Abstract
Background:
Research on adolescent heroin use has focused on national surveillance, access, prevalence of use, and overdose deaths, however, to our knowledge, no study has examined local-level differences in the prevalence of adolescent heroin use in the context of nonmedical prescription opioid (NMPO) use. This study characterizes heroin and NMPO use among US high school students in select urban areas by sex and race/ethnicity.
Methods:
Data are from 21 urban school districts that participate in CDC’s Local Youth Risk Behavior Surveillance System. We describe 2017 prevalence estimates (and 95% confidence intervals) of lifetime heroin and NMPO use among youth stratified by sex and race/ethnicity (i.e., White, Black, Hispanic/Latino).
Results:
The highest estimates of heroin use were in Baltimore, MD (7.6%), Shelby County, TN (6.3%), and Duval County, FL (6.1%), whereas NMPO use was highest in Duval County, FL (18.1%), Cleveland, OH (18.0%), and Shelby County, TN (16.8%). Heroin use was higher among boys than girls, especially among Hispanic/Latino boys in Duval County (12.3%) and Black boys in Baltimore (10.9%). NMPO use was highest among Hispanic/Latino girls (21.3%) and White girls (19.9%) in Duval County.
Discussion:
While some cities and subpopulations with high levels of adolescent heroin use also had elevated levels of NMPO use, others did not, illustrating the complexities of this opioid epidemic.
Keywords: heroin use, opioids, adolescence, surveillance, race/ethnicity, gender
1. Introduction
The recent opioid epidemic in the United States is characterized by significant increases in heroin use over the past decades, with over 800,000 individuals reporting past-year use in 2018 (SAMSHA, 2018; Martins et al., 2017). One in three individuals in treatment for opioid use disorder report use before 18 years of age (Hadland, 2019) and 7,000 adolescents aged 12–17 years initiated heroin use in 2018 (SAMSHA, 2019), highlighting the importance of examining heroin use among adolescents.
In 2017, the prevalence of lifetime heroin use among US high school students was 1.7% (Kann et al., 2018); corresponding prevalence estimates for those aged 18–25 were 1.8% (NIDA, 2018). A recent study showed that the fatality rate for heroin overdose among 15–19-year-olds increased from 0.21 to 1.06 per 100,000 persons between 1999 and 2016, which reflects more than a 400% increase (Gaither et al., 2018). As adolescent heroin use and subsequent consequences increase, the relationship between heroin and nonmedical prescription opioid (NMPO) use in adolescents has been documented. Using repeated cross-sectional data from the National Surveys on Drug Use and Health, Cerda and colleagues (2015) found a strong association (hazard ratio of 13) between adolescent NMPO use and the subsequent initiation of heroin use. Similarly, Kelley-Quon and colleagues (2019) found a strong correlation between adolescent NMPO use and heroin use with longitudinal data from a large sample of high-school attending adolescents. Current research indicates that NMPO use is preceded by medically-directed prescription opioid use in adolescents (McCabe et al., 2017).
Among school-attending youth, adolescent heroin use and NMPO use may be particularly high in certain cities and among specific subpopulations, as has been the case historically for adults (Garfield et al., 2001; Kozel et al., 2002). Despite this possibility, existing research has focused on national surveillance, with limited consideration of local variation in the prevalence of use. In addition, differences in the prevalence of heroin and NMPO use by race/ethnicity, sex, and geographic location are understudied. To address these gaps in the literature, we summarize the 2017 prevalence of lifetime heroin and NMPO use among high school students in a select group of large, urban areas in the US, by sex and race/ethnicity.
2. Methods and Materials
2.1. Youth Risk Behavior Surveillance System
The Centers for Disease Control and Prevention (CDC) implements the Youth Risk Behavior Surveillance System to monitor health behaviors including substance use among adolescents; it includes national, state, and local school-based surveys of 9th-12th graders on a biennial basis. CDC provides technical assistance and a core set of questions so as to facilitate comparability over time and across settings (Brener et al., 2013). Large, urban school districts participate in the Local Youth Risk Behavior Survey (YRBS) program on a voluntary basis. Districts employ a two-stage, cluster sample methodology that is designed to yield samples representative of high school students in the specific jurisdiction. Response rates ranged from 61% (District of Columbia) to 89% (Los Angeles, CA) (Kann et al., 2018). Only districts with response rates greater than 60% are weighted and formally included in the Local YRBS system. Detailed information about the response rates of localities has been previously described by Kann and colleagues (2018). We summarize data from 21 districts. Because one district opted not to include the item on heroin (Cleveland, OH) and another opted not to include NMPO (New York City), we present data for 20 districts for each drug.
2.2. Measures
Lifetime heroin use was assessed using a question that captured whether youth had “ever used heroin (also called “smack,” “junk,” or “China White,” one or more times during their life).” Lifetime NMPO use was assessed using a question that captured whether youth had “ever took prescription pain medicine without a doctor’s prescription or differently than how a doctor told them to use it (counting drugs such as codeine, Vicodin, Oxycontin, Hydrocodone, and Percocet, one or more times during their life).”
2.3. Analysis
First, we describe prevalence estimates (and 95% confidence intervals) for lifetime heroin use and NMPO use among boys, girls, and both sexes across the urban school districts These data are available from CDC (Kann et al., 2018; CDC, 2018) and are presented in the supplemental table. Then, for locales with sample sizes sufficient to generate reliable estimates, we present estimates of the prevalence of both outcomes by race/ethnicity for boys and girls for all sites. Race/ethnicity groups were limited to Black, White, and Hispanic/Latino because those were the only groups large enough to generate stable estimates.
3. Results
3.1. Prevalence of Heroin and NMPO Use
For girls and boys combined, districts in the top quartile had prevalence estimates of lifetime heroin use ranging from 4.9%−7.6%; estimates from the first, second, and third quartiles ranged from 1.3%−2.9%, 3.0%−3.7%, and 3.9%−4.4%, respectively. The top five highest prevalence estimates were in Baltimore City, MD (7.6%, 5.1%–11.1%), Shelby County, TN (6.3%, 4.6%–8.6%), Duval County, FL (6.1%, 4.9%–7.7%), District of Columbia (5.3%, 4.8%–5.9%), and Chicago, IL (4.9%, 3.0%–7.9%). The highest prevalence estimates of lifetime NMPO use were in Duval County (18.1%, 16.5%–19.7%), Cleveland, OH (18.0%, 15.6%–20.6%), Shelby County, TN (16.8%, 14.7%–19.2%), District of Columbia (15.4%, 14.5%–16.3%), Chicago (15.0%, 12.2%–18.4%).
3.2. Gender Differences in Prevalence of Heroin and NMPO Use
Across the different locales, the prevalence of lifetime heroin use was higher for boys than girls. The median prevalence estimate for lifetime heroin use was 1.7% for girls (range: 0.3%−3.7%) and 5.7% for boys (range: 2.2%−11.4%). The district with the highest prevalence of heroin use for girls was Duval County (3.7%, 2.7%−5.0%), and for boys was Baltimore (11.4%, 7.2%−17.6%). Reported heroin use was higher among boys than girls in each of the 20 locales. The male-female difference was 1.5 percentage points or greater for all locales except Fort Worth, TX (male-female difference: 0.9). Significant gender differences were evident in all localities with available data (p<0.05). The gender gap was much narrower for NMPO use than for heroin. The median prevalence for NMPO use was 11.6% for girls (range: 8.4%−18.7%-) and 13.1% for boys (range: 9%−18.8%). The district with the highest prevalence of NMPO use for girls was Duval County (18.7%, 16.7%–20.7%), and for boys was Cleveland, OH (18.8%, 15.5%–22.7%). Gender differences in adolescent NMPO use could be tested for only Broward County, FL (11.0% girls, 11.8% boys), Baltimore, MD, (10.7% girls, 15.3% boys) and Boston, MA (8.4% girls, 9.0% boys). No significant gender differences were evident in these localities (p>0.05).
3.3. Race and Gender Differences in the Prevalence of Heroin and NMPO Use
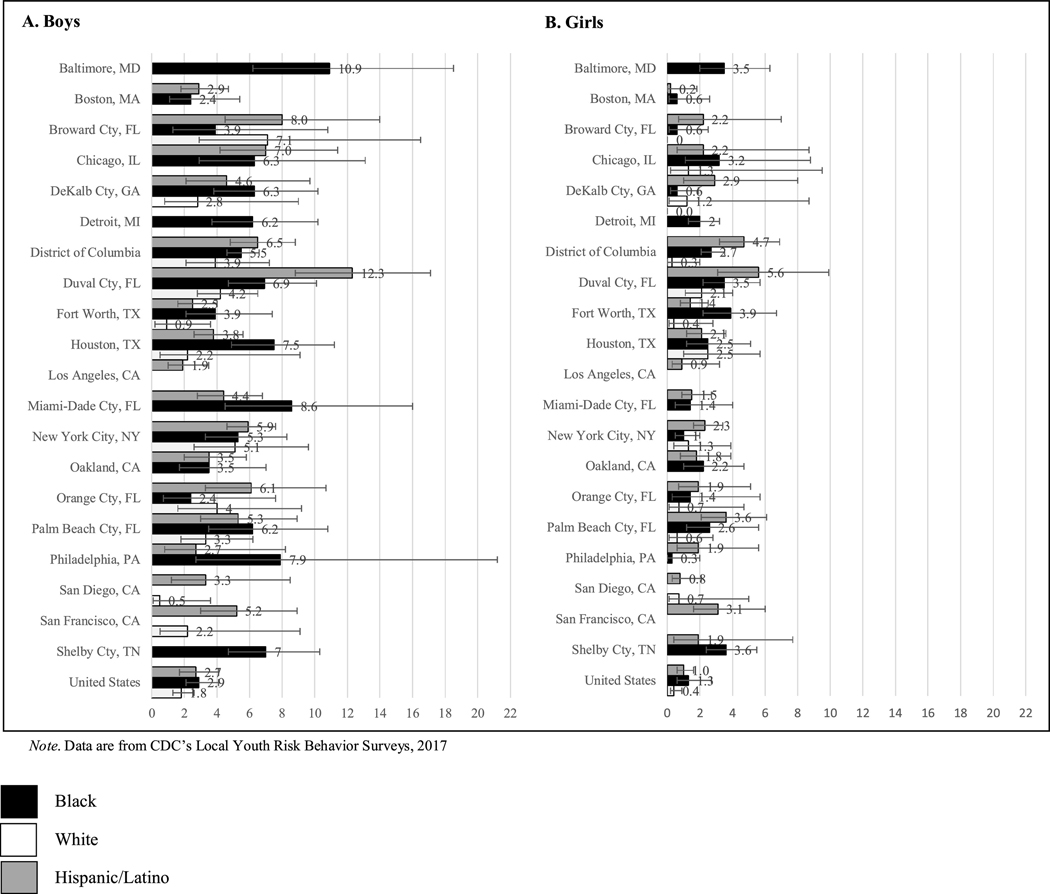
Figure 1 shows the prevalence of heroin use among Black, White, and Hispanic/Latino boys and girls. Among boys, prevalence estimates were highest among Hispanic/Latino youth in Duval County, FL (12.3%, 8.8%−17.1%) and among Black youth in Baltimore (10.9%, 6.2%18.5%). Among girls, prevalence estimates were highest among Hispanic/Latino youth in Duval County, FL (5.6%, 3.1%−9.9%) and the District of Columbia (4.7%, 3.2%−6.9%).
Figure 1.
Prevalence estimates (95% confidence interval) of lifetime heroin use among high school students by sex and by race/ethnicity across 20 urban areas, 2017
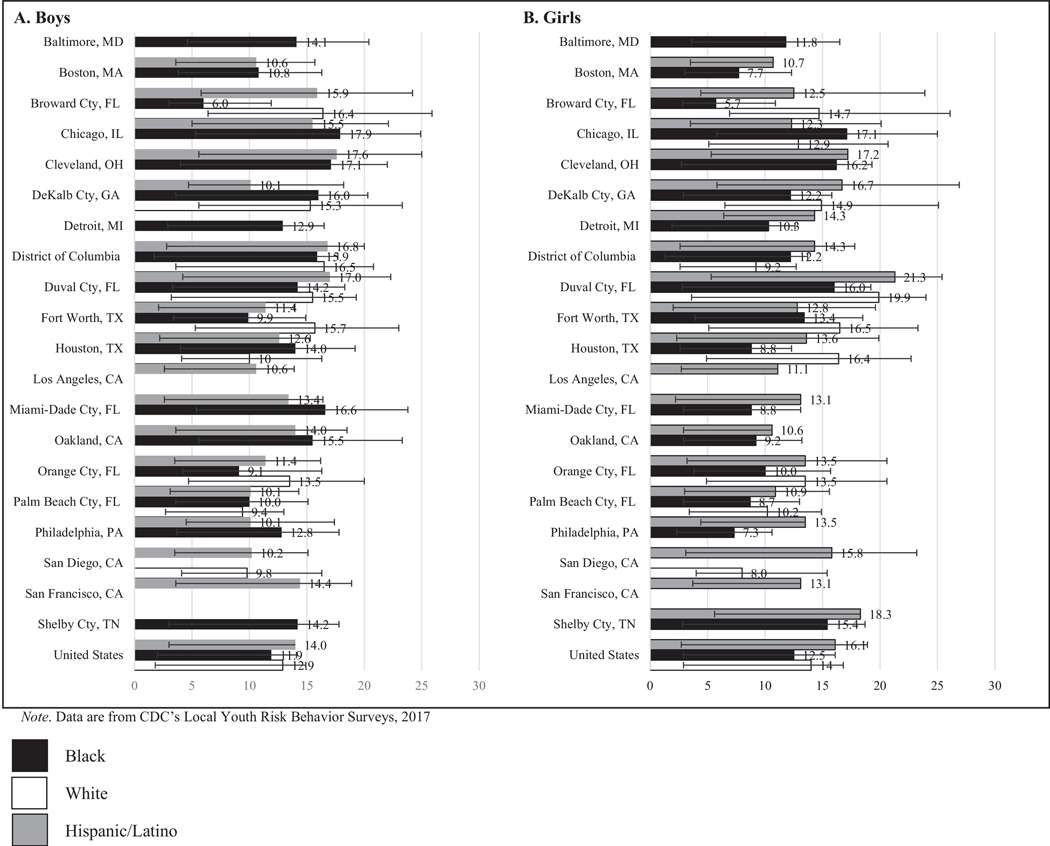
Figure 2 shows the prevalence of NMPO use among Black, White, and Hispanic/Latino boys and girls. Among boys, prevalence estimates were highest among Black youth in Chicago, IL (17.9%, 12.6%–24.9%), and among Hispanic/Latino youth in Cleveland, OH (17.6%, 12.0%–25.0%). Among girls, prevalence estimates were highest among Hispanic/Latino and White youth in Duval County, FL (Hispanic/Latino: 21.3%, 16.0%–27.9%, White: 19.9%, 16.3%–24.0%) and Hispanic/Latino youth in Shelby, TN (18.3%, 12.7%–25.8%).
Figure 2.
Prevalence estimates (95% confidence interval) of lifetime non-medical prescription opioid use among high school students by sex and by race/ethnicity across 20 urban areas, 2017
4. Discussion
The national prevalence of lifetime heroin use among US high school students, 1.7 (1.3%−2.2%), masks significant variation at the local level. The prevalence of lifetime heroin use among 9th−12th graders in a select group of large, urban school districts varied substantially across sites, and use was much higher among boys in all districts. By contrast, the national prevalence of NMPO use was 14% (12.7%−15.4%), with most localities having similar or lower prevalence. Of the five urban areas with the highest prevalence of adolescent heroin use, only Duval County, FL had a prevalence of NMPO use that was substantially higher than the national prevalence.
In addition, although boys were generally 2–3 times more likely to use heroin than girls in many localities, there were no sex differences in adolescent NMPO use. Although national data show low rates of adolescent heroin use, the local data presented here suggest that heroin use is higher than 10% among Black and Hispanic/Latino boys in some areas. However, the highest prevalence of NMPO use was found among Hispanic/Latino girls and White girls. These findings suggest a more complex relationship between heroin use and NMPO use in different geographical areas and social contexts, thus warranting further exploration into socio-contextual determinants of adolescent heroin use initiation.
Trends in heroin use over time provide additional context to our findings. The prevalence of lifetime heroin use in 2007 was low in many localities including Baltimore, MD, (1.8%, 1.1%−2.8%) and Detroit, MI (1.6%, 1.0%−2.6%), but rose significantly in these areas by 2017 (7.6%, 5.1%−11.1%; 4.2%, 2.8%−6.1%), respectively (CDC, 2018). By contrast, the prevalence of adolescent heroin use in Washington D.C. remained stable and high 5.2% (4.0%−6.8%) in 2007, and 5.3% (4.8%−5.9%) in 2017 (CDC, 2018). In addition, research on heroin use trends from 1999–2017 using data from 9 cities, found that trends of heroin use and injection drug use, a related drug use behavior, not only mirrored each other but also followed the same trajectory over time (Brighthaupt et al., 2019). Other consequences related to heroin use, such as opioid use disorder diagnoses, HCV, and non-fatal overdoses, have also significantly increased among adolescents (Hadland, 2019). Data on trends in NMPO are unavailable because NMPO was first including on the YRBS in 2017.
Although these data cannot be generalized beyond school-attending youth, it is possible that districts with high levels of heroin use among high school students have commensurately high levels of use among youth who are not in school. Overdose data in cities we found to have high levels of adolescent heroin use lend credence to this possibility. Heroin overdose deaths sky-rocketed from 260 in 2015 to 454 in 2016 in Baltimore (Maryland Department of Health and Mental Hygiene, 2017), other areas, such as Duval County, FL, have elevated age-adjusted drug poisoning death rates (Rossen et al., 2017). In addition, we are unable to delineate youth who misused prescription opioids for medical purposes (additional pain relief) from those who misused them for recreational purposes.
5. Conclusions
Local surveillance of adolescent heroin and NMPO use is needed and can be used to guide community-based efforts to address opioid use and related problems. Additionally, research to identify social and contextual determinants of adolescent opioid use can enhance our understanding of the mechanisms leading to differences by city, race/ethnicity, and sex, and can inform the development of structural interventions that address the root causes of opioid use among adolescents. Public health planning and interventions should be tailored to adolescents according to local needs, particularly for boys and marginalized race/ethnicity groups. Finally, evidence-based interventions to address the opioid epidemic (such as naloxone distribution and overdose response training, access to resources for recovery, including medication-assisted treatment, and screening for substance use disorders) should be expanded to include adolescents in highly-affected areas (Hadland, 2019).
Supplementary Material
Highlights.
We evaluate adolescent heroin and nonmedical prescription opioid (NMPO) use.
Hispanic and Black boys had the highest prevalence of heroin use.
Hispanic and White girls had the highest prevalence of NMPO use.
Boys were more likely to use heroin, no sex differences in NMPO use were found.
Local-level research on adolescent opioid use and motivations for use is needed.
Acknowledgements:
We thank the youth who participated in the YRBS study and the staff at all YRBS sites.
Role of Funders: Content is solely the responsibility of the authors and does not necessarily reflect the official views of the NIH or any other organizations. The funders had no role in the design and conduct of the study.
Footnotes
Potential Conflict of Interest Disclosures: Dr. AA Jones’ spouse, works as an independent contractor for a 501c3 non-profit educational organization that educates citizens on the science of marijuana with an aim to decrease its use and related consequences. Dr. Jones’ spouse did not play a role in this study. No other disclosures are reported.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Brener ND, Kann L, Shanklin S, Kinchen S, Eaton DK, Hawkins J, Flint KH, 2013. Methodology of the Youth Risk Behavior Surveillance System—2013. MMWR Surv. Summ, 62, 1–20. https://www.cdc.gov/mmwr/pdf/rr/rr6201.pdf Accessed on April 1, 2019. [PubMed] [Google Scholar]
- Brighthaupt SC, Schneider KE, Johnson JK, Jones AA, Johnson RM, 2019. Trends in adolescent heroin and injection drug use in nine urban centers in the U.S., 1999–2017. J Adolesc. Health, 65, 210–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC), 2018. 1991–2017 High School Youth Risk Behavior Survey Data. http://nccd.cdc.gov/youthonline/. Accessed September 1, 2018.
- Cerdá M, Santaella J, Marshall BD, Kim JH, Martins SS, 2015. Nonmedical prescription opioid use in childhood and early adolescence predicts transitions to heroin use in young adulthood: a national study. J. Pediatr, 167, 605–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaither JR, Shabanova V, Leventhal JM, 2018. US national trends in pediatric deaths from prescription and illicit opioids, 1999–2016. JAMA Network Open, 1, e186558–e186558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfield J, Drucker E, 2001. Fatal overdose trends in major US cities: 1990–1997. Addict. Res. Theory, 9, 425–436. [Google Scholar]
- Hadland SE, 2019. How clinicians caring for youth can address the opioid-related overdose crisis. J. Adolesc. Health, 65, 177–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, Lowry R, Chyen D, Whittle L, Thornton J, Bradford D, Yamakawa Y, Leon M, Brener N, Ethier KA, Lim C, 2018. Youth risk behavior surveillance—United States, 2017. MMWR Surv. Summ, 67, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley-Quon LI, Cho J, Strong DR, Miech RA, Barrington-Trimis JL, Kechter A, Leventhal AM, 2019. Association of nonmedical prescription opioid use with subsequent heroin use initiation in adolescents. JAMA Pediatr, e191750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozel NJ, Robertson EB, Falkowski CL, 2002. The community epidemiology work group approach. Subst. Use Misuse, 37, 783–803. [DOI] [PubMed] [Google Scholar]
- Martins SS, Sarvet A, Santaella-Tenorio J, Saha T, Grant BF, Hasin DS, 2017. Changes in US lifetime heroin use and heroin use disorder: prevalence from the 2001–2002 to 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry, 74, 445–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maryland Department of Health and Mental Hygiene, 2017. Drug- and alcohol-related intoxication deaths in Maryland, 2016. https://bha.health.maryland.gov/OVERDOSE_-PREVENTION/Documents/Maryland%202016%20Overdose%20Annual%20report.pdf. Accessed on April 1, 2018.
- McCabe SE, West BT, Veliz P, McCabe VV, Stoddard SA, Boyd CJ, 2017. Trends in medical and nonmedical use of prescription opioids among US adolescents: 1976–2015. Pediatrics, 139, e20162387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse (NIDA)., 2019. National Survey of Drug Use and Health. https://www.drugabuse.gov/national-survey-drug-use-health. Retrieved September 1, 2019
- Rossen LM, Bastian B, Warner M, Khan D, Chong Y, 2017. Drug poisoning mortality: United States, 1999–2016. https://www.cdc.gov/nchs/data-visualization/index.htm. Accessed on April 1, 2018.
- Substance Abuse and Mental Health Services Administration., 2019. Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19‑5068, NSDUH Series H‑54). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/. Accessed on April 1, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.