Abstract
Functional outcome of first metatarsophalangeal joint (MTPJ) arthrodesis using intramedullary implant was reviewed in retrospective series of 12 patients who had MTPJ arthritis. The outcome measures were improvements seen in VAS for pain and AOFAS scores recorded pre-operatively and post-operatively at the time of achieving complete union. VAS for pain improved from mean of 7.5 pre-operative to 1.8 post-operative (p < 0.001). AOFAS Score improved from mean of 35.58 pre-operative to 80.91 post-operative (p < 0.001). The fusion rate was 100 percent and mean time needed for fusion was 9.6 weeks. Only one patient had malunion which was acceptable to patient and was not revised. The fusion using intramedullary intra-osseous Hallux Fusion implant is a promising technique with good functional outcome and low complications.
Keywords: Arthrodesis, Fusion, Intramedullary hallux implant, Hallux rigidus, First MTPJ arthritis
Introduction
The first Metatarsophalangeal joint (MTPJ) is an ellipsoid joint capable of motion in three planes. During the toe push-off phase of normal gait cycle, about 80% of body weight is transmitted through the first MTP joint [1]. Consequently, the primary osteoarthritis of first MTPJ or Hallux Rigidus is a common problem of Foot. First MTPJ is also commonly affected in several conditions of the great toe including Hallux Valgus deformity, Rheumatoid Arthritis, Gout and neuro-muscular diseases. Arthrodesis of the first MTPJ is a commonly performed procedure in end-stage arthritis of any etiology, ranging from post-traumatic arthritis, to those with infection or failed procedures for HV correction around the MTPJ, as a salvage option [2–6].
Hallux MTPJ Arthrodesis was first described by Clutton in 1,894 for the treatment of Hallux Valgus [7]. The primary aim from patient’s perspective is reduction of pain and restoration of ambulation without pain. For the surgeon, the ideal fixation procedure should be simple, reproducible, have high rate of fusion and minimal complications. Though, numerous techniques of hallux MTPJ fusion have been described in literature, the common factors which result in favorable outcome following arthrodesis are—adequate preparation of joint surfaces of MTPJ, rigid fixation, compression to promote primary bone healing and position of arthrodesis across the MTP joint. Proper alignment of fusion is phalanx held at an angle of 15 to 20 degrees of dorsiflexion to 10 to 15 degrees of hallux valgus angle with neutral rotation [8–10]. Arthrodesis has been performed using a variety of implants in this procedure, a commonly used implant being the Dorsal plate together with or without a lag screw [11] However, Dorsal plates are often associated with complications such as hardware impingement on extensor tendons and soft tissue, wound healing and dehiscence of overlying skin. An intra-osseous intramedullary device is another implant being used for MTPJ fusion with relatively reduced implant-related complications [12, 13].
The aim of our study was to review the functional outcome of arthrodesis of the Hallux MTPJ using an intramedullary device (Hallux Intrafix, Extremity Medical, USA) (Fig. 1). Studies with outcomes using this implant and technique for MTPJ arthrodesis in Indian Population are lacking, and we hope that our study will be helpful in guiding the treatment of MTPJ Fusion by this technique. The primary outcome was to study the Visual Analogue Score (VAS) for pain and AOFAS Score before surgery and how they changed after achieving fusion by this surgery. Secondary outcomes such as time needed for bone union, final HV Angle and complications, if any, related to wound healing, implant or infection were also studied.
Fig. 1.

Placement of Hallux intramedullary fusion device implant representation on a model
Materials and Methods
In this retrospective case series, we reviewed 12 patients, each with unilateral and single foot involvement who underwent hallux MTPJ fusion between January 2,016 and October 2,019 performed with Hallux intramedullary Fusion Device (Extremity Medical, USA). These patients were recruited at Foot and Ankle Clinic at Max Healthcare and surgeries were performed by senior author.
The indications for fusion included hallux rigidus, inflammatory conditions such as rheumatoid arthritis, gout, etc.
Patient’s information, medical records and radiographs were collected in a proforma and organized as
Demographic data
Diagnosis
Visual Analogue Score (VAS) for pain on a scale of 0 to 10 where 0 represents no pain and 10 as worst disabling pain
American Orthopedic Foot and Ankle Society (AOFAS) Hallux score—The criteria of motion at hallux MTP joint was dropped (10 marks) leaving 90 as best possible score
Radiographic and clinical union
Hallux valgus angle (HVA) on weight-bearing standing radiographs, and
Complications.
Patients’ records of VAS and AOFAS scores were noted pre-operatively and during radiological and clinical union follow-up visits (often between 7 and 14 weeks from surgery). These data were entered in Microsoft Excel and analyzed by SPSS software version in form of Student’s t test. It was done to calculate the statistical significance between the mean pre-operative and final post-operative value of Visual Analogue Score (VAS) and AOFAS.
Surgical Technique
Surgery was performed under regional anesthesia in supine position. The Hallux Intrafix intramedullary Fusion Device is an implant for MTP arthrodesis, which was chosen for all surgeries reported in our case series. This device is completely intra-osseous and has two basic components—a lag screw and an anchored post with an eyelet for passage of lag screw. The advantage of this design is that it allows the compression force to be distributed uniformly across the broader opposing surfaces of the MTPJ fusion site. It also keeps the fixation stable and firm allowing bridging trabecular bone formation. Using an intramedullary device allows a smaller incision and exposure without much periosteal stripping (unlike plates and screws) and negligible implant-related skin and soft tissue irritation [12–14].
An incision, 5 to 6 cm long, just medial to the extensor hallucis longus tendon was made over the MTPJ. The potential complication during exposure is the injury of dorsal cutaneous nerve of great toe. This is prevented by gentle blunt dissection and staying medial or lateral to cutaneous nerve. The incision was deepened to reach the capsule. The capsule was divided in the same line to expose the base of the proximal phalanx and the metatarsal head. The collateral ligaments were released from base of proximal phalanx and great toe was plantarflexed to expose articular surfaces. The articular surfaces were sequentially prepared for fusion using cup and cone reamers (Fig. 2). Excess removal of bone during preparation of surfaces can be prevented using cup and cone reamers cautiously and in spurts rather than continuously. A guide wire was passed from the central portion of the head of metatarsal into the center of diaphysis. A cannulated drill was passed over guide wire in preparation for passing the Post of our Hallux intramedullary device. A post of appropriate diameter and length filling the distal half of the first metatarsal was placed over the guide wire and inserted in the medullary canal of metatarsal (Fig. 3). Stress fracture of Metatarsal can happen while inserting an oversized intramedullary post. This can be avoided by fluoroscopic check during insertion of intramedullary device. The post was buried about 2 mm deeper to the prepared surface of metatarsal head with the eyelet directed medially (Fig. 4). The guide wire was removed. An alignment guide was inserted into distal end of the post, directed toward the eyelet of the metatarsal Post. A double-ended guide wire was passed in a retro-grade manner through the alignment guide to emerge from the medial cortex of first metatarsal proximal to its head. Alignment guide was removed. The double-ended guide wire was pulled till the other end came to lie just at level of the surface of the metatarsal head. The phalanx was then aligned with the metatarsal head and held in the final position of arthrodesis. The wire was then advanced in an ante-grade manner into the proximal phalanx securing the desired position of arthrodesis. Alignment of proximal phalanx was confirmed fluoroscopically at 10 to 15 degree valgus, at about 20 degree dorsiflexion and at neutral rotation relative to first metatarsal. The error in position of arthrodesis leads to malunion and therefore needs to be checked after provisional fixation with k wires using weight-bearing simulation and fluoroscopy. Another k-wire was passed to secure the position of arthrodesis without interfering with the trajectory of the first guide wire (Fig. 5). A cannulated 4.0 mm lag screw was passed over the guide wire in proximal phalanx and seated in the eyelet of the metatarsal Post (Fig. 6). As the lag screw was tightened, the turns were given gently to observe compression across apposed surfaces of metatarsal and proximal phalanx till the end point was felt. The final position was also confirmed fluoroscopically (Fig. 7). The capsule layer was closed with 2-0 Vicryl and Skin closed with 3-0 Nylon. A well-padded dressing was used, rolled just above the ankle joint.
Fig. 2.

Cup reamer for metatarsal head
Fig. 3.

Metatarsal post insertion over the guide wire
Fig. 4.

Metatarsal post insertion completed
Fig. 5.
Guide wire passed to Phalanx ante-grade manner in position of arthrodesis
Fig. 6.

Lag screw insertion
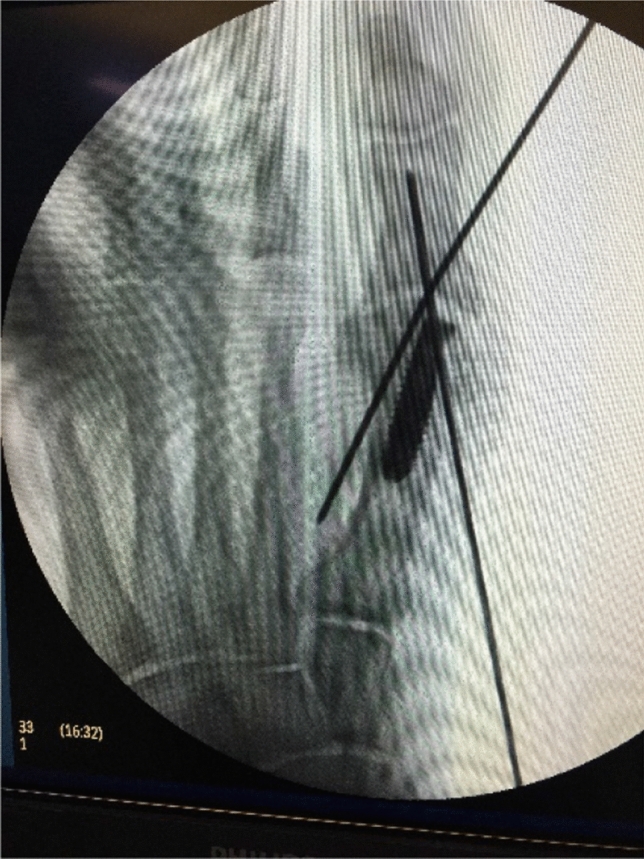
Fig. 7.

Intra-operative C-arm radiographic image with ideal position of MTP fusion
Post-operative Course: The limb was kept elevated for 24 h. Weight bearing was allowed as per patient’s pain tolerance within 1 or 2 days of surgery using front-foot off-loading shoes. After 6 to 12 weeks, unrestricted activity was allowed whenever bone union was evident on radiographs.
Patients were followed up adequately till complete bone union was evident on X-rays in the form of continuous trabeculae across the MTPJ (Fig. 8).
Fig. 8.

Post-operative radiograph after 11 weeks showing bone fusion across MTPJ
Results
Demographics
The age range of patients recruited in this study was from 36 to 83 years, with mean age of 63 years. There were 10 female and 2 male patients. Clinico-radiologically established hallux MTP arthritis was present in all patients. 10 patients had primary osteoarthritis, 1 patient had rheumatoid arthritis and 1 patient had gouty arthritis.
Primary outcomes
All patients were examined at an interval of 2, 4, 6 and 8 weeks from the date of the surgery. Subsequently, the final follow-up visit was when they were nearly painless during ambulation (variable time between 8 and 16 weeks). The standard VAS for pain and AOFAS hallux score were recorded for every patient pre-operatively. These were recorded post-operatively during follow-up visits between the 6th and 16th week. The mean period of follow-up was 12 weeks. Paired t test was applied to know statistical significance of change in VAS and AOFAS scores.
The VAS score was noted to improve from a mean value of 7.5 points (5 to 10) pre-operatively to 1.8 (0 to 4) at the final follow-up (p < 0.001) (Table 1). The mean AOFAS Hallux score improved significantly from 35.58 (24 to 50) to 80.91 (78 to 96) with p < 0.001. AOFAS scores in all patients achieved a statistically significant improvement with p < 0.001 (Table 2).
Table 1.
Statistically mean value and standard deviation of pre-operative and post-operative AOFAS and VAS Scores
| Paired samples statistics | |||
|---|---|---|---|
| Score | Mean | N | Standard deviation |
| AOFAS score pre-operative | 35.5833 | 12 | 10.25545 |
| AOFAS score post-operative | 80.9167 | 12 | 9.22899 |
| VAS score pre-operative | 7.50000 | 12 | 1.16775 |
| VAS score post-operative | 1.83333 | 12 | 0.83485 |
Table 2.
Statistically significant p value of pre-operative and post-operative AOFAS and VAS Score
| Paired samples test | ||||||
|---|---|---|---|---|---|---|
| Score | Paired differences | t | p value | |||
| Mean | Standard deviation | 95% Confidence interval of the difference | ||||
| Lower | Upper | |||||
| AOFAS score (pre-post) | − 45.33 | 13.87 | − 54.15 | − 36.52 | − 11.32 | < 0.001 |
| VAS score (pre-post) | 5.67 | 0.78 | 5.17 | 6.16 | 25.21 | < 0.001 |
Secondary outcomes
-
Time needed for MTPJ fusion—This was based on three major clinical-radiological outcomes. These were—(a) No pain on activities of daily living, (b) absence of local tenderness, and (c) Radiographical evidence of fusion—bone trabeculae seen across MTPJ.
In our study, the minimum time to achieve all three was 7 weeks and maximum time was 13 weeks. The mean time for achieving fusion was 9.6 weeks.
Final Hallux valgus angle (HVA)—The average pre-operative HV angle was 27.3 degrees, whereas post-operative HV angle was 11.8 degrees, on weight-bearing standing radiographs.
- Complications
- Wound healing was uneventful in all patients.
- No patient had implant-related pain.
- There was one case of malunion resulting from high dorsiflexion angle leading to cock-up deformity of great toe. There was no case of nonunion or avascular necrosis.
- No patient in this series had infection.
Discussion
In our case series VAS for pain had reduced from a mean of 7.5 pre-operatively to mean of 1.8 post-operatively. Aas et al. [15] reported in their series of 35 patients, a post-operative mean VAS for pain without and with shoe was 1.8 and 3.2 (18 and 32 out of 100), respectively. In our study, the mean AOFAS Hallux score improved significantly from 35.58 (24 to 50) to 80.96 (78 to 96) with p < 0.001, whereas the study by Aas et al. obtained a mean AOFAS score of 74 which is lower than our study. This difference could probably be due to a larger sample size and more complications requiring revision arthrodesis in 4 cases in their series. Ellington et al. [16] in his retrospective series recorded only post-operative data at 6 months and reported mean VAS for pain and AOFAS as 6.8 and 79.7, respectively.
A variety of techniques using different implants for arthrodesis of First MTPJ have been described in literature [17–19]. Use of other implants in the past have resulted in successful fusion of the MTPJ but have also required removal of implants whenever symptomatic. This is shown in Wassink and Vanden study wherein they reviewed 109 MTPJ fusions using single screw with 96% fusion rate along with removal of implant needed in 78% patients [20]. A similar recent study has reported that approximately 20% of fusions using a dorsal plate and plantar lag screw required implant removal for irritation of the overlying tendons by implant and pain [21]. An acceptable position of fusion is the key to achieve good outcome. A dorsiflexion angle of 15 to 20 degrees and 15 to 20 degrees of hallux valgus angle with neutral rotation at the MTP joint are the most recommended [22, 23]. Achieving the ideal position of arthrodesis and to assess it clinically is easy with the use of intramedullary implant compared to the conventional screws and plate. The common complications described in literature are nonunion, malunion and hardware impingement [16, 20–22].
In our case series with the intra-osseous Hallux Intrafix intramedullary Fusion Device, the average post-operative HV angle was 11.8 degrees, on weight-bearing standing Radiographs, improving from the average pre-operative HV angle of 27.3 degrees. Complications recorded in our case series were minimal, with one case of malunion resulting from high dorsiflexion angle of 35 degrees leading to Cock-up deformity of great toe. There was no case of nonunion or avascular necrosis. Wound healing was uneventful in all patients and no patient had implant-related pain or infection.
The 100% fusion rate in our series is better than most of the series reported in the literature [9, 18, 22]. Fusion at the arthrodesis site can be assessed using two different methods:
Clinical assessment
Imaging studies
The plain radiograph is the most convenient, accessible, and reliable indicator of arthrodesis when used along with clinical assessment by evaluating the tenderness and motion of MTP joint, local swelling and ability to carry out daily activities. CT scan can also be used to detect fusion in patients where it cannot be decided. However, CT was not needed in our study. In the post-operative period, the stability of the MTP joint with this implant permitted mobilizing the patients with weight bearing as per pain tolerance, as early as the second post-operative day. However, we support the viewpoint of other authors that this device has got slightly longer learning curve. It also does not allow adjustments after insertion and final fixation of implant easily, which is allowed by plate and screws [12].
Conclusion
Results of arthrodesis of the MTP joint with Hallux Intramedullary Fusion Device are described in this report. The advantage of this design is that it allows the compression force to be distributed uniformly across the broader opposing surfaces of the MTPJ fusion site. It also which keeps the fixation stable and firm allowing bridging trabecular bone formation [13, 14]. Using an intramedullary device allows a smaller incision and exposure without much periosteal stripping (unlike plates and screws) and negligible implant-related skin and soft tissue irritation [12].
In our study, the intramedullary and intra-osseous Hallux Intrafix devices achieved good functional outcome in terms of AOFAS score, VAS for pain, Fusion rate, final HVA, and time taken for MTPJ fusion.
The potential complications of this procedure are related to injury of dorsal cutaneous nerve of great toe during exposure and possible stress fracture of Metatarsal while inserting inappropriate size intramedullary post. The error in position of arthrodesis leads to malunion and therefore needs to be checked after provisional fixation with k wires using weight-bearing simulation and fluoroscopy.
Complications recorded in our case series were minimal, with one case of malunion resulting from high dorsiflexion angle of 35 degrees leading to Cock-up deformity of great toe. There was no case of nonunion or avascular necrosis. Wound healing was uneventful in all patients and no patient had implant-related pain or infection.
Nonetheless, further prospective, and comparative studies with larger sample size and longer follow-up are needed to confirm the findings.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kamal Dureja, Email: kdureja77@gmail.com.
Shantanu H. Bhardwaj, Email: shantanub88@gmail.com
References
- 1.Hutton WC, Dhanendran M. The mechanics of normal and hallux valgus feet-a quantitative study. Clinical Orthopaedics. 1981;157:7–13. [PubMed] [Google Scholar]
- 2.Besse JL, Chouteau J, Laptoiu D. Arthrodesis of the first metatarsophalangeal joint with ball and cup reamers and osteosynthesis with pure titanium staples radiological evaluation of a continuous series of 54 cases. Foot Ankle Surgery. 2010;16:32–37. doi: 10.1016/j.fas.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 3.Coughlin MJ. Rheumatoid forefoot reconstruction. A long term follow up study. Journal of Bone and Joint Surgery. 2000;82:322–341. doi: 10.2106/00004623-200003000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Coughlin MJ, Grebing BR, Jones CP. Arthrodesis of the first metatarsophalangeal joint for idiopathic hallux valgus: Intermediate results. Foot and Ankle International. 2005;26:783–792. doi: 10.1177/107110070502601001. [DOI] [PubMed] [Google Scholar]
- 5.Ginsburg AI. Arthrodesis of the first metatarsophalangeal joint: A practical procedure. Journal of the American Podiatric Medical Association. 1979;69:367–369. doi: 10.7547/87507315-69-6-367. [DOI] [PubMed] [Google Scholar]
- 6.Grimes JS, Coughlin MJ. First metatarsophalangeal joint arthrodesis as a treatment for failed hallux valgus surgery. Foot and Ankle International. 2006;27:887–893. doi: 10.1177/107110070602701104. [DOI] [PubMed] [Google Scholar]
- 7.Womack JW, Ishikawa SN. First metatarsophalangeal arthrodesis. Foot Ankle Clinic. 2009;14(1):43–50. doi: 10.1016/j.fcl.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 8.Buranosky DJ, Taylor DT, Sage RA, Sartori M, Patwardhan A, Phelan M, et al. First metatarsophalangeal joint arthrodesis: quantitative mechanical testing of six-hole dorsal plate versus crossed screw fixation in cadaveric specimens. Journal of Foot and Ankle Surgery. 2001;40(4):208–213. doi: 10.1016/S1067-2516(01)80020-X. [DOI] [PubMed] [Google Scholar]
- 9.Politi J, John H, Njus G, Bennett GL, Kay DB. First metatarsal-phalangeal joint arthrodesis: a biomechanical assessment of stability. Foot and Ankle International. 2003;24(4):332–337. doi: 10.1177/107110070302400405. [DOI] [PubMed] [Google Scholar]
- 10.Curtis MJ, Myerson M, Jinnah RH, Cox QG, Alexander I. Arthrodesis of the first metatarsophalangeal joint: a biomechanical study of internal fixation techniques. Foot Ankle. 1993;14(7):395–399. doi: 10.1177/107110079301400705. [DOI] [PubMed] [Google Scholar]
- 11.Roukis TS. Nonunion after arthrodesis of the first metatarsal-phalangeal joint: a systematic review. Journal of Foot and Ankle Surgery. 2011;50(6):710–713. doi: 10.1053/j.jfas.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 12.Efstathios D, Shen HV, Irfan F. Intramedullary and intra-osseous arthrodesis of the hallux metatarsophalangeal joint. Journal of Orthopaedic Surgery. 2016;24(3):359–360. doi: 10.1177/1602400317. [DOI] [PubMed] [Google Scholar]
- 13.Parker L, Ray P, Grechenig S, Grechenig W. Does the IOFIX improve compression in ankle fusion? Foot Ankle Surg. 2014;20(4):258–261. doi: 10.1016/j.fas.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Shymon SJ, Moss L, Harris TG. Case series using a novel implant and accelerated rehabilitation for patients undergoing an isolated talonavicular arthrodesis. Foot and Ankle Specialist. 2016;9(3):227–231. doi: 10.1177/1938640015620638. [DOI] [PubMed] [Google Scholar]
- 15.Aas M, Johnsen TM, Finsen V. Arthrodesis of the first metatarsophalangeal joint for hallux rigidus-optimal position of fusion. The Foot. 2008;18(3):131–135. doi: 10.1016/j.foot.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Ellington JK, Jones CP, Cohen BE, Davis WH, Anderson RB. Review of 107 Hallux MTP Joint arthrodesis using dome shaped reamers and a stainless-steel dorsal plate. Foot and Ankle International. 2010;31(5):385–390. doi: 10.3113/FAI.2010.0385. [DOI] [PubMed] [Google Scholar]
- 17.Mueller ME, Allgoewer M, Schneider R, Willenegger H. Manual of internal fixation. Berlin: Springer-Verlag; 1991. [Google Scholar]
- 18.Brodsky JW, Passmore RN, Pollo FE, Shabat S. Functional outcome of arthrodesis of the first metatarsophalangeal joint using parallel screw fixation. Foot and Ankle International. 2005;26:140–146. doi: 10.1177/107110070502600205. [DOI] [PubMed] [Google Scholar]
- 19.Moynihan FJ. Arthrodesis of the metatarso-phalangeal joint of the great toe. Journal of Bone and Joint Surgery. British Volume. 1967;49:544–551. doi: 10.1302/0301-620X.49B3.544. [DOI] [PubMed] [Google Scholar]
- 20.Wassink S, Vanden OM. Arthrodesis of the first metatarso-phalangeal joint using a single screw: retrospective analysis of 109 feet. Journal of Foot and Ankle Surgery. 2009;48(6):653–661. doi: 10.1053/j.jfas.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 21.Wanivenhaus F, Espinosa N, Tscholl PM, Krause F, Wirth SH. Quality of early union after first metatarsophalangeal joint arthrodesis. Journal of Foot and Ankle Surgery. 2017;56(1):50–53. doi: 10.1053/j.jfas.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 22.Coughlin MJ. Arthrodesis of the first metatarsophalangeal joint. Orthopedic Reviews. 1990;19:177–186. [PubMed] [Google Scholar]
- 23.Mann RA, Thompson FM. Arthrodesis of the first metatarsophalangeal joint for hallux valgus in rheumatoid arthritis. Journal of Bone and Joint Surgery. American Volume. 1984;66:687–692. doi: 10.2106/00004623-198466050-00006. [DOI] [PubMed] [Google Scholar]


