Abstract
The focus of the review is to discuss the relevant and essential aspects of pharmaceutical cocrystals in both academia and industry with an emphasis on non-steroidal anti-inflammatory drugs (NSAIDs). Although cocrystals have been prepared for a plethora of drugs, NSAID cocrystals are focused due to their humongous application in different fields of medication such as antipyretic, anti-inflammatory, analgesic, antiplatelet, antitumor, and anti-carcinogenic drugs. The highlights of the review are (a) background of cocrystals and other solid forms of an active pharmaceutical ingredient (API) based on the principles of crystal engineering, (b) why cocrystals are an excellent opportunity in the pharma industry, (c) common methods of preparation of cocrystals from the lab scale to bulk quantity, (d) some latest case studies of NSAIDs which have shown better physicochemical properties for example; mechanical properties (tabletability), hydration, solubility, bioavailability, and permeability, and (e) latest guidelines of the US FDA and EMA opening new opportunities and challenges.
The focus of the review is to discuss the relevant and essential aspects of pharmaceutical cocrystals in both academia and industry with an emphasis on non-steroidal anti-inflammatory drugs (NSAIDs).
1. Introduction
Drug products are an essential commercial commodity of our lifestyle to maintain health and cure us of diseases. About 80% of the drugs used today are utilized in solid forms, as most APIs are crystalline solids at room temperature. Also, oral ingestion is the most expedient and commonly used route for drug delivery because of its ease of administration, high patient compliance, least sterility constraints, cost-effectiveness, and flexibility in dosage form design. Once the drug is developed, it must pass different clinical phases of drug approval before its market delivery. The drugs often fail in clinical development phases due to poor mechanical and physicochemical properties viz. solubility,1 permeability,2 bioavailability,3 dissolution rate,4 hygroscopicity,5 tabletability,6 compressibility,7 and stability of APIs and excipients8 (see Fig. 1), resulting in significant losses to the company both in terms of time and cost.9,10 The poor properties of drugs can be modified by devising different methods, namely salt formation, nano-formulations, co-solvency, complexation with cyclodextrins and surfactants, micronization, solid dispersions, co-amorphous formulations, cocrystallization, etc.11–20 Among all the mentioned techniques, cocrystallization is the promising method for improving physicochemical properties without modification in the chemical structure of the API.21–23 Cocrystallization has countered challenges in the development of new solid forms of non-ionic APIs.
Fig. 1. Different applications of cocrystals in drugs and materials.
The concept of designing cocrystals or pharmaceutical cocrystals was evolved from the basic principles of crystal engineering and brought both industry and academia to explore within their horizons for better solid forms of APIs. In the initial journey of crystal engineering, the work was mainly focused on developing new multi-component systems.24–28 A breakthrough came in 2004 when Zaworotko and Almarsson, for the first time, defined the term pharmaceutical cocrystal as “a subset of a broader group of multi-component crystals that also includes salts, solvates (pseudo polymorphs), clathrates, inclusion crystals, and hydrates.”29 The recognition of pharmaceutical cocrystals was the pinnacle in pharmaceutics and the maturity of crystal engineering. After that, various researchers have done pioneering works on solid-state pharmaceutical cocrystals with the idea of drug translation to make improved medicines with good physicochemical and pharmacokinetic properties. With growing knowledge in cocrystallization and its utility in the formation of pharmaceutical cocrystals, different definitions of cocrystal came up with time due to the overlap of cocrystals in salts, polymorphs, pseudo-polymorphs. Recently, an agreement paper defined cocrystals as “solids that are crystalline single-phase materials composed of two or more different molecular and/or ionic compounds generally in a stoichiometric ratio which are neither solvates nor simple salts.”30–32 Despite outstanding developments in the field of cocrystals, its definition is still under debate which laid an obstacle in the commercial success of pharmaceutical cocrystals. Some researchers claim cocrystal as a physical mixture and might fall within current compendial guidelines, whereas others think that the cocrystal must be regarded as a new chemical entity and require all the associated toxicological and safety testing. In 2018, the United States Food and Drug Administration (FDA) released the latest guidelines on the regulatory classification of pharmaceutical cocrystals for New Drug Applications (NDAs) and Abbreviated New Drug Applications (ANDAs), which blurred the boundary between cocrystals and physical mixtures.
Herein, we discuss improvements in physicochemical and pharmacokinetic properties, specifically the tabletability, hydration stability, permeability, solubility, and intrinsic dissolution rate (IDR) of NSAIDs through cocrystallization with some latest case studies.
2. Solid forms for an API
A drug product mainly consists of an API and some other ingredients that may affect its physicochemical and pharmacokinetic properties. An API is the key ingredient of a drug product that targets the disease. The FDA defined API as “any substance that is represented for use in a drug and that, when used in the manufacturing, processing, or packaging of a drug, becomes an active ingredient or a finished dosage form of the drug. Such substances are intended to furnish pharmacological activity or other direct effects in the diagnosis, cure, mitigation, treatment or prevention of disease, or to affect the structure and function of the body of humans or other animals.”33 The different solid forms of an API play a pivotal role in drug discovery and development in the context of bioavailability optimization, filing intellectual property rights, and innovating suitable manufacturing methods.34
Broadly, there are two solid forms available for an API, viz. amorphous form and crystalline form (Fig. 2). The amorphous form includes amorphous drug substances, amorphous solid dispersions, and co-amorphous systems. Among these different amorphous forms, the amorphous drug substance exhibits high apparent solubility but low physical and chemical stability. To improve the stability and to maintain high apparent solubility, one or more than one type of polymer can be added and produce amorphous solid dispersions. Polymers are added to form a miscible solid (single-phase containing the amorphous API and the polymer) and decrease crystallization both in the solid-state and solution. In addition to polymers, surfactants may also be added to the amorphous drug substance forming ternary or quaternary systems to improve the solubility. Co-amorphous systems include an API and a small molecule, such as amino acids. It is interesting to observe that some ternary systems are also reported, which seems to be the combination of the amorphous solid dispersion form and co-amorphous form, i.e., it contains an API, a small molecule, and a polymer. The initial solvent content and hygroscopicity are the essential considerations while developing these amorphous materials because solvent (or water) content affects both the glass transition temperature (Tg) and amorphous substances' stability.35–39
Fig. 2. Different solid forms of pharmaceuticals for an API.
Despite having various amorphous forms of a drug, crystalline drug products are generally preferred over amorphous solids as they meet the specifications in terms of purity, thermodynamic stability, and processing.40 In the crystalline form of a drug molecule, the API can exist as either a single-component or multi-component. Single-component drug molecules do not provide a wide modification in the API's physicochemical properties because they are limited to polymorphs and allow only a subtle change. However, multi-component drug molecules offer a wide area of altering physicochemical properties. They may be stoichiometric and non-stoichiometric encompassing hydrates, solvates, salts, solid-solutions, and cocrystals (Fig. 3). Non-stoichiometric multi-component drug products (like solid-solutions) enable different physicochemical properties by varying the stoichiometry but are not generally amenable to design because the preparation of reproducible phases is non-trivial.41,42 Hence only stoichiometric multi-component crystalline forms for an API will be discussed in further sections of this article. There is still ambiguity over the nomenclature and definitions of different solid forms due to legal issues.43–45
Fig. 3. Different crystalline solid forms.

2.1. Solvates/hydrates
Solvates of an API can be defined as the multi-component crystalline arrangement of the host molecule (API or excipient) and guest molecule (solvent) incorporated in the crystal lattice structure (Fig. 4(a)).34,43 When water acts as a guest molecule, then the crystalline form is referred to as hydrate. Solvates are known as pseudo polymorphs in which the solvent molecule helps to stabilize the overall packing of the unit cell.46 In pharmaceutics, the drug hydrate is more popular than any other organic solvate because of its small size, atmospheric humidity, and hydrogen donating and accepting property of water.34,47 In marketed drug products, hydrates have been selected and developed for use rather than any other drug solvates because a solvate might suffer from poor thermal and hydration stability.48,49 Examples of single-component drug hydrates are ampicillin trihydrate50 and cephalexin monohydrate.51 The hydrates of multi-component drug products will be discussed in later sections of the article.
Fig. 4. Pictorial representation of different crystalline solid forms: (a) solvates/hydrates, (b) salts, (c) solvates/hydrates of salts, (d) molecular cocrystals (MCCs), (e) solvates/hydrates of MCCs, (f) ionic cocrystals (ICCs), (g) solvates/hydrates of ICCs and (h) polymorphs.
2.2. Salts
In pharmaceutics, salts are the widely used and well-established solid form for improving physicochemical properties, mainly solubility.52–54 The FDA defined salts as “any of numerous compounds that result from the replacement of part or all of the acid hydrogens of an acid by a metal or radical acting like a metal: an ionic or electrovalent crystalline compound. Per the current regulatory scheme, different salt forms of the same active moiety are considered different APIs” (see Fig. 4(b)).55 Salts are relatively stable and possess a good solubility in polar solvents (chiefly water).56 However, a primary drawback of salts is that they are limited to ionizable APIs and the counter-partners of salts must comply with the pharmaceutical acceptability,57,58i.e., must be a GRAS (generally regarded as safe) product.59 Examples of pharmaceutical salts are aspirin sodium salt60 and cetirizine calcium salt.61
These pharmaceutical salts may also get hydrated to produce a new solid form (Fig. 4(c)), which has the advantages of enhanced stability, solubility, hygroscopicity, crystallinity, and bioavailability over the dehydrated form. The high water solubility of a pharmaceutical salt increases the probability of a compound reaching the biological target. Some of the key factors that affect hydrate formation are water activity, the number of donor and acceptor atoms in a chemical system, different pharmaceutically acceptable anion groups, and the chemical system's polar surface.62 Examples of hydrated pharmaceutical salts are aspirin-sodium salt dihydrate60 and norfloxacin-sulphathiazole salt hydrate.63
2.3. Molecular cocrystals (MCCs)
MCCs are a multi-component crystalline arrangement of two or more neutral coformers in a stoichiometric ratio solid under ambient conditions (Fig. 4(d)). These coformers are typically, but not exclusively, sustained by hydrogen bonds.64–66 If at least one of the coformers is pharmaceutically active and other coformers are pharmaceutically acceptable or GRAS compounds, it is termed as pharmaceutical cocrystal.29,44,67 Examples of pharmaceutical MCCs are the apremilast–aspirin cocrystal68 and ibuprofen–nicotinamide cocrystal.69 MCCs are long known but with different nomenclature in the literature. Buehler and Heap described MCCs, in 1926, as ‘molecular organic compounds’70 whereas Anderson used the term ‘organic molecular compounds’ in 1937.71 Later on, in 1959, Hoogsten used the word ‘hydrogen bond complex’ for the MCC between 1-methylthymine and 9-methyladenine, and it is now known as a Hoogsten base pair.72,73 The term cocrystal was popularized after the 1990s because of the extensive study, by Margaret Etter, on the design of multi-component crystals through hydrogen bonding.74–76 Her concepts for determining the plausibility of hydrogen-bond interactions are still used today in the field of cocrystal design. Despite the popularity of the term cocrystal in the crystal engineering field, some researchers even coined different terms. For example, Pekker et al., in 2005, used the word ‘heteromolecular crystals’ for the cocrystal of cubane and fullerene.77 Thus, MCCs have been termed as addition compounds, mixed crystals, hydrogen-bonded complexes, molecular organic compounds, and heteromolecular crystals. Like salts, these MCCs may also get solvated/hydrated to produce another solid form (Fig. 4(e)). Examples of hydrated pharmaceutical MCCs are isoniazid : 4-hydroxybenzoic acid cocrystal monohydrate78 and vanillic acid : theobromine cocrystal dehydrate.79
2.4. Ionic cocrystals (ICCs)
The term ‘ionic cocrystal’ was coined by the Braga research group, in 2010, for the sodium bromide–barbituric acid cocrystal.80 ICCs are the multi-component crystalline arrangement of organic molecules and inorganic salts like an alkali or alkaline earth halide in a stoichiometric ratio (Fig. 4(f)).81,82 Unlike MCCs, ICCs are mainly sustained by charge-assisted hydrogen bonds and/or coordination bonds (if a metal ion is present).83 In the latter case, ICCs are generally regarded as coordination polymers. Thus, large families of ICCs include conjugate acid–base cocrystals (cocrystals containing an ion and its neutral counterpart)84 and acid salts (cocrystals containing a carboxylic acid and carboxylate salt).85 Like MCCs, ICCs are also long known but reported with different nomenclature as molecular compounds,86 such as complex salts,87 additional complexes,88 acid salts,85 metal salt complexes,89 and adducts. Examples of pharmaceutical ICCs are piracetam–CaCl2 (ref. 82) and [Na(carbamazepine)5][I3].90 ICCs have a relatively high affinity to get hydrated to produce a new solid form because of water molecules' competency with other organic components for ion coordination (Fig. 4(g)). An example of a hydrated pharmaceutical ICC is [Na(carbamazepine)4(CH3OH)][I]·H2O.90
2.5. Polymorphs
Polymorphism (from Greek: polys – multiple, morfé – shape) is the tendency of a molecule to crystallize in different crystal lattices due to varying crystallization conditions (Fig. 4(h)).60,61,91,92 The FDA defined polymorphs as “different crystalline forms of the same API. This may include solvation or hydration products (also known as pseudo polymorphs) and amorphous forms. Per the current regulatory scheme, different polymorphic forms are considered the same APIs.”55 The single and multi-component crystals exhibit polymorphism due to different intermolecular forces like van der Waals forces, London dispersion forces, halogen bonding, hydrogen bonding, dipole–dipole interactions, π–π interactions, and quadrupole interactions.93 Polymorphs of either single-component or multi-component crystals show different physical and chemical properties such as hardness, density, solubility, chemical stability, dissolution rate, melting point, hygroscopicity, and interactions with biological systems.94–103 Polymorphs of single-component crystals show a subtle change in the physicochemical properties as the solubility difference between two polymorphic forms of a pure API is typically less than two-fold. Examples of single-component polymorphs are aceclofenac polymorphs104 and mebendazole polymorphs.105
The propensity of polymorphism in cocrystals has been a subject of interest and debate, mainly for crystal engineers and pharmaceutical researchers. Earlier, it was thought that cocrystals are less prone to show polymorphism and can be used as an alternative solid form for drug products to minimize this phenomenon.40 In 2004, Almarsson and Zaworotko reported in their article that “there may be an opportunity to reduce the practical extent of polymorphism of drug compounds specifically by co-crystal formation although there may be exceptions.”29 After ten years, in a review article, Aitipamula et al. asserted only 114 polymorphic cocrystals amongst thousands of cocrystals deposited in the Cambridge Structural Database (CSD).106 However, such data could not lead to a generalization in cocrystal polymorphism as that was not the focus of that study. According to the recent literature, the counting of polymorphic cocrystals reached 150 and still increasing.107 These analyses led the authors to conclude that “cocrystals were found to be just as likely of being polymorphic as single-component systems.” An example of a pharmaceutical cocrystal polymorph is the naproxen–proline cocrystal polymorph.103
3. Cocrystal preparation method
With the advancement in drug development, various methods have been developed to prepare cocrystals ranging from lab-scale synthesis to potentially large scale production.108 The production routes for cocrystal formation can be broadly classified as solid-based, solution-based, and supercritical fluid methods. A brief discussion of these methods has been done below, while the detailed discussion of these methods with their subcategories has been done by Karimi-Jafari et al.109 A list of common cocrystal preparation methods is shown in Fig. 5.
Fig. 5. Common methods for the preparation of pharmaceutical cocrystals.
3.1. Solid-based methods
Solid-based methods employ very little or no amount of solvent for the preparation of cocrystals. They are subcategorized into different routes, namely neat grinding, liquid assisted grinding (LAG), extrusion, hot-melt extrusion, and high shear wet granulation.110–114 The neat grinding (or dry grinding) method consists of mixing two or more coformers in a fixed stoichiometric ratio and grinding them for a particular period either manually or mechanically.115 In the LAG (also known as kneading, solvent drop grinding, wet grinding) method, similar steps to neat grinding are followed, except a minimal amount of solvent is used during the grinding process.116 Extrusion is the method of combining coformers in bespoke extruder equipment (maybe single or twin screw) and is operated below the melting point of either starting material.117 However, hot-melt extrusion is a specialist technique of simultaneous melting and mixing of coformers in a heated screw extruder. Extrusion offers highly intensive mixing, shear, and close material packing (without using any solvent) that improves the surface contact between blends of coformers leading to cocrystal formation.118 High shear wet granulation is a typically employed method for drug product formulations but recently found application in cocrystal preparation. It involves the agglomeration of powder particles (via a liquid medium) in the presence of a binder. A high shear granulator is used, which imparts shear to the powder mixture through impellers and choppers.119,120
3.2. Solution-based methods
A variety of solution-based methods are available for preparing cocrystals, namely evaporative, assisted evaporative, spray drying, slurry, and reactive cocrystallization. Evaporative or solution cocrystallization is a technique based on solvent evaporation from an undersaturated solution of both coformers under ambient conditions.121 This method is famous for developing single-crystal cocrystals needed for diffraction studies and elucidating the crystal structure. Assisted evaporative cocrystallization is similar to evaporative cocrystallization, except the evaporation is done at high temperatures and/or reduced pressure. The spray drying method is commercially used for formulating amorphous solid dispersions, but recent studies show its application in cocrystal synthesis. It is beneficial because of its continuous, highly controllable, and fast process. It is a continuous single-step method of transforming liquids (solutions, suspensions, slurries) into solid powders by dispersing an undersaturated solution of both coformers through a nozzle using nitrogen where fast removal of solvent takes place.118 The slurry conversion method (or isothermal slurry conversion) involves adding solid coformers in a fixed stoichiometric ratio into a solvent (maybe a solvent mixture) for a specified period of equilibration, and the solid remains in excess for the duration.122 Unlike evaporative cocrystallization, this method does not require a clear starting solution. The reactive cocrystallization method involves mixing individual solutions of either coformers or adding one solid coformer into a clear solution of another coformer in a solvent.123 This results in a sudden spontaneous cocrystallization under ambient conditions.
3.3. Supercritical fluid methods
Supercritical fluids (SCFs) are highly compressed pure substances or mixtures at a pressure and temperature above their critical points, Pc and Tc, where the liquid and gas phases are indistinguishable. Supercritical fluid methods are promising methods for synthesizing pharmaceutical cocrystals as they do not involve any toxic organic solvent. These methods depend on three distinct properties of the supercritical fluid viz. solvent, antisolvent, and atomization enhancement. Cocrystallization with supercritical solvent (CSS) involves adding an SCF (like CO2) to a mixture of the API and coformer for a fixed period. The SCF acts as a solvent and molecular mobility enhancer. It is possible to fine-tune the solvent power and density of CO2 by controlling its thermodynamic conditions (like pressure and temperature), which provides control over the cocrystallization between the API and coformer.124 In the rapid expansion of supercritical solution (RESS) method, a solution of the API and coformer in scCO2 is rapidly depressurized (10−5 s) to atmospheric conditions, resulting in high supersaturation of the solute in scCO2. This supersaturation leads to nucleation and forces the fine particles to agglomerate in the form of crystals. Two methods, namely supercritical antisolvent crystallization (SAS) and gas antisolvent crystallization (GAS), work on an exactly different approach as it employs the SCF as an antisolvent that induces precipitation of the API and coformer previously dissolved in an organic solvent. In the SAS method, the addition of scCO2 decreases the solubility of the API and coformer in the precipitation chamber and simultaneously precipitates them in a cocrystalline structure. It is an advantageous technique in controlling the production of polymorphs of pharmaceutical cocrystals.125 In the GAS method, compressed CO2 is added to a stirring solution of the API–coformer in a high-pressure vessel until the desired pressure is obtained. The scCO2 expands the liquid solvent resulting in a decrease in the solvent's solubilizing power that enhances the solutes' crystallization. Two methods, namely atomization and antisolvent crystallization (AAS) and supercritical fluid enhanced atomization (SEA), employ the SCF as a spray enhancer that breaks up liquid jets into smaller droplets upon simultaneous depressurization with liquid solutions. Both methods are similar to the spray drying method as discussed in the previous section, except in place of nitrogen gas, supercritical CO2 is used for the drying chamber at atmospheric pressure. However, the primary difference between these two methods is that AAS is carried out at ambient temperature while SEA is at higher. These methods cannot be used for synthesizing a wide range of pharmaceutical cocrystals because the starting components (both the API and coformer) must be soluble in supercritical CO2, and unfortunately, most of the drug components have low solubility in CO2.126–128
4. Why non-steroidal anti-inflammatory drugs (NSAIDs)
A person generally seeks medical attention if he/she suffers from pain, fever, or inflammation, which are the common symptoms of many diseases known. Most pain relievers function by affecting the central nervous system (CNS), and so incorrect dosage may severely affect a person's health.129,130 The FDA defined some over-the-counter (OTC) pain relievers/fever reducers as safe and effective when used as directed. OTC pain relievers/fever reducers are of two types: acetaminophen (or paracetamol) and NSAIDs. Acetaminophen is a widely used OTC fever reducer and analgesic. It reduces mild to moderate, acute, and chronic types of pain, including muscle aches, headache, sinus pain, toothache, back pain, osteoarthritis, and many more. The antipyretic and analgesic properties of acetaminophen are almost similar to those of NSAIDs, but due to the absence of potent anti-inflammatory properties, it is not categorized as an NSAID.131 Acetaminophen is the safest OTC analgesic for patients, but its use is currently under increased scrutiny by the FDA due to the risk of intentional and, more concerning, unintentional overdose-related hepatotoxicity (liver toxicity).132 The exact mechanism of acetaminophen action is unclear, but it seems to be similar to that of NSAIDs.
NSAIDs are a drug class that can be used as antipyretic (reduces fever),133 analgesic (reduces pain),134 anti-inflammatory (reduces inflammation),135 antiplatelet (or antiaggregant),136 antitumour,137 and cancer preventive agents.138,139 NSAIDs may sometimes also refer to NSAIMs (non-steroidal anti-inflammatory medicines) or NSAIAs (non-steroidal anti-inflammatory agents/analgesics). Although many single therapeutic action drugs viz. antipyretic, analgesic, and anti-inflammatory drugs have been developed, NSAIDs are preferred and widely used in the market because of their multiple therapeutic actions, thus covering an entire class of treatment of common symptoms. It is estimated that more than 73 million NSAIDs are written in a year, and around 30 million people consume NSAIDs daily.140 Among all the therapeutic activities of NSAIDs, they are popularly known for their analgesic properties.141 NSAIDs generally reduce pain and inflammation by inhibiting the cyclooxygenase enzymes (responsible for prostaglandin synthesis) viz. COX-1 and COX-2. COX-2 is responsible for developing prostaglandin mediated pain and inflammation, whereas COX-1 plays some housekeeping role by preventing gastric mucosa and platelet hemostasis. Inhibition of COX-1 can severely damage the mucous membrane causing ulceration throughout the gastrointestinal tract, and so the extensive use of NSAIDs prevails the adverse effects of these relatively safe drugs. The two adverse drug reactions related to NSAIDs are the renal and gastrointestinal (GI) effects of the agents such that they are highly dose-dependent; thereby NSAIDs should be more COX-2 selective inhibitors, if not possible, then COX-2 preferential inhibitors.141–143
NSAIDs are classified into four groups based on their mode of action (see Table 1).130,144
Classification of NSAIDs based on the mode of action.
| Class | Properties | Examples |
|---|---|---|
| Group I | Non-selective weak inhibitors of COX | 5-Aminosalicylic acid, sodium salicylate, nabumetone, sulfasalazine |
| Group II | Non-selective strong inhibitors of COX | Diclofenac, ibuprofen, ketoprofen, flurbiprofen, indomethacin, piroxicam, naproxen, aspirin |
| Group III | Preferential COX-2 inhibitor with 5–50 fold selectivity | Celecoxib, etodolac, meloxicam, nimesulide |
| Group IV | Preferential COX-2 inhibitor with >50-fold selectivity | Rofecoxib |
NSAIDs can also be divided into various classes based on their chemical structure to reveal the fact that the drugs having the same functional group show similar properties and tolerability (Table 2).130,143,144
Classification of NSAIDs based on the functional groups.
| Class | Examples | Skeletal structure |
|---|---|---|
| Oxicams | Lornoxicam, meloxicam, piroxicam |

|
| Salicylates | Aspirin, diflunisal |

|
| 2-Aryl propionic acids (profens) | Naproxen, ibuprofen, ketoprofen, flurbiprofen |

|
| Arylalkanoic acids | Etodolac, indomethacin, acemetacin, diclofenac |

|
| Pyrazolidine derivatives | Sulfinpyrazone, azapropazone |

|
| N-Aryl anthranilic acids (fenamic acids) | Mefenamic acid, meclofenamic acid |

|
| Sulphonanilides | Nimesulide |
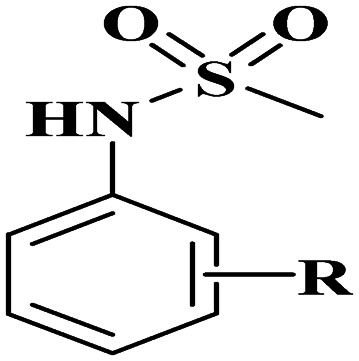
|
| Fluorinated benzene sulphonamide (Coxibs) | Celecoxib, rofecoxib, valdecoxib |

|
Despite the availability of a wide variety of pain-relieving drugs, satisfactory pain treatment has not been attained yet, with only around 25% of patients experiencing significant pain relief. The main reason is the subjective nature of pain, but poor anxieties over long-term safety and exploitation of the available analgesic drug are equally responsible.32 Researchers reveal that, in the area of the drug product, combining existing therapies or multimodal therapies is a good alternative in pain management145–147 and cancer cachexia,148–152 where the monomodal treatments are unable to provide a complete response. The multimodal treatment is preferred over monomodal therapy because of the multimodal behavior of pain in which different signaling pathways, mediators, and molecular mechanisms are involved. Several complementary mechanisms of action of a drug are required to be employed to obtain adequate analgesia.
In aid to the fact, the utilization of combination therapy could sanction lower doses of the API to be used, thereby decreasing the incidence and severity of side effects, resulting in an improved efficacy-to-safety ratio.32,153,154
5. NSAID and BCS classification
According to the Biopharmaceutical Classification System (BCS), drugs are classified into four main categories depending on their intestinal permeability and aqueous solubility (Table 3).155 These two parameters have significant importance in understanding the concept of drug absorption and bioavailability. Currently, BCS guidelines are provided by the FDA,156 WHO,157 and EMA.158 A particular term ‘biowaiver’ is introduced to a regulatory drug approval process when the dossier (application) is accepted based on evidence of equivalence other than through in vivo equivalence testing. The biowaiver means to obtain waive off for carrying out expensive and time-consuming BA (bio availability) and BE (bio equivalence) studies. The BCS provides biowaivers for class I, II, and III drugs with some specifications. This waiver is for both pre-and post-approval phases. For good oral bioavailability, quick absorption of the drug in water or aqueous solvent mixtures must take place, and it requires rapid solubilization of the drug such that the aqueous solubility of the drug must be at least 100 mg L−1. Most of the familiar NSAIDs belong to BCS class II, which leads to high variable bioavailability after oral administration. It is a requisite to increase their dissolution rate and solubility for faster onset of action, minimizing the variability in absorption, and improving its overall bioavailability. Formulating a drug in the form of cocrystal is proved to be a good alternative for optimized bioavailability.63,122,159,160
BCS classification and biowaiver eligibility.
| BCS class | Solubility | Permeability | Biowaiver eligibility |
|---|---|---|---|
| I | High | High | Eligible |
| II | Low | High | Eligible only for weak acids having high solubility at pH 6.8 and high dissolution rate |
| III | High | Low | Eligible if very rapid dissolution rate |
| IV | Low | Low | Not eligible |
6. Case studies of NSAID cocrystals
6.1. Improved mechanical properties
The mechanical properties of drugs, mainly tabletability and compaction pressure, and their relationship with the crystal structure are important for drug approval at their preformulation stage. Tabletability is the powder's ability to be transformed into a tablet of specific strength under the influence of compaction pressure.6 Tabletability is generally represented by a plot between tensile strength and compaction pressure. Poor tabletability of a powder indicates plastic deformation during compaction followed by high elastic recovery.161 Various pharmaceutical cocrystals have been reported in which the crystal packing is controlled to modulate tabletability and compaction, which is an important improvement at the preformulation stage.162–165 Abbas et al. examined the powder of the naproxen–nicotinamide (NAP–NIC) binary cocrystal for better tableting behaviour.166 Naproxen (Aleve®, Naprosyn®) is a widely used NSAID for the relief of pain, fever, swelling, and stiffness. It is a 2-aryl propanoic acid derivative belonging to BCS class-II and a non-selective COX inhibitor. The NAP–NIC cocrystal was prepared by the liquid-assisted grinding method with a small amount of acetonitrile used in grinding. Fig. 6 shows the tabletability profiles of pure NAP, NIC, and the NAP–NIC cocrystal. NAP and NIC have poor compressible properties as on increasing compaction pressure, a drop in tensile strength of tablets is observed at >3000 psi, thus unsuitable for direct tableting. In contrast, the NAP–NIC cocrystal shows a better tabletability and exhibits an increased tensile strength of ∼1.80 times than that of NAP at 5000 psi. The synthesized cocrystal powder is suitable for direct tableting, as indicated by the lower Carr's index for the NAP–NIC cocrystal (9.7%) than the pure NAP drug (22%). Also, the micrometric properties of the cocrystal are improved.
Fig. 6. Molecular structures of (a) naproxen (NIP) and (b) nicotinamide (NIC). (c) Powder compaction properties of NAP, NIC, and 1 : 1 cocrystal. Reproduced with permission from ref. 166. Copyright 2018 The Springer (American Association of Pharmaceutical Scientists).
Jaysheel et al. examined the compaction behaviour of the metformin–salicylic acid (MET–SAL) binary cocrystal for better tableting behaviour of MET (Fig. 7). Metformin (MET) belongs to the biguanide class and is used worldwide to treat type-2 diabetes mellitus. Salicylic acid (SAL) and its derivatives are widely used NSAIDs to treat acne and other skin diseases. The MET–SAL cocrystal was prepared by using the solvent evaporation method under ambient conditions. MET is an orally delivered drug, but its poor tableting behaviour is a common problem for its commercial production. The crystal structure reveals the fact that the poor tabletability of MET might be due to isotropic and stiff interaction energy between MET layers. In contrast, SAL possesses high tabletability and promotes deformation because of the anisotropic interaction topology between strongly hydrogen-bonded salicylate molecules. The combination of both drugs in the form of cocrystal yielded an elastic anisotropy material with intermediate stiffness, improved plastic flow, and overall better tabletability. The authors reasoned the fact that the MET–SAL cocrystal exhibits interlayer hydrogen bonding between two planes with larger d-spacings and lower absolute attachment energies than MET.121
Fig. 7. Molecular structures of (a) metformin (MET) and (b) salicylic acid (SAL). (c) Thermal ellipsoid drawing of the asymmetric unit of the MET–SAL cocrystal. (d) Tabletability profile of MET, SAL, and MET : SAL cocrystal. Reproduced with permission from ref. 121 Copyright 2020 The Elsevier B.V.
6.2. Improved hydration stability
The hydration stability of a drug is a pressing topic for a commercial dosage formulation. Most of the APIs in the market exist in both anhydrous and hydrated forms, and these APIs need to be physically stable in the anhydrous form against hydration. The phase transition of an anhydrous API to a hydrated form leads to changed physicochemical and pharmacokinetic properties. Also, the transformation of the active species to the inactive metabolite reduces the therapeutic activity of a drug.167–170
Li et al. reported piroxicam–clonixin (PXC–CNX) drug–drug cocrystal solvates for enhancing the hydration stability of PXC (see Fig. 8).122 Piroxicam (Feldene®) is a well-known NSAID for the relief of the signs and symptoms of rheumatoid arthritis and osteoarthritis. It is an oxicam derivative belonging to BCS class-II and a non-selective COX inhibitor. PXC has been reported in five anhydrous forms and one monohydrate form, and both forms I and II are available commercially.171,172 CNX (another NSAID commonly used to treat inflammation) was selected as the second component for preparing the drug–drug cocrystal with PXC. In addition to pharmacokinetic improvement, drug–drug cocrystals also offer a potential advantage of multidrug resistance, reducing side effects, increasing drug action synergistically, combination therapies, etc.173,174 Eight different cocrystal solvates of PXC with CNX were screened through the mechanochemical synthesis method and slurry method. The crystalline structures of all cocrystal solvates were almost similar; the solvents might act as a space-filler rather than a binder. Among the eight different solvates, the ethyl acetate solvate (PXC–CNX–EA) was assumed to be a pharmaceutically accepted drug form because of the non-toxic and non-irritating properties of ethyl acetate. The hydration stability of PXC (form II), CNX (form I), and PXC–CNX–EA was tested under controlled conditions (25 °C/95% RH) for four weeks. Anhydrous PXC showed high hydration risk in which phase transformation of PXC into PXC·H2O was detected after two weeks by powder XRD along with a significant colour change. In contrast, PXC–CNX–EA showed better moisture stability as there was no change in its color and crystalline form within one month.
Fig. 8. Molecular structures of (a) piroxicam (PXC) and (b) clonixin (CNX). (c) Thermal ellipsoid drawing of the asymmetric unit of PXC–CNX–solvent (solvent molecule is omitted here for clarity). (d) Color changes of CNX form I, PXC form α2, and PXC–CNX–EA at different time intervals during the moisture stability tests. (e) Powder XRD patterns of CNX, PXC, and PXC–CNX–EA before and after equilibration at 95% RH/25 °C for different periods; simulated powder XRD pattern of PXC·H2O is also provided. Reproduced with permission from ref. 122. Copyright 2019 The Royal Society of Chemistry.
6.3. Improved solubility and IDR
The solubility, dissolution rate, and permeability of drugs are the pillars of their bioavailability. Solubility is the maximum amount of drug dissolved in a solvent until a thermodynamic equilibrium is attained by the solute between the solid and liquid phases. The rate by which the solute particles reach this equilibrium is termed as the dissolution rate. In the first decade of the 21st century, the field of pharmaceutical cocrystals came into existence with the application of solubility enhancement of a drug via cocrystallization.23,175–177 Many pharmaceutical cocrystals have been developed such that around 70% of them have been investigated to have better solubility than the parent drug.178,179
Carmen Almansa et al. reported a novel drug–drug ionic cocrystal of celecoxib and rac-tramadol·HCl in a 1 : 1 molecular ratio, CTC (E-58425/MR308) to improve the physicochemical properties, stability, bioavailability, dissolution profile, and formulation capacity of both drugs (see Fig. 9). Celecoxib (Celebrex®) is a well-known NSAID for treating chronic pain in osteoarthritis, rheumatoid arthritis, juvenile rheumatoid arthritis, ankylosing spondylitis, acute pain, and primary dysmenorrhea. It is a fluorinated benzene sulphonamide derivative belonging to BCS class-II and works by selectively inhibiting the COX-2 enzyme. Tramadol (Ultram®) is a centrally acting weak synthetic μ-opioid receptor agonist prescribed to treat moderate to severe pain. Different screening methods, namely slurrying, wet grinding, vapor diffusion, evaporation, and crystallization, were performed for preparing the binary cocrystal. Here, cocrystallization leads to enhancement in pharmacokinetic profiles and clinical benefits. CTC consists of two APIs with four complementary mechanisms of analgesic action viz., μ-opioid receptor agonism, noradrenaline reuptake inhibition, serotonin reuptake, and COX-2 inhibition. The comparative IDR studies showed that the release of celecoxib was 3-fold faster from CTC than from celecoxib alone, intimating its increased absorption potential. On the other hand, tramadol release was 7-fold slower from CTC than from tramadol alone, suggesting the more sustained release of this API, intimating enhanced safety and tolerability. For the final tablet formulation, CTC has completed phase I and phase II clinical trials, but phase III trials in visceral and somatic musculoskeletal nociceptive-dominated acute pain models are on-going.32,180,181
Fig. 9. Molecular structures of (a) rac-tramadol hydrochloride and (b) celecoxib. (c) Thermal ellipsoid drawing of the asymmetric unit of CTC. (d) Release (amount versus time) of CTC in water at 37 °C in comparison to tramadol·HCl and celecoxib. Reproduced with permission from ref. 32. Copyright 2017 The American Chemical Society.
6.4. Improved permeability
Drug permeability across biological membranes is a key factor influencing the absorption and distribution to sustain a drug's good pharmacokinetics profile. The different factors that influence the drug movement into the bloodstream (called drug absorption) are the physicochemical properties of the drug, formulation, and administration route. Distinctive routes are available for drug administration, including intramuscular injection, intravenous therapy, and enteral injection, but the intestinal pathway (oral treatment) is common. The drug must be dissolved and absorbed efficiently in blood for sound therapeutic effects, no matter what kind of administration route is chosen. By adjusting factors that affect absorption, the pharmacokinetic (ADME/PK) profile of a drug can be changed.182 Since pharmaceutical cocrystals have been known for the past two decades, very few examples have been reported to investigate improved permeability.
Ling et al. reported the first zwitterionic cocrystal of indomethacin (INC) with dl-proline (PL) amino acid for optimized physicochemical properties and accelerated absorption rate (see Fig. 10). INC (Indocid®, Indocin®) is a well-known NSAID for treating patients with moderate to severe rheumatoid arthritis, osteoarthritis, ankylosing spondylitis, and gouty arthritis.183–186 It is an aryl-alkanoic acid derivative belonging to BCS class-II and a non-selective COX inhibitor. INC has been reported in seven polymorphic forms in which the γ form is commercially available. Amino acids (like dl-proline) have been accepted as good cocrystal coformers because of their low toxicity, self-charge compatibility, structural features, and excellent physicochemical properties. The liquid-assisted grinding method was used to prepare the INC–PL–H2O cocrystal, and crystallization was then done by the solvent evaporation method. The optimization of solubility and permeability of a drug is a pivotal task for its oral administration. The solubility of the cocrystal and INC was measured at different pH values, and in all the cases, the solubility of the cocrystal was two to three times higher compared to INC alone. In addition, the cocrystal had the maximum solubility at pH 6.8, which is fruitful for maximum absorption of the drug in the small intestine. The cocrystal had higher cumulative diffused amounts (×1.66) than INC itself, suggesting an enhancement in the permeability of INC after forming a cocrystal with PL. The authors reasoned that the improved solubility, IDR, and permeability were due to the change in crystal packing of INC. While preparing the cocrystal, the O–H⋯O synthon between carboxylic acids of INC was broken and formed a sandwich-like crystal package where the PL molecule was located on the channels between two layers and water molecules as an intermediary.116
Fig. 10. Molecular structures of (a) indomethacin (INC) and (b) proline (PL). (c) Thermal ellipsoid drawing of the asymmetric unit of the INC–PL–H2O cocrystal. (d) Solubility comparisons of INC, the cocrystal, and the physical mixture of INC and PL in pH buffers 1.2, 4.0, and 6.8. (e) Plots of flux for INC and the cocrystal with respect to time. (f) Cumulative amount of INC and the cocrystal permeated vs. time. Reproduced with permission from ref. 116. Copyright 2020 The Royal Society of Chemistry.
Khatioda et al. reported three polymorphic binary cocrystals of ethenzamide (ZMD) with 2,4-dihydroxy benzoic acid (2,4-DHB), see Fig. 11.187 Ethenzamide, a well-known NSAID for the relief of mild to moderate pain including musculoskeletal and joint disorders, is a salicylic acid derivative belonging to BCS class-II and a COX-2 selective inhibitor. Different cocrystals of ZMD have been reported with varying coformers like ferulic acid, gentisic acid, α-resorcylic acid, γ-resorcylic acid, gallic acid, etc. for better solubility and drug permeation.188–191 The reported work specifically focused on understanding solubility and membrane permeation behaviour in various polymorphic phases that could affect drug efficacy. The cocrystal polymorphs reported in the literature were generally isolated in different solvents, but in this case, the authors isolated three different polymorphs in the same solvent with a stoichiometry variation of starting materials. Cocrystal polymorphic form-III was serendipitously obtained while experimenting, and the authors were unable to regenerate it. Therefore, the solubility and permeation studies were carried out on ZMD, cocrystal polymorphic form-I, and form-II. The solubility of both cocrystal forms (form I and II) was 2.5 times higher than pure ZMD at pH 7.4, but at pH 1.2, the solubility of pure ZMD was much higher than the cocrystal polymorphic forms due to the formation of the ZMD hydrochloride salt. Form-I's permeation rate% and flux density at pH 7.4 were much higher than pure ZMD, but form-II showed only a noticeable increment. At pH 1.2 solutions, the improvement in permeation rate% and flux density of form-I over ZMD showed a significant increment while form-II showed lower values than ZMD. The increasing permeability behaviour and flux density of cocrystal form-I could be reasoned due to fewer sites for hydrophilic interactions with the solvent molecule. In contrast, form-II's lower permeability was due to exposure of polar groups toward the crystal surface to interact with the solvent molecule.
Fig. 11. (a) Thermal ellipsoid drawing of the asymmetric unit of the ZMD-2,4-DHB cocrystal. (b) Solubility comparisons of ZMD and its cocrystal polymorphs, form-I and form-II at pH 1.2 and 7.4 phosphate buffer solutions. Permeability rate% (c) at pH 1.2 and (d) at pH 7.4 phosphate buffer solutions. Flux density (e) at pH 1.2 and (f) at pH 7.4 phosphate buffer solutions. Reproduced with permission from ref. 187 Copyright 2018 The American Chemical Society.
The number of reported NSAID cocrystals is high enough to be accommodated in a single review. Therefore, few reported drug–drug cocrystals in which at least one drug is an NSAID are shown in Table 4.
Reported drug–drug cocrystals of NSAIDs.
| Drug 1 (therapeutic activity) | Drug 2 (therapeutic activity) | Observations | Year | Ref. |
|---|---|---|---|---|
| Aspirin (NSAID) | Meloxicam (NSAID) | 44-Fold increase in pH 7.4 phosphate buffer solubility with improved bioavailability and Cmax | 2011 | 195 |
| Sildenafil (erectile dysfunction) | Enhanced IDR | 2014 | 196 | |
| Apremilast (antipsoriatic) | Increased IDR and solubility | 2018 | 68 | |
| Theophylline (antiasthmatic) | No evaluation of pharmaceutical properties | 2018 | 197 | |
| Carbamazepine (antiepileptic) | No evaluation of pharmaceutical properties | 2019 | 198 | |
| Salicylic acid (NSAID) | Nevirapine (antiretroviral) | Increased IDR and solubility | 2012 | 199 |
| Piroxicam (NSAID) | No evaluation of pharmaceutical properties | 2012 | 200 | |
| Tenoxicam (NSAID) | Increased IDR | 2013 | 201 | |
| Andrographolide (antiviral) | Increased solubility, faster dissolution rate, higher drug release | 2013 | 202 | |
| Trospium chloride (antispasmodic) | No evaluation of pharmaceutical properties | 2014 | 203 | |
| Ethionamide (antitubercular) | Enhanced IDR | 2020 | 204 | |
| Nicotinamide (skin restorative) | Mefenamic acid (NSAID) | No evaluation of pharmaceutical properties | 2011 | 205 |
| Naproxen (NSAID) | Increased IDR | 2012 | 206 | |
| Indomethacin (NSAID) | No evaluation of pharmaceutical properties | 2013 | 207 | |
| Acemetacin (NSAID) | Increased solubility | 2014 | 208 | |
| Celecoxib (NSAID) | No evaluation of pharmaceutical properties | 2017 | 209 | |
| Ibuprofen (NSAID) | Increased solubility and in vivo analgesic effect | 2018 | 210 | |
| Curcumin (NSAID) | Increased IDR and antinociceptive/anti-inflammatory potency | 2019 | 211 | |
| Theophylline (antiasthmatic) | Diflunisal and diclofenac (NSAID) | Increased solubility | 2014 | 212 |
| Flufenamic acid (NSAID) | Increased solubility and hygroscopic stability | 2016 | 213 | |
| Aceclofenac (NSAID) | Paracetamol (analgesic) | Increased dissolution rate | 2011 | 214 |
| Indomethacin (NSAID) | Carbamazepine (antiepileptic) | No evaluation of pharmaceutical properties | 2011 | 215 |
| Flufenamic acid(NSAID) | Ethenzamide (NSAID) | Increased solubility | 2017 | 216 |
| Tramadol (NSAID) | Celecoxib (NSAID) | Optimized solubility and IDR, improved Cmax and bioavailability | 2017 | 32 |
| Ibuprofen (NSAID) | Levetiracetam (antiepileptic) | Chiral resolution | 2018 | 217 |
| Piroxicam (NSAID) | Clonixin (NSAID) | Enhanced hydration stability | 2019 | 122 |
| Metacetamol (NSAID) | Levofloxacin (antibacterial) | Improved hygroscopic and photostability of levofloxacin | 2019 | 218 |
7. Regulatory aspects of cocrystals
The development and quality control strategies for a drug molecule (specifically pharmaceutical cocrystals) depend on its regulations. The FDA first did the regulatory classification of pharmaceutical cocrystals in April 2011. In that report, the FDA Center for Drug Evaluation and Research (CDER) classified cocrystals as ‘drug product intermediates (DPIs)’ and defined them as “solids that are crystalline materials composed of two or more molecules in the same crystal lattice.”192,193 This classification was undesirable for the industries because considering cocrystals as DPIs would require different regulatory reporting requirements, unlike polymorphs or salts.21 The FDA made various revisions in the definition of cocrystal, and recently in February 2018, the FDA described pharmaceutical cocrystals as “crystalline materials composed of two or more different molecules, typically an active pharmaceutical ingredient (API) and co-crystal formers (“coformers”), in the same crystal lattice.”55 The regulations for pharmaceutical cocrystals are similar to those of polymorphs of an API because the solvates are of the initial drug substance. Specifically, it is not regarded as a new API. With this guidance, the pharmaceutical industries benefit from producing cocrystals at existing formulation facilities using APIs and coformers without any additional requirements of current good manufacturing practice (cGMPs). However, drug manufacturers should submit appropriate data for new drug applications (NDAs) and abbreviated NDAs (ANDA) containing a cocrystalline form supporting the structure of the cocrystals. For APIs and coformers having ionizable functional groups, data should demonstrate that no ionic interaction exists between the component API and coformers. Also, a substantial dissociation of the API from its cocrystal form should occur before reaching the site of pharmacological activity. In May 2015, a reflection paper released by EMA had given subdivision of solid-state materials based on the internal structure addressing the applications of cocrystals of APIs in medicinal products.
According to EMA, cocrystals are “homogeneous (single-phase) crystalline structures comprising two or more components in a specific stoichiometric ratio where the arrangement in the crystal lattice is not based on ionic bonds (as with salts).”194 Unlike the FDA, EMA recognizes cocrystals mainly as APIs and applies to various formulations if the drug manufacturer can demonstrate different efficacy/or safety (see Table 5).
Comparison of the regulatory status of pharmaceutical cocrystals55,194.
| Factor | US FDA | EMA |
|---|---|---|
| Regulatory status | DPI | APIs |
| Regulatory regard | Similar to solvates | Similar to salts of the same API |
| Similarity with parent API | Yes | No (if their safety and efficacy are proved different) |
| Coformers | Neutral guest compound (excipient) | Non-active components/reagents (excipient) |
| Chemical interactions | Nonionic | Nonionic |
| Manufacturing sites | API manufacturing sites | API manufacturing sites |
| US-Drug master files (DMF)/EMA-active substance master file (ASMF) registration | Not feasible being DPI | Can be filed |
| Applicable good manufacturing practice (GMP) regulations/guide | cGMP for drug product | Part II of EU GMP guide (active substances) and ICH Q7 and in rare cases, part I of EU GMP guide (finished drug product) |
8. Summary and outlook
Pharmaceutical cocrystals are still attracting the solemn interest of researchers from a wide array of fields viz. pharmaceutical industry, chemical science, crystallography, materials science, and drug regulatory agencies. Several drug cocrystals have been commercialized and marketed such as Lexapro (escitalopram oxalate–oxalic acid), Entresto (valsartan sodium–sacubitril sodium), Steglatro (ertugliflozin–l-pyroglutamic acid), and Suglat (ipragliflozin–l-proline). Besides, few are in different phases of clinical trials.
Though possessing high utility, drug cocrystals are limited in the market space due to drug commercial production challenges. (1) The complexity of designing and synthesizing pharmaceutical cocrystals (especially drug–drug cocrystals) is an assiduous task because it does not ensure that the synthesized cocrystal would be a commercially acceptable stable form that provides potent benefits. (2) The drug's dosage is another obstacle in pharmaceutical cocrystals to obtain the stoichiometric ratio for the drug's recommended oral dosage. (3) Investigation for new robust, scalable methods suitable for commercial manufacture of pharmaceutical cocrystals.
In spite of all these challenges, the momentum in the research of pharmaceutical cocrystals is at its apex due to its opulent applications in improving the physicochemical and pharmacokinetic properties of drugs. The cost of formulating a new drug is soaring every day (around US$3.0 billion219), whereas a pharmaceutical cocrystal purveys a lower risk and expense with a beneficial approach to new-age and better medications. Moreover, the probability of getting a new solid form with ionizable and non-ionizable APIs via cocrystallization is several degrees higher than that of salt formation because the number of co-formers present in the list of GRAS (generally recognized as safe)59 compounds is much higher than salt-forming counter ions.
The majority of NSAIDs belong to BCS group II. Solubility plays a crucial role in obtaining the optimal efficacy of a drug, which leads to the cocrystal of an NSAID that can provide a superior solution. The latest guidelines of the FDA (2018) and EMA (2015) have eased up the approval process of drug cocrystals. However, clearer and rational policies are in much dire need to increase cocrystal opportunities as next-generation medicines.
Conflicts of interest
There are no conflicts to declare.
Acknowledgments
UG and YA thank the Department of Applied Chemistry, Aligarh Muslim University. UG is also thankful to the CSIR-JRF (Grant No: 09/112(0633)/2019-EMR-I) for providing financial assistance.
Biographies
Biography
Utsav Garg.

Utsav Garg joined the Ph.D. course at the Department of Applied Chemistry, Zakir Husain College of Engineering & Technology, Aligarh Muslim University in 2018. He obtained his B.Sc. (2015) and M.Sc. (2017) in industrial chemistry from Aligarh Muslim University and was awarded ‘university medals’ for securing 1st rank in both courses. He had qualified in the CSIR-UGC National Eligibility Test and is currently working as Junior Research Fellow under the supervision of Dr. Yasser Azim. His research interests are in crystal engineering, solid-state chemistry, metal organic frameworks and pharmaceutical cocrystals.
Biography
Yasser Azim.

Dr. Yasser Azim was appointed in August 2009 as Assistant Professor in the Department of Applied Chemistry in Zakir Husain College of Engineering & Technology, Aligarh Muslim University, Aligarh, India. He completed his PhD in Chemistry at the Department of Chemistry, Aligarh Muslim University in 2006 and then joined the University of Hyderabad and later on the Indian Institute of Science, Bangalore as DST Young Scientist in the research laboratory of Prof. G.R. Desiraju. His current research interests include mechanochemical synthesis, crystal engineering, polymorphs and pharmaceutical cocrystals.
References
- Rao V. M., Sanghvi R. and Zhu H., in Developing Solid Oral Dosage Forms, Elsevier, 2009, pp. 1–24 [Google Scholar]
- Dahan A. Miller J. M. AAPS J. 2012;14:244–251. doi: 10.1208/s12248-012-9337-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toutain P. L. Bousquet-Melou A. J. Vet. Pharmacol. Ther. 2004;27:455–466. doi: 10.1111/j.1365-2885.2004.00604.x. [DOI] [PubMed] [Google Scholar]
- Kapoor D., Maheshwari R., Verma K., Sharma S., Pethe A. and Tekade R. K., in Drug Delivery Systems, Elsevier, 2020, pp. 1–45 [Google Scholar]
- Zografi G. Drug Dev. Ind. Pharm. 1988;14:1905–1926. doi: 10.3109/03639048809151997. [DOI] [Google Scholar]
- Joiris E. Di Martino P. Berneron C. Guyot-Hermann A. M. Guyot J. C. Pharm. Res. 1998;15:1122–1130. doi: 10.1023/A:1011954800246. [DOI] [PubMed] [Google Scholar]
- Leuenberger H. Rohera B. D. Pharm. Res. 1986;3:12–22. doi: 10.1023/A:1016364613722. [DOI] [PubMed] [Google Scholar]
- Devadasu V. R., Deb P. K., Maheshwari R., Sharma P. and Tekade R. K., in Dosage Form Design Considerations, Elsevier, 2018, pp. 149–178 [Google Scholar]
- Pritchard J. F. Jurima-Romet M. Reimer M. L. J. Mortimer E. Rolfe B. Cayen M. N. Nat. Rev. Drug Discovery. 2003;2:542–553. doi: 10.1038/nrd1131. [DOI] [PubMed] [Google Scholar]
- DiMasi J. A. Hansen R. W. Grabowski H. G. J. Health Econ. 2003;22:151–185. doi: 10.1016/S0167-6296(02)00126-1. [DOI] [PubMed] [Google Scholar]
- Acharya P. C., Marwein S., Mishra B., Ghosh R., Vora A. and Tekade R. K., in Dosage Form Design Considerations, Elsevier, 2018, pp. 435–472 [Google Scholar]
- Alizadeh M. N. Shayanfar A. Jouyban A. J. Mol. Liq. 2018;268:410–414. doi: 10.1016/j.molliq.2018.07.065. [DOI] [Google Scholar]
- Komal K. Kaur T. Singh A. P. Singh A. P. Sharma P. J. Drug Delivery Ther. 2018;8:32–40. doi: 10.22270/jddt.v8i6-s.2074. [DOI] [Google Scholar]
- Sharma D. Joshi S. Asian J. Pharm. 2007;1:9–19. [Google Scholar]
- Karagianni A. Kachrimanis K. Nikolakakis I. Pharmaceutics. 2018;10:98. doi: 10.3390/pharmaceutics10030098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dengale S. J. Grohganz H. Rades T. Löbmann K. Adv. Drug Delivery Rev. 2016;100:116–125. doi: 10.1016/j.addr.2015.12.009. [DOI] [PubMed] [Google Scholar]
- Jones W. Motherwell W. D. S. Trask A. V. MRS Bull. 2006;31:875–879. doi: 10.1557/mrs2006.206. [DOI] [Google Scholar]
- Srivastava D. Fatima Z. Kaur C. D. Mini-Rev. Med. Chem. 2018;18:1160–1167. doi: 10.2174/1389557518666180305163613. [DOI] [PubMed] [Google Scholar]
- Abidi S. S. A. Garg U. Azim Y. Alam M. Gupta A. K. Pradeep C. P. Azum N. Asiri A. M. Arabian J. Sci. Eng. 2021;46:353–364. doi: 10.1007/s13369-020-04822-x. [DOI] [Google Scholar]
- Karashima M. Sano N. Yamamoto S. Arai Y. Yamamoto K. Amano N. Ikeda Y. Eur. J. Pharm. Biopharm. 2017;115:65–72. doi: 10.1016/j.ejpb.2017.02.013. [DOI] [PubMed] [Google Scholar]
- Shaikh R. Singh R. Walker G. M. Croker D. M. Trends Pharmacol. Sci. 2018;39:1033–1048. doi: 10.1016/j.tips.2018.10.006. [DOI] [PubMed] [Google Scholar]
- Schultheiss N. Newman A. Cryst. Growth Des. 2009;9:2950–2967. doi: 10.1021/cg900129f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakuria R. Delori A. Jones W. Lipert M. P. Roy L. Rodríguez-Hornedo N. Int. J. Pharm. 2013;453:101–125. doi: 10.1016/j.ijpharm.2012.10.043. [DOI] [PubMed] [Google Scholar]
- Pepinsky R. Phys. Rev. 1955;100:971–971. [Google Scholar]
- Schmidt G. M. J. Pure Appl. Chem. Res. 1971;27:647–678. [Google Scholar]
- Thomas J. M. Nature. 1981;289:633–634. doi: 10.1038/289633a0. [DOI] [Google Scholar]
- Singh N. B. Singh R. J. Singh N. P. Tetrahedron. 1994;50:6441–6493. doi: 10.1016/S0040-4020(01)89680-0. [DOI] [Google Scholar]
- Desiraju G. R. Angew. Chem., Int. Ed. Engl. 1995;34:2311–2327. doi: 10.1002/anie.199523111. [DOI] [Google Scholar]
- Almarsson Ö. Zaworotko M. J. Chem. Commun. 2004:1889–1896. doi: 10.1039/B402150A. [DOI] [PubMed] [Google Scholar]
- Zhang C. Xiong Y. Jiao F. Wang M. Li H. Cryst. Growth Des. 2019;19:1471–1478. doi: 10.1021/acs.cgd.8b01537. [DOI] [Google Scholar]
- Kumar A. Kumar S. Nanda A. Adv. Pharm. Bull. 2018;8:355–363. doi: 10.15171/apb.2018.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almansa C. Mercè R. Tesson N. Farran J. Tomàs J. Plata-Salamán C. R. Cryst. Growth Des. 2017;17:1884–1892. doi: 10.1021/acs.cgd.6b01848. [DOI] [Google Scholar]
- U.S. FDA Drug Definitions, https://www.registrarcorp.com/definitions [Google Scholar]
- Healy A. M. Worku Z. A. Kumar D. Madi A. M. Adv. Drug Delivery Rev. 2017;117:25–46. doi: 10.1016/j.addr.2017.03.002. [DOI] [PubMed] [Google Scholar]
- Chen L. Okuda T. Lu X.-Y. Chan H.-K. Adv. Drug Delivery Rev. 2016;100:102–115. doi: 10.1016/j.addr.2016.01.002. [DOI] [PubMed] [Google Scholar]
- Wu W. Löbmann K. Rades T. Grohganz H. Int. J. Pharm. 2018;535:86–94. doi: 10.1016/j.ijpharm.2017.10.057. [DOI] [PubMed] [Google Scholar]
- Xie T. Taylor L. S. Pharm. Res. 2016;33:739–750. doi: 10.1007/s11095-015-1823-y. [DOI] [PubMed] [Google Scholar]
- Pokharkar V. B. Mandpe L. P. Padamwar M. N. Ambike A. A. Mahadik K. R. Paradkar A. Powder Technol. 2006;167:20–25. doi: 10.1016/j.powtec.2006.05.012. [DOI] [Google Scholar]
- Jadhav N. Gaikwad V. Nair K. Kadam H. Asian J. Pharm. 2009;3:82. doi: 10.4103/0973-8398.55043. [DOI] [Google Scholar]
- Duggirala N. K. Perry M. L. Almarsson Ö. Zaworotko M. J. Chem. Commun. 2016;52:640–655. doi: 10.1039/C5CC08216A. [DOI] [PubMed] [Google Scholar]
- Lusi M. Vitorica-Yrezabal I. J. Zaworotko M. J. Cryst. Growth Des. 2015;15:4098–4103. doi: 10.1021/acs.cgd.5b00685. [DOI] [Google Scholar]
- Kitaigorodsky A. I., Mixed Crystals, Springer Science & Business Media, 2012 [Google Scholar]
- Grothe E. Meekes H. Vlieg E. ter Horst J. H. de Gelder R. Cryst. Growth Des. 2016;16:3237–3243. doi: 10.1021/acs.cgd.6b00200. [DOI] [Google Scholar]
- Trask A. V. Mol. Pharmaceutics. 2007;4:301–309. doi: 10.1021/mp070001z. [DOI] [PubMed] [Google Scholar]
- Aitipamula S. Banerjee R. Bansal A. K. Biradha K. Cheney M. L. Choudhury A. R. Desiraju G. R. Dikundwar A. G. Dubey R. Duggirala N. Ghogale P. P. Ghosh S. Goswami P. K. Goud N. R. Jetti R. R. K. R. Karpinski P. Kaushik P. Kumar D. Kumar V. Moulton B. Mukherjee A. Mukherjee G. Myerson A. S. Puri V. Ramanan A. Rajamannar T. Reddy C. M. Rodriguez-Hornedo N. Rogers R. D. Row T. N. G. Sanphui P. Shan N. Shete G. Singh A. Sun C. C. Swift J. A. Thaimattam R. Thakur T. S. Kumar Thaper R. Thomas S. P. Tothadi S. Vangala V. R. Variankaval N. Vishweshwar P. Weyna D. R. Zaworotko M. J. Cryst. Growth Des. 2012;12:2147–2152. doi: 10.1021/cg3002948. [DOI] [Google Scholar]
- Griesser U. J., in Polymorphism, Wiley-VCH Verlag GmbH & Co. KGaA, Weinheim, FRG, 2006, pp. 211–233 [Google Scholar]
- Braun D. E. Griesser U. J. Cryst. Growth Des. 2016;16:6405–6418. doi: 10.1021/acs.cgd.6b01078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickey M. B. Peterson M. L. Manas E. S. Alvarez J. Haeffner F. Almarsson Ö. J. Pharm. Sci. 2007;96:1090–1099. doi: 10.1002/jps.20919. [DOI] [PubMed] [Google Scholar]
- Braun D. E. Kahlenberg V. Gelbrich T. Ludescher J. Griesser U. J. CrystEngComm. 2008;10:1617. doi: 10.1039/B809219B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepoittevin J.-P. and Le Coz C. J., in Kanerva's Occupational Dermatology, Springer International Publishing, Cham, 2018, pp. 1–123 [Google Scholar]
- Yousefi Seyf J. Haghtalab A. J. Chem. Eng. Data. 2016;61:2170–2178. doi: 10.1021/acs.jced.6b00163. [DOI] [Google Scholar]
- Berge S. M. Bighley L. D. Monkhouse D. C. J. Pharm. Sci. 1977;66:1–19. doi: 10.1002/jps.2600660104. [DOI] [PubMed] [Google Scholar]
- Sarma B. Thakuria R. Nath N. K. Nangia A. CrystEngComm. 2011;13:3232. doi: 10.1039/C0CE00746C. [DOI] [Google Scholar]
- Thakuria R. Nangia A. Cryst. Growth Des. 2013;13:3672–3680. doi: 10.1021/cg400692x. [DOI] [Google Scholar]
- FDA, Regulatory Classification of Pharmaceutical Co-Crystals Guidance for Industry, 2018 [Google Scholar]
- Hildebrand J. H. J. Am. Chem. Soc. 1916;38:1452–1473. doi: 10.1021/ja02265a002. [DOI] [Google Scholar]
- Gupta D. Bhatia D. Dave V. Sutariya V. Gupta S. V. Molecules. 2018;23:1–15. doi: 10.3390/molecules23071719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould P. L. Int. J. Pharm. 1986;33:201–217. doi: 10.1016/0378-5173(86)90055-4. [DOI] [Google Scholar]
- SCOGS (Select Committee on GRAS Substances), https://www.cfsanappsexternal.fda.gov/scripts/fdcc/?set=SCOGS [Google Scholar]
- Búdová M. Skořepová E. Čejka Jan. Cryst. Growth Des. 2018;18:5287–5294. doi: 10.1021/acs.cgd.8b00718. [DOI] [Google Scholar]
- Yadav M. D. Dikshit S. N. Int. J. Innov. Res. Adv. Stud. 2018;5:191–196. [Google Scholar]
- Gunnam A. Suresh K. Nangia A. Cryst. Growth Des. 2018;18:2824–2835. doi: 10.1021/acs.cgd.7b01600. [DOI] [Google Scholar]
- Gopi S. P. Ganguly S. Desiraju G. R. Mol. Pharmaceutics. 2016;13:3590–3594. doi: 10.1021/acs.molpharmaceut.6b00320. [DOI] [PubMed] [Google Scholar]
- Coates G. W. Dunn A. R. Henling L. M. Ziller J. W. Lobkovsky E. B. Grubbs R. H. J. Am. Chem. Soc. 1998;120:3641–3649. doi: 10.1021/ja974072a. [DOI] [Google Scholar]
- Garg U. Azim Y. Kar A. Pradeep C. P. CrystEngComm. 2020;22:2978–2989. doi: 10.1039/D0CE00106F. [DOI] [Google Scholar]
- Abidi S. S. A. Azim Y. Gupta A. K. Pradeep C. P. J. Mol. Struct. 2017;1150:103–111. doi: 10.1016/j.molstruc.2017.08.080. [DOI] [Google Scholar]
- Vishweshwar P. McMahon J. A. Bis J. A. Zaworotko M. J. J. Pharm. Sci. 2006;95:499–516. doi: 10.1002/jps.20578. [DOI] [PubMed] [Google Scholar]
- Wang F.-Y. Zhang Q. Zhang Z. Gong X. Wang J.-R. Mei X. CrystEngComm. 2018;20:5945–5948. doi: 10.1039/C8CE00689J. [DOI] [Google Scholar]
- Chow S. F. Chen M. Shi L. Chow A. H. L. Sun C. C. Pharm. Res. 2012;29:1854–1865. doi: 10.1007/s11095-012-0709-5. [DOI] [PubMed] [Google Scholar]
- Buehler C. A. Heap A. G. J. Am. Chem. Soc. 1926;48:3168–3172. doi: 10.1021/ja01691a024. [DOI] [Google Scholar]
- Anderson J. S. Nature. 1937;140:583–584. doi: 10.1038/140583b0. [DOI] [Google Scholar]
- Hoogsteen K. Acta Crystallogr. 1959;12:822–823. doi: 10.1107/S0365110X59002389. [DOI] [Google Scholar]
- Hoogsteen K. Acta Crystallogr. 1963;16:907–916. doi: 10.1107/S0365110X63002437. [DOI] [Google Scholar]
- Etter M. C. Frankenbach G. M. Chem. Mater. 1989;1:10–12. doi: 10.1021/cm00001a005. [DOI] [Google Scholar]
- Frankenbach G. M. Etter M. C. Chem. Mater. 1992;4:272–278. doi: 10.1021/cm00020a011. [DOI] [Google Scholar]
- Etter M. C. Frankenbach G. M. Adsmond D. A. Mol. Cryst. Liq. Cryst. 1990;187:25–39. doi: 10.1080/00268949008036024. [DOI] [Google Scholar]
- Pekker S. Kováts É. Oszlányi G. Bényei G. Klupp G. Bortel G. Jalsovszky I. Jakab E. Borondics F. Kamarás K. Bokor M. Kriza G. Tompa K. Faigel G. Nat. Mater. 2005;4:764–767. doi: 10.1038/nmat1468. [DOI] [PubMed] [Google Scholar]
- Aitipamula S. Wong A. B. H. Chow P. S. Tan R. B. H. CrystEngComm. 2013;15:5877. doi: 10.1039/C3CE40729B. [DOI] [Google Scholar]
- Jacobs A. Amombo Noa F. M. CrystEngComm. 2015;17:98–106. doi: 10.1039/C4CE01795A. [DOI] [Google Scholar]
- Braga D. Grepioni F. Maini L. Prosperi S. Gobetto R. Chierotti M. R. Chem. Commun. 2010;46:7715. doi: 10.1039/C0CC02701D. [DOI] [PubMed] [Google Scholar]
- Braga D. Grepioni F. Shemchuk O. CrystEngComm. 2018;20:2212–2220. doi: 10.1039/C8CE00304A. [DOI] [Google Scholar]
- Braga D. Grepioni F. Lampronti G. I. Maini L. Turrina A. Cryst. Growth Des. 2011;11:5621–5627. doi: 10.1021/cg201177p. [DOI] [Google Scholar]
- Shunnar A. F. Dhokale B. Karothu D. P. Bowskill D. H. Sugden I. J. Hernandez H. H. Naumov P. Mohamed S. Chem. – Eur. J. 2020;26:4752–4765. doi: 10.1002/chem.201904672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perumalla S. R. Sun C. C. CrystEngComm. 2012;14:3851. doi: 10.1039/C2CE25193K. [DOI] [Google Scholar]
- Clare Speakman J., in Structure and Bonding, Springer Berlin Heidelberg, Berlin, Heidelberg, 2007, pp. 141–199 [Google Scholar]
- Adler O. and Adler R., U.S. Pat., 1954909, 1934 [Google Scholar]
- Robert L. P., U.S. Pat., 2474758, 1949 [Google Scholar]
- Marcus I., U.S. Pat., 3846486, 1974 [Google Scholar]
- Miller G. A. and Weiler E. D., U.S. Pat., 4150026, 1979 [Google Scholar]
- Buist A. R. Kennedy A. R. Cryst. Growth Des. 2014;14:6508–6513. doi: 10.1021/cg501400n. [DOI] [Google Scholar]
- Kratochvíl B., in Glassy, Amorphous and Nano-Crystalline Materials, 2011, pp. 129–140 [Google Scholar]
- FDA, Cent. Drug Eval. Res., 2007, pp. 1–10 [Google Scholar]
- Berry D. J. Steed J. W. Adv. Drug Delivery Rev. 2017;117:3–24. doi: 10.1016/j.addr.2017.03.003. [DOI] [PubMed] [Google Scholar]
- Xiong X. Du Q. Zeng X. He J. Yang H. Li H. Lange L. Sadowski G. Furuta H. Mori S. Yoshihashi Y. Yonemochi E. Uekusa H. Sugano K. Terada K. Sarceviča I. Grante I. Belyakov S. Rekis T. Bērziņš K. Actiņš A. Orola L. Zieliński W. Katrusiak A. Harriss B. I. Wilson C. Radosavljevic Evans I. Maddileti D. Swapna B. Nangia A. Paisana M. C. Wahl M. A. Pinto J. F. Braun D. E. Griesser U. J. Aitipamula S. Chow P. S. Tan R. B. H. Morissette S. Healy A. M. Worku Z. A. Kumar D. Madi A. M. Cryst. Growth Des. 2016;16:25–46. doi: 10.1021/acs.cgd.5b01388. [DOI] [Google Scholar]
- Morissette S. Adv. Drug Delivery Rev. 2004;56:275–300. doi: 10.1016/j.addr.2003.10.020. [DOI] [PubMed] [Google Scholar]
- Cruz-Cabeza A. J. Reutzel-Edens S. M. Bernstein J. Chem. Soc. Rev. 2015;44:8619–8635. doi: 10.1039/C5CS00227C. [DOI] [PubMed] [Google Scholar]
- Paisana M. C. Wahl M. A. Pinto J. F. Int. J. Pharm. 2016;509:135–148. doi: 10.1016/j.ijpharm.2016.05.038. [DOI] [PubMed] [Google Scholar]
- Santos O. M. M. Reis M. E. D. Jacon J. T. Lino M. E. d. S. Simões J. S. Doriguetto A. C. Braz. J. Pharm. Sci. 2014;50:1–24. doi: 10.1590/S1984-82502011000100002. [DOI] [Google Scholar]
- Sood J. Sapra B. Bhandari S. Jindal M. Tiwary A. K. Ther. Delivery. 2014;5:1123–1142. doi: 10.4155/tde.14.68. [DOI] [PubMed] [Google Scholar]
- Madusanka N. Eddleston M. D. Arhangelskis M. Jones W. Acta Crystallogr., Sect. B: Struct. Sci., Cryst. Eng. Mater. 2014;70:72–80. doi: 10.1107/S2052520613033167. [DOI] [PubMed] [Google Scholar]
- Lange L. Sadowski G. Cryst. Growth Des. 2016;16:4439–4449. doi: 10.1021/acs.cgd.6b00554. [DOI] [Google Scholar]
- Chaurasia G. Int. J. Pharma Sci. Res. 2016;7:2313–2320. [Google Scholar]
- Tumanova N. Tumanov N. Fischer F. Morelle F. Ban V. Robeyns K. Filinchuk Y. Wouters J. Emmerling F. Leyssens T. CrystEngComm. 2018;20:7308–7321. doi: 10.1039/C8CE01338A. [DOI] [Google Scholar]
- Raza K. Ratan S. Kumar M. Kumar P. Chaturvedi S. Katare O. P. J. Drug Delivery Sci. Technol. 2017;39:69–74. doi: 10.1016/j.jddst.2017.03.004. [DOI] [Google Scholar]
- Riggins G., Bai R., Staedtke V., Joshi A. and Williamson T., Mebendazole Polymorph for Treatment and Prevention of Tumors, World Patent, WO2016127168A2 2018
- Aitipamula S. Chow P. S. Tan R. B. H. CrystEngComm. 2014;16:3451. doi: 10.1039/C3CE42008F. [DOI] [Google Scholar]
- Mnguni M. J. Michael J. P. Lemmerer A. Acta Crystallogr., Sect. C: Struct. Chem. 2018;74:715–720. doi: 10.1107/S2053229618006861. [DOI] [PubMed] [Google Scholar]
- Rodrigues M. Baptista B. Lopes J. A. Sarraguça M. C. Int. J. Pharm. 2018;547:404–420. doi: 10.1016/j.ijpharm.2018.06.024. [DOI] [PubMed] [Google Scholar]
- Karimi-Jafari M. Padrela L. Walker G. M. Croker D. M. Cryst. Growth Des. 2018;18:6370–6387. doi: 10.1021/acs.cgd.8b00933. [DOI] [Google Scholar]
- Friščić T. Jones W. Cryst. Growth Des. 2009;9:1621–1637. doi: 10.1021/cg800764n. [DOI] [Google Scholar]
- Friščić T. Childs S. L. Rizvi S. A. A. Jones W. CrystEngComm. 2009;11:418–426. doi: 10.1039/B815174A. [DOI] [Google Scholar]
- Delori A. Friščić T. Jones W. CrystEngComm. 2012;14:2350. doi: 10.1039/C2CE06582G. [DOI] [Google Scholar]
- Tan D. Loots L. Friščić T. Chem. Commun. 2016;52:7760–7781. doi: 10.1039/C6CC02015A. [DOI] [PubMed] [Google Scholar]
- Trask A. V. Motherwell W. D. S. Jones W. Chem. Commun. 2004:890–891. doi: 10.1039/B400978A. [DOI] [PubMed] [Google Scholar]
- Othman M. F. Anuar N. Ad Rahman S. Ahmad Taifuddin N. A. IOP Conf. Ser.: Mater. Sci. Eng. 2018;358:012065. [Google Scholar]
- Wang L.-Y. Yu Y.-M. Jiang F.-B. Li Y.-T. Wu Z.-Y. Yan C.-W. New J. Chem. 2020;44:3930–3939. doi: 10.1039/C9NJ06180K. [DOI] [Google Scholar]
- Kelly A. L. Gough T. Dhumal R. S. Halsey S. A. Paradkar A. Int. J. Pharm. 2012;426:15–20. doi: 10.1016/j.ijpharm.2011.12.033. [DOI] [PubMed] [Google Scholar]
- Walsh D. Serrano D. R. Worku Z. A. Madi A. M. O'Connell P. Twamley B. Healy A. M. Int. J. Pharm. 2018;551:241–256. doi: 10.1016/j.ijpharm.2018.09.029. [DOI] [PubMed] [Google Scholar]
- Bandari S. Nyavanandi D. Kallakunta V. R. Janga K. Y. Sarabu S. Butreddy A. Repka M. A. Int. J. Pharm. 2020;580:119215. doi: 10.1016/j.ijpharm.2020.119215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehder S. Christensen N. P. A. Rantanen J. Rades T. Leopold C. S. Eur. J. Pharm. Biopharm. 2013;85:1019–1030. doi: 10.1016/j.ejpb.2013.04.022. [DOI] [PubMed] [Google Scholar]
- Bhatt J. A. Bahl D. Morris K. Stevens L. L. Haware R. V. Eur. J. Pharm. Biopharm. 2020;153:23–35. doi: 10.1016/j.ejpb.2020.05.031. [DOI] [PubMed] [Google Scholar]
- Li D. Li J. Deng Z. Zhang H. CrystEngComm. 2019;21:4145–4149. doi: 10.1039/C9CE00666D. [DOI] [Google Scholar]
- Machado T. C. Kuminek G. Cardoso S. G. Rodríguez-Hornedo N. Eur. J. Pharm. Sci. 2020;152:105422. doi: 10.1016/j.ejps.2020.105422. [DOI] [PubMed] [Google Scholar]
- Padrela L. Rodrigues M. A. Tiago J. Velaga S. P. Matos H. A. de Azevedo E. G. Cryst. Growth Des. 2015;15:3175–3181. doi: 10.1021/acs.cgd.5b00200. [DOI] [Google Scholar]
- Cuadra I. A. Cabañas A. Cheda J. A. R. Martínez-Casado F. J. Pando C. J. CO2 Util. 2016;13:29–37. doi: 10.1016/j.jcou.2015.11.006. [DOI] [Google Scholar]
- Müllers K. C. Paisana M. Wahl M. A. Pharm. Res. 2015;32:702–713. doi: 10.1007/s11095-014-1498-9. [DOI] [PubMed] [Google Scholar]
- Pando C. Cabañas A. Cuadra I. A. RSC Adv. 2016;6:71134–71150. doi: 10.1039/C6RA10917A. [DOI] [Google Scholar]
- Douroumis D. Ross S. A. Nokhodchi A. Adv. Drug Delivery Rev. 2017;117:178–195. doi: 10.1016/j.addr.2017.07.008. [DOI] [PubMed] [Google Scholar]
- Verma V. Sheikh Z. Ahmed A. S. Acta Neurol. Belg. 2015;115:213–220. doi: 10.1007/s13760-014-0411-y. [DOI] [PubMed] [Google Scholar]
- Rao P. Knaus E. E. J. Pharm. Pharm. Sci. 2008;11:81. doi: 10.18433/j3t886. [DOI] [PubMed] [Google Scholar]
- Shankman G. and Manske R., Fundamental Orthopedic Management for the Physical Therapist Assistant, 3rd edn, 2010 [Google Scholar]
- Herndon C. M. Dankenbring D. M. J. Pain Palliative. Care Pharmacotherapy. 2014;28:109–116. doi: 10.3109/15360288.2014.908993. [DOI] [PubMed] [Google Scholar]
- Aronoff D. M. Neilson E. G. Am. J. Med. 2001;111:304–315. doi: 10.1016/S0002-9343(01)00834-8. [DOI] [PubMed] [Google Scholar]
- Cashman J. N. Drugs. 1996;52(Suppl 5):13–23. doi: 10.2165/00003495-199600525-00004. [DOI] [PubMed] [Google Scholar]
- Vane J. R. Botting R. M. Inflammation Res. 1998;47(Suppl 2):S78–S87. doi: 10.1007/s000110050284. [DOI] [PubMed] [Google Scholar]
- Akagi Y. Nio Y. Shimada S. Aoyama T. Biol. Pharm. Bull. 2011;34:233–237. doi: 10.1248/bpb.34.233. [DOI] [PubMed] [Google Scholar]
- El-Azab A. S. Abdel-Aziz A. A. M. Abou-Zeid L. A. El-Husseiny W. M. ElMorsy A. M. El-Gendy M. A. El-Sayed M. A. A. J. Enzyme Inhib. Med. Chem. 2018;33:989–998. doi: 10.1080/14756366.2018.1474878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairat M. Fournier A. Murphy N. Biessy C. Scalbert A. Rinaldi S. Tjønneland A. Olsen A. Overvad K. Arveux P. Boutron-Ruault M.-C. Cadeau C. Fortner R. T. Kaaks R. Boeing H. Aleksandrova K. Peeters P. H. M. Van Gils C. H. Wareham N. J. Khaw K.-T. Aune D. Riboli E. Gunter M. J. Dossus L. Int. J. Cancer. 2018;143:1688–1695. doi: 10.1002/ijc.31570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakabayashi K. Asian Pac. J. Cancer Prev. 2000;1:97–113. [PubMed] [Google Scholar]
- Vaishnavi P. R. Gaikwad N. Dhaneria S. Indian J. Pharmacol. 2017;49:445. doi: 10.4103/ijp.IJP_189_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fokunang C. MOJ Toxicol. 2018;4:5–13. [Google Scholar]
- Hawkey C. J. Best Pract. Res., Clin. Gastroenterol. 2001;15:801–820. doi: 10.1053/bega.2001.0236. [DOI] [PubMed] [Google Scholar]
- Goltz M. Virology. 2002;294:383–393. doi: 10.1006/viro.2002.1390. [DOI] [PubMed] [Google Scholar]
- Fecker L. F. Stockfleth E. Nindl I. Ulrich C. Forschner T. Eberle J. Br. J. Dermatol. 2007;156:25–33. doi: 10.1111/j.1365-2133.2007.07856.x. [DOI] [PubMed] [Google Scholar]
- Ettrich U. Seifert J. Scharnagel R. Günther K. P. Orthopade. 2007;36:544–551. doi: 10.1007/s00132-007-1103-6. [DOI] [PubMed] [Google Scholar]
- Brunner M. Schwarz T. Zeman F. König M. Grifka J. Benditz A. Arch. Orthop. Trauma Surg. 2018;138:901–909. doi: 10.1007/s00402-018-2916-y. [DOI] [PubMed] [Google Scholar]
- Skinner H. B. Am. J. Orthopsychiatry. 2004;33:5–9. [Google Scholar]
- Fan W. Yung B. Huang P. Chen X. Chem. Rev. 2017;117:13566–13638. doi: 10.1021/acs.chemrev.7b00258. [DOI] [PubMed] [Google Scholar]
- Bosaeus I. Support. Care Cancer. 2008;16:447–451. doi: 10.1007/s00520-007-0388-7. [DOI] [PubMed] [Google Scholar]
- Maddocks M. Hopkinson J. Conibear J. Reeves A. Shaw C. Fearon K. C. H. Curr. Opin. Support. Palliat. Care. 2016;10:298–305. doi: 10.1097/SPC.0000000000000241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo C.-N. Pan J.-J. Huang Y.-W. Tsai H.-J. Chang W.-C. Cancer Epidemiol., Biomarkers Prev. 2018;27:737–745. doi: 10.1158/1055-9965.EPI-17-0876. [DOI] [PubMed] [Google Scholar]
- Hakki S. A. Int. J. Evid. Based Healthc. 2018;5:1660–1663. doi: 10.18410/jebmh/2018/347. [DOI] [Google Scholar]
- Baek S. Singh R. K. Kim T.-H. Seo J. Shin U. S. Chrzanowski W. Kim H.-W. ACS Appl. Mater. Interfaces. 2016;8:8967–8979. doi: 10.1021/acsami.6b00963. [DOI] [PubMed] [Google Scholar]
- Gritsenko K. Khelemsky Y. Kaye A. D. Vadivelu N. Urman R. D. Best Pract. Res., Clin. Anaesthesiol. 2014;28:59–79. doi: 10.1016/j.bpa.2014.03.001. [DOI] [PubMed] [Google Scholar]
- Mehta M., Biopharmaceutics Classification System (BCS): Development, Implementation, and Growth, Wiley, 2017 [Google Scholar]
- FDA, Waiver of In Vivo Bioavailability and Bioequivalence Studies for Immediate-Release Solid Oral Dosage Forms Based on a Biopharmaceutics Classification System Guidance for Industry, 2017 [Google Scholar]
- WHO, General notes on Biopharmaceutics Classification System (BCS)-based biowaiver applications, 2019 [Google Scholar]
- European Medicines Agency, 2018, vol. 44, pp. 1–17 [Google Scholar]
- Ilma N. Dwi U. Benny P. Slamet I. J. Appl. Pharm. Sci. 2018;8:57–63. [Google Scholar]
- Mittapalli S. Mannava M. K. C. Sahoo R. Nangia A. Cryst. Growth Des. 2019;19:219–230. doi: 10.1021/acs.cgd.8b01298. [DOI] [Google Scholar]
- Chou P. C., Elasticity-Tensor, Dyadic and Engineering Approaches, Dover Publications, New York, 1992 [Google Scholar]
- Chattoraj S. Shi L. Chen M. Alhalaweh A. Velaga S. Sun C. C. Cryst. Growth Des. 2014;14:3864–3874. doi: 10.1021/cg500388s. [DOI] [Google Scholar]
- Sun C. C. Hou H. Cryst. Growth Des. 2008;8:1575–1579. doi: 10.1021/cg700843s. [DOI] [Google Scholar]
- Chattoraj S. Shi L. Sun C. C. CrystEngComm. 2010;12:2466. doi: 10.1039/C000614A. [DOI] [Google Scholar]
- Sanphui P. Mishra M. K. Ramamurty U. Desiraju G. R. Mol. Pharmaceutics. 2015;12:889–897. doi: 10.1021/mp500719t. [DOI] [PubMed] [Google Scholar]
- Abbas N. Latif S. Afzal H. Arshad M. S. Hussain A. Sadeeqa S. Bukhari N. I. AAPS PharmSciTech. 2018;19:3249–3257. doi: 10.1208/s12249-018-1152-7. [DOI] [PubMed] [Google Scholar]
- Chen X. Li D. Luo C. Wang J. Deng Z. Zhang H. CrystEngComm. 2018;20:990–1000. doi: 10.1039/C7CE02150J. [DOI] [Google Scholar]
- Souza M. S. Diniz L. F. Vogt L. Carvalho Jr. P. S. D'vries R. F. Ellena J. Cryst. Growth Des. 2018;18:5202–5209. doi: 10.1021/acs.cgd.8b00647. [DOI] [Google Scholar]
- Emami S. Adibkia K. Barzegar-Jalali M. Siahi-Shadbad M. Pharm. Dev. Technol. 2019;24:199–210. doi: 10.1080/10837450.2018.1455210. [DOI] [PubMed] [Google Scholar]
- Thakur T. S. Thakuria R. Cryst. Growth Des. 2020;20:6245–6265. doi: 10.1021/acs.cgd.0c00654. [DOI] [Google Scholar]
- Upadhyay P. P. Bond A. D. CrystEngComm. 2015;17:5266–5272. doi: 10.1039/C5CE00050E. [DOI] [Google Scholar]
- Thomas L. H. Wales C. Wilson C. C. Chem. Commun. 2016;52:7372–7375. doi: 10.1039/C6CC01027J. [DOI] [PubMed] [Google Scholar]
- Sekhon B. S. Daru, J. Pharm. Sci. 2012;20:45. doi: 10.1186/2008-2231-20-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thipparaboina R. Kumar D. Chavan R. B. Shastri N. R. Drug Discovery Today. 2016;21:481–490. doi: 10.1016/j.drudis.2016.02.001. [DOI] [PubMed] [Google Scholar]
- Bolla G. Nangia A. Chem. Commun. 2016;52:8342–8360. doi: 10.1039/C6CC02943D. [DOI] [PubMed] [Google Scholar]
- Remenar J. F. Morissette S. L. Peterson M. L. Moulton B. MacPhee J. M. Guzmán H. R. Almarsson Ö. J. Am. Chem. Soc. 2003;125:8456–8457. doi: 10.1021/ja035776p. [DOI] [PubMed] [Google Scholar]
- Childs S. L. Chyall L. J. Dunlap J. T. Smolenskaya V. N. Stahly B. C. Stahly G. P. J. Am. Chem. Soc. 2004;126:13335–13342. doi: 10.1021/ja048114o. [DOI] [PubMed] [Google Scholar]
- Aitipamula S. Wong A. B. H. Chow P. S. Tan R. B. H. CrystEngComm. 2012;14:8515. doi: 10.1039/C2CE26325D. [DOI] [Google Scholar]
- Aitipamula S. Wong A. B. H. Chow P. S. Tan R. B. H. CrystEngComm. 2014;16:5793. doi: 10.1039/C3CE42182A. [DOI] [Google Scholar]
- López-Cedrún J. Videla S. Burgueño M. Juárez I. Aboul-Hosn S. Martín-Granizo R. Grau J. Puche M. Gil-Diez J. L. Hueto J. A. Vaqué A. Sust M. Plata-Salamán C. Monner A. Casals S. Cebrecos J. Cebrián J. L. García-Linares J. Gascón N. González-Corchón A. Marqués M. Morán M. J. Morte A. Otero A. Ortiz E. Pombo M. Puyada A. Sans A. Sastre J. Velázquez J. M. Drugs R&D. 2018;18:137–148. doi: 10.1007/s40268-018-0235-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gascon N. Almansa C. Merlos M. Miguel Vela J. Encina G. Morte A. Smith K. Plata-Salamán C. Expert Opin. Invest. Drugs. 2019;28:399–409. doi: 10.1080/13543784.2019.1612557. [DOI] [PubMed] [Google Scholar]
- Alavijeh M. S. Chishty M. Qaiser M. Z. Palmer A. M. NeuroRX. 2005;2:554–571. doi: 10.1602/neurorx.2.4.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan M. A. J. Rheumatol. 1987;14:118–123. [PubMed] [Google Scholar]
- Shrestha M. Morgan D. L. Moreden J. M. Singh R. Nelson M. Hayes J. E. Ann. Emerg. Med. 1995;26:682–686. doi: 10.1016/S0196-0644(95)70037-4. [DOI] [PubMed] [Google Scholar]
- Baber N. Halliday L. D. C. Van Den Heuvel W. J. A. Walker R. W. Sibeon R. Keenan J. P. Littler T. Orme M. L. Ann. Rheum. Dis. 1979;38:128–136. doi: 10.1136/ard.38.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujimura A. Kumagai Y. Sugimoto K. Nakashima H. Kajiyama H. Ebihara A. Ohashi K. Eur. J. Clin. Pharmacol. 1990;38:133–137. doi: 10.1007/BF00265971. [DOI] [PubMed] [Google Scholar]
- Khatioda R. Bora P. Sarma B. Cryst. Growth Des. 2018;18:4637–4645. doi: 10.1021/acs.cgd.8b00603. [DOI] [Google Scholar]
- Thakuria R. Sarma B. Crystals. 2018;8:101. doi: 10.3390/cryst8020101. [DOI] [Google Scholar]
- Sokal A. Pindelska E. Szeleszczuk L. Kolodziejski W. Int. J. Pharm. 2017;522:80–89. doi: 10.1016/j.ijpharm.2017.03.004. [DOI] [PubMed] [Google Scholar]
- Sarmah K. K. Boro K. Arhangelskis M. Thakuria R. CrystEngComm. 2017;19:826–833. doi: 10.1039/C6CE02057G. [DOI] [Google Scholar]
- Aitipamula S. Wong A. B. H. Chow P. S. Tan R. B. H. CrystEngComm. 2012;14:8515. doi: 10.1039/C2CE26325D. [DOI] [Google Scholar]
- Karagianni A. Malamatari M. Kachrimanis K. Pharmaceutics. 2018;10:18. doi: 10.3390/pharmaceutics10010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raheem Thayyil A. Juturu T. Nayak S. Kamath S. Adv. Pharm. Bull. 2020;10:203–212. doi: 10.34172/apb.2020.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMA, Eur. Med. Agency, 2015, vol. 44, pp. 1–10 [Google Scholar]
- Cheney M. L. Weyna D. R. Shan N. Hanna M. Wojtas L. Zaworotko M. J. J. Pharm. Sci. 2011;100:2172–2181. doi: 10.1002/jps.22434. [DOI] [PubMed] [Google Scholar]
- Žegarac M. Lekšić E. Šket P. Plavec J. Devčić Bogdanović M. Bučar D.-K. Dumić M. Meštrović E. CrystEngComm. 2014;16:32–35. doi: 10.1039/C3CE42013B. [DOI] [Google Scholar]
- Darwish S. Zeglinski J. Krishna G. R. Shaikh R. Khraisheh M. Walker G. M. Croker D. M. Cryst. Growth Des. 2018;18:7526–7532. doi: 10.1021/acs.cgd.8b01330. [DOI] [Google Scholar]
- Nicolaï B. Fournier B. Dahaoui S. Gillet J.-M. Ghermani N.-E. Cryst. Growth Des. 2019;19:1308–1321. doi: 10.1021/acs.cgd.8b01698. [DOI] [Google Scholar]
- Caira M. R. Bourne S. A. Samsodien H. Engel E. Liebenberg W. Stieger N. Aucamp M. CrystEngComm. 2012;14:2541–2551. doi: 10.1039/C2CE06507J. [DOI] [Google Scholar]
- Wales C. Thomas L. H. Wilson C. C. CrystEngComm. 2012;14:7264. doi: 10.1039/C2CE26069G. [DOI] [Google Scholar]
- Bolla G. Sanphui P. Nangia A. Cryst. Growth Des. 2013;13:1988–2003. doi: 10.1021/cg4000457. [DOI] [Google Scholar]
- Suresh K. Goud N. R. Nangia A. Chem. – Asian J. 2013;8:3032–3041. doi: 10.1002/asia.201300859. [DOI] [PubMed] [Google Scholar]
- Sládková V. Cibulková J. Eigner V. Šturc A. Kratochvíl B. Rohlíček J. Cryst. Growth Des. 2014;14:2931–2936. doi: 10.1021/cg500226z. [DOI] [Google Scholar]
- Bernasconi D. Bordignon S. Rossi F. Priola E. Nervi C. Gobetto R. Voinovich D. Hasa D. Duong N. T. Nishiyama Y. Chierotti M. R. Cryst. Growth Des. 2020;20:906–915. doi: 10.1021/acs.cgd.9b01299. [DOI] [Google Scholar]
- Fábián L. Hamill N. Eccles K. S. Moynihan H. A. Maguire A. R. McCausland L. Lawrence S. E. Cryst. Growth Des. 2011;11:3522–3528. doi: 10.1021/cg200429j. [DOI] [Google Scholar]
- Ando S. Kikuchi J. Fujimura Y. Ida Y. Higashi K. Moribe K. Yamamoto K. J. Pharm. Sci. 2012;101:3214–3221. doi: 10.1002/jps.23158. [DOI] [PubMed] [Google Scholar]
- Majumder M. Buckton G. Rawlinson-Malone C. F. Williams A. C. Spillman M. J. Pidcock E. Shankland K. CrystEngComm. 2013;15:4041. doi: 10.1039/C3CE40367J. [DOI] [Google Scholar]
- Sanphui P. Bolla G. Nangia A. Chernyshev V. IUCrJ. 2014;1:136–150. doi: 10.1107/S2052252514004229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S.-W. Brunskill A. P. J. Schwartz E. Sun S. Cryst. Growth Des. 2017;17:2836–2843. doi: 10.1021/acs.cgd.7b00308. [DOI] [Google Scholar]
- Yuliandra Y. Zaini E. Syofyan S. Pratiwi W. Putri L. Pratiwi Y. Arifin H. Sci. Pharm. 2018;86:23. doi: 10.3390/scipharm86020023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribas M. M. Aguiar G. P. S. Muller L. G. Siebel A. M. Lanza M. Oliveira J. V. Ind. Crops Prod. 2019;139:111537. doi: 10.1016/j.indcrop.2019.111537. [DOI] [Google Scholar]
- Surov A. O. Voronin A. P. Manin A. N. Manin N. G. Kuzmina L. G. Churakov A. V. Perlovich G. L. Mol. Pharmaceutics. 2014;11:3707–3715. doi: 10.1021/mp5004652. [DOI] [PubMed] [Google Scholar]
- Guo M. Wang K. Hamill N. Lorimer K. Li M. Mol. Pharmaceutics. 2016;13:3292–3307. doi: 10.1021/acs.molpharmaceut.6b00612. [DOI] [PubMed] [Google Scholar]
- Chandel N. Gupta V. Pandey A. Saxena S. Sheetal C. Int. J. Pharm. Life Sci. 2011;2(8):1020–1028. [Google Scholar]
- Majumder M. Buckton G. Rawlinson-Malone C. Williams A. C. Spillman M. J. Shankland N. Shankland K. CrystEngComm. 2011;13:6327. doi: 10.1039/C1CE05650F. [DOI] [Google Scholar]
- Nechipadappu S. K. Tekuri V. Trivedi D. R. J. Pharm. Sci. 2017;106:1384–1390. doi: 10.1016/j.xphs.2017.01.033. [DOI] [PubMed] [Google Scholar]
- Harmsen B. Leyssens T. Cryst. Growth Des. 2018;18:441–448. doi: 10.1021/acs.cgd.7b01431. [DOI] [Google Scholar]
- Shinozaki T. Ono M. Higashi K. Moribe K. J. Pharm. Sci. 2019;108:2383–2390. doi: 10.1016/j.xphs.2019.02.014. [DOI] [PubMed] [Google Scholar]
- DiMasi J. A. Grabowski H. G. Hansen R. W. J. Health Econ. 2016;47:20–33. doi: 10.1016/j.jhealeco.2016.01.012. [DOI] [PubMed] [Google Scholar]












