Abstract
Background
Lateral ankle sprains are among the common injuries in the physically active population in different age groups and progress to chronic ankle instability (CAI). Accordingly, the current study assesses the effectiveness of strengthening and proprioceptive training programs on proprioception and balance in those suffering from CAI.
Design
Quasi-experimental design.
Methods
Thirty-six individuals with self-reported CAI were assigned into three groups based on age: group 1 (23 ± 1.84), group 2 (35.80 ± 1.68), group 3 (44.25 ± 4.86), then performed strength and balance exercises for 6 weeks. The study furthermore measured pre- and post-training of joint position sense (JPS), static balance, dynamic balance, chronic ankle instability tool (CAIT) and lower extremity functional scale (LEFS).
Results
Statistical analysis showed significant improvement (P < 0.01) on all outcome measures among all groups. In group 1, mainly the plantar flexion JPS improved to 3.7°, while in group 2 and group 3 the eversion JPS improved to 3.1° and 1.78° (P < 0.01). With reference to static balance with one’s eyes closed and eyes open, the improvement in group 1 was 4.46, 11.05 s, group 2 was 2.23, 7.85 s and group 3 was 1.69, 4.68 s. In relation to dynamic balance, the development in group 1 was 5.85 cm, while group 2 was 4.71 cm and group 3 was 2.49 cm. Moreover, both CAIT and LEFS showed significant differences (P < 0.01) after training.
Conclusion
This study found that combined strengthening and proprioceptive training effectively improves stability, proprioception, balance, and self-reported functional outcomes.
Keywords: Ankle sprains, Joint position sense, Postural balance, Rehabilitation
Introduction
Lateral ankle sprains are one of the most common injuries in the general population, considering they account for more than 20% of all injuries related to the ankle joint [1]. Most ankle sprains are accompanied by abnormal joint kinematics and may lead to the development of various musculoskeletal disorders of the lower extremities [2]. It is expected that, for every 10,000 people, one ankle ligament sprain will happen per day [3] and more than 2 million individuals sustain an ankle injury every year in the US; the expenditure of treating these injuries is a significant healthcare concern [4]. Following an ankle sprain, the individuals are more vulnerable to re-injury that can initiate a string of long-term symptoms like pain, tenderness, weakness and instability. This can cause decreases in muscle strength, range of motion, proprioception, balance, and functional performance, and it may manifest as reduced joint position sense (JPS) [5] leading to ankle osteoarthritis [6]. 32–74% of people with a past history of lateral ankle sprains will experience ill effects and develop chronic ankle instability (CAI) [1].
The individual feeling of the ankle “giving way” after a primary ankle sprain and repetitive sessions of instability causing recurrent ankle sprains has been termed CAI [7]. Individuals with ankle sprains and CAI may experience both mechanical and functional instability of the ankle joint [8]. The instability is due to reduced precision of proprioceptive signals from the ankle joint [5] that are crucial for executing functional activities that require standing balance and to sustain overall posture of the body [9]. Theoretically, proprioception primarily supports responsiveness and controls movement by gaining evidence from a variety of peripheral afferents related to the position sense of mechanoreceptors [10]. Injury to these peripheral mechanoreceptors can change afferent input and efferent output, further altering the neuromuscular control and leading to CAI [11]. Deficits in proprioception correlate with increasing age and affect the postural stability of individuals [12, 13]. Evaluation of this postural stability using simple and inexpensive balance tests should be a standard segment of every ankle rehabilitation program so as to provide information about training progress.
Ankle proprioception is an important component for balance as it provides vital information to allow the adjustment of ankle positions to effectively perform the multifaceted motor tasks [14] that perform a vital role in balance control [15]. The researchers therefore focused primarily on enhancing ankle proprioception and postural stability using strength training programs to prevent the recurrent ankle sprains [16, 17]. Numerous studies specifically examined the effects of ankle strengthening exercises for a short term period and concluded that these were mainly beneficial to increase muscular development and improve neuromuscular control in the ankles of young adults [18–20]. These findings suggest that strength training without any prominence on proprioception may be valuable to develop ankle strength and proprioception deficits.
Researchers who evaluated functional performance after CAI found that, along with strength training, balance training is useful in rehabilitation to improve functional outcomes. Balance training involves single limb stance exercises on even, uneven or both surfaces as most individuals experiencing CAI have a decreased capacity to effectively maintain single limb stance [21]. Traditionally, balance training using wobble board techniques has been common among therapists as a means to decrease the symptoms of ankle instability and improve balance and muscle function [22, 23]. This likely mainly happens through neural information and neuro plasticity [15].
However, most research to date has not evaluate the long-term efficacy of these protocols in diverse populations with different training protocols. We believe increase in strength can differ depending upon on the resistance, number of repetitions, sets and study duration. The purpose of the current study is therefore to determine the effects of both strength and balance training on proprioception, static balance, dynamic balance and self-reported functional outcomes in different age groups.
Methods
Participants
Thirty-six people with a history of CAI volunteered to take part in this study and divided into three groups. Inclusion criteria for participating in this study entailed self-reported unilateral CAI, history of more than one lateral ankle sprain, frequent giving way incidents, must not have sustained an ankle sprain within 6 weeks of the start of the study, those who had a score of Cumberland Ankle Instability Tool (CAIT) of less than 24 points [24] and a lower extremity functional scale (LEFS) score of more than 32 points [25]. Exclusion criteria for the participants included any history of lower extremity injury/surgery, any history of head injury, and any vestibular or balance disorders. The study obtained written informed consent from all the participants and the study received approval from the Ethical Committee of King Khalid University ( ECM # 2019-08).
Procedure
The study divided subjects into 3 groups according to age. Group I consisted of 14 subjects aged 20–30 years, group II consisted of 10 subjects aged 31–40 years and group III consisted of 12 subjects aged 41–50 years. The study took static balance, dynamic balance, proprioception, CAIT and LEFS measurements before initiation and after training; measurements and results were used for statistical analysis.
Tools Used in the Study
CAI is mainly a symptom-based presentation because of its complications and multi-factorial nature. This means that different patient forms or questionnaires have developed for recognizing the pathology. Both CAIT [24] and LEFS [25] are highly reliable and valid, so this study used them to record the self-reported functional outcomes of the participants.
CAIT
CAIT is a highly reliable and valid questionnaire used without comparison to contra lateral ankle that consists of 9 questions and produces a score between 0 and 30 points. Participants may score between 0 and 30 with lower scores indicating decreased ankle stability and higher scores indicating increased stability. This study selected participants with a score of less than 24 points [24].
LEFS
LEFS measures the lower limb function across an extensive range of lower extremity disability levels and circumstances. Although it is imprecise for the ankle, it is a reliable and valid tool used in physical therapy rehabilitation settings. LEFS consists of 20 items that ask participants to rate their noticeable ability to perform various lower extremity tasks on a 5-point scale: 0 = extremely difficult to perform the activity, 1 = relatively difficult to perform the activity, 2 = moderately difficult to perform the activity, 3 = slightly difficult to perform the activity and 4 = no difficulty to perform activity. Ratings are summarized for a total LEFS score from 0 (very poor function) to 80 (excellent function). The current study selected participants with a score exceeding 32 points [25].
Static and Dynamic Balance
Recently, a systematic review also briefed the existing data and suggested that decreased balance is a significant factor related to increased ankle injuries [26]; moreover, these individuals have decreased capability to efficiently maintain balance, causing CAI [27]. We therefore consider that therapists must include balance assessments when evaluating chronic ankle instability. However, balance tests can be static or dynamic, and were considered as efficient clinical measures of the postural instability of the ankle joint.
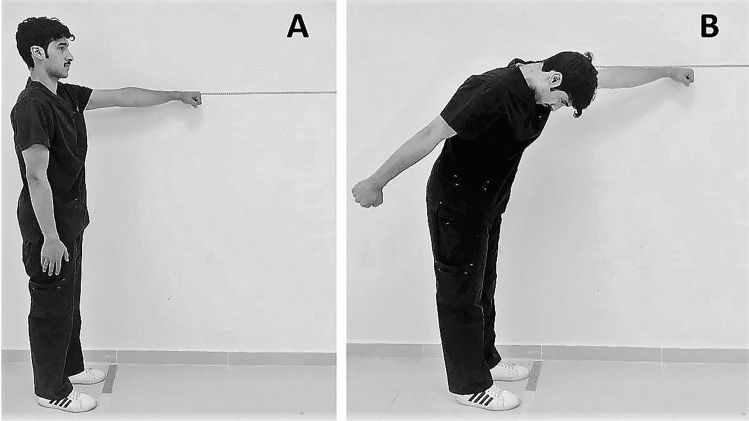
Single Leg Balance Test
The current study used the single leg balance test (SLB test) to assess static balance ability. In this test, the participants stand on a single leg without shoes or socks, with the opposite knee bent without touching the weight bearing leg. Participants’ hands were placed on both hips to prevent using their arms for balance (Fig. 1). The researcher then measured the length of time each participant could maintain their balance. The test was performed three times with the participants’ eyes open, then three times with eyes closed and an average of three trials were recorded in seconds for the study. At least 5 min of rest were permitted between each trial to avoid participant fatigue [11].
Fig. 1.
Measurement of static balance by single leg balance test
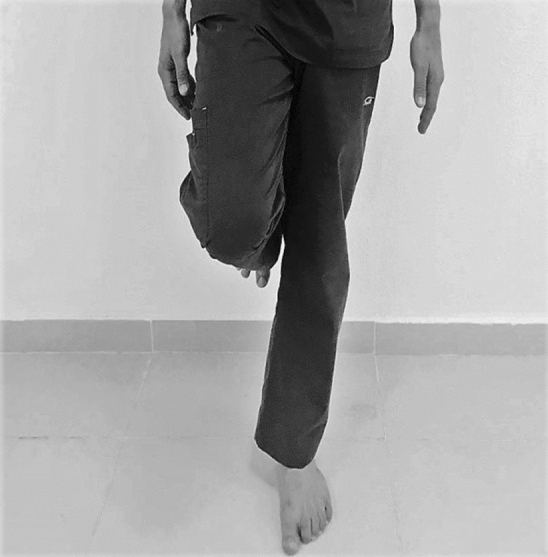
Functional Reach Test
The functional reach test (FRT) used as a simple and a cost-effective clinical tool for examining dynamic balance ability. In the test, the study requested that the participant enter a standing position on a line marked on the floor. An inch tape was attached to a wall at about the shoulder height of the subject. The therapist stood 5–10 feet away from the participant and instructed the participant to stand close to wall without touching it while facing the inch tape with shoulder flexion at 90° and hand fisted. The therapist recorded the starting position at the knuckle of the third metacarpal head on the ruler, then instructed the subject to reach as far forward as possible along the length of the tape without moving the feet (Fig. 2). At this time, the therapist once again recorded the location of the knuckle of the third metacarpal. Participants were required not to lean against the wall at any time during the test. If they did lose balance, the therapist stopped the test. The study determined scores by assessing the difference between the start and end positions, conducted three trials with one minute of rest between each and recorded the average for all the participants in centimeters [28].
Fig. 2.
Measurement of dynamic balance by functional reach test. a Starting position. b Final position
Measurement of Proprioception
A digital dual inclinometer (Dualer IQ PRO Digital Inclinometer, J-TECH, Midvale, UT 84047, USA) was used as a tool to measure the ankle joint proprioceptive sense in this study. The subject sat in an upward position with eyes closed. First, we fixed one part of the inclinometer to the lower section of the lateral face of the tibia along with the joint line with a strap. We fixed the other part of the inclinometer to the middle third lateral section of the foot and applied another strap. The extremity on which we secured the inclinometer was brought to the targeted angle and the subject’s ankle was maintained there for 10 s to remember this position. Next, the therapist took the subject’s extremity back to the initial position. The participant was then asked to bring the extremity actively to the target angle once again [29] (Fig. 3). The measurement procedure was conducted three times and the study used the mean values in degrees for analysis. We used the error angle deviated from the set angle as the result value of the test [20].
Fig. 3.

Measurement of ankle proprioception by digital dual inclinometer
Training Program
All the subjects in three training groups exercised five times per week over the course of a 6-week period. The time consumed in each session varied according to the group. Each training session was supervised by one of the therapists of the research team. The balance training [30] and strength training [19] protocols selected for this study were clinically effective methods focusing on restoring strength, proprioception, static and dynamic balance.
Balance Training
The balance training initiated for all participants when they could bear their full weight without pain, improving balance and postural stability. A variety of devices have been specifically designed for this phase of rehabilitation. Here, we instructed the subject to stand on one foot on the wobble board, thereby altering their weight. These exercises gradually progressed from non-weight bearing to weight bearing; eyes open to eyes closed; bilateral standing to unilateral standing position; and finally hard surface to soft surface using different sized hemispheres [30]. Each session lasted approximately 15–20 min and occurred over a period of 6 weeks (Table 1). During the balance training, the therapist faced different challenges as the modification of surfaces and conditions became extensive.
Table 1.
Ankle balance and strength training protocol
| Exercise | Training | Duration |
|---|---|---|
| Warm-up | Stretching around the ankle joint | 5 min |
| Balance training |
Wobble board: 5 times/week Weeks: 1–3 Move front to back, 15 s, 10 repetitions, 10 s rest between each repetition Move left to right side, 15 s, 10 repetitions, 10 s rest between each repetition Move-in circle, 60 s, 5 repetitions, rest 20 s between each repetition Weeks: 4–6 Knee flexion repeat the same exercises done from week 1–3, each 30 s, 5 repetitions, 20 s rest between each repetition Single leg stance eyes open for 7 s, 5 repetitions, 10 s rest Single leg stance eyes closed for 4 s, 5 repetitions, 10 s rest |
15–20 min/day |
| Strength training |
Thera band: 5 times/week Week 1: blue tubing, 3 sets, 10 repetitions—dorsiflexion, plantar flexion, inversion, eversion Week 2: blue tubing, 4 sets, 10 repetitions—dorsiflexion, plantar flexion, inversion, eversion Week 3: black tubing, 3 sets, 10 repetitions—dorsiflexion, plantar flexion, inversion, eversion Week 4: black tubing, 4 sets, 10 repetitions—dorsiflexion, plantar flexion, inversion, eversion Week 5: silver tubing, 3 sets, 10 repetitions—dorsiflexion, plantar flexion, inversion, eversion Week 6: silver tubing, 4 sets, 10 repetitions—dorsiflexion, plantar flexion, inversion, eversion |
10–15 min/day |
| Cool down | Stretching around the ankle joint | 5 min |
Strength Training
In CAI, the strength training is crucial for a speedy recovery and acts as a precautionary measure against recurrent ankle injury [31]. In this study, the strength training protocol targeted all the muscles around the ankle and participants performed all the exercises bilaterally. The strengthening exercises began with isometric exercises in all four directions of ankle movement and progressed to dynamic resistance exercises using Thera bands. Participants progressed weekly in sets and resistance during the training period. They were asked to sit on the floor with their knees extended. One end of the (doubled) Thera bands was attached to the wall knob and the circled end was secured to the foot while the participant performed dorsiflexion, plantar flexion, inversion and eversion motions (Table 1). Regardless of the color of the band, we determined the training resistance for all the subjects by calculating 70% of the Thera band resting length. We then added the measured distance to the resting length of each Thera band, and marked a line on the floor to which the participants had to stretch the band to perform these strengthening exercises. This type of training protocol was designed to ensure all participants train with a reliable and progressive amount of resistive force [32]. We instructed all the subjects to focus only on the ankle movements and not to enhance any unnecessary movements from either hip or knee joints. Each session lasted approximately 10–15 min for all the subjects occurring over a period of 6 weeks and progress occurred consistently throughout the training period.
Statistical Analysis
This study performed all statistical analyses using SPSS statistical software (version 21.0 for Windows; SPSS, Inc, Chicago, USA). In this study, we assessed the normality of distribution for the quantitative data using the Shapiro–Wilk test (p < 0.05), whereupon the variables of the study showed normal distribution. Each outcome measurement in this study was evaluated and expressed as Mean ± SD between the groups. We analyzed changes in all variables between pre- and post-training and between all the groups through one-way analysis of variance (ANOVA). Moreover, we used the Bonferroni post hoc test to evaluate any statistical difference between pre- and post-training across all treatment groups, setting statistical significance to an α level of p < 0.05 for all analyses.
Results
General Characteristics
Table 2 summarized the general characteristics of all the participants.
Table 2.
General characteristics of the participants
| Characteristic | Group 1 (n = 14) | Group 2 (n = 10) | Group 3 (n = 12) |
|---|---|---|---|
| Age (years) | 23 ± 1.84 | 35.80 ± 1.68 | 44.25 ± 4.86 |
| Height (cm) | 1.93 ± 0.11 | 2.0 ± 0.01 | 1.87 ± .295 |
| Weight (kg) | 75.07 ± 11.9 | 82.70 ± 9.61 | 78.01 ± 10.17 |
| BMI (kg/m2) | 24.32 ± 3.49 | 28.9 ± 3.41 | 28.06 ± 4.27 |
Ankle Proprioception
After the 6-week training program, participants in all three groups showed a significant change in proprioception from pre-training to post-training that varied significantly (P < 0.01) between the groups (Table 3). A significant difference in ankle joint position sense in group 1, group 2 and group 3 in dorsiflexion with 3.5° error (45.2%), 2.59° error (39.3%) and 1.35° (24.8%) in plantar flexion with 3.7° error (44.3%), 2.58° error (34.4%) and 1.16° (18%), in inversion 3.53° error (42.1%), 2.79° error ( 6.3%) and 1.29° (19.7%) and eversion 3.59° error (41%), 3.1° error (43.7%) and 1.78° (30.3%).
Table 3.
Differences in proprioception after training between different age groups (in degrees)
| Measure | Age | Mean ± SD | Standard error | 95% confidence interval | P value | |
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| Dorsiflexion | 20–30 | 3.73 ± 0.37 | 0.10 | 3.51 | 3.95 | < 0.001 |
| 31–40 | 3.10 ± 0.56 | 0.17 | 2.69 | 3.50 | ||
| 41–50 | 1.62 ± 0.52 | 0.15 | 1.29 | 1.95 | ||
| Plantar flexion | 20–30 | 3.67 ± 0.62 | 0.16 | 3.31 | 4.04 | < 0.001 |
| 31–40 | 2.90 ± 0.99 | 0.31 | 2.18 | 3.61 | ||
| 41–50 | 1.44 ± 1.08 | 0.31 | 0.75 | 2.13 | ||
| Inversion | 20–30 | 3.07 ± 1.01 | 0.27 | 2.48 | 3.65 | < 0.001 |
| 31–40 | 2.30 ± 0.48 | 0.15 | 1.95 | 2.64 | ||
| 41–50 | 1.12 ± 0.51 | 0.14 | 0.79 | 1.45 | ||
| Eversion | 20–30 | 3.75 ± 0.36 | 0.09 | 3.54 | 3.96 | < 0.001 |
| 31–40 | 2.7 ± 0.48 | 0.15 | 2.35 | 3.04 | ||
| 41–50 | 1.79 ± 0.39 | 0.11 | 1.54 | 2.04 | ||
Static Balance
In relation to static balance (eyes open), the duration of the time each participant maintained their balance increased in group 1 to 11.05 s (44.3%), group 2 to 7.85 s, (40%) and group 3 to 4.68 s (28.3%). Regarding static balance (eyes closed), the duration of the time each participant who maintained their balance increased in group 1 to 4.46 s (66.2%), group 2 to 2.23 s (40.9%) and group 3 to 1.69 s (36.5%). Outcome measures showed a statistically significant difference (P < 0.01) between all groups (Table 4).
Table 4.
Differences in static balance and dynamic balance between different age groups after training
| Measure | Age | Mean ± SD | Standard error | 95% confidence interval | P value | |
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| Static balance eyes open (s) | 20–30 | − 11.13 ± 0.62 | 0.16 | − 11.498 | − 10.774 | < 0.001 |
| 31–40 | − 8.10 ± 1.19 | 0.37 | − 8.956 | − 7.244 | ||
| 41–50 | − 4.90 ± 30.64 | 0.18 | − 5.315 | − 4.502 | ||
| Static balance eyes closed (s) | 20–30 | − 4.47 ± 0.63 | 0.46 | − 9.162 | − 7.271 | < 0.001 |
| 31–40 | − 2.30 ± 0.48 | 0.17 | − 4.839 | − 4.104 | ||
| 41–50 | − 1.77 ± 0.63 | 0.15 | − 2.646 | − 1.954 | ||
| Dynamic balance (cm) | 20–30 | − 5.75 ± 0.69 | 0.18 | − 2.181 | − 1.369 | < 0.001 |
| 31–40 | − 4.60 ± 0.69 | 0.22 | − 3.431 | − 2.508 | ||
| 41–50 | − 2.55 ± 40.88 | 0.18 | − 6.160 | − 5.354 | ||
Dynamic Balance
In relation to dynamic balance, the mean baseline variability in Functional reach test in subjects in group 1 reached a difference of 5.85 cm (15.1%), while group 2 was 4.71 cm (13.6%) and group 3 was 2.49 cm (9.8%). The Bonferroni post hoc test also showed no significant difference (P > 0.05) between group 2 and group 3, but the scale of variations in all three groups between pre- and post-training was statistically significant (P < 0.01) (Table 4).
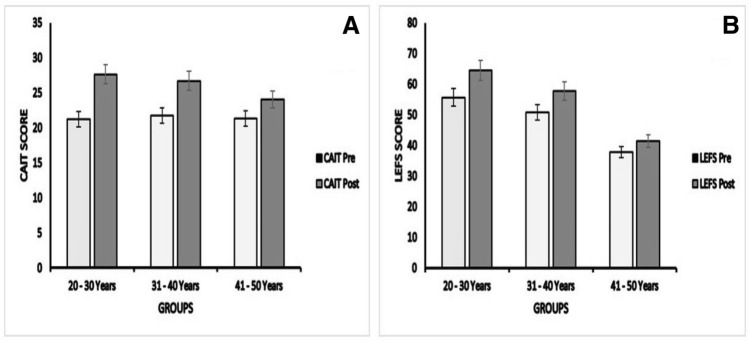
CAIT and LEFS
With reference to ankle stability, the CAIT score after training in group 1 increased by 5.93 points (27.3%), group 2 by 5.1 points (23.4%), and group by 2.67 points (12.5%). LEFS score increased in group 1 by 8.86 points (15.9%), group 2 by 7 points (13.8%) and group 3 by 3.58 points (9.48%). Pre- and post-training showed significant differences (P < 0.01) (Table 5) in both CAIT and LEFS in all age groups; however, the difference in group 3 was lower compared to the other two groups, which Fig. 4 aptly illustrates this effect.
Table 5.
Differences in CAIT and LEFS between different age groups after training
| Measure | Age | Mean ± SD | Standard error | 95% confidence interval | P value | |
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| CAIT | 20–30 | − 6.42 ± 0.85 | 0.22 | − 6.920 | − 5.937 | < 0.001 |
| 31–40 | − 5.0 ± 0.66 | 0.21 | − 5.477 | − 4.523 | ||
| 41–50 | − 2.66 ± 1.07 | 0.30 | − 3.348 | − 1.985 | ||
| LEFS | 20–30 | − 8.85 ± 0.77 | 0.20 | − 9.302 | − 8.412 | < 0.001 |
| 31–40 | − 7.0 ± 1.24 | 0.39 | − 7.892 | − 6.108 | ||
| 41–50 | − 3.58 ± 0.79 | 0.22 | − 4.087 | − 3.080 | ||
CAIT Cumberland Ankle Instability tool, LEFS lower extremity functional scale
Fig. 4.
CAIT and LEFS scores within different age groups. a CAIT scores, b LEFS scores. Pre- and post-training show significant differences in all groups. CAIT Cumberland Ankle Instability tool, LEFS lower extremity functional scale
Discussion
After interpreting the results of our present study, we found that 6 weeks of balance and strength training significantly improved proprioception, balance, stability, and self-reported functional outcomes in subjects suffering from CAI. With this in mind, the results suggest that the balance training protocol using wobble board and strength training protocol using Thera-bands increased ankle stability among subjects in different age groups.
Muscle receptors, which contribute significantly to ankle proprioception, support the sensory feedback on variations in muscle length, joint position sense, and speed of the movement. The central nervous system uses this information for planning and executing movement [33]. This evidence indicates that the tendency for CAI in ankle sprains is due to the decrease in proprioception caused by loss of sensory input; that loss of input is usually caused by interruption of peripheral sensory fibers during trauma to the ankle [34]. The sensory involvement of the tibial nerve undoubtedly contributes to the ankle joint position sense and motor control through stimulating the tibialis posterior, flexor hallucis longus and flexor digitorum muscles [35]. In the present study, we applied the balance exercises to subjects with CAI, thereby significantly improving ankle proprioception with results that agree with previous investigations [30]. For these reasons, proprioceptive training is a crucial component in rehabilitating subjects with CAI.
Researchers have identified a significant relationship between ankle muscle weakness and ankle instability [21, 36]. This muscle weakness may emanate from the disruption of the muscles’ nerve supply or selective inhibition of the invertor muscles’ capability to start affecting in the direction of the initial injury [36]. Therefore, investigators designed different strength training protocols for the ankle and reported that these exercises significantly improve joint stability [19–37]. With regard to static balance (eyes closed), both the current research and the study done by Mckeon et al. [23] reported similar development as the present study ranging from 1.69 to 4.46 s (P < 0.01). This impression shows that ankle strength is an important factor influencing the somatosensory regulation during standing position and balance through its effects on muscle and tendon receptors of the foot and ankle that include the plantar cutaneous receptors [38]. In the present study, results also indicate that ankle strengthening exercises increase the plantar flexion JPS score to 3.7° and inversion JPS to 3.53° (P < 0.01), which is similar to Docherty et al.’s study [19]. There are two possible sensory mechanisms that could have produced such change. Primarily, we believe the stimulation of joint mechanoreceptors during the exercise contributed to the change; the second mechanism is the neural adaptation to primary afferent (Ia, IIa) endings of muscle spindles [39].
Regarding equilibrium, the FRT is an important outcome measure for checking the dynamic balance and it has significant correlation with age, supporting the findings of our study [28]. Ha et al. [18] reported that ankle strengthening and proprioceptive training improves dynamic balance by about 1.60 cm in contrast to our current study where improvement was 5.85 cm and statistically significant (P < 0.01). We believe this development was mainly due to the combination of neural factors [40] and increase in concentric and eccentric muscle activity in subjects with CAI [29]. Indeed, we observed that rigorous ankle training protocols were highly effective for increasing balance ability.
In the present research, we also found even the eversion JPS and dorsiflexion JPS significantly improved after a 6-week strength training with Thera-bands; this is in direct contrast with previous studies [18, 19, 41]. Our study identified the eversion JPS increasing to 3.59° (P < 0.01), contradicting Lee et al. [41] which was saw 2.36°. Studies done by Docherty et al. [19] and Lee et al. [18] concluded that the dorsiflexion JPS had increased to 2.3° after training, seeing disparity with the present study which was 3.55° (P < 0.01). An important reason for this was that the subjects in our current study were trained five times a week instead of three times a week as in previous studies [31, 32] for a period of 6 weeks. We believe this protocol may be strenuous enough to bring a strength variation adaptation, especially in subjects with CAI. This may cause development in muscle function by decreasing motor unit recruitment thresholds and changing the motor neuron excitability [42], thus permitting for dynamic activation during different variations of ankle movement [43]. This finding may have considerable implications for clinical practice to implement the strength training to ankle musculature.
In relation to self-reported functional outcomes, the CAIT score increased by 27.3% (P < 0.01) which was dissimilar to Lee et al. [41] where it was 20% and Kim et al. [44] who reported 26.3%. Whereas in regard to LEFS, Bleakley et al. [45] showed a similar LEFS score improvement of 15.9% (8.86 points), which was significant (P < 0.01) and supports our findings in this study. This enhancement in the outcome measures indicates a significant increase in strength and proprioception in all groups associated with CAI.
To our knowledge, this is the first study that targets the effects of strengthening and proprioceptive training on balance, proprioception, and self-reported functional outcomes among subjects in different age groups. All the outcome measures in the present study were significant (P < 0.01) between all age groups, but the results in group 3 were comparatively less than the others. The proprioception showed a minimal increase of about 1° to 1.7° among middle-aged adults [46]. Indeed, numerous studies showed an increase in age decline proprioception at both peripheral and central levels [47] compared to young adults [12, 13]. At the peripheral level, both anatomical and physiological age-related fluctuations in muscle spindle decreased the dynamic response of the muscle spindle afferents to incline stretch. Structural changes involved a significant decrease in total number of intrafusal muscle fibers and nuclear chain fibers in the spindle, leading to increase the muscle spindle capsule thickness [47]. However, at the central level, aging affects the conductive function from the somatosensory pathways and thereby causes neurochemical changes in the brain [48]. Regarding balance, previous studies [49, 50] have suggested that elderly adults may compensate for decreased balance by improving the sensitivity of the central inputs, reducing the perceptual proprioceptive errors during balance control. The conclusions drawn from these studies advise that proprioception declines as age increases, which supports our findings in the current study.
Limitations of the Study
Although the present study elicited vital observations regarding the effectiveness of strengthening and proprioceptive training on CAI participants, there are some limitations for our research. The sample size here was too small to draw any fixed conclusions; so, there is a need for more studies with a large sample size. Additionally, in future research there should be comparison of different type of training protocols against conventional forms of rehabilitation. We also recommend that future clinical studies evaluate the effects of different lengths of training protocols with regards to improving the stability and self-reported functional outcomes for those with CAI in different age groups. This current study did not conduct a follow up of all the subjects after 6 weeks. We believe the assessment of clinical outcome measures and training protocols efficacy depends on reliable follow-up information if one is to enable critical appraisal.
Conclusion
Six weeks of progressive strengthening and proprioceptive training protocols significantly improved stability, proprioception, balance, and self-reported functional status in subjects with CAI in our current study. Including these protocols in a rehabilitation program could accelerate recovery from ankle sprains and prevent the development of CAI, thereby providing faster return to daily activities.
Acknowledgements
This research work was funded by a Grant (R.G.P1/167/41) from the King Khalid University, Abha, Saudi Arabia.
Author Contributions
KAA and VNK—responsible for the conception and design of study, acquisition and analysis of data. VNK, RSR and PS—drafted the article and approved the final manuscript after critical revision. JST, IA and KR—contributed towards acquisition of data. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This study involved participation of human subjects and recieved approval from Ethical Committee of King Khalid University (ECM #2019-08).
Informed consent
Informed consent was obtained from all participants.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gribble, P. A., Delahunt, E., Bleakley, C., Caulfield, B., Docherty, C., Fourchet, F., et al. (2013). Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the international ankle consortium. JOSPT, Inc. JOSPT, 1033 North Fairfax Street, Suite 304, Alexandria, VA
- 2.Kaufman KR, Brodine SK, Shaffer RA, Johnson CW, Cullison TR. The effect of foot structure and range of motion on musculoskeletal overuse injuries. The American Journal of Sports Medicine. 1999;27(5):585–593. doi: 10.1177/03635465990270050701. [DOI] [PubMed] [Google Scholar]
- 3.Kannus P, Renstrom P. Treatment for acute tears of the lateral ligaments of the ankle. Journal of Bone and Joint Surgery American Volume. 1991;73(2):305–312. [PubMed] [Google Scholar]
- 4.McCriskin BJ, Cameron KL, Orr JD, Waterman BR. Management and prevention of acute and chronic lateral ankle instability in athletic patient populations. World Journal of Orthopedics. 2015;6(2):161. doi: 10.5312/wjo.v6.i2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hertel J. Functional instability following lateral ankle sprain. Sports Medicine. 2000;29(5):361–371. doi: 10.2165/00007256-200029050-00005. [DOI] [PubMed] [Google Scholar]
- 6.McKeon PO, Hubbard TJ, Wikstrom EA. Consequences of ankle inversion trauma: A novel recognition and treatment paradigm. An international perspective on topics in sports medicine and sports injury. Rijeka: IntechOpen; 2012. [Google Scholar]
- 7.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. Journal of Athletic Training. 2002;37(4):364. [PMC free article] [PubMed] [Google Scholar]
- 8.Delahunt E, Coughlan GF, Caulfield B, Nightingale EJ, Lin C-WC, Hiller CE. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Medicine and Science in Sports and Exercise. 2010;42(11):2106–2121. doi: 10.1249/MSS.0b013e3181de7a8a. [DOI] [PubMed] [Google Scholar]
- 9.Zouita ABM, Majdoub O, Ferchichi H, Grandy K, Dziri C, Salah FB. The effect of 8-weeks proprioceptive exercise program in postural sway and isokinetic strength of ankle sprains of Tunisian athletes. Annals of Physical and Rehabilitation Medicine. 2013;56(9–10):634–643. doi: 10.1016/j.rehab.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Park S, Toole T, Lee S. Functional roles of the proprioceptive system in the control of goal-directed movement. Perceptual and Motor Skills. 1999;88(2):631–647. doi: 10.2466/pms.1999.88.2.631. [DOI] [PubMed] [Google Scholar]
- 11.Freeman M, Dean M, Hanham I. The etiology and prevention of functional instability of the foot. The Journal of bone and joint surgery British Volume. 1965;47(4):678–685. [PubMed] [Google Scholar]
- 12.Glencross D. Position sense following joint injury. Journal of Sports Medicine and Physical Fitness. 1981;21:23–27. [PubMed] [Google Scholar]
- 13.Skinner HB, Barrack RL, Cook SD. Age-related decline in proprioception. Clinical Orthopaedics and Related Research. 1984;184:208–211. [PubMed] [Google Scholar]
- 14.Di Giulio I, Maganaris CN, Baltzopoulos V, Loram ID. The proprioceptive and agonist roles of gastrocnemius, soleus and tibialis anterior muscles in maintaining human upright posture. The Journal of Physiology. 2009;587(10):2399–2416. doi: 10.1113/jphysiol.2009.168690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Röijezon U, Clark NC, Treleaven J. Proprioception in musculoskeletal rehabilitation. Part 1: Basic science and principles of assessment and clinical interventions. Manual Therapy. 2015;20(3):368–377. doi: 10.1016/j.math.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 16.McGuine TA, Keene JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. The American Journal of Sports Medicine. 2006;34(7):1103–1111. doi: 10.1177/0363546505284191. [DOI] [PubMed] [Google Scholar]
- 17.Janssen KW, Hendriks MR, van Mechelen W, Verhagen E. The cost-effectiveness of measures to prevent recurrent ankle sprains: Results of a 3-arm randomized controlled trial. The American Journal of Sports Medicine. 2014;42(7):1534–1541. doi: 10.1177/0363546514529642. [DOI] [PubMed] [Google Scholar]
- 18.Ha S-Y, Han J-H, Sung Y-H. Effects of ankle strengthening exercise program on an unstable supporting surface on proprioception and balance in adults with functional ankle instability. Journal of Exercise Rehabilitation. 2018;14(2):301. doi: 10.12965/jer.1836082.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Docherty CL, Moore JH, Arnold BL. Effects of strength training on strength development and joint position sense in functionally unstable ankles. Journal of Athletic Training. 1998;33(4):310. [PMC free article] [PubMed] [Google Scholar]
- 20.Uh BS, Beynnon BD, Helie BV, Alosa DM, Renstrom A. The benefit of a single-leg strength training program for the muscles around the untrained ankle: A prospective, randomized, controlled study. The American Journal of Sports Medicine. 2000;28(4):568–573. doi: 10.1177/03635465000280042101. [DOI] [PubMed] [Google Scholar]
- 21.Tropp H. Pronator muscle weakness in functional instability of the ankle joint. International Journal of Sports Medicine. 1986;7(05):291–294. doi: 10.1055/s-2008-1025777. [DOI] [PubMed] [Google Scholar]
- 22.Fitzgerald D, Trakarnratanakul N, Smyth B, Caulfield B. Effects of a wobble board-based therapeutic exergaming system for balance training on dynamic postural stability and intrinsic motivation levels. Journal of Orthopaedic and Sports Physical Therapy. 2010;40(1):11–19. doi: 10.2519/jospt.2010.3121. [DOI] [PubMed] [Google Scholar]
- 23.McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. Balance training improves function and postural control in those with chronic ankle instability. Medicine and Science in Sports and Exercise. 2008;40(10):1810–1819. doi: 10.1249/MSS.0b013e31817e0f92. [DOI] [PubMed] [Google Scholar]
- 24.Hiller CE, Refshauge KM, Herbert RD, Kilbreath SL. Intrinsic predictors of lateral ankle sprain in adolescent dancers: A prospective cohort study. Clinical Journal of Sport Medicine. 2008;18(1):44–48. doi: 10.1097/JSM.0b013e31815f2b35. [DOI] [PubMed] [Google Scholar]
- 25.Binkley JM, Stratford PW, Lott SA, Riddle DL, Network NAORR The Lower Extremity Functional Scale (LEFS): Scale development, measurement properties, and clinical application. Physical Therapy. 1999;79(4):371–383. [PubMed] [Google Scholar]
- 26.Witchalls J, Blanch P, Waddington G, Adams R. Intrinsic functional deficits associated with increased risk of ankle injuries: A systematic review with meta-analysis. British Journal of Sports Medicine. 2012;46(7):515–523. doi: 10.1136/bjsports-2011-090137. [DOI] [PubMed] [Google Scholar]
- 27.Baier M, Hopf T. Ankle orthoses effect on single-limb standing balance in athletes with functional ankle instability. Archives of physical Medicine and Rehabilitation. 1998;79(8):939–944. doi: 10.1016/s0003-9993(98)90091-0. [DOI] [PubMed] [Google Scholar]
- 28.Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: A new clinical measure of balance. Journal of Gerontology. 1990;45(6):M192–M197. doi: 10.1093/geronj/45.6.m192. [DOI] [PubMed] [Google Scholar]
- 29.Willems T, Witvrouw E, Verstuyft J, Vaes P, De Clercq D. Proprioception and muscle strength in subjects with a history of ankle sprains and chronic instability. Journal of Athletic Training. 2002;37(4):487. [PMC free article] [PubMed] [Google Scholar]
- 30.Wester JU, Jespersen SM, Nielsen KD, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: A prospective randomized study. Journal of Orthopaedic and Sports Physical Therapy. 1996;23(5):332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- 31.Thacker SB, Stroup DF, Branche CM, Gilchrist J, Goodman RA, Weitman EA. The prevention of ankle sprains in sports. The American Journal of Sports Medicine. 1999;27(6):753–760. doi: 10.1177/03635465990270061201. [DOI] [PubMed] [Google Scholar]
- 32.Kaminski T, Buckley B, Powers M, Hubbard T, Ortiz C. Effect of strength and proprioception training on eversion to inversion strength ratios in subjects with unilateral functional ankle instability. British Journal of Sports Medicine. 2003;37(5):410–415. doi: 10.1136/bjsm.37.5.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goble DJ, Coxon JP, Van Impe A, Geurts M, Van Hecke W, Sunaert S, et al. The neural basis of central proprioceptive processing in older versus younger adults: An important sensory role for right putamen. Human Brain Mapping. 2012;33(4):895–908. doi: 10.1002/hbm.21257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Refshauge KM, Kilbreath SL, Raymond J. The effect of recurrent ankle inversion sprain and taping on proprioception at the ankle. Medicine and Science in Sports and Exercise. 2000;32(1):10–15. doi: 10.1097/00005768-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Taira T, Hori T. The role of neurosurgical interventions for control of spasticity in neurorehabilitation: New findings on functional microanatomy of the tibial nerve. Neurosurgical re-engineering of the damaged brain and spinal cord. Berlin: Springer; 2003. pp. 103–105. [DOI] [PubMed] [Google Scholar]
- 36.Ryan L. Mechanical stability, muscle strength and proprioception in the functionally unstable ankle. Australian Journal of Physiotherapy. 1994;40(1):41–47. doi: 10.1016/S0004-9514(14)60453-0. [DOI] [PubMed] [Google Scholar]
- 37.Powers ME, Buckley BD, Kaminski TW, Hubbard TJ, Ortiz C. Six weeks of strength and proprioception training does not affect muscle fatigue and static balance in functional ankle instability. Journal of Sport Rehabilitation. 2004;13(3):201–227. [Google Scholar]
- 38.Jam B. Evaluation and retraining of the intrinsic foot muscles for pain syndromes related to abnormal control of pronation. Advanced Physical Therapy Education Institute. 2006;21:1–8. [Google Scholar]
- 39.Bongiovanni L, Hagbarth K. Tonic vibration reflexes elicited during fatigue from maximal voluntary contractions in man. The Journal of Physiology. 1990;423(1):1–14. doi: 10.1113/jphysiol.1990.sp018007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moritani T. Neural factors versus hypertrophy in the time course of muscle strength gain. American Journal of Physical Medicine. 1979;58(3):115–130. [PubMed] [Google Scholar]
- 41.Lee E, Cho J, Lee S. Short-foot exercise promotes quantitative somatosensory function in ankle instability: A randomized controlled trial. Medical Science Monitor: International Medical Journal of expErimental and Clinical Research. 2019;25:618. doi: 10.12659/MSM.912785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pollock RD, Woledge RC, Martin FC, Newham DJ. Effects of whole body vibration on motor unit recruitment and threshold. Journal of Applied Physiology. 2011;112(3):388–395. doi: 10.1152/japplphysiol.01223.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Torvinen S, Kannus P, Sievänen H, Järvinen TA, Pasanen M, Kontulainen S, et al. Effect of four-month vertical whole body vibration on performance and balance. Medicine and Science in Sports and Exercise. 2002;34(9):1523–1528. doi: 10.1097/00005768-200209000-00020. [DOI] [PubMed] [Google Scholar]
- 44.Kim K-J, Kim Y-E, Jun H-J, Lee J-S, Ji S-H, Ji S-G, et al. Which treatment is more effective for functional ankle instability: Strengthening or combined muscle strengthening and proprioceptive exercises? Journal of Physical Therapy Science. 2014;26(3):385–388. doi: 10.1589/jpts.26.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bleakley CM, O’Connor SR, Tully MA, Rocke LG, MacAuley DC, Bradbury I, et al. Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial. BMJ. 2010;340:c1964. doi: 10.1136/bmj.c1964. [DOI] [PubMed] [Google Scholar]
- 46.Robbins S, Waked E, McClaran J. Proprioception and stability: foot position awareness as a function of age and footware. Age and Ageing. 1995;24(1):67–72. doi: 10.1093/ageing/24.1.67. [DOI] [PubMed] [Google Scholar]
- 47.Miwa T, Miwa Y, Kanda K. Dynamic and static sensitivities of muscle spindle primary endings in aged rats to ramp stretch. Neuroscience Letters. 1995;201(2):179–182. doi: 10.1016/0304-3940(95)12165-x. [DOI] [PubMed] [Google Scholar]
- 48.Masliah E, Mallory M, Hansen L, DeTeresa R, Terry R. Quantitative synaptic alterations in the human neocortex during normal aging. Neurology. 1993;43(1 Part 1):192. doi: 10.1212/wnl.43.1_part_1.192. [DOI] [PubMed] [Google Scholar]
- 49.Horak FB, Shupert CL, Mirka A. Components of postural dyscontrol in the elderly: A review. Neurobiology of Aging. 1989;10(6):727–738. doi: 10.1016/0197-4580(89)90010-9. [DOI] [PubMed] [Google Scholar]
- 50.Stelmach GE, Sirica A. Aging and proprioception. Age. 1986;9(4):99–103. [Google Scholar]