Abstract
Summary: Formation of de novo intracranial aneurysms is rare. Their etiology is not known, but they are seen in patients with inherited collagen disorders, polycystic kidney disease, and familial history of aneurysms. Most de novo intracranial aneurysms are found 3–20 years after diagnosis of the initial aneurysm. We report the imaging findings in a 46-year-old man who developed a de novo intracranial aneurysm only 3 months after surgical clipping of another aneurysm.
Development of a de novo aneurysm is rare, with a frequency of 0.84–1.8% per year (1–6). De novo aneurysms most commonly appear in the anterior circulation (7). Risk factors involved in the development of these aneurysms are unclear. Sex, inherited factors, hemodynamic changes, hypertension, and cigarette smoking correlate with the higher prevalence of de novo aneurysms, but how each factor contributes to the physiopathology and how they interact are unknown. To exclude the development of new aneurysms, follow-up angiography 6 months to 5 years after aneurysm treatment is recommended (1–6, 8). We present the imaging findings in a patient who developed a de novo aneurysm in the anterior circulation after clip placement in another aneurysm. We believe that the short period in which this aneurysm developed is very unusual.
Case Report
A 46-year-old man had an acute onset of slurred speech and altered behavior. A few hours later, he developed right hemiparesis, and a CT scan revealed an acute hemorrhage in the left basal ganglia. The patient was transferred to our hospital for further evaluation and treatment. Physical examination revealed a right lateral gaze, right-central seventh cranial nerve palsy, mild right hemiparesis, slurred speech, and confusion. The patient smoked a pack of cigarettes a day and had a history of hypertension but no familial history of aneurysms. An MR image showed the acute hemorrhage in the left basal ganglia and blood in the laterals and fourth ventricle. Three-dimensional time-of-flight MR angiography of the circle of Willis revealed a saccular aneurysm measuring approximately 1.5 cm in diameter arising from the anterior communicating artery. Angiographic findings confirmed the aneurysm (Fig 1), and the patient was taken to the operating room, where an uneventful clip-placement procedure was performed. Three months after surgery, follow-up digital subtraction angiography revealed no evidence of a neck remnant or aneurysm at the site of the clip but a well-defined, new 1–2-mm de novo saccular aneurysm at the origin of the left ophthalmic artery (Fig 2). Treatment of this new aneurysm is pending.
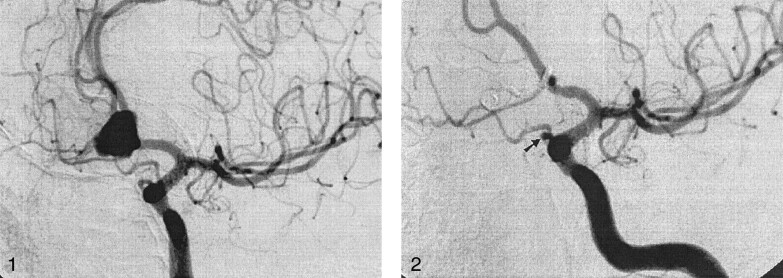
Fig 1.
Preoperative digital subtraction angiogram after injection of the left internal carotid artery, confirming the presence of the saccular aneurysm of the anterior communicating artery. No other aneurysms are seen.
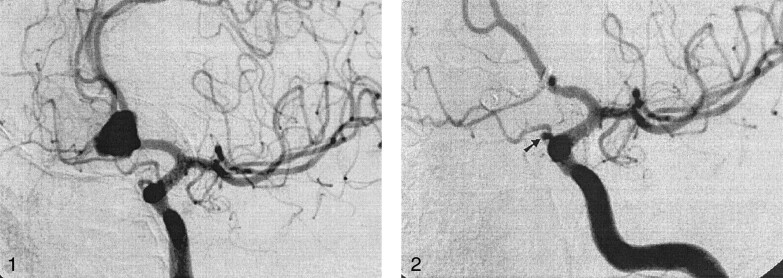
Fig 2.
Follow-up digital subtraction angiogram of the left internal carotid artery, obtained 3 months after the preoperative angiogram. There is a well-defined sacular de novo aneurysm (arrow) in the origin of the left ophthalmic artery. A clip had been placed in the previous anterior communicating aneurysm.
Discussion
In 1964, Graf and Hamby (9) reported the formation of a new aneurysm and introduced the term “de novo” aneurysm. Since then, the formation of new aneurysms remains one of the concerns in the post-treatment follow-up of patients treated for intracranial aneurysms. The pathophysiology of aneurysm formation involves changes in the vascular connective tissue such as the presence or formation of “loci minoris resistantial” and hemodynamic stress. A defect in the arterial media or injury to the elastic lamina (loci minoris resistantial) correlates with a failure of embryonic vessels or acquired changes in vessel walls, resulting from degenerative processes, trauma, hormonal changes, and connective-tissue diseases (10, 11). Hemodynamic stress such as that induced by carotid artery ligation, hypertension, or anatomic variations in the circle of Willis also correlates with aneurysm formation. Aneurysm formation may also be related to hereditary factors. There is a high prevalence of aneurysm formation in some heritable connective disorders. For example, patients with Ehlers-Danlos syndrome type IV, Marfan syndrome, neurofibromatosis type I, autosomal dominant polycystic kidney disease, and other disorders are known to develop aneurysms. Overall, these disorders are found in approximately 5% of patients with intracranial aneurysms (6). In the familial form of intracranial aneurysms, members of a family demonstrate a tendency toward aneurysm formation when no associated disorders are present. Between 7% and 20% of patients with aneurysmal subarachnoid hemorrhage have a first- or second-degree relative with a history of an intracranial aneurysm (6, 12, 13). Some familial lines support an autosomal dominant inheritance, and others support autosomal recessive or multifactorial transmission, and thus the inheritance pattern responsible for the aneurysm formation is still unclear (6, 12). Other factors that appear to correlate with aneurysm formation are hypertension, female sex, middle age, and cigarette smoking (2, 3, 6, 8, 10, 14–16). Risk factors that correlate with de novo aneurysm formation appear to be similar to those described above, in addition to a history of multiple intracranial aneurysms (1, 4, 5, 12, 14, 15, 17–22).
Although all the factors described above correlate with a higher prevalence of de novo aneurysm in several studies, no consistent pattern has been described. The only common significant risk factor that has been observed is cigarette smoking (2–4, 6, 8, 12, 15, 16, 19). The risk factors for rupture are the same for both types of aneurysms (ie, familial vs non-familial) (8, 11, 21). In reality, the incidence of de novo aneurysms may be higher than accepted, because many patients may die before the diagnosis is established.
Conclusion
Development of de novo aneurysms is rare; they are found most commonly 3–20 years after the first aneurysm. In our patient, the de novo aneurysm grew in 3 months, an occurrence seldom reported in the literature (1, 21). This observation suggests that at least some patients, even after successful aneurysm treatment, need routine angiographic follow-up studies. In addition, a new subarachnoid hemorrhage in a patient with a previously treated aneurysm dictates the need for a search of a de novo aneurysm and not only detailed evaluation of the original aneurysm.
References
- 1.David CA, Vishteh AG, Spetzler RF, et al. Late angiographic follow-up review of surgically treated aneurysms. J Neurosurg 1999;91:396–401 [DOI] [PubMed] [Google Scholar]
- 2.Sakaki T, Tominaga M, Miyamoto K, et al. Clinical studies of de novo aneurysms. Neurosurgery 1993;32:512–517 [DOI] [PubMed] [Google Scholar]
- 3.Juvella S, Poussa K, Porras M. Factors affecting formation and growth of intracranial aneurysms: a long-term follow-up study. Stroke 2001;32:485–491 [DOI] [PubMed] [Google Scholar]
- 4.Rinne JK, Hernesniemi JA. De novo aneurysms: special multiple intracranial aneurysms. Neurosurgery 1993;33:981–985 [DOI] [PubMed] [Google Scholar]
- 5.Yasui N, Magarisawa S, Suzuki A, et al. Subarachnoid hemorrhage caused by previously diagnosed, previously unruptured intracranial aneurysms: a retrospective analysis of 25 cases. Neurosurgery 1996;39:1096–1101 [DOI] [PubMed] [Google Scholar]
- 6.Schievink WI. Genetics of intracranial aneurysms. Neurosurgery 1997;40:651–663 [DOI] [PubMed] [Google Scholar]
- 7.Kanemoto Y, Hisanaga M, Bessho H. De novo vertebral artery-posterior inferior cerebellar artery aneurysm: a case report. Surg Neurol 1997;47:473–475 [DOI] [PubMed] [Google Scholar]
- 8.Tsutsumi K, Ueki K, Usui M, et al. Risk of subarachnoid hemorrhage after surgical treatment of unruptured cerebral aneurysms. Stroke 1999;30:1181–1184 [DOI] [PubMed] [Google Scholar]
- 9.Graf C, Hamby WB. Report of a case of cerebral aneurysm in an adult developing apparently de novo. J Neurol Neurosurg Psychiatry 1964;27:153–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krex D, Scharckert HK, Scharkert G. Genesis of cerebral aneurysm: an update. Acta Neurochir (Wien) 2001;143:429–449 [DOI] [PubMed] [Google Scholar]
- 11.Hademenos GJ, Massoud TF, Turjman F, et al. Anatomical and morphological factors correlating with rupture of intracranial aneurysms in patients referred for endovascular treatment. Neuroradiology 1998;40:755–760 [DOI] [PubMed] [Google Scholar]
- 12.Leblanc R. De novo formation of familial cerebral aneurysms: case report. Neurosurgery 1999;44:871–876 [DOI] [PubMed] [Google Scholar]
- 13.Hagen T, Neidl K, Piepgras U. Multiple cerebral aneurysms in identical twins. AJNR Am J Neuroradiol 1997;18:973–976 [PMC free article] [PubMed] [Google Scholar]
- 14.Misra BK, Whittle IR, Steers JW, et al. De novo sacular aneurysms. Neurosurgery 1988;23:10–15 [DOI] [PubMed] [Google Scholar]
- 15.Dietrich W, Reinprecht A, Gruber A, et al. De novo formation and rupture of an azygos pericallosal artery aneurysm. J Neurosurg 2000;93:1062–1064 [DOI] [PubMed] [Google Scholar]
- 16.Miller CA, Hill SA, Hunt WE. “De novo” aneurysms: a clinical review. Surg Neurol 1985;24:173–180 [DOI] [PubMed] [Google Scholar]
- 17.Drapkin AJ, Rose WS. Serial development of de novo aneurysm after carotid ligation: case report. Surg Neurol 1992;38:302–308 [DOI] [PubMed] [Google Scholar]
- 18.Maiuri F, Spaziante R, Signorelli F, et al. De novo aneurysm formation: report of two cases. Clin Neurol Neurosurg 1995;97:233–238 [DOI] [PubMed] [Google Scholar]
- 19.Tonn JC, Hoffmann O, Hofmann E, et al. De novo formation of intracranial aneurysm: who is at risk? Neuroradiology 1999;41:674–679 [DOI] [PubMed] [Google Scholar]
- 20.Marchel A, Bidzinski J, Bojarski P. Formation of new aneurysms: report of five cases. Acta Neurochirugia (Wien) 1991;112:96–99 [DOI] [PubMed] [Google Scholar]
- 21.Sawar M, Batnitzky S, Schecheter MM, et al. Growing intracranial aneurysms. Radiology 1976;120:603–607 [DOI] [PubMed] [Google Scholar]
- 22.Koeleveld RF, Heilman CB, Klucznik RP, et al. De novo development of an aneurysm: case report. Neurosurgery 1991;29:756–759 [DOI] [PubMed] [Google Scholar]