Abstract
Background
Management of complex wounds of the lower extremity with concomitant Achilles tendon injury is a challenging situation for orthopaedic surgeons and plastic surgeons. The objective of the current study was to evaluate the clinical outcome of chronic open defects of the Achilles tendon with composite tissue loss. We have performed single stage reconstruction using the central segment of the proximal part of the Achilles tendon as turn-down flap and was covered immediately with reverse sural flap.
Materials and methods
Between March 2017 and February 2020, five cases of chronic open composite Achilles tendon defects which were treated by a single stage reconstruction method of “Repair and Flap technique” were included in this study. The patient with the defect for more than 4 weeks duration and had substance loss of Achilles tendon together with loss of overlying skin and soft tissue was included the current study.
Results
All the flaps survived and healed well, providing stable coverage of the wound. The mean operative duration, including flap elevation, definitive flap inset and donor-site coverage was 98 min (range 90–120 min). Focal areas of skin graft loss were seen in two patients which healed with conservative management. The functional results evaluation was performed with The Achilles Tendon Total Rupture Score (ATRS). The mean Achilles Tendon Total Rupture Score (ATRS) was 70 (range 65–76)
Conclusion
To conclude, use of proximal turned down flap and coverage with reverse sural flap can be opted as a first option for the management of chronic open wounds with composite defects of the Achilles tendon. “Repair and Flap technique” will be a useful method of reconstruction in centres with limited resources for microsurgical flap. However, a multicenter study with more number of patients are required to further analyse this method.
Keywords: Repair and flap technique, Reverse sural flap, Achilles tendon, Chronic open wounds, Composite defect
Introduction
Composite defects of the Achilles tendon are observed following road traffic accidents and accidental slipping of the foot in the Indian type lavatory [1, 2]. Repair of composite Achilles tendon defects is a contentious issue regarding the timing [Immediate or delayed], stages [single stage or two stage] and primary application of flaps [3]. The management of acute wounds in Achilles tendon region is debridement and immediate repair of tendon. There is a dilemma for treatment of chronic open wounds whether to perform a single stage or multi stage reconstruction and the type of flap to be applied.
The management of chronic closed ruptures of Achilles tendon is a debatable topic and there are no consensus on method of reconstruction to be performed in chronic open wounds with composite tissue loss in the tendon Achilles region [4]. Ghosh et al. had described the use of facial turn-down flap for the repair of chronic Achilles tendon rupture [5]. Though microsurgical reconstruction has become the choice method of reconstruction, it may not be possible in every case owing to the lack of expertise, complexity of the procedure and post op care [6]. We present a series of cases of chronic open composite defects of the Achilles tendon which were repaired in one stage with proximal segment turn-down flap and reverse sural flap.
Materials and Methods
Between March 2017 and February 2020, five cases of chronic open composite Achilles tendon defects which were treated by a single stage reconstruction method of “Repair and Flap technique” were included in this study. Acute wounds and chronic closed wounds and open wounds in which other methods of skin cover used such as anterolateral thigh free flaps, lateral supra-malleolar flaps and perforator flaps were not included in this study.
Informed written consent was obtained from all patients prior to their enrolment in this study was obtained. The ethical committee approval was also obtained. The clinical records of these patients were reviewed. The clinical features reviewed were medical history of patient and medical comorbidites etiologic of injury, associated injuries, size of the defect. The functional results evaluation was performed with The Achilles Tendon Total Rupture Score (ATRS) [7]. This score is a questionnaire that is filled out by the patient and scored by the clinician. It consists of ten questions that evaluate the symptoms and function. Each question has scores ranging between 0 and 10 on a scale and has a maximum score of 100, which corresponds to no symptoms and full function. The mean age was 42.2 (range 11–72 years) and there were four males and one female patients. There was injury to right leg in four patients and affected left leg in one patient (Table 1). The mechanism of injury for Tendon Achilles rupture was two wheeler accident in three patient and accidental slippage in Indian type lavatory in two patients. Diabetes mellitus was observed in one patient and one patient was a chronic smoker.
Table 1.
Patient characteristics and defect details
| S.no | Age/Sex | Side | Aetiology | Associated injuries | Distal end | Gap (cm) | Comorbid conditions | Complications | Result | Follow up |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 38/M | R | Road traffic accident | Nil | Anchored to calcaneum | 10 | Smoker | Focal areas of skin graft loss | Healed with conservative management | 6 months |
| 2 | 11/M | R | Slipping in Indian Lavatory | Nil | Sutured to remnant distal end | 4 | Nil | Nil | Healed well | 1 year |
| 3 | 71/M | R | Slipping in Indian lavatory | Nil | Anchored to calcaneum | 10 | Diabetes | Focal areas of skin graft loss | Healed with conservative management | Lost to follow-up after 6 weeks |
| 4 | 72/F | L | Road traffic accident | Calcaneal fracture | Anchored to calcaneum | 6 | Nil | Nil | Healed well | 6 months |
| 5 | 19/M | R | Road traffic accident | Nil | Sutured to remnant distal end | 6 | Nil | Nil | Healed well | 3 months and still under follow up |
Surgical Technique
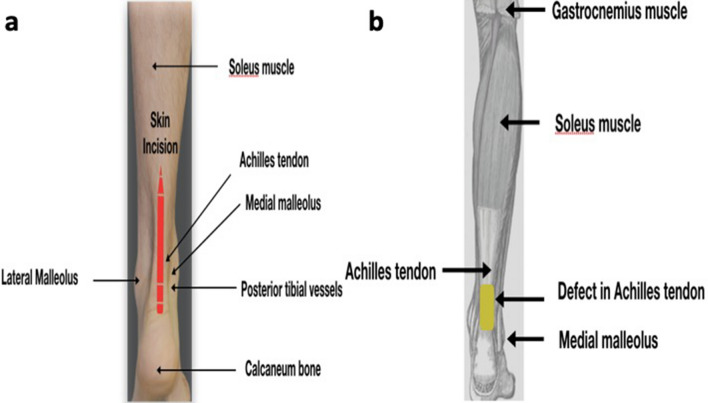
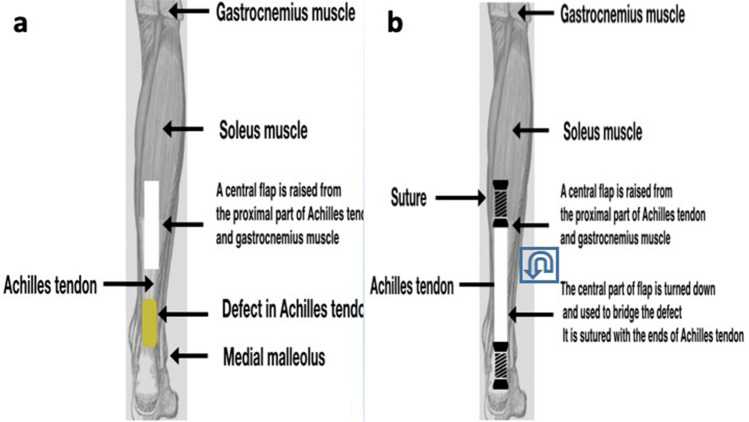
The “Repair and Flap technique” was used for chronic composite Achilles tendon defects and reconstruction was performed in single stage using the proximal turned down central segment of the Achilles tendon and immediate coverage with reverse sural flap (Fig. 1). All the patients were operated under spinal anaesthesia. Skin incision was marked over posterior aspect of leg (Fig. 2a) An approximate size of the defect was assessed. First step of surgical procedure was to achieve a healthy bed of tissue and a through debridement of wound was performed (Fig. 2b). This was followed by lavage of wound with normal saline. The perforators were located using a hand held Doppler and the reverse sural perforator signals were observed. After calculating the exact size of defect, the horizontal length of the expected defect was marked in a vertical direction along the length of the flap using the location of the perforator as a fulcrum for flap transposition. Then, we applied the tourniquet without exsanguination of the limb.
Fig. 1.
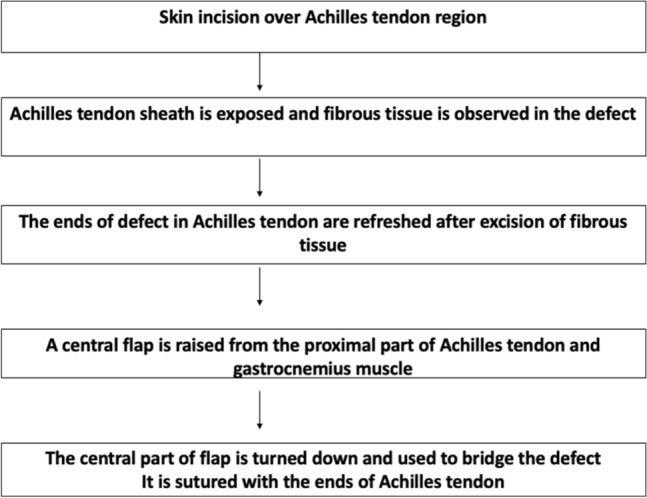
Algorithm of “Repair and Flap technique” was used for chronic composite Achilles tendon defects and reconstruction
Fig. 2.
a Skin incision marked over posterior aspect of leg, b first step of surgical procedure is to achieve a healthy bed of tissue and a through debridement of wound
The reverse sural flap was then raised after marking from distal to proximal until the selected perforator was reached using loupe magnification. The reverse sural flap was mobilised and was kept aside prior to repair of Achilles tendon. The central segment of the proximal fragment of the Achilles tendon was mobilised, folded and sutured to the remaining distal fragment in two cases (Fig. 3a, b). In three patients the distal end of Achilles tendon was anchored to the calcaneum bone. The mean size of defect was 7.2 cm (range 4–10 cm) and was calculated from the proximal bridging segment end of tendon to the point of insertion. We performed suturing of tendon with a help of double stranded Kessler’s technique. Multiple holes were created in calcaneum bone with help of a K wire for anchorage of Achilles tendon. We performed suturing and anchorage of the Achilles tendon with help of 2–0 nylon suture. The closure of flap was performed with 3–0 nylon suture.
Fig. 3.
a The central segment of the proximal fragment of the Achilles tendon mobilised, b the central segment of the proximal fragment of the Achilles tendon was mobilised, folded and sutured to the remaining distal fragment of tendoachilles
The donor site of the flap was covered with split skin grafts and drains were inserted. The lower limb was supported with an anterior below knee plaster slab. Post operatively, the patient was nursed in prone or lateral position for avoiding pressure on the flap and flap monitoring was done through a window in the dressing. Inspection and dressings of the skin graft to the flap donor site was done on fifth post-operative day and then once every week. Non-weight bearing ambulation was allowed at third post-operative day and full weight bearing was allowed after 6 weeks duration.
We have described the case study of patient number 1, which was of 72 years old female presented with post traumatic chronic non-healing wound over the left tendon calcaneal region (Fig. 4a–d). This patient was treated with fix and flap technique (Fig. 5a–d). Secondly we have described the case study of 11 years old boy who presented with a chronic non-healing wound over the right Achilles tendon region following accidental slippage of his foot in Indian type lavatory (Fig. 6a–d). This patient was treated with fix and flap technique (Fig. 7a–d).
Fig. 4.
Case 1: a clinical picture of the defect over the left Tendo Achilles, b radiograph showing the fractured and avulsed fragment of calcaneum, c wound debridement and a flap 7 × 5 cm was marked, d after elevation, the flap is kept aside and the Tendo Achilles reconstructed
Fig. 5.
Case 1: a flap inset given, drain inserted and flap donor site covered with split skin graft, b immediate post-operative clinical picture, c at 1-month follow-up, d at 2-month follow-up
Fig. 6.
Case 2: a clinical picture of the defect and wound over the right Tendo Achilles, b wound debridement and flap marking, c flap raised and kept aside, d after the completion of Tendo Achilles reconstruction, the flap was inset and flap donor site covered with split skin graft
Fig. 7.
Case 2: a immediate post-operative clinical picture. b At follow-up. c At 6 month follow-up. d At 1 year follow-up
Results
All the flaps survived and healed well, providing stable coverage of the wound. Full weight bearing ambulation was started in all the patients by the completion of 6 weeks. One patient was lost to follow-up after full weight bearing mobilisation [Case 3, in Table 1]. One patient [Case 5, in Table 1] is currently under follow-up. Rest of the patients were followed up from 3 months to 1 year. Functional improvement was restored with all the patients back to their routine activities. Total operative time, including flap elevation, definitive flap inset and donor-site coverage was 98 min (range 90–120 min).
All the patients had loss of sensation along the lateral border of the foot which is a known but acceptable side effect of the reverse sural flap [8]. Focal areas of skin graft loss were seen in two patients which healed with conservative management. Cosmetic deformity was acceptable to all the patients. The functional results evaluation was performed with The Achilles Tendon Total Rupture Score (ATRS). The mean Achilles Tendon Total Rupture Score (ATRS) was 70 (range 65–76).
Discussion
Chronic open composite defects of the Achilles tendon are uncommon and are difficult cases to be managed. The reconstructive surgeon faces a challenge of complex technical procedure for treatment. Chronic closed wounds are assessed with radiological investigation and managed according to the type of defect [4]. The open composite wound is evaluated with direct visualisation and assessment of tissue damage. According to review of literature; various methods of management of chronic wound in Achilles region have been described which includes simple skin grafting to complex microvascular procedures. The treatment of chronic open wound includes debridement of the wound and achieve a healthy granulation tissue and cover with split thickness skin graft [9]. The other reconstruction options following debridement includes use of the local pedicle flap and microvascular flap [7, 10–13] . We have compared the outcomes of current study with various published studies in which reverse sural flap was used for reconstruction (Table 2) [1, 10, 17–21].
Table 2.
Review of literature on Tendo Achilles repair with reverse sural flap reconstruction
| Author | Defect region | Achilles tendon repair(n = number of patients) | Type of flap | Complication | Outcome |
|---|---|---|---|---|---|
| Bullocks et al. [1] | Heel and ankle | Achilles tendon repair (n = 4) | Reverse sural artery flap | Partial flap loss (n = 1) | NR |
| Jepegnanam et al. [10] | Heel and ankle | Achilles tendon repair (n = 8) | Reverse sural artery flap | Terminal flap necrosis (n = 1) | Excellent |
| Boopalan et al. [18] | Posterior aspect of lower third leg | Infected Achilles tendon injury | Reverse flow sural flap | None | Excellent |
| Thomas et al. [19] | Heel | Achilles tendon repair | Reverse sural artery flap | None | NR |
| Abhyankar et al. [20] | Posterior aspect of heel | Achilles tendon repair (n = 6) | Superficial sural artery flap | Distal marginal necrosis (n = 1) | Good |
| Zheng et al. [21] | Posterior aspect of heel | Achilles tendon repair (n = 10) | Reverse sural neuro fasciocutaneous artery flap | Distal marginal necrosis (n = 1) |
Excellent (n = 7) Good (n = 3) |
| Current study | Posterior aspect of lower third leg | Achilles tendon repair (n = 5) | Reverse sural artery flap | Focal areas of skin graft loss (n = 2) | Excellent(n = 5) |
Wound debridement and coverage with split skin graft is a technically easy procedure and avoids the problems associated with flap surgery including post-operative positioning and monitoring of flap [8]. The coverage of wound with split thickness skin graft is reserved as last resort following a failure of multiple surgical attempts and patients with multiple medical comorbidites. Monnerie et al. described the treatment of necrosis of Achilles tendon without tendon reconstruction [9]. The authors reported the use of MRI in assessment of neo-tendon formation [9].
Reconstruction of tendoachilles and coverage with local pedicle flaps has been well described technique. The various methods of reconstruction includes fascia lata graft, turned down flaps from the proximal segment of the Achilles tendon and coverage with reverse sural flap, lateral supra-malleolar flap and perforator based propeller flaps [1, 13–15, 20]. Among the local pedicle flaps, the reverse sural flap has evolved as the important flap owing to its versatility, ease of elevation and application [16]. The common complications of reverse sural flap include venous congestion with distal flap necrosis [18]. We had reviewed the published literature and compared various studies of repair of chronic Achilles tendon tear and defect closure with reverse sural artery flaps (Table 2) [1, 10, 18–21].
In a study by Bullock et al. there was assessment of cases of acute injury of Achilles tendon and reconstruction with reverse sural flap [1]. In their series, the total operative time was calculated and was average of 287 min [1]. The flap elevation time with exposure of the Achilles tendon was with an average of 43 min [1]. Jepagnanam et al. had described good outcomes of single stage reconstruction with use of reverse sural flap in acute open wound of the Achilles tendon [10]. The authors in their series sutured the divided ends of Achilles tendon, used fascia lata graft or turned down flaps [10].
The incidence of wound complications following exposure for Achilles tendon surgery are higher than that of other standard surgical incisions [22]. The reason for higher complication rate are thin subcutaneous tissue over the Achilles tendon, limited blood supply and limited mobility of the skin. Bullock et al. a had reported partial loss of flap in a patient [1]. Jepagnanam et al. in a series had reported one partial flap loss which later required skin grafting [10]. In this current study there were no major complications and there were no partial or complete flap loss. The better success rate could be due to technical refinements such as inclusion of additional perforators at the flap base, wider subcutaneous pedicle and avoidance of tunnelling.
The use of microvascular flaps to the reconstruction complex defects of the Achilles tendon involves use of free anterolateral thigh fascia lata flap, latissimus dorsi free muscle flap and gracilis free flaps [6, 10, 11]. Ehrl et al. has suggested that the anterolateral thigh flap provides excellent outcomes [6].
The limitations of current study were this was a retrospective study and had heterogeneity of the study population. The use of nylon 2–0 in current study is not a common suture material for repair of Achilles tendon and needs more studies to justify it [23].
Secondly there were limited number patient with chronic open wound of Achilles tendon. This technique requires further validation with a multi-centre studies.
Conclusion
To conclude, use of proximal turned down flap and coverage with reverse sural flap can emerge as an option for the management of chronic open wounds with composite defects of the Achilles tendon. “Repair and Flap technique” will be a useful method of reconstruction in centres with limited resources for microsurgical flap.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Standard Statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Contributor Information
G. I. Nambi, Email: nambi75@rediffmail.com
Abhijeet Ashok Salunke, Email: drabhijeetsalunke@gmail.com.
References
- 1.Bullocks JM, Hickey RM, Basu CB, et al. Single-stage reconstruction of Achilles tendon injuries and distal lower extremity soft tissue defects with the reverse sural fasciocutaneous flap. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2008;61(5):566–572. doi: 10.1016/j.bjps.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 2.Chatterjee SS, Sarkar A, Misra A. Management of acute open tendo-achilles injuries in Indian lavatory pans. Indian Journal of Plastic Surgery. 2006;39(1):29–33. doi: 10.4103/0970-0358.26900. [DOI] [Google Scholar]
- 3.Said MN, Al Dosari AAM, et al. Open Achilles tendon lacerations. European Journal of Orthopaedic Surgery & Traumatology. 2015;25(3):591–593. doi: 10.1007/s00590-014-1554-5. [DOI] [PubMed] [Google Scholar]
- 4.Periasamy M, Venkatramani H, Shanmuganathan RS. Management of chronic achilles tendon injuries-review of current protocols and surgical options. Indian Journal of Plastic Surgery. 2019;52(1):109–116. doi: 10.1055/s-0039-1687923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghosh S, Laing P, Maffulli N. Fascial turn-down flap repair of chronic Achilles tendon rupture. In: Maffulli N, Almekinders LC, editors. The Achilles Tendon. London: Springer; 2007. pp. 174–179. [Google Scholar]
- 6.Ehrl D, Heidekrueger PI, Schmitt A, et al. The anterolateral thigh flap for achilles tendon reconstruction: Functional outcomes. Plastic and Reconstructive Surgery. 2019;143(6):1772–1783. doi: 10.1097/PRS.0000000000005652. [DOI] [PubMed] [Google Scholar]
- 7.Nilsson-Helander K, Thomeé R, Silbernagel KG, et al. The Achilles tendon Total Rupture Score (ATRS): Development and validation. American Journal of Sports Medicine. 2007;35:421–426. doi: 10.1177/0363546506294856. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed SK, Fung BKK, Ip WY, Fok M, Chow SP. The versatile reverse flow sural artery neurocutaneous flap: A case series and review of literature. Journal of Orthopaedic Surgery and Research. 2008;3:15. doi: 10.1186/1749-799X-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Monnerie C, Le Nen D, Hu W, Letissier H, Kerfant N. Treatment of necrosis of Achilles tendon without tendon reconstruction: About four cases. Annales de Chirurgie Plastique et Esthetique. 2019;64(2):208–214. doi: 10.1016/j.anplas.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Jepegnanam TS, Nithyananth M, Boopalan PR, Cherian VM, Titus VT. Journal of Trauma. 2009;66(3):774–779. doi: 10.1097/TA.0b013e31817c96c7. [DOI] [PubMed] [Google Scholar]
- 11.Upadhyaya DN, Khanna V, Kohli R, Tulsi SP, Garg S. Functional reconstruction of complex tendo Achilles defect by free latissimus dorsi muscle flap. Indian Journal of Plastic Surgery. 2012;45(3):572–575. doi: 10.4103/0970-0358.105983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sabapathy SR, Venkataramani H, Latheef L, Bhardwaj P. Reconstruction of segmental defects of Achilles tendon: Is it a must in infected complex defects? Indian Journal of Plastic Surgery. 2013;46(1):121–123. doi: 10.4103/0970-0358.113729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nambi GI, Varanambigai TKA. Clinical study of the lateral supramalleolar flap in the soft tissue reconstruction around the ankle region. Indian Journal of Plastic Surgery (efirst) 2020 doi: 10.1055/s-0039-3402354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Low OW, Sebastin SJ, Cheah AEJ. A review of pedicled perforator flaps for reconstruction of the soft tissue defects of the leg and foot. Indian Journal of Plastic Surgery. 2019;52(1):26–36. doi: 10.1055/s-0039-1688103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vaienti L, Calori GM, Leone F, Brioschi M, Parodi PC, Marchesi A. Posterior tibial artery perforator flaps for coverage of Achilles region defects. Injury. 2014;45(Suppl 6):S133–S137. doi: 10.1016/j.injury.2014.10.037. [DOI] [PubMed] [Google Scholar]
- 16.Tsai J, Liao HT, Wang PF, et al. Increasing the success of reverse sural flap from proximal part of posterior calf for traumatic foot and ankle reconstruction: Patient selection and surgical refinement. Microsurgery. 2013;33(5):342–349. doi: 10.1002/micr.22099. [DOI] [PubMed] [Google Scholar]
- 17.Daar DA, Abdou SA, David JA, et al. Revisiting the reverse sural artery flap in distal lower extremity reconstruction: A systematic review and risk analysis. Annals of Plastic Surgery. 2020;84(4):463–470. doi: 10.1097/SAP.0000000000002041. [DOI] [PubMed] [Google Scholar]
- 18.Boopalan PR, Jepegnanam TS, Titus VT, Prasad SY, Chittaranjan SB. Open infected Achilles tendon injury—Reconstruction of tendon with fascia lata graft and soft tissue cover with a reverse flow sural flap. Foot and Ankle Surgery. 2008;14(2):96–99. doi: 10.1016/j.fas.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Oommen AT, Poonnoose PM, Padhy D, Korula RJ. Management of open chronic Tendo Achilles injuries: A case report. The Foot and Ankle Online Journal. 2010;3(1):2 Volume 3. [Google Scholar]
- 20.Abhyankar SV, Kulkarni A, Agarwal NK. Single stage reconstruction of ruptured tendoachilles tendon with skin cover using distally based superficial sural artery flap. Annals of Plastic Surgery. 2009;63(4):425–427. doi: 10.1097/SAP.0b013e31819516cc. [DOI] [PubMed] [Google Scholar]
- 21.Zheng L, Zhang XS, Dong ZG, Liu LH, Wei JW. One-staged reconstruction of Achilles tendon and overlying skin defects with suppuration: using peroneus brevis tendon transfer and reversed sural neurofasciocutaneous flap. Archives of Orthopaedic and Trauma Surgery. 2011;131(9):1267. doi: 10.1007/s00402-011-1298-1. [DOI] [PubMed] [Google Scholar]
- 22.Dalton GP, Wapner KL, Hecht PJ. Complications of Achilles and posterior tibial tendon surgeries. Clinical Orthopaedics. 2001;391:133e9. doi: 10.1097/00003086-200110000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Park J, Chun DI, Lee S, Cho J. A comparative evaluation of absorbable and nonabsorbable sutures for open repair of achilles tendon rupture: A pilot study. Korean Journal of Physical Anthropology. 2017;30:39. doi: 10.11637/kjpa.2017.30.2.39. [DOI] [Google Scholar]