Abstract
The aim of this paper was to better understand how child and adult adversities cluster together into classes, and how these classes relate to body weight and obesity. Analyses included 2015 and 2018 data from emerging adults (18–25 years old) who participated in a state surveillance system of 2- and 4-year college students in Minnesota (N=7,475 in 2015 and N=6,683 in 2018). Latent Class Analyses (LCA) of 12 child and adult adversities were run stratified by gender and replicated between 2015 and 2018. The distal outcome procedure and three-step Bolck-Croon-Hagenaars approach were used to estimate predicted BMI means and predicted probabilities of obesity for each class, adjusted for covariates. The LCA identified seven classes in women and 5 in men. In women, BMI ranged from 23.9 kg/m2 in the lowest-BMI class (“Adult Adversities and Childhood Household Dysfunction”; 95% CI: 22.6–25.1) to 27.3 kg/m2 in the highest-BMI class (“High Lifetime Adversities”; 95% CI: 25.9–28.7), a statistically significant difference of 3.4 kg/m2. In men, the adjusted BMIs ranged from 24.6 kg/m2 (“Low Adversities”; 95% CI: 24.3–25.0) to 26.0 kg/m2 (“Childhood Household Mental Illness”; 95% CI: 25.1–26.9), a statistically significant difference of 1.4 kg/m2. The pattern was similar for obesity. These results indicate that specific classes of child and adult adversities are strongly associated with BMI and obesity, particularly in women. A key contribution of LCA appeared to be identification of small classes at high risk for excess weight.
Keywords: adverse childhood experiences, obesity, latent class analysis
INTRODUCTION
An estimated 5.5 million Americans develop obesity by their early 30s,(Gordon-Larsen et al., 2004) setting a course for poor health across the lifespan.(Cheng et al., 2016; Guo et al., 2016; Twig et al., 2014) Individuals with Adverse Childhood Experiences (ACEs), including childhood maltreatment (e.g., sexual, physical, emotional abuse; neglect) and household dysfunction (e.g., parent/caregiver mental illness, incarceration, household domestic violence), have a particularly high risk of obesity.(Danese and Tan, 2014) For example, a meta-analysis of 41 studies estimated childhood abuse was associated with 36% increased risk of adult obesity (BMI≥30 kg/m2).(Danese and Tan, 2014) At least one childhood instance of sexual, verbal, fear of physical and physical abuse accounts for an estimated 8% of population-wide obesity and 17% of class III obesity (BMI≥40kg/m2)(Williamson et al., 2002), on par with high sugar consumption.(Te Morenga et al., 2013) Importantly, ACE-related obesity may first develop in late adolescence or emerging adulthood (18–25 years).(Noll et al., 2007),(Roehrkasse and Wildeman, 2019) This evidence suggests a need for targeted obesity prevention among emerging adults with ACE histories, potentially before the onset of many weight-related problems.(Nelson et al., 2008) However, information is lacking with regard to what ACEs or combinations of ACEs are associated with the greatest weight-related risks at this age, and whether the current approach of measuring ACEs as a unidimensional construct (i.e., a summed score) is adequate for identifying those at greatest risk.
Recent research has used more complex analytic tools, like latent class analysis (LCA), to identify specific combinations of ACE exposures that confer higher risk of various outcomes.(Charak et al., 2019; Menard et al., 2004; Merians et al., 2019; Shin et al., 2018a, 2018b) These analytic tools go beyond the widely-used ACE summary score by acknowledging that ACEs encompass diverse and correlated exposures, and that subsets or combinations of these exposures may have different associations with health outcomes. Because prior LCA studies have examined a heterogeneous array of ACEs, findings are difficult to synthesize. However, studies generally suggest that ACEs cluster into interpretable classes,(Charak et al., 2019; Menard et al., 2004; Merians et al., 2019; Shin et al., 2018a, 2018b) and these classes predict outcomes like mental health and substance use.(Berzenski and Yates, 2011; Charak et al., 2019; Merians et al., 2019; Shin et al., 2018a, 2018b) For example, one study identified an “emotional adverse child experience” class and found this class to be associated with substantially greater mental health symptoms compared to a low ACE class in young adults.(Shin et al., 2018a) There is evidence of gender differences in the types of classes that emerge, and their associations with outcomes,(Cavanaugh et al., 2015; Garraza et al., 2011) consistent with research on gender-specific effects of adversities.(Smith-Marek et al., 2015)
Despite important advances in understanding classes of ACEs and how they are associated with important health outcomes, several research gaps remain. First, adversities in childhood are highly correlated with young adult experiences of victimization, like intimate partner violence and sexual assault.(Assink et al., 2018; Finkelhor et al., 2007; Lünnemann et al., 2019; Relyea and Ullman, 2017; Smith-Marek et al., 2015; Turner et al., 2010) Those exposed to early events may show stronger stress sensitivity to life events in adulthood.(Heim et al., 2000) Yet only one study(Charak et al., 2019) has examined whether childhood adversities cluster with adult victimization experiences in predictable ways that can advance characterization of lifetime adversity. Second, few LCA studies have attempted to replicate their findings;(Merians et al., 2019) due to the data-driven nature of LCA, replication is important to ensure findings are not driven by random variations in the sample. Finally, we know of no study that has examined obesity prevalence across ACE classes in emerging adults.
Therefore, the goals of this study were to better understand how child and adult adversities cluster into meaningful classes, and how these classes relate to body weight and obesity. We used LCA in a large state surveillance system of 2- and 4-year Minnesota college students to identify classes of ACEs and adult victimization exposures among emerging adults aged 18–25. We used two years of data from this surveillance system to replicate our classes. We then compared the risk of obesity across identified classes. Given differences between men and women (Mason et al., 2016),(Hughes et al., 2017) analyses were gender stratified.
METHODS
Data
Data from the 2015 (N=12,220) and 2018 (N=10,579) College Student Health Survey (CSHS) were used. The CSHS is an annual surveillance system that recruits a random sample of undergraduate and graduate students from institutional enrollment lists in 2-year and 4-year public and private Minnesota colleges. Response rates were 31.6% for 2015 and 36.6% for 2018. Survey methodology is documented elsewhere.(Health and Health-Related Behaviors 2015 College Student Health Survey Report 2015 College Student Health Survey Report, n.d., “Health and Health-Related Behaviors 2018 College Student Health Survey Report,” n.d.) Briefly, students are randomly invited through multiple mailings and emails. To our knowledge, this is the only population-based survey with adequate 2- and 4-year college student representation to measure both ACEs and adult adversities. Findings were cross-replicated across two years of data; results from 2018 are presented as the main findings because they are most current. To study emerging adults, only data from participants 18–25 years old(Arnett, 2000) (N=7,475 in 2015, N=6,683 in 2018) were analyzed.
Measures
Childhood adversities.
Childhood adversities were assessed using the 11-question ACEs questionnaire from the Behavioral Risk Factor Surveillance System (BRFSS),(“Behavioral Risk Factor Surveillance System ACE Data |Violence Prevention|Injury Center|CDC,” 2019) which asks respondents to retrospectively report whether they had experienced any of the following before the age of 18: Childhood emotional, physical, and sexual abuse; household mental illness; household alcohol problems; household drug use; incarcerated household member; parental divorce/separation; and witnessed family violence. All childhood adversity measures were operationalized as dichotomous variables. Questions, response options, and dichotomization cut-points are described in Table 1.
Table 1.
Indicator Question and Response Coding
| Child Adversities | Variable Name | Question | Response Options | Coded Response |
|---|---|---|---|---|
| Childhood emotional abuse | How often did a parent or adult in your home ever swear at you, insult you, or put you down? | Never | No | |
| Once | No | |||
| More than once | Yes | |||
| Childhood physical abuse | How often did a parent or adult in your home ever hit, beat, kick, or physically hurt you in anyway? Do not include spanking. |
Never |
No |
|
| Once | Yes | |||
| More than once | Yes | |||
| Childhood sexual abuse | How often did anyone at least 5 years older than you or an adult, ever touch you sexually? | Never | No | |
| Once | Yes | |||
| More than once | Yes | |||
| Childhood sexual abuse | How often did anyone at least 5 years older than you or an adult, try to make you touch them sexually? | Never | No | |
| Once | Yes | |||
| More than once | Yes | |||
| Childhood sexual abuse | How often did anyone at least 5 years older than you or an adult, force you to have sex? | Never | No | |
| Once | Yes | |||
| More than once | Yes | |||
| Household mental illness | Did you live with anyone who was depressed, mentally ill, or suicidal? | Yes | Yes | |
| No | No | |||
| Don’t know/Not sure | Missing | |||
| Household alcohol abuse | Did you live with anyone who was a problem drinker or alcoholic? | Yes | Yes | |
| No | No | |||
| Don’t know/Not sure | Missing | |||
| Household drug abuse | Did you live with anyone who used illegal street drugs or who abused prescription medications? | Yes | Yes | |
| No | No | |||
| Don’t know/Not sure | Missing | |||
| Incarcera'ed household member | Did you live with anyone who served time or was sentenced to serve time in a prison, jail, or other correctional facility? | Yes | Yes | |
| No | No | |||
| Don’t know/Not sure | Missing | |||
| Parental divorce/separation | Were your parents separated or divorced? | Yes | Yes | |
| No | No | |||
| Parents never married | No | |||
| Don’t know/Not sure | Missing | |||
| Witnessed family violence | How often did your parents or adults in your home ever slap, hit, kick, punch or beat each other up? | Never | No | |
| Once | Yes | |||
| More than once | Yes | |||
| Adult Adversities | Lifetime sexual assault | Have you experienced actual or attempted sexual intercourse without your consent or against your will? | Yes-within the past 12 months | Yes |
| No-within the past 12 months | No | |||
| Yes- within your lifetime | Yes | |||
| No- within your lifetime | No | |||
| Lifetime sexual assault | Have you experienced actual or attempted sexual touching without your consent or against your will? | Yes-within the past 12 months | Yes | |
| No-within the past 12 months | No | |||
| Yes- within your lifetime | Yes | |||
| No- within your lifetime | No | |||
| Adult Intimate partner physical abuse | Have you been slapped, kicked or pushed by your significant other or spouse/partner? | Yes-within the past 12 months | Yes | |
| No-within the past 12 months | No | |||
| Yes- within your lifetime | Yes | |||
| No- within your lifetime | No | |||
| Adult Intimate partner emotional abuse | Have you been hurt by threats, "ptf -do wns', or yelling from your significant other or spouse/partner? | Yes-within the past 12 months | Yes | |
| No-within the past 12 months | No | |||
| Yes- within your lifetime | Yes | |||
| No- within your lifetime | No |
Adult adversities.
Adult adversities included sexual assault, intimate partner emotional abuse, and intimate partner physical abuse, each asked regarding lifetime and past 12 months. The past 12 month and lifetime responses were combined to create ever/never adult adversity variables. Full details of variable formation are in Table 1.
Outcomes: BMI and Obesity.
Body mass index (BMI) was calculated using self-reported weight (converted to kilograms) divided by self-reported height (converted to meters) squared. Obesity was defined as a BMI of ≥30 kg/m2 (versus <30 kg/m2).
Sociodemographic variables.
Sociodemographic variables were used to characterize the sample and were included in adjusted models. Gender was defined as male or female; transgender, other, combination, and prefer not to answer were set to missing due to small sample sizes (2% of the sample). Race and ethnicity were defined as Latino/a, Black, Asian, and White; all other categories were set to missing due to small sample sizes (3.5% of the sample). Parental education was dichotomized with the highest education of any parent, stepparent, or adult caretaker into bachelor’s degree or more education versus less than a bachelor’s degree. Respondents’ post-secondary school type was defined as being currently enrolled in either a 2-year or 4-year college.
Statistical analyses
Analyses were conducted using Mplus Version 7.11 for both years and compared against each other. Replication hypotheses for 2018 data were pre-registered (“Classes of adverse experiences and their associations with body weight and obesity in emerging adulthood,” 2020) at the Center for Open Science based on 2015 exploratory findings. LCA was performed using all 12 child and adult adversity variables as indicators, stratified by gender. A one-class model was fit first, then classes were added one at a time until the fit and/or interpretability worsened. Several criteria were used to judge model fit and precision,(Masyn, 2015) including the sample size-adjusted Bayesian Information Criterion (a-BIC) value, Akaike Information Criterion (AIC) value, Vuong- Lo-Mendell-Rubin(VLMR) likelihood ratio test, and entropy. Smaller a-BIC and AIC values indicated better fit. Significant VLMR values indicated that the k class model was a better fit than the k-1 class model. Entropy values closer to 1.00 indicated more precision. The best model optimized fit criteria and had meaningful qualitative interpretation of classes. After identifying class structures with a good fit to the data and replicating our findings across the 2015 and 2018 samples (as described further below and in Appendix Table A), mean BMI and obesity prevalences were assessed across classes. The distal outcome procedure and three-step Bolck-Croon-Hagenaars (BCH)(Asparouhov and Muthén, 2014) approach were used to estimate the crude and adjusted predicted population BMI means and obesity predicted probabilities for each class, estimated at the mean of the covariate levels (race/ethnicity, parental education, 2/4year college).(Lane and Nelder, 1982) The distal outcome procedure estimates class-dependent distributions of BMI and obesity.(Lanza et al., 2013) The BCH method is superior to other methods because it uses weights to correspond to particular latent classes.(Asparouhov and Muthén, 2014) Overall and pairwise comparisons of covariate-adjusted BMI means and obesity probabilities across classes were tested. However, the primary focus was on estimation and patterns of results, not significance testing.(Lane and Nelder, 1982) Finally, a supplementary analysis among those reporting no diagnosed Post Traumatic Stress Disorder was run to explore whether the observed adversity-weight associations are the consequence of the traumatic effect of the adversity.
Missingness was handled differently across analysis stages. In LCA class formation, the model parameters were estimated using maximum likelihood and the expectation-maximization procedure, which included all participants except those for whom all indicators were missing.(Nylund-Gibson and Choi, 2018) The distal outcome procedure and three-step BCH (Asparouhov and Muthén, 2015) approach used listwise deletion if missing an outcome or covariate measure, (Wang and Wang, 2012) which resulted in deleting 607 (8%) and 715 (11%) observations from the 2015 and 2018 subsamples of emerging adults, respectively.
Replication
Analyses were replicated across the 2015 and 2018 data. The optimal number of classes in men and women were first compared across years and found to be identical in 2015 and 2018. Specific classes from 2015 and 2018 were then matched based on item response probabilities. Most classes showed nearly identical item response probabilities across the two years, including all classes in men and 5 out of 7 classes in women. In the remaining two classes in women, differences between item response probabilities were tested using the partial boundary model.(Schmiege et al., 2018) Specifically, a high item response probability (>0.7) in 2015 was considered replicated in 2018 if either the item response in 2018 was >0.7 or the item response was ≤0.7 but the upper 95% confidence limit was >0.7. Likewise, a low item response probability (<0.3) in 2015 was considered replicated in 2018 if the 2018 item response was <0.3 or it was ≥0.3 but the lower 95% confidence limit was <0.3. This study was determined exempt by the Institutional Review Board at the University of Minnesota.
RESULTS
Descriptive
Table 2 displays demographic characteristics of the 2018 sample, stratified by gender. Men and women were similarly distributed across 2 versus 4-year colleges, with 17% of the sample attending 2-year schools. Race and ethnicity distributions were similar for men and women, but 67% of men reported one or both parents had a college education or more compared to 61% of women.
Table 2.
Percentage of Socio-demographic Characteristics by Gender
| 2018 % (n) | |||
|---|---|---|---|
| Men | Women | ||
| Race and Ethnicity | |||
| Latinx | 6.1( 134) | 5.5( 242) | |
| Black | 4.7( 103) | 4.9( 216) | |
| Asian | 12.6( 275) | 11.1( 485) | |
| White | 76.6( 1673) | 78.5( 3440) | |
| 2/4 Year School | |||
| 2-year | 17.6( 389) | 16.8( 747) | |
| 4-year | 82.5( 1828) | 83.2( 3693) | |
| Parental Education | |||
| Less than college | 32.9( 716) | 38.6( 1684) | |
| College or more | 67.1( 1463) | 61.4( 2678) | |
LCA Class Selection
Table 3 displays fit indices for LCA models for males and females. Final models were selected based on which optimized the value of all fit criteria and class interpretability. Both 2015 and 2018 data supported seven classes in women based on fit and class interpretability; although the AIC and BIC values continued to decrease with the 8-class model, the VLMR p-value became non-significant. For men, a 5-class model was best in 2015. For 2018, the VLMR p-value indicated a better fit for the 4-class model, but other indices pointed to the 5-class model. We chose the 5-class model because it optimized fit statistics while avoiding too-small classes. The LCA class formation fit statistics for 2015 data are in Appendix Table A.
Table 3.
Women and Men model fit indices and class prevalence for exploratory latent class analysis
| Number of Class Prevalences | Log-likelihood | Adjusted BIC | AIC | Entropy | Vuong-Lo-Mendell-Rubin p-value | Class Prevalences (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2018 Women Sample (N=4455) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||
| 1 | −24166 | 48394 | 48355 | 1.00 | - | 100.0 | |||||||
| 2 | −21819 | 43768 | 43687 | 0.77 | 0.00 | 68.4 | 31.6 | ||||||
| 3 | −21340 | 42879 | 42757 | 0.80 | 0.00 | 63.8 | 12.7 | 23.5 | |||||
| 4 | −21048 | 42362 | 42197 | 0.78 | 0.01 | 56.3 | 7.0 | 3. 2 2 | 13.5 | ||||
| 5 | −20833 | 41999 | 41793 | 0.76 | 0.01 | 11.4 | 13.0 | 13.5 | 3. 8 5 | 8.4 | |||
| 6 | −20698 | 41798 | 41550 | 0.77 | 0.00 | 52.1 | 12.6 | 11.6 | 13.5 | 4.2 | 6.0 | ||
| 7 | −20629 | 41728 | 41438 | 0.77 | 0.00 | 10.7 | 4.3 | 4.2 | 12.2 | 4.2 | 50.9 | 13.6 | |
| 8 | −20582 | 41702 | 41370 | 0.75 | 0.18 | 48.4 | 10.2 | 12.2 | 4.2 | 4.1 | 6.5 | 4.2 | 10.2 |
| 2018 Men Sample (N=2228) | |||||||||||||
| 1 | −10012 | 20078 | 20048 | 1.00 | - | 100.0 | |||||||
| 2 | −9019 | 18151 | 17843 | 0.78 | 0.00 | 75.1 | 24.9 | ||||||
| 3 | −8884 | 939 | 8374 | 0.69 | 0.00 | 61.0 | 14.0 | 25.1 | |||||
| 4 | −8755 | 17740 | 17611 | 0.71 | 0.00 | 56.4 | 12.9 | 23.3 | 7.4 | ||||
| 5 | −8656 | 17603 | 17441 | 0.76 | 0.11 | 60.2 | 11.8 | 13.6 | 7.6 | 6.9 | |||
| 6 | −8611 | 17571 | 3677 | 0.77 | 0.05 | 59.1 | 13.2 | 13.5 | 6.6 | 3.8 | 3.8 | ||
LCA Class Description
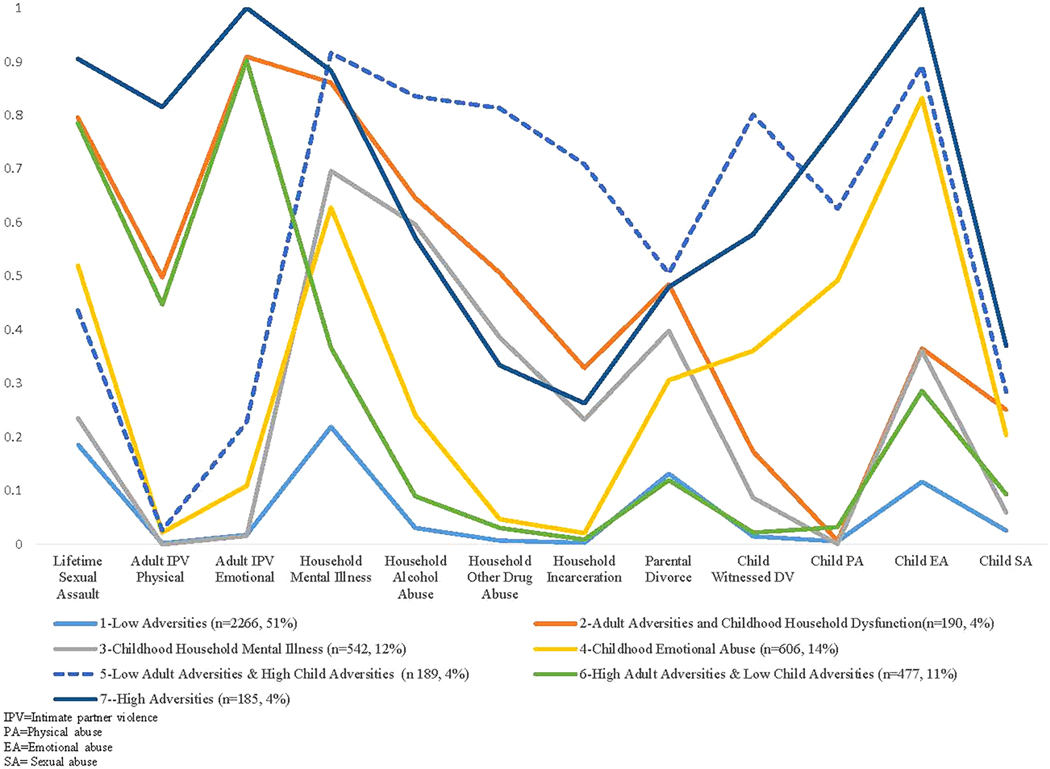
Figure 1 graphically represents item endorsement probabilities for each of the seven classes in the 2018 female sample. A class was interpreted to be homogenous with regard to an item when that item’s response probability was >.70 or <.30.(Masyn, 2015) Class 1,“Low Adversities,” (51% of sample) was characterized by low endorsement of all adversities. Class 2, “Adult Adversities and Childhood Household Dysfunction,” was characterized by high endorsements of lifetime sexual assault (response probability=.80), adult intimate partner emotional abuse (.91), and childhood household mental illness (.86). Classes 3 and 4 were each identified by a single adversity, “Childhood Household Mental Illness” (.70), and “Childhood Emotional Abuse” (.83), respectively. Class 5, “Low Adult Adversities and High Child Adversities,” was characterized by low endorsement of adult adversities and high endorsement of childhood household mental illness (.92), childhood household alcohol abuse (.84), childhood household other drug abuse (.81), childhood household incarceration (.71), child witnessed domestic violence (.80), and childhood emotional abuse (.89). Class 6, “High Adult Adversities and Low Child Adversities,” was characterized by low endorsement of childhood adversities but high endorsement of lifetime sexual assault (.79) and adult intimate partner emotional abuse (.90). Lastly, Class 7, “High Adversities,” was characterized by overall high endorsement across both childhood and adulthood adversities including childhood physical abuse (.78), childhood emotional abuse (1.0), childhood household mental illness (.88), lifetime sexual assault (.91), adult intimate partner physical abuse (.82), adult intimate partner emotional abuse (1.0). Findings for women in 2015 and 2018 replicated well (Appendix Figure A.1), as indicated by nearly identical response probabilities across years for five classes, with a sixth-class meeting replication criteria using the partial boundary model. One class did not replicate well: In 2015, Class 2 was characterized by lifetime sexual assault only, whereas in 2018 the class included sexual assault with other adult adversities and childhood household dysfunction.
Figure 1.
Model-estimate, Class Specific Item Probabilities Profile Plot for the Seven-Class Model in the 2018 Women (% of sample)
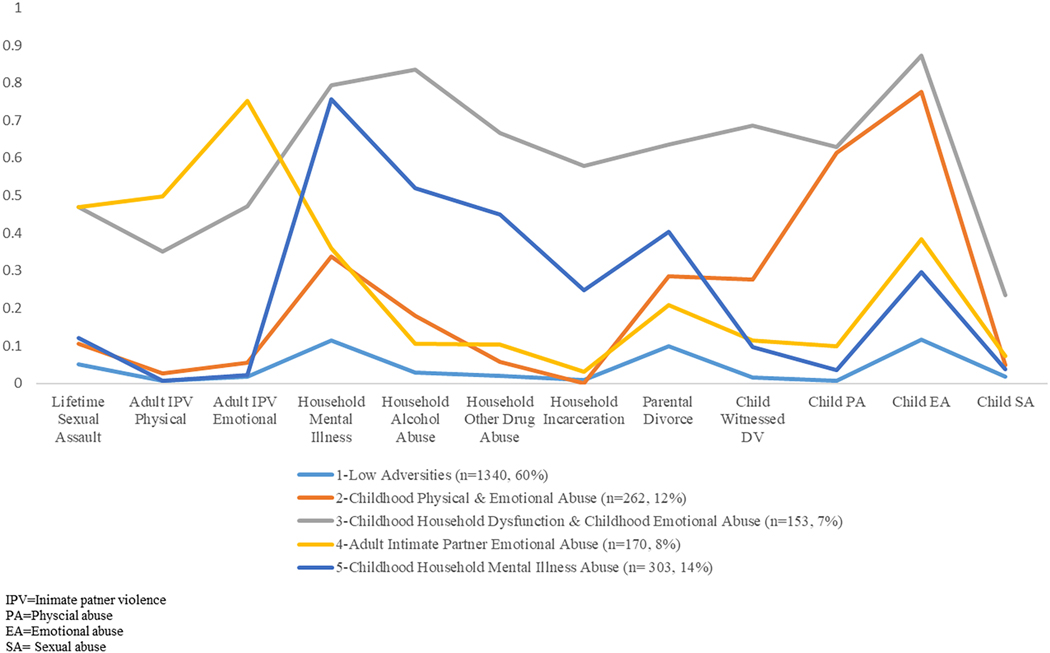
Figure 2 graphically represents item endorsement probabilities for the five classes in the 2018 male sample. Class 1, “Low Adversities,” (60% of sample) was characterized by low endorsement of all the adversities. Class 2 “Childhood Emotional Abuse,” was characterized by high endorsement of child emotional abuse (.78). Class 3, “Childhood Household Dysfunction and Childhood Emotional Abuse,” was characterized by childhood household mental illness (.79), childhood household alcohol abuse (.84), and childhood emotional abuse (.87). Notably, Class 3 showed relatively high endorsement of low-prevalence experiences such as childhood household drug abuse (.67), and child witnessed domestic violence (.69). Class 4 and Class 5 were each distinguished by a single adversity: “Adult Intimate Partner Emotional Abuse” (.75) and “Childhood Household Mental Illness” (.76), respectively. The 5-class model replicated well across the 2015 and 2018 men’s sample. Appendix Figure A.2 has details on the class-specific item response probabilities for the five-class model in the 2015 men’s sample.
Figure 2.
Model-estimate, Class Specific Item Probabilities Profile Plot for the Five-Class Model in the 2018 Men (% of sample)
BMI and Obesity by Class
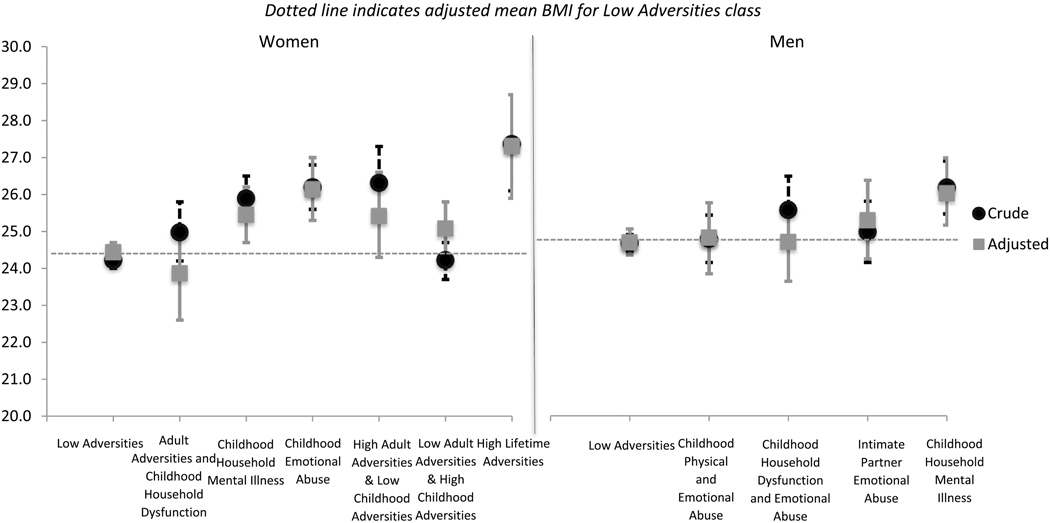
Figure 3 displays crude and adjusted mean BMI scores by latent class in the 2018 samples. Overall, after adjustment, there was a stronger association of adversity classes with BMI in women compared to men. In women, adjusted BMIs ranged from 23.9 kg/m2 (“Adult Adversities and Childhood Household Dysfunction”; 95% CI: 22.6–25.1) to 27.3 kg/m2 in the highest-BMI class (“High Lifetime Adversities”; 95% CI: 25.9–28.7), a statistically significant difference of approximately 3 kg/m2. In men, the adjusted BMIs ranged from 24.6 kg/m2 (“Low Adversity Class”; 95% CI: 24.3–25.0) to 26.0 kg/m2 (“Childhood Household Mental Illness”; 95% CI: 25.1–26.9), a difference of less than 1.5 kg/m2 that was statistically significant. Significant differences between classes for men and women are presented in Appendix Table B; in the figures, a qualitative indication of statistically different estimates are indicated when the confidence intervals of one class do not overlap with the point estimate of another class.
Figure 3.
Crude and Adjusted BMI (kg/m2) by Latent Class in the 2018 Sample
Dotted line indicates adjusted mean BMI for Low Adversities class
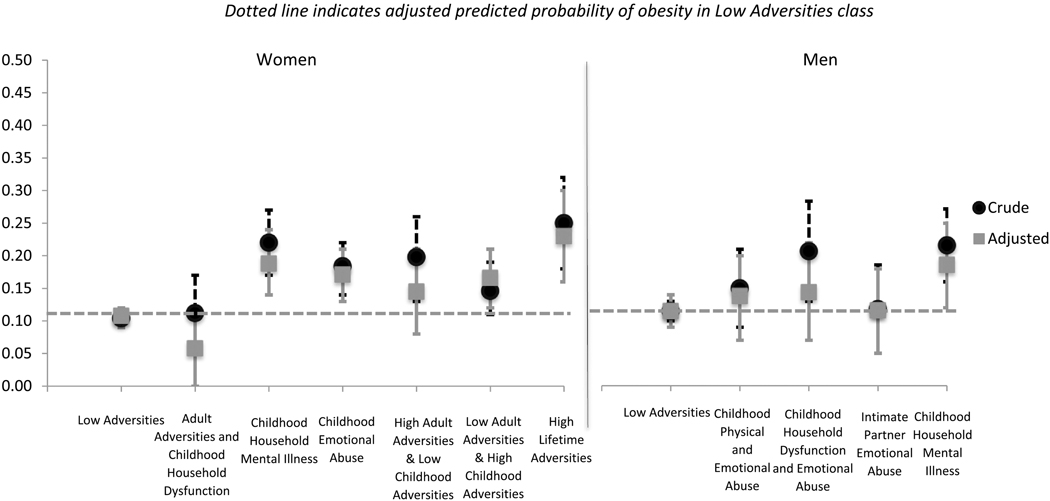
Figure 4 displays the crude and adjusted predicted probabilities (PPs) of obesity (BMI ≥30 kg/m2) by latent class in women and men. In women, the adjusted PP of obesity was lowest among the “Adult Adversities and Childhood Household Dysfunction” class (PP=6%, 95% CI: 0%−11%), followed by the “Low Adversities” class (PP=11%, 95% CI: 9%−12%), and highest among the “High Adversities” class (PP=23%, 95% CI: 16%−30%). These PPs represent a statistically significant range of 17 percentage points from lowest to highest obesity class. In men, the “Adult Intimate Partner Emotional Abuse” class and the “Low Adversities” class both had the lowest PPs of obesity (PP=12%, 95% CI: 5%−18%; PP=12%, 95% CI: 9%−14%, respectively). The highest predicted probability was found in “Childhood Household Mental Illness” at 19% (95% CI: 12%−25%), a statistically significant difference of 7 percentage points. Appendix Table C shows the parallel 2015 results for BMI and obesity by class. Lastly, the supplementary analysis among only those with no PTSD shows similar patterns and magnitudes of association.
Figure 4.
Crude and Adjusted Predicted Probabilities of Obesity by Latent Class in 2018 Sample
Dotted line indicates adjusted predicted probability of obesity in Low Adversities class
DISCUSSION
The goals of this study were to understand how child and adult adversities cluster together and how resulting classes relate to BMI and obesity in emerging adulthood (18–25 years). The LCA provided meaningful and interpretable classes that replicated well in men and women across two samples. Our analyses built on prior work by including childhood and adulthood adversities, which allowed identification of adversity clustering over time. For example, in women, the class characterized by adversities in both childhood and adulthood had a very high probability of childhood emotional abuse, indicating that emotional abuse in childhood may make women particularly vulnerable to later adverse events. In contrast, high childhood household mental illness and household drug use did not appear to cluster with adult adversity in women.
Adversities were strongly associated with BMI and obesity, particularly in women. Prior research has documented associations between ACEs and weight.(Waehrer et al., 2020) These adversities may be related to weight via behavioral and/or biological mechanisms. Biologically, it is possible that adversities trigger a parasympathetic response impacting cortisol and other stress hormones that may increase weight.(Geiker et al., 2018) It may be that adversities reduce capacity for affect regulation (the ability to cope with distress), leading to obesity-promoting behaviors that are soothing or numbing, like overeating highly palatable foods that trigger dopaminergic reward responses.(Cammack et al., 2020; Corwin et al., 2011; Dallman et al., 2003; Pecoraro et al., 2004) The reasons for gender differences in these relationships are unknown. It is possible that these mechanisms are more prominent in women than men, due to social norms around food, differences in biology, and the well-established correlation between sexual abuse and eating disorders, which some survivors report are an attempt to avert sexual attention.(Molendijk et al., 2017) It is possible that, due to their greater metabolic activity, men at this age are buffered against obesogenic impacts of maladaptive eating behaviors. At least one prior study found a stronger association between trauma and BMI in older men, indicating there may be a lagged effect in men.(Smith et al., 2015)
Prior studies have generally used the cumulative ACE score to characterize individuals’ exposure to adversities.(Felitti et al., 1998) These studies have consistently found a stepwise increase in BMI, or prevalence of overweight/obesity, with increasing number of ACEs.(Dallman et al., 2003) In women, the differences in BMI identified across the lowest-BMI and highest-BMI classes in our analysis appeared to be larger than most documented in prior literature using cumulative ACE scores.(Hughes et al., 2017) Using LCA appears to have identified small classes at very high obesity risk.
This study is not without limitations. First, self-report survey data were used for all measures; thus, there may be measurement error in adversities and BMI. However, because self-reported BMI is highly correlated with measured BMI(McAdams et al., 2007), for population research, self-reported BMI is generally considered acceptable. With regard to measurement of adversities, there is no gold standard against which to measure retrospective self-report, as prospective measurements during adulthood or childhood (e.g., from parents) or objective records (e.g., child protection records) are difficult to obtain and likely suffer from under- and/or biased reporting.(Reuben et al., 2016) Retrospective self-report, although imperfect, is therefore considered standard in population research. Further, interventions addressing ACEs in emerging adults will likely rely on retrospective self-report; thus our approach is optimal for informing practice. Second, the CSHS had response rates of 32% and 37% in 2015 and 2018, respectively. Although these response rates are not ideal, they are higher than other similar surveys in emerging adults.(American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2015, 2015) The low response rate may particularly affect external validity. Thus, it is important to replicate these findings across other data sources. Third, the sample is only representative of college students in Minnesota, and may differ from the general public; for example, rates of traumatic events may be lower in our sample than in the general population.(Metzler et al., 2017) Finally, due to the cross-sectional nature of this study, there is no way to determine the temporal order of the relations among variables. In addition, the combination of last 12-month and lifetime adult adversities, which was necessary to obtain adequate endorsement, but limits the ability to estimate different associations of more versus less recent events with BMI and obesity. Other types of adversities (e.g., natural disasters) were not captured in our study. Given the dearth of population-based data on this age group, tolerance for these types of data limitations are necessary.
Despite these limitations, this study is novel in several ways. First, to our knowledge, this is the first study to examine relationships between classes of lifetime adversity and BMI/obesity in emerging adults. Second, stratifying our analyses by gender adds a nuanced understanding of how lifetime adversities are associated with weight status for men and women. Finally, by replicating our findings in two large samples, we were able to ensure that findings of this data-driven approach were not driven solely by variations in the data.
In conclusion, our findings have implications for future research and interventions. Our findings are consistent with other research suggesting adversities are associated with BMI and obesity particularly in women, highlighting the need to address adversity exposure in obesity prevention approaches. Interventions are available to address psychological and behavioral aspects of hypothesized pathways between adversity and obesity (e.g., online interventions reducing psychological distress in those exposed to violence(Gilmore et al., 2019)). Thus, a promising focus of future research is identifying the optimal combination of intervention components to reduce adversity-related obesity, and tailoring these components based on the specific adversities an individual has experienced. This study represents a step toward a tailored approach by identifying specific classes of adversities most associated with elevated BMI and obesity. Given that PTSD may mediate the relationship between adversities and health,(Schnurr and Green, 2004) future longitudinal studies are needed to identify the psychological, behavioral, and biological factors that are on the pathway from specific adversities to weight outcomes.(Mason et al., 2016) Because adversities are highly prevalent, strategies to prevent adversities themselves, as well as appropriate treatments to improve the well-being of individuals who have experienced adversities, are critically needed.
Supplementary Material
Highlights.
Latent Class Analyses identified 7 classes in women and 5 classes in men
Adult adversities clustered with child emotional abuse and household mental illness
A difference between the lowest-BMI and highest-BMI classes was 3.4 kg/m2 in women
A difference between the lowest-BMI and highest-BMI classes was 1.4 kg/m2 in men
Acknowledgments
Funding: This study was funded by Grant R21DK117466 from the National Institute for Diabetes and Digestive and Kidney Diseases (NIDDK). The authors gratefully acknowledge additional support from the Minnesota Population Center (P2C HD041023) and the Interdisciplinary Population Health Science Training Program (T32HD095134) funded through a grant from the Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD). The study sponsors had no involvement in the study design, collection, analysis, interpretation of data, writing, or decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2015, 2015. . Hanover, MD. [Google Scholar]
- Arnett JJ, 2000. Emerging adulthood: A theory of development from the late teens through the twenties. Am. Psychol. 55, 469–480. 10.1037/0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- Asparouhov T, Muthén B, 2015. Residual Associations in Latent Class and Latent Transition Analysis, Structural Equation Modeling. 10.1080/10705511.2014.935844 [DOI] [Google Scholar]
- Asparouhov T, Muthén BO, 2014. Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary second model. Mplus Web Notes 1–22. [Google Scholar]
- Assink M, Spruit A, Schuts M, Lindauer R, van der Put CE, Stams G-JJJM, 2018. The intergenerational transmission of child maltreatment: A three-level meta-analysis. Child Abus. Negl. 84, 131–145. 10.1016/j.chiabu.2018.07.037 [DOI] [PubMed] [Google Scholar]
- Behavioral Risk Factor Surveillance System ACE Data |Violence Prevention|Injury Center|CDC [WWW Document], 2019. URL https://www.cdc.gov/violenceprevention/childabuseandneglect/acestudy/ace-brfss.html (accessed 3.8.20).
- Berzenski SR, Yates TM, 2011. Classes and Consequences of Multiple Maltreatment : A Person-Centered Analysis. Child Maltreat. 16, 250–261. 10.1177/1077559511428353 [DOI] [PubMed] [Google Scholar]
- Cammack AL, Gazmararian JA, Suglia SF, 2020. History of child maltreatment and excessive dietary and screen time behaviors in young adults: Results from a nationally representative study. Prev. Med. (Baltim). 139, 106176. 10.1016/j.ypmed.2020.106176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh CE, Petras H, Martins SS, 2015. Gender-specific profiles of adverse childhood experiences, past year mental and substance use disorders, and their associations among a national sample of adults in the United States. Soc. Psychiatry Psychiatr. Epidemiol. 1257–1266. 10.1007/s00127-015-1024-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charak R, Villarreal L, Schmitz RM, Hirai M, Ford JD, 2019. Patterns of childhood maltreatment and intimate partner violence, emotion dysregulation, and mental health symptoms among lesbian, gay, and bisexual emerging adults: A three-step latent class approach. 10.1016/j.chiabu.2019.01.007 [DOI] [PubMed] [Google Scholar]
- Cheng HL, Medlow S, Steinbeck K, 2016. The Health Consequences of Obesity in Young Adulthood. Curr. Obes. Rep. 5, 30–37. 10.1007/s13679-016-0190-2 [DOI] [PubMed] [Google Scholar]
- Classes of adverse experiences and their associations with body weight and obesity in emerging adulthood [WWW Document], 2020. . Cent. Open Sci. URL https://osf.io/wgj2k/?view_only=8a80715fcc4740d9a15e69e233ff6ac1 (accessed 12.11.20). [Google Scholar]
- Corwin RL, Avena NM, Boggiano MM, 2011. Feeding and reward: perspectives from three rat models of binge eating. Physiol. Behav. 104, 87–97. 10.1016/j.physbeh.2011.04.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallman MF, Pecoraro N, Akana SF, La Fleur SE, Gomez F, Houshyar H, Bell ME, Bhatnagar S, Laugero KD, Manalo S, 2003. Chronic stress and obesity: A new view of “comfort food.” Proc. Natl. Acad. Sci. U. S. A. 100, 11696–11701. 10.1073/pnas.1934666100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danese A, Tan M, 2014. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry 19, 544–554. 10.1038/mp.2013.54 [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS, 1998. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. Am. J. Prev. Med. 14, 245–258. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod RK, Turner HA, 2007. Poly-victimization: A neglected component in child victimization. Child Abus. Negl. 31, 7–26. 10.1016/j.chiabu.2006.06.008 [DOI] [PubMed] [Google Scholar]
- Garraza LG, Azur M, Stephens RL, Walrath CM, 2011. Gender differences in patterns of child risk across programmatic phases of the CMHI: A multiple group latent class analysis (LCA). J. Behav. Heal. Serv. Res. 38, 265–277. 10.1007/s11414-010-9219-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geiker NRW, Astrup A, Hjorth MF, Sjödin A, Pijls L, Markus CR, 2018. Does stress influence sleep patterns, food intake, weight gain, abdominal obesity and weight loss interventions and vice versa? Obes. Rev. 10.1111/obr.12603 [DOI] [PubMed] [Google Scholar]
- Gilmore AK, Walsh K, Frazier P, Meredith L, Ledray L, Davis J, Acierno R, Ruggiero KJ, Kilpatrick DG, Jaffe AE, Resnick HS, 2019. Post-Sexual Assault Mental Health: A Randomized Clinical Trial of a Video-Based Intervention. J. Interpers. Violence 886260519884674. 10.1177/0886260519884674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-Larsen P, Adair LS, Nelson MC, Popkin BM, 2004. Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. Am. J. Clin. Nutr. 80, 569–75. [DOI] [PubMed] [Google Scholar]
- Guo Y, Yue X, Li H, Song Z, Yan H, Zhang P, Gui Y, Chang L, Li T, 2016. Overweight and Obesity in Young Adulthood and the Risk of Stroke: a Meta-analysis. J. Stroke Cerebrovasc. Dis. 25, 2995–3004. 10.1016/j.jstrokecerebrovasdis.2016.08.018 [DOI] [PubMed] [Google Scholar]
- Health and Health-Related Behaviors 2015. College Student Health Survey Report 2015 College Student Health Survey Report, n.d. . Minneapolis. [Google Scholar]
- Health and Health-Related Behaviors 2018. College Student Health Survey Report [WWW Document], n.d. [Google Scholar]
- Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, Miller AH, Nemeroff CB, 2000. Pituitary-adrenal and automatic responses to stress in women after sexual and physical abuse in childhood. J. Am. Med. Assoc. 284, 592–597. 10.1001/jama.284.5.592 [DOI] [PubMed] [Google Scholar]
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Jones L, Dunne MP, 2017. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Heal. 2, e356–e366. 10.1016/S2468-2667(17)30118-4 [DOI] [PubMed] [Google Scholar]
- Lane PW, Nelder JA, 1982. Analysis of Covariance and Standardization as Instances of Prediction. Biometrics 38, 613–621. [PubMed] [Google Scholar]
- Lanza ST, Tan X, Bray BC, 2013. Latent Class Analysis With Distal Outcomes: A Flexible Model-Based Approach. Struct. Equ. Model. 20, 1–26. 10.1080/10705511.2013.742377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lünnemann MKM, Horst F.C.P.V. der, Prinzie P, Luijk MPCM, Steketee M, 2019. The intergenerational impact of trauma and family violence on parents and their children. Child Abus. Negl. 96. 10.1016/j.chiabu.2019.104134 [DOI] [PubMed] [Google Scholar]
- Mason SM, Bryn Austin S, Bakalar JL, Boynton-Jarrett R, Field AE, Gooding HC, Holsen LM, Jackson B, Neumark-Sztainer D, Sanchez M, Sogg S, Tanofsky-Kraff M, Rich-Edwards JW, 2016. Child maltreatment’s heavy toll: The need for trauma-informed obesity prevention. Am. J. Prev. Med. 50, 646–649. 10.1016/j.amepre.2015.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masyn KE, 2015. Latent Class Analysis and Finite Mixture Modeling Oxford Handbooks Online Latent Class Analysis and Finite Mixture Modeling Latent Class Analysis and Finite Mixture Modeling. 10.1093/oxfordhb/9780199934898.013.0025 [DOI]
- McAdams MA, Van Dam RM, Hu FB, 2007. Comparison of self-reported and measured BMI as correlates of disease markers in U.S. adults. Obesity 15, 188–196. 10.1038/oby.2007.504 [DOI] [PubMed] [Google Scholar]
- Menard C, Bandeen-Roche KJ, Chilcoat HD, 2004. Epidemiology of multiple childhood traumatic events: Child abuse, parental psychopathology, and other family-level stressors. Soc. Psychiatry Psychiatr. Epidemiol. 39, 857–865. 10.1007/s00127-0040868-8 [DOI] [PubMed] [Google Scholar]
- Merians AN, Baker MR, Frazier P, Lust K, 2019. Outcomes related to adverse childhood experiences in college students: Comparing latent class analysis and cumulative risk. Child Abus. Negl. 87, 51–64. 10.1016/j.chiabu.2018.07.020 [DOI] [PubMed] [Google Scholar]
- Metzler M, Merrick MT, Klevens J, Ports KA, Ford DC, 2017. Adverse childhood experiences and life opportunities: Shifting the narrative. Child. Youth Serv. Rev. 72, 141–149. 10.1016/j.childyouth.2016.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molendijk ML, Hoek HW, Brewerton TD, Elzinga BM, 2017. Childhood maltreatment and eating disorder pathology: A systematic review and dose-response meta-analysis. Psychol. Med. 47, 1402–1416. 10.1017/S0033291716003561 [DOI] [PubMed] [Google Scholar]
- Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA, 2008. Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity. 10.1038/oby.2008.365 [DOI] [PubMed] [Google Scholar]
- Noll JG, Zeller MH, Trickett PK, Putnam FW, 2007. Obesity risk for female victims of childhood sexual abuse: a prospective study. Pediatrics 120, e61–7. 10.1542/peds.2006-3058 [DOI] [PubMed] [Google Scholar]
- Nylund-Gibson K, Choi AY, 2018. Ten frequently asked questions about latent class analysis. Transl. Issues Psychol. Sci. 4, 440–461. 10.1037/tps0000176 [DOI] [Google Scholar]
- Pecoraro N, Reyes F, Gomez F, Bhargava A, Dallman MF, 2004. Chronic stress promotes palatable feeding, which reduces signs of stress: feedforward and feedback effects of chronic stress. Endocrinology 145, 3754–62. 10.1210/en.2004-0305 [DOI] [PubMed] [Google Scholar]
- Relyea M, Ullman SE, 2017. Predicting Sexual Assault Revictimization in a Longitudinal Sample of Women Survivors : Variation by Type of Assault. Violence Against Women 23, 1462–1483. 10.1177/1077801216661035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuben A, Moffitt TE, Caspi A, Belsky DW, Harrington H, Schroeder F, Hogan S, Ramrakha S, Poulton R, Danese A, 2016. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J. Child Psychol. Psychiatry Allied Discip. 57, 1103–1112. 10.1111/jcpp.12621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roehrkasse AF, Wildeman C, 2019. Administrative data and long-term trends in child maltreatment: the prospects and pitfalls. Lancet Public Heal. 10.1016/S24682667(19)30022-2 [DOI] [PubMed] [Google Scholar]
- Schmiege SJ, Masyn KE, Bryan AD, 2018. Confirmatory Latent Class Analysis: Illustrations of Empirically Driven and Theoretically Driven Model Constraints. Organ. Res. Methods 21, 983–1001. 10.1177/1094428117747689 [DOI] [Google Scholar]
- Schnurr PP, Green BL, 2004. Understanding relationships among trauma, post-tramatic stress disorders, and health outcomes. Adv. Mind. Body. Med. 20, 18–29. 10.1037/10723-010 [DOI] [PubMed] [Google Scholar]
- Shin SH, McDonald SE, Conley D, 2018a. Patterns of adverse childhood experiences and substance use among young adults: A latent class analysis. Addict. Behav. 78, 187–192. 10.1016/j.addbeh.2017.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin SH, McDonald SE, Conley D, 2018b. Profiles of adverse childhood experiences and impulsivity. Child Abus. Negl. 85, 118–126. 10.1016/j.chiabu.2018.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith-Marek EN, Cafferky B, Dharnidharka P, Mallory AB, Dominguez M, High J, Stith SM, Mendez M, 2015. Effects of Childhood Experiences of Family Violence on Adult Partner Violence: A Meta-Analytic Review. J. Fam. Theory Rev. 7, 498–519. 10.1111/jftr.12113 [DOI] [Google Scholar]
- Smith BN, Tyzik AL, Neylan TC, Cohen BE, 2015. PTSD and obesity in younger and older veterans: Results from the mind your heart study. Psychiatry Res. 229, 895–900. 10.1016/j.psychres.2015.07.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Te Morenga L, Mallard S, Mann J, 2013. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ 346, e7492. 10.1136/bmj.e7492 [DOI] [PubMed] [Google Scholar]
- Turner HA, Finkelhor D, Ormrod R, 2010. Poly-Victimization in a National Sample of Children and Youth. Am. J. Prev. Med. 38, 323–330. 10.1016/j.amepre.2009.11.012 [DOI] [PubMed] [Google Scholar]
- Twig G, Afek A, Derazne E, Tzur D, Cukierman-Yaffe T, Gerstein HC, Tirosh A, 2014. Diabetes Risk Among Overweight and Obese Metabolically Healthy Young Adults. Diabetes Care 37, 2989–2995. 10.2337/dc14-0869 [DOI] [PubMed] [Google Scholar]
- Waehrer GM, Miller TR, Marques SCS, Oh DL, Harris NB, 2020. Disease burden of adverse childhood experiences across 14 states. PLoS One 15, 1–18. 10.1371/journal.pone.0226134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Wang X, 2012. Structural Equation Modeling: Applications Using Mplus, Structural Equation Modeling: Applications Using Mplus. Higher Education Press. 10.1002/9781118356258 [DOI] [Google Scholar]
- Williamson DF, Thompson TJ, Anda RF, Dietz WH, Felitti V, 2002. Body weight and obesity in adults and self-reported abuse in childhood. Int. J. Obes. Relat. Metab. Disord. 26, 1075–1082. 10.1038/sj.ijo.0802038 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.