Abstract
Liver transplantation (LT) for alcohol related hepatitis (AH) remains controversial. We convened a consensus conference to examine various aspects of LT for AH. The goal was not to unequivocally endorse LT for AH; instead it was to propose recommendations for programs that perform or plan to perform LT for AH. Criteria were established to determine candidacy for LT in the setting of AH and included the following: (1) AH patients presenting for the first time with decompensated liver disease that are non-responders to medical therapy without severe medical or psychiatric comorbidities (2) A fixed period of abstinence prior to transplantation is not required (3) Assessment with a multidisciplinary psychosocial team including a social worker and a addiction specialist/mental health professional with addiction and transplantation expertise. Supporting factors include lack of repeated unsuccessful attempts at addiction rehabilitation, lack of other substance use/dependency, acceptance of diagnosis/insight with commitment of patient/family to sobriety and formalized agreement to adhere to total alcohol abstinence and counseling. LT should be avoided in AH patients that are likely to spontaneously recover. Short- and long-term survival comparable to other indications for LT must be achieved. There should not be further disparity in LT either by indication, geography, or other sociodemographic factors. Treatment of alcohol use disorders should be incorporated into pre and post-LT care. The restrictive and focused evaluation process described in the initial LT experience for AH worldwide may not endure as this indication gains wider acceptance at more LT programs. Transparency in selection process is crucial with collection of objective data to assess outcomes and minimize center variation in listing. Oversight of program adherence is crucial to harmonize listing practices and outcomes.
Keywords: alcoholic hepatitis, guidelines, mortality, waitlist
Introduction
Alcohol is a major cause of liver disease worldwide(1) with alcohol related liver disease (ALD) being one the most frequent indication for liver transplantation (LT) in the US.(2) In addition to complications of cirrhosis and hepatocellular carcinoma, alcohol related hepatitis (AH) remains an important cause of liver related morbidity and mortality. Influenced by small trials showing acceptable outcomes in highly selected patients, transplantation for AH is increasingly performed in the US and elsewhere.(3–8) The percentage of patients transplanted for AH is likely underestimated; in a recent study only 35% of recipients transplanted for AH were accurately identified.(9)
However, LT for AH faces substantial challenges. The medical criteria for AH LT must be carefully defined such that premature use of LT does not occur for patients likely to recover with supportive care. Additionally, in urgent cases of patients with AH, requirements for specific periods of significant sobriety pre-LT may vary. The ability to provide the potential benefits of LT for AH patients must be balanced against the potential for alcohol relapse with resulting morbidity and mortality post-LT. LT for AH may lead to disparities related to selection of candidates with AH for LT (may favor patients with resources) as well as impacting LT rates for other indications. While it is worthy to consider a more compassionate and thoughtful approach to LT for AH patients the shortened time frame for transplant evaluation in urgent AH cases makes it difficult even for experienced teams to accurately capture psychosocial aspects predictive of outcomes after LT in AH. The public and provider perception of LT for ALD continues to evolve and may not be as controversial as previously thought.(10–18) Further, there is a growing recognition that successful outcomes after LT also depend on appropriate treatment of co-existing alcohol use disorder (AUD). These complexities demand a multidisciplinary team approach to the assessment, selection and post-LT longitudinal care of AH patients.
To address these issues, Baylor University Medical Center in Dallas, Texas organized a two-day consensus conference (April 5–6, 2019) endorsed by International Liver Transplantation Society and American Society of Transplant Surgeons. The goal was not to unequivocally endorse LT for AH; instead was to bring together a multidisciplinary group to discuss AH related practices at their centers and consider how clinical assessment, care, and selection for LT could be improved by the collective experiences.
General considerations: Alcohol related hepatitis
Definition:
Defining AH requires consideration of the pattern of alcohol use, clinical and laboratory presentation and exclusion of other etiologies of liver dysfunction. Guidance is provided by a recent consensus statement on behalf of National Institute on Alcohol Abuse and Alcoholism (NIAAA) though this definition focuses on bringing uniformity to clinical trials and does not address LT.(19) (Table 1 and 2) Liver biopsy should be pursued in cases where the diagnosis of AH is unclear and/or if any alternative diagnosis may affect the treatment plan, especially with regards to eligibility for LT. Considering LT for AH does not obviate program requirements for chronic liver disease/cirrhosis related to alcohol which may follow a separate center specific pathway.
Table 1:
Suggested changes in nomenclature
| Suggested | Current |
|---|---|
| Alcohol related liver disease | Alcoholic liver disease |
| Relapse | Recidivism |
| Alcohol related hepatitis | Alcoholic hepatitis |
| Alcohol use disorder | Alcoholic |
Table 2:
Defining alcohol associated hepatitis, modified from NIAAA AH clinical trial definition (Crabb et al Gastroenterology 2016)
| Definition | Clinical entity with rapid onset of jaundice with elevated AST in background of heavy alcohol use. |
| Pattern of alcohol use | Heavy alcohol use for >6 months, <60 days of abstinence before onset of jaundice. |
| Supporting features | |
| Biopsy | steatohepatitis, cholestasis, severe fibrosis |
| Presentation | malaise, tender hepatomegaly, decompensation |
| Labs | Br>3, AST/ALT ratio 1.5, AST<400 |
| Exclude | Drug induced liver injury, biliary obstruction, viral hepatitis, autoimmune liver disease, Wilson disease |
| Spectrum | AH versus acute on chronic liver failure Presence of cirrhosis |
| Definite | Clinical and biopsy proven |
| Probable | Clinical and exclude competing |
| Possible Biopsy recommended |
Clinically diagnosed but with potential confounding factors (e.g. pt denies alcohol) |
| Associated other diagnoses? | E.g. Viral hepatitis |
Incidence and mortality:
Population based estimates in the US confirm an increase in the incidence of AH mirroring a global increase in ALD. (1, 20–22) There has been an increase among young adults, minorities and women. (20, 23–25) In national data, the age and gender standardized rate of ALD related mortality has increased by 3-fold in persons aged 25–34 (CDC accessed March 2019).
Medical Therapy:
The proposed treatment algorithm in AH differentiates management based on disease severity.(26) Treatment for AH includes supportive medical therapy in addition to abstinence from alcohol, management of withdrawal symptoms, nutritional support and consideration of corticosteroid therapy for definite and probable AH. There is a need to accurately identify patients that are candidates for corticosteroid therapy, those ineligible for corticosteroids or non-responders to therapy as early as possible. If corticosteroids are used, absence of response as defined by the Lille score should lead to their discontinuation. Several investigational compounds are under evaluation for patients with AH but their role in AH remains to be established.(27)
Predictive models:
Several predictive models assess treatment response and predict mortality within 1–6 months after diagnosis of AH (28–33). Most models have high negative predictive value (predict those that will do well) and not necessarily identify all that will not survive. A model combining a static component (MELD) with a dynamic model (Lille) may be useful to identify non-responders to medical therapy and/or patients unlikely to recover (34). Extra hepatic complications most notably serious infection and renal failure profoundly affect outcomes.(2, 35–37)
Liver transplantation for alcohol related hepatitis
Figure 1, Table 3 and 4 summarize recommendations from the consensus conference. The following sections discuss specific recommendations in more detail.
Figure 1:
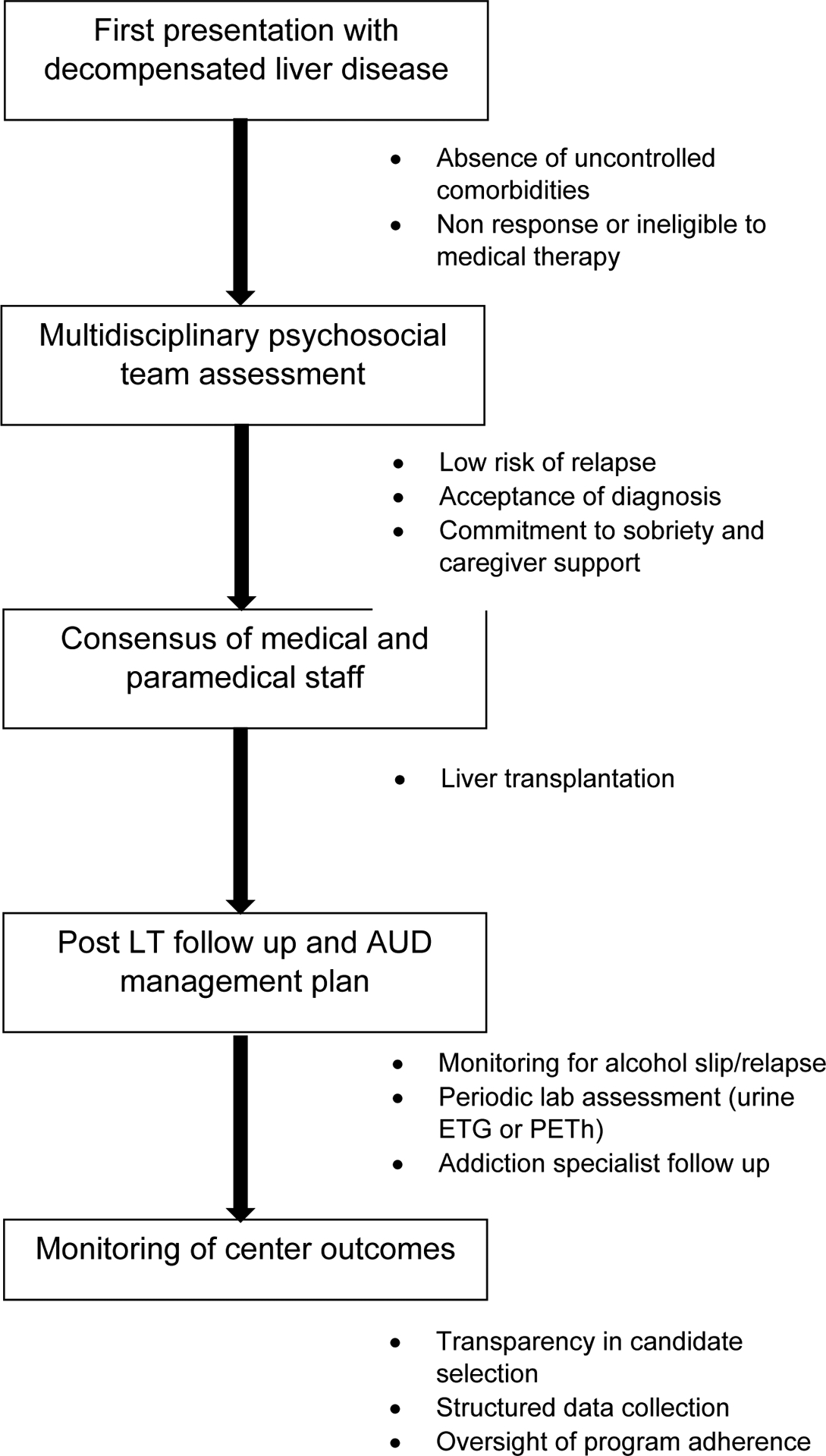
Listing criteria and program components for LT for AH
AH: alcohol related hepatitis; AUD: Alcohol use disorder; PEth: Phosphatidylethanol; ETG: Urinary ethyl glucuronide
Table 3:
Psychosocial domains to be assessed in AH transplant candidates. Most of these predictors are for sustained or harmful relapse (not slips).
| Domain Assessed/Questions Asked | Factors that May Predict Relapse |
|---|---|
| 1. Alcohol Use History | |
|
|
| 2. Other Substance Use History | |
|
|
| 3. Mental Health History | |
|
|
| 4. Treatment Adherence History | |
|
|
| 5. Social Criteria | |
|
|
| Optimal Assessment Criteria | |
| 1. Awake, alert patient (not comatose, altered, or intubated), able to be directly interviewed | |
| 2. Psychosocial team assess patient first to obtain unbiased evaluation of above factors. | |
| 3. Consistent history and commitment verbalized by patient | |
| 4. Multiple assessments over time | |
| 5. Active involvement and sober support by family/caregivers | |
| 6. Corroboration of history from patient collaterals | |
Table 4:
Listing criteria and program components for LT for AH
| Primary criteria | Secondary considerations | |
|---|---|---|
| Alcohol associated hepatitis assessment | First presentation with decompensated AH | No prior liver related hospitalization |
| Absence of severe medical comorbidities |
|
|
| Non-response or ineligible to medical therapy. |
|
|
| Alcohol use disorder assessment | Establish acceptable risk of relapse as assessed by a multidisciplinary psychosocial team composed of a social worker and at least one addiction specialist. |
|
| Direct assessment of patient possible by addiction specialist |
|
|
| A maximum of 1 prior failed attempt at rehabilitation. | ||
| Lack of other active substance use/dependency or active untreated psychiatric disorder | ||
| Acceptance of diagnosis/insight | ||
| Commitment of patient/family to sobriety and formalized agreement to adhere to lifelong total alcohol abstinence | Establish contract and participation in addiction rehabilitation following transplant | |
| Presence of close, supportive family members or caregivers | ||
| Committee Decision making | Consensus of paramedical and medical staff | Consider blinded voting in committee deliberations Consider absolute consensus |
| Program components | Transparency in selection process | LT reserved for patients with a favorable prognosis for long-term abstinence. |
| Independent psychosocial assessment |
|
|
| Structured Post LT follow up mechanism in place |
|
|
| Team mental health |
|
Ethical Considerations:
Liver transplantation balances three principles of justice: urgency, utility, and equity. Urgency demands that organs go to the “sickest first.” AH typically have high MELD scores with 75% mortality at 6 months in those not responding to prednisolone.(32) Utility demands that organs be given to patients in whom post-transplant outcomes will be acceptable. Medically, AH patients compare favorably to other diagnoses, with acceptable post LT patient and graft survival rates.(5, 38) Equity mandates that we adopt principles of liver transplant allocation that are applied similarly to all liver diseases. Where behaviors are responsible for primary liver disease requiring transplant or for graft loss (such as non-adherence) after transplant, allocation decisions should be made in a similar manner and not applied in a more stringent manner only to those with ALD or AH.(39)
European and US Experience in LT for AH:
The initial experience in early “rescue” liver transplant in AH was the French/Belgian trial.(6) Non-responders to medical therapy, defined as a Lille model of ≥ 0.45 or a worsening of MELD score at day 7 of therapy, were considered for rescue LT. Candidates were selected using the following criteria: nonresponse to medical therapy, severe AH as the first liver-decompensating event, presence of close supportive family members, absence of severe coexisting or psychiatric disorders, and agreement to adhere to lifelong total alcohol abstinence. Complete consensus was required among four provider “circles” involved in patient care for LT approval. Ultimately, 26 medical non-responders underwent LT. A significant survival benefit at 6 months was observed (76.9% versus 23.1% for matched non-transplanted patients). Survival after transplant was similar to random responder controls (85%). Relapse rate was low; 10% overall had return to harmful drinking. (6, 40). These results supported future evaluation in selected patients with severe AH failing medical therapy (41).
Studies in the US were subsequently pursued (3–8) As compared to the European experience where a prospective protocol was followed, the US experience was a mix of center specific experience and established protocols. In one study, 20/94 patients (21.2%) with severe AH refractory to medical therapy were approved for LT and 9 ultimately underwent LT (3). Eight of the 9 patients (89%) survived more than 6 months compared to 30% of the patients that did not undergo LT. Two patients had alcohol relapse, neither leading to adverse outcomes. A second pilot study compared the outcomes of LT for AH and alcohol associated cirrhosis (AC). At a median follow-up of 532 days (IQR 281–998 days), rates of alcohol use and harmful drinking post-LT were similar for AH and AC at 28% and 24%, respectively (p=0.80).(7) ACCELERATE-AH, the largest US experience in LT for AH, was a retrospective review from 12 centers, including the two centers that had published the pilot studies.(5) Each center had their own “protocol” and while there were some differences between sites in terms of inclusion/exclusion criteria, there were many similarities.(5) Of the 432 patients evaluated, 155 (35.9%) were accepted as candidates with rates ranging from 13–100% across centers.(5) Psychosocial concerns were the predominant reason for denial of listing for LT. Overall survival after LT for AH was excellent with 1 and 3-year survival rates of 94% (95% CI, 89–97%) and 84 % (95% CI, 75–90%), respectively. In patients surviving to discharge, 28% resumed alcohol use with 11% returning to harmful drinking. Alcohol relapse post-LT had an adverse impact on survival at 3 years when compared with abstainers (75% vs. 97%, respectively, p=0.03) and 7 of the 9 deaths that occurred after one-year were alcohol related. More than 10 drinks per day, non-THC substance use, prior alcohol related legal difficulties, and more than 1 failed alcohol treatment attempt were associated with sustained alcohol use after LT.(42) No long-term follow-up data are available.
Arguments in favor of LT for AH:
First, LT for ALD has been performed since the 1960s.(43) LT for appropriately selected AH prevents premature mortality. In severe AH, failure of medical therapy can be predicted early in the patient’s course and is associated with a 6-month survival around 30%. (32) As most deaths occur within 2 months, early LT is life saving. Second, there are effective treatments for AUDs that patients can participate in following LT. Given the stringent criteria used to select AH LT candidates thus far, relapse rates after LT are similar for patients transplanted for AH versus ALD with cirrhosis.(44–48) Third, LT for those with AH ensures equity of access to life-saving transplant, as in other liver diseases. As an example, LT is offered to obese individuals with NASH even without demonstration of weight loss pre-LT and is also offered to carefully selected patients with acute liver failure following a suicide attempt due to medication overdoses with uncontrolled psychiatric disease. Finally, concern that early LT for AH may decrease organ donation is contrary to a survey showing that most potential organ donors were supportive or neutral with regard to this new indication (16).
Concerns about LT for AH:
First, criteria advocated for LT for AH may not be uniformly adhered to at all centers. There may be a disconnect between the restrictive and focused evaluation process described in the initial experience with LT for AH and its wider acceptance elsewhere across LT programs.(6) There is already wide variation in acceptance of AH for LT and clarity on what criteria are necessary to ensure good outcomes is lacking. Second, relevant outcomes after LT may be inadequately captured. Although survival rates were acceptable, deaths due to fungal infection were frequent in the European experience with most deaths due to infection within 2 weeks after LT. Survival at 6 months for recipients (77%) was much lower than that for ALD reported to UNOS (94%). Variation in medical management (e.g. steroid use) among centers may play a role. Third, the cumulative probability of any alcohol use after LT was 25%, 30% and 34% at 1, 2 and 3 year.(5) Patterns of alcohol use were worrisome with median time to first drink of 160 days (79–346), sustained alcohol use in 38%, and binge or frequent drinking in 42%. Hence, there is an obvious need for predictive tools to identify patients at high risk of relapse especially those with harmful drinking patterns (41). Fourth, high MELD score at LT, common among those presenting with AH, may tilt the balance toward “bending the rules” to transplant these recipients. It is unavoidable that competition between programs will loosen acceptance criteria. The requirements for acceptance should be the same for all patients, regardless of social or financial status. As an example, increasingly women present with AH, though the percent of women undergoing LT for AH is low (5). Hence there may be unrecognized barriers to LT for certain subgroups.
Psychosocial perspective in LT for AH (Table 3)
In addition to being responsible stewards and “gatekeepers,” psychosocial assessors of transplant candidates often create intervention or treatment plans to mitigate risk for potentially poor outcomes. For patients with an AUD and short duration of sobriety this commonly involves engaging the patient in addiction rehabilitation. However, in the urgent AH scenario because there is no time to provide pre-LT rehabilitation, LT teams rely on more stringent selection criteria for AH candidates in hope of preventing poor outcomes post-LT.
Challenges in Evaluation of AUD in an urgent setting:
Evaluation and treatment of AUD that coexists in patients with AH is crucial. During an expedited evaluation, AUD may be inadequately addressed, (2) assessment and selection occurs in a limited and expedited time and (3) treatment for AUD, a chronic disorder with need for ongoing management, is often not accorded priority. In a life-threatening medical condition, it is difficult to expect a patient to contemplate hypotheticals (e.g. lifelong abstinence, willingness to attend addiction rehabilitation, adherence to transplant directives) with no/little evidence they will/can do so. In addition, there is no opportunity to reassess a candidate’s response after addiction treatment initiation. Patients and families may try to manage impressions about or minimize their alcohol use history. Patients may be difficult to interview due to being in denial or feeling ashamed, guilty, overwhelmed, scared, or in pain. In this context, establishment of an effective therapeutic relationship to management AUD can be challenging.
Necessary Components of the psychosocial assessment:
Optimally the patient should be directly interviewed by the social work and mental health and/or addiction professionals. Thus, the request for these evaluations should occur early in the hospital course prior to the development of encephalopathy. The composition of the mental health/social work team and competencies matter and may dictate the quality and strength of recommendations. Transplant centers considering AH transplant should have in place a multidisciplinary psychosocial team composed, at a minimum, of a transplant social worker and a mental health professional preferably with addiction and transplant experience. An addiction specialist may be helpful in ensuring AH patients receive the full spectrum of AUD care. Psychometric scales and instruments can be used to aid the collection and integration of data but should not be used to determine candidacy. Scales may be helpful for tracking treatment response and anticipating further treatment needs. Collateral information should be sought from family members, LT team members and other clinical care providers to provide a comprehensive picture of the patient’s history. Active family or caregiver support is paramount for current and future care. Biochemical markers may also be needed to corroborate drinking history.
Factors associated with risk for post-LT alcohol use:
Until a larger experience is developed with AH alcohol use outcomes, the LT field draws on the substantial experience of predictors of relapse for ALD LT and from the general non-LT population of AUD patients. It is critical to recognize that the presence of a factor associated with alcohol use means the likelihood of alcohol use is greater, not that it is certain.(5, 7, 49–52) Whether a single criterion or cumulative factors are used to determine AH LT candidacy is not settled. Proposed criteria or risk scores have high negative predictive value and predict those who will not return to harmful patters of alcohol use rather than identify those that will.(53)
Duration of sobriety:
Aside from allowing a period of observation to ensure an AH patient has adequate time to respond to medical therapy avoiding preemptive LT, the notion of waiting a specific number of days or months of abstinence to demonstrate the patient’s ability to maintain sobriety is ill-conceived. In AH such a mandated wait could allow the patient to deteriorate increasing the surgical risk, but each month sober only incrementally reduces risk. There is limited support for a specific 6-month cut point(50) Further, in the natural history of AUD, stable abstinence is measured in years not months. Recently, expert guidelines no longer recommend a fixed period of abstinence prior to transplantation (26, 54) and have stopped listing AH as an absolute contraindication (54) to LT contrary to the recommendations from the preceding decade (55).
Post transplantation needs:
After transplantation, the AH LT recipient should be assisted in beginning addiction treatment as soon as medically feasible. This critical requirement should not be lost among the other post-LT care needs. Psychosocial evaluation and treatment should be integrated in the flow of post LT care and should be mandated by center. There should be agreement of LT team to facilitate post-LT participation in addiction treatment and rigorous collection of alcohol use outcome data. To improve adherence, treatment and monitoring expectations should be developed prior to LT. LT teams may need significant assistance from their social work and behavioral health providers to overcome potential barriers to addiction treatment; lack of local care, lack of adequate or appropriate resources, lack of monitoring (biochemical or collateral) and insurance issues.
Living donor transplantation for AH
AH patients listed for deceased donor liver transplantation may also be considered candidates for living donor liver transplantation. The medical risks to the donor are the same regardless of recipient etiology of disease. However, there may be increased psychological risks to donors for recipients with AH related to relapse and graft loss especially long term once routine follow up ends. Adherence to autonomy for both the donor and recipient through the process of informed consent and disclosure is equally important. With AH, the recipient’s etiology of disease and potential for relapse might affect the donor candidate’s decision about donation so centers must have a policy in place regarding disclosure of issues unique to LT for AH. The transplant program must ensure that the urgency of need is not interfering with information disclosure, processing, or the ultimate decisions of donors. The informed consent process also requires voluntariness in decision-making. Voluntariness is defined as the absence of coercion, unwarranted persuasion or undue manipulation. Potential living donors for AH recipients may be victims of unwarranted persuasion because they are asked to decide in a time pressured manner to help a loved one who is at imminent risk of dying. All transplant centers are required to provide an independent living donor advocate for living donor evaluation. For individuals considering living donation to AH recipients, the independent living donor advocate, along with the rest of the donor evaluation team, must ensure that the decision meets the standards of voluntariness.
Payer coverage
The 6-month rule has been enforced and reflected in medical policy set forth by most payers. With recent data and a more definitive set of professional statements and modification of specific institutional criteria referring the 6-month rule, changes in payer coverage policies must follow. This would result in a coverage that better reflects evolving standard of care. A commitment by payers for addiction counseling post transplantation is equally important.
Role of the transplant center
Transparency in center practices and oversight is paramount. The transplant community needs to consider mandated collection of AH specific elements and centers be open to sharing center specific practices to improve outcomes. (Table 5) Local or regional review boards may need to be involved to assure transparency and third party adjudication or oversight will be needed.
Table 5:
Data collection in programs performing LT for AH
| Timing | Main component | Sub component |
|---|---|---|
| Pretransplant | AH | definite, probable, possible |
| Number with AH | ||
| Number evaluated | ||
| Number listed | ||
| Medical and psychosocial Characteristics of evaluated not listed vs listed | Gender, race, MELD, insurance | |
| Medical treatment | Steroids, other | |
| Contraindication or ineligible for steroids | Disease severity Multiorgan failure | |
| Accurate coding for AH | ||
| AUD diagnosis | Mild, moderate, severe | |
| Prior AUD treatment | Types of AUD treatment previously used | |
| Explant and Biopsy characteristics | ||
| Comorbid psychiatric and/or substance use disorders | ||
| Other substance use | ||
| Transplant | Multidisciplinary Team assessment | Addiction specialist Social Worker mental health professional |
| Routine Testing | Alcohol biomarker testing: Phosphatidylethanol (PEth), Urinary ethyl glucuronide | |
| Pattern of alcohol use | Slip, relapse, heavy | |
| Post LT | Documentation of AUD management plan pre and post-LT required | |
| Documentation of EtG or PEtH testing | ||
| Survival 1, 3 5 years |
The need to streamline processes and the anticipated burden to the system (psychosocial assessments, expansion of team, increased hospital volume) is clear. Centers need to invest and ensure having mental health professionals/addiction specialists available not only for pre transplant evaluation, but also for post-transplant assessment and active follow up after discharge. Provider team frustration and burnout may feature prominently as more patients with AH are evaluated. This will require teams to monitor and address the mental health, burnout, and cynicism of their providers and staff. Teams need to insist on and expect psychosocial providers to meet frequently and thoroughly collaborate among themselves.
Expansion of LT for AH will affect center activity. Issues may arise about the number of donor offers, offers accepted for AH candidates but transplanted in other patients and how LT for AH might impact LT for other indications, particularly within the new acuity circle policy. There may be financial gain in transplanting patients with AH; a high MELD patient with AH may inherently have better short-term outcomes than high MELD patients without AH though further data is needed. This could be partially mitigated by requiring centers to meet 2 year survival criterion for AH, as relapse to harmful alcohol use typically leads to deaths beyond the 1st year.
Competition between centers for these patients is a concern. Within a region, there may be market pressures for other centers to follow suit. Hence, failure to offer transplant for patients with AH may reduce referrals for this and other indications. In addition, referral physicians often view an “active plan” such as transplant as a better option than a “passive plan,” i.e., supportive care. So, the perception of the transplant center within the community as an “aggressive” or “forward thinking” or “cutting edge” center plays heavily on the treatment plan for these patients. It needs to be reiterated that only a very small number of patients is expected to fulfill this very strict criteria.
Conclusion
LT for ALD has evolved over the last 40 years, starting from an absolute contraindication to an accepted routine reason for LT. Following in its footsteps, LT for AH remains contentious. With a measured approach that collectively considers and respects the perspectives of all stakeholders in the transplant process, consensus and progress is possible to improve the outcomes of our sickest waitlisted patients, regardless of etiology.
SUMMARY OF RECOMMENDATIONS.
General recommendations: Alcohol related hepatitis
There should be efforts to standardize nomenclature and definition of alcohol related hepatitis (AH) with an emphasis on use of less stigmatizing terminology. (see Table 1 and 2)
Patients with severe AH may be assessed for corticosteroid therapy.
Select patients with severe AH that are unresponsive or ineligible for medical management may be considered for liver transplantation.
Predicting response to therapy or pre-LT mortality is best achieved by assessing response over time (change in Model for end stage liver disease (MELD) score, Lille score or a combination of MELD score plus Lille). Mortality is lower for those that have a Lille score <0.45, respond to therapy, have a declining bilirubin, or are abstinent and these patients may not require LT.
An inflexible period of abstinence prior to transplantation is not desirable. Acceptance for LT listing should be based upon the severity of liver dysfunction and a comprehensive psychosocial evaluation. (see Table 3)
Recommendations for LT for alcohol related hepatitis (see Figure 1 and Table 4)
- The goals of LT for AH include:
- Avoiding LT in patients who will recover without it
- Avoiding futility and achieving short- and long-term survival comparable to other indications for LT
- Avoiding creation of further disparity in LT either by indication (versus other indications), geography, sex, race, insurance status or other sociodemographic factors.
- Identification of LT candidates likely to have long-term abstinence
- Incorporation treatment of alcohol use disorder (AUD) into pre and post-LT care
- Consensus of paramedical and medical staff
- Criteria related to AH
- First presentation with decompensated alcohol-related liver disease
- Absence of severe uncontrolled medical or psychiatric comorbidities.
- Non-response to or ineligible for medical therapy.
- Criteria related to AUD
- Establish acceptable risk of relapse by assessment with a multidisciplinary psychosocial team including a social worker and an addiction medicine specialist/mental health professional with addiction and transplantation expertise.
- Assessment of coherent patient by addiction specialist (i.e. not intubated or floridly encephalopathic).
- Lack of repeated unsuccessful attempts at addiction rehabilitation.
- Lack of current other substance use/dependency.
- Acceptance of ALD diagnosis with insight.
- Commitment of patient to lifelong sobriety and support of sober caregivers to assist patient with abstinence goals.
- Presence of close, supportive family members or caregivers
- Post LT requirements
- Pre-LT confirmation of plan for AUD treatment after LT
- Robust post-transplant monitoring for alcohol slips or relapse during post-LT clinic appointments to include direct interviewing of patient and caregivers about alcohol use.
- Routine monitoring of alcohol use (e.g. with Phosphatidylethanol (PEth), Urinary ethyl glucuronide) for at least 2 years, with frequency and duration individualized beyond this time period.
- Center requirements
- Transparency in the candidate selection process and structured collection of objective data to assess outcomes (see Table 5)
- Ongoing support of abstinence that is integrated into post LT care such as concurrent follow-up by addiction specialist/mental health professional with addiction and transplantation expertise.
- Oversight of program adherence to harmonize listing practices and outcomes.
Acknowledgements
We acknowledge Linda Huante, Katie Hobbs and Amy Waddell for their assistance with organizing the conference.
Attendees: The speakers and participants (total 130) represented members from several states, 3 non-US countries and included transplant programs that had never done a LT for AH as well as programs currently performing LT for AH. The attendees included transplant hepatologists, surgeons, psychiatrists, social workers, coordinators, and administrators representing a broad spectrum of the LT community. A draft of the manuscript was sent to all attendees for their collective input and comments.
Funding source:
Baylor foundation grant
Abbreviations:
- AH
Alcohol related hepatitis
- ALD
Alcohol related liver disease
- AC
Alcohol related cirrhosis
- LT
liver transplantation
Footnotes
Disclosures: The authors of this manuscript have no conflicts of interest to disclose as described by the Liver transplantation
References
- 1.Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009;373:2223–2233. [DOI] [PubMed] [Google Scholar]
- 2.Lee BP, Vittinghoff E, Dodge JL, Cullaro G, Terrault NA. National Trends and Long-term Outcomes of Liver Transplant for Alcohol-Associated Liver Disease in the United States. JAMA Intern Med 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Im GY, Kim-Schluger L, Shenoy A, Schubert E, Goel A, Friedman SL, Florman S, et al. Early Liver Transplantation for Severe Alcoholic Hepatitis in the United States--A Single-Center Experience. Am J Transplant 2016;16:841–849. [DOI] [PubMed] [Google Scholar]
- 4.Lee BP, Chen PH, Haugen C, Hernaez R, Gurakar A, Philosophe B, Dagher N, et al. Three-year Results of a Pilot Program in Early Liver Transplantation for Severe Alcoholic Hepatitis. Ann Surg 2017;265:20–29. [DOI] [PubMed] [Google Scholar]
- 5.Lee BP, Mehta N, Platt L, Gurakar A, Rice JP, Lucey MR, Im GY, et al. Outcomes of Early Liver Transplantation for Patients With Severe Alcoholic Hepatitis. Gastroenterology 2018;155:422–430.e421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mathurin P, Moreno C, Samuel D, Dumortier J, Salleron J, Durand F, Castel H, et al. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med 2011;365:1790–1800. [DOI] [PubMed] [Google Scholar]
- 7.Weeks SR, Sun Z, McCaul ME, Zhu H, Anders RA, Philosophe B, Ottmann SE, et al. Liver Transplantation for Severe Alcoholic Hepatitis, Updated Lessons from the World’s Largest Series. J Am Coll Surg 2018;226:549–557. [DOI] [PubMed] [Google Scholar]
- 8.Puri P, Cholankeril G, Myint TY, Goel A, Sarin SK, Harper AM, Ahmed A. Early Liver Transplantation is a Viable Treatment Option in Severe Acute Alcoholic Hepatitis. Alcohol Alcohol 2018;53:716–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee BP, Im GY, Rice JP, Weinberg E, Hsu C, Fix OK, Therapondos G, et al. Underestimation of Liver Transplantation for Alcoholic Hepatitis in the National Transplant Database. Liver Transpl 2019;25:706–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Antonini TM, Guillaud O, Dumortier J, Dharancy S, Saliba F, Mathurin P, Duclos-Vallee JC, et al. Impact of a first study of early transplantation in acute alcoholic hepatitis: Results of a nationwide survey in french liver transplantation programs. Liver Transpl 2018;24:841–844. [DOI] [PubMed] [Google Scholar]
- 11.Bangaru S, Pedersen MR, MacConmara MP, Singal AG, Mufti AR. Survey of Liver Transplantation Practices for Severe Acute Alcoholic Hepatitis. Liver Transpl 2018;24:1357–1362. [DOI] [PubMed] [Google Scholar]
- 12.Anantharaju A, Van Thiel DH. Liver transplantation for alcoholic liver disease. Alcohol Res Health 2003;27:257–268. [PMC free article] [PubMed] [Google Scholar]
- 13.Dixon J, Welch HG. Priority setting: lessons from Oregon. Lancet 1991;337:891–894. [DOI] [PubMed] [Google Scholar]
- 14.Neuberger J, Adams D, MacMaster P, Maidment A, Speed M. Assessing priorities for allocation of donor liver grafts: survey of public and clinicians. BMJ 1998;317:172–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ratcliffe J. Public preferences for the allocation of donor liver grafts for transplantation. Health Econ 2000;9:137–148. [DOI] [PubMed] [Google Scholar]
- 16.Stroh G, Rosell T, Dong F, Forster J. Early liver transplantation for patients with acute alcoholic hepatitis: public views and the effects on organ donation. Am J Transplant 2015;15:1598–1604. [DOI] [PubMed] [Google Scholar]
- 17.Donckier V, Lucidi V, Gustot T, Moreno C. Ethical considerations regarding early liver transplantation in patients with severe alcoholic hepatitis not responding to medical therapy. J Hepatol 2014;60:866–871. [DOI] [PubMed] [Google Scholar]
- 18.Wong E, Mullins PD, Wallach J-P, Yoshida EM, Erb SR, Ford J-A, Scudamore CH, et al. Patients’ Perspectives on Early Liver Transplantation in Alcohol-Related Liver Disease. Hepatology Communications;0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crabb DW, Bataller R, Chalasani NP, Kamath PS, Lucey M, Mathurin P, McClain C, et al. Standard Definitions and Common Data Elements for Clinical Trials in Patients With Alcoholic Hepatitis: Recommendation From the NIAAA Alcoholic Hepatitis Consortia. Gastroenterology 2016;150:785–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deleuran T, Vilstrup H, Becker U, Jepsen P. Epidemiology of alcoholic liver disease in Denmark 2006–2011: a population-based study. Alcohol Alcohol 2015;50:352–357. [DOI] [PubMed] [Google Scholar]
- 21.Sahlman P, Nissinen M, Pukkala E, Farkkila M. Incidence, survival and cause-specific mortality in alcoholic liver disease: a population-based cohort study. Scand J Gastroenterol 2016;51:961–966. [DOI] [PubMed] [Google Scholar]
- 22.Sandahl TD, Jepsen P, Thomsen KL, Vilstrup H. Incidence and mortality of alcoholic hepatitis in Denmark 1999–2008: a nationwide population based cohort study. Journal of hepatology 2011;54:760–764. [DOI] [PubMed] [Google Scholar]
- 23.Asrani SK, Hall L, Leise MD, Devuni D, Korenblat KM. The changing epidemiology of alcoholic hepatitis: increasing incidence in the young, white, and women. Hepatology 2017;66:704A–704A. [Google Scholar]
- 24.Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ 2018;362:k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, Huang B, et al. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001–2002 to 2012–2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 2017;74:911–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singal AK, Bataller R, Ahn J, Kamath PS, Shah VH. ACG Clinical Guideline: Alcoholic Liver Disease. Am J Gastroenterol 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singal AK, Shah VH. Current trials and novel therapeutic targets for alcoholic hepatitis. J Hepatol 2019;70:305–313. [DOI] [PubMed] [Google Scholar]
- 28.Papastergiou V, Tsochatzis EA, Pieri G, Thalassinos E, Dhar A, Bruno S, Karatapanis S, et al. Nine scoring models for short-term mortality in alcoholic hepatitis: cross-validation in a biopsy-proven cohort. Aliment Pharmacol Ther 2014;39:721–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Forrest EH, Atkinson SR, Richardson P, Masson S, Ryder S, Thursz MR, Allison M, et al. Application of prognostic scores in the STOPAH trial: Discriminant function is no longer the optimal scoring system in alcoholic hepatitis. J Hepatol 2018;68:511–518. [DOI] [PubMed] [Google Scholar]
- 30.O’Leary JG, Reddy KR, Garcia-Tsao G, Biggins SW, Wong F, Fallon MB, Subramanian RM, et al. NACSELD acute-on-chronic liver failure (NACSELD-ACLF) score predicts 30-day survival in hospitalized patients with cirrhosis. Hepatology 2018;67:2367–2374. [DOI] [PubMed] [Google Scholar]
- 31.Choudhury A, Jindal A, Maiwall R, Sharma MK, Sharma BC, Pamecha V, Mahtab M, et al. Liver failure determines the outcome in patients of acute-on-chronic liver failure (ACLF): comparison of APASL ACLF research consortium (AARC) and CLIF-SOFA models. Hepatol Int 2017;11:461–471. [DOI] [PubMed] [Google Scholar]
- 32.Louvet ANS, Abdelnour M, Ramond MJ, Diaz E, Fartoux L, Dharancy S, Texier F, Hollebecque A, Serfaty L, Boleslawski E, Deltenre P, Canva V, Pruvot FR, Mathurin P. The Lille model: a new tool for therapeutic strategy in patients with severe alcoholic hepatitis treated with steroids. Hepatology 2007;45:1348–1354. [DOI] [PubMed] [Google Scholar]
- 33.Louvet A, Labreuche J, Artru F, Boursier J, Kim DJ, O’Grady J, Trepo E, et al. Combining Data From Liver Disease Scoring Systems Better Predicts Outcomes of Patients With Alcoholic Hepatitis. Gastroenterology 2015;149:398–406.e398; quiz e316–397. [DOI] [PubMed] [Google Scholar]
- 34.Kamath PS WR, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D’Amico G, Dickson ER, Kim WR. A model to predict survival in patients with end-stage liver disease. Hepatology 2001;33:464–470. [DOI] [PubMed] [Google Scholar]
- 35.Singal AK, Bashar H, Anand BS, Jampana SC, Singal V, Kuo YF. Outcomes after liver transplantation for alcoholic hepatitis are similar to alcoholic cirrhosis: exploratory analysis from the UNOS database. Hepatology 2012;55:1398–1405. [DOI] [PubMed] [Google Scholar]
- 36.Asrani SK, Saracino G, O’Leary JG, Gonzales S, Kim PT, McKenna GJ, Klintmalm G, et al. Recipient characteristics and morbidity and mortality after liver transplantation. J Hepatol 2018;69:43–50. [DOI] [PubMed] [Google Scholar]
- 37.Kim WR, Lake JR, Smith JM, Schladt DP, Skeans MA, Noreen SM, Robinson AM, et al. OPTN/SRTR 2017 Annual Data Report: Liver. Am J Transplant 2019;19 Suppl 2:184–283. [DOI] [PubMed] [Google Scholar]
- 38.Lee BP, Terrault NA. Early liver transplantation for severe alcoholic hepatitis: moving from controversy to consensus. Curr Opin Organ Transplant 2018;23:229–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dew MA, DiMartini AF, De Vito Dabbs A, Myaskovsky L, Steel J, Unruh M, Switzer GE, et al. Rates and risk factors for nonadherence to the medical regimen after adult solid organ transplantation. Transplantation 2007;83:858–873. [DOI] [PubMed] [Google Scholar]
- 40.Mathurin PMC, Samuel D, Dumortier J, Salleron J, Durand F, Castel H, Duhamel A, Pageaux GP, Leroy V, Dharancy S, Louvet A, Boleslawski E, Lucidi V, Gustot T, Francoz C, Letoublon C, Castaing D, Belghiti J, Donckier V, Pruvot FR, Duclos-Vallee JC. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med 2011;365:1790–1800. [DOI] [PubMed] [Google Scholar]
- 41.Brown RS. Transplantation for alcoholic hepatitis--time to rethink the 6-month “rule”. N Engl J Med 2011;365:1836–1838. [DOI] [PubMed] [Google Scholar]
- 42.Lee BP, Vittinghoff E, Hsu C, Han H, Therapondos G, Fix OK, Victor DW, et al. Predicting Low Risk for Sustained Alcohol Use After Early Liver Transplant for Acute Alcoholic Hepatitis: The Sustained Alcohol Use Post-Liver Transplant Score. Hepatology 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Starzl TE, Van Thiel D, Tzakis AG, Iwatsuki S, Todo S, Marsh JW, Koneru B, et al. Orthotopic liver transplantation for alcoholic cirrhosis. JAMA : the journal of the American Medical Association 1988;260:2542–2544. [PMC free article] [PubMed] [Google Scholar]
- 44.Marot A, Dubois M, Trepo E, Moreno C, Deltenre P. Liver transplantation for alcoholic hepatitis: A systematic review with meta-analysis. PLoS One 2018;13:e0190823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kodali S, Kaif M, Tariq R, Singal AK. Alcohol Relapse After Liver Transplantation for Alcoholic Cirrhosis-Impact on Liver Graft and Patient Survival: A Meta-analysis. Alcohol Alcohol 2018;53:166–172. [DOI] [PubMed] [Google Scholar]
- 46.Al-Saeedi M, Barout MH, Probst P, Khajeh E, Weiss KH, Diener MK, Mehrabi A. Meta-analysis of patient survival and rate of alcohol relapse in liver-transplanted patients for acute alcoholic hepatitis. Langenbecks Arch Surg 2018;403:825–836. [DOI] [PubMed] [Google Scholar]
- 47.Russ KB, Chen NW, Kamath PS, Shah VH, Kuo YF, Singal AK. Alcohol Use after Liver Transplantation is Independent of Liver Disease Etiology. Alcohol Alcohol 2016;51:698–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wells JT, Said A, Agni R, Tome S, Hughes S, Dureja P, Lucey MR. The impact of acute alcoholic hepatitis in the explanted recipient liver on outcome after liver transplantation. Liver Transpl 2007;13:1728–1735. [DOI] [PubMed] [Google Scholar]
- 49.McCallum S, Masterton G. Liver transplantation for alcoholic liver disease: a systematic review of psychosocial selection criteria. Alcohol Alcohol 2006;41:358–363. [DOI] [PubMed] [Google Scholar]
- 50.DiMartini A, Day N, Dew MA, Javed L, Fitzgerald MG, Jain A, Fung JJ, et al. Alcohol consumption patterns and predictors of use following liver transplantation for alcoholic liver disease. Liver Transpl 2006;12:813–820. [DOI] [PubMed] [Google Scholar]
- 51.De Gottardi A, Spahr L, Gelez P, Morard I, Mentha G, Guillaud O, Majno P, et al. A simple score for predicting alcohol relapse after liver transplantation: results from 387 patients over 15 years. Arch Intern Med 2007;167:1183–1188. [DOI] [PubMed] [Google Scholar]
- 52.Altamirano J, Bataller R. Alcoholic liver disease: pathogenesis and new targets for therapy. Nat Rev Gastroenterol Hepatol 2011;8:491–501. [DOI] [PubMed] [Google Scholar]
- 53.Lee BP, Vittinghoff E, Hsu C, Han H, Therapondos G, Fix OK, Victor DW, et al. Predicting Low Risk for Sustained Alcohol Use After Early Liver Transplant for Acute Alcoholic Hepatitis: The Sustained Alcohol Use Post-Liver Transplant Score. Hepatology 2019;69:1477–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.EASL Clinical Practice Guidelines: Management of alcohol-related liver disease. J Hepatol 2018. [DOI] [PubMed] [Google Scholar]
- 55.Bathgate AJ. Recommendations for alcohol-related liver disease. Lancet 2006;367:2045–2046. [DOI] [PubMed] [Google Scholar]


