Abstract
Study design
Retrospective cohort study.
Objectives
To determine the incidence and characteristics of newly injured individuals admitted to a traumatic spinal cord injury (TSCI) referral center during a 4-year period.
Setting
University Hospital of Valle, Cali, Colombia.
Methods
Individuals were identified, and their data was recorded based on the International Spinal Cord Injury Core Data Set. The outcome of interest was the American Spinal Injury Association Impairment Scale (AIS) grade at the last follow-up.
Results
There were 491 individuals admitted in the 4-year period. The mean annual incidence of TSCI was 56.27 per million inhabitants. Considering TSCI in individuals exclusively from Cali, the mean annual incidence was 27.78 per million. The leading cause of TSCI was interpersonal violence (47.25%) and falls (33.60%). There was a strong correlation between AIS grade at admission and last follow-up. The most common AIS grade at the last follow-up was E (34.01%) caused mostly by falls (57.48%), followed by A (31.16%) caused mostly by interpersonal violence (76.27%). The reported employment rate dropped from 75.56% to 18.94% before and after TSCI (p < 0.05). AIS grade A was associated with more post-injury complications (p < 0.05).
Conclusions
This is the first cohort study in Colombia describing the incidence and AIS grades of individuals with TSCI from a trauma referral center. Interpersonal violence was overrepresented in this population. Future research should include the evaluation of prevention strategies, as well as research on interventions towards quality improvement in patient care and post-discharge services especially for individuals with AIS grade A.
Subject terms: Epidemiology, Outcomes research
Introduction
Traumatic spinal cord injuries (TSCI) are a global public health problem due to their high mortality and morbidity [1, 2]. TSCI can cause temporary or permanent changes in sensory, motor, or autonomic functions, frequently associated with trauma of intentional and non-intentional origin. According to the World Health Organization (WHO), the main causes of TSCI are road traffic injuries (RTI), violence, and falls [1]. Annually, there are between 250,000 and 500,000 new cases of TSCI worldwide [1], resulting in a global annual incidence of 10.5 cases per 100,000 persons [3]. This varies between countries and regions.
In addition to physical limitation, TSCI confers concomitant restrictions in leisure and working activities, especially in low resource settings [1], which adds to individual distress. The economic impact of TSCI is reflected by the high level of acute care and secondary complications following the injury. A study in the United States found that the average indirect cost incurred by a TSCI was $29,354 per person [4].
Furthermore, in a region that holds 14% of the world’s population but has 42% of interpersonal violence mortality [5], Colombia is a hot spot for violence. Cali is one of the most populous cities in the country and has been one of the most violent cities in the world for the last two decades [6]. In 2018, Cali had an estimated rate of 193.46 injuries and caused by interpersonal violence and 107.39 RTI per 100,000 inhabitants [7]. Approximately 370,000 disability-adjusted life years are lost yearly due to these events [8]. It has been estimated that 1 out of every 40 Colombians who enter the emergency department has a TSCI [9], and despite efforts to strengthen surveillance in injuries and trauma in the country [7, 10], there is little available information about the epidemiological and clinical characteristics of individuals with TSCI [11, 12]. The WHO has called attention to the lack of accurate identification of incidence and prevalence of TSCI both in high and low-income countries, but especially on the latter [1].
Low to middle-income countries have lower TSCI survival rates compared to high-income countries [2], which could indicate decreased rates of improvement during hospitalization. However, to the best of our knowledge, there is no epidemiological data comparing AIS scales at admission and follow-up in Colombia.
In this study, we describe TSCI and clinical outcomes experienced in Colombia’s main referral trauma center in Cali. We aim to provide epidemiological information on TSCI as well as information related to hospitalization and rehabilitation, in order to identify areas for further research.
Methods
Study type
Retrospective cohort study of individuals with TSCI who consulted to a trauma referral center in Cali between 2009–2012 followed until their last follow-up with physiatry. Sociodemographic and clinical information was collected from medical records using a standardized form based on International Spinal Cord Injury Core Data Sets [13].
Study setting
The study was carried out at the University Hospital of Valle (HUV), which is a public hospital of high complexity located in Cali. It is the main referral center in the public network of hospitals in Valle del Cauca (22,195 km2) and the southwestern region of Colombia. The hospital treats ~7081 individuals per year due to trauma and injuries [10].
Study population
We included all individuals with an emergency who consulted the trauma center. Included individuals had a diagnosis of TSCI according to the International Classification of Disease in its tenth version without discrimination by age, sex, origin, or ethnicity. Individuals were excluded if they had incomplete records (n = 3).
Data collection
Information was collected by healthcare personnel trained in data collection and data quality. The medical records of individuals diagnosed with TSCI were given by the Administrative department at the Hospital and the information was collected in a predesigned form in EpiInfo 7.0. We collected sociodemographic variables, injury mechanism, clinical examination at first and last assessment (general and neurological), and rehabilitation services [13].
Individuals were classified according to the neurological level and extent of the injury, applying the AIS upon admission and at the last consultation on the medical record [14]. The causes of TSCI were categorized as: (1) unintentional injuries (RTI, falls, diving injuries, and work injuries) and (2) intentional injuries (interpersonal violence and self-inflicted injuries). since the last visit since injury was categorized in <30 days, 1–3 months, 3–6 months, and >6 months. Age of participants was categorized as 0–15, 16–30, 31–45, 46–60, 61–75, ≥76, and grouped as ≤60 or >60 years.
Statistical analysis
Data was exported into Stata 16.0 (STATA Corp., Texas, US)® for analysis. Univariate descriptive analysis was performed calculating measures of central tendency and dispersion for quantitative variables, as well as frequencies and proportions for categorical variables. We used population estimates from the National Department of Statistics of Colombia [15] to calculate the mean annual rates of TSCI.
Bivariate analyses were carried out based on the type of variable under analysis and the assumptions of the statistical tests. We used Chi2 and Fisher’s exact test for categorical variables, and t-test, ANOVA and Kruskall-Wallis for continuous variables. R Studio was used to calculate Fisher’s exact test for count data with simulated p value based on 1e + 7 replicates. Simple linear regressions were used to estimate the change in frequencies of types of injuries over time with 95% confidence intervals (95%CI). Pairwise correlation was used between AIS at admission and last follow-up. Statistically significant differences were defined as a p value < 0.05.
Results
Incidence
During the 4-year period, 491 individuals were admitted with TSCI. Almost half of the individuals came from Cali (49.29%). The mean annual incidence of TSCI for all the cases was 56.27 per million. For individuals only from Cali, this was 27.78 per million inhabitants.
TSCI individuals’ characteristics
The mean age was 33 ± 15 years (range 2–76), and 85.95% were male, for a male:female ratio of 6:1. People who were single and without insurance were younger compared to those married and with insurance (married vs. single, Mean difference [MD] = 9.15, 95%CI = 6.33–11.99, p < 0.0001; insured vs. without insurance, MD = 3.90, 95%CI = 1.02–6.78, p = 0.008). Employment rate drop 74.93% when comparing before and after the injury (75.56% vs. 18.94%, p = 0.006).
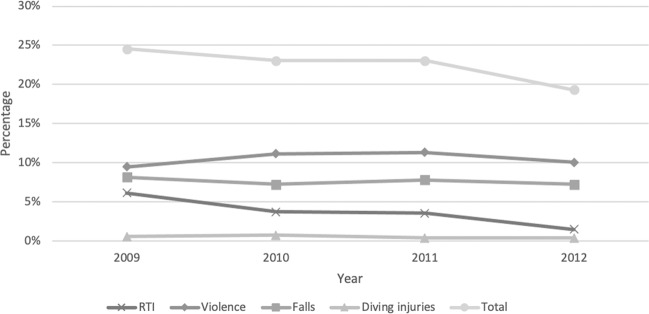
When comparing causes of TSCI over the years, we found a significant decrease in RTIs (β = −0.46, 95%CI = −0.73; −0.20, p = 0.001, R2 = 2.45%) and an increase in violence (β = 0.20, 95%CI = 0.007; 0.40, p = 0.042, R2 = 0.85%) (Fig. 1). We did not observe a change in age of the individuals over time (ANOVA, F = 0.76, p = 0.52), or injury mechanism. Injuries by mechanism are described in Table 1.
Fig. 1. Trends of proportions of traumatic spinal cord injuries by cause over years, 2009–2012.
Line graph showing percentage of traumatic spinal cord injury by cause from 2009 to 2012, and the percentage of total injuries caused in each individual year. Overall 4 years, violence caused the highest percentage of injuries, followed by falls, RTI, and diving injuries respectively. The percentage of total injuries caused in each year declined over time, with the highest proportion of injuries occurring in 2009, followed by 2010, 2011, and 2012, respectively. *RTI: road traffic injury.
Table. 1.
Sociodemographic and clinical characteristics of individuals with SCI at referral, grouped by injury type.
| Characteristics | All injuries (n = 491)* | Unintentional injuries (n = 258) | Intentional injuries (n = 233) | p value | ||
|---|---|---|---|---|---|---|
| Road traffic (n = 80) | Falls (n = 165) | Diving (n = 11) | Interpersonal violence (n = 232) | |||
| Age, mean (standard deviation) | 33.06 (14.75) | 36.59 (13.64) | 42.20 (15.66) | 21.82 (6.85) | 25.82 (9.81) | <0.0001a |
| Sex: Male, n (%) | 422 (85.95) | 63 (78.75) | 134 (81.21) | 11 (100) | 212 (91.38) | <0.002b |
| Educational level: ≥Secondary, n (%) | 223 (45.42) | 43 (53.75) | 59 (35.76) | 2 (18.18) | 116 (50.0) | <0.0001b |
| Origin: Cali, n (%) | 242 (49.29) | 19 (23.75) | 71 (43.03) | 1 (9.09) | 150 (64.66) | <0.0001b |
| Marital status: Without partner, n (%) | 274 (55.80) | 30 (37.50) | 86 (52.12) | 8 (72.73) | 149 (64.22) | <0.0001b |
| Covered by health insurance, n (%) | 323 (65.78) | 76 (95.0) | 104 (63.03) | 3 (27.27) | 139 (59.91) | <0.0001b |
| Injury level, n (%) | <0.0001c | |||||
| Cauda equina: Yes, n (%) | 43 (8.76) | 5 (6.25) | 5 (3.03) | 0 (0) | 32 (13.79) | |
| Cervical: Yes, n (%) | 151 (30.75) | 32 (40.0) | 41 (24.85) | 10 (90.91) | 68 (29.31) | |
| Lumbar: Yes, n (%) | 104 (21.18) | 17 (21.25) | 72 (43.64) | 0 (0) | 14 (6.03) | |
| Thoracic: Yes, n (%) | 192 (39.10) | 26 (32.50) | 47 (28.48) | 0 (0) | 118 (50.86) | |
| AIS Grade Classification first assessment [n (%)] | <0.0001c | |||||
| A | 158 (32.18) | 26 (20.0) | 17 (10.30) | 2 (18.18) | 123 (53.02) | |
| B | 33 (6.72) | 6 (7.50) | 6 (3.64) | 1 (9.09) | 20 (8.62) | |
| C | 38 (7.74) | 10 (12.50) | 13 (7.88) | 2 (18.18) | 13 (5.60) | |
| D | 54 (11.0) | 8 (10.0) | 31 (18.79) | 2 (18.18) | 13 (5.60) | |
| E | 165 (33.60) | 36 (45.0) | 93 (56.36) | 4 (36.36) | 30 (12.93) | |
*Working injuries (n = 1), Self-inflicted injuries (n = 1).
aKruskal–Wallis.
bFisher’s exact test.
cFisher’s exact test for count data with simulated p value based on 1e + 7 replicates.
Most of the individuals went directly to the referral center (80.45%). Once in the hospital, 32.18% were seen by the Physical Medicine and Rehabilitation Department. Additional rehabilitation services were provided in the hospital to 49.49% of the individuals, including physical therapy (41.14%), respiratory therapy (36.05%), occupational therapy (14.66%), and phonoaudiology (2.85%). During hospitalization, 27.29% of the individuals developed complications; 11.20% developed pressure ulcers, 11% urinary infections, 10.39% neuropathic pain, 1.22% autonomic dysreflexia, and 1.02% developed deformities.
Follow-up with physical medicine within the same institution was provided to 41.75% of the individuals; 18.05% of these individuals were seen within the next 30 days, 34.15% within the next 3 months, 29.76% within the next 6 months, and 16.59% after more than 6 months. The median number of appointments for follow-up with the clinic of TSCI was 1 (interquartile range: 0–2).
TSCI by the mechanism of Injury
Based on the trauma mechanism, 47.45% of the TSCIs were caused by intentional injuries and 52.55% were caused by unintentional injuries. Falls were the most common cause of unintentional injuries (33.60%), followed by RTI (16.29%), and diving injuries (2.24%). Amongst intentional injuries, 99.57% (n = 232) were caused by interpersonal violence and 0.43% (n = 1) was a self-inflicted injury.
Only 5.09% of the participants were older than 60 years old. TSCIs caused by violence were significantly higher in the ≤60 years old group (49.23% vs. 4.00%, p < 0.0001). Falls caused more TSCIs in the >60 group (31.21% vs. 76.00%, p < 0.0001). Fig. 2 describes the percentage of injuries by mechanism, sex, and age groups.
Fig. 2. Etiology of spinal cord injury grouped into sex and age categories.
Bar graph showing the percentage of spinal cord injuries grouped by etiology and separated by age and sex. There was a higher percentage of males across all etiologies of spinal cord injury. Interpersonal violence caused the highest percentage of injuries, and the age group of 16–30 years old were most represented in this group.
Unintentional injuries: falls
Individuals with TSCI due to falls had a mean age of 42 ± 16 years, male:female ratio of 4:1, and 33.94% had ages between 46 and 60 years. Only two-thirds of these individuals had healthcare insurance.
Road traffic injuries
RTIs were the only injury type associated with days of the week (weekend days: Friday to Sunday inclusive, 65% vs. 35%, p = 0.03) Male to female ratio was 4:1, and 42.50% of the individuals were between 16 and 30 years of age.
Diving injuries
This was the youngest group of SCI by injury mechanism, with a mean age of 21.82 years (p = 0.0001) with the group from 16 to 30 years of age having 63.64% of the traumas. In this group there were no women and only 9.09% were from Cali. Almost half of individuals had a traumatic brain injury (45.45%), whereas out of all individuals with TSCI 9.37% had a traumatic brain injury (p = <0.0001).
Intentional injuries: interpersonal violence
Individuals with TSCI due to violence were the second youngest group with 61.64% in the age group of 16 to 30 years, with a male:female ratio of 9:1. Individuals were injured mostly by a gunshot (90.52%) followed in a smaller proportion by a knife (8.62%), or other weapons (0.86%). In this subgroup, 53.02% of the individuals had an AIS grade A injury, and the most common etiology was a gunshot (98.37%), out of which, 68.60% (83) occurred at the thoracic level.
Individuals injured by a gunshot were younger (knife: n = 20, mean=30 ± 11, gunshot: n = 210, mean=25 ± 9, others: n = 2, mean = 50 ± 31, Kruskal–Wallis p = 0.01), had more traumatic brain injuries (knife 14.29%, gunshot 71.43%, others 14.29%, p = 0.04), and more commonly classed as AIS grade A compared with other types of weapons (A 98.37%, B 85%, C 46.15%, D 61.54%, E 86.67%; p < 0.05).
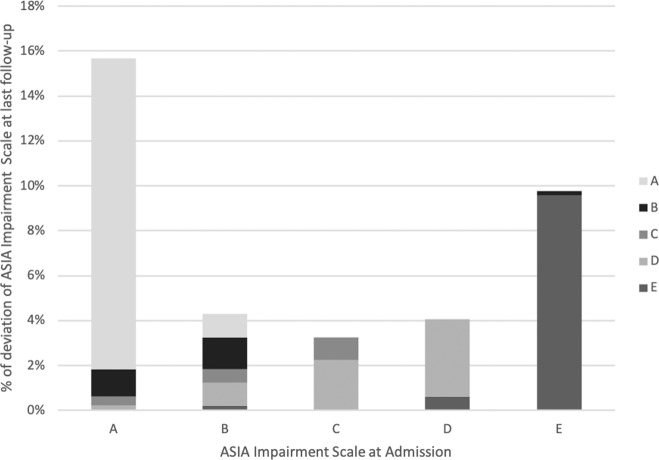
AIS at last follow-up
AIS grade at follow-up was only identified in 41.14% of the individuals and its relationship with the study variables is described in Table. 2. The correlation between AIS grade at admission vs. last follow-up was 92.87% (p < 0.0001). AIS grades B and C were the classifications with higher changes in AIS grade from admission to last follow-up, with 33.33% (7/21) and 31.25% (5/16) of the individuals classified that way in admission remaining the same at the last follow-up, respectively (See Fig. 3). AIS grade A was associated with higher complications rates.
Table 2.
Sociodemographic and clinical characteristics of individuals with SCI, grouped by AIS grade at last follow-up.
| Characteristic | AIS at last follow-up (n = 202, 41.14%) | p value | |||||
|---|---|---|---|---|---|---|---|
| A n = 73 (14.87%) | B n = 14 (2.85%) | C n = 11 (2.24%) | D n = 34 (6.92%) | E n = 51 (10.39%) | Not testable n = 19 (3.87%) | ||
| Age, mean (standard deviation) | 27.27 (10.71) | 28.85 (10.14) | 35.18 (9.38) | 36.47 (14.47) | 40.71 (15.66) | 27.33 (10.28) | 0.0001a |
| Sex: Male, n (%) | 67 (91.78) | 14 (100) | 11 (100) | 28 (82.35) | 35 (68.63) | 17 (89.47) | 0.004b |
| Educational level: ≥Secondary, n (%) | 48 (65.75) | 9 (64.29) | 3 (27.27) | 17 (50) | 28 (54.90) | 7 (36.84) | 0.12b |
| Origin: Cali, n (%) | 45 (61.64) | 8 (57.14) | 5 (45.45) | 18 (52.94) | 19 (37.25) | 13 (68.42) | 0.08b |
| Marital status: Without partner, n (%) | 41 (56.16) | 8 (57.14) | 4 (36.36) | 18 (52.94) | 28 (54.90) | 6 (31.58) | 0.12b |
| Covered by health insurance, n (%) | 50 (68.49 | 7 (50) | 7 (63.64) | 26 (76.47) | 41 (80.39) | 14 (73.68) | 0.35b |
| Mechanism, n (%) | |||||||
| RTI | 5 (6.85) | 2 (14.29) | 2 (18.18) | 6 (17.65) | 14 (27.45) | 1 (5.26) | 0.03b |
| Violence | 62 (84.93) | 11 (78.57) | 6 (54.55) | 16 (47.06) | 3 (5.88) | 12 (63.16) | <0.0001c |
| Fall | 5 (6.85) | 1 (7.14) | 3 (27.27) | 11 (32.35) | 33 (64.71) | 5 (26.32) | <0.0001b |
| Diving injury | 1 (1.37) | 0 (0) | 0 (0) | 1 (2.94) | 0 (0) | 0 (0) | 0.69b |
| Injury level, n (%) | <0.0001d | ||||||
| Cauda equina | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 17 (89.47) | |
| Cervical | 20 (27.40) | 5 (35.71) | 4 (36.36) | 19 (55.88) | 12 (23.53) | 1 (5.26) | |
| Lumbar | 1 (1.37) | 1 (7.14) | 3 (27.27) | 4 (11.76) | 27 (52.94) | 1 (5.26) | |
| Thoracic | 52 (71.23) | 8 (57.14) | 4 (36.36) | 11 (32.35) | 12 (23.53) | 0 (0) | |
| Complications, n (%) | |||||||
| Urinary infection | 22 (30.14) | 4 (28.57) | 3 (27.27) | 6 (17.65) | 0 (0) | 1 (5.26) | <0.0001b |
| Neuropathic pain | 22 (30.14) | 4 (28.57) | 1 (9.09) | 8 (23.53) | 0 (0) | 3 (15.79) | <0.0001b |
| Pressure ulcer | 29 (39.73) | 5 (35.71) | 1 (9.09) | 2 (5.88) | 0 (0) | 0 (0) | <0.0001b |
aKruskal–Wallis.
bFisher’s exact test.
cChi square test.
dFisher’s exact test for count data with simulated p-value based on 1e + 7 replicates.
Fig. 3. ASIA impairment scale deviation from admission (X axis) to last follow-up (Y axis).
Bar graph comparing ASIA Impairment Scale deviation at follow up compared to admission, separated by ASIA Impairment Scale grades. Grade A was the most common grade at admission, followed by E, B, D, and C. Most individuals classified with grade A at admission remained as grade A at last follow-up.
Discussion
To the best of our knowledge, there are no studies describing the incidence of TSCI in Colombia. We found a mean annual incidence of 56.27 TSCI cases per million, with an overall decrease over the study period. This is higher than estimates of global annual TSCI incidence being 23 cases per million [2] and estimates of Andean Latin America having an annual TSCI incidence of 19 cases per million [2]. Considering TSCI cases of individuals from Cali only, the annual incidence was 27.78 cases per million. This is higher than the incidence in the Andean region and is comparable to the rate of 22 cases per million in the high-income country of New Zealand [16]. The differences in annual incidence rates may reflect contextual factors such as population demographics; however, a direct comparison of global incidence rates is hindered by the heterogeneity of different epidemiological studies [17].
There were relatively few individuals aged 60 years or older (n = 25; 5.09%) which differs from global trends of TSCI whereby falls in the elderly contribute to the higher mean age of individuals, such as in Finland where the mean age of TSCI individuals was 58.9 years [17]. Amongst those aged ≥60, falls caused a significantly higher proportion of injuries. This supports previous studies [1, 17], which therefore reinforces the importance of fall prevention amongst the elderly.
We observed a ratio of 6:1 male to female in all TSCI individuals, and a ratio of 9:1 male in those caused by interpersonal violence. Globally, whilst males remain overrepresented in the TSCI population [2], higher income countries report smaller gender gaps between male and female TSCIs [18–20]. Lower to middle income countries, such as Mexico, Afghanistan, Bangladesh, and India reported a similar ratio of male to female individuals as observed in our study [19, 21, 22]. Despite the fact that this gender difference be explained by the higher risk-taking and impulsive behavior of males [23], in the context of our study, interpersonal violence amongst males is more likely to be a contributing factor [10]. Although an increase in the provision of public goods could be an effective strategy to improve urban safety [6], violence in Colombia is a complicated and multifaceted issue that requires a multidisciplinary approach.
In addition, we found high rates of low education levels, single marital status, and lack of insurance in the studied population. Low education levels being associated with TSCI were also reported in Mexico where 50% of the participants with a TSCI only had elementary school education [22]. Marital status may be a positive predictive factor in terms of independent living after TSCI [1]. Being single and lacking insurance was associated with younger age; therefore, prevention programs should target younger age groups.
Overall, the most frequent cause of TSCI was interpersonal violence, followed by falls, RTI, diving injuries, work injuries, and self-inflicted injuries. RTIs were associated with weekends. This may be explained by the higher prevalence of driving under the influence of alcohol on weekends in the city [24]. However, there was also a reduction in the proportion of RTI over time (Fig. 1), which differs from a study in Sao Paulo, Brazil, which found an increase in the frequency of RTIs over time [25]. The different TSCI trends in these two cities may reflect the socioeconomic differences between them and the implementation of road safety interventions in Cali [26, 27].
Across all TSCIs, the most common severity was AIS grade A, which was associated with the TSCIs caused by interpersonal violence. Within this group, gun violence had the most common etiology, causing 90.52% of injuries caused by interpersonal violence and almost 50% of all TSCIs. This is higher than studies in other low- to middle-income countries, which reported rates of firearms causing 16.8 and 15% of TSCIs [21, 22]. The high rate of gun related TSCIs can be explained by the high rates of gun violence in Cali [6]. Even though there have been municipal programs attempting to control gun use in the city, a more effective national gun control scheme would be beneficial [28].
Regarding services accessed during hospitalization, 49.49% of individuals were provided with rehabilitation services. This is comparable to higher income countries such as Portugal, where after the patient becomes clinically stable, more than half are transferred to a rehabilitation center [20]. However, the reported rate of employment dropped 75% after the injury. In Portugal, outpatient services including two specialized vocational rehabilitation programs are provided through the National Health System [20]. Therefore, the provision and engagement with such services in Colombia may be a strategy to increase the rate of post-injury employment.
Furthermore, 11.20% of individuals developed pressure ulcers during hospitalization. This is lower than the 37% prevalence of in-hospital pressure ulcer described in Afghanistan [21]. Urinary tract infections (UTIs) are another preventable issue which occurred in 11% of the observed individuals. This is lower when compared to other studies, such as from Turkey after 50 days post TSCI (22%) [29] and Afghanistan (57%) [21].The fact that UTIs are much more prevalent in women compared to men and that the majority of participants in our study were male may partially explain the comparatively lower rate of UTIs in our study. However, when compared to Afghanistan which had a similar male:female ratio as in our study [21], this may indicate that HUV was relatively successful in preventing and treating UTI. In addition, 10.39% of individuals developed neuropathic pain and 1.22% developed autonomic dysreflexia. UTI may exacerbate SCI-related secondary complications; [1] therefore management and prevention of UTI is essential.
At last follow-up, a strong correlation (92.87%) was found between AIS grade at admission and at discharge. Grades B and C had the highest deviation from initial AIS grade. More than 95% of AIS A individuals maintained this status (68/77). In Norway, 77% of individuals remained grade A at discharge [18]. AIS grade A was also correlated with a higher rate of complications. Therefore, our study shows that while there have been improvements in medium level injuries (AIS grades B and C), there is potential for improvement for AIS grade A injuries as well as increased provision of rehabilitation services within the hospital. However, in our study, follow-up within the same institution and continuity of care are issues to be addressed given that less than half of the individuals had a follow-up AIS assessment. In Finland, there is a government mandate that centralizes life-long SCI follow up to three specific hospitals which has enabled a long-term coverage of TSCI cases [17]. A similar mandate in Colombia could help increase follow-up rates and continuity of care, towards better patient outcomes.
The study has limitations that are adherent to the design. The sampling method limits the extrapolation of results. However, data was collected from the main trauma referral center of southwestern Colombia [10], and by trained personnel based on a standardized dataset [13]. Likewise, the study avoided selection bias that would arise from only collecting data from specialized services. Recent years saw the growth of the Clinic Fundación Valle del Lili [10], from which we were not able to include data. Although our data could underestimate the incidence, our study provides a good approximation of the situation in the region.
Conclusion
This is the first cohort study in Colombia describing the incidence and AIS grades of individuals with TSCI. Interpersonal violence, specifically gun violence in young males, was overrepresented in this study. Greater provision of rehabilitation services during hospitalization would improve the follow-up outcomes of individuals, especially those with AIS A. Quality improvement projects as well as further research are required to identify factors associated with complications and evaluate the efficacy of preventive strategies.
Acknowledgements
The authors thank Adnan Mujanović for his critical revisions to the manuscript.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Compliance with ethical standards
Conflict of interest
The authors declare no competing interests.
Ethics
The study was approved by the University Hospital of Valle Ethics Committee and the Human Ethics Committee of the Universidad del Valle with code 143-018. The authors certify that all applicable institutional and governmental regulations concerning the ethical use of human’s information were followed during the course of this research and the Institutional Review Board waived the requirement for informed consent to access patient health information as the study does not involved more than minimal risk to the privacy of individuals.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.International perspectives on spinal cord injury. World Health Organization International Spinal Cord Society; 2013. Report No.: 9241564660.
- 2.Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 2014;52:110–6. doi: 10.1038/sc.2012.158. [DOI] [PubMed] [Google Scholar]
- 3.Kumar R, Lim J, Mekary RA, Rattani A, Dewan MC, Sharif SY, et al. Traumatic spinal injury: global epidemiology and worldwide volume. World Neurosurg. 2018;113:e345–e63. doi: 10.1016/j.wneu.2018.02.033. [DOI] [PubMed] [Google Scholar]
- 4.Cao Y, Krause JS. Estimation of indirect costs based on employment and earnings changes after spinal cord injury: an observational study. Spinal Cord. 2020;58:908–13. doi: 10.1038/s41393-020-0447-1. [DOI] [PubMed] [Google Scholar]
- 5.Muggah R, Tobón KA. Reducing Latin America’s violent hot spots. Aggress Violent Behav. 2019;47:253–6. doi: 10.1016/j.avb.2018.09.003. [DOI] [Google Scholar]
- 6.Martínez L, Prada S, Estrada D. Homicides, public goods, and population health in the context of high urban violence rates in Cali, Colombia. J Urban Health. 2018;95:391–400. doi: 10.1007/s11524-017-0215-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Institute of Legal Medicine and Forensic Sciences V. [Forensis 2018. Data for life] Bogota, D.C.: National Institute of Legal Medicine and Forensic Sciences; 2019 [cited 27 Dec 2020]. https://www.medicinalegal.gov.co/documents/20143/386932/Forensis+2018.pdf/be4816a4-3da3-1ff0-2779-e7b5e3962d60.
- 8.Instituto Nacional de Salud. Protocolo de Vigilancia en Salud Pública. Lesiones de Causas Externas. Bogotá: Instituto Nacional de Salud; 2016.
- 9.Castaño A. Lesiones no fatales en accidentes de tránsito-Colombia, 2005. Instituto nacional de medicina legal y ciencias Forenses-DRIP; 2006.
- 10.Ordoñez CA, Morales M, Rojas-Mirquez JC, Bonilla-Escobar FJ, Badiel M, Miñán Arana F, et al. Trauma Registry of the Pan-American Trauma Society: one year of experience in two hospitals in southwest Colombia. Colomb Med. 2016;47:148–54. doi: 10.25100/cm.v47i3.1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teheran AACO, Frade LL. Incidence and characteristics of spinal trauma in a level III hospital, Bogotá 2011–2014] Panam J Trauma Crit Care Emerg Surg. 2016;5:140–7. doi: 10.5005/jp-journals-10030-1157. [DOI] [Google Scholar]
- 12.Carvajal CPC, Gomez-Rojo C, Calderon J, Cadavid C, Jaimes F. Clinical and demographic characteristics of patients with spinal cord injury. Six years experience. Acta Med Colomb. 2014;40:45–50. [Google Scholar]
- 13.DeVivo M, Charliefue S, V Noonan V, Post M, Stripling T, Wing P. International spinal cord injury core data set. Nature; 2006. p. 535-40. [DOI] [PubMed]
- 14.Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011) J Spinal Cord Med. 2011;34:535–46. doi: 10.1179/204577211X13207446293695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.(DANE). ADoNS. Population projections. Bogota D.C., DANE 2020 [updated Dec 16, 2020; cited 27 Dec 2020]. https://www.dane.gov.co/index.php/estadisticas-por-tema/demografia-y-poblacion/proyecciones-de-poblacion.
- 16.Mitchell J, Nunnerley J, Frampton C, Croot T, Patel A, Schouten R. Epidemiology of traumatic spinal cord injury in New Zealand (2007–2016) NZ Med J. 2020;133:47. [PubMed] [Google Scholar]
- 17.Johansson E, Luoto TM, Vainionpää A, Kauppila A-M, Kallinen M, Väärälä E, et al. Epidemiology of traumatic spinal cord injury in Finland. Spinal Cord. 2020:1-8. https://www.nature.com/search?q=Epidemiology+of+traumatic+spinal+cord+injury+in+Finland&journal=sc; https://pubmed.ncbi.nlm.nih.gov/33149235/. [DOI] [PMC free article] [PubMed]
- 18.Halvorsen A, Pettersen AL, Nilsen SM, Halle KK, Schaanning EE, Rekand T. Epidemiology of traumatic spinal cord injury in Norway in 2012–2016: a registry-based cross-sectional study. Spinal Cord. 2019;57:331–8. doi: 10.1038/s41393-018-0225-5. [DOI] [PubMed] [Google Scholar]
- 19.Ning G-Z, Wu Q, Li Y-L, Feng S-Q. Epidemiology of traumatic spinal cord injury in Asia: a systematic review. J Spinal Cord Med. 2012;35:229–39. doi: 10.1179/2045772312Y.0000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Campos I, Margalho P, Lopes A, Branco C, Faria F, Caldas J, et al. People with spinal cord injury in Portugal. Am J Phys Med Rehabil. 2017;96(Suppl 1):S106–S8. doi: 10.1097/PHM.0000000000000616. [DOI] [PubMed] [Google Scholar]
- 21.Deconinck H. The health condition of spinal cord injuries in two Afghan towns. Spinal Cord. 2003;41:303–9. doi: 10.1038/sj.sc.3101443. [DOI] [PubMed] [Google Scholar]
- 22.Zárate-Kalfópulos B, Jiménez-González A, Reyes-Sánchez A, Robles-Ortiz R, Cabrera-Aldana EE, Rosales-Olivarez LM. Demographic and clinical characteristics of patients with spinal cord injury: a single hospital-based study. Spinal Cord. 2016;54:1016–9. doi: 10.1038/sc.2016.41. [DOI] [PubMed] [Google Scholar]
- 23.Cross CP, Copping LT, Campbell A. Sex differences in impulsivity: a meta-analysis. Psychol Bull. 2011;137:97–130. doi: 10.1037/a0021591. [DOI] [PubMed] [Google Scholar]
- 24.Bonilla-Escobar FJ, Herrera-López ML, Ortega-Lenis D, Medina-Murillo JJ, Fandiño-Losada A, Jaramillo-Molina C, et al. Driving under the influence of alcohol in Cali, Colombia: prevalence and consumption patterns, 2013. Int J Inj Contr Saf Promot. 2016;23:179–88. doi: 10.1080/17457300.2014.966120. [DOI] [PubMed] [Google Scholar]
- 25.Bellucci CH, Castro Filho JE, Gomes CM, Bessa Junior J, Battistella LR, Souza DR, et al. Contemporary trends in the epidemiology of traumatic spinal cord injury: changes in age and etiology. Neuroepidemiology. 2015;44:85–90. doi: 10.1159/000371519. [DOI] [PubMed] [Google Scholar]
- 26.Martínez-Ruíz DM, Fandiño-Losada A, Ponce de Leon A, Arango-Londoño D, Mateus JC, Jaramillo-Molina C, et al. Impact evaluation of camera enforcement for traffic violations in Cali, Colombia, 2008–2014. Accid Anal Prev. 2019;125:267–74.. doi: 10.1016/j.aap.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 27.Osorio-Cuéllar GV, Pacichana-Quinayaz SG, Bonilla-Escobar FJ, Fandiño-Losada A, Jaramillo-Molina C, Gutiérrez-Martínez MI. First motorcycle-exclusive lane (Motovia) in Colombia: perceptions of users in Cali, 2012–2013. Int J Inj Control Saf Promot. 2017;24:145–51.. doi: 10.1080/17457300.2015.1061563. [DOI] [PubMed] [Google Scholar]
- 28.Gun violence in Colombia. Bull World Health Organ. 2019;97:733–4. [DOI] [PMC free article] [PubMed]
- 29.Togan T, Azap OK, Durukan E, Arslan H. The prevalence, etiologic agents and risk factors for urinary tract infection among spinal cord injury patients. Jundishapur J Microbiol. 2014;7:e8905–e. doi: 10.5812/jjm.8905. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.