Abstract
Summary: To our knowledge, the use of transdermal nitroglycerin ointment (Nitropaste) in the setting of intracranial vasospasm has not been described in the peer-reviewed literature. Five patients with intracranial vasospasm induced by subarachnoid hemorrhage were evaluated angiographically both before and after application of Nitropaste. All cases exhibited mild to moderate improvement in the degree of vasospasm. We conclude that Nitropaste is a simple noninvasive technique to reduce intracranial vasospasm.
The treatment of intracranial vasospasm secondary to subarachnoid hemorrhage frequently requires endovascular intervention, including balloon angioplasty and intraarterial infusion of nitroglycerin or papaverine (1). Because Nitropaste is known to improve extracranial carotid vasospasm, an investigation of Nitropaste’s effect on intracranial vasospasm was performed (2).
Technique
Four female patients and one male patient (age range, 14 months–55 years) underwent clip placement (n = 1) or embolization (n = 4) for ruptured intracranial aneurysms. These patients subsequently developed cerebral vasospasm as determined by clinical criteria or by transcranial Doppler sonography. Each patient underwent conventional cerebral angiography. Next, .5–5 inches (1.3–13 cm) of Nitropaste (E. Fougera & Co., Melville, NY) was applied to the neck or upper chest, and repeat angiography was performed 7–26 minutes later. Any change in the systemic blood pressure following the application of Nitropaste was mild (<15 mm Hg deviation from baseline) and temporary, lasting less than 45 minutes. Furthermore, no patient developed systemic hypotension (systolic <100 mm Hg; diastolic <60 mm Hg). Of the three patients with ventriculostomies, intracranial pressure did not appreciably fluctuate (<5 mm Hg deviation from baseline) with transdermal Nitropaste. Patients received a single (8–12-hour) application of Nitropaste. The duration of improved vasospasm did not diminish while the patient was in the angiography suite (up to 3 hours of observation). One patient, whose severe vasospasm showed moderate angiographic improvement with Nitropaste, was definitively treated with balloon angioplasty during the same procedure. Otherwise, no patient required additional endovascular treatment for vasospasm. Medical management (hypertension, hemodilution, and hypervolemia) was continued for any residual vasospasm, and all patients showed progressive clinical improvement. All patients survived and were subsequently discharged. Overall, no adverse neurologic or cardiovascular events were associated with the application of Nitropaste.
Discussion
Originally used in the treatment of angina pectoris, Nitropaste has gained popularity for its effective use in preventing and relieving catheter-induced vasospasm of the extracranial carotid artery during angiography (2). Nitropaste contains 2% of the active ingredient nitroglycerin, prepared as an ointment. Each inch (2.5 cm) of Nitropaste contains 15 mg of nitroglycerin. For adults, 2–5 inches (5–13 cm) of Nitropaste are measured onto a tongue depressor and then applied to the chest wall, neck, or forehead. In general, the amount applied is determined by patient age and weight, degree of vasospasm, and duration of desired effect. In our experience, we suggest an application of no more than .5 inch for patients younger than 3 years, up to 1 inch for patients 3–8 years years old, and 1–2 inches for patients 8–17 years old. For adults, the baseline dose of 2 inches should be increased an additional inch for each of the following: moderate or severe vasospasm, body weight greater than 100 kg, and extended duration of effect (ie, up to 12 hours). The adult dose should not exceed 5 inches.
Within 30 minutes of application, Nitropaste causes relaxation of vascular smooth muscle with resulting dilatation of arteries and veins (3). Shortening the duration of dilatation is achieved by wiping the Nitropaste from the patient with a towel. Repeated use is ineffective because of development of systemic nitrate tolerance. Although transient, mild headache is not an infrequent side effect; symptomatic hypotension and paradoxical bradycardia are uncommon.
In this series, mild to moderate improvement of vasospasm was confirmed by angiography in all patients. Vasospasm was localized to the supraclinoid occurred to allow passage of the microguidewire and balloon within the narrowed vessels (Fig 1). In another patient whose moderate vasospasm was refractory to intraarterial papaverine infusion, Nitropaste was noted to diminish the degree of vasospasm (Fig 2). Three patients, including a 14-month-old boy with mild vasospasm, required no endovascular intervention after exhibiting angiographic improvement with Nitropaste alone (Fig 3). No patients developed hypotension, arrhythmia, or other cardiovascular symptoms.
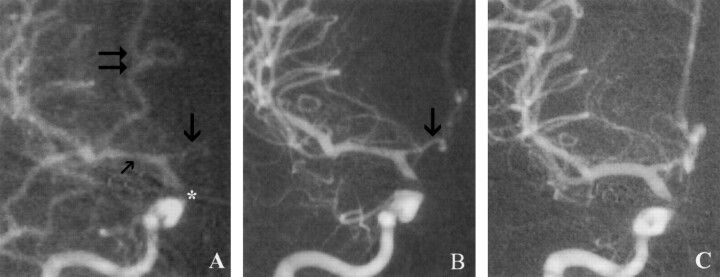
Fig 1.
Angiograms acquired in a 42-year-old female patient with a ruptured right supraclinoid ICA aneurysm.
A, Angiogram obtained 10 days after subarachnoid hemorrhage reveals significant vasospasm of the M1 (small arrow) and A1 segments (arrow) of the middle cerebral artery and anterior cerebral artery, respectively. Note contrast material reflux into external carotid vasculature (double arrows). A filling defect of the internal carotid artery can be explained by aneurysm clip artifact (asterisk).
B, Angiogram obtained 7 minutes after applying 2 inches of Nitropaste to the upper chest shows an increase in the diameter of the distal internal carotid artery and M1 and A1 (arrow) segments, including notably improved distal flow in the anterior cerebral artery branches. Note the lack of contrast material reflux into the external carotid vasculature.
C, Final angiogram obtained after reveals caliber normalization of the supraclinoid ICA and proximal anterior and middle cerebral arteries.
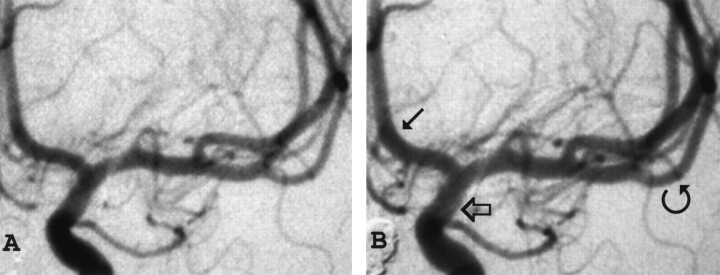
Fig 2.
Angiograms obtained in a 45-year-old female patient with a ruptured basilar tip aneurysm.
A, Angiogram acquired in a patient with mild vasospasm; transcranial sonography revealed subarachnoid hemorrhage 3 days earlier.
B, Twenty-six minutes after applying 3 inches of Nitropaste to the upper chest, the supraclinoid internal carotid artery (open arrow), anterior cerebral artery (arrow), and middle cerebral artery (curved arrow) have definitely increased in diameter.
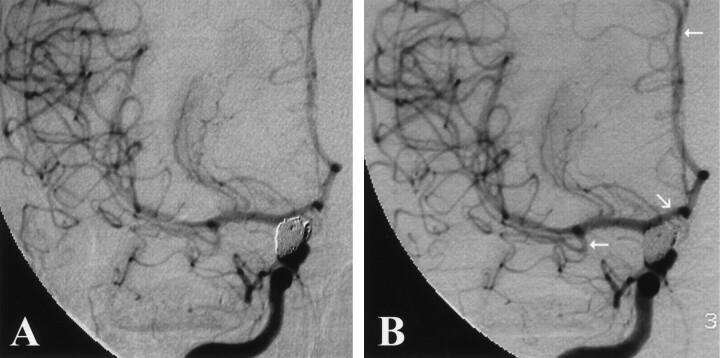
Fig 3.
Angiograms acquired in a 55-year-old patient with a ruptured right paraophthalmic ICA aneurysm.
A, Angiogram, frontal-right projection,of the internal carotid artery depicts mild vasospasm of the anterior and middle cerebral vasculature secondary to a ruptured, and subsequently coiled, paraophthalmic aneurysm.
B, Repeat angiogram obtained 27 minutes after application of transdermal Nitropaste reveals improved vasospasm in the anterior cerebral artery and middle cerebral artery territories (arrows).
Conclusion
The application of Nitropaste is a safe and simple noninvasive technique that can reduce the degree of intracranial vasospasm resulting from subarachnoid hemorrhage. Endovascular surgeons should find Nitropaste useful in this regard.
Footnotes
Presented at the 5th Joint Annual Meeting of the AANS/CNS Section on Cerebrovascular Surgery and the American Society of Interventional and Therapeutic Neuroradiology, Dallas, Texas, February 3–6, 2002.
References
- 1.Treggiari-Venzi MM, Suter PM, Romand JA. Review of medical prevention of vasospasm after aneurysmal subarachnoid hemorrhage: a problem of neurointensive care. Neurosurgery 2001;48:249–262 [DOI] [PubMed] [Google Scholar]
- 2.Erba M, Jungreis CA, Horton JA. Nitropaste for prevention and relief of vascular spasm. AJNR Am J Neuroradiol 1989;15:155–156 [PMC free article] [PubMed] [Google Scholar]
- 3.Corwin S, Reiffel JA. Nitrate therapy for angina pectoris. Arch Intern Med 1985;145:538–543 [DOI] [PubMed] [Google Scholar]