Abstract
Summary: We report a case of spontaneous intracranial hypotension that underwent cerebral angiography. The angiogram showed prominence of the veins and venous phase of the angiogram. This is thought to be secondary to decreased intracranial pressure and subsequent dilation of the venous system to attempt to replace the lost intracranial CSF volume. In situations in which the typical clinical presentation is not present and additional examinations such as cerebral angiography are performed, these findings may be helpful to direct the physicians involved toward the correct diagnosis.
Spontaneous intracranial hypotension (SIH) is being recognized with increasing frequency primarily because of the identification of the various MR imaging features. The initial presentation of the patient with SIH may overlap with other causes of headache and additional neurologic symptoms and therefore lead to other imaging procedures.
Case Report
A 52-year-old woman presented to the emergency department complaining of a generalized headache and pain behind her orbits. This was associated with nausea and vomiting. The previous day, while traveling, her headache became so severe that she visited an emergency department at another institution. She underwent CT. The results were said to be negative, and the patient was discharged home and advised to undergo follow-up CT. This was performed the next day and showed a lack of normal visualization of the basal cisterns (Fig 1). Subarachnoid hemorrhage was suspected, and a neurosurgeon was consulted. Cerebral angiography (including spin angiography with 3D reconstruction) was performed and did not show an aneurysm or source of subarachnoid hemorrhage. It was noted at the time of the angiography that the venules and venous structures appeared unusually prominent (Fig 2). The patient underwent a lumbar puncture with a 20-gauge spinal needle in the lateral decubitus position at the bedside, and the CSF was noted to return very slowly. Pressures were not obtained. The next day, the patient underwent contrast-enhanced MR imaging of the head, which revealed loss of the suprasellar cistern and “sagging” of the brain to the skull base (Fig 3A). Extensive dural enhancement was evident (Fig 3B and C).
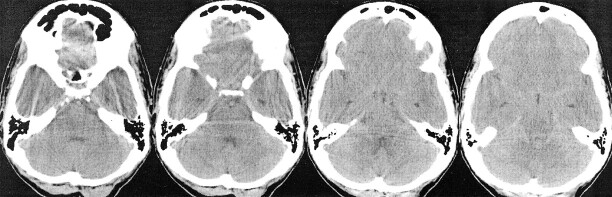
Fig 1.
Unenhanced CT scans of the head show a lack of normal visualization of the basal cisterns mimicking subarachnoid hemorrhage.
Fig 2.
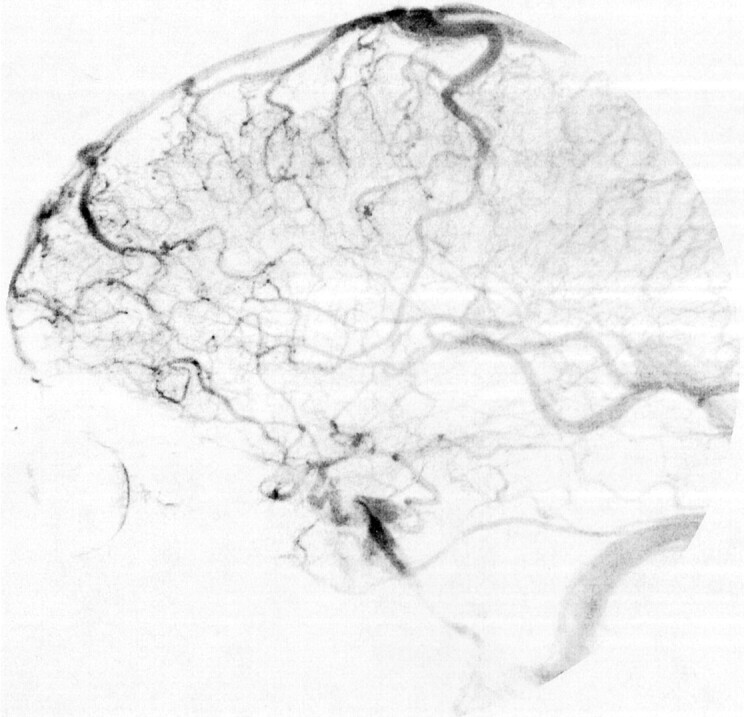
Venous phase of lateral view angiogram of the left internal carotid artery shows prominent dilation of the small and medium sized veins.
Fig 3.
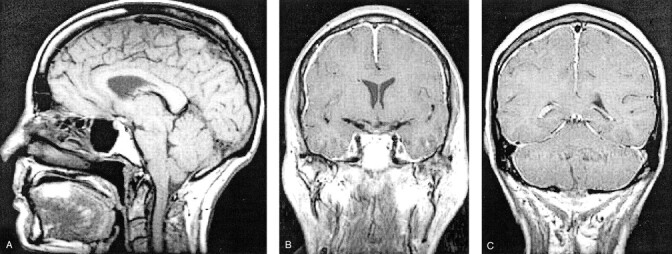
Contrast-enhanced and unenhanced MR images of the head.
A, Sagittal view T1-weighted image shows “sagging” of the brain with obliteration of the suprasellar cistern, deformity of the interpeduncular cistern and pons, and some descent of the cerebellar tonsils.
B and C, Coronal view contrast-enhanced T1-weighted images show diffuse “felt tip pen” thickening with enhancement.
The patient’s history was again carefully reviewed with the patient, and she reported that the moment of onset of her headache was when she stood up 1 month before the admission. She then reported without questioning that the headache resolved when she lay supine. This chronic headache of the previous month was different from her known previous migraine headaches. She had been seen by several physicians at different institutions for this headache during the previous month and was treated with various medications.
Immediately after the MR imaging, the patient underwent a 20-mL epidural blood patch at the C7−T1 level at the anesthesia department. The patient experienced complete relief of her postural headache after the blood patch and continued to experience relief 1 year after treatment.
Discussion
Imaging findings for SIH are largely limited to MR imaging findings. Our patient initially underwent CT, which showed a lack of visualization of the basal cisterns that may mimic subarachnoid hemorrhage. Clinical overlap of the presentation of SIH with subarachnoid hemorrhage has been previously reported (1); however, similar imaging findings have not been reported. These findings that were suggestive of subarachnoid hemorrhage, coupled with her presentation with a severe headache, resulted in evaluation with cerebral angiography.
The prominent venous dilation seen on the angiogram involved the cortical veins. This finding of prominent venous dilation associated with SIH is due to a secondary increase in the venous volume intracranially and in the spinal canal. Dural enhancement, prominent venous structures, subdural effusions and subdural hematomas, prominence of the pituitary gland, and displacement of the brain can be present on MR images of patients with SIH (2, 3). Spinal MR imaging findings include dural enhancement, prominent epidural veins, and ventral extradural fluid collections (4). Descriptions of SIH based on CT of the head are generally limited to the presence of subdural collections.
Because of the high success of treatment with an epidural blood patch, determining the site of CSF leak is usually not necessary (5). Spinal MR imaging, myleography, CT myelography, and radioisotope cisternography may help identify the level of the leak to direct therapy further, if initial blood patches are unsuccessful.
Conclusion
In the evaluation of headache and other neurologic symptoms from SIH, patients may undergo other imaging studies before undergoing MR imaging. CT may show a lack of visualization of the basal cisterns that raises the possibility of subarachnoid hemorrhage. Cerebral angiography may show prominent dilation of veins, as seen in our patient. This finding may be helpful to direct the evaluation to the more definitive tests, including contrast-enhanced MR imaging or lumbar puncture with CSF pressure measurement.
Footnotes
Presented at the 40th Annual Meeting of the American Society of Neuroradiology, Vancouver, B.C., May 10–17, 2002.
References
- 1.Schievink WI, Wijdicks EF, Meyer FB, Sonntag VK. Spontaneous intracranial hypotension mimicking aneurysmal subarachnoid hemorrhage. Neurosurgery 2001;48:513–516 [DOI] [PubMed] [Google Scholar]
- 2.Rando TA, Fishman RA. Spontaneous intracranial hypostension: report of two cases and review of the literature. Neurology 1992;42:481–487 [DOI] [PubMed] [Google Scholar]
- 3.Mokri B, Piepgras DG, Miller GM. Syndrome of orthostatic headaches and diffuse pachymeningeal gadolinium enhancement. Mayo Clin Proc 1997;72:400–413 [DOI] [PubMed] [Google Scholar]
- 4.Rabin BM, Roychowdhury S, Meyer JR, Cohen BA, LaPat KD, Russell EJ. Spontaneous intracranial hypotension: spinal MR findings. AJNR Am J Neuroradiol 1998;19:1034–1039 [PMC free article] [PubMed] [Google Scholar]
- 5.Dillon WP, Fishman RA. Some lessons learned about the diagnosis and treatment of spontaneous intracranial hypotension. AJNR Am J Neuroradiol 1998;19:1001–1002 [PubMed] [Google Scholar]