Abstract
BACKGROUND AND PURPOSE: Percutaneous vertebroplasty procedures require relatively long durations of fluoroscopic guidance, which might lead to substantial radiation dose to operators. Specialized injection devices have been proposed to limit operator exposure. Our purpose was to compare the radiation dose to the operator’s hands during vertebroplasty when using 1-cc syringes versus that when using an injection device.
METHODS: Radiation dosimeters were worn on the left wrist during 39 vertebroplasty injection procedures in 25 patients. Cases were alternated between the use of 1-cc syringes (19 procedures) and the use of an injection device (20 procedures). For each procedure, one dosimeter was worn throughout the procedure, both during needle placement and injection, and a second dosimeter was worn during the injection phase only. Mean doses for the whole case and mean doses for the injection procedure alone were compared between groups.
RESULTS: Mean whole case dose was 128 ± 161 mrem (range, 0–660 mrem) for the 1-cc syringe group versus 98 ± 90 mrem (range, 0–340 mrem) for the injection device group (P = .23). Mean dose during injection was 100 ± 145 mrem (range, 0–660 mrem) for the 1-cc syringe group versus 55 ± 43 mrem (range, 0–130 mrem) for the injection device group (P = .09). Three of 19 1-cc syringe cases yielded zero dose, compared with four of 20 injection device cases. Duration of injection was markedly different between groups, with mean injection times of 4.2 and 7.5 min for 1-cc syringe and injection device cases, respectively (P < .00002). Mean injection dose per minute of lateral fluoroscopy was 23.6 and 7.3 mrem for the 1-cc syringe and injection device groups, respectively (P = .002).
CONCLUSION: The use of an injection device significantly decreased the radiation dose to the operator’s extremity per unit time of injection. However, total dose per injection was equivalent between groups because of significantly longer injection duration for the injection device cohort.
Percutaneous vertebroplasty is safely performed by many practitioners worldwide by using various modifications of published techniques (1–3). Variations in practice include variations in needle gauge, needle trajectory, and use of venography (4–7). The mode of cement injection also varies depending on physician preference. Early reports detailed the use of 1-cc syringes filled in serial fashion from a larger reservoir; more recent works emphasize the use of specialized injection devices (2, 8, 9). A typical injection device includes a single, large cement reservoir to eradicate the need for multiple connections of syringes to the needle and a connector tube to maximize the distance between the operator and the radiation field. This increased distance would be expected to result in a lower radiation dose to the operator during vertebroplasty.
To quantify the expected benefit to the operator regarding radiation dose, we conducted a prospective trial in which we measured the extremity dose to the operator when using 1-cc syringes as compared with that when using an injection device (EZ Flow CDS; Parallax Medical, Scotts Valley, CA).
Methods
We performed a prospective trial comparing the dose to the operator’s extremity during vertebroplasty when using 1-cc syringes versus that when using the CDS injection device. Institutional Review Board approval was obtained for this study, and informed consent was obtained from all patients enrolled. A single primary operator (a fellow physician working as a team with an attending radiologist) performed all needle placement and injection procedures. Procedures were performed by using a biplane Siemens NeuroStar (Siemens, Erlangen, Germany). Throughout the study, which was conducted between September 2001 and February 2002, we alternated between 1-cc syringes and the CDS injection device (ie, for each subsequent needle used, either in the same patient or in a different patient, we alternated between 1-cc syringes and the injection device).
The operator stood at the left side of the angiography table, and patients were positioned in a prone position for the procedure (Figs 1 and 2). The lateral tube on our biplane system was positioned on the left side of the patient, and the lateral image intensifier was on the right side of the angiography table. Thus, the operator was standing closer to the lateral tube than to the lateral image intensifier (Figs 1 and 2). The anteroposterior tube was underneath the table, and the anteroposterior image intensifier was above the patient. Note that a radiation shield was not used during needle placement for 1-cc syringe injection because there was insufficient room to allow its use (Fig 1). Because the injection device had a 17-in-long connector tubing that increased the distance between the needle and the operator, there was sufficient room to position the radiation shield between the operator and the X-ray tube (Fig 2). We acknowledge that because scatter emanating from the patient would have been the predominant radiation source to the operator, the radiation shield may have had limited effect in diminishing the dose.
Fig 1.
Room setup for injections when using 1-cc syringes. The operator is standing to the left of the angiography table. The lateral X-ray tube is immediately to the left of the operator (large arrow). The operator’s hands are holding the 1-cc syringe attached directly to the needle (small arrow). A radiation shield is not used.
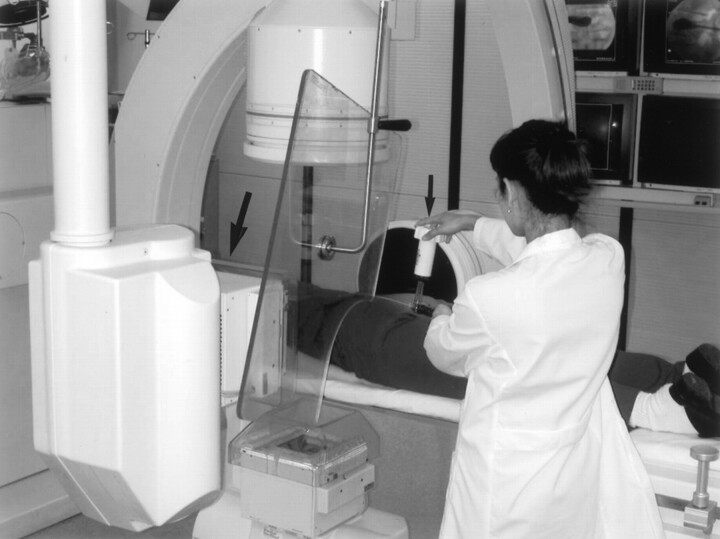
Fig 2.
Room setup for injections when using the EZ Flow CDS injection device. The operator is standing to the left of the angiography table. The lateral X-ray tube is to the left of the operator (large arrow), with a radiation shield interposed between the tube and the operator. The operator’s hands are holding the injection device (small arrow), with the 17-in tubing interposed between the device and the needle.
Dosimetry
Dose was measured by using Luxel optically stimulated luminescence dosimeters (Landauer, Glenwood, IL). We sought to measure the dose to the operator’s extremity during the whole procedure, including needle placement and cement injection, and during cement injection alone. We measured these doses separately because dose during needle placement would likely have been very similar between 1-cc syringe and injection device cases because the choice of injector does not influence dose during needle placement. Conversely, dose differences during cement injection, when the operator’s hands are close to the field when using a 1-cc syringe but far from the field when using an injection device, would be maximized. The operator affixed a dosimeter to her left wrist before beginning needle placement. This dosimeter, termed the whole procedure dosimeter, remained in place until after cement injection was complete. After needle placement was complete, the operator affixed a second dosimeter immediately adjacent to the whole procedure dosimeter; this second dosimeter, termed the injection dosimeter, was worn during cement injection. After injection and acquisition of postprocedural anteroposterior and lateral view spot films, the dosimeters were removed. New dosimeters were used for subsequent needle placement and injection, as necessary.
Vertebroplasty Technique
Using a sterile technique, an 11-gauge needle was placed via a transpedicular approach into the targeted vertebral body. For 1-cc syringe cases, we used 11-gauge needles that had both uni- and multibeveled stylets (Osteo-site Bone Biopsy Needle; Cook, Inc., Bloomington, IN). For injection device cases, we used the needles that were supplied as a kit with the CDS injection device. At the beginning of needle placement, metallic clamps were used to stabilize the needle while anteroposterior and lateral fluoroscopy was performed. After some purchase into the bone had been achieved, the operator’s hands were withdrawn from the radiation field during fluoroscopy to confirm needle placement position. A radiation shield was not used during the needle placement portion of the procedure, because it was inconvenient to have the shield between the operator and the needle. Intermittent anteroposterior and lateral fluoroscopy was used to facilitate needle placement. We used the modified unipedicular needle trajectory that places the needle tip via a transpedicular approach into the central aspect of the ventral portion of the vertebral body (7).
Venography was not performed in any case. Polymethylmethacrylate was mixed in the usual fashion, as described elsewhere (2). Briefly, the cement was prepared by combining polymethylmethacrylate powder (Secour, Parallax), liquid polymethylmethacrylate monomer (Secour), tobramycin powder for infection control, and barium sulfate (Tracers, Parallax) for opacification as previously described (2). The cement was mixed until it obtained a viscous consistency. Injection of polymethylmethacrylate was performed under continuous lateral fluoroscopy; intermittent anteroposterior fluoroscopy was performed to check for lateral extravasation of cement not evident on lateral fluoroscopy. We used maximum magnification and coned the field to include only the vertebral body and the spinal canal, adjacent vertebral end plates, and 1 to 2 cm of the retroperitoneal space.
For injections using the 1-cc syringes, we sequentially filled approximately 0.5 mL into the syringes. Both hands of the operator were used for injection, with the right thumb used to push the plunger and the left hand used to stabilize the plunger and avoid rapid injection of cement (Fig 1). When using the injection device, the operator stood as far as possible from the field (Fig 2). For all injections, slow injection was accomplished by using continuous lateral fluoroscopy. Injection was terminated when cement reached the posterior one-fourth of the vertebral body or when extraosseous extravasation, either through an end plate or lateral vein, was considered to be greater than acceptable. Careful monitoring of exact volume of cement was performed. After injection, the needle was removed and bi-plane radiographs were obtained.
Data Collection
We noted duration of anteroposterior and lateral fluoroscopy for needle placement and cement injection. We also noted the average kV and average mA for both the anteroposterior and lateral tube during needle placement and cement injection. We noted patient weight, height, lateral width, and anteroposterior width. The volume of cement injected was carefully documented.
Statistical Analysis
Independent variables were compared between groups by using a t test for two independent sample means. We compared the mean doses for both the whole case and the injection portion of the procedure for 1-cc syringes and the injection device.
Results
Patient Population
Twenty-five patients were enrolled in the study. A total of 39 injections were performed in these 25 patients, 19 by using 1-cc syringes and 20 by using the CDS injection device. Each of nine patients underwent a single injection with the injection device. Each of six patients underwent a single injection with 1-cc syringes. Ten patients underwent injections with both 1-cc syringes and the injection device, with up to four separate injections for a single patient.
No significant difference was noted between groups regarding patient weight, anteroposterior or lateral width, or height (Table 1). No significant difference was noted in needle placement time or cement volume between groups (Table 1). Levels injected included nine thoracic and 10 lumbar for the 1-cc syringe group and nine thoracic and 11 lumbar for the CDS group. Duration of injection was markedly different between groups, with mean injection times of 4.2 and 7.5 min for 1-cc syringe and injection device cases, respectively (P < .00002).
TABLE 1:
Comparison between groups
| Parameter | 1-cc Syringes | Injection Device* | P value |
|---|---|---|---|
| Volume of cement (cc) | 2.3 | 2.1 | 0.34 |
| Lateral fluoroscopy time, cement injection (min) | 4.2 | 7.5 | 0.00002 |
| Anteroposterior fluoroscopy time, cement injection (min) | 0.5 | 0.6 | 0.23 |
| Lateral fluoroscopy time, needle placement (min) | 1.8 | 1.8 | 0.50 |
| Anteroposterior fluoroscopy time, needle placement (min) | 2.2 | 2.0 | 0.28 |
| Weight (pounds) | 150 | 145 | 0.38 |
| Lateral width (in) | 31.4 | 31.5 | 0.48 |
| Anteroposterior width (in) | 21.8 | 21.5 | 0.42 |
| Height (in) | 64.0 | 63.8 | 0.45 |
| mA (lateral tube, cement injection) | 10.1 | 11.0 | 0.20 |
Ezflow CDS injector device, Parallax Medical, Scotts Valley CA
Mean whole case dose was 128 ± 161 mrem (range, 0–660 mrem) for the 1-cc syringe group versus 98 ± 90 mrem (range, 0–340 mrem) for the injection device group (P = .23). Mean dose during injection was 100 ± 145 mrem (range, 0–660 mrem) for the 1-cc syringe group versus 55 ± 43 mrem (range, 0–130 mrem) for the injection device group (P = .09). Three of 19 1-cc syringe cases yielded zero dose compared with four of 20 injection device cases. Mean injection doses per minute of lateral fluoroscopy was 23.6 and 7.3 mrem for the 1-cc syringe and injection device groups, respectively (P = .002).
Discussion
The vertebroplasty technique has rapidly evolved during the past decade (1–3, 10). Changes have been made regarding needle placement, type of opacification agent, and mode of injection (1–3, 8, 9). Specifically, customized injection devices have been developed not only to eliminate the need for multiple syringe attachments but also to reduce operator radiation dose as compared with that obtained by using 1-cc syringes. This study was designed to test the hypothesis that radiation dose to the operator’s extremity would be diminished with the use of an injection device compared with the use of 1-cc syringes.
With this prospective study, we could not show, when considering radiation dose per injection, a difference in dose to the operator’s extremity when comparing vertebroplasty performed with 1-cc syringes to that performed with an injection device. However, the mean injection duration for the injection device was nearly two times that for the 1-cc syringes. When comparing dose per minute of injection, the dose with the injection device was statistically significantly lower than that with 1-cc syringes (P = .002). The mean dose per minute of injection with 1-cc syringes was nearly four times that with the injection device. This difference likely reflects the increased distance between the operator and the radiation field.
The underlying reason why injection times were significantly longer with the injection device compared with 1-cc syringes remains unclear. Our group has substantially greater experience in performing vertebroplasty with 1-cc syringes than with injection devices; longer injection times may reflect lack of comfort with the device from relative inexperience. Also, the amount of tactile feedback, in our opinion, was greater with the 1-cc syringe compared with that afforded by the injection device. Untoward rapid injection of cement from buildup of pressure proximally in the system was considered less likely with the 1-cc syringes and thus may have prompted us to inject more rapidly in those than in the injection device cases. We surmise that operators with substantial experience with the injection device, for whom injection times may be shorter than ours, would enjoy significantly lower extremity exposures.
This study addresses the importance of dose to the operator during percutaneous vertebroplasty. Across all cases, the mean extremity dose was approximately 100 mrem. Current guidelines for dose to the extremities indicate a maximum safe dosage of 50 rem/year (11). Using these values, operators would approach the extremity dose limit with 500 injections in a given year, which might be approached in a very busy practice.
We used state-of-the-art dosimeters to measure dose. The performance of the dosimeters was benchmarked by a program accredited by the National Voluntary Laboratory Accreditation Program and managed by the National Institute of Standards and Technology. However, we cannot exclude that some error occurred from variation in positioning of the dosimeters on the operator’s wrist or from other variables. We noted zero dose in several cases. The dosimeters used in this study were capable of detecting extremely small doses. We expected that scattered radiation would have been detected in every case and cannot readily explain why zero dose was found in several cases.
The use of continuous fluoroscopy represents a “worst case” scenario regarding dose to the operator, as compared with expected doses from the use of intermittent fluoroscopy. Intermittent imaging has been used when CT guidance was applied (1); small aliquots of cement were deposited blindly and then imaged with CT scanning. We consider blind deposition of cement to be potentially dangerous. We have noted cement within paravertebral veins to rapidly travel to the inferior vena cava. This migration would be missed by using intermittent fluoroscopy.
This study was prospective and involved a design that randomized use of 1-cc syringes versus the CDS injection device. This design was used to minimize bias from factors such as patient size, patient weight, and cement volume. We noted no significant difference between groups for these important parameters. However, there may have been other systematic biases that we did not or could not have accounted for. We measured extremity dose but did not measure whole body dose, which further limits this study. We chose to focus on extremity dose because we hypothesized that because the hands are nearly in the radiation field, this difference would be maximized between groups. Furthermore, exact doses noted by using our angiography system would not be expected to directly apply to other systems. Last, it was not possible to use a radiation shield for cases in which the 1-cc syringes were used; the position of the operator’s arms and torso did not allow placement of the shield between the X-ray tube and the operator. Because we used the shield for cases in which the injection device was used, it remains possible that measured doses were biased in favor of the injection device.
Conclusion
When comparing extremity radiation dose per unit time of cement injection, the CDS injection device afforded significantly lower exposure as compared with 1-cc syringes during percutaneous vertebroplasty. However, because of significantly longer injection times with the injection device, we found no difference in extremity radiation dose on a per-case basis.
Acknowledgments
The authors thank Mary E. Near, William H. Thompson, Theodore J. Bittner, Vanessa K. Morris, and David D. Pillar for technical assistance throughout this project.
Footnotes
This project was funded by Parallax Medical, Inc.
References
- 1.Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine 2000;25:923–928 [DOI] [PubMed] [Google Scholar]
- 2.Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol 1997;18:1897–1904 [PMC free article] [PubMed] [Google Scholar]
- 3.Gangi A, Kastler BA, Dietemann JL. Percutaneous vertebroplasty guided by a combination of CT and fluoroscopy. AJNR Am J Neuroradiol 1994;15:83–86 [PMC free article] [PubMed] [Google Scholar]
- 4.Gaughen JR Jr, Jensen ME, Schweickert PA, Kaufmann TJ, Marx WF, Kallmes DF. Relevance of antecedent venography in percutaneous vertebroplasty for the treatment of osteoporotic compression fractures. AJNR Am J Neuroradiol 2002;23:594–600 [PMC free article] [PubMed] [Google Scholar]
- 5.Vasconcelos C, Gailloud P, Beauchamp NJ, Heck DV, Murphy KJ. Is Percutaneous vertebroplasty without pretreatment venography safe? evaluation of 205 consecutives procedures. AJNR Am J Neuroradiol 2002;23:913–917 [PMC free article] [PubMed] [Google Scholar]
- 6.McGraw JK, Heatwole EV, Strnad BT, Silber JS, Patzilk SB, Boorstein JM. Predictive value of intraosseous venography before percutaneous vertebroplasty. J Vasc Interv Radiol 2002;13:149–153 [DOI] [PubMed] [Google Scholar]
- 7.Kim AK, Jensen ME, Dion JE, Schweickert PA, Kaufmann TJ, Kallmes DF. Unilateral transpedicular percutaneous vertebroplasty: initial experience. Radiology 2002;222:737–741 [DOI] [PubMed] [Google Scholar]
- 8.Schallen EH, Gilula LA. Vertebroplasty: reusable flange converter with hub lock for injection of polymethylmethacrylate with screw-plunger syringe. Radiology 2002;222:851–855 [DOI] [PubMed] [Google Scholar]
- 9.Al-Assir I, Perez-Higueras A, Florensa J, Munoz A, Cuesta E. Percutaneous vertebroplasty: a special syringe for cement injection. AJNR Am J Neuroradiol 2000;21:159–161 [PMC free article] [PubMed] [Google Scholar]
- 10.Cotten A, Boutry N, Cortet B, et al. Percutaneous vertebroplasty: state of the art. Radiographics 1998;18:311–323 [DOI] [PubMed] [Google Scholar]
- 11.U.S. Nuclear Regulatory Commission. Occupational Dose Limits for Adults. Washington: U.S. Government Printing Office;2002. :10 CFR 20.1201