Background
The COVID-2019 pandemic continues to restrict access to endoscopy, resulting in delays or cancellation of non-urgent endoscopic procedures. A delay in the removal or exchange of plastic biliary stents may lead to stent occlusion with consensus recommendation of stent removal or exchange at three-month intervals [1-4]. We postulated that delayed plastic biliary stent removal (DPBSR) would increase complication rates.
Aim: We aim to report our single-centre experience with complications arising from DPBSR.
Methods
This was a retrospective, single-center, observational cohort study. All subjects who had ERCPguided plastic biliary stent placement in Halifax, Nova Scotia between Dec 2019 and June 2020 were included in the study. DPBSR was defined as stent removal >=90 days from insertion. Four endpoints were assigned to patients: 1. Stent removed endoscopically, 2. Died with stent in-situ (measured from stent placement to documented date of death/last clinical encounter before death), 3. Pending removal (subjects clinically well, no liver enzyme elevation, not expired, endpoint 1 Nov 2020), and 4. Complication requiring urgent reintervention. Kaplan-Meier survival analysis was used to represent duration of stent patency (Fig.1).
Results
102 (47.2%) had plastic biliary stents placed between 2/12/2019 and 29/6/2020. 49 (48%) were female, and the median age was 68 (R 16-91). Median follow-up was 167.5 days, 60 (58.8%) subjects had stent removal, 12 (11.8%) died before replacement, 21 (20.6%) were awaiting stent removal with no complications (median 230d, R 30-332), 9 (8.8%) had complications requiring urgent ERCP. Based on death reports, no deaths were related to stent-related complications. 72(70.6%) of patients had stents in-situ for >= 90 days. In this population, median time to removal was 211.5d (R 91-441d). 3 (4.2%) subjects had stent-related complications requiring urgent ERCP, mean time to complication was 218.3d (R 94-441). Stent removal >=90 days was not associated with complications such as occlusion, cholangitis, and migration (p=1.0). Days of stent in-situ was not associated with occlusion, cholangitis, and migration (p=0.57). Sex (p=0.275), cholecystectomy (p=1.0), cholangiocarcinoma (p=1.0), cholangitis (p=0.68) or pancreatitis (p=1.0) six weeks prior to ERCP, benign vs. malignant etiology (p=1.0) were not significantly associated with stent-related complications.
Discussion
Plastic biliary stent longevity may have been previously underestimated. The findings of this study agree with Canadian Association of Gastroenterology recommendations [5] that stent removal be prioritized as elective (P3). Limitations include small sample size that could affect Kaplan-Meier survival analysis. Despite prolonged indwelling stent time as a result of COVID-19, we did not observe an increased incidence of stent occlusion or other complications.
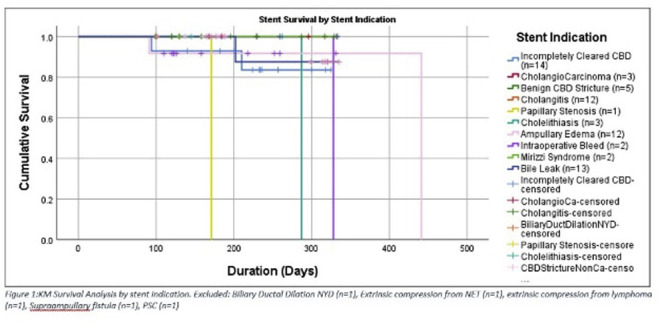
Kaplan-Meier Survival Analysis by Stent Indication


