Abstract
SUMMARY: Brucellosis is a zoonotic disease characterized by multisystem involvement. Nervous system involvement is rare, with a reported incidence of 3%–13%. Brucellosis can also be manifested in the form of vasculopathy. Cerebral vasculopathy due to brucellosis is a very rare entity, with only a few cases reported in the literature. We present a patient with neurobrucellosis who had involvement of cerebral vasculature demonstrated by angiography.
Brucellosis is a multisystem disease with a large spectrum of clinical manifestations. It is endemic in certain parts of the world, especially the Middle East, Central Asia, and Mediterranean countries. The clinical presentations of brucellosis are quiet varied, because any organ system can be involved.1 Although rare, brucella is well known to cause vasculitis. Vasculitic involvement is described in the skin, extremities, aorta, and cerebral vasculature.1–3 In this report, we describe an unusual presentation of neurobrucellosis, an intracranial vasculitis demonstrated on angiography.
Case Report
A 22-year-old man was admitted with a 10-day history of progressive weakness and numbness of his left upper and lower extremities. He also complained of nausea and vomiting. His medical history revealed habitual ingestion of raw goat milk. He had been receiving tetracycline and rifampin for 2 months, with the diagnosis of brucellosis. On admission, he was alert, oriented, and afebrile. His systemic examination was unremarkable, except for mild hepatomegaly. Neurologic examination revealed central facial paralysis, hemiparesis, and mild left-sided hemihypoesthesis. His deep tendon reflexes and cerebellar tests were normal. Routine blood tests were within normal limits, except for an increase in c-reactive protein level (17.4 mg/L). Serum agglutination tests for brucella were positive, with a titer of 1/160. CSF opening pressure was in normal limits. CSF protein was elevated (42 mg/dL), and glucose levels were decreased (26 mg/dL). Brucella agglutination titers in CSF were 1/280. CSF cell count revealed lymphocytic pleocytosis. Abdominal ultrasonography (USG) demonstrated a mild hepatomegaly and the presence of the mesenteric lymph nodes. On the same day, a cranial MR imaging was performed. T2-weighted MR imaging showed a lacunar infarct on the posterior part of corona radiata (Fig 1A). This lesion was hyperintense on diffusion-weighted imaging and isohyperintense on an apparent diffusion coefficient map compatible with subacute ischemia (Fig 1B,–C). With a presumptive diagnosis of a vascular insult, digital substraction angiography (DSA) was performed. The DSA demonstrated occlusion of branches of the right middle cerebral artery (MCA), multiple vascular cutoff signs, vascular contour irregularities, and stenosis, all compatible with vasculopathy (Fig 2). On the basis of clinical history, serological data, MR imaging, and DSA findings, vasculitic involvement of neurobrucellosis was considered. Cotrimoxazole and methylprednisolone were added to the previous antibiotic therapy. With this new regimen, the patient improved clinically, and his titer decreased gradually. On follow-up, most of his symptoms had resolved and he was symptom-free by the sixth month.
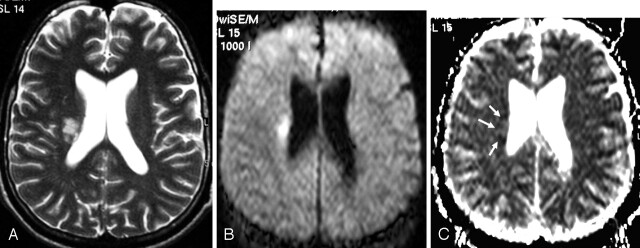
Fig 1.
T2-weighted MR imaging (A) shows an infarct of the posterior part of corona radiata. This lesion is hyperintense on diffusion-weighted imaging (B) and isohyperintense on an apparent diffusion coefficient map (C) compatible with subacute ischemia (arrows).
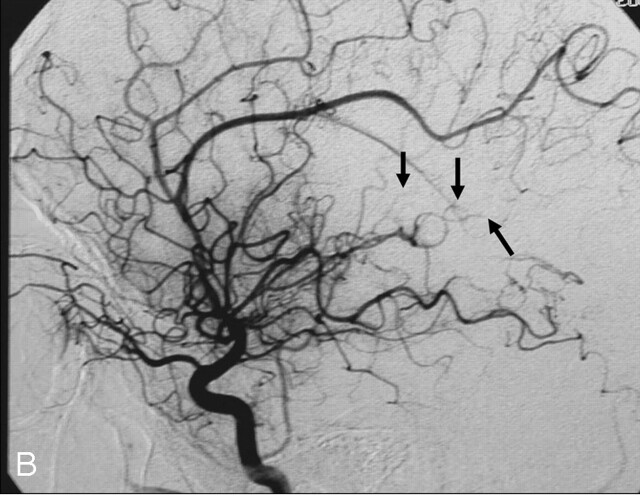
Fig 2.
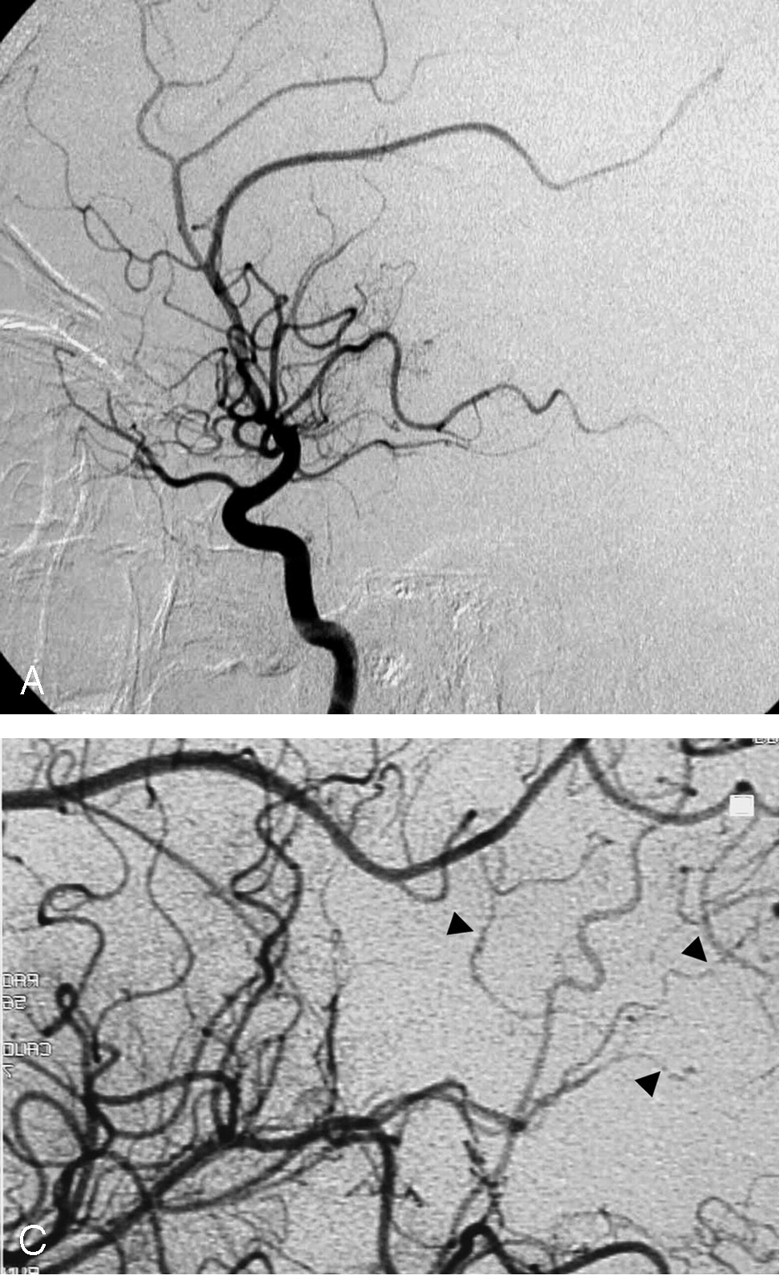
The right internal carotid artery injection with lateral view, early arterial phase (A), late arterial phase (B), and magnified late arterial phase (C) demonstrate occlusion of branches of right MCA (asterisk), multiple vascular cutoff signs (arrows), vascular contour irregularities, and stenosis (arrowheads), compatible with vasculopathy.
Discussion
Brucella remains an important human pathogen in endemic parts of the world. Brucella are gram-negative, nonmotile, facultatively intracellular coccobacilli that can replicate inside mononuclear phagocytes. After ingestion of infected products, hematogenous dissemination occurs, followed by residence in the reticuloendothelial system and resultant involvement of any organ. The spectrum of systemic involvement includes hematologic, gastrointestinal, cardiorespiratory, and musculoskeletal systems. Nervous system involvement is rare, with a reported incidence between 3% and 13%.1
Clinical presentations of neurobrucellosis are diverse and may imitate many other neurologic diseases. Frequently reported presentations are acute, subacute, and chronic meningitis, meningoencephalitis, myelopathy, polyradiculitis, mononeuritis, and vasculitis.1, 2, 4
It is well known that brucella can cause vasculitis. This disease shows no predilection of size or location of vascular structure. The affected vessel may be as small as branches supplying the dermis of the skin, though aortic involvement has also been reported.2, 3 Arterial and/or venous structures may be affected. Most of the previously reported cases include vasculitis of the dermis, presenting with skin lesions. The first case of brucella with vasculitic skin involvement confirmed by histopathologic examination was reported in 1985.5 Biopsy of the macular and purpuric lesions yielded granulomatous vasculitis. The vessels in the dermis showed fibrinoid necrosis and thrombosis. No immunoglobulin or complement deposits were detected in their study. Brucellosis is also known to cause deep venous thrombosis in the extremities. In some of these patients, the mechanism of thrombosis was explained to be due to the compressive effect of a local soft tissue mass or abscess, but it was later understood that thrombosis can also occur in the absence of an abscess, which again suggested the presence of an immune mechanism.4, 5
Most of the later reports suggested an immunologic mechanism underlying cutaneous vasculitis of brucella. Cannat et al6 reported a transient induction of autoantibodies and immune complexes in mice following injection of an extract from Brucella melitensis that was mitogenic for lymphocytes. An association between cryoglobulinemia and cutaneous vasculitis of brucella was defined by Yrivarren and Lopez.7 Three patients with brucella infection who had skin involvement were detected to have cryoglobulinemia, which disappeared after medical treatment. Skin biopsies of these patients revealed leukocytoclastic vasculitis in venules of the dermis associated with polymorphonuclear and mononuclear cell infiltration. Brucella can involve cerebral venous sinuses causing pseudotumor cerebri-like symptoms. There are only a few cases reported in the literature. The first patient with sagittal sinus thrombosis diagnosed with MR angiography was described by Zaidan and Al Tahan.8 Their patient, however, also had brucella meningitis, so it is not clear whether sinus thrombosis was due to meningitis or a vasculitic process.
Although very rare, brucellar infection can manifest as aortitis, and the resultant aneurysm may progress to an aneurysm formation. In a few of these patients, Brucella was isolated from the vascular tissue. There is, however, no definite pathophysiologic mechanism of aortic involvement, whether it is the direct insult of the Brucella or there is an immunologic process.2 Arteritis and aneurysm formation have also been reported in brachial and tibioperoneal arteries.3, 5
Cerebrovascular involvement in neurobrucellosis is explained to mainly by 2 mechanisms. The first mechanism is due to rupture of a mycotic aneurysm, which is probably a consequence of an embolic phenomenon from brucellar endocarditis. Hansmann and Schenken9 reported a case of neurobrucellosis presenting with subarachnoid hemorrhage that was caused by rupture of a mycotic aneurysm of the basilar artery. The other mechanism is inflammatory process of the vessels—namely arteritis, with resultant lacunar infarcts, small hemorrhages, or venous thromboses. In 1988, Pascual et al10 reported 2 patients with vascular insult. One patient had transient ischemic attacks, and the other was detected to have subarachnoid hemorrhage. The angiographic studies of both, however were normal. Vogt and Hasler11 presented a patient with brucellosis, with positive CSF brucella antibody titers, who had nausea, vomiting, double vision, and paresthesia of her arms and face. MR imaging of their patient revealed multiple subcortical lesions compatible with cerebral vasculitis. She was treated with antibiotics and steroids. Angiography was not performed to confirm the possible vasculopathy in that case. Another case report about cerebral vasculitis in neurobrucellosis was described by Hernandez et al,12 in 1988. In 1989, Deeb et al1 described a patient with neurobrucellosis with left hemiplegia. CT demonstrated 2 ischemic foci in the right frontoparietal region. They proposed vasculitic involvement of deep penetrating cerebral vessels, even though DSA findings were normal. To the best of our knowledge, to date there have been only 5 reports in the literature of vasculopathic involvement in neurobrucellosis, including our case.
Our patient with known brucella infection and neurologic symptoms had ischemic findings on cranial MR imaging. The DSA demonstrated occlusion of branches of the right MCA, multiple vascular cutoff signs, vascular contour irregularities, and stenosis, all compatible with vasculopathy. To our knowledge, our case is unique, being the first case of cerebrovasculitic involvement in neurobrucellosis demonstrated on angiography.
References
- 1.al Deeb SM, Yaqub BA, Sharif HS, et al. Neurobrucellosis: clinical characteristics, diagnosis, and outcome. Neurology 1989;39:498–501 [DOI] [PubMed] [Google Scholar]
- 2.Milionis H, Christou L, Elisaf M. Cutaneous manifestations in brucellosis: case report and review of the literature. Infection 2000;28:124–26 [DOI] [PubMed] [Google Scholar]
- 3.Aguado JM, Barros C, Gomez Garces JL, et al. Infective aortitis due to Brucella melitensis. Scand J Infect Dis 1987;19:483–84 [DOI] [PubMed] [Google Scholar]
- 4.Al-Sous MW, Bohlega S, Al-Kawi MZ, et al. Neurobrucellosis: clinical and neuroimaging correlation. AJNR Am J Neuroradiol 2004;25:395–401 [PMC free article] [PubMed] [Google Scholar]
- 5.Franco Vicario R, Balparda J, Santamaria JM, et al. Cutaneous vasculitis in a patient with acute brucellosis. Dermatologica 1985;171:126–28 [DOI] [PubMed] [Google Scholar]
- 6.Cannat A, Escande A, Peraldi F, et al. Induction of autoantibodies and circulating immune complexes in mice after injection of Brucella fraction “Pi” or inoculation with live Brucella suis. Ann Immunol 1983;134:43–53 [DOI] [PubMed] [Google Scholar]
- 7.Yrivarren JL, Lopez LR. Cryoglobulinemia and cutaneous vasculitis in human brucellosis. J Clin Immunol 1987;7:471–74 [DOI] [PubMed] [Google Scholar]
- 8.Zaidan R, Al Tahan AR. Cerebral venous thrombosis: a new manifestation of neurobrucellosis. Clin Infect Dis 1999;28:399–400 [DOI] [PubMed] [Google Scholar]
- 9.Hansmann GH, Schenken JR. Melitensis meningoencephalitis, mycotic aneurysm due to Br Melitensis var. porcine. Am J Pathol 1932;8:435–44 [PMC free article] [PubMed] [Google Scholar]
- 10.Pascual J, Combarros O, Polo JM, et al. Localized CNS brucellosis: report of 7 cases. Acta Neurol Scand 1988;78:282–89 [DOI] [PubMed] [Google Scholar]
- 11.Vogt T, Hasler P. A woman with panic attacks and double vision who liked cheese. Lancet 1999;24:300. [DOI] [PubMed] [Google Scholar]
- 12.Hernandez MA, Anciones B, Frank A, et al. Neurobrucellosis and cerebral vasculitis. Neurologia 1988;3:241–43 [PubMed] [Google Scholar]