Abstract
Introduction
The use of elbow arthroscopy is becoming increasingly common in orthopaedic practice; nevertheless, it is still considered a difficult procedure with a long learning curve. The aim of the study is to evaluate the role of a new elbow Sawbone-Based Arthroscopy Module (e-SBAM) in the training of elbow surgeons.
Methods
Fourteen surgeons were classified as “Expert” (n: 7; more than 10 years of experience in arthroscopic surgery) and “Not-expert” surgeons (n: 7; less than 10 years of experience). During a dedicated arthroscopic session, using the Sawbones Elbow model (Sawbones Europe AB®), all participants were asked to perform an arthroscopic round and to touch three specific landmarks. An independent observer measured the time that each participant needed to perform this task (Performance 1). The same measurement was repeated after two weeks of eSBAM training (Performance 2).
Results
“Not-expert” surgeons needed significantly more time (41 s; range 26–120) than “Expert” ones (13 s; range 8–36) to complete Performance 1. One “Not-expert” surgeon did not complete Performance 1 and needed more than 120 s for Performance 2. The whole study group required a median of 5 s less to complete Performance 2. A tendency towards an improvement was observed in the group of the non-experienced surgeons as compared with the experienced ones.
Conclusions
The simulation training can be advantageous in the learning curve of young elbow surgeons and helpful for experienced surgeons. E-SBAM can be used as an effective tool for the current stepwise arthroscopic elbow training programs with the aim of improving arthroscopic elbow skills.
Level of Evidence
Basic Science Study.
Keywords: Elbow, Arthroscopy, Dry model, Sawbone-based arthroscopy module, Surgeon training
Introduction
At the very beginning of the arthroscopic era, the elbow joint was described as not suitable for this procedure because of the minimal joint space [1]. Over the past years, this dogma has changed, and the interest of the scientific community in elbow arthroscopy has contributed to improve the safety and the potentiality of this procedure significantly [2–6]. Elbow arthroscopy has some advantages over open surgery, the most relevant of which is that it is a minimally invasive surgery that has been reported to require a shorter and easier postoperative rehabilitation protocol [7–9]. However, when elbow arthroscopy is compared to knee or shoulder arthroscopy, the complication rate appears considerably higher [10], and several authors described a high overall reoperation rate in patients who underwent elbow arthroscopy [11, 12].
Nevertheless, although it is still considered a difficult procedure, the use of elbow arthroscopy is increasing progressively, also attracting the interest of young surgeons [13]. However, due to the relatively infrequent indications for elbow arthroscopy, it might be slow and difficult to obtain an adequate learning curve for young orthopaedic surgeons. For these reasons, in this process simulation models can play an essential role. As already demonstrated in general surgery literature, there is a strong correlation between training on a simulator and improved performance in the operating room [14–16], and recent studies describing the positive outcomes of arthroscopic simulator training have been published [17, 18].
Sawbones models are one among the numerous option to simulate basic surgery, which has been validated, with a high level of evidence in the orthopaedic literature [19, 20], with papers describing their potential role and also in different arthroscopic surgeries as a reliable method to acquire and improve surgical skills [21–25].
Nowadays, it is strongly recommended to practice on cadaveric specimens to become more confident with the arthroscopic anatomy of the elbow. However, the availability of cadaveric specimens and the costs of wet training courses differ across different countries, and this logistic or economic difficulty may prevent young surgeons from attending enough training sessions before considering themselves ready to perform their first diagnostic elbow arthroscopy [13]. Furthermore, there are no internationally accepted guidelines for learning, and no structured training programs have been created to help the novice surgeon to master the management of the disorders of this joint. Savoie et al. suggested a stepwise approach to become a good elbow arthroscopic surgeon but did not include the possibility of dry model practice [13] and no studies on the use of a Sawbones elbow model in orthopaedic teaching have been published. Recently, a Sawbone-based elbow arthroscopy simulation model has been developed.
The aim of the study is to evaluate the role of a new elbow Sawbone-Based Arthroscopy Module (e-SBAM) in the training of the arthroscopic technique for elbow surgeons.
Materials and Methods
A total of 14 volunteer participants were enrolled: 3 orthopaedic residents and 11 orthopaedic surgeons. Based on the different level of experience in arthroscopic surgery, participants were classified as “Expert” surgeons (more than 10 years of experience in general arthroscopic surgery, more than 50 cases/year) and “Not-expert” surgeons (less than 10 years of experience in general arthroscopic surgery, less than 50 cases/year) [18, 26].
The Sawbones Elbow model (Sawbones Europe AB®) we used is produced for diagnostic and operative arthroscopic techniques. For this study, a model fixed in neutral forearm pronos more than 10 years of experience supination and 90° of elbow flexion was used. The model is attached to a table using the provided dedicated clamps (Fig. 1). Dry arthroscopy is performed by introducing the 30°-scope through the desired portal and capsule to allow intra-articular diagnostic evaluation through the predetermined standard anterolateral (AL) and anteromedial (AM) portals. This is a study on sawbone elbow simulator therefore it does not need any ethical approval/informed consent.
Fig. 1.

Sawbones Elbow model (Sawbones Europe AB®) fixed using the dedicated support with the forearm hanging free with only gravity force
Study Task
All participants were asked to insert a 30°-scope through the AM portal and a probe through the AL portal and to begin the task in the anterior compartment of the elbow as it happens in standard elbow arthroscopic setting (Fig. 2).
Fig. 2.

a Arthroscopic view from AM portal with the probe touching the coronoid process; b Arthroscopic setting: the 30° arthroscope in the AM portal and the probe is inserted through the AL portal
The study task consisted in performing a simulated arthroscopic diagnostic circuit of the elbow joint model and to visualize and touch sequentially with the probe the following structures; (1) centre of the capitulum humeri, (2) the highest point of the coronoid tip and (3) the centre of the coronoid fossa.
An independent observer measured the time that each participant needed to perform this task, starting from the moment in which the participant grasped the arthroscope and the probe (still outside the model). The timer was stopped when each the participant touched the last reference point with the probe (Performance 1). The same study setting was repeated two weeks later and all the participants were asked to perform the same task (Performance 2) again. Training with eSBAM was done for two weeks and no possibility to repeat the test was allowed to the participants during the period between the two Performances. The measurement was repeated in the previously described fashion.
Statistical Analysis
Patients' characteristics and times of performance are reported as numbers (percentages) or median (minimum–maximum), as appropriate. The Wilcoxon’s Two-Sample Test was used to compare the distribution of time between levels of surgeon experience. The Sign Test was used to show a significant decrease in time between the two performances. All statistical analyses were performed using the SAS software v.9.4 (SAS Institute, Cary, NC, USA).
Results
Seven "Not-expert" surgeons and seven "Expert" surgeons composed the study groups. Demographics of the participants are summarized in Table 1.
Table 1.
Demographics of the surgeons
| Overall (N = 14) | |
|---|---|
| Sex, N (%) | |
| Male | 12 (85.7) |
| Female | 2 (14.3) |
| Age, mean | 40.6 [26–56] |
| Years of experience in orthopedic surgery, mean | 14.8 [2–31] |
| Years of experience in arthroscopic surgery, mean | 10.6 [0–26] |
| Years of experience in arthroscopic elbow surgery, mean | 2.3 [0–15] |
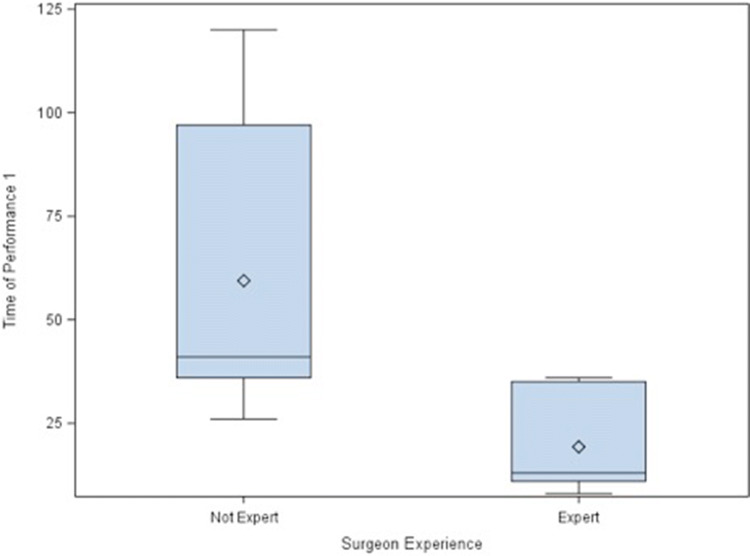
One "Not-expert" surgeon did not complete the arthroscopic round and he was unable to touch the structures sequentially; the same surgeon needed more than 120 s two weeks later. “Not-expert” surgeons needed a median of 41 s (range 26–120) to complete Performance 1, while “Expert” surgeons needed a median on 13 s (range 8–36) (p = 0.006) (Fig. 3, Table 2).
Fig. 3.
Box plot showing the distribution of time of performance 1 (in seconds) between levels of surgeon experience (N = 14), Wilcoxon two-sample test, P-value < 0.01
Table 2.
Time of performance 1, comparison between different levels of surgeons’ experience
| Surgeon experience | Time of performance 1 | ||
|---|---|---|---|
| N | Median (Min–Max) | P value* | |
| Not expert | 7 | 41 (26–120) | 0.006 |
| Expert | 7 | 13 (8–36) | |
*Wilcoxon two-sample test
The whole study group needed a median of 5 s (range − 35 to 1) less to complete Performance 2 compared to Performance 1 (p 0.006) (Table 3). The Spaghetti-plot describes the distribution of change from the participants in relation to their level of experience (Fig. 4).
Table 3.
Distribution of differential time (time of performance 2–time of performance 1), overall and between levels of surgeon experience
| Surgeon experience | Differential time (time P2–time P1) | ||
|---|---|---|---|
| N | Median (Min–Max) | P value | |
| Overall | 14 | − 5 (− 35—1) | 0.006* |
| Not Expert | 7 | − 8 (− 35—0) | > 0.05† |
| Expert | 7 | − 1 (− 7—1) | > 0.05† |
*Sign test under H0: median = 0
†Wilcoxon two-sample test
Fig. 4.
Spaghetti-plot showing times of performance 1 and 2 for each surgeon (N = 14; a blue or a red line if the surgeon is expert or not, respectively), Wilcoxon two-sample test, P value < 0.01
Discussion
The most important finding of the present study is that the time needed by participants with a different level of surgical experience to perform the study task decreases with repeated use of the simulator after two weeks. A tendency towards a more marked improvement was observed in the group of the non-experienced surgeons as compared with the experienced ones.
Elbow arthroscopy is being used more frequently as it allows improved visualization of the intra-articular structures, with minor surgical trauma and subsequent shorter and less painful postoperative rehabilitation [7, 27]. Despite these advantages, arthroscopy of the elbow requires a long learning curve, and this limits the application of arthroscopy for challenging procedures [8, 28–30].
When compared to knee or shoulder arthroscopy, elbow arthroscopy is generally considered more difficult and reported complications are more frequent [10, 11]. Arthroscopic surgery has a steeper learning curve for orthopaedic surgery trainees as compared to open surgery, and extensive hands-on training is required to develop the surgical skills necessary to perform arthroscopic surgery safely [26, 31, 32]. The learning curve for elbow surgery can be considered as even steeper when compared to knee or shoulder arthroscopy, since the minimum number of cases to develop the necessary skills may not be reached throughout the years of training. For these particular reasons, simulation offers a unique field of interest in teaching elbow arthroscopy. If training on a simulator can improve surgical performance as has been demonstrated in general surgery and knee and shoulder arthroscopy [14–18], its use may become widespread, and patients will benefit from better surgeons.
Multiple types of simulators exist, each with specific features, advantages and disadvantages [33]. Currently, simulators based on animal models, synthetic bench models (joint phantoms or sawbones) or virtual reality are available. In arthroscopy simulation, virtual reality is used more frequently as compared to fracture or spine simulators [33]. This growing interest in virtual reality simulators is due to the fact that this technology provides instant feedback of performance in a structured way [34]; however, virtual reality simulators are more expensive than synthetic bench models. On one side, this can prevent smaller institutions from buying them, whereas, on the other hand, this implies that manufacturers are more interested in developing software for "lucrative" joints, i.e., those in which arthroscopy is well established and represents a common surgical indication. Elbow arthroscopy has historically been considered a challenging procedure due to the rare surgical indications and the technical difficulty of the surgical procedure [8, 27, 35, 36]. Hence, simulators based on synthetic bench models can fill this gap offering a realistic simulation experience at an affordable price. Since the ultimate aim of a surgical simulator is to provide an environment for learning skills that will be relevant in the operating theatre and no gold-standard device exists for elbow arthroscopy, it appeared acceptable to begin the evaluation of an elbow arthroscopy simulator on a sawbone model [37].
The results of this study support the finding that training on arthroscopic simulators seems to improve the performance and that more experienced subjects perform better on arthroscopic simulators than less experienced subjects [37].
Moreover, we found that less experienced surgeons seemed to benefit more from the use of the simulator than more experienced ones, showing greater improvement in the performance between sessions. We believe this may be due to an ample "margin of improvement" when compared to an already skilled arthroscopic surgeon. As a consequence of our results, the sawbone module might be used, potentially, as a means of comparing developing proficiency in the educational contest of young and expert orthopaedic surgeons.
This study has some limitations. First of all, the study was aimed at measuring the performance of the participants on a specific task on a simulated arthroscopy setting and cannot be extrapolated to other procedures. Also, the measurement of the actual surgical performance, which can be influenced by anatomical variants and pathological situations, was not included in the study design.
This study, however, was not designed to analyse the various components of the surgical performance, such as the efficiency of each movement, the precision of the task (number of unnecessary structures contacted) or the damage to the soft tissue envelope. Further studies are required to evaluate if the e-SBAM allows a realistic evaluation of these parameters as well since such analysis can help each trainee to refine their surgical skills, monitor their progress over time and identify areas for improvement. Finally, the different level of experience of the participant has grouped arbitrarily in a dichotomic way, which can amplify floor and ceiling effects caused by extremely talented or untalented individuals. Despite these limitations, we believe the Sawbones elbow model as a potential tool to improve the learning curve of novel arthroscopic elbow surgeons.
Further studies are necessary to determine the optimal amount of training on dry elbow models to obtain specific arthroscopic skills and to determine if the skills acquired in a simulated environment can be reproduced in a cadaveric model and daily surgical practice.
Conclusions
The new elbow simulation training can improve the performance of specific tasks in the learning curve of surgeons mastering arthroscopic elbow techniques. Sawbone simulators led the surgeon to reduce the execution time of specific surgical manoeuvres, especially in the case of low-experience surgeons.
E-SBAM is an effective tool for the current stepwise arthroscopic elbow training and can help surgeons to easily approach this complex surgery.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Burman MS. Arthroscopy or the direct visualization of joints: an experimental cadaver study. 1931. Clinical Orthopaedics and Related Research. 2001;390:5–9. doi: 10.1097/00003086-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Arrigoni P, Cucchi D, Menon A, Guerra E, Nicoletti S, Colozza A, et al. The posterior interosseous nerve crosses the radial head midline and increases its distance from bony structures with supination of the forearm. Journal of Shoulder and Elbow Surgery. 2019;28:2. doi: 10.1016/j.jse.2018.08.019. [DOI] [PubMed] [Google Scholar]
- 3.Arrigoni P, Cucchi D, Guerra E, Luceri F, Nicoletti S, Menon A, et al. No neurovascular damage after creation of an accessory anteromedial portal for arthroscopic reduction and fixation of coronoid fractures. Knee Surgery Arthroscopy Sports Traumatology. 2018;1:5. doi: 10.1007/s00167-018-4926-2. [DOI] [PubMed] [Google Scholar]
- 4.Hilgersom NFJ, Cucchi D, Luceri F, van den Bekerom MPJ, Oh LS, Arrigoni P, et al. Locating the ulnar nerve during elbow arthroscopy using palpation is only accurate proximal to the medial epicondyle. Knee Surgery, Sports Traumatology, Arthroscopy. 2018;27:3254–3260. doi: 10.1007/s00167-018-5108-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cucchi D, Guerra E, Luceri F, Lenich A, Nicoletti S, Randelli P, et al. A combination of an anteromedial, anterolateral and midlateral portals is sufficient for 360° exposure of the radial head for arthroscopic fracture fixation. Knee Surgery, Sports Traumatology, Arthroscopy. 2018;27:319–325. doi: 10.1007/s00167-018-5077-1. [DOI] [PubMed] [Google Scholar]
- 6.Cucchi D, Luceri F, Celli A, Menon A, Barco R, Wegmann K, et al. Fracture pattern influences radial head replacement size determination among experienced. Elbow Surgeons. 2020 doi: 10.1007/s43465-020-00039-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen AP, Redden JF, Stanley D. Treatment of osteoarthritis of the elbow: A comparison of open and arthroscopic debridement. Arthroscopy. 2000;16(7):701–706. doi: 10.1053/jars.2000.8952. [DOI] [PubMed] [Google Scholar]
- 8.Luceri, F., Lesman, J.J., Cucchi, D., Domzalski, M., Randelli, P.S., Arrigoni, P. (2020). Antegrade reduction and fixation of coronoid fractures: A new arthroscopic technique https://journals.lww.com/shoulderelbowsurgery/Fulltext/2020/03000/Antegrade_Reduction_and_Fixation_of_Coronoid.1.aspx
- 9.Arrigoni P, Cucchi D, Luceri F, Menon A, Guerra E, Nicoletti S, et al. A 360° axial contact arc for fixation of radial head fractures can be reached combining anteromedial, anterolateral and midlateral arthroscopic portals. Revue de Chirurgie Orthopédique et Traumatologique. 2018;104(8):S85–86. doi: 10.1016/j.rcot.2018.09.059. [DOI] [Google Scholar]
- 10.Kelly EW, Morrey BF, O’Driscoll SW. Complications of elbow arthroscopy. Journal of Bone and Joint Surgery Series A. 2001;83(1):25–34. doi: 10.2106/00004623-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Leong NL, Cohen JR, Lord E, Wang JC, McAllister DR, Petrigliano FA. Demographic trends and complication rates in arthroscopic elbow surgery arthroscopy. Journal of Arthroscopic and Related Surgery. 2015;31(10):1928–1932. doi: 10.1016/j.arthro.2015.03.036. [DOI] [PubMed] [Google Scholar]
- 12.Nelson GN, Wu T, Galatz LM, Yamaguchi K, Keener JD. Elbow arthroscopy: Early complications and associated risk factors. Journal of Shoulder and Elbow Surgery. 2014;23(2):273–278. doi: 10.1016/j.jse.2013.09.026. [DOI] [PubMed] [Google Scholar]
- 13.Savoie FH. Guidelines to becoming an expert elbow arthroscopist arthroscopy. Journal of Arthroscopic and Related Surgery. 2007;23(11):1237–1240. doi: 10.1016/j.arthro.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 14.Price J, Naik V, Boodhwani M, Brandys T, Hendry P, Lam BK. A randomized evaluation of simulation training on performance of vascular anastomosis on a high-fidelity in vivo model: The role of deliberate practice. Journal of Thoracic and Cardiovascular Surgery. 2011;142(3):496–501. doi: 10.1016/j.jtcvs.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 15.Stefanidis D, Scerbo MW, Montero PN, Acker CE, Smith WD. Simulator training to automaticity leads to improved skill transfer compared with traditional proficiency-based training: A randomized controlled trial. Annals of Surgery. 2012;255(1):30–37. doi: 10.1097/SLA.0b013e318220ef31. [DOI] [PubMed] [Google Scholar]
- 16.Korndorffer JR, Dunne JB, Sierra R, Stefanidis D, Touchard CL, Scott DJ. Simulator training for laparoscopic suturing using performance goals translates to the operating room. Journal of the American College of Surgeons. 2005;201(1):23–29. doi: 10.1016/j.jamcollsurg.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 17.Karam MD, Pedowitz RA, Natividad H, Murray J, Marsh JL. Current and future use of surgical skills training laboratories in orthopaedic resident education: A national survey. Journal of Bone and Joint Surgery Series A. 2013;95:1. doi: 10.2106/JBJS.L.00177. [DOI] [PubMed] [Google Scholar]
- 18.Atesok K, Mabrey JD, Jazrawi LM, Egol KA. Surgical simulation in orthopaedic skills training. Journal of the American Academy of Orthopaedic Surgeons. 2012;20(7):410–422. doi: 10.5435/JAAOS-20-07-410. [DOI] [PubMed] [Google Scholar]
- 19.Brubacher JW, Karg J, Weinstock P, Bae DS. A novel cast removal training simulation to improve patient safety. Journal of Surgical Education. 2016;73(1):7–11. doi: 10.1016/j.jsurg.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 20.LeBlanc J, Hutchison C, Hu Y, Donnon T. Topics in training : A comparison of orthopaedic resident performance on surgical fixation of an ulnar fracture using virtual reality and synthetic models. Journal of Bone and Joint Surgery Series A. 2013;95:9. doi: 10.2106/JBJS.K.01284. [DOI] [PubMed] [Google Scholar]
- 21.Dwyer T, Shantz JS, Chahal J, Wasserstein D, Schachar R, Kulasegaram KM, et al. Simulation of anterior cruciate ligament reconstruction in a dry model. American Journal of Sports Medicine. 2015;43(12):2997–3004. doi: 10.1177/0363546515608161. [DOI] [PubMed] [Google Scholar]
- 22.Butler A, Olson T, Koehler R, Nicandri G. Topics in training: Do the skills acquired by novice surgeons using anatomic dry models transfer effectively to the task of diagnostic knee arthroscopy performed on cadaveric specimens? Journal of Bone and Joint Surgery Series A. 2013;95:3. doi: 10.2106/JBJS.L.00491. [DOI] [PubMed] [Google Scholar]
- 23.Dwyer T, Schachar R, Leroux T, Petrera M, Cheung J, Greben R, et al. Performance assessment of arthroscopic rotator cuff repair and labral repair in a dry shoulder simulator arthroscopy. Journal of Arthroscopic and Related Surgery. 2017;33(7):1310–1318. doi: 10.1016/j.arthro.2017.01.047. [DOI] [PubMed] [Google Scholar]
- 24.Howells NR, Auplish S, Hand GC, Gill HS, Carr AJ, Rees JL. Retention of arthroscopic shoulder skills learned with use of a simulator: Demonstration of a learning curve and loss of performance level after a time delay. Journal of Bone and Joint Surgery Series A. 2009;91(5):1207–1213. doi: 10.2106/JBJS.H.00509. [DOI] [PubMed] [Google Scholar]
- 25.Pollard TCB, Khan T, Price AJ, Gill HS, Glyn-Jones S, Rees JL. Simulated hip arthroscopy skills: Learning curves with the lateral and supine patient positions: A randomized trial. Journal of Bone and Joint Surgery Series A. 2012;94:10. doi: 10.2106/JBJS.K.00690. [DOI] [PubMed] [Google Scholar]
- 26.Rebolledo, B., Hammann-Scala, J., Leali, A., Ranawat, A. Arthroscopy skills development with a surgical simulator: A comparative study in orthopaedic surgery residents. https://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=ovftq&NEWS=N&AN=00000475-201506000-00029 [DOI] [PubMed]
- 27.N.L. VZ, K. Y. Arthroscopic capsular release of the elbow [DOI] [PubMed]
- 28.Morrey BF. The posttraumatic stiff elbow. Clinical Orthopaedics and Related Research. 2005;20:26–35. [PubMed] [Google Scholar]
- 29.Lesman, J., Luceri, F., Domzalski, M., Randelli, P.S., Arrigoni, P. The mini-open plication of medial collateral ligament of the elbow: A new arthroscopically assisted technique. https://journals.lww.com/shoulderelbowsurgery/Fulltext/2019/12000/The_Mini_open_Plication_of_Medial_Collateral.3.aspx
- 30.Arrigoni P, Luceri F, Cucchi D, Tamini J, Randelli PS. Reliability of anterior medial collateral ligament plication of the elbow. Musculoskeletal Surgery. 2018;102:89–91. doi: 10.1007/s12306-018-0554-8. [DOI] [PubMed] [Google Scholar]
- 31.Camp CL, Krych AJ, Stuart MJ, Regnier TD, Mills KM, Turner NS. Improving resident performance in knee arthroscopy: A prospective value assessment of simulators and cadaveric skills laboratories. Journal of Bone and Joint Surgery - American. 2016;98(3):220–225. doi: 10.2106/JBJS.O.00440. [DOI] [PubMed] [Google Scholar]
- 32.Price AJ, Erturan G, Akhtar K, Judge A, Alvand A, Rees JL. Evidence-based surgical training in orthopaedics: How many arthroscopies of the knee are needed to achieve consultant level performance? Bone and Joint Journal. 2015;97(10):1309–1315. doi: 10.1302/0301-620X.97B10.35973. [DOI] [PubMed] [Google Scholar]
- 33.Morgan M, Aydin A, Salih A, Robati S, Ahmed K. Current status of simulation-based training tools in orthopedic surgery: A systematic review. Journal of Surgical Education. 2017;74(4):698–716. doi: 10.1016/j.jsurg.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 34.Martin JA, Regehr G, Reznick R, Macrae H, Murnaghan J, Hutchison C, et al. Objective structured assessment of technical skill (OSATS) for surgical residents British Journal of Surgery 1997;84(2):273–78. [DOI] [PubMed]
- 35.Andelman SM, Meier KM, Walsh AL, Kim JH, Hausman MR. Pediatric elbow arthroscopy: indications and safety. Journal of Shoulder and Elbow Surgery. 2017;26(10):1862–1866. doi: 10.1016/j.jse.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 36.Baker CL, Jones GL. Arthroscopy of the elbow. The American Journal of Sports Medicine. 1999;27(2):251–264. doi: 10.1177/03635465990270022401. [DOI] [PubMed] [Google Scholar]
- 37.Frank RM, Wang KC, Davey A, Cotter EJ, Cole BJ, Romeo AA, et al. Utility of modern arthroscopic simulator training models: a meta-analysis and updated systematic review arthroscopy. Journal of Arthroscopic and Related Surgery. 2018;34(5):1650–1677. doi: 10.1016/j.arthro.2017.10.048. [DOI] [PubMed] [Google Scholar]