue: a study of 71 cases with emphasis on atypical features and types of müllerian differentiations. J Am Acad Dermatol. (2007) 57:134–46. 10.1016/j.jaad.2006.11.036 [DOI] [PubMed] [Google Scholar]
- 123.Zhu L, Wong F, Lang JH. Perineal endometriosis after vaginal delivery - Clinical experience with 10 patients. Aust New Zeal J Obstet Gynaecol. (2002) 42:565–7. 10.1111/j.0004-8666.2002.548_12.x [DOI] [PubMed] [Google Scholar]
- 124.Uzunçakmak C, Güldaş A, Özçam H, Dinç K. Scar endometriosis: a case report of this uncommon entity and review of the literature. Case Rep Obstet Gynecol. (2013) 2013:1–4. 10.1155/2013/386783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Galdino JDL, Costa RSC, De Oliveira JG. Reconstruction of abdominal wall and vulvar defects after endometriosis resection. Rev Bras Cir Plást. (2019) 34:355–61. 10.5935/2177-1235.2019RBCP0208 [DOI] [Google Scholar]
- 126.Sauvan M, Chabbert-Buffet N, Canis M, Collinet P, Fritel X, Geoffron S, et al. Medical treatment for the management of painful endometriosis without infertility: CNGOF-HAS endometriosis guidelines. Gynecol Obstet Fertil Senol. (2018) 46:267–72. 10.1016/j.gofs.2018.02.028 [DOI] [PubMed] [Google Scholar]
- 127.Geoffron S, Legendre G, Daraï E, Chabbert-Buffet N. Traitement médical de l'endométriose : prise en charge de la douleur et de l'évolution des lésions par traitement hormonal et perspectives thérapeutiques. Press Medicale. (2017) 46 (12P1):1199–211. 10.1016/j.lpm.2017.10.005 [DOI] [PubMed] [Google Scholar]
- 128.Bedaiwy MA, Allaire C, Alfaraj S. Long-term medical management of endometriosis with dienogest and with a gonadotropin-releasing hormone agonist and add-back hormone therapy. Fertil Steril. (2017) 107:537–48. 10.1016/j.fertnstert.2016.12.024 [DOI] [PubMed] [Google Scholar]
- 129.Ferrero S, Evangelisti G, Barra F. Current and emerging treatment options for endometriosis. Exp Opin Pharmacother. (2018) 19:1109–25. 10.1080/14656566.2018.1494154 [DOI] [PubMed] [Google Scholar]
- 130.Kulkarni N, Patil A, Patel R. Study of preoperative GnRh agonist in cutaneous scar endometriosis. Int J Reprod Contracept Obstet Gynecol. (2016) 5:3191–4. 10.18203/2320-1770.ijrcog20163010 [DOI] [Google Scholar]
- 131.Mistrangelo M, Gilbo N, Cassoni P, Micalef S, Faletti R, Miglietta C, et al. Surgical scar endometriosis. Surg Today. (2014) 44:767–72. 10.1007/s00595-012-0459-3 [DOI] [PubMed] [Google Scholar]
- 132.Purvis RS, Tyring SK. Cutaneous and subcutaneous endometriosis. J Dermatol Surg Oncol. (1994) 20:693–5. 10.1111/j.1524-4725.1994.tb00456.x [DOI] [PubMed] [Google Scholar]
- 133.Raffi L, Suresh R, McCalmont TH, Twigg AR. Cutaneous endometriosis. Int J Womens Dermatol. (2019) 5:384–6. 10.1016/j.ijwd.2019.06.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Rivlin ME, Das SK, Patel RB, Rodney Meeks G. Leuprolide acetate in the management of cesarean scar endometriosis. Obstet Gynecol. (1995) 85:838–9. 10.1016/0029-7844(94)00270-N [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.