Abstract
Background: COVID-19 not only threatened the public's physical health but also brought unbearable psychological pressure, especially for those vulnerable groups like the elderly. However, studies on the psychological status of older adults during this public health emergency remained scant. This study aims to investigate the mental health status among the elderly Chinese population during COVID-19 pandemic and determine the influencing factors of psychological symptoms.
Methods: From February 19 to March 19, 2020, an online survey was administered to Chinese older adults using a convenience sampling method. Information on demographic data, health status and other epidemic related factors were collected. Specifically, the study defined the psychological status as five primary disorder–depression, neurasthenia, fear, anxiety, and hypochondria–which were assessed by the Psychological Questionnaire for Emergent Event of Public Health (PQEEPH). Standard descriptive statistics and multiple logistic regression analyses were conducted to analyze the data.
Results: Of 1,501 participants recruited from 31 provinces in China, 1,278 were valid for further analysis. Participants' scores on each sub-scale were described in median and interquartile [M(Q)]: depression [0.00 (0.33)], neurasthenia [0.00 (0.40)], fear [1.00 (0.83)], anxiety [0.00 (0.17)], hypochondria [0.00 (0.50)]. Chronic diseases (depression p = 0.001; neurasthenia p < 0.001; fear p = 0.023; anxiety p < 0.001; hypochondria p = 0.001) and the BMI index (depression p = 0.015; neurasthenia p = 0.046; fear p = 0.016; anxiety p = 0.015; hypochondria p = 0.013) had significant impacts on all of the five sub-scales. Specifically, the rural dwellers had a higher level of neurasthenia, fear, and hypochondria. Besides, education level (p = 0.035) and outbreak risk level (p = 0.004) had significant impacts on the depression. Higher household monthly income per capita (p = 0.031), and the community-level entry/exit control (p = 0.011) are factors against anxiety.
Conclusions: Most elderly residents reported mild negative emotions during COVID-19 and more attention should be paid to the recognition and alleviation of fear. Our findings also identified factors associated with the mental health status of the elderly, which is of practical significance in the design and implementation of psychological interventions for this vulnerable population during COVID-19 and future emerging diseases.
Keywords: COVID-19, mental health, influencing factors, elderly, China
Introduction
In late December 2019, atypical pneumonia caused by a novel coronavirus (SARS-CoV-2) was found in Wuhan, capital of Hubei province, China, and the disease quickly spread all over China and several overseas regions. On January 30, 2020, the World Health Organization declared a Public Health Emergency of International Concern (PHEIC) over the global outbreak of the novel coronavirus and formally named the disease COVID-19 (1). Due to the strong infectivity and the quick transmission speed, On March 11, WHO has upgraded the outbreak of COVID-19 as a pandemic (2). China has witnessed a rapid increase of COVID-19 confirmed cases from 202 of January 20, 2020 to 74,283 of February 19, 2020. Daily new diagnosed cases began decreasing gradually after February 19, 2020 and the epidemic has been largely under control since May with sporadic cases occasionally occurred (3). However, the international situation is still not optimistic. As of February 28, 2021, the disease has affected 220 countries and regions, causing over 113 million confirmed cases and over 2.5 million deaths worldwide (4).
There has been mounting evidence showing that outbreaks of infection could deteriorate individuals' mental health (5–7), and COVID-19 is not an exception. The threat of COVID-19 on physical health, the overflow of media coverage on COVID-19, and the unprecedented large-scale epidemic control measures taken by the Chinese government to curb the spread of COVID-19 (8), such as lockdown of the Wuhan city, strict management of working and living spaces, closure of schools and non-essential businesses, etc., all induced a considerable degree of negative emotions among the public (9–11).
Older adults are significantly more prone to infection, severe illness, and death of COVID-19 (12–14), besides, their daily routines can also be greatly affected by the epidemic and the control measures due to lack of knowledge on advanced technology, major impacts include drastically reduced social activities and contact with relatives and friends, and difficulty in getting basic living amenities or medical treatments (15). These put them at a greater risk of developing several mental disorders, such as panic (16), fear (17), depression (18), and anxiety (19). Historical researches during SARS have also found that the elderly population experienced more severe psychiatric symptoms (20), worse subjective well-being (21), and higher suicide deaths (22). Both China and the rest of the world are witnessing an ever-increasing elderly population. By the end of 2017, the number of people aged over 60 in China had already reached 241 million, accounting for 17.3% of China's total population (23). The prevalence of depressive symptoms in Chinese older adults reached 23.6% even in a normal period (24), and the situation could be worse during this unprecedented pandemic. Inferior psychological status can also be related to irrational behaviors (25), impeding the containment of the epidemic. Therefore, greater attention should be paid to the mitigation of older adults' negative emotions during COVID-19.
Although the Chinese government has launched a series of notifications to initiate a brunch of online psychological intervention programs to help the public deal with the urgent psychological crisis (26, 27), these online programs can hardly be utilized by older adults due to limited access to internet services and smartphones (28). Thus, more efforts should be made to design targeted psychological intervention strategies for the elderly, and understanding their psychological status during the epidemic and the influencing factors would be the first step.
However, among the copious amount of empirical studies that focus on the mental health of the general population (29), medical staff (30), patients (31), college students (32), and adolescents (33) during the outbreak of COVID-19, studies on the specific mental situation of the elderly population under the pandemic can hardly be found. Therefore, this study aimed to assess the psychological status among the elderly Chinese population during COVID-19 pandemic by quantifying their degree of depression, neurasthenia, fear, anxiety, and hypochondria and to analyze the potential risk factors associated with these symptoms.
Methods
Study Design and Participants
This web-based cross-sectional survey was conducted from February 19, 2020 to March 19, 2020, during which COVID-19 cumulative confirmed cases steadily increased and community-wide COVID-19 prevention activities were launched by local health authorities. We uploaded the electronic questionnaire onto the online survey platform, “Wenjuanxing.” We spread the links or “QR” codes nationwide to elderly people (age ≥ 60 years old) via popular social media platforms like “WeChat.” Participants with serious cognitive impairment and those who were confirmed or suspected COVID-19 cases were excluded. Returned surveys with incomplete information or logic problems were deemed as invalid. Responses from a total of 1,501 participants were received, 197 of which were invalid cases, together with 26 participants who reported having never heard about COVID-19, resulting in an effective sample size of 1,278 participants.
Measurements
Dependent Variable
Psychological status was measured by the Psychological Questionnaire for Emergent Event of Public Health (PQEEPH) (34). This scale has been widely used to investigate individuals' psychological status during public health emergencies (35–37), adequate psychometric properties have been described and a Cronbach's alpha coefficient value of 0.92 was found in this study. The PQEEPH consists of 25 items and assesses 5 dimensions: depression, neurasthenia, fear, anxiety, and hypochondria. All items are rated on a four-point scale ranging from 0 (occasionally) to 3 (always). The total score value for each sub-scale ranging from 0 to 3 can be obtained by summing up scores of each item of a certain sub-scale and then divide the total score by the number of items in that sub-scale. Higher scores correspond to greater psychological symptoms. For each sub-scale, a score higher than the mean score plus one deviation was considered as the cut-off point for higher risk of mental health problem (35) and coded as “1.” In comparison, lower scores were coded as “0.”
Independent Variable
Gender, age, education level, household register, marital status, living condition, employment status, occupation, and monthly household income per capita were included as demographic variables.
Status of chronic diseases and the BMI index were included as health-related factors. Participants were asked to state any history of chronic diseases, and their height and weight were self-reported to calculate the BMI index. Status of Chronic diseases was grouped as no chronic disease, one chronic disease and two or more chronic diseases. The BMI index was categorized as underweight (<18.5), normal (18.5–24) and overweight (≥24).
Environmental control variables included local community-level control measures and outbreak risk level of current location. Respondents were asked to report their current addresses at the district level and community-level control measures in their residential areas, which was classified as free entry/exit as usual, entry/exit control exercised, and lockdown. The outbreak risk level of respondents' current residential provinces was categorized into three levels according to cumulative confirmed COVID-19 cases, provinces with <100 cumulative confirmed cases, 100–1,000 cases, and over 1,000 cases were rated as low, medium, and high-risk areas, respectively.
Respondents were also asked to choose the source they obtained COVID-19 information from internet media platforms, traditional media like TV or newspaper, relatives or friends, and other sources.
Statistical Analysis
Descriptive analysis was used to summarize the respondents' characteristics and psychological status. Frequencies (n) and percentage (%) were used to present categorical variables, while median and interquartile [M(Q)] and means and standard deviation (Mean ± SD) were used to present continuous variables. A univariate analysis (Chi-square test) was used to explore the significant associations between background variables and psychological symptoms. Multiple logistic regression models using scores of each sub-scale as outcome variables and statistically significant background variables as independent variables were built to identify factors associated with each of the five sub-scales. Odds ratios (OR) and the corresponding 95% confidence intervals (CIs) were reported. All the tests were two- sided, with a statistical significance level set at p < 0.05. Data were analyzed by IBM SPSS Version 19.0 (IBM Corp, 2010, Armonk, NY, USA).
Ethics Statement
The protocol was approved by Ethics Committee of School of Public Health, Zhejiang University (approval number: ZGL202002-2). This study is anonymous and voluntary, and the respondents were informed that submission of the questionnaire implied informed consent. The data were kept confidential and the results did not identify the respondents personally.
Results
Study Sample Characteristics
Table 1 demonstrates the characteristics of the study sample. Of the 1,278 participants, over half of the sample were female (n = 707, 55.3%), and 725 (56.7%) participants were aged 70 and below. For education level, a total of 588 (46.0%) participants had attended primary school or below. 690 (54.0%) respondents had registered permanent residences in rural areas. In addition, approximately three-fourths were married or in a cohabitation situation (n = 954, 74.6%), and most of the participants (n = 903, 70.7%) lived with their spouses. The majority of the participants (n = 1,209, 94.6%) had retired from work. As for occupations, 608 (47.6%) participants were farmers, and only 33 (2.6%) participants worked in medical health institutions. Most (n = 852, 66.7%) of the respondents had an average household income between 600 and 6,000 yuan per month. A total of 514 (40.2%) participants had two or more chronic diseases, and 426 (33.3%) participants were overweight. Nearly half of the participants (n = 588, 46.0%) lived in areas with a medium-risk of COVID-19. The majority (n = 1,061, 83.0%) reported that an entry/exit control system was exercised in their community/village. A small proportion of the participants (n = 247, 19.3%) had obtained information about COVID-19 from Internet media platforms like WeChat. Traditional media channels, such as newspapers and television, remained the most widely used way to obtain information among the elderly (n = 572, 44.8%).
Table 1.
Study sample characteristics (N = 1,278).
| Variables | n | % |
|---|---|---|
| Gender | ||
| Male | 571 | 44.7 |
| Female | 707 | 55.3 |
| Age | ||
| ≤ 70 | 725 | 56.7 |
| 70–80 | 459 | 35.9 |
| >80 | 94 | 7.4 |
| Education | ||
| Primary school and below | 588 | 46.0 |
| Middle school | 333 | 26.1 |
| High school | 202 | 15.8 |
| Junior college | 75 | 5.9 |
| Bachelor's degree and above | 80 | 6.3 |
| Residence | ||
| Urban | 588 | 46.0 |
| Rural | 690 | 54.0 |
| Living condition | ||
| Living alone | 122 | 9.5 |
| Living with spouse | 903 | 70.7 |
| Living with children | 232 | 18.2 |
| Living in nursing house with others | 21 | 1.6 |
| Marital status | ||
| Married/co-habited | 954 | 74.6 |
| Others | 324 | 25.4 |
| Employment status | ||
| Retired | 1,209 | 94.6 |
| Employed | 69 | 5.4 |
| Occupation | ||
| Health care worker | 33 | 2.6 |
| Civil servant | 57 | 4.5 |
| Workers in enterprises and institutions | 458 | 35.8 |
| Farmer | 608 | 47.6 |
| Others | 122 | 9.5 |
| Household monthly income per person (Yuan) | ||
| <600 | 221 | 17.3 |
| 600–6,000 | 852 | 66.7 |
| >6,000 | 205 | 16.0 |
| BMIa | ||
| Normal | 744 | 58.2 |
| Underweight | 107 | 8.4 |
| Overweight | 426 | 33.3 |
| Chronic diseases | ||
| No chronic disease | 264 | 20.7 |
| One chronic disease | 500 | 39.1 |
| Two or more chronic diseases | 514 | 40.2 |
| Outbreak risk level of current locationb | ||
| Low | 157 | 12.3 |
| Medium | 588 | 46.0 |
| High | 533 | 41.7 |
| Local community-level control measures | ||
| Free entry/exit as usual | 34 | 2.7 |
| Entry/exit control exercised | 1,061 | 83.0 |
| Lockdown | 183 | 14.3 |
| Source of information | ||
| Internet media platforms | 247 | 19.3 |
| Newspaper and TV | 572 | 44.8 |
| Relatives or friends | 406 | 31.8 |
| Others | 53 | 4.1 |
The BMI index has 1 missing value.
According to authorized data from National Health Commission (accessed on March 20, 2020), the study classified 31 provinces (cities, autonomous regions) with cumulative confirmed cases <100, 100–999, and ≥1,000 as low, medium and high risk areas.
The Mental Health of the Participants During the Pandemic
As shown in Table 2, the participants reported relatively good mental health, with scores on most sub-scales of the PQEEPH <1. The median score on the fear scale reached 1.00, significantly higher than that of the other four scales (the Friedman test χ2 = 2,613.495, p < 0.001). Participants with higher risk of mental health problem on depression, neurasthenia, fear, anxiety, hypochondria were 13.8% (n = 177), 14.9% (n = 190), 14.7% (n = 188), 10.0% (n = 128), 11.9% (n = 152), respectively.
Table 2.
Psychological status of Chinese elderly (N = 1,278).
| Psychological dimensions | Score range | Scores M (Q) | Scores (Mean ± SD)a | Higher risk of mental health problem, n (%) |
|---|---|---|---|---|
| Depression | 0–3 | 0.00 (0.33) | 0.27 ± 0.48 | 177 (13.8) |
| Neurasthenia | 0–3 | 0.00 (0.40) | 0.28 ± 0.45 | 190 (14.9) |
| Fear | 0–3 | 1.00 (0.83) | 0.99 ± 0.59 | 188 (14.7) |
| Anxiety | 0–3 | 0.00 (0.17) | 0.18 ± 0.35 | 128 (10.0) |
| Hypochondria | 0–3 | 0.00 (0.50) | 0.24 ± 0.46 | 152 (11.9) |
A score higher than mean score plus one deviation of each sub-scale is defined as the cut-off point.
Univariate Analysis of Participants' Characteristics With the Scores of the Five Sub-scales of the PQEEPH
As shown in Table 3, significant correlates of depression were marital status, education level, residence registration, employment status, occupation, monthly household income per capita, outbreak risk level of the current location, local community-level control measures, the BMI index, and chronic diseases (all p < 0.05). Significant correlates of anxiety were marital status, residence registration, living conditions, household monthly income per capita, local community-level control measures, source of COVID-19 information, the BMI index, and chronic diseases (all p < 0.05). Related factors of neurasthenia were residence registration, employment status, the BMI index, chronic diseases, and outbreak risk level of the current location (all p < 0.05). Correlates of fear and hypochondria were residence registration, employment status, the BMI index, and chronic diseases (all p < 0.05).
Table 3.
Univariate analysis of participants' characteristics with the scores of the five sub-scales of the PQEEPH (N = 1,278)a.
| Variables | Depression (N = 177) | Neurasthenia (N = 190) | Fear (N = 188) | Anxiety (N = 128) | Hypochondria (N = 152) |
|---|---|---|---|---|---|
| P-value (χ2) | P-value (χ2) | P-value (χ2) | P-value (χ2) | P-value (χ2) | |
| Gender | 0.423 (0.642) | 0.419 (0.653) | 0.153 (2.042) | 0.276 (1.186) | 0.717 (0.132) |
| Age | 0.096 (4.691) | 0.070 (5.323) | 0.451 (1.593) | 0.197 (3.251) | 0.266 (2.647) |
| Education | 0.002 (17.458) | 0.107 (7.621) | 0.063 (8.910) | 0.183 (6.222) | 0.375 (4.237) |
| Residence | 0.003 (8.974) | 0.001 (10.375) | 0.001 (11.603) | 0.016 (5.809) | <0.001 (15.811) |
| Living condition | 0.061 (7.140)d | 0.210 (4.469)d | 0.742 (1.266)d | 0.016 (10.020)d | 0.578 (1.899)d |
| Marital status | 0.024 (5.096) | 0.050 (3.832) | 0.808 (0.059) | 0.024 (5.106) | 0.278 (1.178) |
| Employment status | 0.046 (3.964) | 0.012 (6.377) | 0.032 (4.619) | 0.431 (0.621) | 0.006 (7.593) |
| Occupation | 0.004 (15.221)d | 0.137 (6.889)d | 0.251 (5.307)d | 0.161 (6.417)d | 0.156 (6.553)d |
| Household monthly income per person (Yuan) | 0.011 (9.064) | 0.376 (1.955) | 0.059 (5.655) | 0.004 (10.896) | 0.265 (2.656) |
| BMIb | 0.010 (9.173) | 0.006 (10.217) | 0.002 (13.000) | 0.009 (9.339) | 0.042 (6.341) |
| Chronic diseases | <0.001 (25.123) | <0.001 (28.438) | 0.004 (10.930) | <0.001 (26.086) | <0.001 (19.157) |
| Outbreak risk level of current locationc | <0.001 (20.709) | 0.030 (6.981) | 0.569 (1.129) | 0.696 (0.724) | 0.426 (1.707) |
| Local community-level control measure | 0.051 (5.987)d | 0.183 (3.399) | 0.122 (4.210) | 0.018 (7.708)d | 0.532 (1.239)d |
| Source of information | 0.373 (3.121) | 0.661 (1.592) | 0.180 (4.894) | 0.033 (8.722) | 0.509 (2.317) |
Values were calculated from Chi-Square Test to examine the differences of scores of each sub-scale between populations with different characteristics. Significant P values are printed in bold. The complete univariate analysis form including different groups of all variables is attached in the Supplementary Table 1.
The BMI index has 1 missing value.
According to authorized data from National Health Commission (accessed on March 20, 2020), the study classified 31 provinces (cities, autonomous regions) with cumulative confirmed cases <100, 100–999, and ≥1,000 as low, medium and high risk areas.
1 cell has expected count <5, the Fisher's exact test was used.
Factors Associated With Scores of the Five Sub-scales of the PQEEPH: A Multivariable Analysis
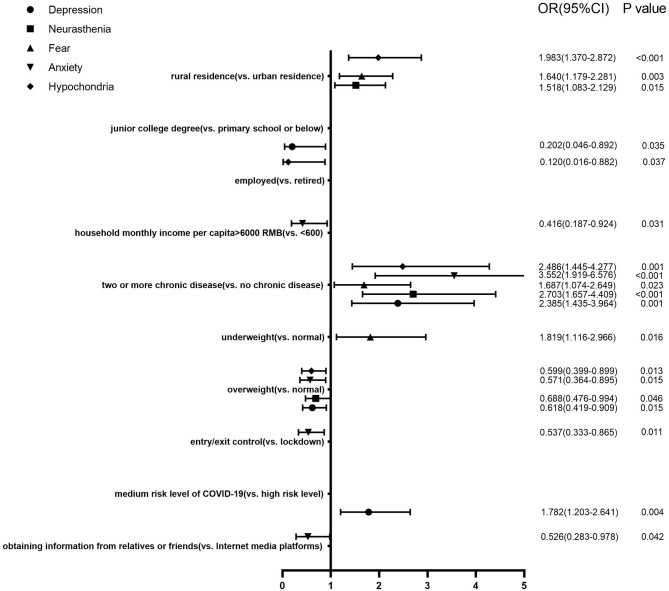
The multiple logistic regression models of scores of the five sub-scales of the PQEEPH (Figure 1) showed that health-related factors had the greatest impact on mental health. Respondents who had two or more chronic diseases were more likely to develop mental problems on all of the five sub-scales. As for the BMI index, those who were underweight experienced more fear, while being overweight was related to positive mental outcomes on the scale of depression, neurasthenia, anxiety, and hypochondria. Rural dwellers had higher levels of neurasthenia, fear, and hypochondria. The respondents with an education level of junior college (vs. primary school or below, OR = 0.202, 95%CI = 0.046–0.892) were less likely to be depressed, while those who lived in medium-risk regions (vs. high- risk region, OR = 1.782, 95%CI = 1.203–2.641) had higher risk of depression. An average household income higher than 6,000 Yuan per month (vs. <600 Yuan, OR = 0.416, 95%CI = 0.187–0.924), community-level entry/exit control (vs. cannot leave the house, OR = 0.537, 95%CI = 0.333–0.865), obtaining COVID-19 related information from relatives or friends (vs. Internet media platforms, OR = 0.526, 95%CI = 0.283–0.978) were protective factors against anxiety. Being employed (vs. retired, OR = 0.120, 95%CI = 0.016–0.882) helped reduce the risk of hypochondria.
Figure 1.
Factors associated with scores of the five sub-scales of the PQEEPH: a multivariable analysis (N = 1,278).
Discussion
The elderly in this study reported mild mental problems with median scores on all five sub-scales of the PQEEPH being ≤ 1, and significantly more symptoms of fear were reported. This finding was consistent with similar studies using the same instrument during SARS, human H7N9 avian influenza, and COVID-19 (35–37), indicating that fear is the most common and serious negative emotion during a public health emergency. More attention should, therefore, be paid to the recognition and mitigation of fear.
The logistic regression analyses showed that health-related factors had the greatest influence on mental status. Participants with two or more chronic diseases showed more symptoms on all of the five sub-scales of the PQEEPH. The elderly, especially those with underlying chronic diseases, are at higher risk of contracting COVID-19 and could suffer from more severe and even fatal symptoms once infected (38). Additionally, people with chronic diseases could have difficulty obtaining maintenance treatments during COVID-19 due to strict epidemic control measures. More efforts should be done to promote the elderly with chronic diseases to uptake prevention behaviors, meanwhile, convenient and safe way of obtaining medical treatments during the epidemic should be provided for the elderly in need. Consistent with previous studies (39–41), underweight people reported poorer mental health. Overweight, however, was unexpectedly related to better mental states on four sub-scales. Lockdown during the pandemic has confined people to very limited spaces and impeded participation of physical exercise (42), but overweight people could be psychologically less affected as they participated less in physical activities (43). Another possible explanation is that overweight people had a poorer health awareness (44) and thereby suffered less psychological burden of the epidemic.
Several demographic factors, including residence registration, education level, employment status, and household monthly income per capita, were found to influence the five dimensions of the PQEEPH differently. Compared with those living in urban areas, rural dwellers expressed more neurasthenia, fear, and hypochondria. Although urban areas had more confirmed cases, medical resources and sanitary conditions in cities are better than in towns and villages, which increases the chances of surviving the virus (45). Besides, cities have better educational resources, and greater efforts have been made to publicize knowledge of epidemic prevention measures, which could alleviate the public's negative emotions (46). Therefore, COVID-19 related health education programs should be strengthened among rural dwellers to mitigate risk of infection. Adequate epidemic protective equipment should also be guaranteed for them and health care systems in rural areas should be further enhanced in the long term.
Participants with a junior college education level were at significantly lower risk of getting depressed than those who only attended primary school and below, which is similar with previous findings (24, 47). The elderly with a lower degree of education were less capable of getting access to and comprehending accurate information and facts regarding COVID-19, such as hygiene and precautionary measures. Health education on COVID-19 should thus pay more attention to this group using more acceptable forms like pictures or videos (48). Although those who were still at work may be at higher risk of exposure to the virus, being employed was surprisingly found to be associated with lower level of hypochondria. Actually, to prevent the spread of the virus, only those factories which passed strict examinations can be approved to reopen (49), therefore the contact with colleagues at work may not trigger panic. Besides, those who were still at work can be less likely to develop hypochondria symptoms as they could have better physical health (50) and working can help provide distraction from various worries (51), the mediation analysis also showed that the influence of employment status on hypochondria symptoms was partially mediated by health status (indirect effect = −0.063, p < 0.001) (see Supplementary Table 2). In line with previous studies (45, 52), the elderly with low average household incomes experienced more anxiety. Special social security measures could be established to help fight the economic challenges.
Other than demographic and health-related factors, environmental control variables were also significantly associated with certain sub-scale. Consistent with previous studies reporting that epidemic control measures like quarantine can have serious impacts on mental health (11, 53, 54), the elderly in our study who could not leave their house showed higher levels of anxiety than those who lived in communities where entry/exit controls were exercised. Against the backdrop of lockdown, offline social activities were inaccessible due to strict epidemic control measures (55, 56), while online interaction could also hardly be utilized by the elderly due to limited access and literacy in digital resources (57). The significantly reduced contact with family members and friends generated social and psychological isolation, triggering psychiatric disorders. Besides, the difficulty in obtaining basic living needs during lockdown could further exacerbate older adults' negative emotions of anxiety (15). However, it should also be noted that epidemic control measures play an important role in containing infectious diseases (58). Those in communities with no control measures also did not show a significantly lower level of anxiety. Therefore, community-level control measures are still necessary before the epidemic comes to the end, and close attention should be paid to the psychological state of those under strict epidemic control measures at the same time to recognize and address psychological problems in time. In contrast to previous studies reporting that people in most affected areas had significantly more negative emotions (9, 52), the elderly in our study who lived in regions with medium- risk levels of COVID-19 showed higher level of depression than those in high-risk regions. Those in high- risk areas were more motivated and had more access to gain knowledge on COVID-19, and a better understanding of the epidemic status can reduce the risk of developing negative emotions (59). High quality medical resources, strict and effective prevention measures as well as the strengthened public health systems in high- risk regions can also help alleviate psychological distress levels (16). Less than one-fifth of our participants obtained COVID-19 related information from Internet media platforms, and they expressed more anxiety than those who acquired information on COVID-19 from relatives or friends. There exist disparities in older adults' access to and knowledge on advanced technologies, and it would also be more difficult for them to distinguish accurate facts from fake information. Instead, family members are the core component of the social support network for the elderly (60). Apart from informing the elderly of important messages on COVID-19, relatives also conveyed spiritual comfort for the elderly, mitigating their anxiety over the pandemic. Therefore, there is a need to enhance family support to outreach COVID-19 information and promote preventive measures for the elderly during the epidemic.
Several limitations of this study should be stated. First, these findings' generalizability is limited, as the online survey only included those who had access to the Internet. However, online surveys can be the most appropriate method for data collection during an epidemic since it can avoid transmission and the distribution of the survey offline was not feasible under strict epidemic control measures. Second, this study's cross-sectional design prevented us from drawing causal associations. Third, the self-reported psychological status may not always be aligned with professional assessment, and recall and social desirability bias may also exist. Besides, despite that the PQEEPH can better reveal epidemic-specific emotions, comparison between older adults' mental health status in our study and that during non-epidemic periods can be restricted as the scale is epidemic-specific. While during epidemics, little attention has been paid to mental health among the elderly. Moreover, some important factors, such as contact history, relatives/friends who have contracted COVID-19, social support, and existing mental health problems, should be included in future studies. Notwithstanding all the above limitations, this study is one of the few studies investigating the psychological status of older adults in China during COVID-19. A large number of respondents from all the provinces in mainland China were recruited, enabling us to obtain a wide range of participants with various demographic backgrounds. Therefore, these findings provide important information for developing psychological interventions to alleviate negative emotions among the elderly during the outbreak of COVID-19.
Conclusion
The elderly, who are at higher risk of getting affected both physically and psychologically during the COVID-19, deserve particular attention from local governments, health authorities as well as the civil society. This study explored Chinese elderly residents' mental health status during COVID-19 and relevant factors. The elderly in our study had mild degree of negative emotions but reported significantly more fear symptoms, suggesting that psychological interventions should give more attention to recognize and alleviate fear. Health condition showed the greatest impact on mental health, more attention should thus be paid to older adults with poorer physical health. Higher education level, better economic condition, and obtaining COVID-19 information from friends or relatives were associated with lower risk of mental health problems, while rural dwellers and those lived in medium risk or lockdown regions experienced significantly more symptoms. These findings can be used to formulate psychological interventions to improve the mental health and psychological resilience of the elderly during the COVID-19 epidemic.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
HW and ZC conceived and designed the study. YC and BC assisted in questionnaire design and data collection. HC, YL, and HZ assisted in data collection. RZ and HC contributed to the statistical analysis and drafted the manuscript. LZ participated in statistical analysis. HW, RZ, and HC finalized the manuscript. All authors have read and agreed to the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors are grateful to all the survey participants.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.645938/full#supplementary-material
References
- 1.World Health Organization . 2019-nCoV Outbreak is an Emergency of International Concern. (2020). Available from: http://www.euro.who.int/en/health-topics/emergencies/pages/news/news/2020/01/2019-ncov-outbreak-is-an-emergency-of-international-concern (accessed January 31,2020).
- 2.World Health Organization . WHO Director-General's Opening Remarks at the Media Briefing on COVID-19 - 20 March 2020. (2020). Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19 (accessed March 11, 2020).
- 3.World Health Organization . WHO Coronavirus Disease (COVID-19) Dashboard. (2021). Available from: https://covid19.who.int/table (accessed March 3, 2021).
- 4.World Health Organization . Weekly Epidemiological Update - 2 March 2021. (2021). Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update–2-march-2021 (accessed March 3,2021).
- 5.Peng EY-C, Lee M-B, Tsai S-T, Yang C-C, Morisky DE, Tsai L-T, et al. Population-based post-crisis psychological distress: an example from the SARS outbreak in Taiwan. J Formosan Med Assoc. (2010) 109:524–32. 10.1016/S0929-6646(10)60087-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Bortel T, Basnayake A, Wurie F, Jambai M, Koroma AS, Muana AT, et al. Psychosocial effects of an Ebola outbreak at individual, community and international levels. Bull World Health Organ. (2016) 94:210–4. 10.2471/BLT.15.158543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bults M, Beaujean D, de Zwart O, Kok G, van Empelen P, van Steenbergen JE, et al. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: results of three consecutive online surveys. BMC Public Health. (2011) 11:13. 10.1186/1471-2458-11-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peng FJ, Tu L, Yang YS, Hu P, Wang RS, Hu QY, et al. Management and treatment of COVID-19: the Chinese experience. Can J Cardiol. (2020) 36:915–30. 10.1016/j.cjca.2020.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang HY, Ma JJ. How an epidemic outbreak impacts happiness: factors that Worsen (vs. protect) emotional well-being during the Coronavirus Pandemic. Psychiatry Res. (2020) 289:113045. 10.1016/j.psychres.2020.113045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Su Z, McDonnell D, Wen J, Kozak M, Abbas J, Segalo S, et al. Mental health consequences of COVID-19 media coverage: the need for effective crisis communication practices. Glob Health. (2021) 17:4. 10.1186/s12992-020-00654-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Losada-Baltar A, Jimenez-Gonzalo L, Gallego-Alberto L, Pedroso-Chaparro MDS, Fernandes-Pires J, Marquez-Gonzalez M. “We're staying at home”. Association of self-perceptions of aging, personal and family resources and loneliness with psychological distress during the lock-down period of COVID-19. J Gerontol B Psychol Sci Soc Sci. (2021) 76:e10–6. 10.1093/geronb/gbaa048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 395:1054–62. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. (2020) 55:105924. 10.1016/j.ijantimicag.2020.105924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Banerjee D. 'Age and ageism in COVID-19': Elderly mental health-care vulnerabilities and needs. Asian J Psychiatr. (2020) 51:102154. 10.1016/j.ajp.2020.102154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. (2020) 33:e100213. 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Satici B, Saricali M, Satici SA, Griffiths MD. Intolerance of uncertainty and mental wellbeing: serial mediation by rumination and fear of COVID-19. Int J Ment Health Addict. (2020) 1–12. 10.1007/s11469-020-00305-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou S-J, Zhang L-G, Wang L-L, Guo Z-C, Wang J-Q, Chen J-C, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. (2020) 29:749–58. 10.1007/s00787-020-01541-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meng H, Xu Y, Dai J, Zhang Y, Liu B, Yang H. Analyze the psychological impact of COVID-19 among the elderly population in China and make corresponding suggestions. Psychiatry Res. (2020) 289:112983. 10.1016/j.psychres.2020.112983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee TM, Chi I, Chung LW, Chou KL. Ageing and psychological response during the post-SARS period. Aging Ment Health. (2006) 10:303–11. 10.1080/13607860600638545 [DOI] [PubMed] [Google Scholar]
- 21.Lau AL, Chi I, Cummins RA, Lee TM, Chou KL, Chung LW. The SARS (Severe Acute Respiratory Syndrome) pandemic in Hong Kong: effects on the subjective wellbeing of elderly and younger people. Aging Ment Health. (2008) 12:746–60. 10.1080/13607860802380607 [DOI] [PubMed] [Google Scholar]
- 22.Yip PSF, Cheung YT, Chau PH, Law YW. The impact of epidemic outbreak the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis. (2010) 31:86–92. 10.1027/0227-5910/a000015 [DOI] [PubMed] [Google Scholar]
- 23.Liu YL. China's Aging Population: From a Global Perspective. Beijing: Social Sciences Acadeimc Press; (2019). [Google Scholar]
- 24.Li D, Zhang DJ, Shao JJ, Qi XD, Tian L. A meta-analysis of the prevalence of depressive symptoms in Chinese older adults. Arch Gerontol Geriatr. (2014) 58:1–9. 10.1016/j.archger.2013.07.016 [DOI] [PubMed] [Google Scholar]
- 25.Li LJ, Zhang D, Wu XM. Progress on collective behavior in emergency pubfic health events. J Chin J Health Educ. (2014) 30:631–3. 10.16168/j.cnki.issn.1002-9982.2014.07.026 [DOI] [Google Scholar]
- 26.National Health Commission of the People's Republic of China . Notice on the Issuance of Guidelines for Emergency Psychological Crisis Intervention in the Pneumonia Epidemic of New Coronavirus Infection. (2020). Available from: http://www.nhc.gov.cn/jkj/s3577/202001/6adc08b966594253b2b791be5c3b9467.shtml (accessed January 27, 2020).
- 27.National Health Commission of the People's Republic of China . Notice on the Issuance of Guidelines for the Psychological Assistance Hotline During the Prevention and Control of the New Coronavirus Pneumonia Epidemic. (2020). Available from: http://www.nhc.gov.cn/jkj/s3577/202002/f389f20cc1174b21b981ea2919beb8b0.shtml (accessed February 27, 2020).
- 28.Yang Y, Li W, Zhang Q, Zhang L, Cheung T, Xiang Y-T. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e19. 10.1016/S2215-0366(20)30079-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. (2020) 288:112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu K, Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med Sci Monit Basic Res. (2020) 26:e924085. 10.12659/MSMBR.924085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wei N, Huang BC, Lu SJ, Hu JB, Zhou XY, Hu CC, et al. Efficacy of internet-based integrated intervention on depression and anxiety symptoms in patients with COVID-19. J Zhejiang Univ Sci B. (2020) 21:400–4. 10.1631/jzus.B2010013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu J, Zhu Q, Fan WL, Makamure J, Zheng CS, Wang J. Online mental health survey in a Medical College in China during the COVID-19 outbreak. Front Psychiatry. (2020) 11:6. 10.3389/fpsyt.2020.00459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Commodari E, La Rosa VL. Adolescents in quarantine during COVID-19 pandemic in Italy: perceived health risk, beliefs, psychological experiences and expectations for the future. Front Psychol. (2020) 11:559951. 10.3389/fpsyg.2020.559951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gao Y, Xu MZ, Yang YF, Yao KN. Discussion on the coping style of undergraduates and the correlative factors during the epidemic period of SARS. Chin Med Ethics. (2004) 17:60–3. 10.3969/j.issn.1001-8565.2004.02.028 [DOI] [Google Scholar]
- 35.Gao Y, Yang YF, Ma YS, Yao KN. Research on the status of emotion response in college students during the epidemic period of SARS. Chin J Behav Med Sci. (2004) 13:658–60. 10.3760/cma.j.issn.1674-6554.2004.06.029 [DOI] [Google Scholar]
- 36.Zhang RJ, Jiang TT, Li N, Wang Z, Liu BY, Fang L, et al. The negative psychology for the public in Zhejiang province during the epidemic of human H7N9 avian influenza. Chin J Prev Med. (2015) 49:1073–9. 10.3760/cma.j.issn.0253-9624.2015.12.011 [DOI] [PubMed] [Google Scholar]
- 37.Wang XZ. Survey and analysis of public mentality in COVID-19 epidemic. J Yibin Univ. (2020) 20:15–20. 10.19504/j.cnki.issn1671-5365.2020.04.004 [DOI] [Google Scholar]
- 38.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. (2020) 395:507–13. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ul-Haq Z, Mackay DF, Fenwick E, Pell JP. Association between body mass index and mental health among Scottish adult population: a cross-sectional study of 37,272 participants. Psychol Med. (2014) 44:2231–40. 10.1017/S0033291713002833 [DOI] [PubMed] [Google Scholar]
- 40.McHiza ZJ-R, Parker W-A, Hossin MZ, Heshmati A, Labadarios D, Falkstedt D, et al. Social and psychological predictors of body mass index among South Africans 15 years and older: SANHANES-1. Int J Environ Res Public Health. (2019) 16:3919. 10.3390/ijerph16203919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sugai T, Suzuki Y, Yamazaki M, Shimoda K, Mori T, Ozeki Y, et al. High prevalence of underweight and undernutrition in Japanese inpatients with schizophrenia: a nationwide survey. BMJ Open. (2015) 5:e008720. 10.1136/bmjopen-2015-008720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Robinson E, Boyland E, Chisholm A, Harrold J, Maloney NG, Marty L, et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. (2021) 156:104853. 10.1016/j.appet.2020.104853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zbronska I, Medrela-Kuder E. The level of physical activity in elderly persons with overweight and obesity. Roczniki Panstwowego Zakladu Higieny. (2018) 69:369–73. 10.32394/rpzh.2018.0042 [DOI] [PubMed] [Google Scholar]
- 44.Schoberberger R, Dorner T, Rieder A. Health awareness as dominating impact factor on the development of overweight - a health questionnaire among the rural population of Austria. Gesundheitswesen. (2014) 76:336–8. 10.1055/s-0033-1347219 [DOI] [PubMed] [Google Scholar]
- 45.Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tang B, Bragazzi NL, Li Q, Tang S, Xiao Y, Wu J. An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov). Infect Dis Model. (2020) 5:248–55. 10.1016/j.idm.2020.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Luo F, Lai SF, Peng WH, Luo YCD, Wang BG. Investigation on novel coronavirus pneumonia knowledge and attitude among some urban and rural residents in Guangdong. J Guangdong Pharm Univ. (2020) 36:159–64. 10.16809/j.cnki.2096-3653.2020022401 [DOI] [Google Scholar]
- 49.Huang Y, Wu QQ, Wang P, Xu Y, Wang L, Zhao YS, et al. Measures undertaken in China to avoid COVID-19 infection: internet-based, cross-sectional survey study. J Med Internet Res. (2020) 22:12. 10.2196/18718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kajitani S. Working in old age and health outcomes in Japan. Japan World Econ. (2011) 23:153–62. 10.1016/j.japwor.2011.06.001 [DOI] [Google Scholar]
- 51.Arnold KA, Turner N, Barling J, Kelloway EK, McKee MC. Transformational leadership and psychological well-being: the mediating role of meaningful work. J Occup Health Psychol. (2007) 12:193–203. 10.1037/1076-8998.12.3.193 [DOI] [PubMed] [Google Scholar]
- 52.Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med Sci Monit. (2020) 26:e924609. 10.12659/MSM.924609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fontes WHA, Goncalves Junior J, de Vasconcelos CAC, da Silva CGL, Gadelha MSV. Impacts of the SARS-CoV-2 pandemic on the mental health of the elderly. Front Psychiatry. (2020) 11:841. 10.3389/fpsyt.2020.00841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ko CH, Yen CF, Yen JY, Yang MJ. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin Neurosci. (2006) 60:397–403. 10.1111/j.1440-1819.2006.01522.x [DOI] [PubMed] [Google Scholar]
- 55.Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. (2020) 5:e256. 10.1016/S2468-2667(20)30061-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Reynolds K, Pietrzak RH, El-Gabalawy R, Mackenzie CS, Sareen J. Prevalence of psychiatric disorders in US older adults: findings from a nationally representative survey. World Psychiatry. (2015) 14:74–81. 10.1002/wps.20193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Niehaves B, Plattfaut R. Internet adoption by the elderly: employing IS technology acceptance theories for understanding the age-related digital divide. Eur J Inform Syst. (2014) 23:708–26. 10.1057/ejis.2013.19 [DOI] [Google Scholar]
- 58.Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ. (2020) 368:m313. 10.1136/bmj.m313 [DOI] [PubMed] [Google Scholar]
- 59.Xie XF, Stone E, Zheng R, Zhang RG. The ‘Typhoon Eye Effect’: determinants of distress during the SARS epidemic. J Risk Res. (2011) 14:1091–107. 10.1080/13669877.2011.571790 [DOI] [Google Scholar]
- 60.Zhang MY, Wang DH, Power M, Laidlaw K. The features of significant others' social support and its relationship with the attitudes toward aging among older adults. Psychol Sci. (2011) 34:441–6. 10.16719/j.cnki.1671-6981.2011.02.045 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.