Abstract
Summary: We report 2 patients with dural arteriovenous fistula of the anterior condylar vein in which the patients presented with rare clinical symptoms related to unusual venous drainage patterns. The first patient had progressive myelopathy and showed venous drainage into the anterior spinal vein. The second had ocular signs and showed retrograde drainage into the superior ophthalmic vein. Complete cure was attained by transarterial glue injection in the first patient and transvenous coil embolization in the latter.
Dural arteriovenous fistula of the anterior condylar vein is an important, but rare, subgroup of posterior fossa dural arteriovenous fistula. This lesion tends to be confused with marginal sinus dural arteriovenous fistula, and, to our knowledge, there are only 4 previous reports in the literature (1–4). In most of the reported cases, the dural arteriovenous fistula drained into the jugular bulb and only presented with pulse-synchronous tinnitus. Here we report 2 cases of dural arteriovenous fistula of the anterior condylar vein with unusual venous drainage. Clinically, one patient showed myelopathy, whereas the other showed ocular manifestations. The consideration of therapeutic strategy was made on the key points of establishing accurate image diagnosis, the functional anatomy of the anterior condylar vein, and the tactics for successful endovascular treatment based on the specific anatomical features of each patient.
Case Reports
Case 1
History.
A 70-year-old man first noticed sensory disturbance of the left lower extremity 2 years before admission. The symptoms had slowly progressed since then, and the sensory disturbance had spread to the lower half of the body. Furthermore, the patient had difficulty walking because of progressive weakness of both lower extremities in the 2 months before admission.
Examination.
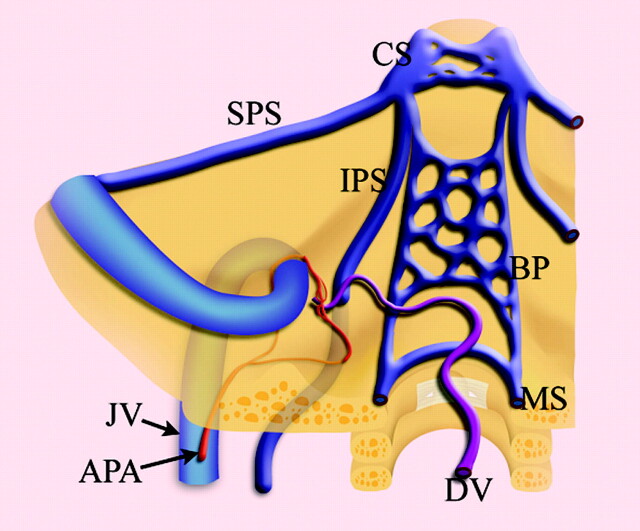
Neurologic examination on admission demonstrated slight weakness of the right upper extremity, moderate weakness of the bilateral lower extremities, and sensory disturbance of the lower half of the body (all modalities). T2-weighted MR imaging showed diffuse swelling and high signal intensity spreading from the medulla oblongata down to the entire cervical cord and tortuous signal intensity voids in the premedullary subarachnoid space (Fig 1). Transcatheter arteriography demonstrated a dural arteriovenous fistula fed by neuromeningeal branches of the ascending pharyngeal artery and jugular branches of the occipital artery. The dural arteriovenous fistula drained into the anterior spinal vein via the transverse and medial anterior pontomesencephalic vein (Fig 2). We identified the fistulous point on the intracranial portion of the anterior condylar vein on the source images of contrast-enhanced MR angiography (Fig 3). The anterior condylar vein usually joins the inferior petrosal sinus that drains to the jugular bulb, but in this case, the inferior petrosal sinus went straight down to the jugular vein without joining the jugular bulb in the venous phase of the vertebral angiography. These anatomical features are shown schematically in Figure 4.
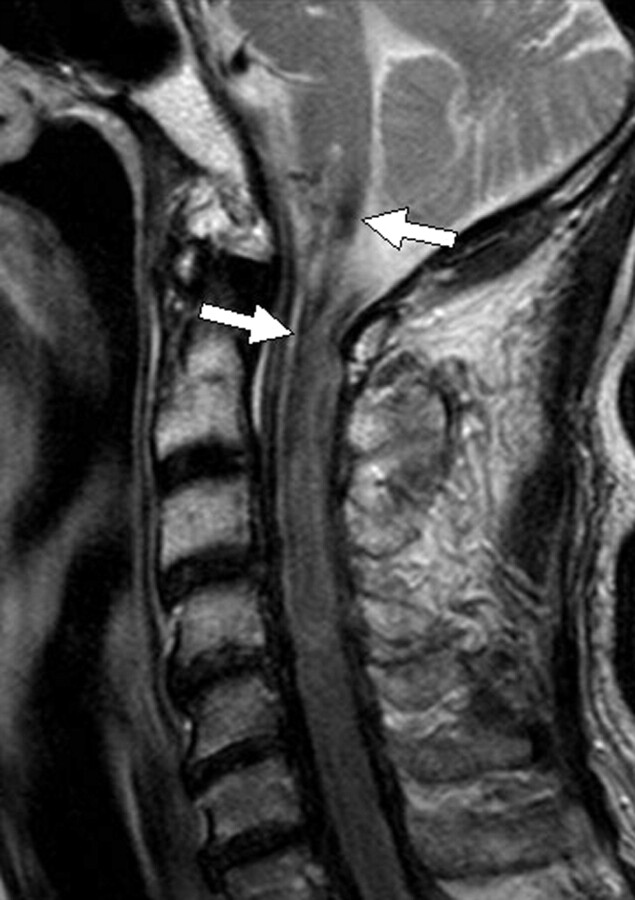
Fig 1.

Preoperative T2-weighted MR image. The medulla oblongata and cervical spinal cord show diffuse high signal intensity. Note the tortuous signal intensity voids in the premedullary subarachnoid space (arrows).
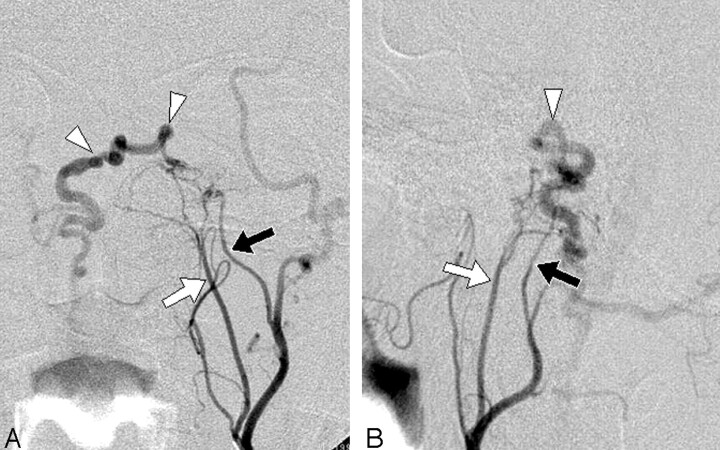
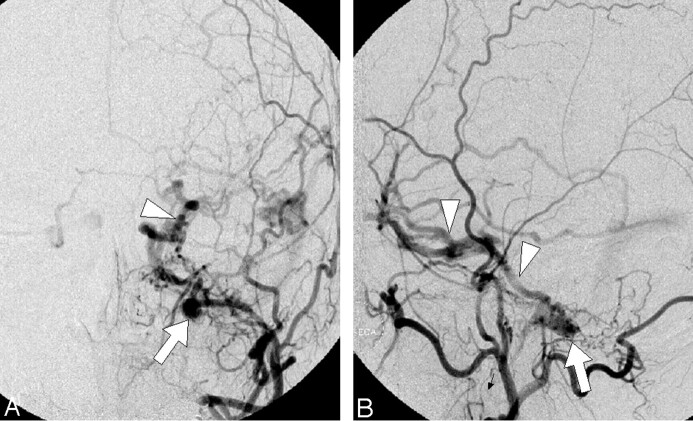
Fig 2.
Frontal (A) and lateral (B) views of preoperative external carotid arteriography. The dural arteriovenous fistula is fed by neuromeningeal branches of the ascending pharyngeal artery (white arrow) and a jugular branch of the occipital artery (black arrow) and drains into the pontomesencephalic vein (arrowheads).
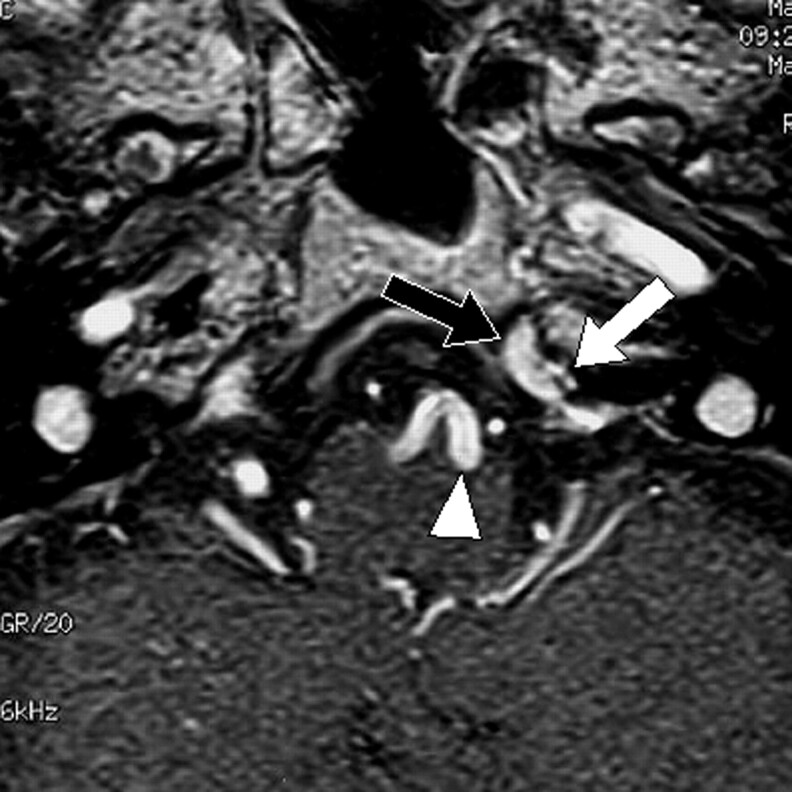
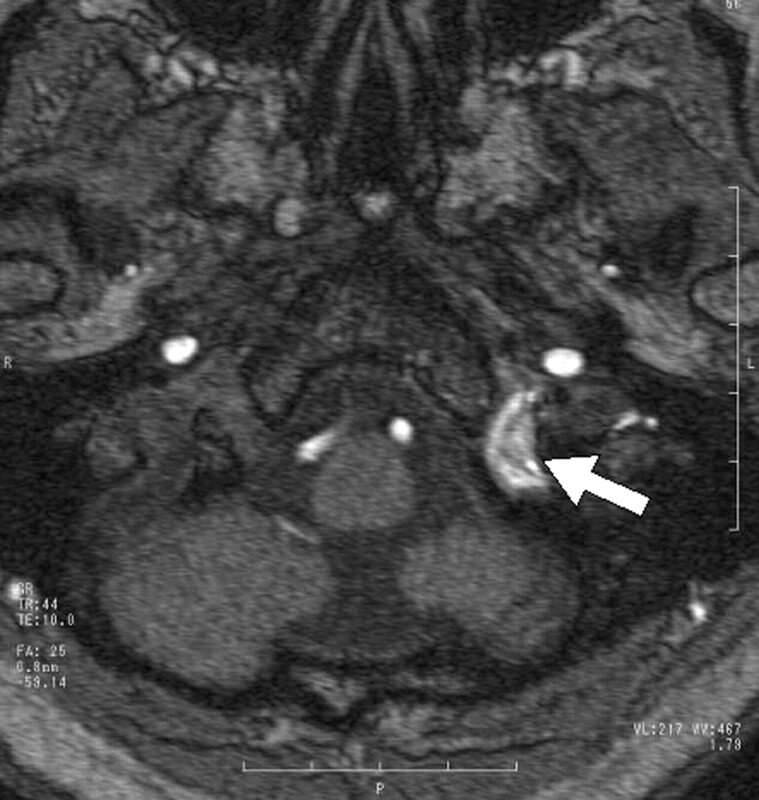
Fig 3.
Source image of contrast-enhanced 3D MR angiography. The branches of the ascending pharyngeal artery (white arrow) flow into the anterior condylar vein (black arrow). The arrowhead indicates the dilated anterior pontomesencephalic vein draining from the anterior condylar vein.
Fig 4.
Schematic drawing of the dural arteriovenous fistula and surrounding venous structures in case 1. APA indicates the ascending pharyngeal artery; DV, drainage vein; CS, cavernous sinus; SPS, superior petrosal sinus; IPS, inferior petrosal sinus; BP, basilar plexus; MS, marginal sinus; JV, jugular vein.
Embolization.
Initially, a microcatheter (Renegade, Boston Scientific Japan, Tokyo, Japan) was advanced into the neuromeningeal branch of the ascending pharyngeal artery through a 6F guiding catheter (Guider, Boston Scientific Japan), followed by injection of 20% N-butyl cyanoacrylate in Lipiodol (iodized oil, Andre Guerbet, Aulnay-sous-bois, France). Because the control angiography revealed some residual filling of the fistula, the jugular branch of the occipital artery was also embolized using 20% N-butyl cyanoacrylate. The amount of diluted N-butyl cyanoacrylate used for each feeding pedicle was 0.15 and 0.1 mL, respectively.
Postprocedural course.
A small amount of shunt flow was seen on the control angiography performed immediately after the procedure, but the follow-up angiography performed after 1 week demonstrated complete disappearance of the shunt. The premedullary signal intensity voids disappeared on MR images obtained at 5 days after the treatment. Follow-up MR images obtained after 14 months revealed marked regression of the brain stem and spinal cord edema (Fig 5). A neurologic check-up performed at 1 year after the procedure revealed that the weakness of the upper extremity had fully recovered, whereas the paralysis of the lower extremities had only slightly recovered.
Fig 5.
MR image obtained at 14 months after the procedure. The brain stem and spinal cord edema has completely disappeared. Low-signal-intensity areas (arrows) indicate deposition of hemosiderin due to previous venous congestion and infarction.
Case 2
History.
A 65-year-old woman had suffered from left tinnitus for 13 years but had never sought medical attention. The patient developed left exophthalmus and chemosis 6 months before admission.
Examination.
A physical examination demonstrated marked exophthalmus and chemosis on the left side. Pulse-synchronous tinnitus was audible over the left eye and mastoid process. T2-weighted MR imaging showed a saccular signal intensity void in the left hypoglossal canal (Fig 6). Transcatheter arteriography demonstrated a dural arteriovenous fistula located just medial to the left jugular bulb. The dural arteriovenous fistula was fed by meningeal branches of the left ascending pharyngeal and occipital arteries (Fig 7). The dural arteriovenous fistula drained into the superior ophthalmic vein via the inferior petrosal and cavernous sinuses in a retrograde fashion. There was no antegrade drainage into the jugular bulb. The source images of preoperative time-of-flight MR angiography revealed that the fistula was in the plexal part of the anterior condylar vein within the left hypoglossal canal (Fig 8).
Fig 6.
Preoperative T2-weighted MR image. A saccular signal intensity void is seen in the left hypoglossal canal (arrow).
Fig 7.
Frontal (A) and lateral (B) views of preoperative external carotid arteriography. The dural arteriovenous fistula is fed by meningeal branches of the ascending pharyngeal artery and occipital artery. A dilated venous sac is seen at the fistulous point (arrow). Note the retrograde venous drainage via the inferior petrosal sinus and cavernous sinus (arrowheads).
Fig 8.
Source image of time-of-flight MR angiography. The saccular high signal intensity indicates the venous sac of the anterior condylar dural arteriovenous fistula (arrow).
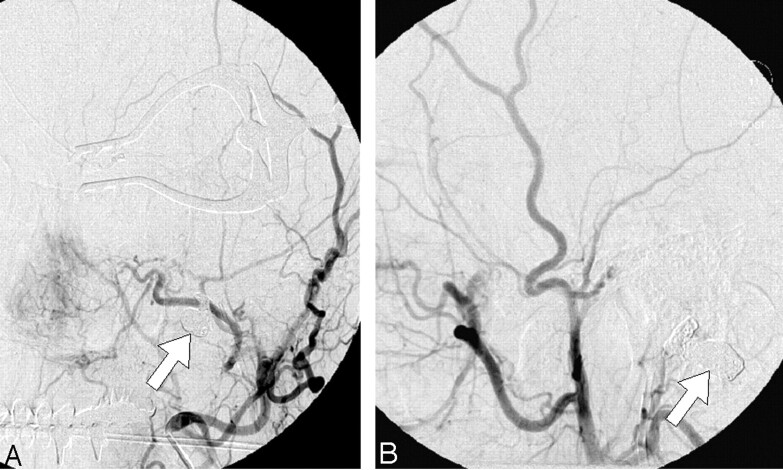
Embolization.
Because there was no accessible route to the anterior condylar vein via the jugular bulb, a mirocatheter (Excelsior, Boston Scientific Japan) was introduced into the left superior ophthalmic vein after surgically exposing the frontal vein in the upper eyelid. The microcatheter was then advanced into the anterior condylar vein. The dilated venous pouch was tightly packed with Guglielmi detachable coils and fibered platinum coils (Boston Scientific Japan). A left carotid arteriogram obtained immediately after the procedure showed complete disappearance of the dural arteriovenous fistula (Fig 9).
Fig 9.
Frontal (A) and lateral (B) views of a postoperative angiogram. The dural arteriovenous fistula has completely disappeared. The arrows indicate the mass of metallic coils placed in the venous pouch.
Clinical course after the procedure.
There was instantaneous disappearance of the pulse-synchronous bruit. The exophthalmus and chemosis showed marked improvement 1 day after the procedure and completely disappeared after 1 week.
Discussion
Anatomic knowledge of the venous system of the craniocervical region is important for understanding the physiology of cephalic venous drainage. It is also important for elucidating the pathomechanisms of clinical manifestations and establishing treatment strategies for dural arteriovenous fistulas in this region. The condylar and mastoid emissary veins are venous connections between the dural sinuses of the posterior fossa and the vertebral venous system. Regarding the functions of these venous systems, recent anatomical studies have suggested that the jugular veins are the primary route and the plexuses are inactive when mammals and reptiles are in a horizontal position. Head tilting induces partial jugular collapse and increased shunt of the cephalic efflux into the plexuses. Such a positional discrepancy is brought about by the structural differences between the 2 venous systems because the compliant jugular veins are incapable of sustaining the negative intraluminal pressures induced by upright posture, whereas the plexuses remain patent and provide a low-pressure route for venous return (5, 6).
For successful transvenous embolization of a dural arteriovenous fistula of the craniocervical junction, precise catheterization to the fistulous point based on accurate knowledge of the complex anatomy is mandatory. As a drainage route from the cavernous sinus, the inferior petrosal sinus joins the jugular bulb immediately after branching the anterior condylar vein. Passing through the hypoglossal canal, the anterior condylar vein connects the jugular vein to the internal vertebral venous plexus. In addition, it is known that the anterior condylar vein has anastomoses to the prevertebral venous plexus and basilar plexus (7). Venous structures around the jugular foramen have connections with premedullary veins via bridging veins (8). Thus, the anterior condylar vein has many communications with surrounding venous structures, and it is therefore natural that an anterior condylar dural arteriovenous fistula may have several different venous drainage patterns.
Digital subtraction angiography is a standard examination for diagnosing intracranial dural arteriovenous fistulas, but its capability for identifying the accurate location of the fistulous point of a skull base dural arteriovenous fistula is occasionally limited. Recent developments in radiologic equipment and imaging techniques, such as MR angiography and CT angiography, now allow accurate identification of the location of arteriovenous shunts. In our case, the source images of MR angiography, namely contrast-enhanced fast gradient-echo MR angiography and time-of-flight MR angiography, clearly depicted the locations of the dural arteriovenous fistulas and the relationships of their feeding and draining vessels. As previously reported, contrast-enhanced MR images are especially useful for depicting venous structures at the craniocervical junction (9). It is known that the flow of the anterior condylar vein and other venous structures are affected by the patient’s body position. Therefore, transcatheter angiography and time-of-flight MR angiography in a resting supine position cannot depict all of the emissary veins. In contrast, enhanced MR images, which are least affected by the flow velocity, can show the details of the veins.
A dural arteriovenous fistula in the posterior fossa rarely involves the anterior condylar vein. To our knowledge, there are only 4 reports of dural arteriovenous fistulas of the anterior condylar vein (1–4), which contain a total of 6 cases. Four of the patients had pulse-synchronous tinnitus because the fistula exclusively drained into the jugular bulb. The remaining 2 presented ocular symptoms caused by retrograde drainage of the fistulas into the inferior petrosal and cavernous sinuses (2, 3). Our case 2 may be the first reported with myelopathy caused by venous hypertension in the anterior spinal vein related to unusual drainage from the anterior condylar vein.
Intracranial dural arteriovenous fistulas causing myelopathy are uncommon. Asakawa et al (10) reported a case of a foramen magnum dural arteriovenous fistula with myelopathy and reviewed previous reports. The authors commented that 31 cases of intracranial dural arteriovenous fistulas, including craniocervical junction dural arteriovenous fistulas, with myelopathy had been reported. According to their review, the dural arteriovenous fistulas were predominantly located at the foramen magnum, tentorium, and superior petrosal sinus. These anatomical locations contain venous structures, including the marginal sinus and petrosal vein, which are directly related to the spinal and pontomesencephalic veins. Therefore, it is understandable that dural arteriovenous fistulas located at these points may have unusual spinal venous drainage.
Transfemoral transvenous coil embolization has long been recognized as the most effective measure for treating an intracranial dural arteriovenous fistula (11–14). However, this was not appropriate for our case 1 because a transvenous approach was not possible. Therefore, we were obliged to resort to transarterial embolization. Transarterial embolization with solid embolic materials, such as particulate emboli or metallic coils, was not indicated because of the high possibility of recurrence. Dural arteriovenous fistulas with a small and localized fistula can be obliterated by penetrating the fistula with a small amount of a low-concentration liquid embolic material such as N-butyl cyanoacrylate (15–17). Transarterial embolization of neuromeningeal arteries using liquid embolic material, such as in our case 1, has a risk of cranial nerve palsy. Because the patient had presented with progressive palsy of the upper and lower extremities, we emphasized prevention of tetraplegia and decided to embolize the neuromeningeal branches, despite a risk of cranial nerve palsy. For our case 2, a transjugular approach to the anterior condylar vein could not be applied because of the lack of a connection between this vein and the jugular bulb. Therefore, the dural arteriovenous fistula was approached via the superior ophthalmic vein by surgically exposing the frontal vein in the upper eyelid. This technique has been reported to be useful for cavernous dural arteriovenous fistulas with occlusion of the inferior petrosal sinuses (18).
Conclusion
Dural arteriovenous fistula of the anterior condylar vein is rare but should be noted as a possible cause of cervical myelopathy and ocular symptoms. Transcatheter embolization performed using an appropriate approach and embolic material can bring about a complete cure. For successful embolization, precise recognition of the location of the dural arteriovenous fistula and its drainage pattern is mandatory. Judicious use of digital subtraction angiography and source images of MR angiography provides useful information regarding the location of the dural arteriovenous fistula and its relationships with drainage vessels.
References
- 1.Ernest R, Bulas R, Tomsick T, van Loveren H, Aziz KA. Three cases of dural arteriovenous fistula of the anterior condylar vein within the hypoglossal canal. AJNR AM J Neuroradiol 1999;20:2016–2020 [PMC free article] [PubMed] [Google Scholar]
- 2.Kiyosue H, Tanoue S, Okahara M, Mori M, Mori H. Occular symptoms associated with a dural arteriovenous fistula involving the hypoglossal canal: selective transvenous coil embolization. J Neurosurg 2001;94:630–632 [DOI] [PubMed] [Google Scholar]
- 3.Arai Y, Ishii H, Handa Y, et al. Dural arteriovenous fistula within the hypoglossal canal successfully treated by transvenous embolization. Interventional Neuroradiology 2004;10:59–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Komiyama M, Ishiguro T, Matsuzuka Y, Yasui T. Intense pulse-synchronous tinnitus caused by dural arteriovenous fistula at the hypoglossal canal [in Japanese]. No To Shinkei 2002;54:830–831 [PubMed] [Google Scholar]
- 5.San Millan Ruiz D, Gailloud P, Rufenacht DA, Delavelle J, Henry F, Fasel JH. The craniocervical venous system in relation to cerebral venous drainage. AJNR Am J Neuroradiol 2002;23:1500–1508 [PMC free article] [PubMed] [Google Scholar]
- 6.Zippel KC, Lillywhite HB, Mladinich CR. New vascular system in reptiles: anatomy and postural hemodynamics of the vertebral venous plexus in snakes. J Morphol 2001;250:173–184 [DOI] [PubMed] [Google Scholar]
- 7.Katsuta T, Rhoton AL, Matsushima T. The jugular foramen: microsurgical anatomy and operative approaches. Neurosurgery 1997;41:149–201 [DOI] [PubMed] [Google Scholar]
- 8.Rhoton AL. The posterior fossa veins. Neurosurgery 2000;47(suppl):S69–92 [DOI] [PubMed] [Google Scholar]
- 9.Caruso RD, Rosenbaum AE, Chang JK, Joy SE. Craniocervical junction venous anatomy on enhanced MR images: the suboccipital cavernous sinus. AJNR Am J Neuroradiol 1999;20:1127–1131 [PMC free article] [PubMed] [Google Scholar]
- 10.Asakawa H, Yanaka K, Fujita K, Marushima A, Anno I, Nose T. Intracranial dural arteriovenous fistula showing diffuse MR enhancement of the spinal cord: case report and review of the literature. Surg Neurol 2002;58:251–257 [DOI] [PubMed] [Google Scholar]
- 11.Halbach VV, Higashida RT, Hieshima GB, Mehringer CM, Hardin CW. Transvenous embolization of dural fistulas involving the transverse and sigmoid sinuses. AJNR Am J Neuroradiol 1989;10:385–392 [PMC free article] [PubMed] [Google Scholar]
- 12.Halbach VV, Higashida RT, Hieshima GB, Hardin CW, Pribram H. Transvenous embolization of dural fistulas involving the cavernous sinus. AJNR Am J Neuroradiol 1989;10:377–383 [PMC free article] [PubMed] [Google Scholar]
- 13.Urtasun F, Biondi A, Casaco A, et al. Cerebral dural arteriovenous fistulas: percutaneous transvenous embolization. Radiology 1996;199:209–217 [DOI] [PubMed] [Google Scholar]
- 14.Roy D, Raymond J. The role of transvenous embolization in the treatment of intracranial dural arteriovenous fistulas. Neurosurgery 1997;40:1133–1144 [DOI] [PubMed] [Google Scholar]
- 15.Iizuka Y, Maehara T, Hisii M, Miyajima M, Arai H. Successful transarterial glue embolization by wedged technique for a tentorial dural arteriovenous fistula presenting with a conjunctival injection. Neuroradiology 2001;43:677–679 [DOI] [PubMed] [Google Scholar]
- 16.Nelson PK, Russell SM, Woo HH, Alastra AJ, Vidovich DV. Use of a wedged microcatheter for curative transarterial embolization of complex intracranial dural arteriovenous fistulas: indications, endovascular technique, and outcome in 21 patients. J Neurosurg 2003;98:498–506 [DOI] [PubMed] [Google Scholar]
- 17.Liu HM, Huang YC, Wang YH, Tu YK. Transarterial embolisation of complex cavernous sinus dural arteriovenous fistulae with low-concentration cyanoacrylate. Neuroradiology. 2000;42:766–770 [DOI] [PubMed] [Google Scholar]
- 18.Venturi C, Bracco S, Cerase A, et al. Endovascular treatment of a cavernous sinus dural arteriovenous fistula by transvenous embolisation through the superior ophthalmic vein via cannulation of a frontal vein. Neuroradiology 2003;45:574–578. Epub 2003 Jul 10 [DOI] [PubMed] [Google Scholar]