Abstract
BACKGROUND AND PURPOSE: The purpose of this study was to document the incidence and radiologic appearance of thromboembolic events during Guglielmi detachable coil (GDC) embolization for asymptomatic basilar artery (BA) bifurcation and BA-superior cerebellar artery (SCA) aneurysms by using diffusion-weighted (DW) MR imaging, with special emphasis on the evidence of thromboembolic events in vascular territories proximal from the treated aneurysm, which cause cerebellar infarction, and to discuss which step of the procedure (aneurysm or catheter manipulation) may play a role for most thromboembolic events.
METHODS: Since 1999, 38 asymptomatic BA bifurcation and BA-SCA aneurysms were treated with GDCs at the National Cardiovascular Center. DW studies were performed for 26 patients between 2 and 5 days after GDC embolizations. All DW images were reviewed by two radiologists for depiction of abnormalities. These findings were retrospectively evaluated with clinical and technical factors of thromboembolic events.
RESULTS: DW images showed new hyperintense lesions in 18 patients (69%), with seven (27%) incurring neurologic deteriorations. All symptomatic patients fully recovered by discharge. Fourteen (78%) of 18 patients showed new lesions proximal to the treated aneurysm; that is, in the cerebellar hemispheres. In three cases treated with the balloon-assisted technique, new hyperintense lesions were seen.
CONCLUSION: In our experience, most thromboembolic events related to the use of the GDC embolization may be caused by catheter manipulation, especially in the case of the balloon-assisted technique. Caution should be exercised in the handling of catheters. Furthermore, a softer and smaller caliber catheter and simple GDC technique should be considered.
The significant advances of endovascular embolization with Guglielmi detachable coils (GDCs; Target Therapeutics/Boston Scientific, Fremont, CA) contribute to the overall treatment of patients harboring cerebral aneurysms (1). Clinical thromboembolic complications have been reported to occur in a range of 1–31%; the most frequent and serious complications of this technique is thromboembolic events (2–4). Emboli could occur during diagnostic angiography, the introduction of catheter and coil placement, and during and after treatment (5–7). One transcranial Doppler study showed that delayed microemboli after endovascular embolization were detected in 31% of the patients in the middle cerebral artery (8). Such transcranial Doppler studies, however, could not discriminate upstream from downstream thromboembolic events of treated aneurysm. In addition, most studies reported thromboembolic events mainly caused by aneurysmal anatomic factors, including larger aneurysm diameter, protruding coils, and the use of the balloon-assisted technique (4, 9). It may be theoretically understood that aneurysmal rests and catheter manipulations will promote thromboembolic complication. At present, however, it is not known which step of the procedure may play a role for most thromboembolic events.
We reported previously that thromboembolic events occurred at a rate of 61% after GDC treatment by using diffusion-weighted (DW) MR imaging (4). The previous case series provided us with several valuable lessons from DW findings. In basilar artery (BA) bifurcation and BA-superior cerebellar artery (SCA) aneurysms, in association with vessels that supply the posterior circulation, most embolic lesions occurred in the distribution of the cerebellum and occipital convexties. The ability to measure these phenomena is critical for further refinement of the GDC technique. Clarifying which step of the procedure may be responsible for thromboembolic events and the frequency with which they occur will help practitioners determine the risks associated with different techniques.
The purpose of this study was to retrospectively evaluate the incidence of thromboembolic events with endosaccular embolization of BA bifurcation and BA-SCA aneurysms by using DW imaging, with special emphasis on cerebellar infarctions, and to discuss the possible pathogenetic mechanism underlying microemboli.
Methods
Between January 1999 and April 2002, we performed endosaccular embolization with GDCs for 38 patients with 30 asymptomatic BA bifurcations and eight BA-SCA aneurysms at the National Cardiovascular Center, Osaka, Japan. Cases in which DW imaging was performed after GDC treatment were selected. Cases in which patients refused MR study and those with parenchymal hemorrhage due to aneurysmal perforation or vessel rupture during the procedure were excluded (10). For the remaining cases, we analyzed the clinical and DW image findings.
The technique for the GDC procedures has been previously reported (4). Systemic heparinization was used to keep the activated clotting time at 2–2.5 times the baseline throughout the endovascular procedure. In the cases of wide-neck aneurysms (neck diameter ≥4 mm or the dome-neck ratio <1.5) or large aneurysms and some small-neck aneurysms, balloon-assisted techniques were performed to fix the GDCs in the sac of the aneurysm (11, 12). The results of the embolization were classified into complete occlusion (no filling of aneurysmal rests without neck remnant) or incomplete occlusion (small neck remnant or partial occlusion). In all cases, systemic heparinization was not reversed, and the patients were transferred to a neurosurgical intensive care unit and received intravenous infusion of antithrombin agents (Argatroban Abbott Laboratories, North Chicago, Illinois, U.S.A.) for 2 days and oral antiplatelet agents (ticlopidine hydrochloride or aspirin) for the following 3 months postoperatively. After June, 2001, all cases received oral antiplatelet agents for 1 week preoperatively and were treated with general anesthesia.
MR imaging was scheduled at 2–5 days after the GDC procedures. The imaging was performed on a 1.5-T system (Magnetom Vision, Siemens, Erlangen, Germany). The details of the MR technique in this study were reported previously (4). All MR images were reviewed by either of two neuroradiologists (N.Y., S.I.), both of whom were unaware of clinical information. If diffusion abnormalities were detected, the incidence and distribution of new hyperintense lesions were assessed.
Cerebellar infarction was classified by using previously published anatomic templates (13), and those that did not correspond to an arterial territory as border zone infarcts defined by Amarenco et al (14).
Results
Twenty-six of 38 patients underwent postprocedural DW imaging and were enrolled in the study (BA bifurcation aneurysm, 21; BA-SCA aneurysm, five). The remaining 12 patients were excluded because of patient refusal (four patients) or the presence of another ruptured aneurysm before treatment (six patients) or parenchymal hemorrhage due to aneurysmal perforation (one) or vessel rupture (one) during the procedure. After June 2001, five patients received oral antiplatelet agents for 1 week preoperatively and were treated with general anesthesia and enrolled in this study. Eight patients were male and 18 were female. The patients’ ages ranged from 38 to 77 years (mean age, 60 years). Twenty-one aneurysms were small (diameter ≦10 mm) and five large (diameter 10–25 mm). Thirteen aneurysms had small necks (neck diameter <4 mm), and 13 had wide necks (neck diameter ≥4mm). Three aneurysms (12%) were treated with the balloon-assisted technique. Fifteen (58%) aneurysms were completely occluded. No iatrogenic vertebral artery occlusion, dissection, or stenosis was encountered. There were seven (27%) symptomatic complications. Two patients had minimal neurologic deficits (slight motor weakness, disorientation) during the intervention and fully recovered by the end of the procedure as a result of volume-expansion therapies. Neurologic deficits in the remaining five patients persisted after the procedure; three patients (visual field cut: two, ataxia) showed complete recovery within a few days, and two (ataxia, visual field cut) during the following week.
In 18 (69%) of 26 procedures, new hyperintense lesions were detected. The findings in these 18 patients are summarized in the Table 1. Seven of the 18 patients with positive DW image findings demonstrated neurologic complications. Overall, seven (27%) symptomatic and 11 (42%) silent thromboembolic events occurred after 26 procedures. The numbers of new lesions were one to three in 11 (42%) patients and greater than three in seven (27%). New hyperintense lesions located in the vascular territory downstream from the treated aneurysms were detected in four (15%) patients: two (8%) of these aneurysms were upstream and 12 (46%) were up- and downstream. Fourteen (54%) patients showed new lesions in the cerebellar hemispheres: two (8%) were territorial infarction and the remaining 12 (46%) were nonterritorial small infarctions. In 15 (58%) patients, such abnormalities were located in the cerebral convexties, 14 (54%) were located in occipital convexties, five (19%) were in the thalamus, and two (8%) had new lesions in the vascular distributions remote from the treated aneurysm. In the three cases treated with the balloon-assisted technique, new hyperintense lesions were shown in all cases.
Clinical, radiologic characteristics and GDC treatment in 18 patients with thromboembolic complications
| Case* | Age (y)/Sex | An. | Dome/Neck (mm) | Options | Angiographic Results | Hyperintense Lesion |
Presenting Symptom (Duration) | ||
|---|---|---|---|---|---|---|---|---|---|
| Number | Location | Patterns of CI | |||||||
| 1 | 52/M | BB | 12/4 | Complete | 2 | O | None | ||
| 2 | 59/M | BB | 6/4 | Incomplete | Multiple | O, C, T | Borderzone | Visual field cut (7 days) | |
| 3 | 66/F | BB | 8/4.5 | BAT | Incomplete | Multiple | C, B | Territorial | Cerebellar ataxia (3 days) |
| 4 | 51/F | BB | 10/5 | Incomplete | Multiple | C | Borderzone | Slight lt-hemiparesis (DP) | |
| 5 | 65/F | BB | 12/3 | Incomplete | 4 | O, C | Borderzone | Cerebellar ataxia (7 days) | |
| 6 | 73/F | BB | 9/5 | Incomplete | Multiple | O, C, T | Territorial | Disorientation (DP) | |
| 7 | 65/F | BB | 15/5 | Incomplete | Multiple | O, C, F, P | Borderzone | None | |
| 8 | 73/F | BB | 8/4 | BAT | Incomplete | 3 | O, C | Borderzone | Visual field cut (One day) |
| 9 | 56/M | BB | 4/3 | Complete | 3 | O, C | Borderzone | None | |
| 10 | 64/F | BB | 4/3 | Incomplete | 2 | O, T | Visual field cut (One day) | ||
| 11 | 68/F | BB | 15/5 | Complete | 3 | O, C | Borderzone | None | |
| 12 | 55/M | BB | 6/3 | Complete | 3 | O, C | Borderzone | None | |
| 13 | 65/F | BB | 6/2 | Complete | Multiple | O, C | Borderzone | None | |
| 14 | 54/M | BB | 8/5 | BAT, G | Complete | 1 | F | None | |
| 15 | 53/M | BB | 9/4 | G | Incomplete | 2 | O, T | None | |
| 16 | 38/M | BS | 22/4 | G | Incomplete | 3 | O, C | Borderzone | None |
| 17 | 60/F | BB | 4/3 | G | Complete | 3 | O, C, B | Borderzone | None |
| 18 | 53/F | BS | 5/3 | G | Incomplete | 2 | C, T | Borderzone | None |
Note.—AN indicates aneurysm; BS, basilar artery-superior cerebellar artery aneurysm; BB, basilar bifurcation aneurysm; rt, right; lt, left; VA, vertebral artery; G, general anesthesia; BAT, balloon-assisted technique; CI, cerebellar infarction; O, occipital convexty; C, cerebellum; F, frontal convexty; P, parietal convexty; T, thalamus; B, brain stem; DP, during procedure;
, Case 1–13: Reported previously (4)
Discussion
Herein we report on thromboembolic events associated with GDC treatment for cerebral aneurysm. Our results of GDC treatment provide us with precautions of this technique for avoidance of thromboembolic complication.
Thromboembolic factors occurred proximal to treated aneurysms related to navigation of catheters, where coils and occlusion balloons are responsible for various events, including vessel dissection, vasospasm, and thrombus formation. Small blood clots or arterosclerotic plaques were scraped off the vessel wall or by catheter manipulation. In this study, 78% of patients with hyperintense lesions had cerebellar infarctions. This result suggested that most the emboli were connected to intravascular instruments.
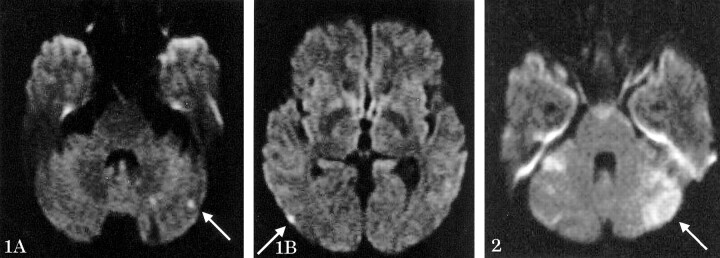
The location of the lesion depends both on the flow patterns in the patient’s brain and other unresolved factors. Canaple et al (15) reported that the most frequent type of multiple cerebellar infarctions involved the posterior inferior cerebral artery (PICA) plus SCA territory, followed by PICA plus anterior inferior cerebral artery plus SCA territory infarctions, and half of the patients presented other infarctions in the posterior circulation. In the present study, most infarctions were located at the boundary region between two main arterial territories, so-called junctional infarctions (Fig 1). There was a common occurrence of very small multiple cerebellar infarcts, whose small territorial infarcts may be end zone infarcts from the involvement of small distal arteries (15). Most of the present patients with cerebellar infarctions did not develop a focal neurologic deficit, which suggested that in most cases microemboli do not result in deficits. In cases in which infarctions enlarge, however, results in more extensive focal deficits (Fig 2).
Fig 1.
Case 9, a silent embolism in a 56-year-old man with basilar bifurcation aneurysm. A DW MR image shows small border zone infarcts in the cerebellum (1A) and occipital convexity (1B) (arrows).
Fig 2.
Case 6, a representive symptomatic embolism, in a 73-year-old woman with basilar bifurcation aneurysm. A DW MR image shows large territorial infarcts of the cerebellum (arrow).
Conclusion
The authors reported that thromboembolic events related to the use of GDC embolization are relatively common, especially in large aneurysms or in cases associated with the balloon-assisted technique (4). In addition, the present detailed analysis supported previous results and suggested that most thromboembolic events occurred during the catheter manipulation. Caution should be exercised in the handling of catheters. Furthermore, a softer and smaller caliber catheter and simple GDC technique should be considered.
References
- 1.International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. Lancet 2002;360:1267–1274 [DOI] [PubMed] [Google Scholar]
- 2.Vinuela F, Duckwiler G, Mawad M. Guglielmi detachable coil embolization of acute intracranial aneurysm: perioperative anatomical and clinical outcome in 403 patients. J Neurosurg 1997;86:475–482 [DOI] [PubMed] [Google Scholar]
- 3.Murayama Y, Vinuela F, Duckwiler GR, et al. Embolization of incidental cerebral aneurysms by using the Guglielmi detachable coil system. J Neurosurg 1999;90:207–214 [DOI] [PubMed] [Google Scholar]
- 4.Soeda A, Sakai N, Sakai H, et al. Thromboembolic events associated with Guglielmi detachable coil embolization of asymptomatic cerebral aneurysms: evaluation of 66 consecutive cases with use of diffusion-weighted MR imaging. AJNR Am J Neuroradiol 2003;24:127–132 [PMC free article] [PubMed] [Google Scholar]
- 5.Bendszus M, Koltzenburg M, Burger R, et al. Silent embolism in diagnostic cerebral angiography and neurointerventional procedures: a prospective study. Lancet 1999;354:1594–1597 [DOI] [PubMed] [Google Scholar]
- 6.Rordorf G, Bellon RJ, Budzik RF, et al. Silent thromboembolic events associated with the treatment of unruptured cerebral aneurysms by use of Guglielmi detachable coils: prospective study applying diffusion-weighted imaging. AJNR Am J Neuroradiol 2001;22:5–10 [PMC free article] [PubMed] [Google Scholar]
- 7.Sakai H, Sakai N, Higashi T, et al. Embolic complications associated with neurovascular intervention: prospective evaluation by use of diffusion-weighted MR imaging [in Japanese]. No Shinkei Geka 2002;30:43–49 [PubMed] [Google Scholar]
- 8.Klotzsch C, Nahser HC, Henkes H, et al. Detection of microemboli distal to cerebral aneurysms before and after therapeutic embolization. AJNR Am J Neuroradiol 1998;19:1315–1318 [PMC free article] [PubMed] [Google Scholar]
- 9.Derdeyn CP, CrossIII DT, Moran CJ, et al. Postprocedure ischemic events after treatment of intracranial aneurysms with Guglielmi detachable coils. J Neurosurg 2002;96:837–843 [DOI] [PubMed] [Google Scholar]
- 10.Ebisu T, Tanaka C, Umeda M, et al. Hemorrhagic and nonhemorrhagic stroke: diagnosis with diffusion-weighted and T2-weighted echo-planer MR imaging. Radiology 1997;203:823–828 [DOI] [PubMed] [Google Scholar]
- 11.Moret J, Cognard C, Weill A, et al. The “remodeling technique” in the treatment of wide neck intracranial aneurysms. Intervent Neuroradiol 1997;3:21–35 [DOI] [PubMed] [Google Scholar]
- 12.Lefkowitz MA, Gobin YP, Akiba Y, et al. Balloon-assisted Guglielmi detachable coiling of wide-necked aneurysms. Part II. Clinical results. Neurosurgery 1999;45:531–538 [DOI] [PubMed] [Google Scholar]
- 13.Amarenco P. The spectrum of cerebellar infarction. Neurology 1991;41:973–979 [DOI] [PubMed] [Google Scholar]
- 14.Amarenco P, Kase CS, Rosengart A, et al. Very small (border zone) cerebellar infarcts: distribution, causes, mechanisms and clinical features. Brain 1993;116:161–186 [DOI] [PubMed] [Google Scholar]
- 15.Canaple S, Bogousslavsky J. Multiple large and small cerebellar infarcts. J Neurol Neurosurg Psychiatry 1999;66:739–745 [DOI] [PMC free article] [PubMed] [Google Scholar]