Abstract
Summary: Patients who have undergone thyroidectomy may have recurrent laryngeal nerve injury; until recently, Teflon injection was commonly used for vocal cord medialization. We present a case of a patient who underwent thyroidectomy who had significantly increased and unilateral 18F-fluorodeoxyglucose uptake in the neck, which was found to be localized to the left vocal cord by use of combined positron emission tomography (PET) and CT, presumably because of a Teflon-induced granuloma. Knowledge of this potential source of false-positive PET interpretation because of its inability to precisely localize neoplastic lesions, and the use of combined PET and CT imaging, may allow precise diagnosis and prevention of unnecessary interventions.
Positron emission tomography (PET) with 18F-fluorodeoxyglucose (FDG) is a powerful tool in the diagnosis, staging, and therapeutic monitoring of extracranial head and neck cancers (1, 2). The use of PET for thyroid cancer recurrence has shown promise in patients with known differentiated thyroid cancer who have negative findings with whole-body 131I scintigraphy and elevated thyroglobulin levels (3–5). The limited anatomic localization of PET led to the development of a combined PET and CT tomograph, which can precisely localize neoplastic lesions and prevent false-positive interpretations of non-neoplastic disease (6). Zimmer et al (7) conclude that combined PET and CT imaging is valuable in the detection of thyroid cancer recurrence.
Typically, patients with thyroid cancer undergo total thyroidectomy. Laryngeal nerve injury with vocal cord paralysis is a well-known complication of this procedure. Thyroplasties are surgical techniques used to medialize the true vocal cord and improve hoarseness by implanting silastic, fat, or Teflon under the cord. Teflon (polytetrafluoroethylene) injections have recently fallen out of favor because of a well-documented propensity to cause reactive granulomas. We discuss a patient with a history of thyroid cancer who had significantly increased and unilateral FDG uptake in the larynx secondary to Teflon thyroplasty.
Case Report
A 77-year-old man with a history of well-differentiated follicular carcinoma of the thyroid was referred to the PET facility of the University of Pittsburgh Medical Center for evaluation. Six and a half years previously, he had undergone total thyroidectomy. Postoperatively, he had left recurrent laryngeal nerve paralysis, for which he underwent Teflon injection into the paralyzed vocal cord. He received standard radioactive iodine thyroid ablation therapy postoperatively and 1 year after surgery. He was followed up with 131I scintigraphy yearly and serum thyroglobulin levels five times a year. Radiation therapy was repeated 4 years and 5 years after surgery on the basis of elevated thyroglobulin levels. Six months before the PET and CT imaging was performed, when the patient was not receiving Synthroid, findings of repeat 131I scintigraphy were negative, thyroid-stimulating hormone level exceeded 150 ìU/mL, and thyroglobulin level was 97 ng/mL. Although the thyroglobulin had decreased after radiation therapy, it had risen again to 22.5 ng/mL within 6 months.
Written informed consent was obtained from the patient for participation in a research protocol involving a prototype combined PET and CT device (CTI PET Systems, Knoxville, TN). Whole-body PET scan and helical CT imaging of the neck and chest were performed approximately 1 hour after 6.6-mCi IV injection of FDG. This study showed a marked focal area of increased metabolic activity in the anterior neck (Fig 1) that was localized to the left vocal cord by use of combined PET and CT imaging (Fig 2). The CT portion of the examination revealed an amorphous focus of high attenuation within a medialized left vocal cord (Fig 2). There was also a compression deformity of a lower thoracic vertebral body, which did not appear to show significant FDG uptake. This deformity, as well as the high attenuation in his larynx, had appeared on previous CT scans.
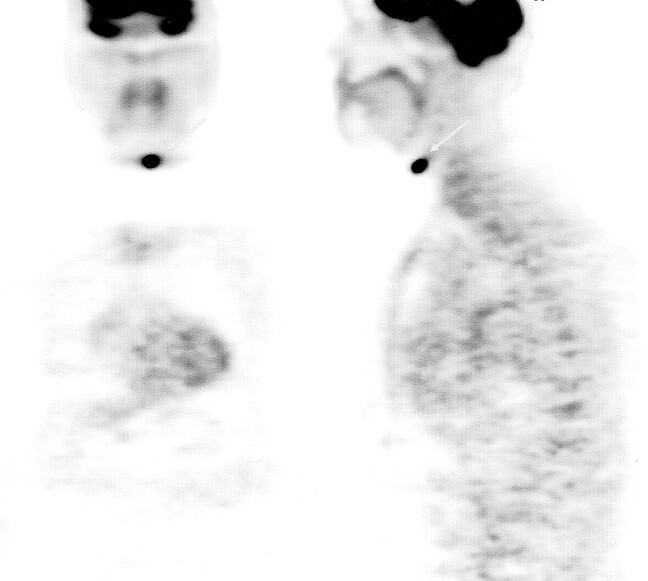
Fig 1.
Coronal (left) and sagittal (right) views acquired with PET. Increased FDG uptake just left of midline in the anterior neck (arrows) is shown.
Fig 2.
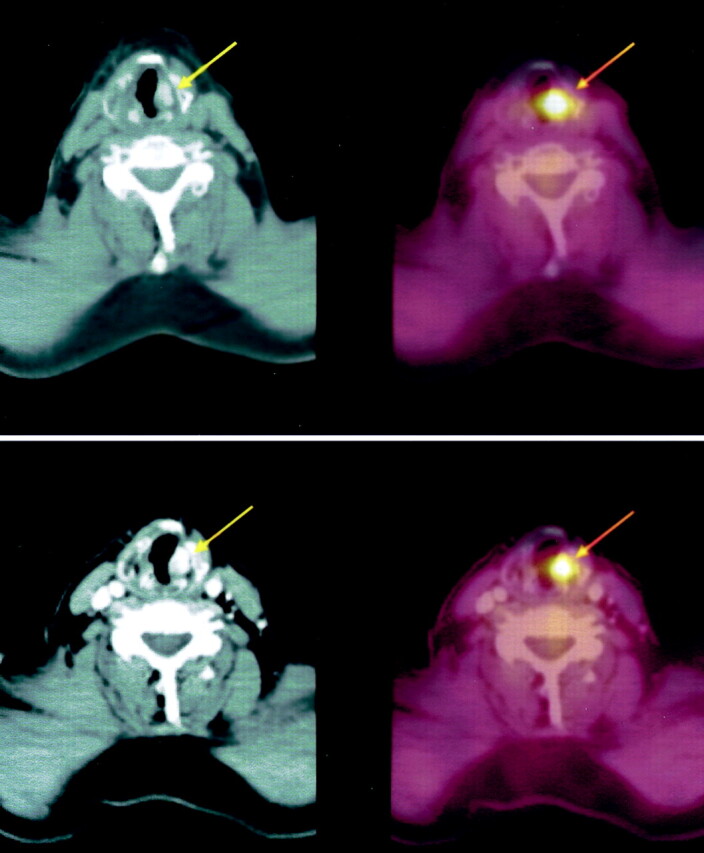
Top left, Initial CT image of the neck shows an amorphous area of high attenuation in the left medialized vocal cord (arrow). Top right corresponds to the area of increased FDG uptake (arrow) shown by combined PET and CT. Bottom left shows CT findings acquired 6 months later; no change in high attenuation is noted. Bottom right shows combind CT and PET findings; no change in FDG uptake (arrow) is noted.
Approximately 2 weeks after the PET and CT study, fiberoptic laryngoscopy revealed a paralyzed left vocal cord with good approximation of the cords on phonation. There were no areas suspicious for malignancy. Six months later, a repeat examination by use of a commercial PET and CT system (CPS Innovations, Knoxville, TN) after IV injection of 10.7-mCi FDG showed stability of the marked FDG uptake and the high attenuation in the left vocal cord; however, a source of thyroglobulin production was not identified, and the patient’s thyroglobulin rose to 36 ng/mL 1 year after the original PET and CT study was performed.
Discussion
We present a case of a patient with thyroid cancer who underwent thyroidectomy and had a stable, marked focus of FDG uptake in his left vocal cord, presumably because of a Teflon-induced granuloma. Although follicular cell thyroid carcinoma is generally a benign disease, 5–20% of patients have local or regional recurrences, and 10–15% have distant metastases (8). Evidence supports the utility of FDG-PET in detecting thyroid cancer recurrence; however, the radiologist must be aware of potential false-positive PET interpretations in these patients. FDG is variably taken up by a variety of inflammatory tissues, including atherosclerotic plaques (9), abscesses (10), fungal infections (11), and granulomas (12). Zhuang et al (13) report that dual-time-point FDG-PET may be useful in distinguishing malignant from benign lesions; however, this technique is not part of the standard practice. In our case, the use of combined PET and CT imaging allowed us to precisely localize and explain the area of increased FDG uptake. Although this finding was not histologically confirmed, we think that Teflon-induced granuloma is the diagnosis because of the stability of FDG uptake over a 6-month period, the stability of the area of increased attenuation on CT images acquired over several years, and the lack of findings at fiberoptic laryngoscopy.
Permanent vocal fold paralysis secondary to recurrent laryngeal nerve injury occurs in approximately 1% of patients who undergo thyroidectomy (14). Symptoms include hoarseness, decreased vocal volume, and decreased range of pitch. Vocal fold medialization adducts the glottic folds, thus improving phonation and reducing complications such as aspiration pneumonia. Surgical techniques to medialize the vocal cord (thyroplasty) include implantation of silastic and direct injection of Teflon, fat, or Gelfoam. Teflon has been widely used for vocal cord medialization since the 1960s; however, its use has declined because of the rate of complications related to improper injection, overinjection, and the formation of granulomas. Adverse effects were first described by Rubin in 1972 (15) and have been reported in approximately 2–3% of patients (16); however, some investigators feel that this is an underestimation (17). Adverse reactions may occur immediately or many years after injection.
Both experimental and postmortem studies have shown a chronic foreign body granulomatous reaction from Teflon. On injection into canine vocal folds, Teflon causes an immediate inflammatory reaction with active phagocytosis and formation of giant cells. By 2 months, the acute inflammation subsides and actively phagocytosing giant cells are seen surrounding Teflon particles (18, 19). In humans, dense collagenous tissue encapsulating a granulomatous reaction is seen within 3–6 months after injection (20). This foreign-body reaction persists and may progress, sometimes causing a stiff vocal cord and poorer voice quality that is difficult to correct surgically.
With improper, or excessive, injection, Teflon can penetrate extralaryngeal tissues (21) where it can form granulomas. These “Teflonomas” have been documented to simulate thyroid carcinoma, precricoid swelling, or an endotracheal nodule (22–24). Thus, it is reasonable to assume that there is a significant potential for false-positive PET findings in tissues adjacent to the injected vocal cord, as well as in the cord itself.
Whether secondary to infectious or autoimmune processes, granulomas introduce the potential for false-positive PET intreprations. In vitro studies have shown FDG accumulation in lymphocytes and macrophages, thus providing a mechanism for the increased uptake in macrophage-laden granulomas (25). Pulmonary nodules secondary to tuberculomas or sarcoid granulomas have been shown to have FDG uptake comparable to that of malignant tissue (12). Although there has been a case report of foreign-body granuloma secondary to retained textile in a patient with a history of back surgery (26), we do not know of any false-positive cases secondary to a Teflon granuloma. Because combined PET and CT is frequently used in the staging and monitoring of head and neck cancer, a “Teflonoma” is important to consider for patients with a history of head and neck surgery, neoplasm, or vocal cord paralysis.
Conclusion
Teflon has been established as a cause of a foreign-body granulomatous reaction, and it is well known that foreign–body and infectious granulomas can demonstrate increased FDG uptake. Teflon was the mainstay of vocal cord medialization for almost 30 years; knowledge of this common surgical intervention is important to avoid false-positive PET interpretations in the injected vocal cord and in the surrounding tissues to which Teflon may migrate. The additional information obtained from precise localization with PET and CT prevents unnecessary medical and surgical interventions.
References
- 1.Jabour BA, Choi Y, Hoh CK, et al. Extracranial head and neck: PET imaging with 2-[F-18] fluoro-2-deoxy-D-glucose and MR imaging correlation. Radiology 1993;186:27–35 [DOI] [PubMed] [Google Scholar]
- 2.Lowe VJ, Kim H, Boyd JH, et al. Primary and recurrent early stage laryngeal cancer: preliminary results of 2-[fluorine 19] fluoro-2-deoxy-D-glucose PET imaging. Radiology 1999;212:799–802 [DOI] [PubMed] [Google Scholar]
- 3.Frilling A, Tecklenborg K, Gorges R, et al. Preoperative diagnostic value of [18F] fluorodeoxyglucose positron emission tomography in patients with radioiodine-negative recurrent well-differentiated thyroid carcinoma. Ann Surg 2001;234:804–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grunwald F, Kalicke T, Feine U, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography in thyroid cancer: results of a multicentre study. Eur J Nucl Med 1999;26:1547–1552 [DOI] [PubMed] [Google Scholar]
- 5.Conti PS, Durski JM, Bacqai F, et al. Imaging of locally recurrent and metastatic thyroid cancer with positron emission tomography. Thyroid 1999;9:797–804 [DOI] [PubMed] [Google Scholar]
- 6.Beyer T, Townsend DW, Brun T, et al. A combined PET/CT scanner for clinical oncology. J Nucl Med 2000;41:1369–1379 [PubMed] [Google Scholar]
- 7.Zimmer LA, McCook B, Meltzer CC, et al. Combined PET/CT imaging of recurrent thyroid cancer. Otolaryngol Head Neck Surg 2003;128:178–184 [DOI] [PubMed] [Google Scholar]
- 8.Schlumberger MJ. Medical progress: papillary and follicular thyroid carcinoma. N Engl J Med 1998;338:297–306 [DOI] [PubMed] [Google Scholar]
- 9.Rudd JHF, Warburton EA, Fryer TD, et al. Imaging atherosclerotic plaque inflammation with [18F]-fluorodeoxyglucose positron emission tomography. Circulation 2002;105:2708–2711 [DOI] [PubMed] [Google Scholar]
- 10.Tahara T, Ichiya Y, Kuwabara Y, et al. High [18F]-fluorodeoxyglucose uptake in abdominal abscesses: a PET study. J Comput Assist Tomogr 1989;13:829–831 [DOI] [PubMed] [Google Scholar]
- 11.Kawabe J, Okamura T, Koyama K, et al. Relatively high F-18 fluorodeoxyglucose uptake in paranasal sinus aspergillosis: a PET study. Ann Nucl Med 1998;12:145–148 [DOI] [PubMed] [Google Scholar]
- 12.Patz EF, Lowe VJ, Hoffman JM, et al. Focal pulmonary abnormalities: evaluation with 18F-fluorodeoxyglucose PET scanning. Radiology 1993;188:487–490 [DOI] [PubMed] [Google Scholar]
- 13.Zhuang H, Pourdehnad M, Lambright ES, et al. Dual time point 18F-FDG PET imaging for differentiating malignant from inflammatory processes. J Nucl Med 2001;42:1412–1417 [PubMed] [Google Scholar]
- 14.Flynn MB, Lyons KJ, Tartar JW, Ragsdale TL. Local complications after surgical resection for thyroid cancer. Am J Surg 1994;168:404–407 [DOI] [PubMed] [Google Scholar]
- 15.Rubin HJ. Misadventures with injectable Polytef (Teflon). Arch Otolaryngol 1975;101:114–116 [DOI] [PubMed] [Google Scholar]
- 16.Dedo H. Injection and removal of Teflon for unilateral vocal cord paralysis. Ann Otol Rhinol Laryngol 1992;101:81–86 [DOI] [PubMed] [Google Scholar]
- 17.Nakayama M, Ford CN, Bless DM. Teflon vocal fold augmentation: failures and management in 28 cases. Otolaryngol Head Neck Surg 1993;109:493–498 [DOI] [PubMed] [Google Scholar]
- 18.Kirchner F, Toledo P, Svoboda D. Studies of the larynx after Teflon injection. Arch Otolaryngol 1966;83:350–354. [DOI] [PubMed] [Google Scholar]
- 19.Toomy JM, Brown BS. The histological response to intracordal injection of Teflon paste. Laryngoscope 1967;77:110–120 [DOI] [PubMed] [Google Scholar]
- 20.Dedo HH, Carlsoo B. Histologic evaluation of Teflon granulomas of human vocal cords: a light and electron microscopic study. Acta Otolaryngol (Stockh) 1982;93:475–484 [DOI] [PubMed] [Google Scholar]
- 21.Ellis JC, McCaffrey TV, DeSanto LW, Reiman HV. Migration of Teflon after vocal cord injection. Otolaryngol Head Neck Surg 1987;96:63–66 [DOI] [PubMed] [Google Scholar]
- 22.Walsh FM, Castelli JB. Polytef granuloma clinically simulating carcinoma of the thyroid. Arch Otolaryngol 1975;101:262–265 [DOI] [PubMed] [Google Scholar]
- 23.Jol J, Seedat R, Skinner D. A precricoid swelling in a patient treated with Teflon injection in the vocal fold after idiopathic left vocal fold palsy. J Laryngol Otol 1998;112:878–879 [DOI] [PubMed] [Google Scholar]
- 24.McCarthy MP, Gideon JK, Schnadig VJ. A Teflon granuloma presenting as an endotracheal nodule. Chest 1993;104:311–313 [DOI] [PubMed] [Google Scholar]
- 25.Kubota R, Yamada S, Kubota K, et al. Intratumoral distribution of fluorine-18-fluorodeoxyglucose in vivo: high accumulation in macrophages and granulocytes studied by microautoradiography. J Nucl Med 1992;33:1972–1980 [PubMed] [Google Scholar]
- 26.De Winter F, Huysse W, De Paepe P, et al. High F-18 FDG uptake in a paraspinal textiloma. Clin Nucl Med 2002;27:132–133 [DOI] [PubMed] [Google Scholar]