Abstract
BACKGROUND AND PURPOSE: Pituitary cysts are common findings on pathologic examination and imaging studies. They are generally considered to be rarer in children than in adults; however, no good data exist to substantiate this opinion. We reviewed MR imaging studies to evaluate the frequency and imaging features of pituitary cysts in children.
METHODS: We retrospectively reviewed T1-weighted sagittal images in 341 patients <15 years of age to evaluate for pituitary cysts. Paramagnetic contrast was administered in 86 of the 341 patients. Sagittal or coronal fast spin-echo T2-weighted images were performed in 166 patients. For patients having pituitary cysts, pituitary function was examined by assessing blood levels of pituitary hormones.
RESULTS: A cystic pituitary lesion was recognized in 4 patients (1.2%) aged 1–4 years. None of the 4 manifested endocrinologic signs or symptoms or were the results of their laboratory studies abnormal. All the lesions were sharply demarcated and situated just posterior to the anterior pituitary lobe. All were iso- or hypointense compared with the pons on T1-weighted images without contrast enhancement, suggesting a Rathke cleft cyst. MR imaging of a patient with probable low-grade gliomas in the left hypothalamic region and optic chiasma showed complete resolution of a pituitary cyst at a 1-year follow-up study.
CONCLUSION: The frequency of pituitary cysts on MR imaging in childhood is almost equal to that of Rathke cleft cysts, as assessed in autopsy studies of subjects aged 10 to 29 years. These cysts are common in children and should be considered, in the absence of signs or symptoms of pituitary dysfunction, as incidental findings.
Modern neuroimaging allows the detection of tiny pituitary lesions, including not just adenomas but also small cysts. Rathke cleft cysts, the most common pituitary cysts, are nonneoplastic lesions of the sellar region, arising from embryonic remnants of Rathke’s pouch (1, 2). Although Rathke cleft cysts are congenital nonneoplastic lesions, they may enlarge, causing visual disturbances or pituitary dysfunction. They typically lie in the pars intermedia, between the anterior and posterior pituitary lobes. An evaluation of 1000 nonselected autopsy specimens revealed that 113 of the pituitary glands (11.3%) harbored incidental Rathke cleft cysts (2). Among them, 37 (3.7%) were >2 mm, which might be detected by high-resolution MR imaging (matrix size <1 × 1 mm) with thin sections.
Rathke cleft cysts in children are considered rarer than those in adults and are most often asymptomatic. In an autopsy series, no Rathke cleft cyst >2 mm was seen in children younger than 9 years of age (0/44 patients) (3). However, it is not unusual to detect a pituitary cyst on MR imaging of asymptomatic (with respect to the hypothalamic–pituitary axis) children. As a result of this observation, we retrospectively reviewed MR imaging studies of a group of children in an effort to determine the frequency of pituitary cysts in children. During the course of this study, we also found one patient in whom a cyst disappeared on a 1-year follow-up study (for an unrelated condition).
Patients and Methods
T1-weighted sagittal images from 341 patients younger than 15 years of age were retrospectively reviewed. The neurologic outpatient department of Chiba University Hospital cared for all patients between April 1994 and November 2004. The diagnosis or chief complaint (and reason for imaging) was epilepsy in 108, psychomotor retardation in 72, and headache in 40 patients.
MR imaging was performed with a 1.5-T superconducting magnet (Signa Horizon or LX, GE Healthcare, Milwaukee, WI). The parameters for spin-echo T1-weighted sagittal images were as follows: TR/TE, 400–500/9–11; matrix size, 256 × 256; field of view, 22 or 25 cm; section thickness, 4 or 3 mm; and interslice gap, 1 or 0.5 mm. Paramagnetic contrast agent was administered to 86 of the 341 patients. Sagittal or coronal fast spin-echo T2-weighted images (TR/TE, 4000/100) were obtained in 166 patients. For patients found to have a pituitary cyst, pituitary function was examined hormonally, including studies for somatomedin-C, thyroid-stimulating hormone, and thyroxine levels. No neurosurgery or brain biopsy was performed in any patient.
Results
A cystic pituitary lesion was recognized in 4 (1.2%) of the 341 patients; the ages of the affected children ranged from 1 to 4 years old. None of the 4 patients manifested any endocrinologic symptoms or any abnormalities on the results of their pituitary function tests. Their radiologic and clinical information is summarized in the Table.
Clinical and radiological data for four patients with a pituitary cyst
| Patient No./Age (y)/Sex | Chief complaint or diagnosis | MRI Findings |
|||
|---|---|---|---|---|---|
| Size (mm) | T1WI | Enhance | T2WI | ||
| 1/1/M | Developmental delay | 5 × 6 | Low | Neg | High |
| 2/1/F | Developmental delay | 4 × 4 | Low | Neg | NE |
| 3/4/M | Venous malformation | 4 × 5 | Low | Neg | High |
| 4/2/M* | Low-grade glioma | 10 × 7 | Low | Neg | High |
Note.—T1WI indicates T1-weighted image; T2WI, T2-weighted image; NE, not examined.
The MRI of the patient no. 4 at 4 years showed complete resolution of the cyst.
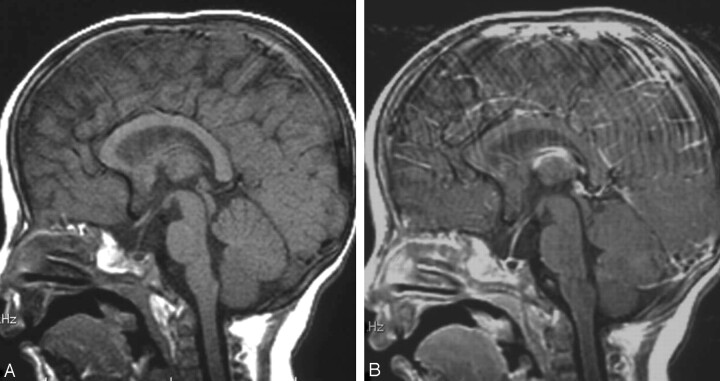
All the cystic pituitary lesions were sharply demarcated and situated just posterior to the anterior pituitary lobe. The size of the lesion ranged from 4 × 4 mm to 10 × 7 mm (the height of a normal pituitary gland is 2–6 mm during childhood before puberty, but during puberty, the height of the gland can increase to 9 mm (4). T1-weighted images revealed homogenously hypointense signal intensity compared with the pons with no enhancement of the lesion (Fig 1A, -B). T2-weighted images for 3 patients (patients 1, 3, 4) showed hyperintensity of the lesions similar to that of cerebrospinal fluid.
Fig 1.
MR images of patient 1.
Pre- (A) and postcontrast (B) T1-weighted images reveal a homogeneously hypointense (compared with the pons) mass located in the middle portion of the pituitary gland with no enhancement of the lesion; these findings suggest a diagnosis of Rathke cleft cyst (5 × 6 mm). A normal anterior lobe was recognized in the parasagittal sections (not shown).
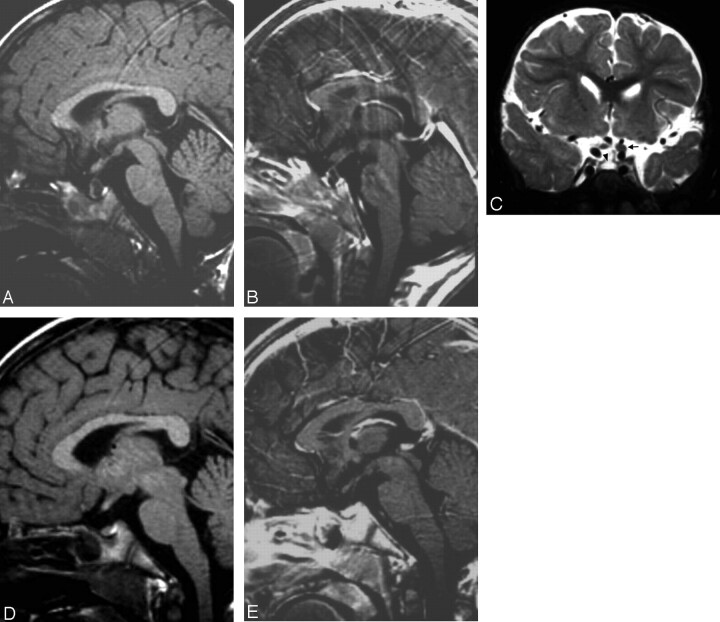
Serial MR imaging for patient 4, who had asymptomatic lesions in the left hypothalamic region and optic system, showed complete resolution of a pituitary cyst. Initial and second MR imaging at 2 and 3 years of age revealed T2 prolongation in the left hypothalamic region, left optic nerve, and optic chiasm without peripheral edema or contrast enhancement, in addition to a large pituitary cyst (hypointensity on T1- and hyperintensity on T2-weighted images, Fig 2A–C). This appearance was suggestive of a low-grade infiltrating glioma. The pituitary cyst disappeared completely at 4 years of age with no changes of the parenchymal lesions (Fig 2D, -E).
Fig 2.
MR images of patient 4.
MR images obtained when the patient was 2 years of age reveal a pituitary cyst (10 × 7 mm) without contrast enhancement, low intensity on T1-weighted images (A, B) and high intensity on T2-weighted images (arrowhead, C). Swelling of left optic nerve was recognized on T2-weighted images (arrow, C), suggesting left optic glioma. When the patient was aged 4 years (D, E), the pituitary cyst disappeared completely with no interval change of the presumed low-grade glioma.
Discussion
Asymptomatic pituitary cysts were incidentally discovered on MR imaging studies of 4 children (1.2%) <15 years of age. Although definitive distinction of pathological entities is impossible by MR imaging, their imaging features and location are suggestive of the diagnosis of Rathke cleft cysts: sharply demarcated cystic lesion situated just posterior to the anterior pituitary lobe, homogenous signal intensity, and absence of enhancement. Other types of lesions that could have a similar appearance include cystic craniopharyngiomas and cystic pituitary adenomas. Craniopharyngiomas are tumors that are postulated to arise from remnants of the craniopharyngeal duct, and thus are embryologically related to Rathke cleft cysts (2).
Radiologically the following comparisons can be drawn between cystic craniopharyngiomas and Rathke cleft cysts: the normal pituitary gland is usually identified inferior to cystic craniopharyngiomas, which are most frequently suprasellar in location; tumor wall enhancement is observed in craniopharyngiomas, but not in Rathke cleft cysts; and calcification is frequently found in craniopharyngiomas, but infrequently in Rathke cleft cysts (5). Also, enhancing solid components are present in craniopharyngiomas but not in Rathke cleft cysts.
Pituitary adenomas are typically located within the adenohypophysis, whereas Rathke cleft cysts typically lie centrally between the anterior and posterior pituitary lobes (3). Normal pituitary tissue partially or completely surrounds pituitary adenomas. In cystic adenomas, the cyst wall is composed of tumor and, therefore, is thick and irregular and enhances after contrast administration (5). On pathologic examination, cystic pituitary lesions other than Rathke cleft cysts are extremely rare; no subject was found to have a cystic lesion other than a Rathke cleft cyst in 1000 autopsied specimens (3). Therefore, although no brain pathology was available, it seems most likely that the pituitary cysts identified in our 4 patients were Rathke cleft cysts.
Rathke cleft cysts in children are considered rarer than those in adults; actually no Rathke cleft cysts >2 mm were found in 44 autopsy specimens of children <9 years of age. However, the exact prevalence in children is uncertain because of the small number of autopsy specimens. The frequency of pituitary cysts in children (4/341, 1.2%) on this MR imaging study is almost equal to that of Rathke cleft cysts in autopsy specimens from subjects aged 10 to 29 years (2/115, 1.7%) (3). If pituitary cysts seen in this study are Rathke cleft cysts, the results are compatible with the fact that Rathke cleft cysts are congenital nonneoplastic lesions. It is important for clinicians to recognize that pituitary cysts in childhood are fairly common incidental findings on MR imaging, to prevent further expensive and unnecessary evaluations. The frequency of Rathke cleft cysts >2 mm seems to increase with age to an incidence of 4.2% in patients aged >30 years (35/841) (3). This change in frequency has been attributed to the slow growth of the cysts (6).
However, despite the similarity in the numbers in our study and that of autopsy specimens of subjects from 10 to 29 years of age, we believe that we likely have underestimated the frequency of cysts as a result of the imaging techniques used in this study. Sagittal and coronal T2-weighted images and postcontrast images increase our sensitivity in the detection of these lesions; however, we do not typically perform all of these sequences in our evaluation of patients with seizures or developmental delay. When a pituitary cyst is isointense to the anterior pituitary gland on T1-weighted images, it might be overlooked if no contrast enhanced or T2-weighted images are obtained. In addition, our use of 4-mm sagittal sections likely causes smaller lesions to be missed; 2- or 3-mm sections would likely increase sensitivity. Therefore, we suspect that we might be underestimating the frequency of pituitary cysts in this retrospective study (1.2%), and the real frequency of pituitary cysts in children might be close to that of autopsy specimens in subjects aged 10 to 29 years (1.7%).
Interestingly, serial imaging of patient 4 showed complete resolution of the pituitary cyst. Rathke cleft cysts are postulated to slowly and progressively increase in size as the volume of the cyst contents increases (6). It is speculated that the imbalance between the secretion from and absorption into the cyst wall (secretion being greater than absorption) is the cause of their growth (7, 8). However, imaging of 3 patients with pathologically proven Rathke cleft cysts showed reduction of the cyst size (7). It appears, therefore, that the size of Rathke cleft cysts can both increase and decrease (albeit transiently). However, there has been no report of complete resolution of Rathke cleft cysts, as far as we know. It is tempting to explain the reduction in the size of the cysts by a decrease in the secretions of the cyst wall relative to the absorptions. Another possibility would be a partial rupture of the cyst wall. The wall of large suprasellar cystic craniopharyngiomas becomes weak as the cyst expands, rarely resulting in spontaneously rupturing into the subarachnoid space (9, 10). There has also been no report of rupture of intrasellar pituitary cysts; however, a parenchymal lesion very close to the pituitary stalk might have affected the cyst wall and caused it to rupture. More studies of longitudinal MR imaging of pituitary cysts of childhood are necessary to answer these questions.
In conclusion, the frequency of pituitary cysts on MR imaging is 1.2% in childhood, which is almost equal to that of Rathke cleft cysts in patients aged 10 to 29 years. These results suggest that incidental identification of a small cyst in the pituitary gland of a child should be considered an incidental finding in the absence of signs or symptoms referable to pituitary dysfunction.
References
- 1.Barkovich AJ. Intracranial, orbital, and neck tumor of childhood. In: Barkovich AJ, ed. Pediatric neuroimaging. 3rd ed. New York, NY: Lippincott Williams & Wilkins;2000. :443–580
- 2.Harrison MJ, Morgello S, Post KD. Epithelial cystic lesions of the sellar and parasellar region: a continuum of ectodermal derivatives? J Neurosurg 1994;80:1018–1025 [DOI] [PubMed] [Google Scholar]
- 3.Teramoto A, Hirakawa K, Sanno N, Osamura Y. Incidental pituitary lesions in 1,000 unselected autopsy specimens. Radiology 1994;193:161–164 [DOI] [PubMed] [Google Scholar]
- 4.Barkovich AJ. Normal development of the neonatal and infant brain, skull, and spine. In: Barkovich AJ, ed. Pediatric neuroimaging. 3rd ed. New York, NY: Lippincott Williams & Wilkins;2000. :13–69
- 5.Sumida M, Uozumi T, Mukada K, Arita K, Kurisu K, Eguchi K. Rathke cleft cysts: correlation of enhanced MR and surgical findings. AJNR Am J Neuroradiol 1994;15:525–532 [PMC free article] [PubMed] [Google Scholar]
- 6.Saeki N, Sunami K, Sugaya Y, Yamaura A. MRI findings and clinical manifestations in Rathke cleft cyst. Acta Neurochir 1999;141:1055–1061 [DOI] [PubMed] [Google Scholar]
- 7.Saeki N, Kubota M, Yamaura A, Ishige N. Fluctuating visual field defects in Rathke cleft cysts: MRI analysis. J Clin Neurosci 1999;6:524–527 [DOI] [PubMed] [Google Scholar]
- 8.Yoshida J, Kobayashi T, Kageyama N, Kanzaki M. Symptomatic Rathke’s cleft cyst: morphological study with light and electron microscopy and tissue culture. J Neurosurg 1977;47:451–458 [DOI] [PubMed] [Google Scholar]
- 9.Satoh H, Uozumi T, Arita K, et al. Spontaneous rupture of craniopharyngioma cysts: a report of five cases and review of the literature. Surg Neurol 1993;40:414–419 [DOI] [PubMed] [Google Scholar]
- 10.Petito CK, DeGirolami U, Earle KM. Craniopharyngiomas: a clinical and pathological review. Cancer 1976;37:1944–1952 [DOI] [PubMed] [Google Scholar]