Abstract
Background:
Absenteeism is costly, yet evidence suggests that presenteeism—illness-related reduced productivity at work—is costlier. We quantified employed patients’ presenteeism and absenteeism before and after total joint arthroplasty (TJA).
Methods:
We measured presenteeism (0–100 scale, 100 full performance) and absenteeism using the World Health Organization’s Health and Work Performance Questionnaire before and after TJA among a convenience sample of employed patients. We captured detailed information about employment and job characteristics and evaluated how and among whom presenteeism and absenteeism improved.
Results:
In total, 636 primary, unilateral TJA patients responded to an enrollment email, confirmed employment, and completed a pre-operative survey (mean age: 62.1, 55.3% female). Full at-work performance was reported by 19.7%. Among 520 (81.8%) who responded to a one-year follow-up, 473 (91.0%) were still employed, and 461 (88.7%) had resumed working. Among patients reporting at baseline and one year, average at-work performance improved from 80.7 to 89.4. A Wilcoxon signed-rank test indicated that post-operative performance was significantly higher than pre-operative performance (p<0.0001). The percentage of patients who reported full at-work performance increased from 20.9% to 36.8% (delta=15.9%, 95%CI=[10.0%, 21.9%], p<0.0001). Presenteeism gains were concentrated among patients who reported declining work performance leading up to surgery. Average changes in absences were relatively small. Combined, the average monthly value lost by employers to presenteeism declined from 15.3% to 8.3% and to absenteeism from 16.9% to 15.5% (i.e., mitigated loss of 8.4% of monthly value).
Conclusion:
Among employed patients before TJA, presenteeism and absenteeism were similarly costly. After, employed patients reported increased performance, concentrated among those with declining performance leading up to surgery.
Keywords: presenteeism, absenteeism, return to work, performance, productivity, employment
Introduction
Illness can reduce worker effectiveness through absenteeism and presenteeism. Absenteeism refers to time spent away from work. Presenteeism refers to decreased productivity or performance at work because of illness (1). A cross-sectional study of randomly dialed US workers from 2001–2002 estimated that the lost value from absenteeism and presenteeism from health conditions was $225.8 billion per year, with more than 60% attributable to presenteeism (2). More recent evidence suggests presenteeism accounts for more economic loss than absenteeism (3),(4) across different occupations (5) and medical conditions (6),(7),(8).
Musculoskeletal conditions cost approximately $213 billion in direct and indirect costs in the US in 2011 (9) and accounted for the greatest proportion of lost productivity in the workplace (10). Several studies have shown increased presenteeism in patients with musculoskeletal conditions (4) such as arthritis,(1),(11),(12),(13),(14),(15) chronic knee pain,(16) and low back pain (17),(18). Although total joint arthroplasties (TJAs) are among the most common procedures (19),(20), little is known about their impact on worker performance.
Many orthopedic studies measuring work-related outcomes focus on return to work (21). Although existing evidence indicates TJA improves workplace performance,(22),(23),(24) to our knowledge, no existing study estimates the economic cost of presenteeism and absenteeism around TJA. One previous study investigated absenteeism and presenteeism six and 24 months after knee replacement, but not before surgery (25). Other studies have evaluated the impact of non-TJA musculoskeletal surgery on presenteeism (26),(27).
This study quantifies presenteeism and absenteeism among patients with advanced osteoarthritis of the hip and knee prior to primary, unilateral total hip or knee arthroplasty (THA or TKA) and evaluates time to return to work and changes in presenteeism and absenteeism among a convenience sample of employed patients six months and one year after surgery.
Materials and Methods
This prospective cohort study was based on a convenience sample of patients visiting one single high-volume urban musculoskeletal specialty hospital who were at least 18 years old, not retired, and scheduled to undergo primary unilateral THA or TKA with one of 40 surgeons between August 2017 and October 2018 (and willing to participate if eligible). Patients were emailed once 2–4 weeks before surgery, inviting them to provide consent online, confirm employment and eligibility, and complete a pre-operative survey (28),(29). We only attempted to enroll patients scheduled to undergo arthroplasty who were contactable through email (i.e., had a valid email address on file) with a single email outreach. We did not attempt to contact patients for enrollment in-person during any of their pre-surgical screening or other appointments, nor via telephone, nor letter, nor through repeated email requests. The resulting cohort of patients who responded to this single email invitation constituted the convenience sample. Patients were considered enrolled if they affirmed being employed and completed the online presenteeism questions before surgery. Patients receiving workers’ compensation were excluded. Enrolled patients were invited to complete follow-ups six and 12 months later. Patients who did not complete a follow-up were reminded twice, called, and, for 12 month follow-ups, mailed paper versions. The study was approved by our hospital’s Institutional Review Board.
Surveys
Presenteeism and absenteeism were measured using the World Health Organization’s Health and Work Performance Questionnaire (WHO-HPQ) (30),(31). Although systematic reviews have found no superior instrument,(12),(32) the WHO-HPQ was designed to work across a variety of job types (31) and health conditions (33) and has demonstrated validity, reliability, and sensitivity to measuring changes in presenteeism and absenteeism (30),(31),(34).
The presenteeism battery asked three questions on a scale of 0–10 (worst performance to top performance): “The usual performance of most workers in a job similar to yours?”, “Your usual job performance over the past year or two?”, and “Your overall job performance on the days you worked during the past 4 weeks?” We multiplied the third question by 10 to create an “absolute presenteeism” score, the percentage of time spent productively at work over the past four weeks (35). We also compared the second question to the third to gauge how presenteeism changed leading up to surgery.
The absenteeism battery asked about the past 28 days as well as the past seven. The former included questions about the number of workdays missed for personal health; for other reasons (e.g. vacation); and days worked early, late, or overtime. We added a question about work missed for family members’ health. The latter (7-day absenteeism) included questions about the number of hours expected to work and actually worked, from which we estimated hours absent from work per month. We added a question about the number of days expected to work per week.
We also asked about job status; job industry; main responsibilities at work; employer accommodations; commute to work; physical activities (including job requirements and general difficulty); and a single assessment numerical evaluation (SANE) of joint health. Follow-up surveys were identical to each other, asking about changes in employment status, and, if still employed, whether and when work was resumed. Presenteeism and absenteeism questions were also repeated.
Analyses
Baseline patient demographics and survey responses were summarized with descriptive statistics. Changes in employment status, and, among those still employed, the number who resumed working, and their average and median days to return, were calculated. Differences in days to return between THA and TKA patients were tested with a two-sided Wilcoxon rank-sum (Mann-Whitney) test.
Our primary outcome was change in absolute presenteeism between baseline and one year. We first evaluated its mean and distribution. Noting non-normality, we evaluated whether absolute presenteeism increased between baseline and one year with a Wilcoxon matched-paired signed-rank test. We also compared the percentage of participants who reported full (100/100) at-work performance at baseline and one year with a two-sided, two-sample test of proportions. We repeated these analyses between baseline and 6 months.
We stratified our analysis of changes in absolute presenteeism in two ways. First, we stratified between patients who reported (1) full (100/100) pre-operative at-work performance and (2) less than full pre-operative at-work performance, applying the same methods as above. We also analyzed which patient characteristics (age, sex, body mass index, race, ethnicity, type of joint replacement) and employment characteristics (employment status, job industry, main job responsibilities, job accommodations, commute, job involving various physical activities, and difficulty with various physical activities) were associated with reporting full pre-operative performance (dichotomous outcome) using multivariable linear regressions. Second, we stratified based on type of joint (hip or knee) and whether patients reported static (identical), declining, or improving performance leading up to surgery. We also analyzed which patient and employment characteristics were associated with reporting declining performance leading up to surgery (dichotomous outcome) using multivariable linear regressions.
We next detailed changes in 28-day and 7-day absenteeism, evaluating the mean and distribution of each relevant metric. However, once again, noting non-normality, we evaluated whether each metric changed with Wilcoxon matched-paired signed-rank tests.
Finally, we quantified the monthly average value an employer loses to presenteeism and absenteeism by combining the two measures to be on the same scale (in percentage terms). Following a human capital accounting approach,(4),(5),(36) for each patient we assumed that the percentage of time spent absent from scheduled work was lost to absenteeism (including time spent away because of own health, family health, and for other reasons including vacation), and the percentage of remaining time spent present but unproductive at work was lost to presenteeism. We performed these analyses at baseline and one year after surgery (among patients answering both and who were still employed and back to work) and reported how the associated average percentages changed.
All analyses were performed with Stata/SE version 14.2 for Windows.
Results
A single email inviting potential subjects to participate was sent to 4,233 patients. Among the resulting convenience sample of 958 patients who responded, 322 (33.6%) did not meet our enrollment criteria (Figure 1). An additional 47 originally met all enrollment criteria and filled out a baseline survey, but ended up delaying or cancelling their surgery; 39 either never rescheduled or did not re-take the survey before their new surgery (their responses were therefore dropped); 8 rescheduled and re-took the survey before their new surgery (only their final responses were counted). One participant took a baseline survey and met enrollment criteria but withdrew from the study. The remaining 636 patients enrolled in the study, among whom 482 (75.8%) responded at six-months, and 520 (81.8%) at one-year (Figure 1). Among enrolled patients, 325 underwent THA, and 311 underwent TKA.
Figure 1. Patient enrollment and follow-ups.
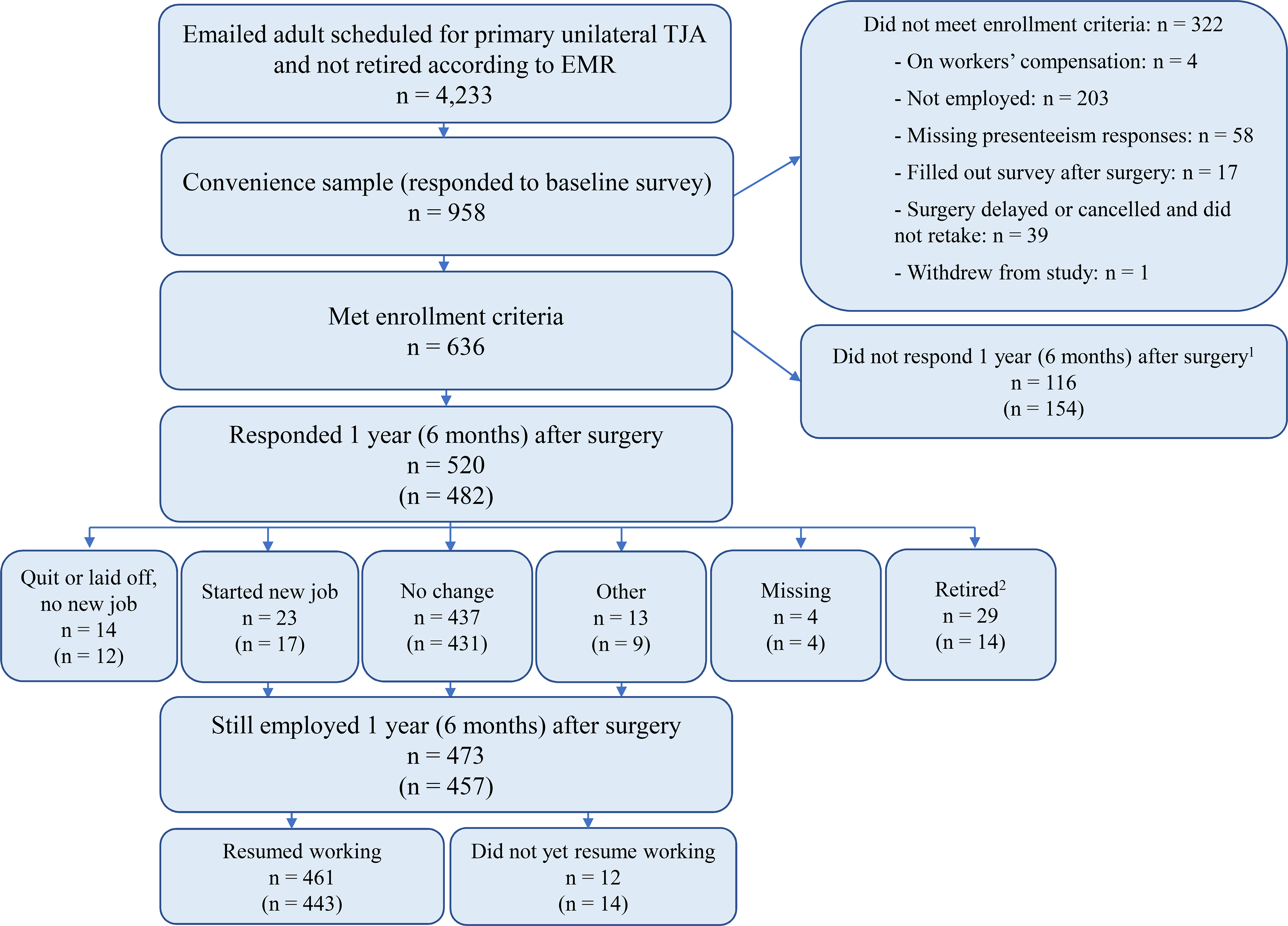
A single email was sent to 4,233 patients who were at least 18 years old, not retired according to our electronic medical record, and scheduled for primary unilateral TJA. Note that 39 patients (not included in the 636) filled out a baseline survey but ended up cancelling their surgery and either did not reschedule or did not re-take the baseline survey before their surgery. An additional 8 patients cancelled their original surgery but ended up rescheduling and filling out the baseline survey again (only their final responses were counted). One participant enrolled but subsequently withdrew from the study (not included in the 636). Footnote 1: n=123 completed neither follow-up; n=80 completely only the 1-year follow-up; n=73 completed only the 6-month follow-up; and n=360 completed both follow-ups.
Footnote 2: at 1 year n=10 retired before returning to work and n=19 retired after returning to work; and at 6 months n=4 retired before returning to work and n=10 retired after returning to work.
Before surgery, mean age was 62.1; a majority of patients were female (55.3%) and white (88.1%) (Table 1). Mean body mass index (BMI) was 29.9 kg/m2. In terms of employment, 73.1% reported full-time employment, 9.1% part-time, and 17.8% self-employed. Moreover, 19.5% reported some type of employer job accommodation. Before surgery, average at-work performance was 78.9/100 (median 80.0/100), and 19.7% reported full (100/100) at-work performance. Modal job industry and main job responsibilities reported were “Health Care and Social Assistance” (15.4%) and “Professional” (33.5%), respectively (Appendix Table 1). Patients reported having jobs that most consistently require standing, walking, and sitting (Appendix Table 2), and difficulty with squatting (Appendix Table 3).
Table 1.
Demographics and pre-surgical work characteristics
| Variable | Total Hip Arthroplasty | Total Knee Arthroplasty | Overall | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 325) | (n =311) | (n = 636) | ||||||||||
| Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max | |
| Age (years) | 61.1 | 8.8 | 29.0 | 85.0 | 63.2 | 7.3 | 43.0 | 83.0 | 62.1 | 8.2 | 29.0 | 85.0 |
| BMI (kg/m2) | 28.6 | 6.1 | 18.1 | 51.6 | 31.2 | 6.3 | 18.7 | 64.1 | 29.9 | 6.3 | 18.1 | 64.1 |
| SANE score * | 41.4 | 21.3 | 0.0 | 95.0 | 43.2 | 21.4 | 1.0 | 98.0 | 42.2 | 21.3 | 0.0 | 98.0 |
| Sex | Number (%) | Number (%) | Number (%) | |||||||||
| Female | 182 | 56.0% | 170 | 54.7% | 352 | 55.3% | ||||||
| Male | 143 | 44.0% | 141 | 45.3% | 284 | 44.7% | ||||||
| Race/Ethnicity | Number (%) | Number (%) | Number (%) | |||||||||
| Asian | 3 | 0.9% | 4 | 1.3% | 7 | 1.1% | ||||||
| Black | 17 | 5.2% | 9 | 2.9% | 26 | 4.1% | ||||||
| Hispanic | 8 | 2.5% | 8 | 2.6% | 16 | 2.5% | ||||||
| White | 281 | 86.5% | 279 | 89.7% | 560 | 88.1% | ||||||
| Other | 12 | 3.7% | 13 | 4.2% | 25 | 3.9% | ||||||
| Missing | 12 | 3.7% | 6 | 1.9% | 18 | 2.8% | ||||||
| Employment | Number (%) | Number (%) | Number (%) | |||||||||
| Yes, full-time | 237 | 72.9% | 228 | 73.3% | 465 | 73.1% | ||||||
| Yes, part-time | 30 | 9.2% | 28 | 9.0% | 58 | 9.1% | ||||||
| Self-employed | 58 | 17.8% | 55 | 17.7% | 113 | 17.8% | ||||||
| Job Accomodations | Number (%) | Number (%) | Number (%) | |||||||||
| Someone to help you out | 12 | 3.7% | 9 | 2.9% | 21 | 3.3% | ||||||
| Shorter work day | 5 | 1.5% | 5 | 1.6% | 10 | 1.6% | ||||||
| More breaks and rest periods | 7 | 2.2% | 9 | 2.9% | 16 | 2.5% | ||||||
| Special transportation | 5 | 1.5% | 2 | 0.6% | 7 | 1.1% | ||||||
| Special equipment | 11 | 3.4% | 5 | 1.6% | 16 | 2.5% | ||||||
| Change time to start and stop work | 21 | 6.5% | 21 | 6.8% | 42 | 6.6% | ||||||
| Change job to somehting you can do | 6 | 1.8% | 4 | 1.3% | 10 | 1.6% | ||||||
| Learn new skills | 1 | 0.3% | 1 | 0.3% | 2 | 0.3% | ||||||
| None | 234 | 72.0% | 231 | 74.3% | 465 | 73.1% | ||||||
| Missing | 23 | 7.1% | 24 | 7.7% | 47 | 7.4% | ||||||
|
Presenteeism (0: Worst, 10: Top) How would you rate the usual performance of… |
Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max |
| … most workers in a job similar to yours? | 8.00 | 1.49 | 3.00 | 10.00 | 7.93 | 1.63 | 0.00 | 10.00 | 7.96 | 1.56 | 0.00 | 10.00 |
| … your usual job performance over the past year or two? | 8.68 | 1.35 | 3.00 | 10.00 | 8.74 | 1.29 | 4.00 | 10.00 | 8.71 | 1.32 | 3.00 | 10.00 |
| … your overal job performance on the days you worked during the past 4 weeks (28 days)? | 7.78 | 2.03 | 0.00 | 10.00 | 7.99 | 1.99 | 0.00 | 10.00 | 7.89 | 2.01 | 0.00 | 10.00 |
|
Absenteeism (28-Day Recall) ** In the past 4 weeks (28 days), how many days did you. |
Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max |
| … miss work because of problems with your physical or mental health? | 1.61 | 4.30 | 0.00 | 28.00 | 1.16 | 3.65 | 0.00 | 28.00 | 1.39 | 4.00 | 0.00 | 28.00 |
| … miss work because of problems with a family member’s physical or mental health? | 0.31 | 1.12 | 0.00 | 10.00 | 0.16 | 0.80 | 0.00 | 10.00 | 0.24 | 1.02 | 0.00 | 10.00 |
| … miss work for any othe reason (including vacation)? | 2.00 | 3.70 | 0.00 | 28.00 | 2.20 | 4.30 | 0.00 | 28.00 | 2.10 | 4.00 | 0.00 | 28.00 |
| … come in early, go home late, work extra from home, or work on your day off? | 6.07 | 7.78 | 0.00 | 28.00 | 5.41 | 7.16 | 0.00 | 28.00 | 5.75 | 7.48 | 0.00 | 28.00 |
| Absenteeism (7-Day Recall) *** | Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max |
| How many days are you expected to work in a typical 7-day week? | 4.86 | 0.99 | 0.00 | 7.00 | 4.69 | 1.22 | 0.00 | 7.00 | 4.78 | 1.11 | 0.00 | 7.00 |
| How many hours does your employer expect you to work in a typical 7-day week? | 36.67 | 12.72 | 0.00 | 70.00 | 34.64 | 15.24 | 0.00 | 97.00 | 35.68 | 14.03 | 0.00 | 97.00 |
| About how many hours altogether did you work in the past 7 days? | 35.92 | 17.24 | 0.00 | 70.00 | 35.76 | 18.47 | 0.00 | 97.00 | 35.84 | 17.84 | 0.00 | 97.00 |
SANE = Single Assessment Numerical Evaluation, n=300, 285, 585
n=308, 292, 600
n=319, 306, 625
Among one-year respondents, 473 patients were still employed (91.0%), among whom 461 had resumed work. Patients reported returning to work on average 51.1±46.9 days after surgery (median 42 days), with a significant, meaningful difference between THA (mean 44.2±38.4 days, median 33.5 days) and TKA (mean 58.9±53.5 days, median 46.0 days) (p=0.0007).
Among patients who responded at both baseline and follow-up, mean at-work performance moved from 81.9 to 89.0 at six months and 80.7 to 89.4 at one year (Table 2). Both Wilcoxon signed-rank tests yielded p<0.0001, indicating significant increased performance between baseline and each follow-up. Among THA patients these mean numbers were 80.9 to 90.0 at six months and 79.9 to 89.4 at one year, and among TKA patients the numbers were 82.9 to 88.0 and 81.6 to 89.3 (Appendix Table 4). All Wilcoxon signed-rank tests yielded p<0.0001.
Table 2.
Statistical tests of changes in presenteeism and absenteeism at pairs of time points
| Presenteeism | Before Surgery to 6 Months After | Before Surgery to 1 Year After | ||||||||
| N | Mean Before | Mean After | Mean Δ | Rank P-value | N | Mean Before | Mean After | Mean Δ | Rank P-value | |
| Absolute Presenteeism, All Patients | 433 | 81.9 | 89.0 | 7.2 | <0.0001 | 440 | 80.7 | 89.4 | 8.7 | <0.0001 |
| Full Performance (Absolute Presenteeism = 100%) | 433 | 21.2% | 37.2% | 15.9% | <0.0001* | 440 | 20.9% | 36.8% | 15.9% | <0.0001* |
| Absolute Presenteeism, Before Surgery < 100% | 341 | 77.0 | 87.5 | 10.6 | <0.0001 | 348 | 75.6 | 88.1 | 12.5 | <0.0001 |
| Absolute Presenteeism, Before Surgery = 100% | 92 | 100.0 | 94.6 | −5.4 | <0.0001 | 92 | 100.0 | 94.1 | −5.9 | <0.0001 |
|
Absenteeism (28-Day Recall) In the past 4 weeks (28 days), how many days did you… |
Before Surgery to 6 Months After | Before Surgery to 1 Year After | ||||||||
| N | Mean Before | Mean After | Mean Δ | Rank P-value | N | Mean Before | Mean After | Mean Δ | Rank P-value | |
| … miss work because of problems with your physical or mental healt | 4101 | 0.86 | 0.43 | −0.43 | <0.0001 | 409 | 1.15 | 0.68 | −0.47 | <0.0001 |
| … miss work because of problems with a family member’s physical or mental health? | 401 | 0.28 | 0.26 | −0.02 | 0.7262 | 409 | 0.25 | 0.26 | 0.01 | 0.4032 |
| … miss work for any other reason (including vacation)? | 401 | 2.08 | 1.62 | −0.45 | 0.0074 | 409 | 2.08 | 2.40 | 0.33 | 0.0941 |
| … come in early, go home late, work extra from home, or work on your day off? | 399 | 5.99 | 5.41 | −0.58 | 0.2209 | 408 | 6.16 | 5.20 | −0.96 | 0.0829 |
| Absenteeism (7-Day Recall) | Before Surgery to 6 Months After | Before Surgery to 1 Year After | ||||||||
| N | Mean Before | Mean After | Mean Δ | Rank P-value | N | Mean Before | Mean After | Mean Δ | Rank P-value | |
| How many days are you expected to work in a typical 7-day week? | 418 | 4.83 | 4.76 | −0.07 | 0.4457 | 428 | 4.84 | 4.76 | −0.08 | 0.066 |
| How many hours does your employer expect you to work in a typical 7-day week? | 416 | 36.15 | 36.23 | 0.08 | 0.8225 | 425 | 35.83 | 35.91 | 0.08 | 0.3281 |
| About how many hours altogether did you work in the past 7 days? | 418 | 36.36 | 37.35 | 0.99 | 0.122 | 427 | 35.89 | 36.74 | 0.85 | 0.1458 |
| 7-Day Absenteeism Score (hours per month) | 416 | −1.38 | −4.62 | −3.25 | 0.2769 | 423 | −1.10 | −3.43 | −2.32 | 0.3991 |
Note: P-values are from Wilcoxon signed-rank tests, except those with an astericks, which are from two-sample test of proportions.
The overall proportion of patients who reported full performance increased from 21.2% at baseline to 37.2% at six months (delta=15.9%, 95% CI = [10.0%, 21.9%], p<0.0001) and from 20.9% to 36.8% at one year (delta = 15.9%, 95% CI = [10.0%, 21.8%], p<0.0001) (Table 2). Among THA patients these numbers were 21.0% to 42.0% (p<0.0001) at six months and 21.6% to 35.5% at one year (p<0.0001) (Appendix Table 4). Among TKA patients, they were 21.5% to 32.1% (p=0.0151) and 20.1% to 38.3% (p<0.0001) (Appendix Table 4).
Stratifying by pre-surgical performance, among patients who did not report 100/100 pre-surgical performance, mean performance moved from 77.0 to 87.5 at six months and from 75.6 to 88.1 at one year (Table 2). Both Wilcoxon signed-rank tests yielded p<0.0001, indicating significant increases in performance. Among patients who reported 100/100 pre-surgical performance, mean performance moved from 100 to 94.6 and from 100 to 94.1, respectively (Table 2). Both Wilcoxon signed-rank tests yielded p<0.0001, indicating decreases in performance at each time point. That said, among patients who reported 100/100 pre-surgical performance, 68.5% remained fully productive at one year.
Reporting full (100/100) performance before surgery was significantly associated with employment type, as well as lack of difficultly standing, lifting, and walking, but not with patient nor other employment characteristics. In particular, self-employed workers were 9.1% less likely than full-time employees to report full performance before surgery (95% CI = [−17.3%, −0.99%], p=0.028).
Moving on to performance leading up to surgery, 53.0% reported static performance in the year or two leading up to surgery; 5.0% reported improving performance; and 42.0% reported declining performance. Patients with declining performance leading up to surgery, undergoing THA and TKA procedures, reported average performance gains between baseline and one year from 68.7 to 88.9 (delta=20.2) and 70.1 to 89.5 (delta=19.3), respectively (Appendix Table 5). Both associated rank tests were significant (p<0.0001). Patients with static or improving performance leading up to surgery had more or less flat presenteeism between baseline and one year (with averages in the 80–90 range before and after surgery). This means that the overall gains in average performance were concentrated among those with declining productivity leading up to surgery. This is driven for the most part by their initially lower scores. These results generally held at six months: the overall average performance gains for patients with declining performance leading up to surgery were 17.2 and 14.1, for patients undergoing THA and TKA, respectively (Appendix Table 5).
Reporting declining performance leading up to surgery was associated with being younger; having a job that involves squatting, lifting, or walking; difficulty with all physical activities; and having job accommodations. In particular, while 37.2% of patients reporting no job accommodations had declining performance leading up to surgery, among those who reported job accommodations of “change time to start and stop work” or “someone to help you out” an additional 29.5% had declining performance leading up to surgery (95% CI = [14.1%, 44.8%], p<0.001 and 95% CI = [8.2%, 50.7%], p=0.007, respectively).
For 28-day absenteeism, between baseline and one year, average reported days missed because of one’s own health decreased (1.15 to 0.68 days per month), stayed nearly constant because of family’s health (0.25 to 0.26 days), increased for other reasons (2.08 to 2.40 days), and decreased for extra work (6.16 to 5.20 days) (Table 2). No average changes were large in magnitude. In fact, the first three components net approximately zero average change in absences. The exception was perhaps the decrease in average extra work (about one day per month); however, the Wilcoxon signed-rank test did not indicate the underlying distributional decrease was significant (p=0.0829). The associated test for problems with one’s own health did indicate decreased absenteeism along that dimension (p<0.0001). The other two Wilcoxon tests were not significant (p=0.4032 and 0.0941, respectively). Between baseline and 6 months results were similar, although there was additional evidence of decreased absenteeism because of other reasons including vacation (p<0.0001) (Table 2).
All 7-day absenteeism metrics stayed approximately the same on average between each pair of time points, with associated non-parametric tests indicating non-significant distributional changes (Table 2).
Finally, we turn to the average monthly value lost to presenteeism and absenteeism, combining the two measures to be on the same scale (in percentage terms). Among patients who had THA, before surgery, given the above estimates, an average 32.3% of monthly value was lost to absenteeism and presenteeism combined. Breaking this out, 16.4% was attributable to absenteeism and 15.9% was attributable to presenteeism (Figure 2). By one year, these numbers moved to 16.1% attributable to absenteeism and 7.7% to presenteeism. The mitigated losses were therefore, on average, 8.5% of monthly value. For patients who had TKA, results were similar. Before surgery, an average 32.0% was lost to absenteeism and presenteeism combined (with 17.4% attributable to absenteeism and 14.6% to presenteeism). By one year, these numbers moved to 14.7% and 9.0%, respectively, for an average mitigated loss of 8.4% of monthly value (Figure 3).
Figure 2. Monthly value lost before and after total hip arthroplasty.
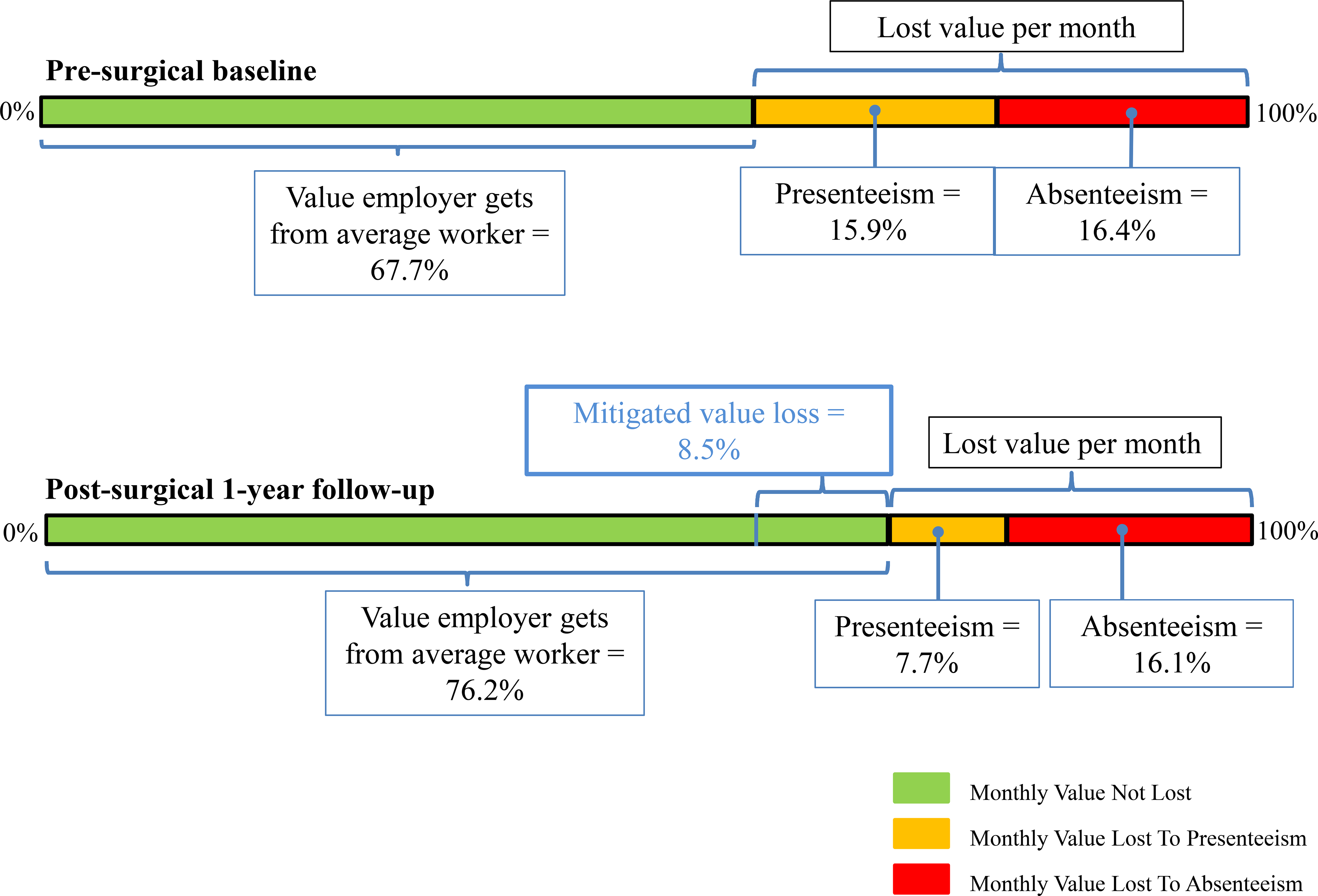
Shown is the average monthly value lost in percentage terms from absenteeism (red, assuming time absent because of personal health problems, family health problems, or other reasons including vacation is completely lost) and presenteeism (orange, assuming value of non-absent work is reduced proportionally) at both pre-surgical baseline (top) and post-surgical one-year follow-up (bottom). Green indicates the value not lost to absenteeism nor presenteeism per month. The green to the right of the blue line (below) indicates the monthly value loss mitigated after surgery, i.e., the combined reduction in absenteeism and presenteeism between baseline and one year.
Figure 3. Monthly value lost before and after total knee arthroplasty.
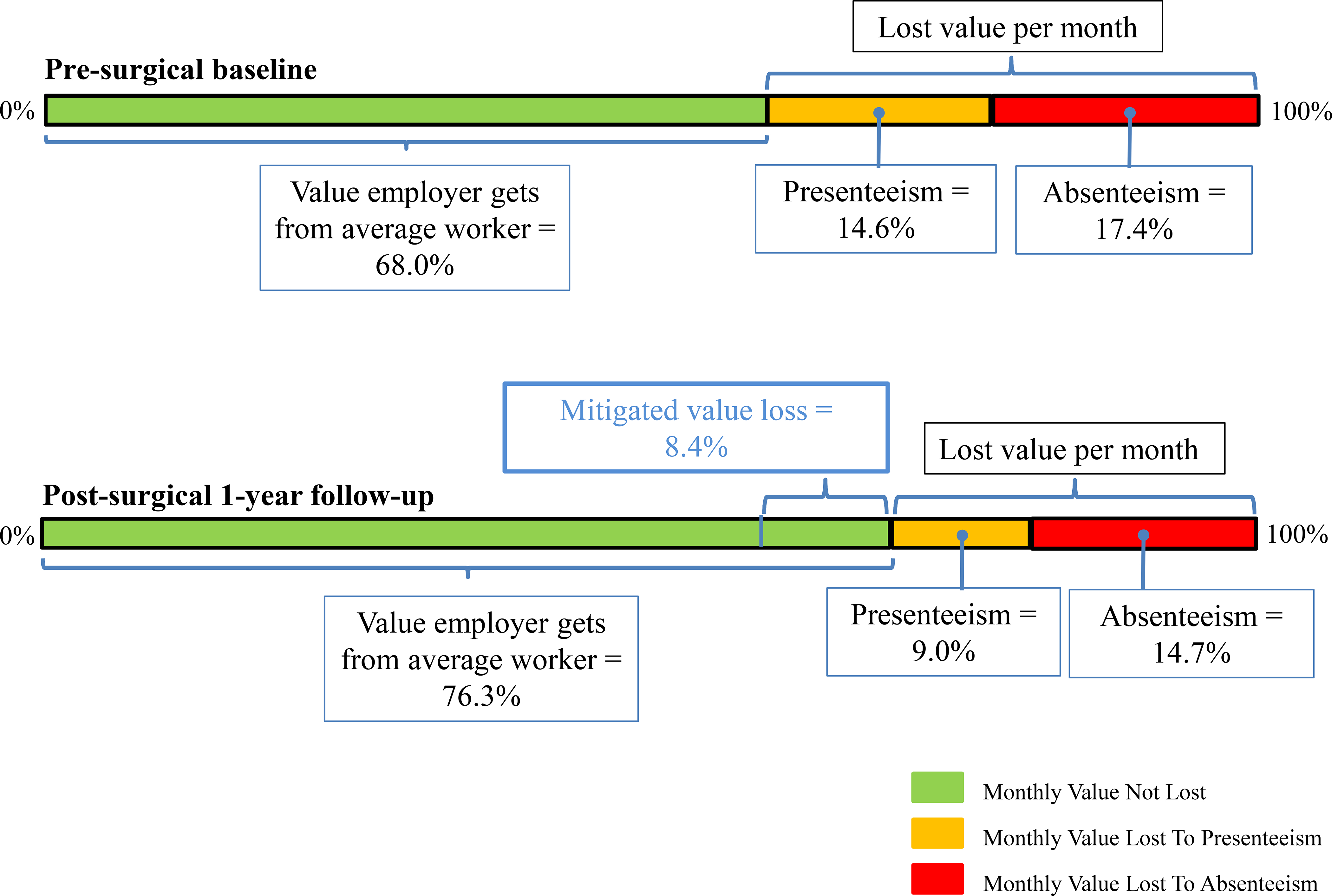
Shown is the average monthly value lost in percentage terms from absenteeism (red, assuming time absent because of personal health problems, family health problems, or other reasons including vacation is completely lost) and presenteeism (orange, assuming value of non-absent work is reduced proportionally) at both pre-surgical baseline (top) and post-surgical one-year follow-up (bottom). Green indicates the value not lost to absenteeism nor presenteeism per month. The green to the right of the blue line (below) indicates the monthly value loss mitigated after surgery, i.e., the combined reduction in absenteeism and presenteeism between baseline and one year.
Discussion
We demonstrated that patients reported substantial presenteeism (and to a lesser extent, absenteeism) before elective TJA. Our estimates were consistent with past, general reports of presenteeism being costly (3),(4), with the additional, key findings that (1) patients reported moderate ~10% average improvement in presenteeism one year after surgery and (2) the percentage reporting full performance increased from 21% to 37%. We also found that among patients who returned to work, those who had THA returned an average ~2 weeks sooner than those who had TKA. With respect to absenteeism, we found average changes between baseline and one year were small in magnitude (even if the underlying distributional changes were statistically significant), with the exception that patients reported working extra about one day less per month on average one year after surgery (although the underlying distributional change was not statistically significant).
Two related studies, measuring pre- and post-operative presenteeism around orthopedic procedures, involved hand surgery. One measured post-surgical improvement in presenteeism, but on a small, non-US sample (26), and another focused associations with six-month “work role functioning” (combining return to work and presenteeism) (27). For TJA, another study included 38 patients employed pre-operatively, which focused on return to work, but also reported that workplace performance increased by 27% (higher than our results), yet the exact instrument is not specified (23). Another study measured whether “performance at work [had] improved since the operation,” finding 63% of THA patients answered affirmatively, but their focus was on return to work, and they did not measure pre-operative performance (22).
The closest study to ours measured presenteeism and sick leave on 76 workers at six and 24 months after TKA (25). Although we did not measure 24-month outcomes, we collected pre-surgical outcomes, allowing assessment of improvements after surgery. Their study reported that workers were on average 81.6/100 productive six months after TKA, which is similar to our 88.0/100. Assuming a 40-hour work week (and four 5-day work weeks per month), their study reported on-average 0.3 days sick per month six months after TKA, which was similar to our 0.2 personal health days per month. At twelve months, we found 89.3/100 average performance and 0.6 days sick per month among TKAs. Their study did not report 12 month outcomes, but at 24 months they reported TKA workers were on average 85.8/100 productive and took 0.1 days sick per month. Differences in absenteeism likely reflect the fact that that many patients attend one-year but not two-year follow-up appointments.
More broadly, one paper (31), which does not focus on a population undergoing surgery, also reported absolute presenteeism using the WHO-HPQ among several professions: reservation agents, customer service agents, railroad engineers, and executives. For the latter group, which is most similar to our sample, the authors reported that 8.2% of participants report between 0–7 on the original 0–10 presenteeism scale, 80.0% reported 8–9, and 11.9% reported 10/10. For our sample, between baseline and one year, the percentage of patients moved from 29.8% to 8.2% reporting 0–7; from 49.4% to 55.0% reporting 8–9; and from 20.9% to 36.8% reporting 10. So, on the low end, our patient population went from reporting a much higher incidence of low at-work productivity to reporting a comparable rate. This is consistent with related work finding elevated absolute presenteeism on a population with arthritis (33), which is exactly what TJA is meant to alleviate. On the higher end, we had a lower percentage of patients reporting high-but-imperfect productivity, but a higher percentage reporting perfect productivity both before, and to an even greater extent, after surgery. This is consistent with these patients being actually more productive, or else being more optimistic in their self-reports.
In terms of stratified analyses, we found performance gains after surgery were almost entirely concentrated among patients who reported declining performance in the year leading up to surgery, which in turn was associated with being younger, certain physical activities, and job accommodations. Moreover, these patients had lower baseline at-work performance, so it is not surprising that, given greater room for improvement, they indeed improved more. An additional hypothesis is that patients with static or improving presenteeism before surgery had more stable OA, allowing them to learn how to work around their condition or adjust employment, and hence had better baseline work performance. This could also explain the relatively low levels of average absenteeism we reported, as well as the high percentage of patients with stable at-work performance leading up to surgery, and their lack of improvement. We are not aware of other research investigating declining work performance before surgery and its association with changes in outcomes.
Our study is also novel in its calculation of mitigated loss in value to an employer, given that once patients returned to work, they were more present and productive on average. Altogether, average improvements that we estimated one year after surgery represented approximately 8.4% of monthly value to an employer that would have otherwise been lost to presenteeism and absenteeism. Although employees might have the good fortune to retain their full salaries while off, it is important to acknowledge that employers likely do not reap any productivity or output gains until a patient returns to work. Even then, the impact may not be immediate (the soonest we measured was 6 months after surgery). From an employer’s perspective, there is therefore a sort of up-front “cost” in terms of an employee being out of work because of their surgery, but a medium- to long-term sustained benefit in terms of improved performance.
There were limitations to this study. First, it was based on a convenience sample from a single high-volume institution located in a large urban setting. As such, it is likely that enrolled patients were not representative of employed patients undergoing TJA broadly. However, we are aware of no other study reporting this information about patients before and after TJA. Future work would benefit from conducting a representative study of TJA patients. Second, we measured presenteeism and absenteeism with self-reported surveys, which are subject to recall bias and misreporting. It would be ideal to get absenteeism and performance reports directly from employers, but this would have been infeasible. We also did not account for “frictions” incurred by employers, such as resources spent temporarily replacing a patient, or the opportunity cost of their colleagues’ time in terms of taking over work. To the extent that patients’ work can be handled seamlessly while absent, it is also possible that our value calculations may be inflated from an employer’s perspective (37). We also did not measure patients’ work-related benefits (beyond excluding workers’ compensation recipients), which may affect absenteeism and presenteeism, and would be necessary to better appraise the impact of these phenomena on patients. Next, for 28-day absenteeism, it was unclear how to compare days absent from work with days working extra; one day working extra does not necessarily offset one day of absence. It was therefore not possible for us to evaluate the extent to which extra work might “compensate” for absences or reduced performance, nor how this changed over time. This led us to omit working extra days from the absenteeism component of our value calculations, which means the relative cost of absenteeism at each time point was likely inflated. Future studies should endeavor to ask how much extra patients work, not just the number of days they do so. We also did not know patients’ salaries, so made calculations of lost value in percentage terms; this allowed us to combine absenteeism and presenteeism on the same scale, although not in dollars, which would have been ideal. Moreover, we did not explicitly account for whether patients had post-operative complications impacting their ability to work. However, these were implicitly factored into our calculations, given complications would have impacted how patients responded to follow-up absenteeism and presenteeism questions. But, we cannot say exactly how this subset of patients were affected. We also did not measure nor account for other painful joints (beside the one being operated on) nor back pain, which would likely be consequential for presenteeism and absenteeism. Finally, our sample was restricted to patients undergoing unilateral TJAs; patients undergoing bilateral total joint arthroplasty, revision arthroplasty, or other orthopedic procedures could differ, and further research is warranted to investigate how.
In conclusion, this is the first study to demonstrate how presenteeism and absenteeism among employed patients changed after TJA. Presenteeism and absenteeism were similarly costly in terms of average monthly value lost to employers among patients before having TJA. Patients reported significantly increased average work performance six months and one year after surgery, concentrated among patients whose self-reported performance declined leading up to surgery. Although some measures of absenteeism significantly changed, the associated magnitudes were small; changes in presenteeism were more consequential.
Supplementary Material
Highlights.
We measured presenteeism and absenteeism among employed patients before and 1 year after total joint replacement
Presenteeism is illness-related reduced at-work productivity or performance
Average at-work performance moved from 80.7 to 89.4 (of 100); the percentage reporting 100/100 moved from 20.9% to 36.8%
Average changes in absences were relatively small
Altogether, average improvements represented mitigated losses to an employer of 8.4% of an employee’s monthly value
Acknowledgments
Study data were collected and managed using REDCap electronic data capture tools hosted at Weill Cornell Medicine with support from Clinical and Translational Science Center grant, UL1TR002384.
Appendix Table 1.
Job characteristics before surgery
| Characteristic | Overall | Total Hip Arthroplasty | Total Knee Arthroplasty | |||
|---|---|---|---|---|---|---|
| (n = 636) | (n = 325) | (n = 311) | ||||
| What sector best describes your current job? | Number (%) | Number (%) | Number (%) | |||
| Agriculture, Forestry, Fishing, and Hunting | 1 | 0.2% | 1 | 0.3% | 0 | 0.0% |
| Utilities | 4 | 0.6% | 3 | 0.9% | 1 | 0.3% |
| Construction | 21 | 3.3% | 10 | 3.1% | 11 | 3.5% |
| Manufacturing | 9 | 1.4% | 4 | 1.2% | 5 | 1.6% |
| Wholesale Trade | 7 | 1.1% | 2 | 0.6% | 5 | 1.6% |
| Retail Trade | 12 | 1.9% | 6 | 1.8% | 6 | 1.9% |
| Transportation and Warehousing | 6 | 0.9% | 3 | 0.9% | 3 | 1.0% |
| Information | 7 | 1.1% | 4 | 1.2% | 3 | 1.0% |
| Finance and Insurance | 74 | 11.6% | 32 | 9.8% | 42 | 13.5% |
| Real Estate and Rental and Leasing | 21 | 3.3% | 10 | 3.1% | 11 | 3.5% |
| Professional, Scientific, and Technical Services | 87 | 13.7% | 50 | 15.4% | 37 | 11.9% |
| Management of Companies and Enterprises | 23 | 3.6% | 13 | 4.0% | 10 | 3.2% |
| Administrative and Support and Waste Management and Remediation Services | 5 | 0.8% | 1 | 0.3% | 4 | 1.3% |
| Educational Services | 82 | 12.9% | 46 | 14.2% | 36 | 11.6% |
| Health Care and Social Assistance | 98 | 15.4% | 48 | 14.8% | 50 | 16.1% |
| Arts, Entertainment, and Recreation | 32 | 5.0% | 20 | 6.2% | 12 | 3.9% |
| Accommodation and Food Services | 5 | 0.8% | 3 | 0.9% | 2 | 0.6% |
| Other Services (except Public Administration) | 7 | 1.1% | 4 | 1.2% | 3 | 1.0% |
| Public Administration | 10 | 1.6% | 3 | 0.9% | 7 | 2.3% |
| Other | 81 | 12.7% | 40 | 12.3% | 41 | 13.2% |
| Missing | 44 | 6.9% | 22 | 6.8% | 22 | 7.1% |
| Which category best describes your main job? | Number (%) | Number (%) | Number (%) | |||
| Executive, administrator, or senior manager (e.g. CEO, sales VP, plant manager) | 167 | 26.3% | 83 | 25.5% | 84 | 27.0% |
| Professional (e.g. engineer, accountant, systems analyst) | 213 | 33.5% | 122 | 37.5% | 91 | 29.3% |
| Technical support (e.g. lab technician, legal assistant, computer programmer) | 8 | 1.3% | 5 | 1.5% | 3 | 1.0% |
| Sales (e.g. sales representative, stockbroker, retail sales) | 46 | 7.2% | 24 | 7.4% | 22 | 7.1% |
| Clerical and administrative support (e.g. secretary, billing clerk, officer supervisor) | 36 | 5.7% | 15 | 4.6% | 21 | 6.8% |
| Service occupation (e.g. security officer, food service worker, janitor) | 13 | 2.0% | 7 | 2.2% | 6 | 1.9% |
| Precision production and crafts worker (e.g. mechanic, carpenter, machinist) | 14 | 2.2% | 8 | 2.5% | 6 | 1.9% |
| Operator or laborer (e.g. assembly line worker, truck driver, construction worker) | 10 | 1.6% | 2 | 0.6% | 8 | 2.6% |
| Other | 85 | 13.4% | 37 | 11.4% | 48 | 15.4% |
| Missing | 44 | 6.9% | 22 | 6.8% | 22 | 7.1% |
| How do you get to work? | Number (%) | Number (%) | Number (%) | |||
| Bike | 4 | 0.6% | 3 | 0.9% | 1 | 0.3% |
| Drive | 334 | 52.5% | 164 | 50.5% | 170 | 54.7% |
| Public Transportation | 117 | 18.4% | 56 | 17.2% | 61 | 19.6% |
| Taxi | 17 | 2.7% | 12 | 3.7% | 5 | 1.6% |
| Walk | 22 | 3.5% | 15 | 4.6% | 7 | 2.3% |
| Work from home | 85 | 13.4% | 46 | 14.2% | 39 | 12.5% |
| Other | 12 | 1.9% | 7 | 2.2% | 5 | 1.6% |
| Missing | 45 | 14.5% | 22 | 6.8% | 23 | 7.4% |
NAICS = North American Industry Classification System
Appendix Table 2.
Frequency of job involving different physical activities
| How often does your job involve… | Overall (n=636) | |||||||||||
| Always | Often | Sometimes | Seldom | Never | Missing | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Squatting | 17 | 2.7% | 38 | 6.0% | 97 | 15.3% | 149 | 23.4% | 273 | 42.9% | 62 | 9.7% |
| Standing | 113 | 17.8% | 198 | 31.1% | 184 | 28.9% | 52 | 8.2% | 37 | 5.8% | 52 | 8.2% |
| Lifting | 21 | 3.3% | 47 | 7.4% | 130 | 20.4% | 186 | 29.2% | 181 | 28.5% | 71 | 11.2% |
| Walking | 157 | 24.7% | 204 | 32.1% | 148 | 23.3% | 39 | 6.1% | 33 | 5.2% | 55 | 8.6% |
| Sitting | 247 | 38.8% | 246 | 38.7% | 63 | 9.9% | 23 | 3.6% | 5 | 0.8% | 52 | 8.2% |
| How often does your job involve… | Total Hip Arthroplasty (n=325) | |||||||||||
| Always | Often | Sometimes | Seldom | Never | Missing | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Squatting | 10 | 3.1% | 18 | 5.5% | 53 | 16.3% | 80 | 24.6% | 136 | 41.8% | 28 | 8.6% |
| Standing | 59 | 18.2% | 111 | 34.2% | 92 | 28.3% | 23 | 7.1% | 15 | 4.6% | 25 | 7.7% |
| Lifting | 12 | 3.7% | 23 | 7.1% | 71 | 21.8% | 92 | 28.3% | 95 | 29.2% | 32 | 9.8% |
| Walking | 87 | 26.8% | 101 | 31.1% | 78 | 24.0% | 16 | 4.9% | 17 | 5.2% | 26 | 8.0% |
| Sitting | 132 | 40.6% | 124 | 38.2% | 32 | 9.8% | 9 | 2.8% | 4 | 1.2% | 24 | 7.4% |
| How often does your job involve… | Total Knee Arthroplasty (n=311) | |||||||||||
| Always | Often | Sometimes | Seldom | Never | Missing | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Squatting | 7 | 2.2% | 20 | 6.2% | 44 | 13.5% | 69 | 21.2% | 137 | 42.2% | 34 | 10.5% |
| Standing | 54 | 16.6% | 87 | 26.8% | 92 | 28.3% | 29 | 8.9% | 22 | 6.8% | 27 | 8.3% |
| Lifting | 9 | 2.8% | 24 | 7.4% | 59 | 18.2% | 94 | 28.9% | 86 | 26.5% | 39 | 12.0% |
| Walking | 70 | 21.5% | 103 | 31.7% | 70 | 21.5% | 23 | 7.1% | 16 | 4.9% | 29 | 8.9% |
| Sitting | 115 | 35.4% | 122 | 37.5% | 31 | 9.5% | 14 | 4.3% | 1 | 0.3% | 28 | 8.6% |
Appendix Table 3.
Difficulty with different physical activities
| How much difficulty do you have with… | Overall (n=636) | |||||||||||||
| Extreme | A lot | Moderate | A little | None | Does not apply | Missing | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Squatting | 257 | 40.4% | 141 | 22.2% | 87 | 13.7% | 34 | 5.3% | 10 | 1.6% | 51 | 8.0% | 56 | 8.8% |
| Standing | 27 | 4.2% | 113 | 17.8% | 177 | 27.8% | 166 | 26.1% | 94 | 14.8% | 4 | 0.6% | 55 | 8.6% |
| Lifting | 55 | 8.6% | 104 | 16.4% | 136 | 21.4% | 146 | 23.0% | 79 | 12.4% | 54 | 8.5% | 62 | 9.7% |
| Walking | 60 | 9.4% | 154 | 24.2% | 205 | 32.2% | 124 | 19.5% | 33 | 5.2% | 4 | 0.6% | 56 | 8.8% |
| Sitting | 17 | 2.7% | 48 | 7.5% | 127 | 20.0% | 138 | 21.7% | 245 | 38.5% | 7 | 1.1% | 54 | 8.5% |
| How much difficulty do you have with… | Total Hip Arthroplasty (n=325) | |||||||||||||
| Extreme | A lot | Moderate | A little | None | Does not apply | Missing | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Squatting | 122 | 37.5% | 71 | 21.8% | 53 | 16.3% | 18 | 5.5% | 3 | 0.9% | 29 | 8.9% | 29 | 8.9% |
| Standing | 12 | 3.7% | 55 | 16.9% | 99 | 30.5% | 75 | 23.1% | 53 | 16.3% | 2 | 0.6% | 29 | 8.9% |
| Lifting | 38 | 11.7% | 65 | 20.0% | 65 | 20.0% | 61 | 18.8% | 34 | 10.5% | 31 | 9.5% | 31 | 9.5% |
| Walking | 33 | 10.2% | 88 | 27.1% | 111 | 34.2% | 53 | 16.3% | 10 | 3.1% | 2 | 0.6% | 28 | 8.6% |
| Sitting | 13 | 4.0% | 32 | 9.8% | 84 | 25.8% | 74 | 22.8% | 90 | 27.7% | 4 | 1.2% | 28 | 8.6% |
| How much difficulty do you have with… | Total Knee Arthroplasty (n=311) | |||||||||||||
| Extreme | A lot | Moderate | A little | None | Does not apply | Missing | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Squatting | 135 | 41.5% | 70 | 21.5% | 34 | 10.5% | 16 | 4.9% | 7 | 2.2% | 22 | 6.8% | 27 | 8.3% |
| Standing | 15 | 4.6% | 58 | 17.8% | 78 | 24.0% | 91 | 28.0% | 41 | 12.6% | 2 | 0.6% | 26 | 8.0% |
| Lifting | 17 | 5.2% | 39 | 12.0% | 71 | 21.8% | 85 | 26.2% | 45 | 13.8% | 23 | 7.1% | 31 | 9.5% |
| Walking | 27 | 8.3% | 66 | 20.3% | 94 | 28.9% | 71 | 21.8% | 23 | 7.1% | 2 | 0.6% | 28 | 8.6% |
| Sitting | 4 | 1.2% | 16 | 4.9% | 43 | 13.2% | 64 | 19.7% | 155 | 47.7% | 3 | 0.9% | 26 | 8.0% |
Appendix Table 4.
Statistical tests of changes in presenteeism and absenteeism at pairs of time points, stratified by joint
| Total Hip Arthroplasty | ||||||||||
| Presenteeism | Before Surgery to 6 Months After | Before Surgery to 1 Year After | ||||||||
| N | Mean Before | Mean After | Mean Δ | Rank P-value | N | Mean Before | Mean After | Mean Δ | Rank P-value | |
| Absolute Presenteeism, All Patients | 224 | 80.9 | 90.0 | 9.0 | <0.0001 | 231 | 79.9 | 89.4 | 9.5 | <0.0001 |
| Full Performance (Absolute Presenteeism = 100%) | 224 | 21.0% | 42.0% | 21.0% | <0.0001* | 231 | 21.6% | 35.5% | 0.1 | 0.001* |
| Absolute Presenteeism, Before Surgery < 100% | 177 | 75.9 | 88.0 | 12.1 | <0.0001 | 181 | 74.4 | 88.8 | 14.4 | <0.0001 |
| Absolute Presenteeism, Before Surgery = 100% | 47 | 100.0 | 97.2 | −2.8 | 0.0003 | 50 | 100.0 | 91.6 | −8.4 | <0.0001 |
|
Absenteeism (28-Day Recall) In the past 4 weeks (28 days), how many days did you... |
Before Surgery to 6 Months After | Before Surgery to 1 Year After | ||||||||
| N | Mean Before | Mean After | Mean Δ | Rank P-value | N | Mean Before | Mean After | Mean Δ | Rank P-value | |
| ... miss work because of problems with your physical or mental health? | 214 | 0.89 | 0.61 | −0.27 | <0.0001 | 220 | 1.16 | 0.77 | −0.39 | <0.0001 |
| ... miss work because of problems with a family member’s physical or mental health? | 214 | 0.37 | 0.33 | −0.04 | 0.2642 | 220 | 0.33 | 0.26 | −0.07 | 0.1457 |
| ... miss work for any other reason (including vacation)? | 214 | 2.05 | 1.91 | −0.14 | 0.2581 | 220 | 1.86 | 2.53 | 0.67 | 0.0785 |
| ... come in early, go home late, work extra from home, or work on your day off? | 212 | 6.22 | 5.84 | −0.38 | 0.7105 | 219 | 6.26 | 5.41 | −0.85 | 0.5795 |
| Absenteeism (7-Day Recall) | Before Surgery to 6 Months After | Before Surgery to 1 Year After | ||||||||
| N | Mean Before | Mean After | Mean Δ | Rank P-value | N | Mean Before | Mean After | Mean Δ | Rank P-value | |
| How many days are you expected to work in a typical 7-day week? | 219 | 4.87 | 4.82 | −0.05 | 0.4267 | 228 | 4.92 | 4.85 | −0.07 | 0.3547 |
| How many hours does your employer expect you to work in a typical 7-day week? | 218 | 36.59 | 36.86 | 0.27 | 0.3513 | 227 | 36.73 | 36.87 | 0.14 | 0.2252 |
| About how many hours altogether did you work in the past 7 days? | 219 | 36.61 | 37.12 | 0.51 | 0.254 | 228 | 36.50 | 37.35 | 0.85 | 0.1503 |
| 7-Day Absenteeism Score (hours per month) | 218 | −0.39 | −1.38 | −0.99 | 0.4381 | 227 | 0.63 | −2.21 | −2.84 | 0.4507 |
| Total Knee Arthroplasty | ||||||||||
| Presenteeism | Before Surgery to 6 Months After | Before Surgery to 1 Year After | ||||||||
| N | Mean Before | Mean After | Mean Δ | Rank P-value | N | Mean Before | Mean After | Mean Δ | Rank P-value | |
| Absolute Presenteeism, All Patients | 209 | 82.9 | 88.0 | 5.2 | <0.0001 | 209 | 81.6 | 89.3 | 7.7 | <0.0001 |
| Full Performance (Absolute Presenteeism = 100%) | 209 | 21.5% | 32.1% | 10.6% | 0.0151* | 209 | 20.1% | 38.3% | 0.2 | <0.0001* |
| Absolute Presenteeism, Before Surgery < 100% | 164 | 78.2 | 87.0 | 8.8 | <0.0001 | 167 | 77.0 | 87.4 | 10.4 | <0.0001 |
| Absolute Presenteeism, Before Surgery = 100% | 45 | 100.0 | 91.8 | −8.2 | <0.0001 | 42 | 100.0 | 97.1 | −2.9 | 0.0016 |
|
Absenteeism (28-Day Recall) In the past 4 weeks (28 days), how many days did you... |
Before Surgery to 6 Months After | Before Surgery to 1 Year After | ||||||||
| N | Mean Before | Mean After | Mean Δ | Rank P-value | N | Mean Before | Mean After | Mean Δ | Rank P-value | |
| ... miss work because of problems with your physical or mental health? | 187 | 0.83 | 0.21 | −0.62 | <0.0001 | 189 | 1.14 | 0.57 | −0.57 | <0.0001 |
| ... miss work because of problems with a family member’s physical or mental health? | 187 | 0.18 | 0.18 | 0.00 | 0.4488 | 189 | 0.15 | 0.25 | 0.10 | 0.6449 |
| ... miss work for any other reason (including vacation)? | 187 | 2.10 | 1.29 | −0.81 | 0.0054 | 189 | 2.34 | 2.26 | −0.08 | 0.572 |
| ... come in early, go home late, work extra from home, or work on your day off? | 187 | 5.71 | 4.93 | −0.78 | 0.1538 | 189 | 6.04 | 4.95 | −1.09 | 0.0488 |
| Absenteeism (7-Day Recall) | Before Surgery to 6 Months After | Before Surgery to 1 Year After | ||||||||
| N | Mean Before | Mean After | Mean Δ | Rank P-value | N | Mean Before | Mean After | Mean Δ | Rank P-value | |
| How many days are you expected to work in a typical 7-day week? | 199 | 4.78 | 4.69 | −0.09 | 0.7576 | 200 | 4.74 | 4.65 | −0.09 | 0.0907 |
| How many hours does your employer expect you to work in a typical 7-day week? | 198 | 35.66 | 35.54 | −0.12 | 0.5423 | 198 | 34.80 | 34.81 | 0.01 | 0.9361 |
| About how many hours altogether did you work in the past 7 days? | 199 | 36.09 | 37.60 | 1.51 | 0.3197 | 199 | 35.20 | 36.05 | 0.85 | 0.5584 |
| 7-Day Absenteeism Score (hours per month) | 198 | −2.45 | −8.19 | −5.74 | 0.4684 | 196 | −3.10 | −4.84 | −1.74 | 0.6664 |
Note: P-values are from Wilcoxon signed-rank tests, except those with an astericks, which are from two-sample test of proportions.
Appendix Table 5.
Absolute presenteeism stratified by joint and whether static, declining, or improving performance leading up to surgery
| Absolute Presenteeism | Before Surgery to 6 Months After | Before Surgery to 1 Year After | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean Before | Mean After | Mean Δ | Rank P-value | N | Mean Before | Mean After | Mean Δ | Rank P-value | |
| Knee, Static | 126 | 88.9 | 88.8 | −0.1 | 0.5961 | 123 | 87.8 | 89.4 | 1.5 | 0.0415 |
| Knee, Declining | 75 | 72.5 | 86.7 | 14.1 | <0.0001 | 74 | 70.1 | 89.5 | 19.3 | <0.0001 |
| Knee, Improving | 8 | 85.0 | 88.8 | 3.8 | 0.666 | 12 | 89.2 | 88.3 | −0.8 | 0.6851 |
| Hip, Static | 116 | 89.9 | 91.9 | 2.0 | 0.0614 | 118 | 89.5 | 90.6 | 1.1 | 0.0663 |
| Hip, Declining | 100 | 70.5 | 87.7 | 17.2 | <0.0001 | 104 | 68.7 | 88.9 | 20.2 | <0.0001 |
| Hip, Improving | 9 | 83.3 | 88.9 | 5.6 | 0.4147 | 9 | 83.3 | 80.0 | −3.3 | 0.7192 |
Note: n=1 respondent cannot be classified as static, declining, or improving because of insufficient baseline responses
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Zhang W, Gignac MA, Beaton D, Tang K, Anis AH. Productivity loss due to presenteeism among patients with arthritis: Estimates from 4 instruments. J Rheumatol 2010;37(9):1805–14. [DOI] [PubMed] [Google Scholar]
- 2.Stewart WF, Ricci JA, Chee E, Morganstein D. Lost Productive Work Time Costs from Health Conditions in the United States: Results from the American Productivity Audit. J Occup Environ Med 2003;45(12):1234–46. [DOI] [PubMed] [Google Scholar]
- 3.Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, Absence, Disability, and Presenteeism Cost Estimates of Certain Physical and Mental Health Conditions Affecting U.S. Employers. J Occup Environ Med 2004;46(4):398–412. [DOI] [PubMed] [Google Scholar]
- 4.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the us workforce. JAMA. 2003. November;290(18):2443–54. [DOI] [PubMed] [Google Scholar]
- 5.Pauly MV, Nicholson S, Polsky D, Berger ML, Sharda C. Valuing reductions in on-the-job illness: “Presenteeism” from managerial and economic perspectives. Health Econ 2008;17(4):469–85. [DOI] [PubMed] [Google Scholar]
- 6.Lamb CE, Ratner PH, Johnson CE, Ambegaonkar AJ, Joshi AV., Day D, et al. Economic impact of workplace productivity losses due to allergic rhinitis compared with select medical conditions in the United States from an employer perspective. Curr Med Res Opin 2006;22:1203–10. [DOI] [PubMed] [Google Scholar]
- 7.Canavan C, West J, Card T. Review article: The economic impact of the irritable bowel syndrome. Aliment Pharmacol Ther 2014;40(9):1023–34. [DOI] [PubMed] [Google Scholar]
- 8.Wada K, Arakida M, Watanabe R, Negishi M, Sato J, Tsutsumi A. The economic impact of loss of performance due to absenteeism and presenteeism caused by depressive symptoms and comorbid health conditions among Japanese workers. Ind Health. 2013;51(5):482–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andersson G, American Academy of Orthopaedic Surgeons. The burden of musculoskeletal disorders on Americans - Opportunities for Action. 2015;247. Available from: http://www.boneandjointburden.org/docs/BMUSExecutiveSummary2016%282%29.pdf [Google Scholar]
- 10.World Health Organization [Internet]. Musculoskeletal Conditions. 2019. [cited 2020 Apr 20]. Available from: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions
- 11.Gignac MAM, Cao X, Tang K, Beaton DE. Examination of arthritis-related work place activity limitations and intermittent disability over four-and-a-half years and its relationship to job modifications and outcomes. Arthritis Care Res 2011;63(7):953–62. [DOI] [PubMed] [Google Scholar]
- 12.Beaton DE, Tang K, Gignac MAM, Lacaille D, Badley EM, Anis AH, et al. Reliability, validity, and responsiveness of five at-work productivity measures in patients with rheumatoid arthritis or osteoarthritis. Arthritis Care Res 2010;62(1):28–37. [DOI] [PubMed] [Google Scholar]
- 13.Lerner D, Reed JI, Massarotti E, Wester LM, Burke TA, Knottnerus JA, et al. The Work Limitations Questionnaire’s validity and reliability among patients with osteoarthritis. J Clin Epidemiol 2002;55(2):197–208. [DOI] [PubMed] [Google Scholar]
- 14.Zhang W, Bansback N, Kopec J, Anis AH. Measuring time input loss among patients with rheumatoid arthritis: validity and reliability of the Valuation of Lost Productivity questionnaire. J Occup Environ Med 2011;53(Number 5):530–6. [DOI] [PubMed] [Google Scholar]
- 15.Bansback N, Zhang W, Walsh D, Kiely P, Williams R, Guh D, et al. Factors associated with absenteeism, presenteeism and activity impairment in patients in the first years of RA. Rheumatology. 2012;51(2):375–84. [DOI] [PubMed] [Google Scholar]
- 16.Agaliotis M, Mackey MG, Jan S, Fransen M. Burden of reduced work productivity among people with chronic knee pain: A systematic review. Occup Environ Med 2014;71(9):651–9. [DOI] [PubMed] [Google Scholar]
- 17.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 2008;8(1):8–20. [DOI] [PubMed] [Google Scholar]
- 18.Lerner D, Rogers WH, Chang H, Rodday AM, Greenhill A, Villagra VG, et al. The health care and productivity costs of back and neck pain in a multi-employer sample of utility industry employees. J Occup Environ Med 2015;57(1):32–43. [DOI] [PubMed] [Google Scholar]
- 19.Etkin CD, Springer BD. The American Joint Replacement Registry—the first 5 years. Arthroplast Today [Internet]. 2017;3(2):67–9. Available from: 10.1016/j.artd.2017.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williams S, Wolford M, Bercovitz A. Centers for Disease Control [Internet]. Hospitalization for Total Knee Replacement Among Inpatients Aged 45 and Over: United States, 2000–2010. 2010. [cited 2018 Nov 28]. Available from: http://www.cdc.gov/nchs/data/databriefs/db32.htm
- 21.Scott CEH, Turnbull GS, Powell-Bowns MFR, MacDonald DJ, Breusch SJ. Activity levels and return to work after revision total hip and knee arthroplasty in patients under 65 years of age. Bone Jt J. 2018;100B(8):1043–53. [DOI] [PubMed] [Google Scholar]
- 22.Kleim BD, Malviya A, Rushton S, Bardgett M, Deehan DJ. Understanding the patient-reported factors determining time taken to return to work after hip and knee arthroplasty. Knee Surg Sport Traumatol Arthrose. 2015;23:3646–52. [DOI] [PubMed] [Google Scholar]
- 23.Bohm ER. The Effect of Total Hip Arthroplasty on Employment. J Arthroplasty [Internet]. 2010;25(1):15–8. Available from: 10.1016/j.arth.2008.11.011 [DOI] [PubMed] [Google Scholar]
- 24.Sankar A, Davis AM, Palaganas MP, Beaton DE, Badley EM, Gignac MA. Return to work and workplace activity limitations following total hip or knee replacement. Osteoarthr Cartil [Internet]. 2013;21(10):1485–93. Available from: 10.1016/j.joca.2013.06.005 [DOI] [PubMed] [Google Scholar]
- 25.Hylkema TH, Stevens M, Selzer F, Amick BA, Katz JN, Brouwer S. Activity Impairment and Work Productivity Loss After Total Knee Arthroplasty: A Prospective Study. J Arthroplasty [Internet]. 2019;34(11):2637–45. Available from: 10.1016/j.arth.2019.06.015 [DOI] [PubMed] [Google Scholar]
- 26.Marks M, Vliet Vlieland TPM, Audigé L, Herren DB, Nelissen RGHH, Van Den Hout WB. Healthcare costs and loss of productivity in patients with trapeziometacarpal osteoarthritis. J Hand Surg Eur Vol 2015;40(9):927–34. [DOI] [PubMed] [Google Scholar]
- 27.Amick BC, Habeck RV., Ossmann J, Fossel AH, Keller R, Katz JN. Predictors of Successful Work Role Functioning after Carpal Tunnel Release Surgery. J Occup Environ Med. 2004;46(5):490–500. [DOI] [PubMed] [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform [Internet]. 2009;42(2):377–81. Available from: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019;95:31078660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kessler RC, Ames M, Hymel PA, Loeppke R, McKenas DK, Richling DE, et al. Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to evaluate the indirect workplace costs of illness. J Occup Environ Med 2004;46(6 SUPPL.):23–37. [DOI] [PubMed] [Google Scholar]
- 31.Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, et al. The World Health Organization Health and Work Performance Questionnaire (HPQ). J Occup Env Med 2003;45:156–74. [DOI] [PubMed] [Google Scholar]
- 32.Mateen BA, Doogan C, Hayward K, Hourihan S, Hurford J, Playford ED. Systematic Review of Health-Related Work Outcome Measures and Quality Criteria-Based Evaluations of Their Psychometric Properties. Arch Phys Med Rehabil 2017;98:534–60. [DOI] [PubMed] [Google Scholar]
- 33.Wang PS, Beck A, Berglund P, Leutzinger JA, Pronk N, Richling D, et al. Chronic medical conditions and work performance in the health and work performance questionnaire calibration surveys. J Occup Env Med 2003;45(12):1303–11. [DOI] [PubMed] [Google Scholar]
- 34.Scuffham PA, Vecchio N, Whiteford HA. Exploring the validity of HPQ-based presenteeism measures to estimate productivity losses in the health and education sectors. Med Decis Mak 2014;34(1):127–37. [DOI] [PubMed] [Google Scholar]
- 35.Kessler R, Petukhova M, McInnes K, Üstün TB. Re: Content and scoring rules for the WHO HPQ absenteeism and presenteeism questions. 2007. [cited 2020 Oct 20]. Available from: https://www.hcp.med.harvard.edu/hpq/ftpdir/absenteeism%20presenteeism%20scoring%20050107.pdf
- 36.Ospina MB, Dennett L, Waye A, Jacobs P, Thompson AH. A systematic review of measurement properties of instruments assessing presenteeism. Am J Manag Care. 2015;21:e171–85. [PubMed] [Google Scholar]
- 37.Joish VN, Brixner DI. Back pain and productivity: measuring worker productivity from an employer’s perspective. J Pain Palliat Care Pharmacother 2004;18:79–85. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


