Abstract
Introduction
Autologous platelet rich plasma (PRP) local injection has been recently proposed as a treatment of plantar fasciitis. The autologous PRP does not have much side effects compared to steroid injections. So far PRP injections have shown promising results in various studies. This study assessed the efficacy of a single local injection of PRP in chronic unilateral plantar fasciitis through a prospective case series.
Methodology
A hospital-based prospective case series of 30 unilateral plantar fasciitis patients with symptom duration of 6 months or more were included in the study. All patients included in the study were assessed clinically and by visual analogue score for heel pain, AHS component of AOFAS and FADI scores before injection and at 6 and 12 week follow-up. USG measurement of plantar fascia thickness was done at pre-injection and at 12 weeks follow-up. All patients were observed for 12 weeks.
Results
The mean age was 39 years (range 20–55 years). The pre-injection VAS score for heel pain was 6.5 ± 1.1 which improved to 2.7 ± 0.5 and 1.8 ± 0.8 at 6 and 12 week respectively and difference was significant (p < 0.001). The baseline FADI and AHS component of AOFAS scores were 53.1 ± 9.0 and 72.2 ± 5.7 which improved to 65.5 ± 5.3 and 76.1 ± 4.5 at 6 weeks and, 77.9 ± 4.4 and 85.7 ± 4.6 at 12 weeks respectively which was significant (p < 0.001). The baseline mean plantar fascia thickness was 4.9 ± 0.3 mm which was significantly (p < 0.001) reduced to 3.9 ± 0.3 mm at 12 weeks post PRP injection. All pairwise comparisons by the post-hoc Wilcoxon signed rank test with p-value adjustment were also significant.
Conclusion
The short-term results of single dose PRP injections shows clinical and statistically significant improvements in VAS for heel pain, functional outcome scores and plantar fascia thickness measured by USG. This study concludes that local PRP injection is a viable management option for chronic plantar fasciitis.
Keywords: Plantar fasciitis, Platelet rich plasma, Ultrasound, USG, Plantar fascia thickness
Introduction
Plantar fasciitis is one of the common aetiologies of foot and heel pain in adults. It is bilateral in 30% of patients [1–3]. The peak incidence is between 40 and 60 years, with a younger peak in athletes [4]. The pathology involves the origin of the plantar fascia at the medial calcaneal tuberosity hence the pain is localized at that point. The aetiology is multifactorial and poorly understood. The known risk factors are obesity, poor foot and ankle biomechanics, flat feet, prolonged standing, jumping, running and ill-fitting footwear. Plantar fasciitis can be isolated or associated with other systemic diseases like seronegative spondyloarthropathies [5–9].
Various therapies have been reported, but the available evidence for a single modality of management is inadequate and conflicting. As of now there is no gold standard treatment for plantar fasciitis. Even though the corticosteroid injections have shown satisfactory short-term results, they were associated with various local and systemic adverse effects [10, 11]. These adversities have led to search for other options for the treatment of plantar fasciitis.
Injection of autologous platelet rich plasma (PRP) has been recently proposed as a treatment for plantar fasciitis on the evidence that it contains various growth factors and cytokines that may induce local factors to accelerate healing process [12]. The autologous PRP does not have side effects compared to steroid injections. So far, PRP injections have shown promising results in various studies. This prospective case series makes use of the VAS score for heel pain, functional outcome scores and ultrasonographic (USG) measurement of plantar fascia thickness as an outcome measure to study the actual role of single local injection of PRP in the management of plantar fasciitis. Literature utilising USG measurement of plantar fascia thickness as an outcome measure to study the effectiveness of PRP injection are very few which makes this study unique. The null hypothesis is that PRP injection has no effect in the outcome of plantar fasciitis management.
Methodology
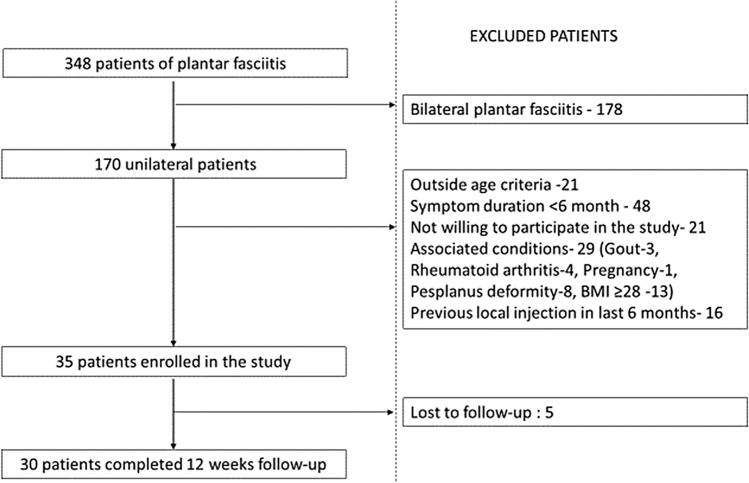
This is a hospital-based prospective case series, conducted between January 2018 and January 2019. Patients aged between 20 and 60 years, presented with unilateral heel pain or pain on first step in the morning relieved by unloading and diagnosed as a case of unilateral plantar fasciitis of at least 6 months duration in whom symptoms did not improve despite conservative treatment were included. Patients with BMI ≥ 28, bilateral disease, nerve related pathologies, Achilles tendinitis or tendinosis, Rheumatoid arthritis, ankylosing spondylitis, local infection, Gout, pregnant or breastfeeding, metastatic disease, complex regional pain syndrome, bony spur on plain radiograph, Previous intra-lesional injection in the last 6 months for the same condition, Previous foot surgery and those not willing for consent or follow-up were excluded from the study (Flowchart showing the scheme of patient enrolment shown in Fig. 1).
Fig. 1.
Flowchart showing the scheme of patient enrolment in the study
After fulfilling the inclusion and exclusion criteria, 30 patients were enrolled in the study. After ethical clearance, all patients were informed about the methodology. Informed and written consent were taken. All patients were assessed by pain and disability measurement of the foot through questionnaires (visual analogue pain score, AHS component of American Orthopaedic Foot and Ankle Society clinical rating system and the Foot and Ankle Disability Index) were taken before injection and at 6 and 12 week post injection to monitor the functional status. Thickness of plantar fascia at its origin was measured by USG at pre-injection and at 12 weeks post-injection to assess the response of plantar fascia to the PRP injection. PRP was prepared by centrifuging 30–35 ml of patient's blood collected by sterile venepuncture (Method shown in Fig. 2). Under aseptic precautions all patients received 3 cc autologous PRP injection into the origin of the plantar fascia, by peppering technique for expansive zone of delivery. All injections were administered by a single orthopaedic surgeon. After injection all patients were monitored for 30 min for any adverse reaction. Following which they were allowed weight bearing as tolerated. After 2 weeks, plantar fascia stretching exercises were initiated. Foot inversion exercises, tip toe and heel walking were permitted after 6 weeks. All patients were followed up for 12 weeks.
Fig. 2.

Flowchart showing the method of preparation of PRP
Statistics Descriptive statistics were used initially. The Shapiro–Wilk test was performed on each variable to assess for Normality. Since VAS, FADI and AHS were found to violate Normality at one or more of the assessed weeks, Friedman’s test for repeated measures was used to assess the significance of differences between the assessments at 0, 6 and 12 weeks. A significant Friedman test was followed up by post-hoc tests using Wilcoxon signed rank test with p-value adjustment by the Holm’s method [13, 14]. Since the USG measurements of plantar fascia thickness did not show significant departure from Normality, a paired t-test was used to test the difference between the USG measurements at 12 weeks to the USG measurements at baseline.
For all assessments of the significance tests, a p-value of 0.05 or less was considered to be statistically significant. All tests were done using R statistical software [15] version 3.6.0 along with the add-on “Rcmdr.EZR” [14].
Results
The mean age of the study cohort was 39 years (SD 8.8 year) with a range of 20–55 year. Females were predominantly affected and right foot was more commonly involved. The mean symptom duration was 19 weeks (SD 4.9 weeks) (Demographic profile shown in Table 1).
Table 1.
Demographic profile
| Mean ± SD | |
|---|---|
| Age | 39.0 ± 8.8 years (range 20–55 years) |
| Symptom duration | 19.1 ± 5 weeks (range 12–28 weeks) |
| Gender | Male = 4; female = 26 |
| Side affected | Right = 18; left = 12 |
The pre-injection VAS score for heel pain was 6.5 ± 1.1 which improved to 2.7 ± 0.5 and 1.8 ± 0.8 at 6 and 12 week respectively which was statistically significant (p < 0.001). The baseline FADI and AHS scores were 53.1 ± 9.0 and 72.2 ± 5.7 which post PRP injection improved to 65.5 ± 5.3 and 76.1 ± 4.5 at 6 weeks and, 77.9 ± 4.4 and 85.7 ± 4.6 at 12 weeks respectively. The improvement in all the scores were statistically significant at both 6 weeks and 12 weeks post PRP injection (p < 0.001 by the Friedman test). All pairwise comparisons by the post-hoc Wilcoxon signed rank test with p-value adjustment were also significant. For each outcome, the median and range are summarized in Table 2.
Table 2.
Summarizing the baseline and post-intervention outcome measures
| Pre-intervention median (range) | 6 weeks median (range) | 12 weeks median (range) | p value | ||
|---|---|---|---|---|---|
| Pre vs. 6 weeks | Pre vs. 12 weeks | ||||
| VAS score | 7 (4–8) | 2 (1–5) | 2 (1–4) | p < 0.001 | p < 0.001 |
| FADI score | 52.4 (27.0–66.3) | 67.3 (44.0–71.0) | 78.9 (67.9–84.8) | p < 0.001 | p < 0.001 |
| AHS score | 72.0 (59.0–83.0) | 75.0 (64.0–84.0) | 84.0 (74.0–96.0) | p < 0.001 | p < 0.001 |
The mean thickness of plantar fascia of the affected foot assessed by USG at baseline was 4.9 mm with a standard deviation (SD) of 0.4 mm which was significantly (p < 0.001 by the paired t-test) reduced to a mean of 3.9 mm and SD of 0.3 mm at 12 weeks post PRP injection (Table 3). The study also showed that the mean thickness of plantar fascia of the normal foot to be 3.5 mm with a SD of 0.3 mm. USG images showing the thickness of plantar fascia of normal and affected foot are shown in Figs. 3, 4 respectively.
Table 3.
Summarizing plantar fascia thickness assessed by USG at baseline and at 12 weeks post PRP injection
| USG (Mean ± SD) | |||
|---|---|---|---|
| Pre-intervention (0 weeks) mm | Post-intervention (12 weeks) mm | p value | |
| Affected foot | 4.9 ± 0.4 | 3.9 ± 0.3 | p < 0.001 |
Fig. 3.
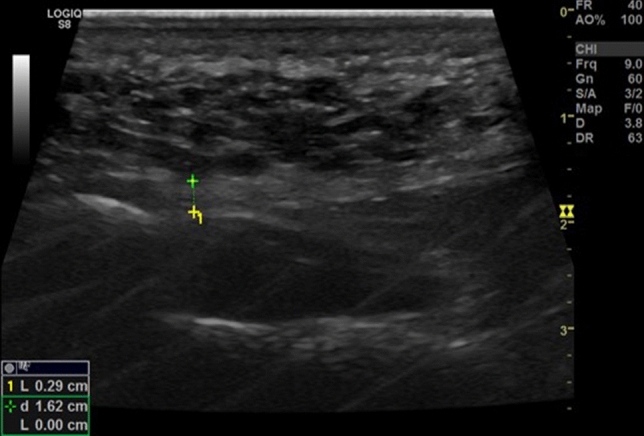
Plantar fascia thickness measured by ultrasonogram in an asymptomatic foot
Fig. 4.
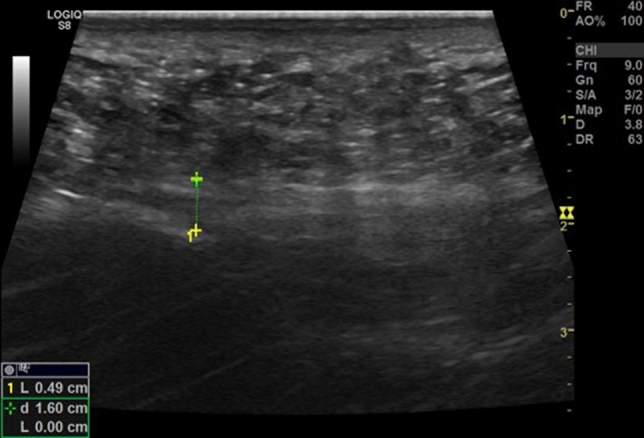
Plantar fascia thickness measured by ultrasonogram in a symptomatic foot
Discussion
Plantar fasciitis is often a self-limiting condition. In nearly 80% of the patients, the symptoms resolves spontaneously by 1 year from the onset [16], while in some patients it takes a chronic course and seriously affecting their day to day activities and quality of living in addition to a heavy health care burden [17, 18]. The aetiology and management of Plantar fasciitis is not fully understood [19, 20]. Contrary to the name, plantar fasciitis is not an inflammatory but a degenerative pathology due to repetitive microtrauma leading to wear of the plantar fascia at its origin [21, 22].
The treatment of plantar fasciitis is mainly aimed at alleviating pain and functional improvement. Plantar fasciitis is mainly treated by conservative therapies including activity modification, NSAID’s, ice application, arch support, splinting/strapping, deep tissue massage, plantar fascia stretching exercises and physical therapy to alleviate the symptoms [23, 24]. RCT by Gupta et al. reported that plantar fascia stretching exercises provide significant symptomatic relief than heat, silicone heel pad or calf stretching exercises [9]. Despite the conservative treatment, in around 10% patients, the symptoms persist and leads to chronic plantar fasciitis. Currently local corticosteroid injections are the mainstay in the treatment of chronic plantar fasciitis as they provide satisfactory short-term outcomes. The anti-inflammatory property of corticosteroids are effective in reducing the heel pain [25, 26]. They also inhibit the proliferation of fibroblasts and ground substance proteins [27]. Although the advantages are significant, multiple injections are often required and are associated with rupture or tear of plantar fascia, abscesses, osteomyelitis and infection, depigmentation of skin, nerve and muscle injury, post-injection flare, and heel fat pad atrophy [10, 11, 28].
Local injection of PRP is a recently introduced treatment of plantar fasciitis. PRP is rich in growth factors (TGF, VEGF, PDGF), cytokines and interleukins [29]. In plantar fasciitis, the growth factors and anti-inflammatory cytokines in the PRP initiate the healing process at the site of degeneration of plantar fascia and alleviates the symptoms [29, 30]. PRP injection is ideally infiltrated at the point of maximum tenderness of the affected heel.
Several case series and RCT’s were published in the literature reporting the effectiveness of PRP injection in plantar fasciitis. Martinelli et al. [30] reported a case series of 14 patients of plantar fasciitis treated with three doses of PRP injection, in their study the VAS scores had reduced from 7.1 pre-treatment to 1.9 at the 12-month follow-up. Another case series by Ragab and Othman [31] reported a complete alleviation of pain with a single dose PRP injection in 88% of their patients (n = 25) at 12 month follow-up. Kumar et al.[32] in their cases series of 44 patients (50heels) treated with single PRP injection reported that at 6 month post-injection, baseline RM score, VAS score and AOFAS improved from mean 4 to 2 (p < 0.001), 7.7 to 4.2 (p < 0.001) and 60.6 to 81.9 (p < 0.001) respectively. All the three studies concluded that PRP injection is very much effective in the treatment of plantar fasciitis.
RCT by Jain et al. [33], comparing PRP with steroid injections reported that the mean VAS, AOFAS, and RM scores in the PRP group was 3.3, 88.5, and 1.9 respectively and in the steroid group was 5.3, 75, and 2.6 respectively at the 12 month follow-up and the difference was significant. Similar study by Say et al. [34] reported that the mean AOFAS in PRP group was 85.5 ± 4.2 and 90.6 ± 2.6, compared with 75.3 ± 4.8 and 80.3 ± 4.7 in the steroid group, respectively at 6 weeks and 6 months of follow-up. The difference in the scores were statistically significant (p < 0.001) at both the follow-up. Changes in AOFAS and VAS scores were significantly higher in the PRP group (p < 0.001). Another similar study by Shetty et al. [35] reported that at the 3-month follow-up, VAS, AOFAS and Foot and Ankle Disability Index (FADI) scores were significantly improved in both steroid and PRP groups. The study concluded that PRP injection gives a better outcome than that of the steroid injections.
All the three studies that compared the outcomes of PRP with steroid injection concluded that PRP injection had better patient related outcome measures than steroids. (Various case series that studied the efficacy of PRP injection in plantar fasciitis is summarized in Table 4). The results obtained in this study shown that PRP injection definitely reduces pain and improves the VAS score for heel pain and functional scores (FADI and AHS) in patients with plantar fasciitis. The difference from the baseline was statistically significant at both 6 and 12-week follow-up (p < 0.001).
Table 4.
Summarizing various case series that studied the efficacy of PRP injection in plantar fasciitis
| Study | Type of case series | No of patients | No of PRP injections | Outcome measures | Final follow-up | Study conclusion (effectiveness of PRP injection) |
|---|---|---|---|---|---|---|
| Ragab and Othman [26] (2012) | Prospective | 25 | 1 | VAS, Ultrasound | 12 months | Effective |
| Martinelli et al. [25] (2013) | Prospective | 14 | 3 | VAS, RM score | 12 months | Effective |
| Kumar et al. [27] (2013) | Prospective | 44 (50 heels) | 1 | VAS, AOFAS score, RM score | 6 months | Effective |
| Wilson et al. [35] (2014) | Prospective | 12 (24 heels) | 1 | FAAM, Foot-SANE score, SF-12v2 | 12 months | Effective |
VAS, visual analogue scale, AOFAS score, The American Orthopaedic Foot and Ankle Society Ankle-Hindfoot Score, RM-Roles and Maudsley score, FAAM- Foot and Ankle Ability Measure Score, SANE- Single Assessment Numeric Evaluation, SF-12v2- Short Form 12 item (version 2)
Plantar fasciitis causes abnormal thickening of the plantar fascia (> 4.0 mm) in almost all cases [36]. This change in plantar fascia thickness can be easily assessed by ultrasonography (USG) [37]. These measurements can be used to monitor response to the treatment. Several studies reported that both the corticosteroid and PRP injections are effective in reducing the plantar fascia thickness [25, 38, 39]. Study by Jain et al. [33] reported that the thickness of plantar fascia was reduced significantly following the steroid injection than that of PRP injection at 1 and 3 month follow-up (p = 0.004 and p = 0.011 respectively) but the difference at the 6-month follow-up was not significant (P = 0.148). They concluded that corticosteroid injection provides rapid reduction in the plantar fascia thickness in the first 3 months of injection but the results are comparable at 6 months. In this study, at 12 week follow-up, the thickness of plantar fascia was reduced to 3.9 ± 0.3 mm from 4.9 ± 0.3 mm at preintervention which was statistically significant (p < 0.001).
All patients in the study tolerated the local PRP injection without any significant local or systemic adverse events. Limitations of this study were small study population, a short duration of follow-up and lack of a control group. To overcome the shortcomings of this study, RCT with a larger study population and a longer follow-up will be helpful in better understanding of the long-term benefits and efficacy of the PRP injection in the management of chronic plantar fasciitis.
Conclusion
The outcomes of this study suggest that the short-term results of single dose PRP injection in chronic plantar fasciitis showed clinically and statistically significant improvements in VAS for heel pain, functional outcome scores and restoration of plantar fascia thickness confirmed by USG measurements. Hence, the null hypothesis is rejected. The study concludes that local PRP injection is a viable and safe treatment option for chronic plantar fasciitis.
Funding
This study was funded by All-India Institute of Medical Sciences, Rishikesh (IN) (IM/RC100/2016/25).
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
The Institutional Ethics Committee approved the study.
Informed consent
Informed and written consent were obtained from all participants of the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
R. B. Kalia, Email: roop.orth@aiimsrishikesh.edu.in
Vivek Singh, Email: singhvr27@gmail.com.
Nilotpal Chowdhury, Email: nilotpal.chowdhury@gmail.com.
Ashish Jain, Email: ashish.jain.modi@gmail.com.
Sanny Kumar Singh, Email: sunnysanny797@gmail.com.
Lakshmana Das, Email: sekarldas@gmail.com.
References
- 1.Furey JG. Plantar fasciitis. The painful heel syndrome. Journal Bone Joint Surgery Am. 1975;57(5):672–673. doi: 10.2106/00004623-197557050-00016. [DOI] [PubMed] [Google Scholar]
- 2.Lapidus PW, Guidotti FP. Painful heel: report of 323 patients with 364 painful heels. Clinical Orthopaedics and Related Research. 1965;39:178–186. [PubMed] [Google Scholar]
- 3.Sadat-Ali M. Plantar fasciitis/calcaneal spur among security forces personnel. Military Medicine. 1998;163(1):56–57. doi: 10.1093/milmed/163.1.56. [DOI] [PubMed] [Google Scholar]
- 4.Nahin RL. Prevalence and pharmaceutical treatment of plantar fasciitis in United States adults. The Journal of Pain. 2018;19(8):885–896. doi: 10.1016/j.jpain.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. British Journal of Sports Medicine. 2002;36(2):95–101. doi: 10.1136/bjsm.36.2.95.PMID:11916889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for plantar fasciitis: a matched case-control study. Journal of Bone and Joint Surgery American. 2003;85(5):872–877. doi: 10.2106/00004623-200305000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Rano JA, Fallat LM, Savoy-Moore RT. Correlation of heel pain with body mass index and other characteristics of heel pain. The Journal of Foot and Ankle Surgery. 2001;40(6):351–356. doi: 10.1016/s1067-2516(01)80002-8. [DOI] [PubMed] [Google Scholar]
- 8.Weiler A, Helling HJ, Kirch U, Zirbes TK, Rehm KE. Foreign-body reaction and the course of osteolysis after polyglycolide implants for fracture fixation: experimental study in sheep. Journal of Bone and Joint Surgery. British. 1996;78(3):369–376. doi: 10.1302/0301-620X.78B3.0780369. [DOI] [PubMed] [Google Scholar]
- 9.Gupta R, Malhotra A, Masih GD, Khanna T, Kaur H, Gupta P, Kashyap S. Comparing the role of different treatment modalities for plantar fasciitis: a double blind randomized controlled trial. Indian Journal of Orthopaedics. 2020;54(1):31–37. doi: 10.1007/s43465-019-00038-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buccilli TA, Jr, Hall HR, Solmen JD. Sterile abscess formation following a corticosteroid injection for the treatment of plantar fasciitis. The Journal of Foot and Ankle Surgery. 2005;44(6):466–468. doi: 10.1053/j.jfas.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 11.Acevedo JI, Beskin JL. Complications of plantar fascia rupture associated with corticosteroid injection. Foot and Ankle International. 1998;19(2):91–97. doi: 10.1177/107110079801900207. [DOI] [PubMed] [Google Scholar]
- 12.Lee TG, Ahmad TS. Intralesional autologous blood injection compared to corticosteroid injection for treatment of chronic plantar fasciitis. A prospective, randomized, controlled trial. Foot Ankle International. 2007;28(9):984–990. doi: 10.3113/FAI.2007.0984. [DOI] [PubMed] [Google Scholar]
- 13.Holm S. A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics. 1979;6(2):65–70. [Google Scholar]
- 14.Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplantation. 2013;48(3):452–458. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; (2019).
- 16.Wolgin M, Cook C, Graham C, Mauldin D. Conservative treatment of plantar heel pain: long-term follow-up. Foot and Ankle International. 1994;15(3):97–102. doi: 10.1177/107110079401500303. [DOI] [PubMed] [Google Scholar]
- 17.Tong KB, Furia J. Economic burden of plantar fasciitis treatment in the United States. American Journal of Orthopaedics (Belle Mead NJ). 2010;39(5):227–231. [PubMed] [Google Scholar]
- 18.Irving DB, Cook JL, Young MA, Menz HB. Impact of chronic plantar heel pain on health-related quality of life. Journal of the American Podiatric Medical Association. 2008;98(4):283–289. doi: 10.7547/0980283. [DOI] [PubMed] [Google Scholar]
- 19.Beeson P. Plantar fasciopathy: revisiting the risk factors. Foot and Ankle Surgery. 2014;20(3):160–165. doi: 10.1016/j.fas.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Kirkland P, Beeson P. Use of primary corticosteroid injection in the management of plantar fasciopathy: is it time to challenge existing practice? Journal of the American Podiatric Medical Association. 2013;103(5):418–429. doi: 10.7547/1030418. [DOI] [PubMed] [Google Scholar]
- 21.Buchbinder R. Clinical practice. Plantar fasciitis. New England Journal of Medicine. 2004;350(21):2159–2166. doi: 10.1056/NEJMcp032745. [DOI] [PubMed] [Google Scholar]
- 22.Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. Journal of the Ameican Podiatric Medical Association. 2003;93(3):234–237. doi: 10.7547/87507315-93-3-234. [DOI] [PubMed] [Google Scholar]
- 23.Cornwall MW, McPoil TG. Plantar fasciitis: etiology and treatment. Journal of Orthopaedic and Sports Physical Therapy. 1999;29(12):756–760. doi: 10.2519/jospt.1999.29.12.756. [DOI] [PubMed] [Google Scholar]
- 24.Toomey EP. Plantar heel pain. Foot and Ankle Clinics. 2009;14(2):229–245. doi: 10.1016/j.fcl.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 25.Genc H, Saracoglu M, Nacir B, Erdem HR, Kacar M. Long-term ultrasonographic follow-up of plantar fasciitis patients treated with steroid injection. Joint Bone Spine. 2005;72(1):61–65. doi: 10.1016/j.jbspin.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 26.Kiter E, Celikbas E, Akkaya S, Demirkan F, Kiliç BA. Comparison of injection modalities in the treatment of plantar heel pain: a randomized controlled trial. Journal of the American Podiatric Medical Association. 2006;96(4):293–296. doi: 10.7547/0960293. [DOI] [PubMed] [Google Scholar]
- 27.McMillan AM, Landorf KB, Gilheany MF, Bird AR, Morrow AD, Menz HB. Ultrasound guided injection of dexamethasone versus placebo for treatment of plantar fasciitis: protocol for a randomised controlled trial. Journal of Foot and Ankle Research. 2010;16(3):15. doi: 10.1186/1757-1146-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sellman JR. Plantar fascia rupture associated with corticosteroid injection. Foot and Ankle International. 1994;15(7):376–381. doi: 10.1177/107110079401500706. [DOI] [PubMed] [Google Scholar]
- 29.Molloy T, Wang Y, Murrell G. The roles of growth factors in tendon and ligament healing. Sports Medicine (Auckland, N. Z.) 2003;33(5):381–394. doi: 10.2165/00007256-200333050-00004. [DOI] [PubMed] [Google Scholar]
- 30.Martinelli N, Marinozzi A, Carnì S, Trovato U, Bianchi A, Denaro V. Platelet-rich plasma injections for chronic plantar fasciitis. International Orthopaedics. 2013;37(5):839–842. doi: 10.1007/s00264-012-1741-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ragab EM, Othman AM. Platelets rich plasma for treatment of chronic plantar fasciitis. Archives of Orthopaedic and Trauma Surgery. 2012;132(8):1065–1070. doi: 10.1007/s00402-012-1505-8. [DOI] [PubMed] [Google Scholar]
- 32.Kumar V, Millar T, Murphy PN, Clough T. The treatment of intractable plantar fasciitis with platelet-rich plasma injection. The Foot (Edinb) 2013;23(2–3):74–77. doi: 10.1016/j.foot.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 33.Jain K, Murphy PN, Clough TM. Platelet rich plasma versus corticosteroid injection for plantar fasciitis: a comparative study. The Foot (Edinb) 2015;25(4):235–237. doi: 10.1016/j.foot.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 34.Say F, Gürler D, İnkaya E, Bülbül M. Comparison of platelet-rich plasma and steroid injection in the treatment of plantar fasciitis. Acta Orthopaedica Traumatologica Turcica. 2014;48(6):667–672. doi: 10.3944/AOTT.2014.13.0142. [DOI] [PubMed] [Google Scholar]
- 35.Shetty VD, Dhillon M, Hegde C, Jagtap P, Shetty S. A study to compare the efficacy of corticosteroid therapy with platelet-rich plasma therapy in recalcitrant plantar fasciitis: a preliminary report. Foot and Ankle Surgery. 2014;20(1):10–13. doi: 10.1016/j.fas.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 36.McMillan AM, Landorf KB, Barrett JT, Menz HB, Bird AR. Diagnostic imaging for chronic plantar heel pain: a systematic review and meta-analysis. Journal of Foot Ankle Research. 2009;13(2):32. doi: 10.1186/1757-1146-2-32.PMID:19912628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kane D, Greaney T, Shanahan M, Duffy G, Bresnihan B, Gibney R, FitzGerald O. The role of ultrasonography in the diagnosis and management of idiopathic plantar fasciitis. Rheumatology (Oxford) 2001;40(9):1002–1008. doi: 10.1093/rheumatology/40.9.1002. [DOI] [PubMed] [Google Scholar]
- 38.Radwan A, Wyland M, Applequist L, Bolowsky E, Klingensmith H, Virag I. Ultrasonography, an effective tool in diagnosing plantar fasciitis: a systematic review of diagnostic trials. International Journal of Sports Physical Therapy. 2016;11(5):663–671. [PMC free article] [PubMed] [Google Scholar]
- 39.Tsai WC, Hsu CC, Chen CP, Chen MJ, Yu TY, Chen YJ. Plantar fasciitis treated with local steroid injection: comparison between sonographic and palpation guidance. Journal of Clinical Ultrasound. 2006;34(1):12–16. doi: 10.1002/jcu.20177. [DOI] [PubMed] [Google Scholar]