Abstract
BACKGROUND:
COVID-19 pandemic has forced medical colleges around the world to shift to online teaching. There is hardly any evidence regarding such rapid transitions to online teaching, especially from resource-poor settings. We share our experience of developing an online teaching program based on teachers’ and students’ feedback.
MATERIALS AND METHODS:
A mixed methods study was conducted during the COVID-19 lockdown period in a public-funded medical institute of India. Online feedback was obtained 3 weeks after the beginning of emergency remote teaching. The responses by the students and teachers shaped the final online teaching program which reinforced the perceived strengths and addressed the weaknesses. Observations were made for the proportion of scheduled lectures delivered through digital platform and students’ attendance in the 1st week and last week of the study period.
RESULTS:
Feedback was obtained from 367 students and 56 teachers. Around three-fourths of the students (76.7%) and teachers (73.2%) were satisfied with online teaching. The themes generated for benefits of online teaching were similar for both students and teachers, but the perceived challenges differed. Students found online teaching more stressful, and teachers were apprehensive of the new technology and lack of a controlled environment.
CONCLUSIONS:
A rapid transition to development and implementation of an online teaching program was found to be feasible and acceptable to the primary stakeholders. Not only the content but student engagement and supportive environment for both students and teachers are essential requirements in the context of an online undergraduate teaching program.
Keywords: COVID-19, graduate medical education, online teaching, pandemic
Introduction
The COVID-19 pandemic is now compared to a black swan event,[1] an event which was an outlier and had an enormous effect on human life. Medical institutes had to shut down their campus teaching to restrict COVID-19 spread, disrupting medical training programs.[2,3] Going online was the only recourse available to continue medical education in the given scenario. The medical institutes in the low- and middle-income countries did not have the institutional readiness in terms of human and infrastructural resources to shift to online learning, when this pandemic hit.[4] An increasing number of medical colleges will have to rapidly transition to online teaching in the coming months, as COVID-19 further spreads in more geographical areas, and the emerging reports of the second wave of the pandemic hitting those already affected.[5,6]
The future uncertainty of this pandemic requires that all medical institutions strive to shift to online mode soon, just as some have already begun with. In India, unprepared teachers and students got immersed in a lesser-known online teaching environment.[7] This hurried shift in most of the medical colleges did not follow the principles of online learning and therefore cannot be labeled as an online teaching program, but it can be called “emergency remote teaching.”[8] We could not find any report about the transition from emergency remote teaching to online teaching program for the medical undergraduates. Evidence is required to make informed decisions about rapid development of structured online teaching programs, which follow the principles of online learning. We describe the development of an online teaching program which was initiated as emergency remote teaching in a medical college of India during the COVID-19 lockdown period, based on the feedback of students and teachers.
Materials and Methods
The study protocol was reviewed and approved by the Institutional Ethics Committee, Human Research No. IEC-HR/2020/44/4.
This study was conducted in an autonomous, public-funded medical college of Delhi, India, from March 15 to May 15, 2020. The college has four cohorts, with around 150 students in each of the admission years 2016–2019. The institution has a functional department of biostatistics and medical informatics to manage computer hardware and software issues and a medical education unit (MEU) for faculty development.
The college was closed from mid of March as a measure for mitigation of COVID-19 pandemic and the closure continued throughout the study period. To continue with medical education, the college immediately shifted to remote teaching and the medical teachers were instructed to upload their scheduled lecture handouts on the college website.
A committee was constituted to develop the online teaching program. The online teaching program was defined as primarily didactic lectures accessed through digital platforms that do not require active interaction with the video playback interface.[9] The digital platform, GoToWebinar (LogMeIn, Inc., Boston, Massachusetts, 2020), was selected, based on the available features, data privacy concerns, and cost. Social media messaging groups such as WhatsApp were created for the students for respective batches. Student representatives worked as coordinators between teachers and students for sharing online lecture joining links and class announcements. Guides for using the digital platform were developed and circulated, and online orientation training for the faculties was organized.
Three weeks after the initiation of online teaching using the digital platform, an online survey was done to find students’ and teachers’ perceptions to develop a structured and sustainable teaching program which adheres to the principles of online learning.[10,11,12]
The survey consisted of Google Forms-based questionnaires, separate for the students and the teachers.
The students’ questionnaire had sections pertaining to sociodemographic characteristics, prior exposure to online teaching platforms, reaction, and learning. Reaction was measured by the satisfaction status and level of comfort with the new modality of teaching. A five-point Likert scale was used to measure the level of comfort and for the agreement level to the statement, “The concepts taught by online teaching lectures are better than conventional classroom teaching.”
The teachers’ questionnaire was similar to that for the students except that the reaction was measured by satisfaction status only.
Both the teachers and students were asked to write in text format their reasons of dissatisfaction and challenges faced if any and to indicate the level of agreement for continuation of online classes in the post lockdown period.
The responses by the students and teachers were used to construct the final online teaching program which reinforced the strengths perceived (the benefits associated with) and addressed the weaknesses (challenges faced while using the digital platform), especially the modifiable ones.
Observations were also made for the lectures delivered through digital platform and students’ attendance in the 1st week of online teaching and last week of the study period.
Data analysis
A mixed methods data analysis was done. For quantitative analysis, SPSS software (Version 20.0 for Windows, Armonk, NY, USA: IBM Corp) was used and simple descriptive statistics such as proportion and means were calculated. The attendance of students in the 1st week of online teaching and last week of the study period was presented as the median (interquartile range) and compared by the Wilcoxon test. ANOVA was used to compare the mean comfort levels and understanding of concept scores across the four undergraduate students’ batches.
Thematic analysis was done for description of challenges faced and benefits associated with online teaching. Coding and recoding of the responses were done independently by the authors and matched. A mutually agreeable set of themes were generated. We present the list of themes with select quotations.
Results
Characteristics of the study participants
A total of 487 students responded to the online survey. Two students did not give consent and 13 students did not attend any current online classes and hence were excluded. One hundred and six forms were not complete. Finally, a total of 367 forms were included for the final analysis.
A total of 57 teachers responded, while one teacher did not give consent for participation. Fifteen teachers did not have any online classes scheduled at the study period.
Table 1 presents the basic demographic characteristics, previous exposure, and device used to access online teaching by the students and teachers.
Table 1.
Biosocial characteristics, previous exposure to online teaching, and access to online teaching among the teachers and students in a medical college
| Characteristics | Students (n=367) | n (%) | Teachers (n=56) | n (%) |
|---|---|---|---|---|
| Current designation (batch) | 2016 | 99 (27) | Assistant professor | 6 (10.7) |
| 2017 | 112 (30.5) | Associate professor | 11 (19.6) | |
| 2018 | 74 (20.2) | Professor | 39 (69.7) | |
| 2019 | 82 (22.3) | |||
| Age (years) | 17-19 | 79 (21.5) | 35-43 | 13 (23.2) |
| 20 | 72 (19.6) | 44-48 | 18 (32.1) | |
| 21 | 102 (27.8) | 49-55 | 11 (19.6) | |
| ≥22 | 114 (31.1) | ≥56 | 14 (25.1) | |
| Sex | Female | 76 (20.7) | Female | 33 (58.9) |
| Male | 289 (78.8) | Male | 23 (41.1) | |
| Prefer not to say | 2 (0.5) | |||
| Previous exposure to online teaching | No | 249 (68) | No | 43 (76.8) |
| Yes | 118 (32) | Yes | 13 (23.2) | |
| Place from where online teaching was accessed* | Within Delhi | 180 (49.0) | Home only | 32 (78.0) |
| Outside Delhi | 187 (51.0) | Home and college | 2 (4.9) | |
| College only | 7 (17.1) | |||
| Primary device used to access online teaching* | Desktop/laptop (windows based) | 55 (14.99) | Desktop/laptop (windows) | 37 (90.2) |
| Laptop (mac OS) | 24 (6.54) | Laptop (macOS) | 4 (9.8) | |
| Smartphone (android) | 261 (71.12) | |||
| Smartphone (iOS) | 27 (7.35) |
*Teachers (n=41)
Reaction and learning in online teaching
Among the study participants, three-fourths of the students (76.7%, 245/367) and teachers (73.2%, 30/41) were satisfied, 9% (33/367) of the students and 14.6% (6/41) of the teachers were dissatisfied, whereas 24% (89/367) of the students and 12.2% (5/41) of the teachers gave a neutral response.
The mean (standard deviation) level of comfort among students was 3.77 (0.92) and comprehension in online teaching was 3.17 (1.2). Both these scores showed an increasing trend with respect to the academic year (P < 0.001).
We found that around half of the students and two-fifths of the teachers were not in favor of continuing online teaching in the post lockdown period [Figure 1].
Figure 1.
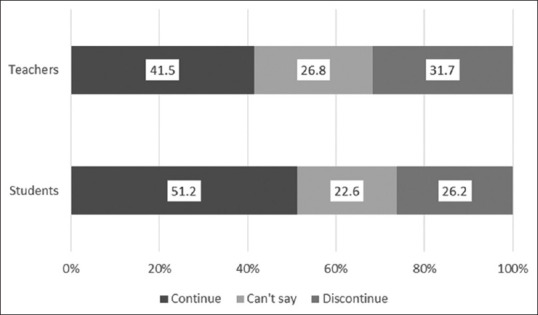
Proportion (%) of students and teachers with respect to their opinion about continuation of online teaching even after the lockdown period is over
Perceived benefits of online teaching
Six themes were identified [Figure 2].
Figure 2.
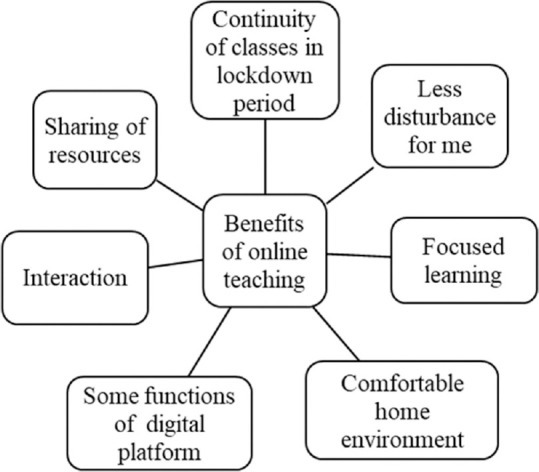
Nonhierarchical diagram showing the benefits of online teaching perceived by medical students and teachers.
Continuity of classes in lockdown period
”Could connect and conduct classes well during corona pandemic” (teacher).
”Our college schedule is being followed so that gives a sense of normalcy and maintains the pace good to attend online classes in this lockdown” (student).
Less disturbance for me
”That one can deliver a talk without getting disturbed as what happens in classroom teaching when students keep walking in, talk to each other or is noticed not paying attention” (teacher).
”No disturbance from students who don't want to listen and keeps on talking continuously as in LT [Lecture Theater]” (student).
Comfortable home environment
”Convenience and flexibility;” “Specifically, useful for medical students with disabilities as it allows them reasonable accommodation” (teacher).
”Ease of study from home” (student).
Interaction
”Students are not hesitant to ask even simplest [of] doubts, which they may not be able to ask in classrooms” (teacher).
”I can type my question directly to the teacher without hesitation” (student).
Sharing of resources
”A lot of learning material, videos can be shared with the students by synchronous or asynchronous means” (teacher).
”Availability of most of the ppts [powerpoint presentations of lectures] in handout section” (student).
Some functions of digital platform
”I like that it can be recorded” (teacher).
”Clear audio and video;” “I can take screen shot;” “I get reminders” (student).
Focused learning
”I feel that students are not distracted if they are sitting with their laptop and have their head-phone plugged in and listening to the lecture” (teacher).
”I feel that the teacher is talking to me only;” “Slides shown in personal screen helps to focus better;” “Can easily focus and concentrate” (student).
Perceived challenges of online teaching
Out of the ten themes generated, four were common for students and teachers, two were exclusive for teachers, and four for students [Figure 3].
Figure 3.
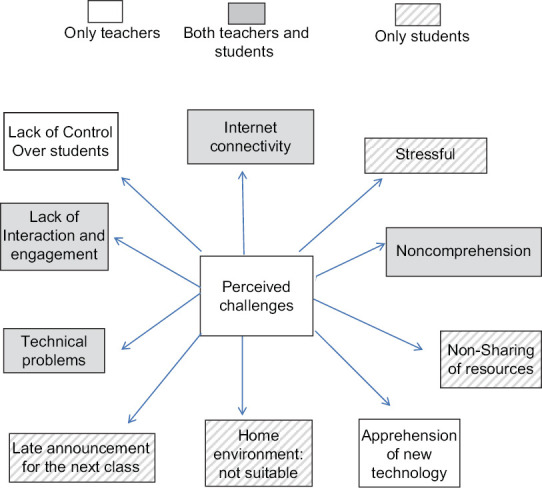
Nonhierarchical diagram showing the challenges of online teaching perceived by medical students and teachers
Internet connectivity
”Many a times faculty's internet connection also does not have enough speed which leads to audio disturbances;” “I get logged out due to poor speed which leaves me in doubt of attendance.” “I only get limited data on my sim cards per day which isn't sufficient to attend all the classes” (student).
”At times audio and video are disrupted due to poor internet connectivity” (teacher).
Lack of interaction and engagement
”I can't ask questions or talk to teacher;” “This hinders not only teacher-student interaction but also student-student interaction” (student).
”To teach your own screen/PC is so boring.” “Not able to see faces (of the students)” (teacher).
Technical problems
”I could not join into 3 lectures as it (the digital platform) was showing waiting for the organizers for the entire class” (student).
”Chat box [digital platform] was not functioning during my lecture” (teacher).
Noncomprehension
”Sometimes there is a lot being taught at once and it is hard for me to grasp” (student).
”Cannot judge how much the students are understanding the concept delivered by me” (teacher).
Stressful
”Too many classes a day, [it] just stress up the mind by staring on smart phone screen for too long” (student).
Home environment not suitable
”It is easy to concentrate at classroom [and] my home environment is not suitable for attending lectures” (student).
Late announcement of class
”I got the link just 1 h prior and I was not prepared” (student).
Nonsharing of resources
”Due to immediate lockdown I was not able to bring my books with me;” “Please upload the powerpoint presentation files of online lectures; [it] will be helpful” (student).
Lack of control
”Failure to create a classroom climate of control” (teacher).
Apprehensions about new technology
”I am very much apprehensive about next classes and actually unable to focus on subject or talk due to lack of knowledge of webinar technology support” (teacher).
Observation from records
The proportion of scheduled lectures held online in the 1st week of online teaching was 60% (27/45) and 72.9% (43/59) in the last week of the study period (P = 0.16). The median (IQR) number of students attending an online lecture was 121 (116–130) in the 1st week of online teaching and 135.5 (129–139) in the last week of the study period (P < 0.001).
Main components of the online teaching program developed
Organized plan for content delivery: The heads of departments were involved in selection of the topics which can be taught online to develop an effective schedule which was circulated among both teachers and students. Plan was made for communication with students in case rescheduling classes were required.
Availability of support system for teachers: A dedicated space with internet facility and supporting staffs was made available for teachers. Both online and on-site training and support were provided to the teachers for conducting online teaching. Social media messaging groups (WhatsApp) for teachers and heads of all departments were used for communication and consultation
Availability of support system to students: Student representatives coordinated the communication between teachers and students. In addition to this, the queries from different students’ social media messaging groups were also directly addressed by the teachers
Sharing of online learning resource material: Uploading of learning resources on the digital platform and of recorded videos on college website was done to take care of bandwidth issues and different learning styles
Plan for student engagement: Guidelines were developed and circulated among the teachers to engage the students during online teaching. Other strategies being used were seminars, multiple choice questions (MCQ)-through Google Forms, and short answer questions through social media messaging groups.
Discussion
Similar to the current pandemic, even during natural disasters such as earthquake floods, cyclones, the medical education gets disrupted in the affected areas, leading to suboptimal delivery of training content.[13] A rapid shift to online teaching is the only viable option in such a scenario. Online teaching as a rapid emergency response was started in the current study during the ongoing COVID-19 pandemic. Such situations also give us an opportunity to study the medical college's response to continue and strengthen teaching. The students’ and teachers’ feedback enabled the decision-makers at the institute level to identify the areas of concern and address them. Our experience can help other institutes, especially of resource-poor setting in evidence-based decision-making in case of a rapid shift to online teaching.
We found that most of the students (68%) and teachers (77%) did not have previous exposure to online teaching, as was also reported for students in a recent study from India.[7]
Teachers and students were forced by circumstances to immerse and experiment with online teaching. More so, there was no time to conduct faculty development programs[14] to implement online teaching during this sudden lockdown, despite having a functional MEU. The development of the online teaching program presented in this study may work as enablers for professional and personal development of teachers and students.[15]
It was observed that most (71%) of the students accessed online teaching through smartphones which may be due to their relative affordability and widespread availability. The online teaching activities should be decided considering the functionality and limitations of smartphones compared to a personal computer.[16]
In the present study with the progression of the academic years, the students reported an increasingly positive effect with online teaching which was consistent with a study done earlier.[17] The acclimatization of students with the medical curriculum in higher academic years may also have made them more comfortable with online teaching program. This shows that more guidance may be required for the students during initial period of medical school.
Even though most of the students and teachers were satisfied with online teaching, it was noticed that around half of them did not agree for continuation of online teaching in the post lockdown period. It is possible that the participants were satisfied with online teaching only as a short-term measure. This might reflect the need for continuous technical, logistical, and training support among study participants for the long-term success of online teaching.[18]
While studying the perceived benefits and the challenges by the study participants, it was observed that some criteria were perceived as an enabler by some, whereas the same was considered an obstacle by others. For example, home environment was perceived as comfortable, whereas it was perceived as not suitable by others. Similar to another study from China,[19] student–teacher interaction was perceived as easier in online teaching by some students, while others found it more difficult. More focused learning was reported by some, whereas noncomprehension of the subject taught was reported. This paradox may be explained by individual variation and styles of learning among students. A balanced approach of traditional and online program may be helpful in this context.[20,21]
Teachers’ concern for student not monitored was addressed by student engagement by creating multiple participatory activities.[22]
Teachers have a limited role in peer relationship and communication, however, an attempt was made to monitor the dynamics with reports from student representatives by addressing queries so that negative impact on learning can be minimized. Similarly, teachers’ ownership with the program was ensured by organizing orientation activities, communication through social messaging groups, and developing guidelines.
Care was taken to create an online effective learning environment which is consistent with culture of the institute keeping in mind the issues of learner safety (choosing of the digital platform) and learner belonging taking ownership.
Limitations
This experience is from a single medical college and during a limited period in the initial months of development of the program, thus limiting its generalizability. Participation being voluntary in nature, the nonrespondent's views might not have been captured in the study. Our study primarily focused on synchronous teaching during this period. Asynchronous teaching was limited, by way of uploading of lectures in the initial days of the lockdown period.
Conclusions
A rapid transition to development and implementation of an online teaching program was found to be feasible and acceptable to the primary stakeholders. Not only the content but student engagement and supportive environment for both students and teachers are essential requirements in the context of an online undergraduate teaching program
We recommend that the online teaching program developed during this pandemic lockdown should be used to promote self-directed learning as envisioned in competency-based medical education.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank Ramansh Bandhu Gupta, a medical undergraduate student of UCMS, Delhi, for his support in pretesting the student feedback form.
References
- 1.Mazzoleni S, Turchetti G, Ambrosino N. The COVID-19 outbreak: From “black swan” to global challenges and opportunities. Pulmonology. 2020;26:117–8. doi: 10.1016/j.pulmoe.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sandhu P, de Wolf M. The impact of COVID-19 on the undergraduate medical curriculum. Med Educ Online [serial online] 2020;25:1764740. doi: 10.1080/10872981.2020.1764740. cited 2020 Jul 23. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7269089/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferrel MN, Ryan JJ. The impact of COVID-19 on medical education. Cureus. 2020;12:e7492. doi: 10.7759/cureus.7492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frehywot S, Vovides Y, Talib Z, Mikhail N, Ross H, Wohltjen H, et al. E-learning in medical education in resource constrained low- and middle-income countries. Hum Resour Health. 2013;11:4. doi: 10.1186/1478-4491-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leung K, Wu JT, Liu D, Leung GM. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: A modelling impact assessment. Lancet. 2020;395:1382–93. doi: 10.1016/S0140-6736(20)30746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Brouwer R, van Veldhuisen DJ, de Boer RA. Surviving the first COVID-19 wave and learning lessons for the second [published online ahead of print, 2020 Jun 21] Eur J Heart Fail. 2020. 10.1002/ejhf. 1938. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7323385/ [DOI] [PMC free article] [PubMed]
- 7.Singh K, Srivastav S, Bhardwaj A, Dixit A, Misra S. Medical education during the COVID-19 pandemic: A single institution experience. Indian Pediatr [online ahead of print] 2020. cited 2020 Jul 23. S097475591600174. Available from: https://pubmed.ncbi.nlm.nih.gov/32366728/ [DOI] [PMC free article] [PubMed]
- 8.Hodges CB, Moore S, Lockee BB, Trust T, Bond MA. The Difference Between Emergency Remote Teaching and Online Learning. Educase Review [serial online] 2020. cited 2020 Jul 23. Available from: https://er.educause.edu/articles/2020/3/the-difference-between-emergency-remote-teaching-and-onlinelearning .
- 9.Tang B, Coret A, Qureshi A, Barron H, Ayala AP, Law M. Online lectures in undergraduate medical education: Scoping Review. JMIR Med Educ. 2018;4:e11. doi: 10.2196/mededu.9091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merzouk A, Kurosinski P, Kostikas K. e-Learning for the medical team: The present and future of ERS Learning Resources. Breathe. 2014;10:296–304. [Google Scholar]
- 11.Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online [serial online] 2019;24:1666538. doi: 10.1080/10872981.2019.1666538. cited 2020 Jul 23. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6758693/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ellaway R, Masters K. AMEE Guide 32: E-Learning in medical education Part 1: Learning, teaching and assessment. Med Teach. 2008;30:455–73. doi: 10.1080/01421590802108331. [DOI] [PubMed] [Google Scholar]
- 13.Wilkinson TJ, Ali AN, Bell CJ, Carter FA, Frampton CM, McKenzie JM. The impact of learning environment disruption on medical student performance. Med Educ. 2013;47:210–3. doi: 10.1111/medu.12065. [DOI] [PubMed] [Google Scholar]
- 14.Childs S, Blekinsopp E, Hall A, Walton G. Effective e-learning for health professionals and students-barriers and solutions. A systematic review of the literature Findings from the HeXL project. Health Info Lib J. 2005;22:20–32. doi: 10.1111/j.1470-3327.2005.00614.x. [DOI] [PubMed] [Google Scholar]
- 15.Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323:2131–2. doi: 10.1001/jama.2020.5227. [DOI] [PubMed] [Google Scholar]
- 16.Chandra A, Nongkynrih B, Gupta SK. Role of smartphone technology in medical education in India. Indian J Community Fam Med. 2019;5:103–7. [Google Scholar]
- 17.Nanda B, Bhattacharjee M, Chawla O, Rajajeyakumar M, Kapoor R. Incorporating e-learning as a tool for medical education in India: Investigating student perspectives. J Educ Technol Health Sci. 2018;5:25–30. [Google Scholar]
- 18.Shahmoradi L, Changizi V, Mehraeen E, Bashiri A, Jannat B, Hosseini M. The challenges of E-learning system: Higher educational institutions perspective. J Educ Health Promot. 2018;7:116. doi: 10.4103/jehp.jehp_39_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shih KC, Chan JC, Chen JY, Lai JS. Ophthalmic clinical skills teaching in the time of COVID-19: A crisis and opportunity. Med Educ. 2020;54:663–4. doi: 10.1111/medu.14189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mokaripour P, Shokrpour N, Bazrafkan L. Comparison of readiness for e-learning from the perspective of students and professors of Medical Sciences. J Educ Health Promot. 2020;9:111. doi: 10.4103/jehp.jehp_668_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mosalanejad L, Ahmady S. Implementation of blended learning with native systems: A new model for the application of new technology in Iranian medical education. J Educ Health Promot. 2019;8:239. doi: 10.4103/jehp.jehp_402_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kay D, Pasarica M. Using technology to increase student (and faculty satisfaction with) engagement in medical education. Adv Physiol Educ. 2019;43:408–13. doi: 10.1152/advan.00033.2019. [DOI] [PubMed] [Google Scholar]


