Abstract
Summary: Subacute granulomatous thyroiditis is an uncommon disease that occurs most often in women in their second to fifth decades of life. This disease usually presents with thyroid tenderness, a low grade fever, and occasional dysphagia. The disease resolves spontaneously, usually without thyroid function abnormalities. We herein present the CT and MR imaging findings of two cases of subacute granulomatous thyroiditis.
Subacute granulomatous thyroiditis (nonsuppurative thyroiditis, subacute thyroiditis, or de Quervain thyroiditis) is a self-limited inflammatory disease of the thyroid gland that most often occurs secondary to a viral infection (1, 2). Although a number of articles have described the sonographic features associated with this disease (3–5), very few reports describe the CT and MR imaging features associated with subacute granulomatous thyroiditis (6, 7). Our purpose was to present the CT and MR imaging features of subacute thyroiditis. The radionuclide iodine scintigraphic findings of one case are also presented.
Case Reports
Patient 1
A 35-year-old woman presented with a 1-week history of low grade fever, mild dysphagia, and anterior neck pain. Clinical examination revealed marked tenderness in the anterior neck bilaterally. Laboratory evaluation showed an elevatederythrocyte sedimentation rate and mild leucocytosis. Mild elevation of T3 (190 ng/dL) and T4 (as thyroxine, 13.5 mcg/dL) values were noted. A radionuclide study showed diffusely decreased radioiodine uptake in the thyroid (Fig 1). CT showed the thyroid gland to have a diffusely decreased attenuation on the unenhanced scans (Figs 2 and 3), with only moderate enhancement on the contrast-enhanced scans (Fig 4). MR imaging of the neck was subsequently performed. The thyroid gland showed a mild increase in signal intensity on T1-weighted MR images and a more pronounced increase in signal intensity on T2-weighted MR images (Fig 5). No focal lesion or neck lymphadenopathy was observed, and a diagnosis of subacute thyroiditis was made. The case was managed conservatively with analgesics and steroids. The patient achieved complete recovery and euthyroidism by 2 months.
Fig 1.

Patient 1. Iodine-131 radionuclide scan shows virtually no uptake of radioactive iodine by the thyroid gland.
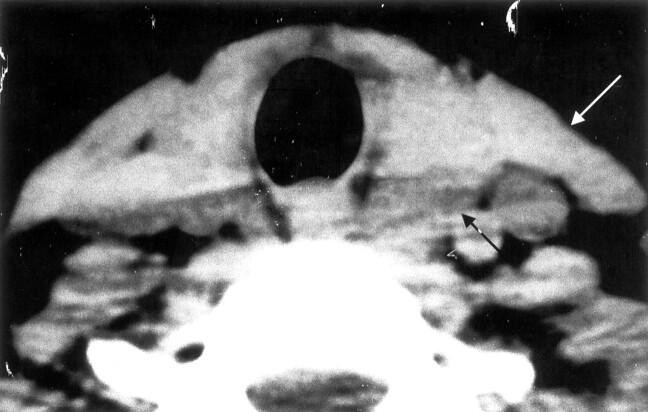
Fig 2.
Patient 1. Unenhanced axial CT scan shows diffuse decrease in the attenuation of the thyroid gland (black arrow), which is isoattenuated to the muscle. White arrow indicates the sternocleidomastoid muscle.
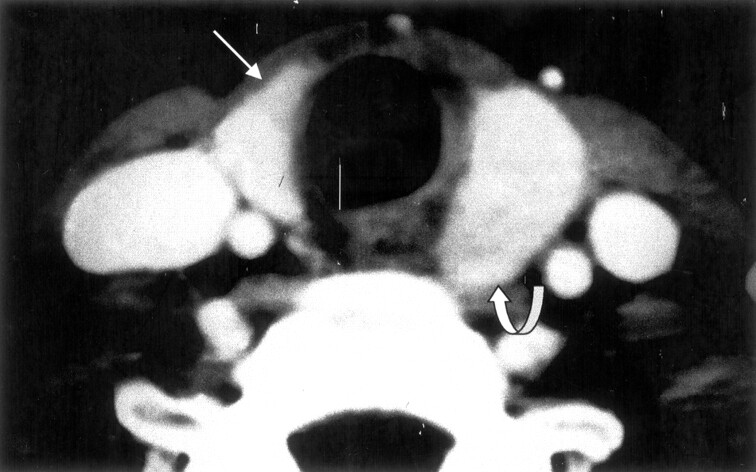
Fig 3.
Patient 1. Contrast-enhanced axial CT scan shows slight enlargement of the left thyroid lobe. Decreased attenuation can be seen in the posterior portion of the left thyroid lobe (curved arrow), and slightly decreased attenuation can be seen anteriorly in the right thyroid lobe (straight arrow).
Fig 4.
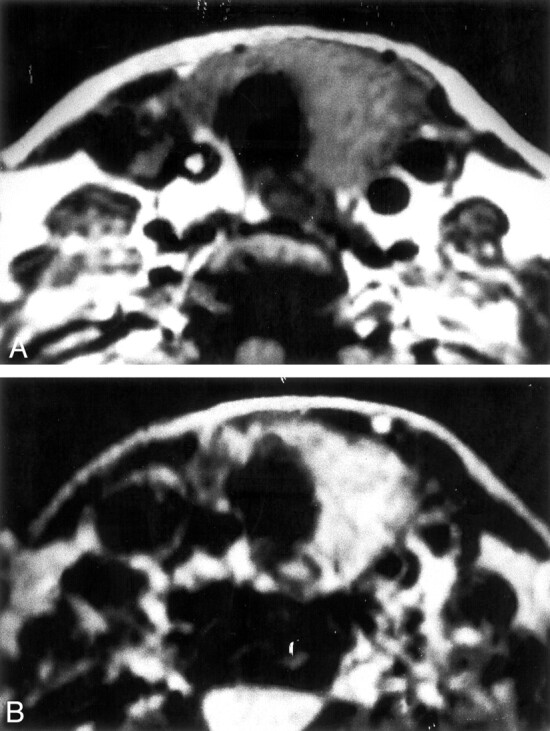
Patient 1. Axial MR images of the neck.
A, T1-weighted image shows mild hyperintensity in the thyroid gland.
B, T2-weighted image shows a more pronounced hyperintensity, compared with muscle, in the thyroid gland.
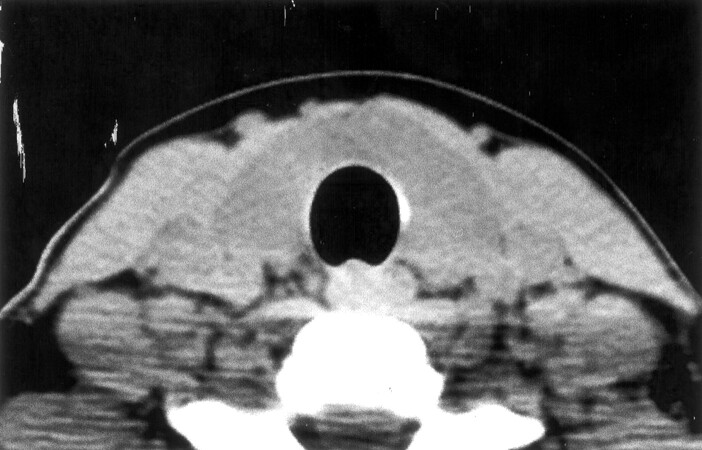
Fig 5.
Patient 2. CT scan shows thyroid gland to have diffusely decreased attenuation.
Patient 2
A 29-year-old woman presented with a 2-week history of anterior neck pain and low grade fever. On palpation, the thyroid gland was tender and diffusely swollen. However, there was no evidence of a focal mass. The patient had no other significant medical or surgical history. Laboratory studies showed a normal hemoglobin level (13.8 g/dL) and a normal WBC count (5500/mm3). Sonography showed a diffusely enlarged predominantly hypoechoic thyroid gland. Unenhanced CT of the neck showed a homogeneously enlarged thyroid gland with attenuation lower than that of muscle (Fig 4). Thyroid function tests showed reduced T3 (48 ng/dL) and T4 (as thyroxine, 3 mcg/dL) levels. A diagnosis of subacute thyroiditis was made. The patient was treated with steroids and recovered completely within 4 weeks.
Patient 3
A 31-year-old woman presented with a 2-day history of right anterior neck swelling and tenderness. The fullness was painful to palpation. No other physical findings were present, and her medical history was not significant. Laboratory evaluation showed a mildly elevated erythrocyte sedimentation rate and mild leucocytosis. Thyroid function tests showed reduced T3 (60 ng/dL) and T4 (as thyroxine, 8 mcg/dL) levels. Contrast-enhanced CT showed an enlarged right thyroid lobe with decreased attenuation (Fig 6). A diagnosis of subacute thyroiditis was made, and the patient was treated with antibiotics and steroids. She became symptom free within 2 weeks and achieved euthyroidism by 2 months.
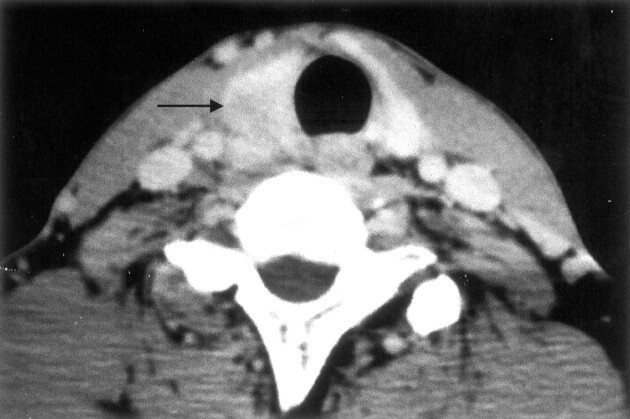
Fig 6.
Contrast-enhanced CT scan shows enlarged right thyroid lobe with decreased attenuation (arrow).
Discussion
Thyroiditis can occur in acute, subacute, and chronic forms. Of the diseases that have a shorter clinical course, one must consider acute thyroiditis, subacute granulomatous thyroiditis, and multifocal granulomatous thyroiditis.
Acute thyroiditis is a rare infectious disease that often results from infection by pyogenic bacteria, although it has been caused by fungi, parasites, or viruses. The disease is most often encountered in immunosuppressed persons, in whom there is a noted association with Pneumocystis carinii infection (8, 9). Acute thyroiditis can also occur in otherwise healthy patients after trauma. Preexisting thyroid disease, particularly nodular goiter, is reported to be present in 50% of adult patients. A high association with pyriform sinus fistulae exists, as found in fourth branchial cysts. Patients with acute thyroiditis present with an acute onset of anterior neck pain and fever. These patients usually have euthyroidism, although there may be a transient elevation of the thyroid hormone levels. Treatment is with antibiotics and, if indicated, surgical drainage. Permanent sequelae are rare (8, 9).
Subacute granulomatous thyroiditis, also known as nonsuppurative thyroiditis, subacute thyroiditis, or de Quervain thyroiditis, is an uncommon disease that represents 0.16% to 0.36% of all thyroid disorders (10). It most commonly occurs in female persons during the second to fifth decades of life. There is a possible genetic predisposition as there is an association with human leukocyte antigen Bw35. This disease is generally thought to be the result of a viral infection, as it is often preceded by an upper respiratory inflammatory viral illness (1, 2). Rising antibody titers to viral antigens such as mumps, measles, rhinoviruses, adenovirus, and coxsackievirus have been noted, and this disease occurs more often during the summer and fall months.
Patients present with systemic findings such as weakness, fever, and an elevated erythrocyte sedimentation rate. Typically, a sudden onset of unilateral anterior neck pain occurs and may radiate to the ear, mandible, or upper chest. There usually is thyroid tenderness and occasional dysphagia. The thyroid tenderness results from a stretching of the thyroid capsule due to the underlying inflammatory disease process. Release of T3 and T4 due to damage of the follicular epithelium may induce transient hyperthyroidism. A subsequent hypothyroid phase may occur, and it may last for several months. Rarely, permanent hypothyroidism may occur. Pathologically, early in the process, disruption of the thyroid follicles occurs, with subsequent release of colloid into the stroma. This results in an inflammatory response dominated initially by neutrophils and microabscess formation and subsequently by a granulomatous process with lymphocytes, histiocytes, and multinucleated giant cells surrounding and engulfing deposits of colloid. Ultimately, fibrosis occurs, especially in areas of severe tissue destruction. Generally, treatment consists of aspirin and nonsteroidal anti-inflammatory agents. Steroids may also be administered until symptoms disappear (8, 9).
The pathologic differential diagnosis includes multifocal granulomatous thyroiditis, sarcoidosis, and tuberculosis. Granulomatous thyroiditis secondary to infection by Mycobacteria is rare and usually occurs as a result of hematogenous dissemination or by direct extension from an adjacent lymph node. Thyroid involvement by sarcoidosis is rare (11, 12). Larger lesions, particularly in fibrotic phases, may simulate carcinoma grossly. Clinically, the differential diagnosis also includes acute hemorrhage into a thyroid adenoma, painful Graves disease, and possibly anaplastic carcinoma (13).
On images, subacute granulomatous thyroiditis (de Quervains thyroiditis) shows a low uptake of iodine on radionuclide scintigraphy (radioiodine uptake), probably because of follicular cell destruction (Fig 1). Considering that the administration of iodinated contrast material before measuring radioiodine uptake has been shown to falsely result in a low iodine uptake, contrast-enhanced CT scans should be obtained after radioiodine uptake is studied. On CT scans, the normal thyroid gland has a high attenuation (80–100 HU) because the normal thyroid gland concentrates iodine almost 100 times more than does the serum (6). In both our cases, we observed the diffusely swollen thyroid glands to have a low attenuation corresponding to 45 HU (Figs 2 and 3). This can be explained on the basis of follicular cell destruction and loss of iodine concentration within the thyroid gland. After the administration of contrast material, the normal thyroid gland has marked enhancement, and this is attributed to its rich vascularity. We observed moderate enhancement of the thyroid gland on the contrast-enhanced scans, suggesting the diffuse inflammatory nature of the disease process (Fig 4).
On MR images, the normal thyroid gland shows homogeneous T1-weighted signal intensity that is slightly greater than that of skeletal muscle. On T2-weighted sequences, the normal thyroid gland is hyperintense to the neck muscles; after the administration of contrast material, the normal gland enhances diffusely and homogeneously. Otsuka et al (7) reported the cases of three patients with subacute thyroiditis. They found the thyroid glands to have slightly irregular margins and a higher than normal T1-weighted signal intensity. They also noted a much higher than normal T2-weighted signal intensity. Our patient 1, who underwent MR imaging, showed mild increased signal intensity of the thyroid gland on the T1-weighted images and more pronounced increase in the signal intensity on the T2-weighted images, consistent with the diffuse inflammatory nature of subacute granulomatous thyroiditis (Fig 5).
Multifocal granulomatous thyroiditis, or palpation thyroiditis, refers to changes found in the thyroid gland secondary to minor trauma, most often the result of palpation. As such, it occurs almost exclusively in patients undergoing neck surgery for thyroid disease. Histologically, there is a loss of follicular epithelium and the presence of mononuclear histiocytes, lymphocytes, plasma cells, and multinucleated giant cells. Focal hemorrhage and hemosiderin deposition may occur. The lesions most often regress (6, 7).
Conclusion
Subacute thyroiditis is an uncommon disease that should be considered in the differential diagnosis of acute anterior neck pain. In this clinical setting, CT and MR imaging can help exclude other diseases and speed appropriate therapy to relieve symptoms.
References
- 1.LiVolsi VA. The thyroid and parathyroid. In: Sternberg SS, ed. Diagnostic Surgical Pathology. 2nd ed. New York: Lippincott Williams & Wilkins;1994. :523–560
- 2.De Lellis RA. The endocrine system. In: Cotram R, Kumar V, Robbins SL, eds. Robbins Pathologic Basis of Disease. 4th ed. Philadelphia: Saunders;1989. :1214–1242
- 3.Bennedbaek FN, Hegedus L. The value of ultrasonography in the diagnosis and follow-up of subacute thyroiditis. Thyroid 1997;7:45–50 [DOI] [PubMed] [Google Scholar]
- 4.Brander A. Ultrasound appearances in de Quervain’s subacute thyroiditis with long-term follow-up. J Intern Med 1992;232:321–325 [DOI] [PubMed] [Google Scholar]
- 5.Takashima S, Sone S, Horii A, Honjho Y, Yoshida J. Subacute thyroiditis in Hashimoto’s thyroiditis which mimicked primary thyroid lymphoma. J Clin Ultrasound 1997;25:279–281 [DOI] [PubMed] [Google Scholar]
- 6.Loevner LA. Imaging of the thyroid gland. Semin Ultrasound CT MR 1996;17:539–562 [DOI] [PubMed] [Google Scholar]
- 7.Otsuka N, Nagai K, Maurita K, et al. Magnetic resonance imaging of subacute thyroiditis. Radiat Med 1994;12:273–276 [PubMed] [Google Scholar]
- 8.DeLellis RA, Guiter G, Weinstein BJ. Pathology of the thyroid and parathyroid glands. In: Gnepp DR, ed. Diagnostic Surgical Pathology of the Head and Neck. Philadelphia: WB Saunders;2001. :441–442
- 9.LiVolsi VA. Pathology of the thyroid gland. In: Barnes L, ed. Surgical Pathology of the Head and Neck. 2nd ed. vol 3. New York: Marcel Dekker, Inc.;2001. :1682–1683
- 10.Meachim G, Young MH. de Quervain’s subacute granulomatous thyroiditis: histologic identification and incidence. J Clin Pathol 1963;16:189–199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sachs MK, Dickinson G, Amazon K. Tuberculous adenitis of the thyroid mimicking subacute thyroiditis. Am J Med 1988;85:573–575 [DOI] [PubMed] [Google Scholar]
- 12.Karlish AJ, MacGregor GA. Sarcoidosis, thyroiditis, and Addison’s disease. Lancet 1970;2:230–333 [DOI] [PubMed] [Google Scholar]
- 13.Larsen PR. The thyroid. In: Wingaarden JB, Smith LH, Bennett JC, eds. Cecil Textbook of Medicine. 19th ed. Philadelphia: W.B. Saunders Co.;1992;1248–1271