Abstract
SUMMARY: We present the CT and MR imaging findings in acute methanol intoxication in a 35-year-old man who was admitted to the emergency department with weakness, blurred vision, mild bilateral areactive mydriasis, and a progressive decrease in the level of consciousness. CT and MR imaging showed bilateral putaminal hemorrhagic necrosis and subcortical white matter lesions with peripheral contrast enhancement. There was only partial improvement in patient’s Glasgow Coma Scale score during follow-up.
Methanol is a clear, colorless, highly toxic liquid with a smell and taste similar to ethanol. It is used as a constituent of a large number of commercially available solvents.
Methanol intoxication appears after accidental or suicidal oral ingestion of industrial solvents or cleaning and antifreeze liquids or occasionally is due to fraudulent adulteration of wine or other alcoholic beverages. Its ingestion can cause severe metabolic acidosis and clinical disturbances such as blindness, permanent neurologic dysfunction, and death. CT and MR imaging are able to demonstrate toxic effects of methanol in the central nervous system. Putaminal necrosis, with or without hemorrhage, and subcortical white matter lesions are the most frequent reported findings.1 We describe CT and MR imaging findings in a 35-year-old man who developed bilateral hemorrhagic putaminal necrosis and subcortical white matter confluent lesions. The case reported is unusual in that there was intense peripheral enhancement of subcortical and putaminal lesions.
Case Report
A 35-year-old man with a history of chronic alcoholism was referred to the emergency department with chest pain upon minimal exertion and autonomic dysfunction. Electrocardiography, chest radiograph, urinalysis, hemoglobin value, white blood cell count, electrolytes, and blood glucose levels were normal. The patient was discharged home with the diagnosis of probable muscular atypical chest pain.
The patient was readmitted to the hospital 24 hours later because of weakness and blurred vision. On admission, he presented mildly areactive bilateral mydriasis. Fundoscopic examination did not show papilledema. Cranial CT was normal, and arterial gasometry showed systemic metabolic acidosis (pH, 7.08; pCO2 28; CO3H, 7.6; BE-27) with high anion gap and high osmolar gap (40 mEq/L). The patient was in a comatose state and was intubated and taken to the intensive care unit (ICU). With a presumed diagnosis of methanol intoxication, bicarbonate and ethanol were administered while awaiting blood methanol level determination. Methanol blood level was 50 mg/dL. The patient underwent continuous venovenous hemodiafiltration for 96 hours after residual blood methanol levels were found. His Glasgow Coma Scale (GCS) score was 4 at that time. A cranial CT performed on day 5 showed low attenuation confluent lesions in superficial white matter and putamina consistent with acute toxic edema with high attenuation foci in the putamina consistent with hemorrhage (Fig 1).
Fig 1.
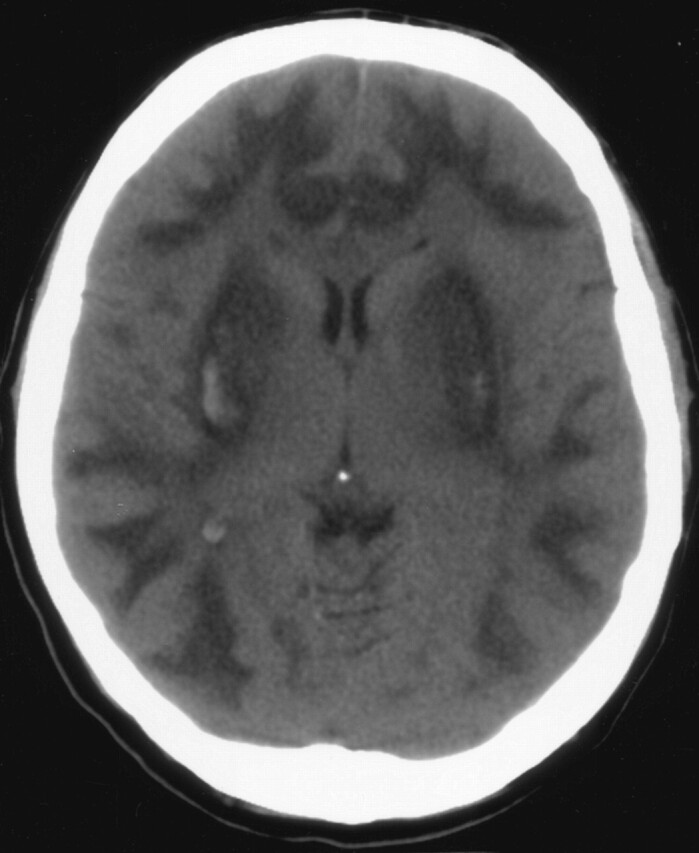
CT performed on day 5 shows low attenuation areas in subcortical white matter and both putamina with high attenuation putaminal foci consistent with hemorrhage.
MR imaging performed on a 1.5T unit on day 7 showed extensive subcortical white matter and basal ganglia abnormalities consistent with edema and bilateral putaminal hemorrhagic changes. There was peripheral rim of intense contrast enhancement in the subcortical and putaminal lesions (Figs 2–4).
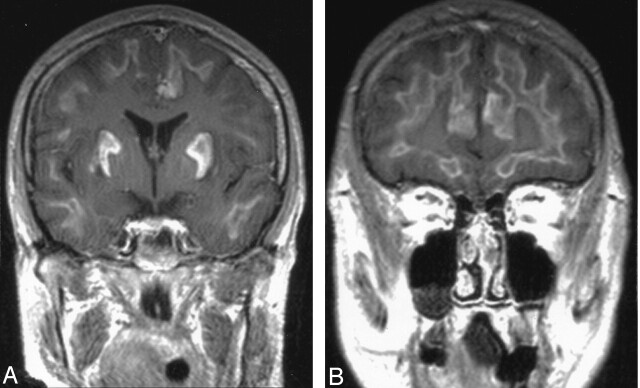
Fig 2.
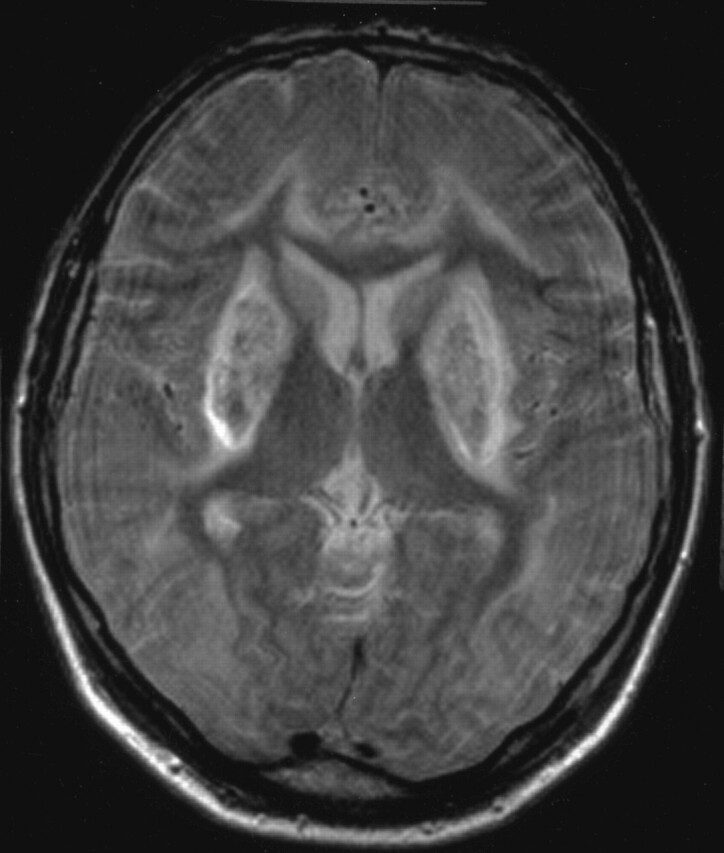
Axial fast spin-echo T2-weighted MR on day 7 shows subcortical white matter and basal ganglia hyperintensity and low-signal-intensity bilateral putaminal foci.
Fig 3.
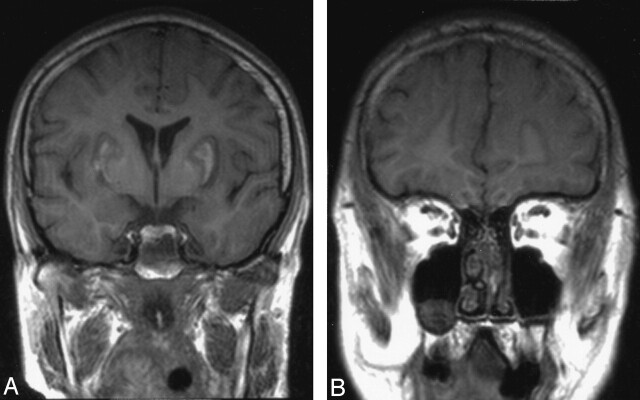
Unenhanced coronal T1-weighted image shows low signal intensity subcortical white matter and basal ganglia lesions with high-signal-intensity foci in both putamina.
Fig 4.
Contrast-enhanced coronal T1-weighted image shows intense linear peripheral enhancement in subcortical and putaminal lesions
Visual evoked potentials with closed eyes showed bilateral visual conduction disturbance. Repeat fundoscopic examination showed no abnormality. Brain stem auditory evoked potentials showed no alteration. The patient was discharged from the ICU on day 20 with a GCS score of 7, with tracheostomy in place. Pre- and postcontrast follow-up CT performed on day 24 showed bilateral putaminal volume loss and very slight enhancement of subcortical lesions (Figs 5A, -B). On day 25 the patient was discharged with family training for patient care. According to his family, the patient’s intoxication was accidental.
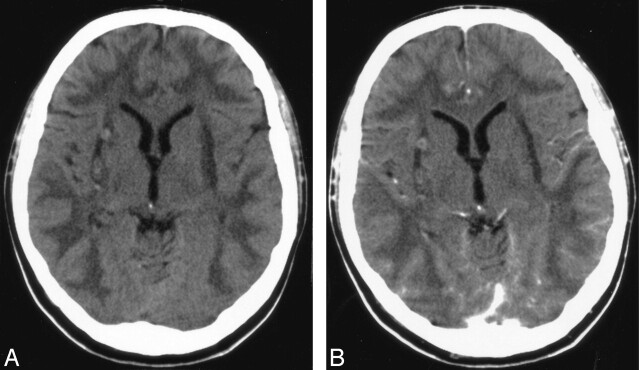
Fig 5.
Pre- (A) and postcontrast (B) follow-up CT performed on day 24 shows bilateral putaminal volume loss and very slight enhancement of subcortical and putaminal lesions.
Discussion
Acute methanol poisoning is a rare accidental or suicidal intoxication. It has also been described as a result of fraudulent adulteration of alcoholic drinks.2 The clinical presentation of methanol intoxication can vary greatly from patient to patient. A latent period of 12–24 hours often follows methanol ingestion.1 The latent period most likely corresponds to the time period in which methyl alcohol is metabolized into formaldehyde and formic acid, 2 chemicals that are more toxic than methanol.3
Susceptibility to methanol poisoning varies greatly. Acute metabolic intoxication produces severe metabolic acidosis and serious neurologic sequelae. Most patients note visual disturbances, secondary to optic nerve necrosis or demyelination, as one of the first symptoms. Central nervous symptoms are common and include headache, dizziness, weakness, and malaise. Large amounts of methanol ingestion can result in seizure, stupor, coma, and sometimes death. Gastrointestinal symptoms are common. The diagnosis is based on the presence of severe metabolic acidosis with high anion and osmolar gap and high serum methanol levels. In acute methanol intoxication, to prevent the conversion of methanol into toxic metabolites, ethanol is administered because its affinity for alcohol dehydrogenase enzyme is 10–20 times greater than that of methanol. Other therapeutic procedures include gastric lavage, correction of acidosis with sodium bicarbonate, folic acid, and secondary detoxication with hemodialysis.
The most characteristic MR findings in methanol toxicity are bilateral putaminal necroses, which may have varying degrees of hemorrhage. This finding is by no means specific to methanol toxicity but is seen also in a variety of conditions, including Wilson disease and Leigh disease.4 Putaminal necrosis and hemorrhage probably result from the direct toxic effects of methanol metabolites and metabolic acidosis in the basal ganglia.5 Cerebral and intraventricular hemorrhage, cerebellar necrosis, diffuse cerebral edema, bilateral subcortical white matter necrosis or edema, and optic nerve necrosis all have been described in severe methanol intoxication.3,5 Optic nerve demyelination secondary to myelinoclastic effect of formic acid has been suggested as responsible for optic nerve damage with or without axonal loss5 It is possible that direct toxic effects of methanol metabolites also were responsible for the subcortical and putaminal lesions.5,6 It has also been suggested that putamen is particularly at risk to various pathologic processes because of its high metabolic demand and because it lies in the boundary zones of vascular perfusion,4 though for some authors the nature of the distribution of the lesions seems to be counterevidence of a vascular cause.5 The basis for the selective vulnerability in these regions remains unknown.5 It is probably a combination of factors, including cerebral microvascular anatomy and direct toxic effects of methanol metabolites, that causes the characteristic distribution of pathologic findings, including severe alterations of subcortical white matter and central gray matter alteration with sparing of peripheral gray matter.
What is interesting in our case is the presence of intense peripheral enhancement in subcortical and putaminal lesions, a result of brain-blood barrier damage.
References
- 1.Rubinstein D, Escott E, Kelly JP. Methanol intoxication with putaminal and white matter necrosis: MR and CT findings. AJNR Am J Neuroradiol 1995;16:1492–94 [PMC free article] [PubMed] [Google Scholar]
- 2.Kuteifan K, Oesterle H, Tajahmady T, et al. Necrosis and haemorrhage of the putamen in methanol poisoning shown on MRI. Neuroradiology 1998;40:158–60 [DOI] [PubMed] [Google Scholar]
- 3.Halavaara J, Valanne L, Setala K. Neuroimaging supports the clinical diagnosis of methanol poisoning. Neuroradiology 2002;44:924–28 [DOI] [PubMed] [Google Scholar]
- 4.Hsu HH, Chen CY, Chen FH, et al. Optic atrophy and cerebral infarcts caused by methanol intoxication: MRI. Neuroradiology 1997;39:192–94 [DOI] [PubMed] [Google Scholar]
- 5.Gaul HP, Wallace CJ, Auer RN, et al. MR findings in methanol intoxication. AJNR Am J Neuroradiol 1995;16:1783–86 [PMC free article] [PubMed] [Google Scholar]
- 6.Chen JC, Schneiderman JF, Wortzman G. Methanol poisoning: bilateral putaminal and cerebellar cortical lesions on CT and MR. J Comput Assist Tomogr 1991;15:522–24 [PubMed] [Google Scholar]