Abstract
Summary: An acute intracranial embolus may be associated with a hyperdense artery sign on CT, related to acute thrombus within the affected artery, a phenomenon that is well known and has been extensively documented. We present an unusual case of a middle cerebral artery territory acute infarct with a hypodense artery on CT. The Hounsfield unit attenuation of the embolic lesion was fat density. CT angiography and MR imaging confirmed the fatty lesion to be within the middle cerebral artery.
CT findings in acute stroke may be subtle or even undetectable on initial examinations, even when a large territory is involved (1). Various signs have been described as markers of early acute stroke on CT. Increased attenuation of the middle cerebral artery due to clot was first described in the early 1980s (2). Since that time, the “hyperdense middle cerebral artery” sign has been described as a marker of thrombus in the middle cerebral artery (3, 4), and several studies have demonstrated that the hyperdense middle cerebral artery sign is a common finding when CT is performed within a few hours from the onset of symptoms (5–8). False-positive hyperdense middle cerebral artery signs have been noted in patients with a high hematocrit level or calcification in the middle cerebral artery, but in these cases, the abnormal attenuation is usually bilateral (5, 8–10). In our patient, a fat embolus caused a hypodense appearance of the middle cerebral artery with an associated acute middle cerebral artery territory infarct.
Case Report
A 78-year-old woman with no significant medical history underwent an abdominoperineal resection for rectal adenocarcinoma in February 2002. At that time, mitral regurgitation was discovered, which progressed clinically to the point where she required surgical treatment. On January 28, 2004, she underwent mitral valve replacement. The surgical anatomy was complicated, but there were no intraoperative complications. In the immediate postoperative period, she was noted to have a decreased level of consciousness, a dense right hemiplegia, and aphasia. CT of the head performed on the first postoperative day demonstrated an early acute large left middle cerebral artery territory infarct. There was a hypodense filling defect in the left M1 proximal trunk, and the Hounsfield unit measurement of it indicated fat attenuation, with the lowest Hounsfield unit measurement of the intraluminal embolus being −25 H (Fig 1). Two subsequent CT scans, obtained during the next few days, demonstrated similar findings. CT angiography performed on the 13th postoperative day confirmed that the fatty lesion was intraluminal (Fig 2). CT angiography also demonstrated patent left common and internal carotid arteries without significant stenosis or atherosclerotic plaque. The fat embolus likely came from the surrounding tissues during the cardiac surgery.
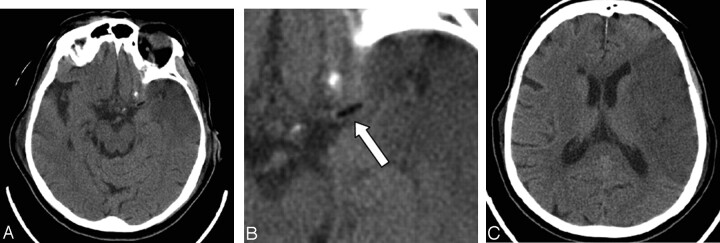
Fig 1.
A 78-year-old woman who had undergone a mitral valve replacement.
A–C, Axial images from the initial CT head scan obtained on the first postoperative day demonstrate an early left middle cerebral artery territory infarct. There is a fat attenuation filling defect (arrow, B) in the region of the proximal left middle cerebral artery trunk.
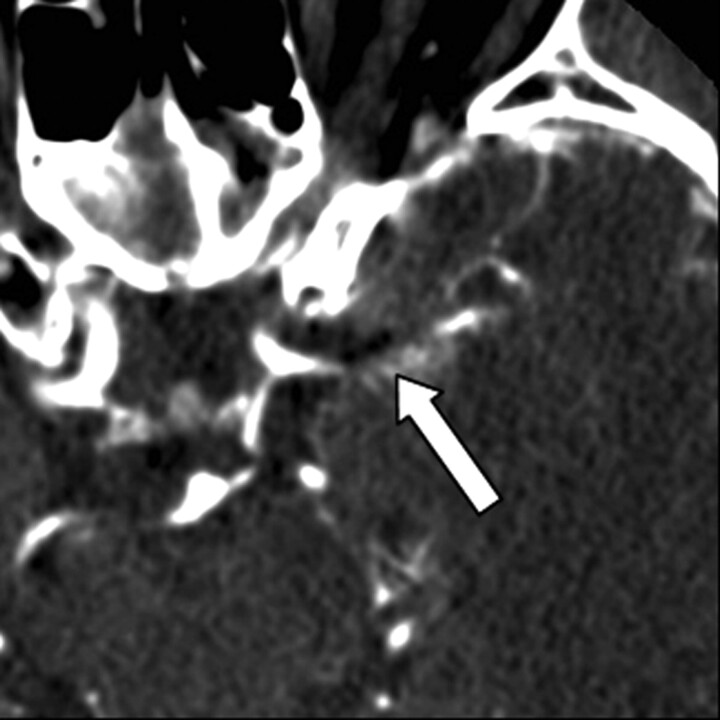
Fig 2.
CT angiography axial image obtained 13 days postoperatively confirms that the fat attenuation lesion (arrow) is within the proximal left middle cerebral artery trunk.
She remained in the cardiovascular intensive care unit with ventricular pacing for nearly 2 months following the operation. MR imaging was performed 49 days after her stroke, once the pacemaker was removed. MR imaging showed interval evolution of the large left middle cerebral artery infarct. The previously seen infarct edema had resolved. There was hemorrhage within the infarcted territory and in the ventricles, which had occurred in the interval since the prior CT scans but was not clinically symptomatic. Imaging through the left proximal middle cerebral artery, without and with fat saturation, showed remnants of the fat embolus within the M1 segment (Fig 3).
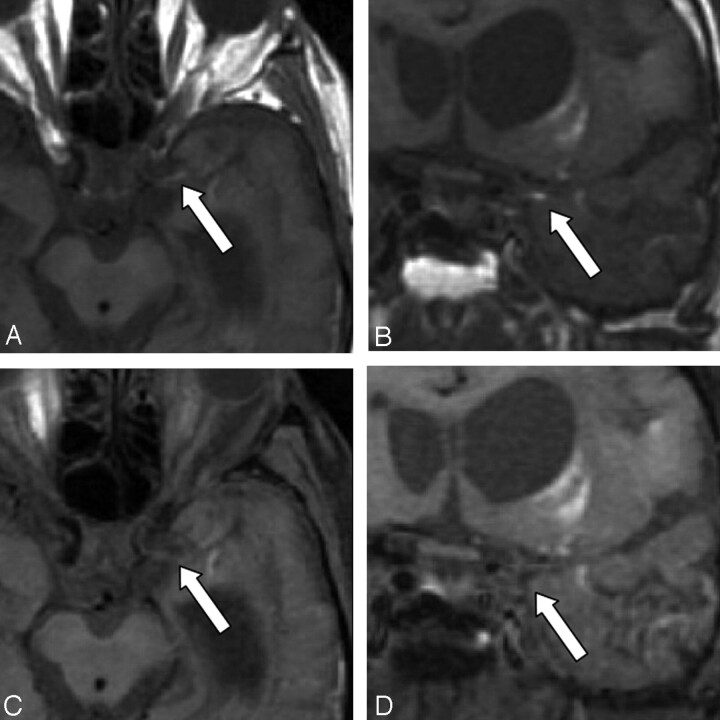
Fig 3.
Axial and coronal T1-weighted MR images obtained 49 days postoperatively without fat saturation (A,B) and with fat saturation (C,D). The images without fat saturation demonstrate the T1-hyperintense embolus (arrow) in the proximal left M1 trunk. After fat saturation, the T1 hyperintensity of the embolus is saturated (arrow), confirming its fatty composition. High-signal-intensity methemoglobin in the adjacent infarct is unchanged before and after fat saturation.
Discussion
Emboli to the intracranial circulation can originate from numerous sources. Emboli can originate in the heart, particularly in the setting of atrial fibrillation. Emboli commonly propagate from the carotid arteries as a result of stenosis or complicated atherosclerotic plaque. Thrombus can form at the site of a vessel dissection with subsequent embolization to the intracranial circulation. In these scenarios, the emboli are thrombotic in composition. Fat emboli to the intracranial circulation are uncommon.
Aside from mortality due to other causes, stroke is the most feared complication of cardiac surgery. The incidence of stroke after coronary artery bypass is 1.4%, whereas the risk of perioperative stroke for valve surgery is higher, quoted at 2.5% (11). Persistent atrial fibrillation is the most significant risk factor for stroke after mechanical mitral valve replacement (12).
Fat emboli that usually originate from long bone fractures are more commonly described in the trauma and orthopedic literature. The major clinical criteria for diagnosing fat embolism include respiratory distress and petechiae. Cerebral fat embolism has been described in patients with a venous-to-arterial shunt (13).
The typical fat emboli syndrome is generally thought to be a result of microglobules. The high-resolution chest CT findings of mild fat embolism are nonspecific, consisting of bilateral ground-glass opacities and thickening of the interlobular septa. Centrilobular nodular opacities are present in some patients (13). Therefore, the clinical situation is the most important determinant in diagnosing fat embolus (14, 15).
In our patient, the diagnosis of a fat embolus was suspected on the basis of the negative Hounsfield unit attenuation in the middle cerebral artery. Presumably the mitral valve replacement procedure resulted in dislodgement of a macroscopic portion of fat from the cardiac or surrounding tissue, which subsequently embolized to the left middle cerebral artery. Alternately, fat may have been dislodged during the sternotomy and paradoxically embolized to the brain through an intraoperative atrial defect. Fat containing emboli could also originate from fatty atherosclerotic plaque within the carotid artery or aortic arch. However, there was only minor atherosclerotic plaque in the proximal left internal carotid artery of this patient on CT angiography; therefore, a carotid artery source was excluded. Although the hyperdense middle cerebral artery sign has been widely described as a sign of thromboembolism, a hypodense middle cerebral artery sign associated with acute stroke from a fat embolus is not commonly known.
References
- 1.von Kummer R, Nolte PN, Schnittger H, Thron A, Ringelstein EB. Detectability of cerebral hemisphere ischaemic infarction by CT within 6 hours of stroke. Neuroradiology 1996;38:31–33 [DOI] [PubMed] [Google Scholar]
- 2.Gacs G, Fox AJ, Barnett HJM, Vinuela F. CT visualization of intracranial arterial thromboembolism. Stroke 1983;14:756–762 [DOI] [PubMed] [Google Scholar]
- 3.Pressman BD, Tourje EJ, Thompson JR. An early sign of ischemic infarction: increased density in a cerebral artery. AJNR Am J Neuroradiol 1987;8:645–648 [DOI] [PubMed] [Google Scholar]
- 4.Schuierer G, Huk W. The unilateral hyperdense middle cerebral artery: an early CT sign of embolism or thrombosis. Neuroradiology 1988;30:120–122 [DOI] [PubMed] [Google Scholar]
- 5.Bastianello S, Pierallini A, Colonnese C, et al. Hyperdense middle cerebral artery CT sign: comparison with angiography in the acute phase of ischemic supratentorial infarction. Neuroradiology 1991;33:207–211 [DOI] [PubMed] [Google Scholar]
- 6.Leys D, Pruvo JP, Godefroy O, Rondepierre PH, Leclerc X. Prevalence and significance of hyperdense middle cerebral artery in acute stroke. Stroke 1992;23:317–324 [DOI] [PubMed] [Google Scholar]
- 7.Tomsick T, Brott T, Barsan W, et al. Prognostic value of the hyperdense middle cerebral artery sign and stroke scale score before ultraearly thrombolytic therapy. AJNR Am J Neuroradiol 1996;17:79–85 [PMC free article] [PubMed] [Google Scholar]
- 8.von Kummer R, Meyding-Lamade U, Forsting M, et al. Sensitivity and prognostic value of early CT in occlusion of the middle cerebral artery trunk. AJNR Am J Neuroradiol 1994;15:9–15 [PMC free article] [PubMed] [Google Scholar]
- 9.Tomsick TA, Brott TG, Olinger CP, et al. Hyperdense middle cerebral artery: incidence and quantitative significance. Neuroradiology 1989;31:312–315 [DOI] [PubMed] [Google Scholar]
- 10.von Kummer R, Holle R, Gizyska U, et al. Interobserver agreement in assessing early CT signs of middle cerebral artery infarction. AJNR Am J Neuroradiol 1996;17:1743–1748 [PMC free article] [PubMed] [Google Scholar]
- 11.David TE. The Toronto Hospital Cardiac Surgical Program. In: Cheng DCH, David TE, eds. Perioperative care in cardiac anesthesia and surgery. Georgetown, TX: Landes Bioscience;1999;2 [Google Scholar]
- 12.Bando K, Kobayashi J, Hirata M, et al. Early and late stroke after mitral valve replacement with a mechanical prosthesis: risk factor analysis of a 24-year experience. J Thorac Cardiovasc Surg 2003;126:358–64 [DOI] [PubMed] [Google Scholar]
- 13.Malagari K, Economopoulos N, Stoupis C, et al. High-resolution CT findings in mild pulmonary fat embolism. Chest 2003;123:1196–1201 [DOI] [PubMed] [Google Scholar]
- 14.Georgopoulos D, Bouros D. Fat embolism syndrome: clinical examination is still the preferable diagnostic method. Chest 2003;123:982–983 [DOI] [PubMed] [Google Scholar]
- 15.Riding G, Daly K, Hutchinson S, Rao S, Lovell M, McCollum C. Paradoxical cerebral embolization: an explanation for fat embolism syndrome. J Bone Joint Surg Br 2004;86:95–98 [PubMed] [Google Scholar]