Abstract
BACKGROUND AND PURPOSE: Color duplex ultrasonography (CDU) is a standard method of noninvasive evaluation of internal carotid artery stenosis (ICAS). B-flow imaging (BFI), on the other hand, is a newer method. We investigated the accuracy of the two noninvasive tests—CDU and BFI—each separately and as a combination of the two tests by comparing with digital subtraction angiography as a reference standard.
METHODS: We performed CDU, BFI, and digital subtraction angiography on 95 consecutive patients with ICAS. Separate and combined test results of CDU and BFI were compared with digital subtraction angiography results.
RESULTS: For identifying 70% to 99% ICAS, as CDU criterion, the ratio of internal carotid artery to common carotid artery peak systolic velocity had the highest diagnostic accuracy (sensitivity, 94%; specificity, 96%). The sensitivity and specificity of BFI were 65% and 98%, respectively. With CDU and BFI, results were concordant in 144 (89%) cases for 70% to 99% ICAS. Sensitivity and specificity of combined CDU and BFI results for identification of ICAS were 95% and 99%, respectively. The misclassification rates of CDU and BFI were 4.7% and 8.1%, respectively. When combined test results were concordant, the misclassification rate decreased to 1.4%.
CONCLUSION: CDU showed a slightly better accuracy than did BFI in the diagnosis of carotid artery stenosis. Combined use of CDU and BFI is more accurate than use of either test alone.
The results of the North American Symptomatic Carotid Endarterectomy Trial, the European Carotid Surgery Trial, and the Asymptomatic Carotid Atherosclerosis Study trials have shown the importance of detecting and grading symptomatic and asymptomatic internal carotid artery stenosis (ICAS) (1–4). Those studies, which showed that severity of carotid stenosis is a fundamental criterion for surgical intervention, were based on the use of angiography. Angiography has associated neurologic and systemic risks, although less so in experienced hands (5), which decreases the benefit obtained from surgical operation (5–9). Noninvasive tests, such as color duplex ultrasonography (CDU), MR angiography, and, most recently, CT angiography have been used without the use of digital subtraction angiography in screening for carotid disease and in indicating carotid endarterectomy (10–19). Invasive diagnostic methods are necessary in only a small proportion of patients, mainly because of poor quality or inadequacy of noninvasive tests (19–23). The most widely used method among these is CDU. Although the accuracy of CDU in diagnosis of carotid stenosis is satisfactory (13–15, 24–33), benefit could be gained by pursuing further improvement.
A novel imaging technique for the detection of blood flow by using sonography (B-flow) has been developed (34–37). B-flow uses digitally encoded sonography techniques to boost blood echoes and to preferentially suppress non-moving tissue signals. B-flow imaging (BFI) provides real-time visualization of blood flow by directly visualizing blood reflectors and presenting this information in grayscale. BFI has higher spatial and temporal resolution than does Doppler imaging because of the clearer definition of the vessel lumen. The aim of this study was to assess the accuracy of the two noninvasive tests—CDU and BFI—each alone and as a combination of the two tests, by comparing their results with the results of digital subtraction angiography as a reference standard in the diagnosis of ICAS.
Methods
From April 2002 to July 2003, before undergoing coronary artery bypass grafting, 95 consecutive patients who were screened for carotid artery stenosis with CDU and who were sent for digital subtraction angiography after being diagnosed as having carotid artery stenosis were examined with BFI before digital subtraction angiography. The study group included 67 men and 28 women with a mean age of 66 years (age range, 46–85 years). Patients were excluded from this study if they had any of the following: 1) previous ipsilateral carotid endarterectomy; 2) calcification extensive enough to obscure sonography signal intensity in the stenotic area; 3) high bifurcation of the carotid artery or a short neck, which would mean that the more normal distal portion of the ICA beyond the post-stenosis dilation could not be observed; or 4) a situation that had no role in duplex velocity measurement, such as occlusion or string sign. All patients provided oral informed consent. The institutional review board approved the study.
All CDU and BFI examinations were performed by the same radiologists (M.T. and M.Y., respectively). The radiologists were unaware of each other’s test results. CDU and BFI were performed on a longitudinal plane by using a GE Logiq 700 (General Electric Company, Milwaukee, WI) equipped with a 5- to 10-MHz linear array transducer. The common carotid artery (CCA) and internal carotid artery (ICA) were scanned in transverse and longitudinal planes by using B-mode and color mode. Velocity waveforms were obtained routinely from the CCA in the center stream approximately 2 cm below the bifurcation. The ICA was sampled proximally just beyond the bulb widening. When color flow imaging showed areas of abnormal flow that appeared as heterogeneous color patterns, luminal narrowing, or both, the sample volume was moved slowly, from proximal to distal in the ICAS to obtain the highest flow velocity. The measured angle of insonation was kept at the 60-degree standard. The highest peak systolic velocity (PSV) and the end diastolic velocity of blood flow in the CCA and ICA were recorded. On the basis of these values, the ratio of the ICA to the CCA PSV (PSVICA/CCA) was calculated and recorded. Criteria for identification of 70% to 99% ICAS by CDU was based on an unpublished study of 147 patients at our laboratory who had undergone both CDU and digital subtraction angiography (Table 1). With BFI, time gain compensation was fixed in a medium position for all patients, gain was adapted for optimized image quality at approximately 50%, and the dynamic range was 60 dB, with linear grayscale calibration.
Table 1:
Color duplex ultrasonography criteria for identification of 70% to 99% internal carotid artery stensosis
| Parameters | Criteria |
|---|---|
| PSV | ≥230 cm/s |
| EDV | ≥75 cm/s |
| PSVICA/CCA | ≥3.6 |
Note.—PSV indicates peak systolic velocity; EDV, end diastolic velocity; PSVICA/CCA, ratio of internal carotid artery to common carotid artery peak systolic velocity.
Thirty-six patients with 40 ICAS were examined for interobserver variability (25 men and 11 women; mean age, 65 years; age range, 48–85 years) with mean angiographic diameter stenosis of 58 ± 17% (range, 24–84%). Each patient was examined with BFI on the same day. Two radiologists (M.Y. and M.T.) measured carotid stenosis. The radiologists were unaware of each other’s test results.
Digital subtraction angiography was performed with a Polytron V 1000 angiographic unit (Siemens, Germany) by using a Seldinger technique. The tip of a 5-French Siomons Sidewinder (Cordis, The Netherlands) catheter was positioned in the right and left CCA. From each carotid bifurcation, at least two projections were acquired. For each projection, 8 mL of contrast medium (320 mg Iodium/mL Iodixanol; Nycomed, Ireland) was injected with a flow rate of 4 mL/s.
In BFI and digital subtraction angiography studies, the degree of stenosis was assessed by comparing the maximum stenotic area of the ICA with a more normal distal portion of the depicted ICA by using North American Symptomatic Carotid Endarterectomy Trial methodology. Stenosis was calculated as [1 − (s / n)] × 100, where s is the diameter of the maximum stenotic lumen and n is the diameter of the normal vessel. The radiologist who assessed the angiograms (T.C.) was blinded for the results of ultrasonography examinations.
Test results of CDU and BFI were first analyzed separately and each compared with the reference standard digital subtraction angiography. Results were interpreted by calculating sensitivity, specificity, positive predictive value (PPV), negative predictive value, and accuracy. Secondly, CDU and BFI results were combined and considered as a single test. The combined results were again compared with digital subtraction angiography.
Interobserver agreement was analyzed by using the statistical method described by Bland and Altman (38). We calculated the mean difference of each data point as an estimate of the average bias of one observer relative to the other. Additionally, we defined the 95% confidence limits.
Results
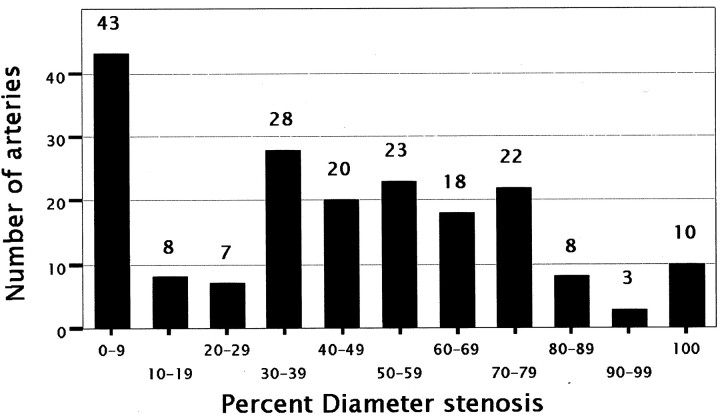
In our study, 29 carotid arteries were excluded (11 extensive calcifications, six high bifurcation of carotid artery or short neck, 10 occlusion, and two string sign). All the occlusions were diagnosed correctly with both CDU and BFI. A carotid artery in one patient that showed string sign was incorrectly evaluated as occlusion by both methods. The remaining 161 ICAs with 0–99% stenosis were included in the statistical evaluation. Seventy percent to 99% ICAS was present in 33 (17%) of nonoccluded imaged vessels. The overall distribution of carotid arteries with respect to degree of stenosis is shown in Figure 1. Images from one patient are shown in Figure 2.
Fig 1.
Graph shows distribution of ICAS according to angiographic interpretation.
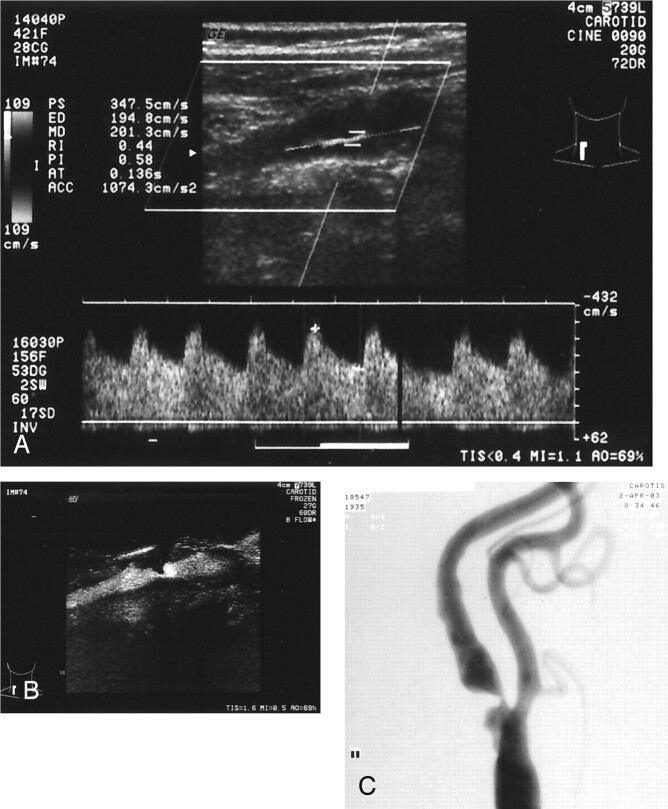
Fig 2.
Severe left ICAS in a 68-year-old woman.
A, CDU shows >70% ICAS with PSV of 347.5 cm/s, end diastolic velocity of 194.8 cm/s, and ICA to CCA ratio of 11.6.
B, 82% of ICAS is measured with BFI.
C, Digital subtraction angiography assesses 83% stenosis.
Interobserver difference of BFI measurement was 0.1% (95% confidence limits: −16.3%, 16.5%). When PSV, end diastolic velocity, and PSV ratio each was used as the CDU criterion, the results of CDU and BFI were concordant in 143 of 161 (89%), 138 of 161 (86%), and 144 of 161 (89%) of the cases, respectively.
Table 2 summarizes the sensitivity, specificity, PPV, negative predictive value, accuracy, and misclassification rate results obtained with CDU, BFI, and a combination of the two tests. Compared with digital subtraction angiography, BFI underestimated ICAS so that the sensitivity and specificity values were 65% and 98%, respectively. CDU results had slightly better accuracy compared with BFI for detection of ICAS. For identifying 70% to 99% ICAS, CDU criterion PSVICA/CCA had the highest diagnostic accuracy (its sensitivity was 94% and its specificity was 96%). The PPVs of CDU for detection of 70% to 99% ICAS were 74% for PSV, 81% for end diastolic velocity, and 83% for PSVICA/CCA, respectively. These values increased to 90%, 95%, and 95%, respectively, when combined with BFI finding. The misclassification rate of the combined test is significantly decreased in comparison with each test used alone. This decrease is more apparent when end diastolic velocity and PSVICA/CCA is used as CDU criterion.
Table 2:
Diagnostic performance color duplex ultrasonography, B-flow imaging, and a combination of these tests in detecting 70% of 99% internal carotid artery stensosis
| Criteria | Sens (%) | Spec (%) | PPV (%) | NPV (%) | ACC (%) | MRate (%) |
|---|---|---|---|---|---|---|
| BFI ≥ 70% | 65 | 98 | 91 | 92 | 92 | 8.1 |
| PSV ≥ 230 cm/s | 91 | 93 | 74 | 98 | 92 | 7.6 |
| PSV ≥ 230 cm/s + BFI ≥ 70% | 90 | 98 | 90 | 98 | 97 | 2.8 |
| EDV ≥ 75 cm/s | 91 | 95 | 81 | 98 | 94 | 5.8 |
| EDV ≥ 75 cm/s + BFI ≥ 70% | 95 | 99 | 95 | 99 | 99 | 1.4 |
| PSVICA/CCA ≥ 3.6 | 94 | 96 | 83 | 99 | 95 | 4.7 |
| PSVICA/CCA ≥ 3.6 + BFI ≥ 70% | 95 | 99 | 95 | 99 | 99 | 1.4 |
Note.—Sens indicates sensitivity; Spec, specificity; PPV, positive predictive value; NPV, negative predictive value; Acc, accuracy; MRate, misclassification rate; BFI, B-flow imaging; PSV, peak systolic velocity; EDV, end diastolic velocity; PSVICA/CCA, ratio of ICA to common carotid artery peak systolic velocity.
Discussion
CDU has now become the principal method of investigation for carotid artery stenosis. CDU is used as the sole imaging test before carotid endarterectomy in some centers. Although the accuracy of CDU for categorizing disease severity approaches 90% in accredited vascular laboratories (13–15, 24–33), concern exists regarding its reliability. A reliable confirmatory noninvasive test is needed to improve confidence in correct patient selection for carotid endarterectomy.
In deciding whether carotid endarterectomy is necessary in cases of ICAS, the use of an MR angiography and CDU combination has been proposed and has received wide acceptance (16, 21, 23, 33, 39–44). MR angiography also provides assessments of the carotid artery high in the neck, in the head and the intracranial branches.
In this study, we assessed the accuracy of CDU and BFI separately and as a combination of the two tests for determining carotid artery stenosis. BFI is a method that has been used recently in the evaluation of carotid artery stenosis. This method uses Digitally Encoded Sonography Technology (34–37). Coded sound waves are transmitted into the body and vasculature and then the returning signals to enhance sensitivity of weak signals and to suppress nonmoving tissue signals. The remainder of the data processing is essentially the same as with the conventional B-mode. Consequently, B-flow can visualize real-time hemodynamic flow in relation to stationary tissue. Advantages of this technique are simultaneous imaging of tissue and blood-echo information, so that blooming artifacts are not possible. A high frame rate is possible, as is high spatial and transverse resolution, so that imaging of complex flow phenomena becomes possible. BFI also has some limitations (34, 35). A significant technical limitation of direct BFI measurement of carotid stenoses arises in the presence of extensive plaque calcification in the carotid artery. Calcification interferes with the ability to achieve a clear sonographic window to the carotid artery. In cases in which BFI measurement cannot be made because of calcification, changing the angle and position of the probe on the patient’s neck usually can provide a sonographic window that is clear enough to measure velocities. Although BFI measurement cannot be made because of extensive calcification, it was possible to make duplex velocity measurement in nine of 11 carotid arteries in our patient group. A limitation of BFI is that excessive pulsation of the vessel leads to movement of the surrounding structures, so that the vessel wall is sometimes ill defined. Another is that sensitivity in BFI is decreased with increasing depth because of strong dependence on signal intensity strength. This limitation is especially significant in evaluation of post-bulbar ICA, because ICA toward distal is more deeply rooted. Finally, the remaining two limitations are background flash and difficulty in showing slow flow. Slow flow limitation, especially in high degree stenosis, may reduce flow velocity at distal normal ICA and may cause difficulty in imaging of lumen and measurement of diameter.
CDU also has some limitations. With CDU, duplex velocity measurement at the site of stenosis is a primary diagnostic criterion. Velocity criteria may be inaccurate in a number of clinical conditions. Although cardiac arrhythmia, aortic valve insufficiency, and tandem plaques may result in underestimation of the degree of stenosis, carotid arterial coiling or kinking, arteriovenous malformations, carotid arterial body tumors, and contralateral severe stenosis or occlusion may promote overestimation of luminal narrowing (45). Many of the limitations of duplex Doppler can be overcome by performing velocity ratio measurement (46). This ratio is not clearly superior to absolute flow velocity (24), probably because of CCA diameter variation and variable collateral flow.
Our data show that CDU is more sensitive but that BFI is more specific for the detection of 70% to 99% ICAS. Concordant results of both tests had similar sensitivity, slightly better specificity, moderately high accuracy, and markedly high PPV, compared with CDU.
When a noninvasive test is to be used as a definitive diagnostic tool for an individual patient, however, the most important parameter is the PPV of the test. In the study, combining concordant data from both tests markedly increased PPV compared with CDU. By combining CDU with BFI, the PPV increased on average by 14%. CDU provides an anatomic picture of the carotid artery and 3D physiological assessment, whereas BFI provides an anatomic 2D picture of the carotid arteries. The reason for the improved performance of a combination of these tests may be, at least in part, the use of complementary methods for determining the degree of carotid stenosis.
BFI examination does not require separate equipment and can be implemented by using the same Doppler equipment that has the necessary hardware by adding some software. Both examinations can be performed by using single equipment, which is advantageous in terms of time and cost compared with the combination of CDU and MR angiography or CT angiography. However, as is the case in our study, calcification and high bifurcation or short neck anatomy causes limitation in evaluation of carotid bifurcation with ultrasonography methods. Additionally, it is not possible to evaluate distal ICA with ultrasonography methods. The results of BFI in determining ICA stenosis are less accurate compared with the results of CDU. Despite the several disadvantages of BFI examination mentioned above, it reaches a significant value when it is used in combination with CDU.
Conclusion
CDU showed slightly better accuracy than did BFI in the diagnosis of carotid artery stenosis. Combined use of CDU and BFI provides better diagnostic accuracy than either method alone. The combined use of CDU and BFI affords accurate noninvasive evaluation of carotid artery stenosis that is sufficient for surgical planning in most cases. Digital subtraction angiography remains indicated in cases in which both tests are discordant. Because of its high specificity and good interobserver variability, BFI can be used in combination with CDU as a confirmatory test for assessment of ICAS.
References
- 1.North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 1991;325:445–453 [DOI] [PubMed] [Google Scholar]
- 2.European Carotid Surgery Trialist Collaborative Group. MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70–99%) or with mild (0–29%) carotid stenosis. Lancet 1991;337:1235–1243 [PubMed] [Google Scholar]
- 3.North American Symptomatic Carotid Endarterectomy Trial Collaborators. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. N Engl J Med 1998;339:1415–1425 [DOI] [PubMed] [Google Scholar]
- 4.Asymptomatic Carotid Atherosclerosis Study Collaborators. Endarterectomy in asymptomatic carotid artery stenosis. JAMA 1995;273:1421–1428 [PubMed] [Google Scholar]
- 5.Willinsky RA, Taylor SM, TerBrugge K, Farb RI, Tomlinson G, Montanera W. Neurologic complication of cerebral angiography: prospective analysis of 2,899 procedures and review of the literature. Radiology 2003;227:522–528 [DOI] [PubMed] [Google Scholar]
- 6.Hankey GJ, Warlow CP, Molyneux AJ. Complications of cerebral angiography for patients with mild carotid territory ischaemia being considered for carotid endarterectomy. J Neurol Neurosurg Psychiatry 1990;53:542–548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davies KN, Humphrey PR. Complications of cerebral angiography in patients with symptomatic carotid territory ischaemia screened by carotid ultrasound. J Neurol Neurosurg Psychiatry 1993;56:967–972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.AbuRahma AF, Robinson PA, Boland JP, et al. Complications of arteriography in a recent series of 707 cases: factors affecting outcome. Ann Vasc Surg 1993;7:122–129 [DOI] [PubMed] [Google Scholar]
- 9.Waugh JR, Sacharias N. Arteriographic complications in DSA era. Radiology 1992;182:243–246 [DOI] [PubMed] [Google Scholar]
- 10.Fontenelle LJ, Simper SC, Hanson TL. Carotid duplex scan versus angiography in evaluation of carotid artery disease. Am Surg 1994;60:864–868 [PubMed] [Google Scholar]
- 11.Golledge J, Ellis M, Sabharwal T, Sikdar T, Davies AH, Greenhalgh RM. Selection of patients for carotid endarterectomy. J Vasc Surg 1999;30:122–130 [DOI] [PubMed] [Google Scholar]
- 12.Collier PE. Changing trends in the use of preoperative carotid arteriography: the community experience. Cardiovasc Surg 1998;6:485–489 [DOI] [PubMed] [Google Scholar]
- 13.Winkelaar GB, Chen JC, Salvian AJ, Taylor DC, Teal PA, Hsiang YN. New duplex ultrasound scan criteria for managing symptomatic 50% or greater carotid stenosis. J Vasc Surg 1999;29:986–994 [DOI] [PubMed] [Google Scholar]
- 14.Filis KA, Arko FR, Johnson BL, et al. Duplex ultrasound criteria for defining the severity of carotid stenosis. Ann Vasc Surg 2002;16:413–421 [DOI] [PubMed] [Google Scholar]
- 15.Dinkel HP, Moll R, Debus S. Colour flow Doppler ultrasound of carotid bifurcation: can it replace routine angiography before carotid endarterectomy? Br J Radiol 2001;74:590–594 [DOI] [PubMed] [Google Scholar]
- 16.Borisch I, Horn M, Butz B, et al. Preoperative evaluation of carotid artery stenosis: comparison of contrast-enhanced MR angiography and duplex sonography with digital subtraction angiography. AJNR Am J Neuroradiol 2003;24:1117–1122 [PMC free article] [PubMed] [Google Scholar]
- 17.Moll R, Dinkel HP. Value of the CT angiography in the diagnosis of common carotid artery bifurcation disease: CT angiography versus digital subtraction angiography and color flow Doppler. Eur J Radiol 2001;39:155–162 [DOI] [PubMed] [Google Scholar]
- 18.Patel SG, Collie DA, Wardlaw JM, et al. Outcome, observer reliability, and patient preferences if CTA, MRA, or Doppler ultrasound were used, individually or together, instead of digital subtraction angiography before carotid endarterectomy. J Neurol Neurosurg Psychiatry 2002;73:21–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friese S, Krapf H, Fetter M, Klose U, Skalej M, Kuker W. Ultrasonography and contrast-enhanced MRA in ICA-stenosis: is conventional angiography obsolete? J Neurol 2001;248:506–513 [DOI] [PubMed] [Google Scholar]
- 20.Kuntz KM, Skillman JJ, Whittemore AD, Kent KC. Carotid endarterectomy in asymptomatic patients: is contrast angiography necessary? a morbidity analysis. J Vasc Surg 1995;22:706–716 [DOI] [PubMed] [Google Scholar]
- 21.Johnston DC, Goldstein LB. Clinical carotid endarterectomy decision making: noninvasive vascular imaging versus angiography. Neurology 2001;56:1009–1015 [DOI] [PubMed] [Google Scholar]
- 22.Calton WC, Franklin DP, Elmore JR, Han DC. Carotid endarterectomy: the financial impact of practice changes. J Vasc Surg 2000;32:643–648 [DOI] [PubMed] [Google Scholar]
- 23.Back MR, Wilson JS, Rushing G, et al. Magnetic resonance angiography is an accurate imaging adjunct to duplex ultrasound scan in patient selection for carotid endarterectomy. J Vasc Surg 2000;32:429–438 [DOI] [PubMed] [Google Scholar]
- 24.Hunink MG, Polak JF, Barlan MM, O’Leary DH. Detection and quantification of carotid artery stenosis: efficacy of various Doppler parameters. AJR Am J Roentgenol 1993;160:619–625 [DOI] [PubMed] [Google Scholar]
- 25.Moneta GL, Edwards JM, Papanicolaou G, et al. Screening for asymptomatic internal carotid artery stenosis: duplex criteria for discriminating 60% to 99% stenosis. J Vasc Surg 1995;21:989–994 [DOI] [PubMed] [Google Scholar]
- 26.Moneta GL, Edwards JM, Chitwood RW, et al. Correlation of North American Symptomatic Carotid Endarterectomy Trial (NASCET) angiographic definition of 70% to 99% internal carotid artery stenosis with duplex scanning. J Vasc Surg 1993;17:152–159 [DOI] [PubMed] [Google Scholar]
- 27.Carpenter JP, Lexa FJ, Davis JT. Determination of sixty percent or greater carotid artery stenosis by duplex Doppler ultrasonography. J Vasc Surg 1995;22:697–703 [DOI] [PubMed] [Google Scholar]
- 28.Carpenter JP, Lexa FJ, Davis JT. Determination of duplex Doppler ultrasound criteria appropriate to the North American Symptomatic Carotid Endarterectomy Trial. Stroke 1996;27:695–699 [DOI] [PubMed] [Google Scholar]
- 29.Neale ML, Chambers JL, Kelly AT, et al. Reappraisal of duplex criteria to assess significant carotid stenosis with special reference to reports from the North American Symptomatic Carotid Endarterectomy Trial and the European Carotid Surgery Trial. J Vasc Surg 1994;20:642–649 [DOI] [PubMed] [Google Scholar]
- 30.Hood DB, Mattos MA, Mansour A, et al. Prospective evaluation of new duplex criteria to identify 70% internal carotid artery stenosis. J Vasc Surg 1996;23:254–261 [DOI] [PubMed] [Google Scholar]
- 31.Wilterdink JL, Feldmann E, Easton JD, Ward R. Performance of carotid ultrasound in evaluating candidates for carotid endarterectomy is optimized by an approach based on clinical outcome rather than accuracy. Stroke 1996;27:1094–1098 [DOI] [PubMed] [Google Scholar]
- 32.Faugtht WE, Mattos MA, Van Bemmelen PS, et al. Color-flow duplex scanning of carotid arteries: new velocity criteria based on receiver operator characteristic analysis for threshold stenoses used in the symptomatic and asymptomatic carotid trials. J Vasc Surg 1994;19:818–827 [DOI] [PubMed] [Google Scholar]
- 33.Turnipseed WD, Kennell TW, Turski PA, Acher CW, Hoch JR. Combined use of duplex imaging and magnetic resonance angiography for evaluation of patients with symptomatic ipsilateral high-grade carotid stenosis. J Vasc Surg 1993;17:832–839 [DOI] [PubMed] [Google Scholar]
- 34.Henri P, Tranquart F. B-flow ultrasonographic imaging of circulating blood [in French]. J Radiol 2000;81:465–467 [PubMed] [Google Scholar]
- 35.Weskott HP. B-flow: a new method for detecting blood flow [in German]. Ultraschall Med 2000;21:59–65 [DOI] [PubMed] [Google Scholar]
- 36.Umemura A, Yamada K. B-mode flow imaging of the carotid artery. Stroke 2001;32:2055–2057 [DOI] [PubMed] [Google Scholar]
- 37.Bucek RA, Reiter M, Koppensteiner I, Ahmadi R, Minar E, Lammer J. B-flow evaluation of carotid arterial stenosis: initial experience. Radiology 2002;225:295–299 [DOI] [PubMed] [Google Scholar]
- 38.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;8:307–310 [PubMed] [Google Scholar]
- 39.Polak JF, Kalina P, Donaldson MC, O’Leary DH, Whittemore AD, Mannick JA. Carotid endarterectomy: preoperative evaluation of candidates with combined Doppler sonography and MR angiography. Radiology 1993;186:333–338 [DOI] [PubMed] [Google Scholar]
- 40.Patel MR, Kuntz KM, Klufas RA, et al. Preoperative assessment of carotid bifurcation. Can magnetic resonance angiography and duplex ultrasonography replace contrast arteriography? Stroke 1995;26:1753–1758 [DOI] [PubMed] [Google Scholar]
- 41.Huston J, Nichols DA, Luetmer PH, et al. MR angiographic and sonographic indication for endarterectomy. AJNR Am J Neuroradiol 1998;19:309–315 [PMC free article] [PubMed] [Google Scholar]
- 42.Serfaty JM, Chirossel P, Chevallier JM, Ecochard R, Froment JC, Douek PC. Accuracy of three-dimensional gadolinium-enhanced MR angiography in the assessment of extracranial carotid artery disease. AJR Am J Roentgenol 2000;175:455–463 [DOI] [PubMed] [Google Scholar]
- 43.Nederkoorn PJ, Mali WP, Eikelboon BC, et al. Preoperative diagnosis of carotid artery stenosis: accuracy of noninvasive testing. Stroke 2002;33:2003–2008 [DOI] [PubMed] [Google Scholar]
- 44.Johnston DC, Eastwood JD, Nguyen T, Goldstein LB. Contrast-enhance magnetic resonance angiography of carotid arteries: utility in routine clinical practice. Stroke 2002;33:2834–2838 [DOI] [PubMed] [Google Scholar]
- 45.Nicolaides AN, Shifrin EG, Bradbury A, et al. Angiography and duplex grading of internal carotid stenosis: can we overcome the confusion? J Endovasc Surg 1996;3:158–165 [DOI] [PubMed] [Google Scholar]
- 46.Zwiebel WJ. Doppler evaluation of carotid stenosis. In: Zwiebel WJ, ed. Introduction to Vascular Ultrasonography. 4th ed. Philadelphia: WB Saunders Co.;2000. :137–154