Abstract
In this short review, drug delivery systems, formed by polysaccharide-based (i.e., agarose, alginate, and chitosan) aerogels, are analyzed. In particular, the main papers, published in the period 2011–2020 in this research field, have been investigated and critically discussed, in order to highlight strengths and weaknesses of the traditional production techniques (e.g., freeze-drying and air evaporation) of bio-aerogels with respect to supercritical CO2 assisted drying. Supercritical CO2 assisted drying demonstrated to be a promising technique to produce nanostructured bio-aerogels that maintain the starting gel volume and shape, when the solvent removal occurs at negligible surface tension. This characteristic, coupled with the possibility of removing also cross-linking agent residues from the aerogels, makes these advanced devices safe and suitable as carriers for controlled drug delivery applications.
Keywords: agarose, alginate, chitosan, aerogel, supercritical CO2, drug delivery
Introduction
Pharmaceutical industry is evolving from traditional drug delivery systems, in which a biopolymeric matrix is used to provide weight, volume and flowability, toward new formulations, in which a biopolymer is adopted as drug performance enhancer in terms of release time and bioavailability (Agüero et al., 2017; Yuan et al., 2018; Shi et al., 2019; Wei et al., 2020; Liu et al., 2021).
In this field, the production of micro- and nanoparticles has been widely investigated, since they provide effective ways to address issues related to poorly water-soluble drugs and patient compliance (Agnihotri et al., 2004; Markman et al., 2013; Singh et al., 2019; Guastaferro et al., 2020).
Nowadays, also polymeric gels are becoming promising matrices for drug delivery, thanks to their nanostructured morphology that allows to reach larger drug loadings and an improved controlled release of the active compounds over time. In this regard, Cardea et al. (2018) realized poly(vinylidene fluoride-hexafluoropropylene) (PVDF-HFP) aerogels loaded with curcumin in order to obtain a prolonged drug release. Nanofibrous aerogels characterized by open interconnected pores and high porosity value (almost 94%) were produced by supercritical drying, and curcumin release was extended up to 44 h. Also Follmann et al. (2020) realized nanofibrous silica-based hybrid gels, with the aim to deliver camptothecin (CPT), a poorly water-soluble anticancer drug, in a sustained manner. In this case, aerogels ensured CPT release for more than 2 weeks. Giray et al. (2012) realized a composite gel consisting of a silica core coated by polyethyleneglycol (PEG). The results indicated that a slower release of ketoprofen was achieved increasing PEG diacrylate concentration, since it lowered aerogel permeability when it was immersed in an aqueous solution. Therefore, the main advantages of these systems over the traditional ones are: (i) tendency to deliver pharmaceutical compounds more selectively to a specific site, (ii) to maintain drug levels in the desired range, (iii) to increase patient compliance, and (iv) to prevent side effects (Van der Lubben et al., 2001; Guenther et al., 2008; Mehling et al., 2009; García-González et al., 2011; Marin et al., 2014; Lovskaya et al., 2015; Sosnik et al., 2021).
In this context, biocompatibility and biodegradability are essential features; therefore, polysaccharide-based polymers can be considered as “key formulation ingredients,” due to their natural properties (Zheng et al., 2015; Ferreira et al., 2016; Manivasagan and Oh, 2016; Wang et al., 2019). However, the final porous structure of these gels, required for drug release, depends on the kind of drying technique used. In particular, gels can be termed as “xerogel” when sample drying is carried out under ambient pressure and at room temperature, for some days (Conzatti et al., 2017; Takeshita et al., 2020b). Despite the energy-saving advantage of this technique, it leads to the formation of a condense structure that may have low porosity values and large shrinkage (Mirzaei et al., 2013; Buchtová and Budtova, 2016; Sukhodub et al., 2018; López-Iglesias et al., 2019). “Cryogels” are produced when the solvent inside the gel matrix is extracted by freeze drying. During this process, the liquid part in the wet-gel is frozen and, subsequently, under low pressure, the frozen wet-gel is dried by sublimation (Cheng et al., 2012; Gupta and Nayak, 2016; Mahmoud and Salama, 2016; You et al., 2017; Rubio-Elizalde et al., 2019; Yang et al., 2019).
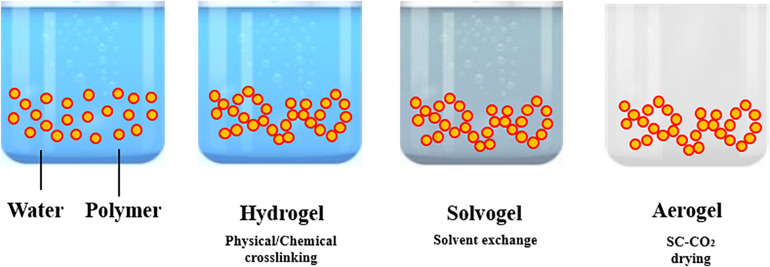
The processing steps involved in “aerogels” production are summarized in Figure 1. Aerogel production frequently starts from the formation of a gel in an aqueous solution, adding a chemical, physical or enzymatic cross-linker. Operating in this way, a hydrogel is obtained. The following step is the replacement of the water present in the 3-D network of the hydrogel by an organic solvent; the resulting gel is named as solvogel. Solvent exchange step is a critical and dynamic process that can strongly affect the final aerogel morphology. In particular, solvent composition, kind of solvent and exchange rate are the main parameters to be investigated (Takeshita et al., 2020a). According to Takeshita et al. (2020a), a low affinity between the polymer forming the gel and the substituting solvent induces the formation of an aerogel-like structure during the solvent exchange itself and a drastic shrinkage of the gel. Therefore, to minimize this phenomenon, some guidelines can be followed: (i) to select an organic solvent at high affinity with the biopolymer (Takeshita et al., 2020a); (ii) to perform a multi-step solvent exchange (García-González et al., 2011; Baldino et al., 2019), at increasing percentage by volume of the solvent substituting water. Operating in this way, the liquid-liquid extraction and substitution of water with the organic solvent selected, evolves gradually, reducing gel shrinkage and other undesired structure modifications. Then, the solvent is extracted from the solid network by supercritical CO2 (SC-CO2): a supercritical mixture with an almost zero surface tension is formed, at the opportune operative conditions of pressure and temperature, between CO2 and the organic solvent that avoids the collapse of the delicate gel nanostructure (Reverchon et al., 2008; Cardea et al., 2009; Baldino et al., 2016; Muñoz-Ruíz et al., 2019).
FIGURE 1.
Aerogel production procedure.
Gels dried under supercritical conditions show unique properties, such as large porosity, uniform pore sizes, and high surface area, in the range of 500–1,200 m2/g, due to mesoporous (<50 nm and >2 nm) and micropores (<2 nm) distribution inside the polymeric matrix (Soleimani Dorcheh and Abbasi, 2008; Baldino et al., 2015, 2019; García-González et al., 2015). Moreover, they are made up of about 95% of air or gas by volume and, consequently, are very light in weight (Del Gaudio et al., 2013; Della Porta et al., 2013; Lu et al., 2014; Mallepally et al., 2015; Quraishi et al., 2015; Baldino et al., 2019). Aerogels could overcome the problems associated with slow drug dissolution rate, unfavorable pharmacokinetics, poor bio-distribution and lack of selectivity for target tissues (Ulker and Erkey, 2014; Lovskaya et al., 2015; Mohammadian et al., 2018). Therefore, the combination of the outstanding structural properties of aerogels with the physiological compatibility of polysaccharides would result in high potential drug delivery systems (Huang et al., 2011; Matricardi et al., 2013; Shelke et al., 2014; Ren et al., 2018).
In this short review, the attention will be focused on the production of chitosan (CS), alginate (ALG), and agarose (AGR) aerogels for the pharmaceutical field. Indeed, among the other applications, these biopolymers have also been studied for drug delivery, and the respective percentages of investigation are: 11.92% agarose, 37.74% alginate and 50.34% chitosan. They were calculated using the database Science Direct, looking at the number of papers written in the period 2011–2020. The path used was the following one: “biopolymer (AGR/ALG/CS), drug delivery, aerogel/cryogel.” Strengths and weaknesses of the traditional production techniques (e.g., freeze-drying and air evaporation) of these bio-aerogels will be critically compared with supercritical CO2 assisted drying, to highlight possible indications to obtain advanced bio-carriers for controlled drug delivery applications.
Chitosan-Based Gels
Chitosan is derived from chitin that is the major component of the crustacean exoskeleton, and is naturally hydrophilic. CS exhibits biocompatible, biodegradable, and non-toxic properties (Pillai et al., 2009; Venkatesan and Kim, 2010).
The first step toward CS-based aerogel production is represented by hydrogel formation (Shi et al., 2021). CS hydrogels can be prepared by non-covalent strategies that take advantage of ionic interactions, H-bonding and Van der Waals forces. In these cases, gel formation can be reversed (Cerchiara et al., 2002; Berger et al., 2004; Boucard et al., 2005). However, physically cross-linked gels could present some drawbacks; i.e., weak mechanical strength, uncontrolled gel pore size and fast dissolution kinetics (Dash et al., 2011). Improvements of mechanical properties can be obtained by permanent hydrogel networks, using covalent bonding between polymeric chains. In particular, the presence of –NH2 and –OH groups on CS chains offers the possibility to create different linkages, such as amide and ester bonding, as well as Schiff base formation (Croisier and Jérôme, 2013). The production of chemically cross-linked gels is achieved by mixing chitosan aqueous solutions with cross-linkers or charged polymers, under specific conditions of pH and temperature (López-León et al., 2005; Liang et al., 2009; Cui et al., 2014; Pellá et al., 2018). Glutaraldehyde (GTA), diglycidyl ether, diisocyanate, and diacrylate, are generally used for this purpose (Hoare and Kohane, 2008). However, their use in pharmaceutical and biomedical applications is restricted, since these cross-linking agents can deactivate or limit drug efficiency and can be cytotoxic for cells (Zeiger et al., 2005; Takigawa and Endo, 2006). In order to overcome these limitations, Takeshita et al. (2021) synthesized chitosan aerogels using a green technology that avoided the use of harmful chemicals, such as aldehyde cross-linkers. In particular, CS aerogels were produced by urea-induced gelation. Urea is an industrial reagent that is widely used due to its low cost and low toxicity. In this study, urea-induced gelation was followed by ethanol exchange and SC-CO2 drying. However, a drastic shrinkage was observed for CS samples at each value of urea concentration. Also genipin, that is a natural chemical compound ables to bind amino groups between amino molecules, can be used to produce a cross-linked CS at good mechanical and degradative properties (Dimida et al., 2015). CS hydrogels can be also prepared by increasing pH of the acidic polymer solutions. In this way, a sol-gel transition is promoted, due to hydrophobic interactions (Moura et al., 2007; Tabernero et al., 2020). Pereira et al. (2020) synthesized CS microspheres loaded with silver (Ag) nanoparticles, through pH inversion mechanism, to be used as bactericidal agent. The results revealed that these systems were effective against Gram-positive and Gram-negative microorganisms. The Ag-loaded CS microspheres were also tested as drug delivery systems, and ibuprofen was used as model drug. The addition of Ag nanoparticles into polymeric matrix promoted a significant delay of ibuprofen release that was extended up to 6 h, with respect to CS-only based microparticles. Gómez et al. (2018) fabricated colloidal suspensions of CS/chondroitin that were subsequently freeze dried to obtain lyophilized nanocomplexes. These cryogels were loaded with a garlic extract and tested against Staphylococcus aureus (S. aureus), a pathogenic microorganism in chronic skin lesions. The dried gels showed a non-homogeneous morphology consisting of fibers and sheets. The introduction of the extract led to an increase of pristine gel hardness and to an enhanced antibacterial action against S. aureus. Obaidat et al. (2015) prepared CS-based aerogel carriers using two different technologies, i.e., SC-CO2 assisted drying and freeze drying. Then, these carriers were loaded with salbutamol. SEM analysis revealed several cracks and voids in the freeze dried samples; whereas aerogels preserved a high open porosity and textural properties. The release profile of salbutamol from samples produced by supercritical drying could be considered suitable for pulmonary drug delivery systems; the release from cryogels was instead negatively affected by a low porosity and a low value of surface area. Terzić et al. (2018) prepared CS-based gels and investigated how the drying technique used could affect the drug release system behavior. With the aim of increasing CS hydrophilicity, it was blended with itaconic acid and methacrylic acid. Then, thymol, that represents the main constituent of oregano essential oil and has a strong antibacterial action, was supercritically impregnated into the polymeric matrix. Two different techniques were used for drying: air drying that led to xerogels formation, and SC-CO2 drying, for aerogel production. SEM analysis showed that xerogels structure was non-porous; indeed, stresses occurred on the pore walls during the extraction of the solvent, inducing the collapse of the gel native structure. On the other hand, during SC-CO2 drying, time resulted the key factor of the process to ensure the desired value of porosity: short processing time led to an incomplete removal of the solvent and, subsequently, a low value of porosity was detected. Due to the high specific surface area, the amount of thymol incorporated into CS aerogel was much higher than the amount loaded into CS xerogel. López-Iglesias et al. (2019) produced CS aerogels loaded with vancomycin to treat infections in chronic wounds. Hydrogel macroparticles were prepared via sol-gel processing and alcogels were subsequently dried. However, xerogels were not able to preserve the intrinsic gel nanoporous structure and high shrinkage values were detected; whereas CS aerogels preserved the overall porosity. A fast release of vancomycin from CS aerogel particles was measured during the first hour and it was followed by a slower release during the next hours.
The initial drug burst effect can be considered a relevant drawback when a sustained drug release is required (Spinks et al., 2006; Aryaei et al., 2014; Xie et al., 2018; Wahba, 2020). To address this issue, CS hydrogels can be covalently cross-linked using UV irradiation or GTA, to obtain an improved mechanical stability (Zeiger et al., 2005; Takigawa and Endo, 2006; Baldino et al., 2015). Baldino et al. (2015) produced CS aerogels by SC-CO2 drying. These samples were characterized by a nanofibrous structure, with an average pore size of 100 nm. Moreover, they demonstrated that, thanks to this process, it was possible to obtain a complete removal of GTA from CS gels: the supercritical mixture (CO2 + ethanol) showed a high affinity toward GTA, favoring its removal from the samples. For this reason, SC-CO2 drying can be considered a promising process to purify chemically cross-linked CS aerogels, to be used for pharmaceutical applications. Mirzaei et al. (2013) prepared CS aerogels cross-linked with GTA for drug delivery. SEM images demonstrated that these xerogels had an average pore size ranging from 100 to 500 μm. Moreover, the swelling trend of these CS xerogels decreased by increasing the amount of cross-linker.
Recently, nanohybrid gels have been used as drug delivery carriers. These pharmaceutical systems are composite materials; they are made up using organic polymers loaded with inorganic nanoparticles. Nanoparticles are supposed to suppress burst drug release behavior, leading to a slower and more continuous release of drugs. Wang et al. (2017) prepared hybrid cryogels of CS, carboxymethyl cellulose (CMC) and graphene oxide (GO), crosslinked by Ca+2. These gels were synthesized using an electrostatic self-assembly approach, followed by freeze drying. SEM images showed a cryogel morphology that was mainly characterized by irregular CS-CMC clusters located on GO sheets. These samples were used to investigate the release of 5-fluorouracil (5-FU), a chemotherapeutic agent adopted in the treatment of cancer. GO addition delayed the release of 5-FU and overcame burst release problems associated with CS-based aerogels. Dinu et al. (2016) synthesized CS/clinoptilolite (CPL) biocomposite cryogels by cryogelation. DIC and indomethacin (IDM) were loaded into these cryogels using the solvent evaporation technique. The release profiles of DIC and IDM from CS/CPL composites were pH-dependent, and drug release increased when pH varied from 1.2 to 7.4. Mahanta et al. (2019) realized CS nanohybrid cryogels using two kinds of disk-shaped nanofillers of opposite surface charges, 30B nanoclay (CS-C), negatively charged, and layer double hydroxide (CS-L), positively charged. The antibacterial drug, tetracycline hydrochloride (TC), was used as a model drug to investigate the release kinetics. Nanohybrids exhibited sustained release kinetics in both cases (hydrogel and dried gels). Scaffolds induced a 90, 69, and 56% of drug release in 15 h, from CS, CS-C, and CS-L, respectively; whereas a 58, 40, and 28% of drug release was measured using the respective hydrogels. A critical summary of these papers is reported in Table 1.
TABLE 1.
Gels of agarose, alginate and chitosan, applied in drug delivery.
| References | Materials | Process | Advantages | Disadvantages |
| Mirzaei et al. (2013) | GTA/CS | SC-CO2 drying | Improved mechanical stability of CS upon the addition of GTA | GTA caused negative effects on pepsin activity |
| García-González et al. (2015) | KET/ALG | SC-CO2 drying | Accelerated KET release | pH-sensitive aerogels |
| Obaidat et al. (2015) | Salbutamol/CS | SC-CO2 drying Freeze drying | Aerogel provided good salbutamol release kinetics | Salbutamol release was negatively affected by low porosity values |
| De Cicco et al. (2016) | ALG/Aminated pectin/Doxycycline | Prilling + SC-CO2 drying | Aerogel characterized by open pore structure and high specific surface area | Complex process |
| Dinu et al. (2016) | CPL/DIC/IDM/CS | Cryogelation + solvent evaporation | The addition of inorganic particles (CPL) improved CS gel stability during drug release | Time-consuming process |
| Sukhodub et al. (2018) | HAp/ALG/CHX | Air drying Freeze drying | Air drying is an energy-save process | During air drying, only a small amount of CHX was incorporated into the scaffolds |
| Wang et al. (2017) | CS/CMC/GO/5-FU | Electrostatic self-assembly approach + SC-CO2 drying | Burst effect associated to CS-based aerogel was eliminated after GO addition | Time-consuming process; Irregular morphology |
| Gómez et al. (2018) | CS/Chondroitin/ S. aureus | Freeze-drying of colloidal suspensions | Cryogels with enhanced antibacterial action against S. aureus | Time-consuming process |
| Mustapa et al. (2018) | C. nutans/ALG | SC-CO2 drying + SC-CO2 impregnation | The same amount of drug was incorporated into the gel using supercritical impregnation instead of organic solvents | Time-consuming process |
| Athamneh et al. (2019) | Sodium Alginate/Hyaluronic acid | Emulsion gelation + SC-CO2 drying | High specific surface area | No experiments in vitro were performed |
| Franco and De Marco (2020) | NIM/KET/DIC/MSTR/CAALG | SC-CO2 drying + SC-CO2 impregnation | CAALG aerogel promoted a controlled release of non-steroidal anti-inflammatory drugs | Not all the solubilised drug in SC-CO2 was absorbed onto the aerogel, and the non-absorbed drug can precipitate in form of nanoparticles |
| López-Iglesias et al. (2019) | Vancomycin/CS | SC-CO2 drying Freeze drying Air evaporation | Overall aerogel porosity preserved during the supercritical drying | Cryogels and xerogels showed a condense structure; Burst effect was detected during the drug release from aerogel |
| Kim et al. (2019) | βCD/ETAGR/BSA/DOX | Freeze drying | AGR derivatives allowed the production of a DD system | ETAGR had a lower cross-linking density than unmodified AGR and, for this reason, burst effect was detected during the drug release test |
| Lynam et al. (2015) | Sucrose-AGR/Proteins | SC-CO2 drying | Sucrose modified hydrogels were characterized by smaller and more uniform pore size | Sucrose particles could be present on the gel |
| Mahanta et al. (2019) | CS-C/CS-L/TC | Freeze drying | The addition of nanofillers provided a less collapsible pore structure; Nanocomposite exhibited a sustained drug release | CS aerogel showed a collapsible cell structure |
| Yuan et al. (2018) | KGM/AGR/Ciprfloxacin | Freeze drying | Drug load efficiency and sustained release capacity of AGR hydrogels were enhanced by KGM incorporation | AGR hydrogels showed a significant burst effect |
| Witzler et al. (2019) | Amoxicillin/AGR-coated HAp | Freeze drying SC-CO2 drying | Supercritically dried samples did not exhibit large pores and seemed to be very homogeneous; Composite materials slowed down drug release for both water-soluble drugs | AGR scaffolds exhibited an initial burst release |
| Pereira et al. (2020) | Ibuprofen/Ag/CS | pH inversion + under vacuum evaporation | A sustained release of ibuprofen was ensured | Epichlorohydrin was used as chemical cross-linker |
| Trucillo et al. (2020) | Ampicillin-loaded liposomes/CAALG | SuperLip + SC-CO2 drying | A more sustained ampicillin release was ensured using the meta-carrier | Part of the liposomes was lost in the solvent used for solvent-exchange |
| Takeshita et al. (2021) | Urea/CS | Urea-induced gelation + SC-CO2 drying | Toxic chemical cross-linkers were avoided | Low values of urea concentration led to a drastic shrinkage of the final sample |
Alginate-Based Gels
Alginate is a naturally occurring anionic polymer, typically obtained from brown seaweed, and has been extensively used for pharmaceutical applications, thanks to its biocompatibility, low toxicity, low cost and easy gelation (García-González et al., 2015; Pantić et al., 2016; Athamneh et al., 2019; Lovskaya and Menshutina, 2020). ALG hydrogels formation can be induced by different cations, such as: H+, Ca+2, Ba+2, Cu+2, Sr+2, Zn+2, Mn+2, Fe+2, Al+3, and Fe+3 (Cao et al., 2020). Indeed, the presence of negatively charged ions in ALG molecules can lead to the formation of polyelectrolyte complexes, because they give the possibility to bind positively charged ions (Hu et al., 2021). Ca+2 is the most used divalent cation to induce alginate gelation, since it shows a high affinity toward the bio-polymer guluronate (G) blocks (Hu et al., 2021). Reynolds and Enquist (1973) proposed, for the first time, the theory of Ca+2 induced ALG gelation mechanism, defining the gel structure as an egg-box model. In this structure, Ca+2 coordinates with six oxygen atoms of two neighboring G units and one to three oxygen atoms of H2O to form a stable structure. However, depending on the final application, different kind of ions can be used: e.g., Ba-ALG gels have been widely used in nanomedicine and Sr-ALG gels show a great potential for tissue regeneration, since they can enhance cell proliferation (Hu et al., 2021). One critical drawback of ionically cross-linked ALG gels is the limited long-term stability in physiological conditions, because these gels can easily dissolve due to the release of divalent ions into the surrounding media, as a consequence of exchange reactions with monovalent cations (Waldman et al., 1998; Qin, 2004, 2005; Santos Miranda et al., 2006).
ALG hydrogels similarity to the extracellular matrices of living tissues allows wide applications in the delivery of small chemical drugs and proteins (Rowley et al., 1999; Augst et al., 2006; Bidarra et al., 2014). Athamneh et al. (2019) realized aerogel microspheres based on sodium alginate and hyaluronic acid for pulmonary drug delivery. Emulsion gelation was combined with SC-CO2 gel drying and, at the end, aerogels, at high specific surface area and good aerodynamic properties, were obtained. García-González et al. (2015) investigated the release kinetics of ketoprofen (KET) from ALG-based aerogels. These authors found that ALG aerogels accelerated KET release at simulated gastric pH conditions. Moreover, it was noted that KET release was mainly governed by a Fickian diffusion mechanism. Sukhodub et al. (2018) synthesized a hydroxyapatite-alginate (HAp)-ALG nanostructured composite for the controlled release of chlorexidine (CHX). The dried samples were obtained by hydrogel drying at 37°C in warm ambient and by freeze drying for 24 h. The densest morphology corresponded to the composite xerogel dried at 37°C; whereas the freeze dried sample had a porous morphology whose homogeneity was slightly improved after HAp addition. Increasing the amount of ALG in the composite gels led to an increase in the volume of adsorbed and released CHX, and the release time also increased from 24 to 72 h. Trucillo et al. (2020) produced a meta-carrier; namely, a carrier entrapped inside another carrier, formed by a liposome loaded aerogel. The antibiotic (ampicillin) was encapsulated into the liposomes, produced by a supercritical assisted liposomes formation (SuperLip) technique. SC-CO2 drying was selected to produce ALG aerogels loaded with ampicillin loaded liposomes. The structures obtained in the case of water exchange with ethanol and acetone were characterized by different morphologies; in particular, the structures obtained in the first case showed nanofibers and open pores, whereas the other ones were uniformly nanoporous. Drug release tests demonstrated that ampicillin release time from these meta-carriers was about twice than its release time from liposomes alone.
Franco and De Marco (2020) used SC-CO2 adsorption to incorporate three non-steroidal anti-inflammatory drugs (NSAIDs), nimesulide (NIM), (KET) and diclofenac sodium (DIC), into maize starch (MSTR) and calcium alginate (CAALG) aerogels. For each NSAID, it can be noted that the amount of drug adsorbed in CAALG was generally higher than the amount loaded in MSTR. Both aerogels were formed by a microporous structure, preserved after supercritical adsorption. The dissolution tests revealed that the adsorption into MSTR allowed a faster release of NSAIDs than pure crystalline drugs; whereas CAALG promoted a controlled release of NSAIDs. Gonçalves et al. (2016) realized ALG-based hybrid aerogels in form of particles to be used as mucosal drug delivery systems. Gel drying and KET loading were performed using SC-CO2. All ALG-based macroparticles showed high specific surface area and large pore volume. Moreover, these formulations were able to provide a slower release of KET in comparison with the pure one. De Cicco et al. (2016) realized aerogel formulations based on ALG and amidated pectin, in form of core-shell microparticles, that were dried using SC-CO2. At the end of the process, these samples were characterized by an open pore structure and high specific surface area. These polymeric aerogels were loaded with doxycycline and the results demonstrated that drug release was affected by pectin and ALG amount. Moreover, doxycycline release kinetics was mainly governed by swelling matrix and erosion phenomena. Mustapa et al. (2018) produced ALG hydrogels that were supercritically dried. Plant extracts of Clinacanthus nutans (C. nutans) were impregnated into ALG aerogels via SC-CO2 assisted impregnation. C. nutans-50 extract was released faster from ALG when was impregnated using supercritical conditions. A critical summary of these papers is reported in Table 1.
Agarose-Based Gels
Agarose is currently used in various research fields including food, DD, DNA electrophoresis, and tissue engineering, owing to its thermo-reversible gel forming ability (Sakai et al., 2007; Gu et al., 2017).
In order to create an AGR gel, heating and cooling processes are involved, and gelation occurs at high temperatures, making difficult to load heat-sensitive drugs. Therefore, researchers have developed AGR gels with low gelling temperatures by modification through acetylation (García-Ruiz et al., 2001), alkylation, alkenylation, acylation, and oxyalkylation (Zhang et al., 2018). The introduction of functional groups hinders the formation of the helicoidal structure at low temperatures, thereby lowering the gelling temperature of AGR (Forget et al., 2015). Moreover, for the development of more innovative AGR-based materials, AGR should comprise special functional groups, such as tosyl or amine moieties (Gericke and Heinze, 2015).
The diffusion characteristics of various substances, including drugs, from AGR gels, are related to the rheological properties of the gels (Normand et al., 2000; Kim et al., 2019). Therefore, AGR derivatives with low gelation temperatures can deliver the substance quickly because the double helicoidal structure during gelation is reduced and, subsequently, the storage modulus is lowered. For this reason, there is a limit in developing effective DD systems that can control the release rates using AGR derivatives with low gelation temperatures (Kim et al., 2019).
Kim et al. (2019) described the introduction of β-cyclodextrin (βCD) into an ethylenediamine-modified agarose (ETAGR) for the development of AGR at low gelling temperatures. The modified gels were prepared by freeze drying and used for both bovine serum albumin (BSA) and doxorubicin (DOX) release. The section of non-functionalized AGR gel was characterized by a non-uniform distribution of pore sizes. The release profiles showed that increasing the cross-linking density of the gel or increasing AGR concentration, the diffusion rate and, subsequently, the release kinetics of BSA, slowed down. Since CFAs had lower cross-linking density than AGR, due to the presence of ethylenediamine groups, BSA was released within a few hours with a non-negligible initial burst effect. Lynam et al. (2015) developed AGR scaffolds used for the controlled release of proteins, for nerve repair. Solvogels were supercritically dried after the replacement of water in AGR hydrogel with ethanol. Pores of 0.10 μm were identified; moreover, SEM images showed a homogeneous and nanoporous morphology. Witzler et al. (2019) investigated the release behavior from AGR-coated Hap, using two model drugs, i.e., adenosine 5′-triphosphate (ATP) and suramin. A prolonged release over 4 days was found for both samples (cryogel and aerogel). However, freeze dried samples exhibited large pores in the range of several hundred micrometers. This was due to the growth of ice crystals during the freezing process. In contrast to the freeze dried samples, the SC-CO2 dried ones were characterized by a higher specific surface area. Yuan et al. (2018) produced a polymeric blend with konjac glucomannan (KGM) and AGR, for ciprofloxacin release, using freeze drying. KGM is a natural polysaccharide found in the tuber of Amorphophallus konjac. The addition of KGM determined a clear effect on the internal morphology of AGR gels: the increase in KGM led to a more compact internal structure with smaller pores. The release results demonstrated that encapsulation, drug loading efficiencies, and sustained release capacity of AGR cryogels, were enhanced by the incorporation of KGM. However, more than 95% of ciprofloxacin was released in the first half hour, because most of the drug was localized on the surface of the polymeric matrix. A critical summary of these papers is reported in Table 1.
Conclusion
In this short review, the main production techniques of drug delivery systems, based on natural, biocompatible and biodegradable polymers, were analyzed. Bio-based aerogels are supposed to be promising candidates as drug carriers, thanks to the native overall nanoporosity and the high specific surface area. These features allow to reach a high drug loading and to obtain a sustained drug release over time.
Freeze drying and air evaporation are the most consolidate and frequently used drying techniques to produce these bio-polymeric systems. However, they can lead to dense and/or not homogeneous final gel structures; therefore, alternative drying techniques should be selected to preserve these relevant characteristics for drug release. Supercritical CO2 assisted drying can overcome these drawbacks, allowing to produce nanostructured bio-aerogels, that maintain the starting gel volume and shape. These aerogel properties are preserved when (i) water/solvent exchange step is carefully performed by selecting the opportune organic solvent and a slow exchange rate, and (ii) the process operative conditions guarantee the formation of a supercritical mixture (CO2 + organic solvent) at negligible surface tension. Moreover, SC-CO2 assisted drying can also remove cross-linking agent residues from the aerogels, making these advanced bio-carriers safe and suitable for controlled drug delivery applications.
Author Contributions
MG and LB: conceptualization. MG: writing—original draft preparation. LB: writing—review and editing. ER: supervision. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
- Ag
silver
- AGR
agarose
- ALG
alginate
- ATP
adenosine 5′-triphosphate
- BSA
bovine serum albumin
- CAALG
calcium alginate
- CPT
camptothecin
- β CD
β-cyclodextrin
- CMC
carboxymethyl cellulose
- CHX
chlorexidine
- CPL
clinoptilolite
- CS
chitosan
- CS-C
nanoclay-loaded chitosan
- CS-L
layer double hydroxide-loaded chitosan
- DIC
diclofenac sodium
- DOX
doxorubicin
- ETAGR
ethylenediamine-modified agarose
- 5-FU
5-fluorouracil
- GO
graphene oxide
- GTA
gluteraldehyde
- G
guluronate
- HAp
hydroxyapatite
- IDM
indomethacin
- KET
ketoprofen
- KGM
konjac glucomannan
- MSTR
maize starch
- NIM
nimesulide
- NSAIDs
non-steroidal anti-inflammatory drugs
- PEG
polyethyleneglycol
- PVDF-HFP
poly(vinylidene fluoride-hexafluoropropylene)
- S. aureus
staphylococcus aureus
- SC-CO2
supercritical CO2
- SuperLip
supercritical assisted liposomes formation
- TC
tetracycline hydrochloride.
References
- Agnihotri S. A., Mallikarjuna N. N., Aminabhavi T. M. (2004). Recent advances on chitosan-based micro- and nanoparticles in drug delivery. J. Control. Release 100 5–28. 10.1016/j.jconrel.2004.08.010 [DOI] [PubMed] [Google Scholar]
- Agüero L., Zaldivar-Silva D., Peña L., Dias M. (2017). Alginate microparticles as oral colon drug delivery device: a review. Carbohydr. Polym. 168 32–43. 10.1016/j.carbpol.2017.03.033 [DOI] [PubMed] [Google Scholar]
- Aryaei A., Jayatissa A. H., Jayasuriya A. C. (2014). Mechanical and biological properties of chitosan/carbon nanotube nanocomposite films. J. Biomed. Mater. Res. A 102 2704–2712. 10.1002/jbm.a.34942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athamneh T., Amin A., Benke E., Ambrus R., Leopold C. S., Gurikov P., et al. (2019). Alginate and hybrid alginate-hyaluronic acid aerogel microspheres as potential carrier for pulmonary drug delivery. J. Supercrit. Fluids 150 49–55. 10.1016/j.supflu.2019.04.013 [DOI] [Google Scholar]
- Augst A. D., Kong H. J., Mooney D. J. (2006). Alginate hydrogels as biomaterials. Macromol. Biosci. 6 623–633. 10.1002/mabi.200600069 [DOI] [PubMed] [Google Scholar]
- Baldino L., Cardea S., Scognamiglio M., Reverchon E. (2019). A new tool to produce alginate-based aerogels for medical applications, by supercritical gel drying. J. Supercrit. Fluids 146 152–158. 10.1016/j.supflu.2019.01.016 [DOI] [Google Scholar]
- Baldino L., Concilio S., Cardea S., Reverchon E. (2016). Interpenetration of natural polymer aerogels by supercritical drying. Polymers 8:106. 10.3390/polym8040106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldino L., Concilio S., Cardea S., De Marco I., Reverchon E. (2015). Complete glutaraldehyde elimination during chitosan hydrogel drying by SC-CO2 processing. J. Supercrit. Fluids 103 70–76. 10.1016/j.supflu.2015.04.020 [DOI] [Google Scholar]
- Berger J., Reist M., Mayer J. M., Felt O., Gurny R. (2004). Structure and interactions in chitosan hydrogels formed by complexation or aggregation for biomedical applications. Eur. J. Pharm. Biopharm. 57 35–52. 10.1016/S0939-6411(03)00160-7 [DOI] [PubMed] [Google Scholar]
- Bidarra S. J., Barrias C. C., Granja P. L. (2014). Injectable alginate hydrogels for cell delivery in tissue engineering. Acta Biomater. 10 1646–1662. 10.1016/j.actbio.2013.12.006 [DOI] [PubMed] [Google Scholar]
- Boucard N., Viton C., Domard A. (2005). New aspects of the formation of physical hydrogels of chitosan in a hydroalcoholic medium. Biomacromolecules 6 3227–3237. 10.1021/bm050653d [DOI] [PubMed] [Google Scholar]
- Buchtová N., Budtova T. (2016). Cellulose aero-, cryo- and xerogels: towards understanding of morphology control. Cellulose 23 2585–2595. 10.1007/s10570-016-0960-8 [DOI] [Google Scholar]
- Cao L., Lu W., Mata A., Nishinari K., Fang Y. (2020). Egg-box model-based gelation of alginate and pectin: a review. Carbohydr. Polym. 242:116389. 10.1016/j.carbpol.2020.116389 [DOI] [PubMed] [Google Scholar]
- Cardea S., Baldino L., Reverchon E. (2018). Comparative study of PVDF-HFP-curcumin porous structures produced by supercritical assisted processes. J. Supercrit. Fluids 133 270–277. 10.1016/j.supflu.2017.10.026 [DOI] [Google Scholar]
- Cardea S., Gugliuzza A., Sessa M., Aceto M. C., Drioli E., Reverchon E. (2009). Supercritical gel drying: a powerful tool for tailoring symmetric porous PVDF-HFP membranes. ACS Appl. Mater. Interfaces 1:171–180. 10.1021/am800101a [DOI] [PubMed] [Google Scholar]
- Cerchiara T., Luppi B., Bigucci F., Orienti I., Zecchi V. (2002). Physically cross-linked chitosan hydrogels as topical vehicles for hydrophilic drugs. J. Pharm. Pharmacol. 54 1453–1459. 10.1211/00223570281 [DOI] [PubMed] [Google Scholar]
- Cheng Y., Lu L., Zhang W., Shi J., Cao Y. (2012). Reinforced low density alginate-based aerogels: preparation, hydrophobic modification and characterization. Carbohydr. Polym. 88 1093–1099. 10.1016/j.carbpol.2012.01.075 [DOI] [Google Scholar]
- Conzatti G., Faucon D., Castel M., Ayadi F., Cavalie S., Tourrette A. (2017). Alginate/chitosan polyelectrolyte complexes: a comparative study of the influence of the drying step on physicochemical properties. Carbohydr. Polym. 172 142–151. 10.1016/j.carbpol.2017.05.023 [DOI] [PubMed] [Google Scholar]
- Croisier F., Jérôme C. (2013). Chitosan-based biomaterials for tissue engineering. Eur. Polym. J. 49 780–792. 10.1016/j.eurpolymj.2012.12.009 [DOI] [Google Scholar]
- Cui L., Jia J., Guo Y., Liu Y., Zhu P. (2014). Preparation and characterization of IPN hydrogels composed of chitosan and gelatin cross-linked by genipin. Carbohydr. Polym. 99 31–38. 10.1016/j.carbpol.2013.08.048 [DOI] [PubMed] [Google Scholar]
- Dash M., Chiellini F., Ottenbrite R. M., Chiellini E. (2011). Chitosan - A versatile semi-synthetic polymer in biomedical applications. Prog. Polym. Sci. 36 981–1014. 10.1016/j.progpolymsci.2011.02.001 [DOI] [Google Scholar]
- De Cicco F., Russo P., Reverchon E., García-González C. A., Aquino R. P., Del Gaudio P. (2016). Prilling and supercritical drying: a successful duo to produce core-shell polysaccharide aerogel beads for wound healing. Carbohydr. Polym. 147 482–489. 10.1016/j.carbpol.2016.04.031 [DOI] [PubMed] [Google Scholar]
- Del Gaudio P., Auriemma G., Mencherini T., Porta G., Della Reverchon E., Aquino R. P. (2013). Design of alginate-based aerogel for nonsteroidal anti-inflammatory drugs controlled delivery systems using prilling and supercritical-assisted drying. J. Pharm. Sci. 102 185–194. 10.1002/jps.23361 [DOI] [PubMed] [Google Scholar]
- Della Porta G., Del Gaudio P., De Cicco F., Aquino R. P., Reverchon E. (2013). Supercritical drying of alginate beads for the development of aerogel biomaterials: optimization of process parameters and exchange solvents. Ind. Eng. Chem. Res. 52 12003–12009. 10.1021/ie401335c [DOI] [Google Scholar]
- Dimida S., Demitri C., De Benedictis V. M., Scalera F., Gervaso F., Sannino A. (2015). Genipin-cross-linked chitosan-based hydrogels: reaction kinetics and structure-related characteristics. J. Appl. Polym. Sci. 132:42256. 10.1002/app.42256 [DOI] [Google Scholar]
- Dinu M. V., Cocarta A. I., Dragan E. S. (2016). Synthesis, characterization and drug release properties of 3D chitosan/clinoptilolite biocomposite cryogels. Carbohydr. Polym. 153 203–211. 10.1016/j.carbpol.2016.07.111 [DOI] [PubMed] [Google Scholar]
- Ferreira A. R. V., Alves V. D., Coelhoso I. M. (2016). Polysaccharide-based membranes in food packaging applications. Membranes 6:22. 10.3390/membranes6020022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Follmann H. D. M., Oliveira O. N., Martins A. C., Lazarin-Bidóia D., Nakamura C. V., Rubira A. F., et al. (2020). Nanofibrous silica microparticles/polymer hybrid aerogels for sustained delivery of poorly water-soluble camptothecin. J. Colloid Interface Sci. 567 92–102. 10.1016/j.jcis.2020.01.110 [DOI] [PubMed] [Google Scholar]
- Forget A., Pique R. A., Ahmadi V., Lüdeke S., Shastri V. P. (2015). Mechanically tailored agarose hydrogels through molecular alloying with β-sheet polysaccharides. Macromol. Rapid Commun. 36 196–203. 10.1002/marc.201400353 [DOI] [PubMed] [Google Scholar]
- Franco P., De Marco I. (2020). Supercritical CO2 adsorption of non-steroidal anti-inflammatory drugs into biopolymer aerogels. J. CO2 Util. 36 40–53. 10.1016/j.jcou.2019.11.001 [DOI] [Google Scholar]
- García-González C. A., Alnaief M., Smirnova I. (2011). Polysaccharide-based aerogels - promising biodegradable carriers for drug delivery systems. Carbohydr. Polym. 86 1425–1438. 10.1016/j.carbpol.2011.06.066 [DOI] [Google Scholar]
- García-González C. A., Jin M., Gerth J., Alvarez-Lorenzo C., Smirnova I. (2015). Polysaccharide-based aerogel microspheres for oral drug delivery. Carbohydr. Polym. 117 797–806. 10.1016/j.carbpol.2014.10.045 [DOI] [PubMed] [Google Scholar]
- García-Ruiz J. M., Novella M. L., Moreno R., Gavira J. A. (2001). Agarose as crystallization media for proteins I: transport processes. J. Cryst. Growth 232 165–172. 10.1016/S0022-0248(01)01146-0 [DOI] [Google Scholar]
- Gericke M., Heinze T. (2015). Homogeneous tosylation of agarose as an approach toward novel functional polysaccharide materials. Carbohydr. Polym. 127 236–245. 10.1016/j.carbpol.2015.03.025 [DOI] [PubMed] [Google Scholar]
- Giray S., Bal T., Kartal A. M., Kizilel S., Erkey C. (2012). Controlled drug delivery through a novel PEG hydrogel encapsulated silica aerogel system. J. Biomed. Mater. Res. A 100 1307–1315. 10.1002/jbm.a.34056 [DOI] [PubMed] [Google Scholar]
- Gómez M. A., Bonilla J. M., Coronel M. A., Martínez J., Morán-Trujillo L., Orellana S. L., et al. (2018). Antibacterial activity against Staphylococcus aureus of chitosan/chondroitin sulfate nanocomplex aerogels alone and enriched with erythromycin and elephant garlic (Allium ampeloprasum L. var. ampeloprasum) extract. Pure Appl. Chem. 90 885–900. 10.1515/pac-2016-1112 [DOI] [Google Scholar]
- Gonçalves V. S. S., Gurikov P., Poejo J., Matias A. A., Heinrich S., Duarte C. M. M., et al. (2016). Alginate-based hybrid aerogel microparticles for mucosal drug delivery. Eur. J. Pharm. Biopharm. 107 160–170. 10.1016/j.ejpb.2016.07.003 [DOI] [PubMed] [Google Scholar]
- Gu Y., Cheong K. L., Du H. (2017). Modification and comparison of three Gracilaria spp. agarose with methylation for promotion of its gelling properties. Chem. Cent. J. 11:104. 10.1186/s13065-017-0334-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guastaferro M., Baldino L., Cardea S., Reverchon E. (2020). Supercritical assisted electrospray/spinning to produce PVP+quercetin microparticles and microfibers. J. Taiwan Inst. Chem. Eng. 117 278–286. 10.1016/j.jtice.2020.12.017 [DOI] [Google Scholar]
- Guenther U., Smirnova I., Neubert R. H. H. (2008). Hydrophilic silica aerogels as dermal drug delivery systems - dithranol as a model drug. Eur. J. Pharm. Biopharm. 69 935–942. 10.1016/j.ejpb.2008.02.003 [DOI] [PubMed] [Google Scholar]
- Gupta P., Nayak K. K. (2016). Optimization of keratin/alginate scaffold using RSM and its characterization for tissue engineering. Int. J. Biol. Macromol. 85 141–149. 10.1016/j.ijbiomac.2015.12.010 [DOI] [PubMed] [Google Scholar]
- Hoare T. R., Kohane D. S. (2008). Hydrogels in drug delivery: progress and challenges. Polymer 49 1993–2007. 10.1016/j.polymer.2008.01.027 [DOI] [Google Scholar]
- Hu C., Lu W., Mata A., Nishinari K., Fang Y. (2021). Ions-induced gelation of alginate: mechanisms and applications. Int. J. Biol. Macromol. 177 578–588. 10.1016/j.ijbiomac.2021.02.086 [DOI] [PubMed] [Google Scholar]
- Huang D., Zuo Y., Zou Q., Zhang L., Li J., Cheng L., et al. (2011). Antibacterial chitosan coating on nano-hydroxyapatite/polyamide66 porous bone scaffold for drug delivery. J. Biomater. Sci. Polym. Ed. 22 931–944. 10.1163/092050610X496576 [DOI] [PubMed] [Google Scholar]
- Kim C., Jeong D., Kim S., Kim Y., Jung S. (2019). Cyclodextrin functionalized agarose gel with low gelling temperature for controlled drug delivery systems. Carbohydr. Polym. 222:115011. 10.1016/j.carbpol.2019.115011 [DOI] [PubMed] [Google Scholar]
- Liang S., Liu L., Huang Q., Yam K. L. (2009). Preparation of single or double-network chitosan/poly(vinyl alcohol) gel films through selectively cross-linking method. Carbohydr. Polym. 77 718–724. 10.1016/j.carbpol.2009.02.007 [DOI] [Google Scholar]
- Liu Z., Zhang S., He B., Wang S., Kong F. (2021). Synthesis of cellulose aerogels as promising carriers for drug delivery: a review. Cellulose 28 2697–2714. 10.1007/s10570-021-03734-9 [DOI] [Google Scholar]
- López-Iglesias C., Barros J., Ardao I., Monteiro F. J., Alvarez-Lorenzo C., Gómez-Amoza J. L., et al. (2019). Vancomycin-loaded chitosan aerogel particles for chronic wound applications. Carbohydr. Polym. 204 223–231. 10.1016/j.carbpol.2018.10.012 [DOI] [PubMed] [Google Scholar]
- López-León T., Carvalho E. L. S., Seijo B., Ortega-Vinuesa J. L., Bastos-González D. (2005). Physicochemical characterization of chitosan nanoparticles: electrokinetic and stability behavior. J. Colloid Interface Sci. 283 344–351. 10.1016/j.jcis.2004.08.186 [DOI] [PubMed] [Google Scholar]
- Lovskaya D. D., Lebedev A. E., Menshutina N. V. (2015). Aerogels as drug delivery systems: in vitro and in vivo evaluations. J. Supercrit. Fluids 106 115–121. 10.1016/j.supflu.2015.07.011 [DOI] [Google Scholar]
- Lovskaya D., Menshutina N. (2020). Alginate-based aerogel particles as drug delivery systems: investigation of the supercritical adsorption and in vitro evaluations. Materials 13:329. 10.3390/ma13020329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu T., Li Q., Chen W., Yu H. (2014). Composite aerogels based on dialdehyde nanocellulose and collagen for potential applications as wound dressing and tissue engineering scaffold. Compos. Sci. Technol. 94 132–138. 10.1016/j.compscitech.2014.01.020 [DOI] [Google Scholar]
- Lynam D. A., Shahriari D., Wolf K. J., Angart P. A., Koffler J., Tuszynski M. H., et al. (2015). Brain derived neurotrophic factor release from layer-by-layer coated agarose nerve guidance scaffolds. Acta Biomater. 18 128–131. 10.1016/j.actbio.2015.02.014 [DOI] [PubMed] [Google Scholar]
- Mahanta A. K., Patel D. K., Maiti P. (2019). Nanohybrid scaffold of chitosan and functionalized graphene oxide for controlled drug delivery and bone regeneration. ACS Biomater. Sci. Eng. 5 5139–5149. 10.1021/acsbiomaterials.9b00829 [DOI] [PubMed] [Google Scholar]
- Mahmoud A. A., Salama A. H. (2016). Norfloxacin-loaded collagen/chitosan scaffolds for skin reconstruction: preparation, evaluation and in-vivo wound healing assessment. Eur. J. Pharm. Sci. 83 155–165. 10.1016/j.ejps.2015.12.026 [DOI] [PubMed] [Google Scholar]
- Mallepally R. R., Marin M. A., Surampudi V., Subia B., Rao R. R., Kundu S. C., et al. (2015). Silk fibroin aerogels: potential scaffolds for tissue engineering applications. Biomed. Mater. 10:035002. 10.1088/1748-6041/10/3/035002 [DOI] [PubMed] [Google Scholar]
- Manivasagan P., Oh J. (2016). Marine polysaccharide-based nanomaterials as a novel source of nanobiotechnological applications. Int. J. Biol. Macromol. 82 315–327. 10.1016/j.ijbiomac.2015.10.081 [DOI] [PubMed] [Google Scholar]
- Marin M. A., Mallepally R. R., McHugh M. A. (2014). Silk fibroin aerogels for drug delivery applications. J. Supercrit. Fluids 91 84–89. 10.1016/j.supflu.2014.04.014 [DOI] [Google Scholar]
- Markman J. L., Rekechenetskiy A., Holler E., Ljubimova J. Y. (2013). Nanomedicine therapeutic approaches to overcome cancer drug resistance. Adv. Drug Deliv. Rev. 65 1866–1879. 10.1016/j.addr.2013.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matricardi P., Di Meo C., Coviello T., Hennink W. E., Alhaique F. (2013). Interpenetrating polymer networks polysaccharide hydrogels for drug delivery and tissue engineering. Adv. Drug Deliv. Rev. 65 1172–1187. 10.1016/j.addr.2013.04.002 [DOI] [PubMed] [Google Scholar]
- Mehling T., Smirnova I., Guenther U., Neubert R. H. H. (2009). Polysaccharide-based aerogels as drug carriers. J. Non. Cryst. Solids 355 2472–2479. 10.1016/j.jnoncrysol.2009.08.038 [DOI] [Google Scholar]
- Mirzaei B. E., Ramazani S. A., Shafiee M., Danaei M. (2013). Studies on glutaraldehyde crosslinked chitosan hydrogel properties for drug delivery systems. Int. J. Polym. Mater. Polym. Biomater. 62 605–611. 10.1080/00914037.2013.769165 [DOI] [Google Scholar]
- Mohammadian M., Kashi T. S. J., Erfan M., Soorbaghi F. P. (2018). In-vitro study of ketoprofen release from synthesized silica aerogels (As drug carriers) and evaluation of mathematical kinetic release models. Iran. J. Pharm. Res. 17 818–829. 10.22037/ijpr.2018.2255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moura M. J., Figueiredo M. M., Gil M. H. (2007). Rheological study of genipin cross-linked chitosan hydrogels. Biomacromolecules 8 3823–3829. 10.1021/bm700762w [DOI] [PubMed] [Google Scholar]
- Muñoz-Ruíz A., Escobar-García D. M., Quintana M., Pozos-Guillén A., Flores H. (2019). Synthesis and characterization of a new collagen-alginate aerogel for tissue engineering. J. Nanomater. 2019:2875375. 10.1155/2019/2875375 [DOI] [Google Scholar]
- Mustapa A. N., Martín Á, Cocero M. J. (2018). Alginate aerogels dried by supercritical CO2 as herbal delivery carrier. Malays. J. Anal. Sci. 22 522–531. 10.17576/mjas-2018-2203-21 [DOI] [Google Scholar]
- Normand V., Lootens D. L., Amici E., Plucknett K. P., Aymard P. (2000). New insight into agarose gel mechanical properties. Biomacromolecules 1 730–738. 10.1021/bm005583j [DOI] [PubMed] [Google Scholar]
- Obaidat R. M., Tashtoush B. M., Bayan M. F., Al Bustami R., Alnaief M. (2015). Drying using supercritical fluid technology as a potential method for preparation of chitosan aerogel microparticles. AAPS PharmSciTech 16 1235–1244. 10.1208/s12249-015-0312-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantić M., Knez Ž, Novak Z. (2016). Supercritical impregnation as a feasible technique for entrapment of fat-soluble vitamins into alginate aerogels. J. Non. Cryst. Solids 432 519–526. 10.1016/j.jnoncrysol.2015.11.011 [DOI] [Google Scholar]
- Pellá M. C. G., Lima-Tenório M. K., Tenório-Neto E. T., Guilherme M. R., Muniz E. C., Rubira A. F. (2018). Chitosan-based hydrogels: from preparation to biomedical applications. Carbohydr. Polym. 196 233–245. 10.1016/j.carbpol.2018.05.033 [DOI] [PubMed] [Google Scholar]
- Pereira A. K., dos S., Reis D. T., Barbosa K. M., Scheidt G. N., da Costa L. S., et al. (2020). Antibacterial effects and ibuprofen release potential using chitosan microspheres loaded with silver nanoparticles. Carbohydr. Res. 488:107891. 10.1016/j.carres.2019.107891 [DOI] [PubMed] [Google Scholar]
- Pillai C. K. S., Paul W., Sharma C. P. (2009). Chitin and chitosan polymers: chemistry, solubility and fiber formation. Prog. Polym. Sci. 34 641–678. 10.1016/j.progpolymsci.2009.04.001 [DOI] [Google Scholar]
- Qin Y. (2004). Gel swelling properties of alginate fibers. J. Appl. Polym. Sci. 91 1641–1645. 10.1002/app.13317 [DOI] [Google Scholar]
- Qin Y. (2005). Ion-exchange properties of alginate fibers. Text. Res. J. 75 165–168. 10.1177/004051750507500214 [DOI] [Google Scholar]
- Quraishi S., Martins M., Barros A. A., Gurikov P., Raman S. P., Smirnova I., et al. (2015). Novel non-cytotoxic alginate–lignin hybrid aerogels as scaffolds for tissue engineering. J. Supercrit. Fluids 105 1–8. 10.1016/j.supflu.2014.12.026 [DOI] [Google Scholar]
- Ren B., Chen X., Du S., Ma Y., Chen H., Yuan G., et al. (2018). Injectable polysaccharide hydrogel embedded with hydroxyapatite and calcium carbonate for drug delivery and bone tissue engineering. Int. J. Biol. Macromol. 118 1257–1266. 10.1016/j.ijbiomac.2018.06.200 [DOI] [PubMed] [Google Scholar]
- Reverchon E., Cardea S., Rapuano C. (2008). A new supercritical fluid-based process to produce scaffolds for tissue replacement. J. Supercrit. Fluids 45 365–373. 10.1016/j.supflu.2008.01.005 [DOI] [Google Scholar]
- Reynolds A. E., Enquist L. W. (1973). Biological interactions between polysaccharides. Rev. Med. Virol. 16 393–403. [DOI] [PubMed] [Google Scholar]
- Rowley J. A., Madlambayan G., Mooney D. J. (1999). Alginate hydrogels as synthetic extracellular matrix materials. Biomaterials 20 45–53. 10.1016/S0142-9612(98)00107-0 [DOI] [PubMed] [Google Scholar]
- Rubio-Elizalde I., Bernáldez-Sarabia J., Moreno-Ulloa A., Vilanova C., Juárez P., Licea-Navarro A., et al. (2019). Scaffolds based on alginate-PEG methyl ether methacrylate-Moringa oleifera-Aloe vera for wound healing applications. Carbohydr. Polym. 206 455–467. 10.1016/j.carbpol.2018.11.027 [DOI] [PubMed] [Google Scholar]
- Sakai S., Hashimoto I., Kawakami K. (2007). Synthesis of an agarose-gelatin conjugate for use as a tissue engineering scaffold. J. Biosci. Bioeng. 103 22–26. 10.1263/jbb.103.22 [DOI] [PubMed] [Google Scholar]
- Santos Miranda M. E., Marcolla C., Rodriguez C. A., Wilhelm H. M., Sierakowski M. R., BelleBresolin T. M., et al. (2006). Chitosan and N-carboxymethylchitosan: I. the role of N-carboxymethylation of chitosan in the thermal stability and dynamic mechanical properties of its films. Polym. Int. 55 961–969. 10.1002/pi [DOI] [Google Scholar]
- Shelke N. B., James R., Laurencin C. T., Kumbar S. G. (2014). Polysaccharide biomaterials for drug delivery and regenerative engineering. Polym. Adv. Technol. 25 448–460. 10.1002/pat.3266 [DOI] [Google Scholar]
- Shi M., Zhang H., Song T., Liu X., Gao Y., Zhou J., et al. (2019). Sustainable dual release of antibiotic and growth factor from pH-responsive uniform alginate composite microparticles to enhance wound healing. ACS Appl. Mater. Interfaces 11 22730–22744. 10.1021/acsami.9b04750 [DOI] [PubMed] [Google Scholar]
- Shi W., Ching Y. C., Chuah C. H. (2021). Preparation of aerogel beads and microspheres based on chitosan and cellulose for drug delivery: a review. Int. J. Biol. Macromol. 170 751–767. 10.1016/j.ijbiomac.2020.12.214 [DOI] [PubMed] [Google Scholar]
- Singh A. P., Biswas A., Shukla A., Maiti P. (2019). Targeted therapy in chronic diseases using nanomaterial-based drug delivery vehicles. Signal Transduct. Target. Ther. 4:33. 10.1038/s41392-019-0068-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soleimani Dorcheh A., Abbasi M. H. (2008). Silica aerogel; synthesis, properties and characterization. J. Mater. Process. Technol. 199 10–26. 10.1016/j.jmatprotec.2007.10.060 [DOI] [Google Scholar]
- Sosnik A., García-gonz C. A., Marco I., De Erkey C., Concheiro A., Alvarez-lorenzo C. (2021). Aerogels in drug delivery: from design to application. J. Control. Release 332 40–63. 10.1016/j.jconrel.2021.02.012 [DOI] [PubMed] [Google Scholar]
- Spinks G. M., Shin S. R., Wallace G. G., Whitten P. G., Kim S. I., Kim S. J. (2006). Mechanical properties of chitosan/CNT microfibers obtained with improved dispersion. Sens. Actuators B Chem. 115 678–684. 10.1016/j.snb.2005.10.047 [DOI] [Google Scholar]
- Sukhodub L. F., Sukhodub L. B., Litsis O., Prylutskyy Y. (2018). Synthesis and characterization of hydroxyapatite-alginate nanostructured composites for the controlled drug release. Mater. Chem. Phys. 217 228–234. 10.1016/j.matchemphys.2018.06.071 [DOI] [Google Scholar]
- Tabernero A., Baldino L., Misol A., Cardea S., del Valle E. M. M. (2020). Role of rheological properties on physical chitosan aerogels obtained by supercritical drying. Carbohydr. Polym. 233:115850. 10.1016/j.carbpol.2020.115850 [DOI] [PubMed] [Google Scholar]
- Takeshita S., Sadeghpour A., Sivaraman D., Zhao S., Malfait W. J. (2020a). Solvents, CO2 and biopolymers: structure formation in chitosan aerogel. Carbohydr. Polym. 247:116680. 10.1016/j.carbpol.2020.116680 [DOI] [PubMed] [Google Scholar]
- Takeshita S., Zhao S., Malfait W. J. (2021). Transparent, aldehyde-free chitosan aerogel. Carbohydr. Polym. 251:117089. 10.1016/j.carbpol.2020.117089 [DOI] [PubMed] [Google Scholar]
- Takeshita S., Zhao S., Malfait W. J., Koebel M. M. (2020b). Chemistry of chitosan aerogels: three-dimensional pore control for tailored applications. Angew. Chemie Int. Ed. Engl. 60 9828–9851. 10.1002/anie.202003053 [DOI] [PubMed] [Google Scholar]
- Takigawa T., Endo Y. (2006). Effects of glutaraldehyde exposure on human health. J. Occup. Health 48 75–87. 10.1539/joh.48.75 [DOI] [PubMed] [Google Scholar]
- Terzić I., Ivanović J., Žižović I., Lučić Škorić M., Milosavljević N., Milašinović N., et al. (2018). A novel chitosan gels: supercritical CO2 drying and impregnation with thymol. Polym. Eng. Sci. 58 2192–2199. 10.1002/pen.24834 [DOI] [Google Scholar]
- Trucillo P., Cardea S., Baldino L., Reverchon E. (2020). Production of liposomes loaded alginate aerogels using two supercritical CO2 assisted techniques. J. CO2 Util. 39:101161. 10.1016/j.jcou.2020.101161 [DOI] [Google Scholar]
- Ulker Z., Erkey C. (2014). An emerging platform for drug delivery: aerogel based systems. J. Control. Release 177 51–63. 10.1016/j.jconrel.2013.12.033 [DOI] [PubMed] [Google Scholar]
- Van der Lubben I. M., Verhoef J. C., Borchard G., Junginger H. E. (2001). Chitosan for mucosal vaccination. Adv. Drug Deliv. Rev. 52 139–144. 10.1016/S0169-409X(01)00197-1 [DOI] [PubMed] [Google Scholar]
- Venkatesan J., Kim S. K. (2010). Chitosan composites for bone tissue engineering - an overview. Mar. Drugs 8 2252–2266. 10.3390/md8082252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahba M. I. (2020). Enhancement of the mechanical properties of chitosan. J. Biomater. Sci. Polym. Ed. 31 350–375. 10.1080/09205063.2019.1692641 [DOI] [PubMed] [Google Scholar]
- Waldman A. S., Schechinger L., Govindarajoo G., Nowick J. S., Pignolet L. H., Labuza T. (1998). The alginate demonstration: polymers, food science, and ion exchange. J. Chem. Educ. 75 1430–1431. 10.1021/ed075p1430 [DOI] [Google Scholar]
- Wang R., Shou D., Lv O., Kong Y., Deng L., Shen J. (2017). pH-Controlled drug delivery with hybrid aerogel of chitosan, carboxymethyl cellulose and graphene oxide as the carrier. Int. J. Biol. Macromol. 103 248–253. 10.1016/j.ijbiomac.2017.05.064 [DOI] [PubMed] [Google Scholar]
- Wang Y., Su Y., Wang W., Fang Y., Riffat S. B., Jiang F. (2019). The advances of polysaccharide-based aerogels: preparation and potential application. Carbohydr. Polym. 226:115242. 10.1016/j.carbpol.2019.115242 [DOI] [PubMed] [Google Scholar]
- Wei S., Ching Y. C., Chuah C. H. (2020). Synthesis of chitosan aerogels as promising carriers for drug delivery: a review. Carbohydr. Polym. 231:115744. 10.1016/j.carbpol.2019.115744 [DOI] [PubMed] [Google Scholar]
- Witzler M., Ottensmeyer P. F., Gericke M., Heinze T., Tobiasch E., Schulze M. (2019). Non-Cytotoxic Agarose/Hydroxyapatite composite scaffolds for drug release. Int. J. Mol. Sci. 20:3565. 10.3390/ijms20143565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie Y., Liao X., Zhang J., Yang F., Fan Z. (2018). Novel chitosan hydrogels reinforced by silver nanoparticles with ultrahigh mechanical and high antibacterial properties for accelerating wound healing. Int. J. Biol. Macromol. 119 402–412. 10.1016/j.ijbiomac.2018.07.060 [DOI] [PubMed] [Google Scholar]
- Yang W., Xu H., Lan Y., Zhu Q., Liu Y., Huang S., et al. (2019). Preparation and characterisation of a novel silk fibroin/hyaluronic acid/sodium alginate scaffold for skin repair. Int. J. Biol. Macromol. 130 58–67. 10.1016/j.ijbiomac.2019.02.120 [DOI] [PubMed] [Google Scholar]
- You C., Li Q., Wang X., Wu P., Ho J. K., Jin R., et al. (2017). Silver nanoparticle loaded collagen/chitosan scaffolds promote wound healing via regulating fibroblast migration and macrophage activation. Sci. Rep. 7:10489. 10.1038/s41598-017-10481-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan Y., Wang L., Mu R. J., Gong J., Wang Y., Li Y., et al. (2018). Effects of konjac glucomannan on the structure, properties, and drug release characteristics of agarose hydrogels. Carbohydr. Polym. 190 196–203. 10.1016/j.carbpol.2018.02.049 [DOI] [PubMed] [Google Scholar]
- Zeiger E., Gollapudi B., Spencer P. (2005). Genetic toxicity and carcinogenicity studies of glutaraldehyde - A review. Mutat. Res. Rev. Mutat. Res. 589 136–151. 10.1016/j.mrrev.2005.01.001 [DOI] [PubMed] [Google Scholar]
- Zhang Z., Wang X., Wang Y., Hao J. (2018). Rapid-forming and self-healing agarose-based hydrogels for tissue adhesives and potential wound dressings. Biomacromolecules 19 980–988. 10.1021/acs.biomac.7b01764 [DOI] [PubMed] [Google Scholar]
- Zheng Y., Monty J., Linhardt R. J. (2015). Polysaccharide-based nanocomposites and their applications. Carbohydr. Res. 405 23–32. 10.1016/j.carres.2014.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]