Abstract
Background
Wnt-catenin signaling antagonists sclerostin and dickkopf-related protein-1 (Dkk-1) inhibit bone formation and are involved in the pathogenesis of postmenopausal osteoporosis (PO). However, the association between sclerostin and Dkk-1 and bone mineral density (BMD) in women with PO remains unclear.
Objective
This study aimed to determine the association between sclerostin and Dkk-1 and BMD, bone microarchitecture, and bone strength in PO.
Methods
Trabecular bone specimens were obtained from the femoral heads of 76 Chinese women with PO who underwent hip arthroplasty for femoral neck fractures. Micro-computed tomography (Micro-CT) was used to assess the BMD and bone microarchitecture of the trabecular bone. Subsequently, a mechanical test was performed. Finally, sclerostin and Dkk-1 in the bone were measured by enzyme-linked immunosorbent (Elisa) assay. Serum ionized serum ionised calcium, propeptide of type 1 collagen, C-terminal β-telopeptide of type-1 collagen, sclerostin, and Dkk-1 were also detected.
Results
Bone sclerostin was positively correlated with serum ionised calcium, serum sclerostin, BMD, bone volume/tissue volume (BV/TV), trabecular number (Tb.N), maximum compressive force, and yield strength (r = 0.32, 0.906, 0.355, 0.401, 0.329, 0.355, and 0.293, respectively, P < 0.05) and negatively correlated with age and trabecular separation (Tb.Sp) (r = − 0.755 and − 0.503, respectively, P < 0.05). Bone Dkk-1 was positively correlated with serum ionised calcium, serum Dkk-1, BMD, BV/TV, trabecular thickness, Tb.N, maximum compressive force, yield strength, and Young’s modulus (r = 0.38, 0.809, 0.293, 0.293, 0.228, 0.318, 0.352, 0.315, and 0.266, respectively, P < 0.05) and negatively correlated with age and Tb.Sp (r = − 0.56 and − 0.38, respectively, P < 0.05). Serum levels of sclerostin and Dkk-1 reflected the levels of sclerostin and Dkk-1 in the bone.
Conclusion
Bone sclerostin and Dkk-1 were positively correlated with BMD in women with PO, and higher levels of bone sclerostin and Dkk-1 might predict better BMD, bone microarchitecture, and bone strength. The potential molecular mechanisms still require further study.
Keywords: Sclerostin, Dickkopf-related protein-1, Postmenopausal osteoporosis, Bone mineral density, Bone microarchitecture, Bone strength
Background
Osteoporosis is a major bone metabolic disease characterized by low bone mass and deterioration of the bone microarchitecture, resulting in fragility and increased risk of fracture. Postmenopausal osteoporosis (PO), the most common type of osteoporosis, is mainly caused by imbalanced bone turnover, which is characterized by enhanced bone resorption exceeding bone formation following estrogen decline [1]. A large number of studies have reported the critical roles of osteoblasts and osteoclasts, which are the main executors of bone formation and bone resorption, respectively, in the pathogenesis of PO. Recent breakthrough studies highlighted the central role of osteocytes in bone remodeling and revealed that osteoblasts and osteoclasts are under the control of osteocytes [2, 3].
The canonical Wnt pathway plays a key role in determining the fate of mesenchymal stem cells, which favors the maturation and survival of osteoblasts [4]. In addition, the Wnt pathway promotes the expression of osteoprotegerin rather than RANKL, thus indirectly inhibiting osteoclast activity [5, 6]. The canonical Wnt pathway in the bone is mainly regulated by osteocytes, which act through the production of sclerostin and Dickkopf-related protein 1 (Dkk-1), [7–10]. By preventing the binding between Wnt and specific cell surface receptors (Frizzled and lipoprotein receptor-related protein 5/6), sclerostin and Dkk-1 block the activation of the Wnt canonical pathway; furthermore, β-catenin is sequestered and degraded in the absence of Wnt. Therefore, sclerostin and Dkk-1 are potent inhibitors of bone formation [4, 11, 12].
In vitro evidence has shown that estrogen inhibits the expression of sclerostin in osteocytes, mesenchymal stromal cells, and osteoblastic cells [13–15]. In addition, in vivo data from an ovariectomized mouse model and clinical population investigations indicated that sclerostin levels are negatively correlated with estrogen levels [16–18]. Conversely, sclerostin antibody has been shown to significantly increase bone mineral density (BMD) in women with PO [19–21]. Similarly, Dkk-1 antibody has been demonstrated to aid the recovery of bone formation in animal models [22]. In conclusion, sclerostin and Dkk-1 play pivotal roles in the pathogenesis of PO and have emerged as valuable treatment targets.
However, the association between sclerostin and Dkk-1 and BMD in postmenopausal women remains controversial. Reportedly, as blood sclerostin levels increase, BMD decreases in postmenopausal women, and postmenopausal women with significantly increased serum Dkk-1 exhibit more significant osteoporosis [23, 24]. Other studies have suggested paradoxical associations between circulating sclerostin and Dkk-1 and BMD, revealing that serum sclerostin and Dkk-1 are positively associated with BMD in women with PO [25–29].
Although sclerostin is mainly secreted by osteocytes, recent studies have demonstrated that other cells and tissues, including osteoblasts, vascular smooth muscle cells, and livers, are also sources of sclerostin [30, 31]; therefore, we speculated that the serum levels of sclerostin and Dkk-1 could not reflect those in the bone. Because sclerostin and Dkk-1 levels reported in most previous studies were measured in the serum, we measured sclerostin and Dkk-1 levels directly in the bone tissue and further elucidated the associations between bone sclerostin and Dkk-1 and BMD, bone microarchitecture, and bone strength.
Methods
Subjects
From January 1 to December 31, 2018, 76 postmenopausal women who underwent hip arthroplasty for femoral neck fracture were recruited for the present study (mean age, 74.66 ± 9.23 years; range, 56–92 years). All patients suffered from fracture due to falling (fragility fracture) and not violent trauma. Exclusion criteria were as follows: (1) presence of known metabolic or bone disorders that could affect bone metabolism and BMD, such as diabetes, parathyroid disease, and severe renal impairment; (2) presence of known joint diseases that could influence bone architecture and quality, such as osteoarthritis, rheumatoid arthritis, and congenital hip dysplasia; (3) receiving drugs that affect bone metabolism, such as hormones, steroids, diphosphate and calcitonin; and (4) hip surgery history.
Specimen preparation
The trabecular bone was obtained according to a previously reported method [32, 33]. Briefly, subchondral bone columns (15 mm in diameter and 30 mm in height) were extracted using a coring reamer at a position 15 mm outside the lateral edge of the fovea of the capitis femoris, and the axes of the specimens were perpendicular to the articular surface. The specimens were wrapped in gauze containing normal saline and stored at − 80 °C, which were prepared for mechanical testing and micro-CT scanning. Bone samples (0.05 g) from each specimen were obtained from the remaining trabecular bone in the femoral head and stored in protein lysate containing a protease inhibitor to prevent protein degradation.
Imaging
The specimens were positioned with gauze in the sample holder and allowed to reach room temperature. Densitometric and morphometric micro-CT analyses were performed after calibrated by SP-4004(Shysan Bruker, Belgium). The bone was analyzed using a Skyscan 1172 (Skyscan, Bruker, Belgium) with a 9-μm voxel size, 59 KVp, 127 uA, and 0.48 rotation steps. Cone-beam reconstruction software version 2.6, based on the Feldkamp algorithm, was used for three-dimensional reconstruction and data processing. The trabecular region of interest was 10 mm in diameter and 30 mm in height (to exclude the external compression part of the trabecular columns). The following parameters of the specimens were calculated: BMD (g/cm3), bone volume/tissue volume (BV/TV, %), trabecular thickness (Tb.Th, mm), trabecular number (Tb.N, 1/mm), and trabecular separation (Tb.Sp, mm).
Mechanical testing
A vertical compression test was performed to assess the mechanical properties of the trabecular bone after the micro-CT scan following after calibrated standard product from Sawbone. Briefly, the bone core was compressed in the inferosuperior direction between two platens at 2 mm/min on an Instron 5569 materials testing machine (Instron Inc., Norwood, MA, USA). Three parameters, including the maximum compression force (Mac, N), compressive strength (Cos, MPa), and Young’s modulus (Yom, MPa), were recorded.
Determination of sclerostin and Dkk-1 levels in the bone
Bone samples (0.05 g) were ground in liquid nitrogen. The bone powder was then lysed in a 1.5 mL tube (the volume of protein lysate in each tube was 1 mL) on a shaking table overnight at 4 °C. The next morning, protein lysate containing a protease inhibitor was added to each tube to ensure that the total volume of the solution in the tube was 1.5 mL. Sclerostin and Dkk-1 levels were measured by enzyme-linked immunosorbent assay (ELISA; R&D Systems, Minneapolis, MN, USA), following the manufacturer’s protocols. The sclerostin and Dkk-1 levels in the trabecular bone were calculated and expressed in μg/g (X μg sclerostin/X g trabecular bone and X ug Dkk-1/ X g trabecular bone).
Serum biochemistry
Serum was collected in the next morning after admission before the patients had breakfast. The markers were measured at the clinical laboratory of the Second Affiliated Hospital of Soochow University. Propeptide of type 1 collagen (P1NP) and C-terminal β-telopeptide of type-1 collagen (β-CTX) were measured using IDS-iSYS assays (Immunodiagnosis System Ltd., East Boldon, UK). Serum sclerostin (sensitivity:3.8 pg/L, specificity:natural and recombinant human SOST) and Dkk-1(sensitivity:0.948 pg/ml, specificity:natural and recombinant human Dkk-1) levels were measured with ELISA (R&D Systems), following the manufacturer’s protocols.
Statistical analysis
Statistical analysis was performed using SPSS ver.16.0 (SPSS, Chicago, IL, USA). The correlations among age, bone turnover markers, bone sclerostin and Dkk-1, bone microarchitecture, and bone strength were analyzed using Spearman’s rank correlation coefficient test. The level of statistical significance was established at P < 0.05 for all analyses.
Results
Descriptive statistical results
Descriptive statistical results are listed in Table 1. The levels of sclerostin and Dkk-1 in the trabecular bone of the femoral head of Chinese postmenopausal women were 57.54 ± 11.32 μg/g and 1.15 ± 0.38 μg/g, respectively.
Table 1.
Description statistical results
| Median (25th,75th percentile) | |
|---|---|
| Age(y) | 74.5 (68.00, 81.75) |
| calcium ion (uM) | 2.08 (1.99, 2.19) |
| P1NP(ug/L) | 47.2 (2.08, 2.20) |
| CTX (ug/L) | 516. 481.1 (281.25, 694.73) |
| Serum sclerostin (ug/L) | 1.02 (0.68, 1.64) |
| Serum DKK (ug/L) | 0.02 (0.16, 0.26) |
| Bone sclerostin (ug/g) | 58.53 (48.70, 67.00) |
| Bone DKK-1(ug/g) | 1.12 (0.95, 1.34) |
| BMD (g/cm3) | 0.64 (0.60, 0.68) |
| BV/TV (%) | 52.07 (48.04, 56.93) |
| Tb.Th (mm) | 0.30 (0.28, 0.32) |
| TB.N(1/mm) | 1.10 (0.97, 1.20) |
| Tb.SP (mm) | 0.60 (0.54, 0.69) |
| Mac(N) | 62.44 (59.45, 68.12) |
| Cos (Mpa) | 3.24 (2.99, 3.54) |
| Yom (Mpa) | 29,837 (27,893, 31,284) |
Association of serum sclerostin and Dkk-1 levels and bone sclerostin and Dkk-1 levels
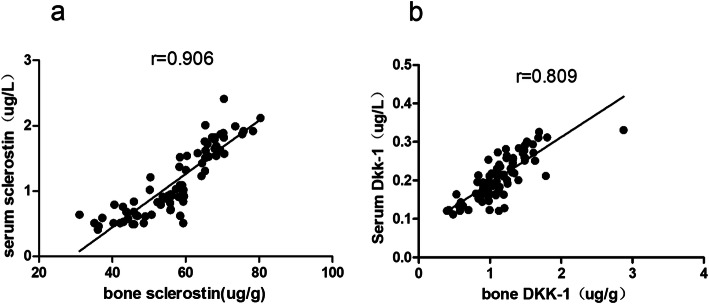
The serum level of sclerostin was positively correlated with bone sclerostin level (r = 0.906, P = 0.000, Fig. 1a), and serum levels of Dkk-1 were positively correlated with bone Dkk-1 level (r = 0.809, P = 0.000, Fig. 1b).
Fig. 1.
a The serum levels of sclerostin was positively correlated with bone sclerostin levels (P < 0.05). b The serum levels of Dkk-1 were positively correlated with bone Dkk-1 levels (P < 0.05)
Correlation of bone sclerostin and Dkk-1 with age, serum ionised calcium, P1NP, and β-CTX
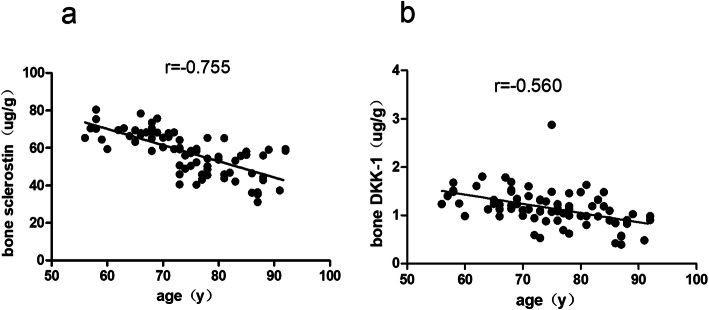
As shown in Table 2, age was negatively correlated with bone sclerostin (r = − 0.755, P = 0.000, Fig. 2a) and Dkk-1 (r = − 0.560, P = 0.000, Fig. 2b) levels. Serum ionised calciums were positively correlated with bone sclerostin (r = 0.320, P = 0.005) and Dkk-1 (r = 0.293, P = 0.01) levels. Although there was no significant association between P1NP and β-CTX and bone sclerostin and Dkk-1 (P > 0.05), bone Dkk-1 seemed to be negatively correlated with P1NP (P = 0.054).
Table 2.
Correlation of bone sclerostin and Dkk-1 between age, calcium ion, P1NP and CTX
| Sclerostin (ug/g) | Dkk-1(ug/g) | |||
|---|---|---|---|---|
| r | P | r | P | |
| Age(y) | −0.755 | < 0.05 | −0.560 | < 0.05 |
| Calcium ion (uM) | 0.320 | < 0.05 | 0.293 | < 0.05 |
| P1NP(ug/L) | 0.028 | > 0.05 | −0.222 | > 0.05 |
| CTX (ug/L) | 0.070 | > 0.05 | −0.074 | > 0.05 |
Fig. 2.
a-b Age was negatively correlated with bone sclerostin and bone Dkk-1 (P < 0.05)
Correlation of bone sclerostin and Dkk-1 with BMD, bone microarchitecture, and bone strength
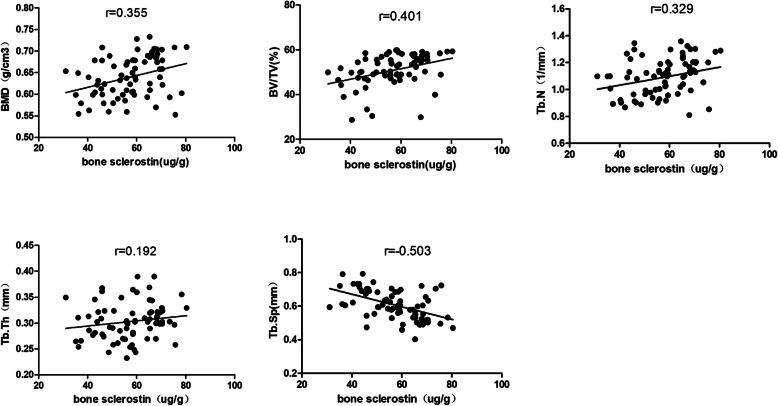
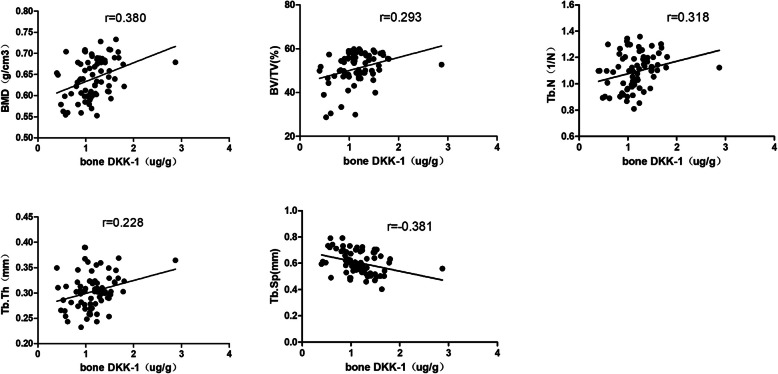
Micro-CT was performed on the trabecular bone from the femoral neck, and a representative three-dimensional reconstruction image is shown in Fig. 3. Bone sclerostin was positively correlated with BMD (r = 0.355, P = 0.002), BV/TV (r = 0.401, P = 0.000), Tb.N (r = 0.329, P = 0.004), Mac (r = 0.355, P = 0.002), and Cos (r = 0.293, P = 0.01) and negatively correlated with Tb.Sp (r = − 0.503, P = 0.000) (Fig. 4). Bone Dkk-1 was positively correlated with BMD (r = 0.293, P = 0.001), BV/TV(r = 0.293, P = 0.01), Tb.Th (r = 0.228, P = 0.048), and Tb.N (r = 0.318, P = 0.005), Mac (r = 0.352, P = 0.002), Cos (r = 0.315, P = 0.006), and Yom (r = 0.266, P = 0.02) and negatively correlated with Tb.Sp (r = -0.38, P = 0.01) (Fig. 5).
Fig. 3.
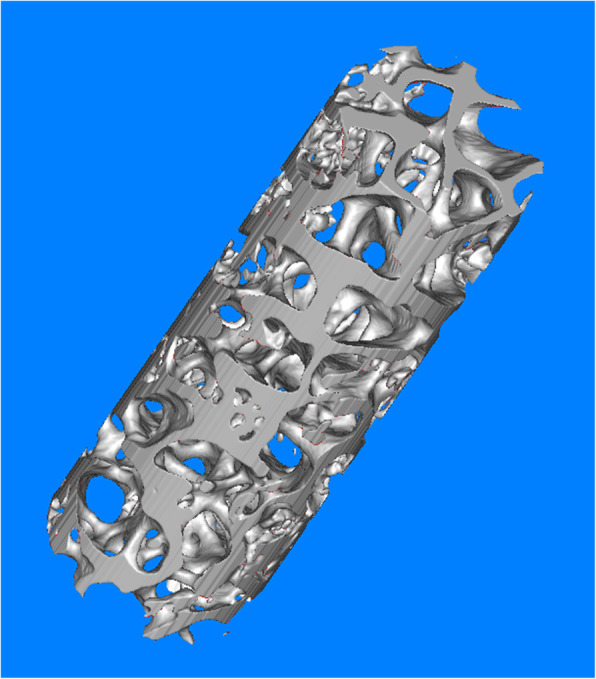
The representative Micro-CT picture of trabecular bone from femoral head
Fig. 4.
The correlationship of bone sclerostin and BMD, bone microarchitecture
Fig. 5.
The correlationship of bone Dkk-1 and BMD, bone microarchitecture
Correlation between bone sclerostin and Dkk-1 with bone strength
As shown in Table 3, the levels of bone sclerostin and Dkk-1 were positively correlated with the bone strength markers, including Mac, Cos, and Yom.
Table 3.
Correlation of bone sclerostin and Dkk-1 between BMD, bone microarchitecture and bone strength
| Sclerostin (ug/g) | Dkk-1(ug/g) | |||
|---|---|---|---|---|
| r | P | r | P | |
| Mac(N) | 0.355 | 0.05 | 0.352 | 0.05 |
| Cos (Mpa) | 0.293 | 0.05 | 0.315 | 0.05 |
| Yom (Mpa) | 0.194 | 0.05 | 0.266 | 0.05 |
Discussion
In this study, the levels of sclerostin and Dkk-1 in the trabecular bone were measured and were found to be positively correlated with BMD, bone microarchitecture, and bone strength. To our knowledge, this study is the first to report the bone protein levels of sclerostin and Dkk-1 in Chinese postmenopausal women and to show the association between protein levels of sclerostin, Dkk-1, and bone microarchitecture and bone strength.
Sclerostin and Dkk-1 are secreted primarily by osteocytes and inhibit bone formation by blocking the osteoblast Wnt/β-catenin signaling pathway [4]. Downregulation of sclerostin and Dkk-1 is associated with significantly increased bone formation. Moreover, it has been demonstrated in both animal models and clinical experiments that the administration of sclerostin antibody is markedly effective in the prevention of osteoporosis after the decrease in estrogen level [22, 34, 35]. In addition, estrogen has been shown to decrease sclerostin expression [13, 14, 18]. Therefore, based on the results of several studies, it is reasonable to expect that sclerostin and Dkk-1 would be inversely correlated with BMD in postmenopausal women. Although a previous study supported this notion that as blood sclerostin and Dkk-1 levels increased, BMD decreased in postmenopausal women, there is more evidence indicating that BMD is positively associated with sclerostin and Dkk-1 [23–29, 36, 37]. Most of these studies analyzed data on serum sclerostin, Dkk-1, and BMD measured by DXA. Considering serum sclerostin and Dkk-1 are also secreted by other cells and tissues, which might not reflect the levels of sclerostin and Dkk-1 in the bone, we measured the protein levels of sclerostin and Dkk-1 in the trabecular bone directly and assessed the local BMD by micro-CT. Our results demonstrated that the serum levels of sclerostin and Dkk-1 could reflect the bone levels of sclerostin and Dkk-1. Consistent with the results from the serum data, we found that the bone protein levels of sclerostin and Dkk-1 were positively associated with BMD. Moreover, these results were also supported by the mRNA levels of sclerostin and Dkk-1 reported by Jemtland et al. [38]. More importantly, the only study that reported the bone protein levels of sclerostin and Dkk-1, published recently, also demonstrated a positive relationship between bone sclerostin and Dkk-1 and BMD [39]. Compared with this study, one advantage of our study was that the specimens were kept in storage for a relatively short time, which could prevent the degradation of the protein levels of sclerostin and Dkk-1. Another paradoxical association discovered in our study was that protein levels of sclerostin and Dkk-1 were negatively associated with age; however, another study reported that serum sclerotin increased with age in men but not in women. We believe that the natural life of osteocytes after estrogen withdrawal and aging led to the paradoxical results mentioned above. Osteocytes constitute more than 90–95% of bone cells in the adult skeleton and are extremely long-lived cells that survive for up to decades in the bone matrix [40]. The life span of osteocytes is most likely determined by the rates of bone turnover, the process by which osteoclasts resorb the bone and osteoblasts replace the resorbed bone [3]. In postmenopausal women, as estrogen declines, bone turnover accelerates, which leads to the apoptosis of osteocytes [3]. It has been shown in bone samples from aged patients with hip fracture that the number of osteocytes and osteocyte activity decreased, whereas osteocyte apoptosis increased [41]. Therefore, a reasonable explanation for the positive correlation of bone sclerostin and Dkk-1 levels with BMD may be that these two proteins are mainly produced by live osteocytes and the number of live osteocytes decrease because of increased apoptosis. Consequently, sclerostin and Dkk-1 levels would reflect the number of osteocytes. From another perspective, when women with PO received teriparatide or denosumab treatment, BMD and sclerostin increased, which was accompanied by reduced bone turnover and increased osteocyte number [42, 43]. Conversely, the number of live osteocytes decreased significantly with age, which might have resulted in the reduced levels of bone sclerostin and Dkk-1.
In addition to BMD, we also evaluated bone microarchitecture and bone strength. Higher levels of sclerostin and Dkk-1 might predict better bone microarchitecture and bone strength. This finding was in accordance with that of Szulc et al., who reported that bone microarchitectural parameters are positively correlated with sclerostin in men [28]. Osteocyte number and activity play a crucial role in determining bone strength and microarchitecture. Ablation of osteocytes rapidly results in decreased bone strength and osteoporosis [44–46]. Hence, as sclerostin and Dkk-1 are mainly secreted by osteocytes, they could reflect the number and activity of osteocytes. Therefore, the bone levels of sclerostin and Dkk-1 could also reflect bone microarchitecture and strength.
However, this study has several limitations. First, no bone specimens were obtained from healthy women as a control group. Second, the number of patients enrolled in the study was relatively low. This might be the reason why we did not find any association between bone sclerosin and Dkk-1 and P1NP and β-CTX, whereas other studies, including a total of 100 patients, reported that serum sclerostin was negatively correlated with β-CTX and P1NP [27, 29]. Third, each patient lacked estrogen dectection, although we confirmed that every patient was postmenopausal according to the medical history; fourth, the patients enrolled in the study were all Chinese women, and our observations originating from bone specimens were consistent with the serum results that were also obtained from Chinese patients; therefore, the results might differ among different races [26, 29].
Conclusion
Based on the findings of previous studies and our research, bone sclerostin and Dkk-1 were positively correlated with BMD in Chinese women with PO, and higher levels of bone sclerostin and Dkk-1 might predict better BMD, bone microarchitecture, and bone strength. The potential molecular mechanisms still require further study.
Acknowledgements
Jia Peng and Zhang Dong contributed equally to this paper. And we were pleased to express our sincere thanks to Qi Jin.
Authors’ contributions
Jia Peng, Xu Yujia and Deng Lianfu designed the study and revised the paper. Jia Peng and Zhang Dong wrote the paper. Zhang Dong, Zhang Hui and Wang Aifei carried out the experiments, collected the data and analyzed the data. The authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (81803242, 81874018), China Postdoctoral Science Foundation (2017 M621820), Youth Medicine Talent of Suzhou, and Youth Medicine Talent of Second Affiliated Hospital of Soochow University (XKTJ-RC202012).
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author upon request.
Declarations
Ethics approval and consent to participate
All study procedures were approved by the ethical review board of the Second Affiliated Hospital of Soochow University (approval number: 2017-H-16) and performed in compliance with the Helsinki Declaration. Informed written consent was obtained from all individual participants and is available from the corresponding author upon request.
Consent for publication
Not applicable.
Competing interests
Jia Peng, Zhang Dong, Zhang Hui, Wang Aifei, Deng Lianfu, and Xu Youjia declare that there are no conflicts of interest regarding this manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jia Peng and Zhang Dong contributed equally to this work.
Contributor Information
Deng Lianfu, Email: lianfu_deng@163.com.
Xu Youjia, Email: xuyoujia@suda.edu.cn.
References
- 1.Jäckle K, Kolb JP, Schilling AF, Schlickewei C, Amling M, Rueger JM, Lehmann W. Analysis of low-dose estrogen on callus BMD as measured by pQCT in postmenopausal women. BMC Musculoskelet Disord. 2020;21(1):1. doi: 10.1186/s12891-020-03713-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bellido T. Osteocyte-driven bone remodeling. Calcif Tissue Int. 2014;94(1):25–34. doi: 10.1007/s00223-013-9774-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dallas SL, Prideaux M, Bonewald LF. The Osteocyte: an endocrine cell … and more. Endocr Rev. 2013;34(5):658–690. doi: 10.1210/er.2012-1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rossini M, Gatti D, Adami S. Involvement of WNT/beta-catenin signaling in the treatment of osteoporosis. Calcif Tissue Int. 2013;93(2):121–132. doi: 10.1007/s00223-013-9749-z. [DOI] [PubMed] [Google Scholar]
- 5.Spencer GJ, Utting JC, Etheridge SL, Arnett TR, Genever PG. Wnt signalling in osteoblasts regulates expression of the receptor activator of NFkappaB ligand and inhibits osteoclastogenesis in vitro. J Cell Sci. 2006;119(Pt 7):1283–1296. doi: 10.1242/jcs.02883. [DOI] [PubMed] [Google Scholar]
- 6.Glass DA, 2nd, Bialek P, Ahn JD, Starbuck M, Patel MS, Clevers H, Taketo MM, Long F, McMahon AP, Lang RA, et al. Canonical Wnt signaling in differentiated osteoblasts controls osteoclast differentiation. Dev Cell. 2005;8(5):751–764. doi: 10.1016/j.devcel.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 7.Spatz JM, Wein MN, Gooi JH, Qu Y, Garr JL, Liu S, Barry KJ, Uda Y, Lai F, Dedic C, et al. The Wnt inhibitor Sclerostin is up-regulated by mechanical unloading in osteocytes in vitro. J Biol Chem. 2015;290(27):16744–16758. doi: 10.1074/jbc.M114.628313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brunkow ME, Gardner JC, Van Ness J, Paeper BW, Kovacevich BR, Proll S, Skonier JE, Zhao L, Sabo PJ, Fu Y, et al. Bone dysplasia sclerosteosis results from loss of the SOST gene product, a novel cystine knot-containing protein. Am J Hum Genet. 2001;68(3):577–589. doi: 10.1086/318811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Winkler DG, Sutherland MK, Geoghegan JC, Yu C, Hayes T, Skonier JE, Shpektor D, Jonas M, Kovacevich BR, Staehling-Hampton K, et al. Osteocyte control of bone formation via sclerostin, a novel BMP antagonist. EMBO J. 2003;22(23):6267–6276. doi: 10.1093/emboj/cdg599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gifre L, Vidal J, Carrasco JL, Filella X, Ruiz-Gaspa S, Muxi A, Portell E, Monegal A, Guanabens N, Peris P. Effect of recent spinal cord injury on wnt signaling antagonists (sclerostin and dkk-1) and their relationship with bone loss. A 12-month prospective study. J Bone Miner Res. 2015;30(6):1014–1021. doi: 10.1002/jbmr.2423. [DOI] [PubMed] [Google Scholar]
- 11.Polyzos SA, Anastasilakis AD, Kountouras J, Makras P, Papatheodorou A, Kokkoris P, Sakellariou GT, Terpos E. Circulating sclerostin and Dickkopf-1 levels in patients with nonalcoholic fatty liver disease. J Bone Miner Metab. 2016;34(4):447–456. doi: 10.1007/s00774-015-0687-x. [DOI] [PubMed] [Google Scholar]
- 12.Tanaka S, Matsumoto T. Sclerostin: from bench to bedside. J Bone Miner Metab. 2021;39(3):332–40. [DOI] [PubMed]
- 13.Deepak V, Kayastha P, McNamara LM. Estrogen deficiency attenuates fluid flow-induced [Ca(2+)]i oscillations and mechanoresponsiveness of MLO-Y4 osteocytes. FASEB J. 2017;31(7):3027–3039. doi: 10.1096/fj.201601280R. [DOI] [PubMed] [Google Scholar]
- 14.Galea GL, Meakin LB, Sugiyama T, Zebda N, Sunters A, Taipaleenmaki H, Stein GS, van Wijnen AJ, Lanyon LE, Price JS. Estrogen receptor alpha mediates proliferation of osteoblastic cells stimulated by estrogen and mechanical strain, but their acute down-regulation of the Wnt antagonist Sost is mediated by estrogen receptor beta. J Biol Chem. 2013;288(13):9035–9048. doi: 10.1074/jbc.M112.405456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim RY, Yang HJ, Song YM, Kim IS, Hwang SJ. Estrogen modulates bone morphogenetic protein-induced Sclerostin expression through the Wnt signaling pathway. Tissue Eng Part A. 2015;21(13–14):2076–2088. doi: 10.1089/ten.tea.2014.0585. [DOI] [PubMed] [Google Scholar]
- 16.Mirza FS, Padhi ID, Raisz LG, Lorenzo JA. Serum sclerostin levels negatively correlate with parathyroid hormone levels and free estrogen index in postmenopausal women. J Clin Endocrinol Metab. 2010;95(4):1991–1997. doi: 10.1210/jc.2009-2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fujita K, Roforth MM, Demaray S, McGregor U, Kirmani S, McCready LK, Peterson JM, Drake MT, Monroe DG, Khosla S. Effects of estrogen on bone mRNA levels of sclerostin and other genes relevant to bone metabolism in postmenopausal women. J Clin Endocrinol Metab. 2014;99(1):E81–E88. doi: 10.1210/jc.2013-3249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim BJ, Bae SJ, Lee SY, Lee YS, Baek JE, Park SY, Lee SH, Koh JM, Kim GS. TNF-alpha mediates the stimulation of sclerostin expression in an estrogen-deficient condition. Biochem Biophys Res Commun. 2012;424(1):170–175. doi: 10.1016/j.bbrc.2012.06.100. [DOI] [PubMed] [Google Scholar]
- 19.Recker RR, Benson CT, Matsumoto T, Bolognese MA, Robins DA, Alam J, Chiang AY, Hu L, Krege JH, Sowa H, et al. A randomized, double-blind phase 2 clinical trial of blosozumab, a sclerostin antibody, in postmenopausal women with low bone mineral density. J Bone Miner Res. 2015;30(2):216–224. doi: 10.1002/jbmr.2351. [DOI] [PubMed] [Google Scholar]
- 20.Li X, Ominsky MS, Warmington KS, Morony S, Gong J, Cao J, Gao Y, Shalhoub V, Tipton B, Haldankar R, et al. Sclerostin antibody treatment increases bone formation, bone mass, and bone strength in a rat model of postmenopausal osteoporosis. J Bone Miner Res. 2009;24(4):578–588. doi: 10.1359/jbmr.081206. [DOI] [PubMed] [Google Scholar]
- 21.McClung MR, Grauer A, Boonen S, Bolognese MA, Brown JP, Diez-Perez A, Langdahl BL, Reginster JY, Zanchetta JR, Wasserman SM, et al. Romosozumab in postmenopausal women with low bone mineral density. N Engl J Med. 2014;370(5):412–420. doi: 10.1056/NEJMoa1305224. [DOI] [PubMed] [Google Scholar]
- 22.Florio M, Gunasekaran K, Stolina M, Li X, Liu L, Tipton B, Salimi-Moosavi H, Asuncion FJ, Li C, Sun B, et al. A bispecific antibody targeting sclerostin and DKK-1 promotes bone mass accrual and fracture repair. Nat Commun. 2016;7:11505. doi: 10.1038/ncomms11505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rossini M, Viapiana O, Idolazzi L, Ghellere F, Fracassi E, Troplini S, Povino MR, Kunnathully V, Adami S, Gatti D. Higher level of Dickkopf-1 is associated with low bone mineral density and higher prevalence of vertebral fractures in patients with Ankylosing spondylitis. Calcif Tissue Int. 2016;98(5):438–445. doi: 10.1007/s00223-015-0093-3. [DOI] [PubMed] [Google Scholar]
- 24.Kalem MN, Kalem Z, Akgun N, Bakirarar B. The relationship between postmenopausal women’s sclerostin levels and their bone density, age, body mass index, hormonal status, and smoking and consumption of coffee and dairy products. Arch Gynecol Obstet. 2017;295(3):785–793. doi: 10.1007/s00404-017-4288-x. [DOI] [PubMed] [Google Scholar]
- 25.Thorson S, Prasad T, Sheu Y, Danielson ME, Arasu A, Cummings SR, Cauley JA. Sclerostin and bone strength in women in their 10th decade of life. J Bone Miner Res. 2013;28(9):2008–2016. doi: 10.1002/jbmr.1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sheng Z, Tong D, Ou Y, Zhang H, Zhang Z, Li S, Zhou J, Zhang J, Liao E. Serum sclerostin levels were positively correlated with fat mass and bone mineral density in central south Chinese postmenopausal women. Clin Endocrinol. 2012;76(6):797–801. doi: 10.1111/j.1365-2265.2011.04315.x. [DOI] [PubMed] [Google Scholar]
- 27.Garnero P, Sornay-Rendu E, Munoz F, Borel O, Chapurlat RD. Association of serum sclerostin with bone mineral density, bone turnover, steroid and parathyroid hormones, and fracture risk in postmenopausal women: the OFELY study. Osteoporos Int. 2012;24(2):489–494. doi: 10.1007/s00198-012-1978-x. [DOI] [PubMed] [Google Scholar]
- 28.Szulc P, Boutroy S, Vilayphiou N, Schoppet M, Rauner M, Chapurlat R, Hamann C, Hofbauer LC. Correlates of bone microarchitectural parameters and serum sclerostin levels in men: the STRAMBO study. J Bone Miner Res. 2013;28(8):1760–1770. doi: 10.1002/jbmr.1888. [DOI] [PubMed] [Google Scholar]
- 29.He J, Zhang H, Wang C, Zhang Z, Yue H, Hu W, Gu J, Fu W, Hu Y, Li M, et al. Associations of serum sclerostin and polymorphisms in the SOST gene with bone mineral density and markers of bone metabolism in postmenopausal Chinese women. J Clin Endocrinol Metab. 2014;99(4):E665–E673. doi: 10.1210/jc.2013-2086. [DOI] [PubMed] [Google Scholar]
- 30.Weivoda MM, Youssef SJ, Oursler MJ. Sclerostin expression and functions beyond the osteocyte. Bone. 2017;96:45–50. doi: 10.1016/j.bone.2016.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martínez-Gil N, Roca-Ayats N, Cozar M, Garcia-Giralt N, Ovejero D, Nogués X, Grinberg D, Balcells S. Genetics and genomics of SOST: functional analysis of variants and genomic regulation in Osteoblasts. Int J Mol Sci. 2021;22(2):489. doi: 10.3390/ijms22020489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Okazaki N, Chiba K, Taguchi K, Nango N, Kubota S, Ito M, Osaki M. Trabecular microfractures in the femoral head with osteoporosis: analysis of microcallus formations by synchrotron radiation micro CT. Bone. 2014;64:82–87. doi: 10.1016/j.bone.2014.03.039. [DOI] [PubMed] [Google Scholar]
- 33.Tanck E, Bakker AD, Kregting S, Cornelissen B, Klein-Nulend J, Van Rietbergen B. Predictive value of femoral head heterogeneity for fracture risk. Bone. 2009;44(4):590–595. doi: 10.1016/j.bone.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 34.McColm J, Hu L, Womack T, Tang CC, Chiang AY. Single- and multiple-dose randomized studies of blosozumab, a monoclonal antibody against sclerostin, in healthy postmenopausal women. J Bone Miner Res. 2014;29(4):935–943. doi: 10.1002/jbmr.2092. [DOI] [PubMed] [Google Scholar]
- 35.Padhi D, Jang G, Stouch B, Fang L, Posvar E. Single-dose, placebo-controlled, randomized study of AMG 785, a sclerostin monoclonal antibody. J Bone Miner Res. 2011;26(1):19–26. doi: 10.1002/jbmr.173. [DOI] [PubMed] [Google Scholar]
- 36.Dovjak P, Dorfer S, Foger-Samwald U, Kudlacek S, Marculescu R, Pietschmann P. Serum levels of sclerostin and dickkopf-1: effects of age, gender and fracture status. Gerontology. 2014;60(6):493–501. doi: 10.1159/000358303. [DOI] [PubMed] [Google Scholar]
- 37.Ahmed SF, Fouda N, Abbas AA. Serum dickkopf-1 level in postmenopausal females: correlation with bone mineral density and serum biochemical markers. J Osteoporos. 2013;2013:460210. doi: 10.1155/2013/460210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jemtland R, Holden M, Reppe S, Olstad OK, Reinholt FP, Gautvik VT, Refvem H, Frigessi A, Houston B, Gautvik KM. Molecular disease map of bone characterizing the postmenopausal osteoporosis phenotype. J Bone Miner Res. 2011;26(8):1793–1801. doi: 10.1002/jbmr.396. [DOI] [PubMed] [Google Scholar]
- 39.Ueland T, Stilgren L, Bollerslev J. Bone matrix levels of Dickkopf and Sclerostin are positively correlated with bone mass and strength in postmenopausal Osteoporosis. Int J Mol Sci. 2019;20(12):2896. doi: 10.3390/ijms20122896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Manolagas SC, Parfitt AM. What old means to bone. Trends Endocrinol Metab. 2010;21(6):369–374. doi: 10.1016/j.tem.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lim Y, Kim CH, Lee S-Y, Kim H, Ahn SH, Lee SH, Koh J-M, Rhee Y, Baek KH, Min Y-K, et al. Decreased plasma levels of Sclerostin but not Dickkopf-1 are associated with an increased prevalence of osteoporotic fracture and lower bone mineral density in postmenopausal Korean women. Calcif Tissue Int. 2016;99(4):350–359. doi: 10.1007/s00223-016-0160-4. [DOI] [PubMed] [Google Scholar]
- 42.Polyzos SA, Anastasilakis AD, Bratengeier C, Woloszczuk W, Papatheodorou A, Terpos E. Serum sclerostin levels positively correlate with lumbar spinal bone mineral density in postmenopausal women--the six-month effect of risedronate and teriparatide. Osteoporos Int. 2012;23(3):1171–1176. doi: 10.1007/s00198-010-1525-6. [DOI] [PubMed] [Google Scholar]
- 43.Gatti D, Viapiana O, Fracassi E, Idolazzi L, Dartizio C, Povino MR, Adami S, Rossini M. Sclerostin and DKK1 in postmenopausal osteoporosis treated with denosumab. J Bone Miner Res. 2012;27(11):2259–2263. doi: 10.1002/jbmr.1681. [DOI] [PubMed] [Google Scholar]
- 44.Tatsumi S, Ishii K, Amizuka N, Li M, Kobayashi T, Kohno K, Ito M, Takeshita S, Ikeda K. Targeted ablation of osteocytes induces osteoporosis with defective mechanotransduction. Cell Metab. 2007;5(6):464–475. doi: 10.1016/j.cmet.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 45.O'Brien CA, Nakashima T, Takayanagi H. Osteocyte control of osteoclastogenesis. Bone. 2013;54(2):258–263. doi: 10.1016/j.bone.2012.08.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xiong J, Piemontese M, Thostenson JD, Weinstein RS, Manolagas SC, O'Brien CA. Osteocyte-derived RANKL is a critical mediator of the increased bone resorption caused by dietary calcium deficiency. Bone. 2014;66:146–154. doi: 10.1016/j.bone.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author upon request.