Abstract
IgG4-related disease (IgG4-RD) is a systemic fibroinflammatory disease characterised by dense lymphoplasmacytic infiltration rich in IgG4-positive plasma cells, storiform fibrosis and obliterative phlebitis. Serum IgG4 levels are typically elevated but half of the patients had normal serum IgG4 levels. IgG4-RD represents a spectrum of diseases that involve various organs such as the pancreas, liver, kidneys, and salivary glands often manifesting as diffuse organ enlargement or a mass-like lesion mimicking cancer. An increased incidence of malignancy among patients with IgG4-RD has been reported. Thus, differentiating malignancy from IgG4-RD manifestation is important as the treatment differs. Glucocorticoids are considered first-line therapy and should be started early to prevent fibrosis. Patients usually have an excellent clinical response to steroids, and poor steroid response is indicative of an alternative diagnoses such as malignancy. This case report describes a case of IgG4-RD with renal mass in a young man that resolved with glucocorticoid therapy alone.
Keywords: connective tissue disease, urology, immunology
Background
In the past, Mikulicz disease, type 1 autoimmune pancreatitis (AIP), sclerosing cholangitis and retroperitoneal fibrosis were considered unrelated, single-organ disease entities which were distinct from one another. However, in recent years, the striking similarities of these diseases in terms of clinical manifestation, histopathology features,1 and serological characteristic have grouped these diseases under the umbrella term of IgG4-related disease (IgG4-RD). Clinically, they usually present as mass-like lesions or diffuse enlargement of the organs. Histopathologically, dense lymphoplasmacytic infiltration rich in IgG4-positive plasma cells, storiform fibrosis and obliterative phlebitis are the characteristic features of IgG4-RD.2 Serologically, raised serum IgG4 levels are found in two-thirds of the patients. Glucocorticoid therapy has proven to be an effective treatment for IgG4-RD, especially in the early proliferative inflammatory stage.3 Some may need other immunosuppressant therapies such as rituximab to achieve disease remission.4 Steroids and other immunosuppressive therapies’ efficacy is limited in the fibrotic stage. Hence, early diagnosis and prompt steroid initiation lead to better treatment outcomes.
Case presentation
The patient is a 33-year-old man with no known comorbidities. He presented with progressive painless swelling of the bilateral submandibular glands and bilateral upper eyelid swellings for 5-month duration prior to the first medical consultation. There was no blurring of vision, gaze palsy or eye protrusion.
He denied sicca symptoms such as xerostomia or dry eye. In addition, there was no ‘B’ symptoms such as fever, night sweats or weight loss. He had no positive tuberculosis contact and had no respiratory symptoms such as chronic cough, haemoptysis or reduced effort tolerance. Besides that, there were no joint pains or swelling, and there were no painful rashes over the shins. Other aspects of the systemic review were unremarkable, in particular, there was no history of urinary tract symptoms.
Clinical examination revealed enlarged bilateral lacrimal glands, bilateral submandibular glands and right parotid gland. There were multiple palpable lymphadenopathies involving the bilateral cervical, bilateral supraclavicular, bilateral post-auricular and right inguinal region. Among these, the right supraclavicular lymphadenopathy was the largest, measuring 2×2 cm. There was no proptosis, gaze palsy, jaundice or goitre clinically. Schirmer’s test was negative.
Examination of the lower limbs did not reveal any presence of erythema nodosum. The respiratory examination identified normal vesicular breath sounds with no additional crackles auscultated. Cardiovascular and abdomen examinations were unremarkable. A rheumatological assessment revealed that the joints were neither tender nor swollen.
Investigations
His full blood counts were within normal range with a normal white cell count (8.8 x 109/L), haemoglobin level (144 g/L), platelet level (333 x 109/L) and eosinophil count (0.32×109/L). Full blood picture was unremarkable and bone marrow aspiration and trephine biopsy (BMAT) showed no evidence of abnormal lymphoid cell or blast, which excludes a diagnosis of lymphoma.
Tuberculosis work-up which included sputum for acid-fast bacilli and bone marrow aspirate mycobacterium cultures was negative. The inflammatory markers were raised with erythrocyte sedimentation rate of 64 mm/hour (normal range <12 mm/hour), and C reactive protein of 34.7 mg/L (normal range <5 mg/L).
Serum amylase was within the normal range (71 µ/L, normal range 30–118 µ/L). The renal profile, liver function test, thyroid function test and calcium level were normal. Full and microscopic examination of urine was negative for blood and protein. HIV screening in this patient was negative. Epstein-Barr virus antibody test was also negative.
Serum total IgG was raised at 3450 mg/dL (normal range 767–1590 mg/dL), but Ig4 level was normal at 19.1 mg/dL (normal range 2.4–121 mg/dL). Other subclasses of IgG were raised: IgG1 2230 mg/dL (normal range 341–894 mg/dL), IgG2 1090 mg/dL (normal range 171–632 mg/dL) and IgG3 404 mg/dL (18.4–106 mg/dL). In addition, his serum IgE level was also markedly raised at 749 mg/dL (normal range 32–117 mg/dL). Antineutrophil cytoplasmic antibodies, antinuclear antibodies (ANA), extractable nuclear antigen, in particular, anti-SSA and anti-SSB, were negative. His complement levels were normal, with a C3 level of 0.8 g/L (normal range 0.8–1.2 g/L) and C4 of 0.1 g/L (normal range 0.1–0.4 g/L). The patient’s chest radiograph was normal, with no enlarged hila, interstitial infiltrates, or upper zone consolidation or cavitation.
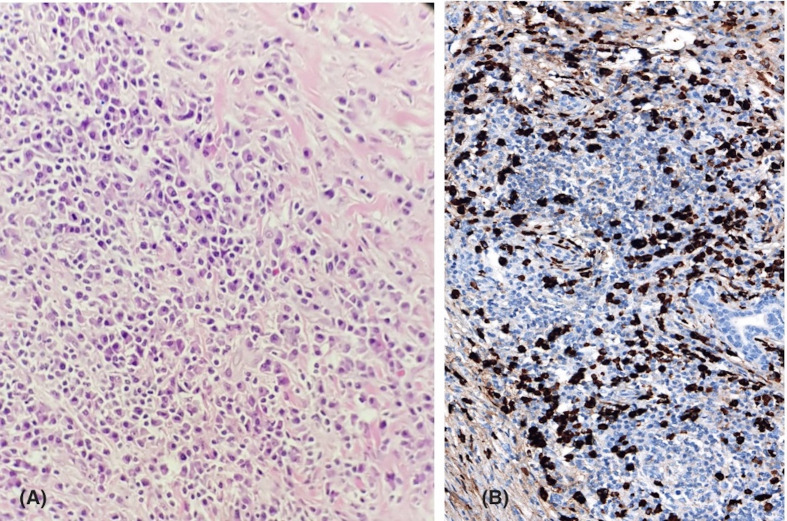
For diagnostic confirmation, he underwent an excision biopsy of the enlarged cervical lymph node and left submandibular gland. Cervical lymph node histology examination revealed patchy lymphoid aggregate with fibrotic stroma. There were no atypical lymphoid cells, granuloma or malignancy seen. Histopathology examination of the left submandibular gland revealed marked hyperplastic lymphocytic infiltration with loss of salivary gland acini. The remaining ducts were surrounded by a polymorphous population of lymphocytes and plasma cell infiltrates highlighted by CD3, CD20 and CD79a immunostains (figure 1A). In addition, there was also presence of storiform fibrosis with mild eosinophil infiltration. However, no demonstrable obliterating phlebitis, calcification or atypical plasma cells. Further immunohistology staining of the submandibular gland biopsy showed IgG4-positive plasma cells >100 cell/high-power field (HPF), which confirmed the diagnosis of IgG4-RD (figure 1B).
Figure 1.
(A) Submandibular lymph node histopathology sample showing diffuse infiltration by lymphocytes and plasma cells with occasional eosinophils. (B) Positive IgG4 staining of submandibular lymph node at high magnification.
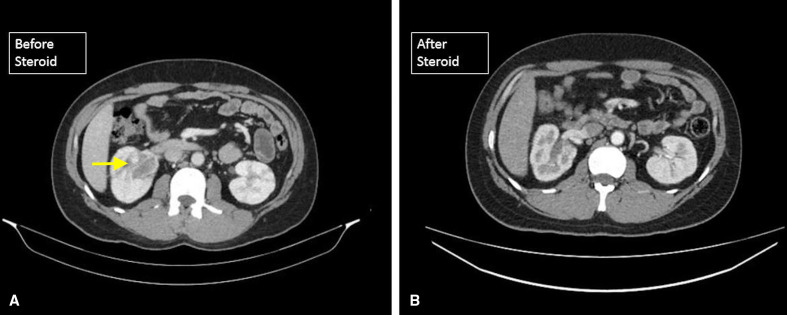
In order to ascertain disease extent, and at the same time exclude underlying malignancy, the patient underwent a series of contrasted CT scans. CT scan of the neck and orbit revealed bilateral symmetrically enlarged and enhanced lacrimal glands, showing features of infiltrative disease of bilateral lacrimal glands and parotid glands. There were multiple subcentimetre lymph nodes enlargement from level I to III, with supraclavicular and mediastinal node involvement. CT of the thorax, abdomen and pelvis (CT-TAP) incidentally revealed a right renal pelvic mass measuring about 3.9×4.5×3.4 cm, extending into the proximal third of the right ureter causing narrowing of its lumen (figure 2A). There were several subcentimetre mediastinal and cervical lymphadenopathies, with no evidence of peripelvic or retroperitoneal fibrosis. In the presence of a right renal mass and multiple lymphadenopathies, transitional renal cell carcinoma and lymphoma were considered.
Figure 2.
(A) A right renal mass (arrow) seen on the CT abdomen. (B) Absence of right renal mass after 6 months of steroid therapy.
The patient was referred immediately for renal biopsy, but unfortunately the renal biopsy date was repeatedly postponed and delayed for 6 months due to scheduling conflicts brought about by the COVID-19 pandemic. Prior to his renal biopsy, a renal ultrasound scan after 6 months of steroid therapy failed to identify the renal mass, and a subsequent CT renal scan confirmed the absence of the initially seen renal mass (figure 2B).
Differential diagnosis
The possible differential diagnoses for a patient with bilateral lacrimal and submandibular glands enlargement, together with cervical lymphadenopathies, are Sjogren’s syndrome, lymphoma and sarcoidosis. The absence of sicca symptoms, normal Schirmer’s test, negative ANA and anti-SSA excluded Sjogren’s syndrome in this patient. He had extensive work-up done for lymphoma which included cervical lymph node excision biopsy, bone marrow aspiration and trephine biopsy. Both the histopathological examinations of the lymph node biopsy and BMAT did not reveal any atypical lymphoid cells. Sarcoidosis is less likely in this patient with absence of hilar lymphadenopathy on chest X-ray, normal calcium level, and absence of granuloma seen in both submandibular gland and cervical lymph node biopsy. With the CT-TAP showing presence of right pelvic renal mass, transitional cell renal carcinoma was considered.
Treatment
In view of the progressive swelling of the patient’s bilateral lacrimal glands and cervical lymph nodes, significantly impacting on the patient’s appearance and work performance, a decision was made to commence steroids before CT-TAP which was repeatedly delayed due to various unforeseen circumstances. After the BMAT procedure, he was commenced on intravenous hydrocortisone 100 mg three times per day for 3 days which was later converted to oral prednisolone 40 mg once a day (0.6 mg/kg/day prednisolone) and tapered down 5 mg every 2 weeks until 10 mg once a day. The patient’s condition improved significantly with complete resolution of the bilateral lacrimal glands swelling and cervical lymphadenopathies within 1 month of steroid commencement.
When CT-TAP revealed a right renal pelvis mass, the patient was immediately referred to the urology team for further management. A retrograde pyelogram was performed which confirmed right ureteric obstruction with hydronephrosis, and stenting was done to relieve the obstruction.
Outcome and follow-up
After 1 year of diagnosis and treatment of IgG4-RD, this patient has no symptoms suggestive of disease recurrence. The steroid therapy is slowly tapered down and he is currently on low-dose prednisolone 7.5 mg once a day. His right ureteric stent was eventually removed with regular follow-up at the urology clinic.
Discussion
Historically, Mikulicz disease—a painless symmetrical swelling of the lacrimal, parotid and submandibular glands—was thought to be a subset of Sjogren’s syndrome due to histological similarities.5 However, studies among patients with Mikulicz disease noted significant elevated serum concentration of IgG4, characteristic histopathological finding, glands infiltration of IgG4-bearing plasma cells and good glucocorticoid treatment response. These findings have revolutionised the classification of Mikulicz disease, and it is now considered to be a part of a larger constellation of diseases—IgG4-RD.6 Similar findings are also seen in type 1 AIP, sclerosing cholangitis, retroperitoneal fibrosis, etc. IgG4-RD is now recognised as a new distinct disease by itself. It is a chronic systemic fibroinflammatory disease characterised by dense lymphoplasmacytic infiltration rich in IgG4-positive plasma cells with storiform fibrosis, often but not always, raised serum IgG4 level. It can affect multiple organs concurrently or metachronously. The intense inflammation and fibrosis can lead to organ dysfunction and subsequent failure.
The prevalence of the disease in Japan was reported to be 0.28–1.08 per 100 000 population.7 However, this disease prevalence may be underestimated as the disease is newly recognised and, therefore, likely to be under-reported. There is a slight predominance of middle-aged and elderly men.
Recent studies have proposed that the interaction between the various subsets of CD4+ and B cell subsets is the likely underlying pathogenesis of IgG4-RD. It is proposed that continuous activation of the CD4+ cytotoxic T cells stimulates the selective production of IgG4.8 As a result, serum IgG4 is elevated in IgG4-RD, although approximately 50% of biopsy-proven IgG4-RD has normal serum IgG4.9 A raised serum IgG4 concentration is not specific for IgG4-RD as it can be found in other disorders such as sarcoidosis and multicentric Castleman disease. Furthermore, the IgG4 antibody appears not to be pathogenic, but rather represents an epiphenomenon in IgG4-RD.
In an appropriate clinical context, characteristic morphological features form the fundamental diagnosis of IgG4-RD. Dense lymphoplasmacytic infiltrates bearing IgG4-plasma cells, storiform fibrosis and obliterative phlebitis are the three major characteristic histopathological findings in IgG4-RD.2 In most instances, the presence of two out of three major histological features diagnoses IgG4-RD confidently. However, storiform fibrosis and obliterative phlebitis may be absent in certain organs, for example, lymph nodes and minor salivary glands.
The risk of malignancies is increased among patients with IgG4-RD. SMART Database (Sapporo Medical University and Related institutes database for investigation and best treatments of IgG4-RD) has shown that 10.4% of patients with IgG4-RD had cancers.10 When compared with the general population, the incidence of cancer was about 3.5 times higher.10 IgG4-RD-associated malignancy can be divided into lymphoma and solid organ tumours, such as lung cancer and colon carcinoma. Mucosa-associated lymphoid tissue lymphoma and non-Hodgkin's lymphoma are the common lymphomas associated with IgG4-RD.11 12 The pathogenesis contributing to malignancy among patients with IgG4-RD remains unclear. However, it is postulated that chronic inflammatory process in IgG4-RD may contribute to the occurrence of malignancy.
As IgG4-RD can present as mass-like lesions in various organs, it can manifest as a mimicker of malignancy. There have been various case reports of IgG4-RD mimicking urothelial carcinoma,13 lung carcinoma14 and metastatic colon cancer.15 In the majority of cases, the diagnosis of IgG4-RD was only made postoperatively after immunohistological examination of the resected organs. To date, apart from histopathology and IgG4 immunostain, there are no other diagnostic features that can confidently differentiate true malignancy from IgG4-RD mass lesions. Hence, a high index of suspicions of IgG4-RD needs to be considered before subjecting patients to unnecessary radical surgical interventions. In the case of our patient, the right renal pelvic mass poses a dilemma whether it was primary renal cell carcinoma or part of the manifestations of IgG4-RD. A renal mass biopsy was planned but delayed due to unforeseen reasons. After 6 months of steroid therapy alone, the renal mass disappeared. Thus, we are convinced that the renal mass was part of the renal manifestation of IgG4-RD instead of renal cell carcinoma.
Based on the latest recommendation, the treatment of IgG4-RD is divided into remission and maintenance therapy.16 As fibrosis, a consequence of inflammation is irreversible, therapy needs to be initiated at the earliest time frame. To date, corticosteroid is the recommended first-line therapy for remission induction.3 17 The usual initiation steroid dose was 30–40 mg prednisolone per day, after which was tapered down gradually. The majority of patients showed rapid response to corticosteroid within weeks of treatment, as demonstrated by our patient. However, in steroid-resistance IgG4-RD cases, rituximab, a B cell depleting agent, has proven to be an effective alternative treatment to achieve disease remission.4 Hart et al reported a complete remission rate of 83% following rituximab therapy in patients with AIP who were resistant to steroid treatment.18 The early use of conventional steroid-sparing agents, such as azathioprine and mycophenolate mofetil in combination with steroid as remission therapy, varies between experts from different regions. Majority of the Japanese physicians disagreed with the addition of steroid-sparing agents in the early disease treatment course, while physicians from other countries opted for early initiation of steroid-sparing agents. As relapse occurred in 20%–30% of patients when glucocorticoid dose was tapered down or discontinued, adding a steroid-sparing agent is appropriate in patients with persistent active disease while on steroid.19 Once remission is achieved, maintenance therapy helps to reduce disease recurrence, especially those with organ-threatening IgG4-RD manifestations. Low-dose prednisolone, steroid-sparing agents and rituximab have been proven to be effective maintenance therapies.20 21 However, the optimal duration of the maintenance therapy is unknown and is likely to vary between patients.
Our patient fulfilled the 2019 American College of Rheumatology/European League Against Rheumatism classification criteria for IgG4-RD, based on bilateral lacrimal and submandibular gland involvement, renal pelvis soft tissue involvement, histopathology findings of dense lymphocytic infiltration and storiform fibrosis, and positive IgG4 immunostain on submandibular gland biopsy.22 He responded convincingly to glucocorticoid therapy with resolution of the cervical lymphadenopathy, lacrimal and submandibular glands enlargement within the first month of treatment. After 6 months of steroid therapy, the right renal pelvis mass resolved, which retrospectively we believed was part of IgG4-RD manifestation rather than renal malignancy.
In a confirmed case of IgG4-RD, we postulate that a period of observation for steroid response may be applied to suspicious masses that fall into the category of typical IgG4-RD organ manifestations, sparing patients the need for invasive interventions. However, the optimal observation period remains uncertain and future research is needed.
Patient’s perspective.
When I noticed unexplained swellings over my neck in November 2018, I sensed something amiss with my health. I was more concerned when I noticed the swelling became increasingly bigger. It was then when I decided to seek for medical opinion. Things became more distressing when I was informed that those swellings were actually lymph nodes enlargement and could mean infections, tuberculosis, or cancer.
Being the sole bread winner of my family with two young children, the word cancer weighed heavily on my mind. I underwent multiple scans, tissue biopsies and multiple surgeries to remove my neck lymph nodes. I also underwent a painful bone marrow aspiration procedure. All the procedural pain and fear was somewhat abated when I was told that I most likely do not have a lymphoma. Tuberculosis screen were also negative.
For more than six months, nobody knew what was my diagnosis. I was treated with repeated courses of antibiotics to no avail. I was finally referred to the hospital’s rheumatologist in late April 2019. I was then informed by the rheumatologist that I may have a rare condition known as the IgG4 related disease, and that I would need further detailed investigations in order to confirm the diagnosis. A special staining procedure was done on one of my biopsied lymph nodes samples and confirmed the diagnosis. I was started on steroids, and in a short period of time, my neck and eye swellings improved remarkably.
A further CT scan of my whole body showed a worrying mass within my right kidney. My world shattered when I was once again informed that the mass could represent cancer, and a biopsy would be necessary. Due to coronavirus pandemic, the renal biopsy was postponed multiple times. Right before the scheduled biopsy date, a repeated ultrasound and CT scan showed complete resolution of the kidney mass. It was a shocking, but pleasant news. I am now under both rheumatology and urology follow up.
My current concern is mainly raised blood pressure due to the steroids that I am taking. I am hopeful that this is temporary and my blood pressure will normalize when I no longer require steroids, and the disease will not recur. All in all, I am very thankful for the doctors who have treated me with utmost professionalism, and acted promptly to elucidate the cause of my symptoms.
Learning points.
IgG4-related disease (IgG4-RD) is characterised by dense lymphoplasmacytic infiltration rich in IgG4-positive plasma cells with storiform fibrosis, often but not always, raised serum IgG4 level.
It affects various organs, manifests as diffuse organ enlargement or mass-like lesion, mimicking malignancy.
There is an increased incidence of malignancy among patients with IgG4-RD.
First-line treatment for IgG4-RD is glucocorticoid, which has excellent treatment response.
Acknowledgments
We would like to thank the patient for consenting to the writing up of this case report.
Footnotes
Contributors: ELL consulted and diagnosed the patient’s disease. SHN arranged for the patient’s tissue samples for staining. ELL, SHN and JST were involved in the care and management of the patient, and contributed equally to the writing up of this case report.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kamisawa T, Zen Y, Pillai S, et al. Igg4-Related disease. Lancet 2015;385:1460–71. 10.1016/S0140-6736(14)60720-0 [DOI] [PubMed] [Google Scholar]
- 2.Deshpande V, Zen Y, Chan JK, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol 2012;25:1181–92. 10.1038/modpathol.2012.72 [DOI] [PubMed] [Google Scholar]
- 3.Brito-Zerón P, Bosch X, Ramos-Casals M, et al. Igg4-Related disease: advances in the diagnosis and treatment. Best Pract Res Clin Rheumatol 2016;30:261–78. 10.1016/j.berh.2016.07.003 [DOI] [PubMed] [Google Scholar]
- 4.Khosroshahi A, Bloch DB, Deshpande V, et al. Rituximab therapy leads to rapid decline of serum IgG4 levels and prompt clinical improvement in IgG4-related systemic disease. Arthritis Rheum 2010;62:1755–62. 10.1002/art.27435 [DOI] [PubMed] [Google Scholar]
- 5.Morgan WS. The probable systemic nature of Mikulicz's disease and its relation to Sjögren's syndrome. N Engl J Med 1954;251:5–10. 10.1056/NEJM195407012510102 [DOI] [PubMed] [Google Scholar]
- 6.Yamamoto M, Takahashi H, Ohara M, et al. A new conceptualization for Mikulicz's disease as an IgG4-related plasmacytic disease. Mod Rheumatol 2006;16:335–40. 10.3109/s10165-006-0518-Y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Umehara H, Okazaki K, Masaki Y, et al. A novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Mod Rheumatol 2012;22:1–14. 10.3109/s10165-011-0508-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mattoo H, Mahajan VS, Maehara T, et al. Clonal expansion of CD4(+) cytotoxic T lymphocytes in patients with IgG4-related disease. J Allergy Clin Immunol 2016;138:825–38. 10.1016/j.jaci.2015.12.1330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wallace ZS, Deshpande V, Mattoo H, et al. Igg4-Related disease: clinical and laboratory features in one hundred twenty-five patients. Arthritis Rheumatol 2015;67:2466–75. 10.1002/art.39205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yamamoto M, Takahashi H, Tabeya T, et al. Risk of malignancies in IgG4-related disease. Mod Rheumatol 2012;22:414–8. 10.3109/s10165-011-0520-x [DOI] [PubMed] [Google Scholar]
- 11.Bledsoe JR, Wallace ZS, Stone JH, et al. Lymphomas in IgG4-related disease: clinicopathologic features in a Western population. Virchows Arch 2018;472:839–52. 10.1007/s00428-017-2286-9 [DOI] [PubMed] [Google Scholar]
- 12.Ahn SS, Song JJ, Park Y-B, et al. Malignancies in Korean patients with immunoglobulin G4-related disease. Int J Rheum Dis 2017;20:1028–35. 10.1111/1756-185X.13093 [DOI] [PubMed] [Google Scholar]
- 13.Lei W-H, Xin J, Shao C-X, et al. Igg4-Related kidney disease mimicking malignant ureter tumor: case report and literature review. Medicine 2016;95:e2550. 10.1097/MD.0000000000002550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bertoglio P, Viti A, Paiano S, et al. Igg4-Related disease: a new challenging diagnosis mimicking lung cancer. Interact Cardiovasc Thorac Surg 2019;28:410–2. 10.1093/icvts/ivy279 [DOI] [PubMed] [Google Scholar]
- 15.Malik SM, Raina A, Hartman DJ. Immunoglobulin G4-related pseudotumor presenting as metastatic colon cancer. Clin Gastroenterol Hepatol 2015;13:e1–2. 10.1016/j.cgh.2014.08.034 [DOI] [PubMed] [Google Scholar]
- 16.Khosroshahi A, Wallace ZS, Crowe JL, et al. International consensus guidance statement on the management and treatment of IgG4-related disease. Arthritis Rheumatol 2015;67:1688–99. 10.1002/art.39132 [DOI] [PubMed] [Google Scholar]
- 17.Kamisawa T, Okazaki K, Kawa S, et al. Japanese consensus guidelines for management of autoimmune pancreatitis: III. treatment and prognosis of AIP. J Gastroenterol 2010;45:471–7. 10.1007/s00535-010-0221-9 [DOI] [PubMed] [Google Scholar]
- 18.Hart PA, Topazian MD, Witzig TE, et al. Treatment of relapsing autoimmune pancreatitis with immunomodulators and rituximab: the Mayo clinic experience. Gut 2013;62:1607–15. 10.1136/gutjnl-2012-302886 [DOI] [PubMed] [Google Scholar]
- 19.Yamamoto M, Takahashi H, Ishigami K, et al. Relapse patterns in IgG4-related disease. Ann Rheum Dis 2012;71:1755. 10.1136/annrheumdis-2012-201694 [DOI] [PubMed] [Google Scholar]
- 20.Pozdzik AA, Brochériou I, Demetter P, et al. Azathioprine as successful maintenance therapy in IgG4-related tubulointerstitial nephritis. Clin Kidney J 2012;5:225–8. 10.1093/ckj/sfs048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yunyun F, Yu P, Panpan Z, et al. Efficacy and safety of low dose mycophenolate mofetil treatment for immunoglobulin G4-related disease: a randomized clinical trial. Rheumatology 2019;58:52–60. 10.1093/rheumatology/key227 [DOI] [PubMed] [Google Scholar]
- 22.Wallace ZS, Naden RP, Chari S, et al. The 2019 American College of Rheumatology/European League against rheumatism classification criteria for IgG4-related disease. Ann Rheum Dis 2020;79:77–87. 10.1136/annrheumdis-2019-216561 [DOI] [PubMed] [Google Scholar]