Abstract
Background
The importation of SARS-CoV-2 through air travel poses substantial risks to generate new COVID-19 outbreaks. Timely contact tracing is particularly crucial to limit onwards transmission in settings without established community transmission.
Methods
We conducted an in-depth analysis of the response to a big flight-associated COVID-19 outbreak in Vietnam in March 2020 that involved contact tracing, systematic testing and strict quarantine up to third generation contacts.
Results
183 primary contacts from the flight as well as 1000 secondary and 311 third generation contacts were traced, tested, and quarantined across 15 provinces across Vietnam. The protracted confirmation of the index case at 3 days and 19 h after arrival resulted in isolation/quarantine delays of 6.8 days (IQR 6.3–6.8) and 5.8 days (IQR 5.8–7.0) for primary and secondary cases, respectively, which generated 84.0 and 26.4 person-days of community exposure from primary and secondary cases, respectively. Nevertheless, only 5 secondary cases occurred.
Conclusions
A large flight-related COVID-19 cluster was successfully contained through timely, systematic and comprehensive public health responses despite delayed index case identification. Multiagency collaboration and pre-established mechanisms are crucial for low and middle income countries like Vietnam to limit community transmission after COVID-19 importation through air travel.
Keywords: COVID-19, Case importation, Contact tracing, Cluster containment, Air travel, Vietnam
Abbreviations: NSCPC, National Steering Committee of COVID-19 Prevention and Control; rt-PCR, Reverse transcriptase Polymerase chain reaction
1. Introduction
In March 2020, as the world began to experience the global spread of COVID-19, we detected a large cluster of COVID-19 cases arising from a flight arriving from London, UK to Hanoi, Vietnam at 5.20am on March 2 (flight VN54). A 27-year-old business class passenger who was symptomatic while on board and who tested positive for SARS-CoV-2 four days after arrival in Vietnam on 6 March was identified as index case. In-depth epidemiological investigations revealed in-flight transmission during the 10 h flight duration as the most likely route of transmission [1].
Until then, Vietnam had recorded three minor instances of COVID-19 importation through air travel but no intensive contact tracing for passengers and their contacts was performed. Flight VN54 resulted in the first extensive case finding and contact tracing operations to prevent further transmission in Vietnam. As contact tracing activities have been conducted to find potential exposed passengers on flight with cases of H1N1, SARS, MERS, Tb, and measles, COVID-19 is certainly not an exception for infectious disease on transportation. Mass transmission instances of COVID-19 on flights had been explored and described in previous publications, however, the focus is limited to transmission risk from infected individuals on the flight [2], with criteria of contact trace for 2 or lesser seats from index case. While an infectious person, with an unpredicted novel disease, can still transmit to larger scale of passengers on flight and also more contacts in local settings, contact tracing should not stop at the current boundary of proximity, but to be tested its containment capacity at large. Here we analyze epidemiological characteristics of the flight VN54 cluster and the subsequent containment efforts undertaken among passengers, crew and their contacts to prevent further transmission of SARS-CoV-2 in Vietnam. This work provides valuable information of how to contain COVID-19 importation through air-travel successfully in a low-middle income setting.
2. Methods
2.1. Contact and case definitions
A case of COVID-19 was defined according to the Vietnam Ministry of Health guidelines in place at the time of our investigation [3]. All passengers and crew members on board VN54 flight were considered as primary contacts of the index case. Secondary contacts were defined as persons who had close contacts (≤2 m for ≥ 15 min/in the same closed space, e.g. house, workplace, public transport, during the incubation period) with a primary contact between arrival of flight VN54 to Vietnam and start of isolation or quarantine. Third generation contacts were defined as non-close contacts (>2 m apart/in an open space during the incubation period) with a primary and/or a secondary contact between arrival of flight VN54 to Vietnam and start of isolation or quarantine. Persons testing positive for SARS-CoV-2 using reverse transcriptase Polymerase chain reaction (rt-PCR) were considered primary cases if they arose among primary contacts, secondary cases if they arose among secondary contacts, and third generation cases if they arose among third generation contacts, all regardless of COVID-19 symptoms.
2.2. Case investigation, contact tracing, testing and quarantine
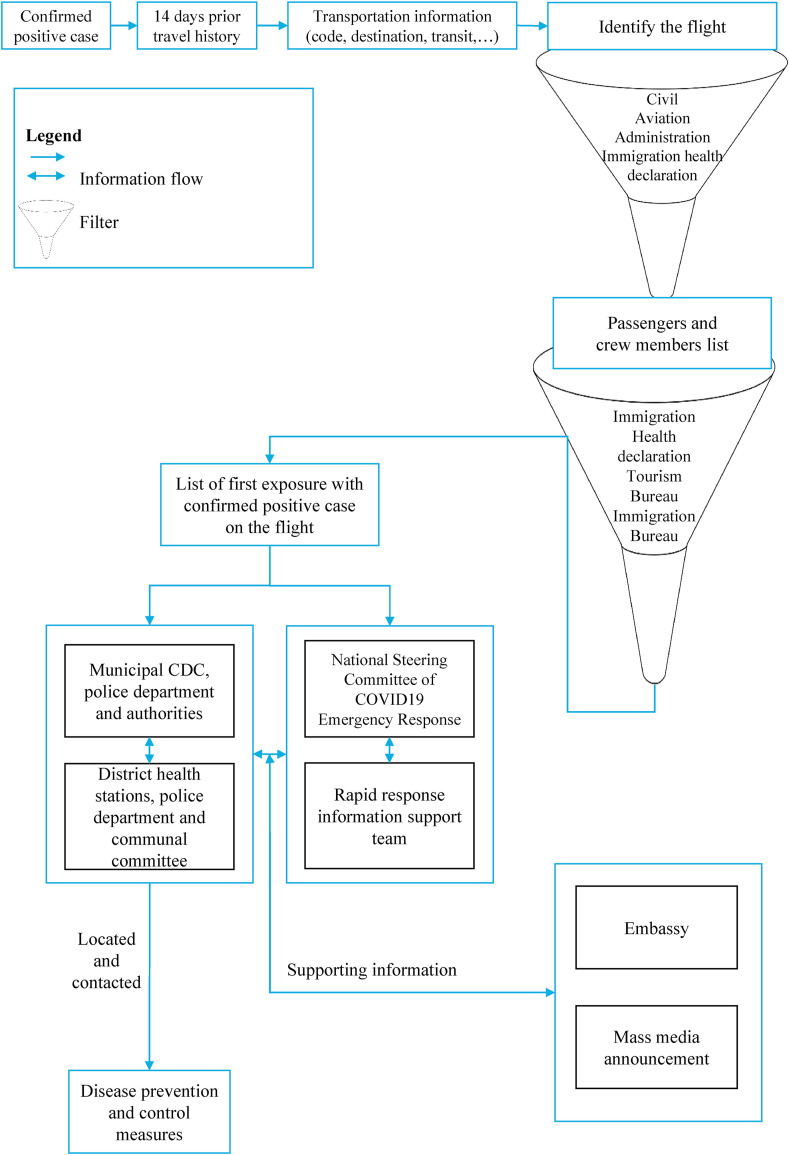
Contact tracing started on the early morning of 6 March, four days after the arrival of flight VN54 in Vietnam. The Ministry of Health and the National Steering Committee for COVID-19 Prevention and Control (NSCPC) were tasked with intensive contact tracing of all flight-related primary and secondary contacts. The flight manifest was obtained from the Immigration Bureau and the Vietnam Civil Aviation Administration on the same day. The passenger list was distributed to relevant provincial Center of Disease Control for contact tracing. At provincial levels, local health staffs cooperated with local government authorities, social security departments, and local volunteers in order to locate and contact passengers and identify their contacts. Since the majority of passengers were tourists and non-Vietnamese nationals, tourism companies and hotel administrations in all provinces were asked to report the presence of foreign tourists to local authorities and health authorities. Provincial health staff communicated contact tracing status back to NSCPC daily (Fig. 1 ).
Fig. 1.
Contact tracing strategy for primary contacts of VN54 flight in Vietnam.
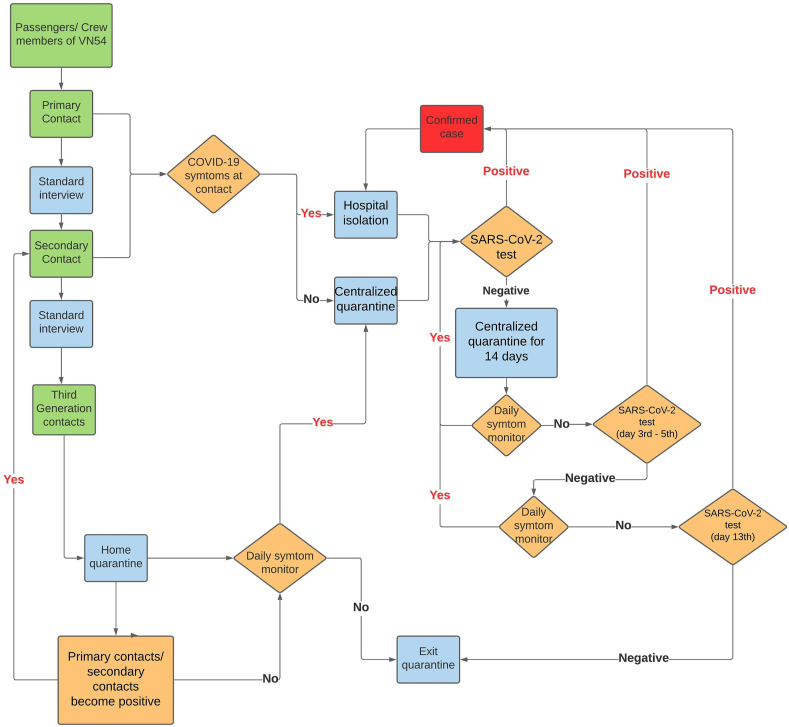
All traced primary contacts who could be reached were interviewed using a standard questionnaire regarding their secondary and third generation contacts since arrival to Vietnam. In addition, they were tested for SARS-CoV-2 and transferred to mandatory 14-day quarantine immediately at centralized facilities, regardless of symptoms and test result. All flight passengers who had already transited out of Vietnam were contacted through border health control authorities at their last traceable destinations. Similar to primary contacts, secondary contacts were traced, tested for SARS-CoV-2, and systematically quarantined for 14 days in centralized facilities (at first). Third generation contacts were asked by local health staffs to quarantine at home for 14 days, with daily symptom monitoring by local health staffs. If their primary or secondary contact became a confirmed case, they would be treated as secondary contacts, i.e. tested and transferred to centralized quarantine immediately.
All persons in centralized quarantine had their symptoms and temperature checked twice daily, and in addition to testing at start of quarantine, they also had oropharyngeal swabs collected after 3–5 days and on day 13 before exiting quarantine. Accommodation, meals, and basic hygiene necessities were provided free of charge under the Ministry of Health's Mandatory Quarantine Scheme. Any person showing COVID-19 symptoms, either at time of being successfully traced by local health staffs or at any point during centralized or home quarantine, got immediately transferred to a reference hospital for isolation and monitoring, as did anyone who got tested positive. Details of contact tracing and testing strategy can be found in Fig. 2 .
Fig. 2.
Testing and quarantine strategy for traceable primary, secondary, and third generation contacts of VN54 flight in Vietnam.
2.3. Laboratory and case management capacity
In response to the increased testing needs resulting from the response to flight VN54, SARS-CoV-2 RT-PCR laboratory testing capacity was quickly scaled up in Vietnam [4]. From relatively limited and centralized testing capacities, within 10 days, over thirty local CDCs and all tertiary level hospitals were enabled to handle up to 1500 tests per day. Similarly, ICU capacity and isolation wards were ramped up in all provincial health facilities, and military-run bases, dormitories, and hotels were repurposed as centralized quarantine facilities. At designated COVID-19 hospitals, infection control measures were strengthened, including strict visitor controls, triage of patients with pneumonia or other symptoms of respiratory infection, hand hygiene and mask wearing requirements, and maintenance of strict infection control practices with personal protective equipment. Healthcare workers at these designated hospitals were required to avoid non-essential travel outside of hospitals. All confirmed COVID-19 cases were isolated in designated COVID-19 hospitals, and received treatment free-of-charge until confirmation of SARS-CoV-2 clearance as per Vietnam Ministry of Health's criteria.
2.4. Border control measures
Since mid-January, the Government of Vietnam implemented temperature screening for all international passengers (air and land) arriving in Vietnam. At the time of flight VN54, all passengers with a history of travel to Mainland China, Hong Kong, Taiwan (from 1 February), South Korea (from 24 February), Iran and Italy (from 28 February) had to undergo compulsory SARS-CoV-2 testing and quarantine. There was no requirement to wear masks on board commercial flights at that time. Since VN54 departed in the UK, which was not covered by this policy at that time, none of its passengers got tested and/or quarantined upon arrival.
2.5. Non pharmaceutical measures
At time of arrival of flight VN54, targeted lock-downs around locations with confirmed COVID-19 cases, such as hospital wards, resident buildings, hotels, etc. Were the population-level method of choice in response to a newly confirmed cases. In addition, anonymized information about newly confirmed COVID-19 cases and newly identified clusters were shared publicly through mass media and official governmental websites by NSCPC. Once the index case on flight VN54 got confirmed, official messages calling for all passengers and crew members on that flight to seek medical services were broadcasted daily on mass media nationwide. Regular hand washing, mask wearing, and social distancing was encouraged. At the same time, the NSCPC monitored the media landscape for misinformation. Schools and universities in Vietnam were already closed since February, and mass gatherings were mostly canceled. At most workplaces, temperature screening, health and international travel history monitoring were already in place. Mask wearing policies were turned from mandatory for high-risk workers (healthcare workers, essential workers) into mandatory in public places [5].
2.6. Ethics
This analysis was approved and exempted for ethics by the National Institute of Hygiene as a part of national COVID-19 outbreak investigation and response activities.
3. Results
A total of 16 crew members and 201 passengers were on board flight VN54, with 71.6% (n = 144) of passengers being foreigners, while 93.7% (n = 15) of crew members were Vietnamese (Table 1 ). Contact tracing for primary contacts of the flight was completed on 10 March (eight days after the flight arrival; four days after contact tracing initiation). All of the 167 (83.1%) passengers and the 16 (100%) crew members who were still in the country at that time were successfully traced. The remaining 33 passengers transited to other countries (Table 1).
Table 1.
Demographic information and tracing outcomes for passengers and crew members of flight VN54.
| Passengers (N = 201) (n, %) | Crew members (N = 16) (n, %) | |
|---|---|---|
| Nationality | ||
| Vietnamese | 33 (16.4) | 15 (93.7) |
| British | 144 (71.6) | 0 (0) |
| Other | 24 (11.9) | 1 (6.3) |
| Contact tracing status | ||
| Traced | 168 (83.6) | 16 (100) |
| Transited | 33 (16.4) | 0 (0) |
By 13 March (11 days after arrival; seven days after contact tracing initiation), we had identified a total of 1000 secondary contacts, who were all placed into centralized quarantine facilities, and 311 third generation contacts, who were asked to self-quarantine at their homes for 14 days.
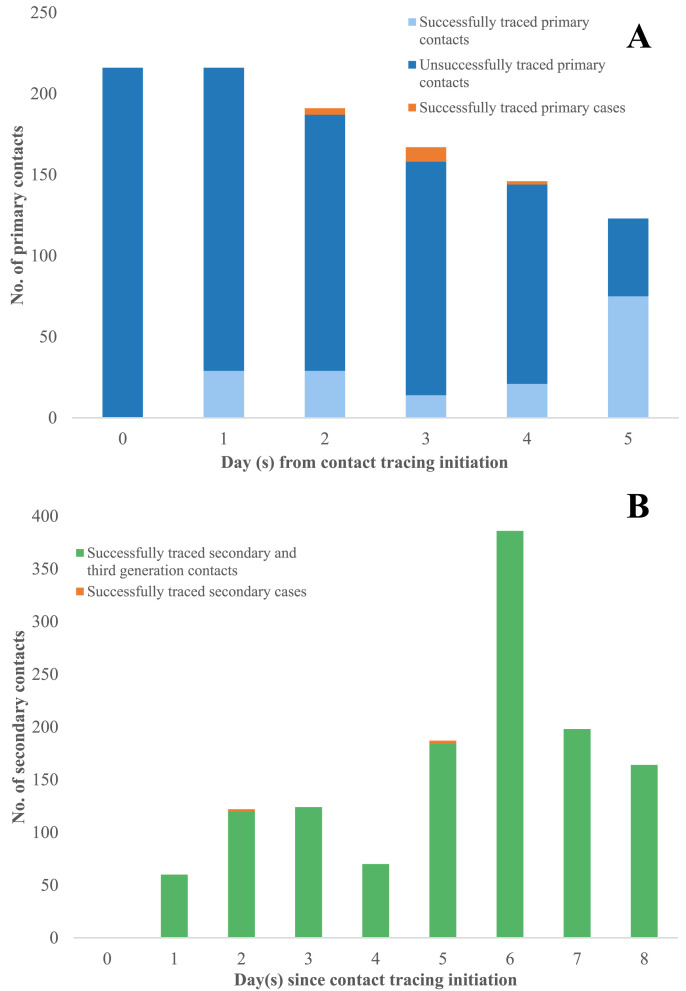
Tracing activities for primary, secondary, and third generation contacts is illustrated in Fig. 3 . The majority of primary and secondary contacts were traced and quarantined/isolated four to five days after the index case confirmation. For primary contacts, the median duration from flight arrival to start of quarantine was 5.8 days (Interquartile range - IQR 4.8–6.8), while the median time from index case confirmation to start of quarantine was 2.0 days (IQR 1.0–3.0) (Table 2 ). These data were not available for secondary and third generation contacts.
Fig. 3.
Time course for contact tracing of primary, secondary, and third generation contacts of VN54 flight in Vietnam.
Table 2.
Containment delays and epidemiological profiles of primary contacts, primary cases and secondary cases resulting from the VN54 cluster.
| Time interval | Primary contactsa (N = 183) | Primary cases (N = 15) | Secondary cases (N = 5) |
|---|---|---|---|
| Index case confirmation to isolation/quarantine (median, IQR) (days) | 2.0 (1.0–3.0) | 3.0 (2.5–3.0) | 2.0 (2.0–5.1) |
| Last exposure to isolation/quarantine (median, IQR) (days) | 5.8 (4.8–6.8) | 6.8 (6.3–6.8) | 5.8 (5.8–7.0) |
| Last exposure to symptom onset (median, IQR) (days) | – | 10.8 (6.6–15.1) | 4.8 (4.0–4.8) |
| Cumulative duration of community exposure (person-days) | – | 84.0 | 26.4 |
| Cumulative duration of symptomatic community exposure (person-days) | – | 4.0 | 7.0 |
| Case categories (n, %) | |||
| Symptomatic | – | 3 (20) | 4 (80) |
| Pre-symptomatic | – | 7 (47) | 1 (20) |
| Asymptomatic | – | 5 (33) | 0 |
Note: Data for secondary contacts were not available.
All flight passengers and staff who were still in Vietnam at time of contact tracing initiation.
Among primary contacts, we identified 15 primary COVID-19 cases in addition to the index case, of which 14 were passengers and one was a crew member. One of the passenger cases had already transited to Cambodia, where she was identified, tested, and confirmed for SARS-CoV-2 infection by the Cambodia Center of Disease Control. On-board transmission during the 10-h flight duration was found to have been the most likely route of transmission for these primary cases [1]. Subsequently, five secondary cases emerged among secondary contacts of four primary cases. Of these, three were family members of primary cases, one was a local tourist operator and one was a saleswoman who had contact with primary cases. No third generation cases were reported.
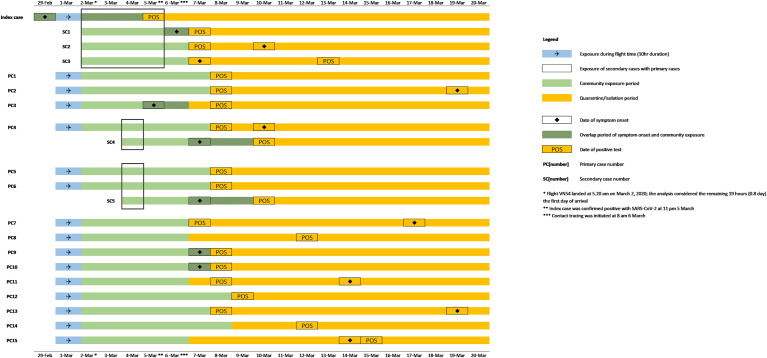
Fig. 4 and Table 2 shows the temporal sequence of exposure, symptom onset and isolation for primary and secondary cases. The index case, who was symptomatic during the flight, presented at a health facility in Hanoi on 5 March (three days after landing) and received a nasopharyngeal swab. The laboratory test result was reported positive at 11pm the same day (5 March), and the index case was immediately isolated (3 days and 19 h after arrival). Contact tracing was only started the following morning at 8 a.m. on 6 March (4 days and 3 h after arrival of the flight).
Fig. 4.
Temporal sequence of exposure, symptom onset and isolation for all primary and secondary cases of VN54 flight in Vietnam.
Consequently, for primary cases, the median duration between last exposure (arrival of the flight) and start of isolation/quarantine was 6.8 days (IQR 6.3–6.8), of which the delay from index case confirmation to isolation/quarantine was 3.0 days (IQR 2.5–3.0). The equivalent delays for secondary cases were 5.8 days (IQR 5.8–7.0) (from last exposure to their epi-linked primary cases) and 2.0 days (IQR 2.0–5.1), respectively (Table 2). Among the remaining 15 primary cases who got infected by the index case during the flight, 10 (67%) subsequently developed symptoms, of which three developed symptoms before being isolated. This resulted in a total of 84.0 person-days of community exposure, of which 4.0 person-days were symptomatic community exposure (6.8 days if the index case is included). The median time interval from last exposure to symptom onset was 10.8 days (IQR 6.6–15.1) for primary cases. Transmission occurred from three primary cases during symptomatic, pre-symptomatic, and asymptomatic stages of infection to three, one, and one secondary case, respectively (Fig. 4). All secondary cases developed symptoms after a median of 4.8 days (IQR 4.0–4.8) after last contact with the primary cases. Three secondary cases were symptomatic before or at start of quarantine, while two developed symptoms after isolation, resulting in 26.4 person-days of community exposure, of which 7.0 person-days were symptomatic community exposure (Table 2). The serial interval between transmission pairs was between −2 days and 10 days (average 3.4 days).
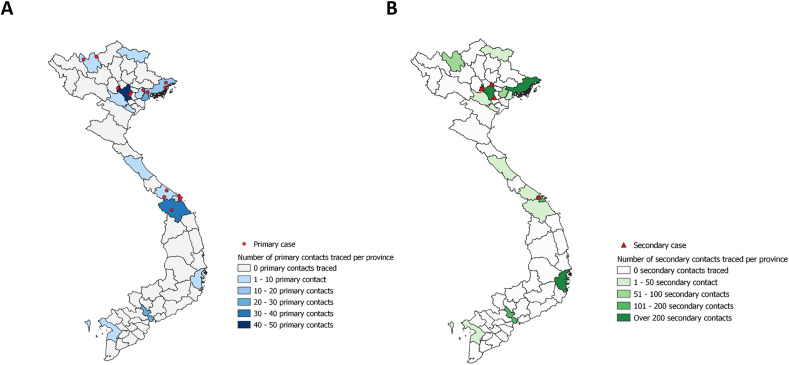
Fig. 5 illustrates the geographical distribution of primary cases and contacts (part A), and secondary cases and contacts (part B) in Vietnam. When contacted by local health authorities, primary and secondary contacts had already dispersed to 15 provinces and cities extending from the northernmost (Cao Bang) to the southernmost (Kien Giang) of Vietnam. Primary and secondary cases were identified in six and two provinces, respectively. On average, 7.1 secondary contacts were traced per primary contact, while 0.3 secondary cases were identified per primary case (Supplement 1). An average of 87.4 secondary contacts were traced for every primary case. The attack rate among secondary contacts was 0.3%.
Fig. 5.
A. Geographical distribution of primary cases and contacts of VN54 flight in Vietnam. B. Geographical distribution of secondary cases and contacts of VN54 flight in Vietnam.
4. Discussion
We report on the first commercial flight arriving in Vietnam with imported COVID-19 cases on board where exhaustive contact tracing and quarantine of all passengers and their contacts was undertaken. We successfully contained a large COVID-19 outbreak with unfolding community transmission through intensive identification, tracing, testing and quarantine measures among 217 flight passengers/crew and more than 1300 of their contacts. These rapid, nationwide efforts limited the outbreak to 16 primary cases among flight passengers/crew and 5 secondary cases within the community in Vietnam.
There were delays before contact tracing initiation. First, the index case was not detected directly upon arrival but only passively by self-presentation at a hospital in Hanoi on 5 March, three days after arrival despite being symptomatic on the flight. Three secondary infections resulted from this extended community exposure. Second, since the positive PCR result was confirmed positive in the late evening of 5 March, the contact tracing process for contacts beyond the index case was only initiated the next morning (9 h later). By this time, 4 days and 3 h after arrival of flight VN54, flight passengers had dispersed already all across Vietnam (Fig. 5) and had generated numerous secondary and third generation contacts, which complicated and delayed timely tracing further.
The case finding and contact tracing activities that followed occurred almost simultaneously, which required the close cooperation of local government authorities and health agencies from all provinces around the country. During the course of four days, contact tracing reached all passengers and crew members who remained in Vietnam at time of investigation (168 of passengers and 16 crew members). Concurrently, after seven days of intensive contact tracing, we had placed into quarantine over 1300 secondary and third degree contacts, among who we identified five additional secondary cases, which corresponds to seven secondary contacts per primary contact and about 87.4 contacts per case. This is higher than the contact-per-case ratios estimated in a study from Singapore (30.8 ratio) [6], Taiwan (27.6 ratio) [7], and several cities in Mainland China (20–40 ratios) [8] during the peak of the outbreak. However, similar estimations of secondary cases per primary cases and per secondary contacts (0.3%) of flight associated cases were observed in the US (0.4%) [9], Taiwan (0.8%) [7] and Singapore (0.5%) [10]. These could be explained by the testing and contact strategy in place at that time, as inclusion criteria for close contacts included both confirmed and suspected cases of COVID-19 [11]. Even though several general prevention measures were in place, in the absence of community cases for 23 consecutive days, no restrictions on in-country travel or on social distancing existed in Vietnam, which might explain the relatively high ratios observed in our study. Pung et al. hypothesized that for most primary cases detected after the arrival date, transmission might had ended early [10], since the viral load and viral viability decreased over time with risk of secondary transmission [12]. In comparison with several studies suggesting that transmission happens shortly before symptom onset [13,14], our findings of limited transmission between flight cases and community cases might be a result of the fact that many primary cases were isolated for a substantial amount of time before symptom onset. The timeliness of isolating/quarantine of all traceable passengers and crew members, indiscriminate of their seating location on the plane in relation to the index case or their time of symptoms onset surely mitigated the extend of community transmission in Vietnam.
Timeliness is of essence for effective contact tracing in infectious disease control. Both the timing of arrival/exposure in relation to the timing of symptom onset and isolation/quarantine are relevant for the control of COVID-19 associated with international air travel. In this cluster containment response, 15 additional cases were isolated/quarantined after four days of contact tracing initiation; seven of whom (47%) were quarantined before symptom onset. This was higher than the 24.5% of pre-symptomatic cases reported in Singapore's contact tracing efforts [15]. The relatively high percentage of 80% of case not showing symptoms at time of testing positive or at all during isolation observed in our study (Fig. 3) is consistent with the rate of asymptomatic carriage in another study of asymptomatic cases among flight passengers in Japan [16], and a flight-related COVID-19 investigation from Singapore to Hangzhou [17]. Notably, we also observed symptom onset among primary cases that was at the upper end of the incubation period described in previous epidemiological reports collated in a systematic review (95th percentile of patients at 11.7 (95% CI 9.7–14.2) days) [18], China (97th percentile at 11.5 (8.2–15.6) days) [19], Wuhan, China (95th percentile at 12.5 days) [20], estimating an average incubation period of 11 days, longer than secondary cases'. Although this was discussed in previous report by the unpredictable clinical characteristics of SARS-CoV-2 and possibly a second in-flight transmission [1], long incubation times and high proportions of asymptomatic infections certainly have public health implications for COVID-19 outbreak response. Importantly, transmission in this cluster was observed from symptomatic, pre-symptomatic and asymptomatic primary cases (Fig. 3), with observed incubation periods (4.8 days) and serial interval (3.4 days) among secondary cases at lower ends of previous estimate [19,21]. This is consistent with current literature on the variety of infection pathways by phase of illness. Given the mounting evidence of pre-symptomatic COVID-19 transmission, this certainly challenges containment effort as the effectiveness of contact tracing decreases if transmission occurs before symptom onset in the index case [22]. As a result, asymptomatic testing is increasingly recommended around the world to ensure the sensitivity and timeliness of case confirmation [[23], [24], [25]], and 14-day isolation is required in many countries for cases and high-risk contacts [26,27]. In Vietnam, rigorous contact tracing, frequent testing and systematic quarantine guaranteed a highly sensitive approach and allowed us to timely and effectively identify all case associated with flight VN54. However, as all cases were detected through contact-based surveillance, the average delay from exposure to isolation for primary cases in this study (6.8 days) was higher than those of similar mode of detection and similar to those of symptom-based surveillance [28]. Among those who were symptomatic before quarantine/isolation, the observed 6.3 days of delay in admission in our study were also higher than the delay from onset to admission observed in Mainland China (average 4.9 days for travelers) [28], and in Hong Kong (2.6–4.2 days for imported cases) [29]. This may be explained by the delay in the initial confirmation of the index case as explained above. Longer delays for successful contact tracing and isolation/quarantine were also observed for primary cases than for secondary cases, which in our study was due to the fact that three out of five secondary cases, who were direct epi-linked to the index case of the flight, were very quickly identified and isolated. The remaining two secondary cases were isolated only five days after exposure to their primary cases, and two days after their primary case confirmation. Both were detected by their own presentation at healthcare facilities (Fig. 4).
The analysis of our response efforts offers a number of lessons learnt for future outbreaks in similar settings: contact tracing and case findings activities require timeliness, equipped staffs and prepared facilities [30,31]. Indeed, the organizational resources and structures needed for public health measures at national scale in response to the flight VN54 cluster were required and utilized for the first time in Vietnam. Required facilities, included quick available passenger's information, consistent and rapid communication means for internal uses and public uses, testing and quarantine facilities, were mobilized to help multi-agency staffs to conduct an effectively exhaustive contact tracing effort. Many studies showed the challenges to access data and mobilize resources in complex multi-jurisdictional contexts [31,32]. The flow of passenger data from airlines to public-health agencies can easily be delayed since many airlines do not share these data willingly, and many public health agencies do not have the authority to access such information on time [33,34]. In addition, a broken feedback loop of information across health jurisdictions for national-wide contact tracing can also quickly stagnant the contact tracing process. One study from the US CDC's airport quarantine stations showed incomplete information gathered from local health agencies during a Tboutbreak rendered it difficult to indicate whether potential contacts were found or tested [35]. Another study from Germany showed that completeness of information for passengers on board is crucial to improve a comprehensive international contact tracing process, coupled with health education for passengers about infectious disease transmission on public transport [36]. In Vietnam, even though the process was newly introduced and not yet tested in a simulation exercise, passenger information was obtained and distributed during the first day of the outbreak response, which greatly enhanced the process of subsequent contact tracing. Although complete information was not available for all passengers since passengers did not have to disclose their address in Vietnam upon arrival at that time, national cooperation and support from local authorities, tourism and police departments ensured effectively tracing of all passengers who remained in Vietnam at time of contact tracing was initiated. Additionally, clear and sensitive inclusion criteria for contact tracing are crucial. The fact that we applied a blanket definition of primary contacts to all passengers and crew members on flight VN54 was novel to traditional public health measures for COVID-19 at time of investigation. Before VN54, there was three instances of non-quarantined imported cases detected in Vietnam, however, investigation was scoped at close contacts in community, and to passengers within two seats away from index case. Following the country's approach of “To miss one case is to ignite two others”, this cluster containment effort showed that it is possible to quickly contain a highly infectious pathogen such as SARS-CoV-2 through national collective efforts and multi-agency. The delays inherent to case finding measures such as testing, tracing and quarantine/isolation highlight the need for rapid adaptation of response mechanisms in public health emergencies. While the delay in the detection of the index case could have been shortened by systematic obligatory testing at arrival, contact tracing initiation could have been accelerated by pre-established and pre-tested standard operating procedures to trigger immediate activation of public health response following laboratory confirmation. Lessons were learnt quickly in Vietnam. For example, as a result of the difficulties experienced to trace highly-mobile tourists across the country, as soon as from 6 March 2020 onwards, all inbound passengers were required to fill out health declaration forms that included passengers' contact information in Vietnam. Soon thereafter, starting on 21 March 2020, mandatory SARS-CoV-2 testing and quarantine were implemented for all passengers arriving in Vietnam regardless of their place of departure, which in turn greatly reduced contact tracing efforts and resources for provincial health jurisdictions. To justify the need for the extensive contact tracing and testing regime as implemented in our study, appropriate resources and training as well as a good understanding of the local context of the COVID-19 situation are needed.
Our analysis had several limitations. The VN54 cluster was an early event during the COVID-19 epidemic in Vietnam after nearly a month of no new confirmed cases nationwide. Hence, a lot of information was missing due to the lack of standard data collection and reporting at that time. We lacked individual-level data about secondary and third generation contacts, including demographics, type and location of exposure, date of quarantine for each individual, number of secondary and third generation contacts per epi-linked primary contacts, and unsuccessfully traced contacts. Such data would have allowed an in-depth analysis of contact behaviors and to assess differences in risks of infection.
The longer the ongoing pandemic lasts, the less sustained border control measures such as total border closures or blanket quarantine policies are to remain practical and acceptable. Vietnam, as many countries, is now considering to resume commercial air travel despite considerable risk of disease importation and very low in-country transmission. Sustainable and flexible surveillance and contact tracing system is crucial to adapt to the ever-changing situation, and to achieve a balance between containing disease spread while reducing the overall health and socioeconomic impact due to COVID-19.
5. Conclusion
Intensive tracing, testing and quarantine of all flight passengers, crew and their contacts helped to contain an unfolding COVID-19 outbreak in Vietnam caused by in-flight transmission from one symptomatic passenger on board. Multi-agency collaboration, sensitive testing policy and strict quarantine mechanisms allow COVID-19 outbreaks to be managed with limited secondary cases in the community. Low and middle income countries need to establish a combination of appropriate measures in response to the risk of COVID-19 importation through air travel and subsequent community transmission.
CRediT authorship contribution statement
Ha-Linh Quach: Conceptualization, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing. Ngoc-Anh Thi Hoang: Data curation, Investigation, Visualization, Writing – review & editing. Cong Khanh Nguyen: Project administration, Investigation, Supervision, Writing – review & editing. Quang Thai Pham: Project administration, Investigation, Supervision, Writing – review & editing. Cong Dinh Phung: Resources, Software, Visualization. Nhu Duong Tran: Investigation, Methodology, Resources. Quynh Mai Thi Le: Investigation, Methodology, Resources. Duy Nghia Ngu: Formal analysis, Investigation, Resources. Anh Tu Tran: Formal analysis, Investigation, Resources. Ngoc Quang La: Data curation, Validation. Dai Quang Tran: Data curation, Validation. Trong Tai Nguyen: Data curation, Validation. Florian Vogt: Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing. Duc Anh Dang: Project administration, Supervision.
Declaration of competing interest
The authors declare no conflicts of interest.
Acknowledgement
We acknowledge important contributions and guidelines from the following institution and committee: National Steering Committee for COVID-19 Prevention and Control, Ministry of Health, Ministry of Science and Technology, and National Institute of Hygiene and Epidemiology. We thank health-care workers from Provincial Centers of Disease Control and local authorities from provinces and cities in Vietnam for their great works in case finding, contact tracing, disease control, and prevention measures. We would like to thank the cooperation and support from Civil Aviation Administration, Immigration Bureau and Vietnam Airlines, and all passengers on the VN54 plane. This work was conducted as part of Master of Applied Epidemiology program in collaboration between the National Institute of Hygiene and Epidemiology, Hanoi, Vietnam and the Australian National University, Canberra, Australia. Ngoc-Anh Thi Hoang and Ha-Linh Quach were students of the program and received scholarship from the ASEAN-Australia Health Security Fellowship by the Commonwealth Department of Foreign Affairs and Trade.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.tmaid.2021.102084.
Funding
HLQ and NATH are funded by the ASEAN-Australia Health Security Fellowship by the Commonwealth, Department of Foreign Affairs and Trade, and the Master of Applied Epidemiology Scholarship by the Australian National University.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Khanh N.C., Thai P.Q., Quach H.-L., Thi N.-A.H., Dinh P.C., Duong T.N., et al. Transmission of SARS-CoV 2 during long-haul flight. Emerg Infect Dis. 2020 Nov;26(11) doi: 10.3201/eid2611.203299. https://wwwnc.cdc.gov/eid/article/26/11/20-3299_article [Internet] 2617–24. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freedman D.O., Wilder-Smith A. In-flight transmission of SARS-CoV-2: a review of the attack rates and available data on the efficacy of face masks. J Trav Med. 2020 Sep 25;2020:1–7. doi: 10.1093/jtm/taaa178. https://academic.oup.com/jtm/advance-article/doi/10.1093/jtm/taaa178/5910636 [Internet] Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vietnam Ministry of Health . Vietnam Ministry of Health Portal; 2020. Decision No. 343/QĐ-BYT date February 7 2020 on “Official guidelines for surveillance, prevention and control measures for acute pneumonia infecition caused by novel corona virus nCoV”.https://moh.gov.vn/web/dich-benh/huong-dan-chuyen-mon/-/asset_publisher/NxZAa8ST2KXb/content/quyet-inh-so-343-q-byt-ngay-07-02-2020-ve-viec-ban-hanh-huong-dan-tam-thoi-giam-sat-va-phong-chong-benh-viem-uong-ho-hap-cap-do-chung-moi-cua-vi-rut-c [Internet] Available from. [Google Scholar]
- 4.General Department of Preventive Medicine VM of H . Digital Communication Department, General Department of Preventive Medicine; 2020. Lists of Eligible laboratory departments for COVID-19 testing and confirmation.http://vncdc.gov.vn/vi/phong-chong-dich-benh-viem-phoi-cap-ncov/11871/cac-phong-xet-nghiem-viet-nam-co-the-xet-nghiem-covid-19 [Internet] Available from. [Google Scholar]
- 5.Official Page for acute respiratory disease COVID-19 . Vietnam Ministry of Health; 2020. Compulsory mask wearing measures in Vietnam: q&A.https://ncov.moh.gov.vn/en/-/khi-bat-buoc-eo-khau-trang-noi-cong-cong-ung-lam-ieu-nay-e-khau-trang-khong-thanh-o-benh- [Internet] Available from. [Google Scholar]
- 6.Wong J.E.L., Leo Y.S., Tan C.C. COVID-19 in Singapore - current experience: critical global issues that require attention and action. JAMA, J Am Med Assoc. 2020 Apr 7;323(13) doi: 10.1001/jama.2020.2467. https://clinicaltrials.gov/ct2/show/NCT04257656 [Internet] 1243–4. Available from. [DOI] [PubMed] [Google Scholar]
- 7.Cheng H.Y., Jian S.W., Liu D.P., Ng T.C., Huang W.T., Lin H.H. Contact tracing assessment of COVID-19 transmission dynamics in taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern Med. 2020 Sep 1;180(9) doi: 10.1001/jamainternmed.2020.2020. https://jamanetwork.com/ [Internet] 1156–63. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fu H., Xi X., Wang H., Boonyasiri A., Wang Y., Hinsley W., et al. Report 30: the COVID-19 epidemic trends and control measures in mainland China. 2020 Jul. [Internet], Available from. [DOI]
- 9.Burke R.M., Midgley C.M., Dratch A., Fenstersheib M., Haupt T., Holshue M., et al. Active monitoring of persons exposed to patients with confirmed COVID-19 — United States, january–february 2020. MMWR Morb Mortal Wkly Rep. 2020 Mar 6;69(9) doi: 10.15585/mmwr.mm6909e1. http://www.cdc.gov/mmwr/volumes/69/wr/mm6909e1.htm?s_cid=mm6909e1_w [Internet] 245–6. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pung R., Chiew C.J., Young B.E., Chin S., Chen M.I.C., Clapham H.E., et al. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020 Mar 28;395(10229) doi: 10.1016/S0140-6736(20)30528-6. [Internet] 1039–46. Available from 10.1016/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kucharski A.J., Klepac P., Conlan A.J.K., Kissler S.M., Tang Mmath M., Fry Phd H., et al. Effectiveness of isolation, testing, contact tracing and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. Lancet Infect Dis. 2020;20(10):1151–1160. doi: 10.1016/S1473-3099(20)30457-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeong H.W., Kim S.M., Kim H.S., Kim Y Il, Kim J.H., Cho J.Y., et al. Viable SARS-CoV-2 in various specimens from COVID-19 patients. Clin Microbiol Infect. 2020 Jul 23 doi: 10.1016/j.cmi.2020.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moghadas S.M., Fitzpatrick M.C., Sah P., Pandey A., Shoukat A., Singer B.H., et al. The implications of silent transmission for the control of COVID-19 outbreaks. Proc Natl Acad Sci U S A. 2020 Jul 28;117(30) doi: 10.1073/pnas.2008373117. www.pnas.org/cgi/doi/10.1073/pnas.2008373117 [Internet] 17513–5. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tindale L.C., Stockdale J.E., Coombe M., Garlock E.S., Lau W.Y.V., Saraswat M., et al. Evidence for transmission of covid-19 prior to symptom onset. Elife. 2020 Jun 1;9:1–34. doi: 10.7554/eLife.57149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng Y., Li Z., Chua Y.X., Chaw W.L., Zhao Z., Er B., et al. MMWR Morb Mortal Wkly Rep; 2020 Mar 20. Evaluation of the effectiveness of surveillance and containment measures for the first 100 patients with COVID-19 in Singapore — january 2–february 29, 2020.http://www.cdc.gov/mmwr/volumes/69/wr/mm6911e1.htm?s_cid=mm6911e1_w [Internet] 69(11):307–11. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nishiura H., Kobayashi T., Miyama T., Suzuki A., Jung S mok, Hayashi K., et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020 May 1;94 doi: 10.1016/j.ijid.2020.03.020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7270890/ [Internet] 154–5. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen J., He H., Cheng W., Liu Y., Sun Z., Chai C., et al. Potential transmission of SARS-CoV-2 on a flight from Singapore to Hanghzou, China: an epidemiological investigation. Trav Med Infect Dis. 2020 Jul 1;36 doi: 10.1016/j.tmaid.2020.101816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McAloon C., Collins Á., Hunt K., Barber A., Byrne A.W., Butler F., et al. Incubation period of COVID-19: a rapid systematic review and meta-analysis of observational research. BMJ Open [Internet] 2020 Aug 16. http://bmjopen.bmj.com/ Available from. 10, 8. [DOI] [PMC free article] [PubMed]
- 19.Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R., et al. The incubation period of coronavirus disease 2019 (CoVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020 May 5;172(9) doi: 10.7326/M20-0504. https://zenodo.org/record/3692048 [Internet] 577–82. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., et al. Early transmission dynamics in wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020 Mar 26;382(13) doi: 10.1056/NEJMoa2001316. https://www.nejm.org/doi/10.1056/NEJMoa2001316 [Internet] 1199–207. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nishiura H., Linton N.M., Akhmetzhanov A.R. Serial interval of novel coronavirus (COVID-19) infections. Int J Infect Dis. 2020 Apr 1;93:284–286. doi: 10.1016/j.ijid.2020.02.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hellewell J., Abbott S., Gimma A., Bosse N.I., Jarvis C.I., Russell T.W., et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Heal. 2020 Apr 1;8(4) doi: 10.1016/S2214-109X(20)30074-7. www.thelancet.com/lancetgh [Internet] e488–96. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gandhi M., Yokoe D.S., Havlir D.V. Asymptomatic transmission, the achilles' heel of current strategies to control covid-19. N Engl J Med. 2020 May 28;382(22) doi: 10.1056/NEJMe2009758. https://www.nejm.org/doi/full/10.1056/NEJMe2009758 [Internet] 2158–60. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Day M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ. 2020 Apr 2;369(m1375) doi: 10.1136/bmj.m1375. http://group.bmj.com/group/rights-licensing/ [Internet] Available from. [DOI] [PubMed] [Google Scholar]
- 25.Marcel S., Christian A.L., Richard N., Silvia S., Emma H., Jacques F., et al. COVID-19 epidemic in Switzerland: on the importance of testing, contact tracing and isolation. Swiss Med Wkly. 2020 Mar 19;150(11–12) doi: 10.4414/smw.2020.20225. https://pubmed.ncbi.nlm.nih.gov/32191813/ [Internet] Available from. [DOI] [PubMed] [Google Scholar]
- 26.US Centers for Disease Control and Prevention . 2020. Public health guidance for potential COVID-19 exposure associated with international or domestic travel | CDC.https://www.cdc.gov/coronavirus/2019-ncov/php/risk-assessment.html [Internet] Available from. [Google Scholar]
- 27.Peak C.M., Kahn R., Grad Y.H., Childs L.M., Li R., Lipsitch M., et al. Individual quarantine versus active monitoring of contacts for the mitigation of COVID-19: a modelling study. Lancet Infect Dis. 2020 Sep 1;20(9):1025–1033. doi: 10.1016/S1473-3099(20)30361-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bi Q., Wu Y., Mei S., Ye C., Zou X., Zhang Z., et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect Dis. 2020 Aug 1;20(8) doi: 10.1016/S1473-3099(20)30287-5. www.thelancet.com/infection [Internet] 911–9. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lam H.Y., Lam T.S., Wong C.H., Lam W.H., Leung C.M.E., Au K.W.A., et al. The epidemiology of COVID-19 cases and the successful containment strategy in Hong Kong–January to May 2020. Int J Infect Dis. 2020 Sep 1;98 doi: 10.1016/j.ijid.2020.06.057. https://pubmed.ncbi.nlm.nih.gov/32579906/ [Internet] 51–8. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.US Centers for Disease Control and Prevention Case investigation and contact Tracing : Part of a multipronged approach to fight the COVID-19 pandemic. 2020. https://www.cdc.gov/coronavirus/2019-ncov/php/principles-contact-tracing.html [Internet], Available from.
- 31.Al-Tawfiq J.A., Sattar A., Al-Khadra H., Al-Qahtani S., Al-Mulhim M., Al-Omoush O., et al. Incidence of COVID-19 among returning travelers in quarantine facilities: a longitudinal study and lessons learned. Trav Med Infect Dis. 2020 Nov 1;38:101901. doi: 10.1016/j.tmaid.2020.101901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kotila S.M., Payne Hallström L., Jansen N., Helbling P., Abubakar I. Systematic review on tuberculosis transmission on aircraft and update of the European Centre for Disease Prevention and Control risk assessment guidelines for tuberculosis transmitted on aircraft (RAGIDA-TB) Euro Surveill. 2015 Jan 28;21(4):30114. doi: 10.2807/1560-7917.ES.2016.21.4.30114. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=21357 [Internet] Available from. [DOI] [PubMed] [Google Scholar]
- 33.Flanagan P., O'Donnell J., Mereckiene J., O'Flanagan D. Tuberculosis contact investigations associated with air travel in Ireland, September 2011 to November 2014. Euro Surveill. 2016 Oct 6;21(40):1. doi: 10.2807/1560-7917.ES.2016.21.40.30358. [Internet] Available from:, /pmc/articles/PMC5071608/?report=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McKenna Maryn. Center for Infectious Disease Research and Policy, University of Minnesota; 2008. Tracing air travelers at risk for disease still tough.https://www.cidrap.umn.edu/news-perspective/2008/06/tracing-air-travelers-risk-disease-still-tough [Internet] Available from. [Google Scholar]
- 35.Powell K., Lamb M.M., Sisk M.K., Federline L., Seechuk K., Lambert L.A., et al. Passenger contact investigation associated with a transport driver with pulmonary tuberculosis. Publ Health Rep. 2012;127(2) doi: 10.1177/003335491212700209. http://pmc/articles/PMC3268805/?report=abstract [Internet] 202–7. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Glasauer S., Kröger S., Haas W., Perumal N. International tuberculosis contact-tracing notifications in Germany: analysis of national data from 2010 to 2018 and implications for efficiency. BMC Infect Dis. 2020 Apr 6;20(1):267. doi: 10.1186/s12879-020-04982-z. https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-020-04982-z [Internet] Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.