Abstract
Patient’s active participation in therapy is a key component of successful rehabilitation. In fact, low participation has been shown to be a prognostic factor of poor outcome; however, participation is rarely assessed in clinical settings. The Pittsburgh Rehabilitation Participation Scale (PRPS) is a validated, quick, and accurate measure of participation, relying on clinicians’ observation, and not requiring any self-report by patients. The aim of this study was to validate an Italian version of the PRPS. Following forward and back-translation of PRPS into Italian, the translated version was validated in a total of 640 therapy sessions, related to a cohort of 32 patients admitted to an Italian hospital. It was tested for concurrent validity, finding significant correlations with Barthel Index (R > 0.58, p < 0.001) and SF-36 Physical and Mental Health (R > 0.4, p < 0.02), for predictive validity, finding significant correlation with the effectiveness of rehabilitation (R = 0.358, p = 0.045), and for inter-rater and intra-rater reliability, computing an Intra-class correlation coefficient (ICC = 0.926 and 0.756, respectively). These psychometric properties results were similar to those of the original version of this scale. The proposed PRPS can be helpful for Italian clinicians in the assessment of patient’s participation during rehabilitation.
Keywords: rehabilitation, neurorehabilitation, participation, compliance, stroke, psychometry, reliability, validity
1. Introduction
Patient’s active participation to their own therapy has progressively been considered as a key point for a patient-centered treatment [1], and as a relevant factor influencing the efficacy of rehabilitation [2]. Patient’s motivation has been stated as the most important, although the most difficult, part of the work of the therapeutic professions [1]. In fact, participation is associated with the treatment outcome in terms of autonomy in activities of daily living (ADL) and of mobility [3]. Despite this interest about the role played by an active patient’s participation during therapy, only a few studies have assessed it [3,4,5,6,7,8].
Poor participation in rehabilitation could be due to many different factors: older age, depression, apathy, cognitive impairment, severe motor impairment, immobility syndrome, low self-efficacy, low confidence in the therapist’s ability to successfully rehabilitate, fatigue, comorbidities such as cardiac diseases, and personality factors [4,9].
Some studies measured the intensity of therapy in terms of total hours per day [10,11]. Although intensity is important, a crucial dimension is the quality of the interaction between patient and therapist for its potential role in rehabilitation, an aspect rarely evaluated. The quality of this interaction should be carefully assessed, especially in experimental rehabilitative programs, including those in which the patient–therapist interaction is mediated by a device related to newly emerging rehabilitation technologies [12,13].
Furthermore, patient’s participation is considered as a process that allows patients to be an integral part of the decisions and of the activities that influence their health [14]. In fact, patient participation is acknowledged as a key component of quality and effective rehabilitation, and it should be a core element of person-centered care, an approach focused on the patients’ individual needs, wants, and preferences [2].
The Pittsburgh Rehabilitation Participation Scale (PRPS) has been validated as the first published scale for rating patient participation [8]. This scale measures the participation of patients in their physical and occupational therapy. It is a very simple scale, with a single item having 6 possible scores: (1) no participation (the patient refused the entire session); (2) poor; (3) fair; (4) good; (5) very good; and (6) excellent participation (the patient participated in all exercises with maximal effort, finished all exercises, and actively took interest in exercises and/or future therapy sessions). The original version of this scale is reported in the Supplementary Material with detailed descriptions of the above six levels. This scale relies on clinicians’ observation, requiring no self-reported data from the patients [8]. The objective of this study was to validate an Italian version of the PRPS.
2. Materials and Methods
The validation of an Italian version of PRPS included two main parts: the translation procedure, and the evaluation of its psychometric properties compared with those of the original version of the scale [8]. The translating procedure [15,16] and that for evaluating psychometric properties were similar to those already performed for validating other clinical scales in previous studies [8,17,18].
The translation procedure included three steps. Firstly, two official translators, English native speakers, independently of each other, translated the original PRPS into Italian language (forward translation). This phase involved the joint work of a translator with a technical background and one with a medical background, the latter also judging the efficiency of the translation. Subsequently, two bilingual people, independently from each other and unaware of the original version, translated the Italian scale into English. These last two translations of the English-language scale were then independently re-translated into Italian by two health professionals with English language certification, unaware of the original version (backward translation). Lastly, all the translators gathered to decide the definitive translation of the PRPS Scale. With the purpose of adapting the translated scale to Italian culture, the translated scale was reanalyzed by a group of experts specializing in different medical disciplines. Experts had the opportunity to comment on elements of the translation by inserting their comments on a form. Once tested for validity and reliability, the translation judge examined this final version of cultural adaptation and approved it. The final Italian version of PRPS is reported in the Supplementary Material of this paper. Given its simplicity, neither particular difficulties nor controversies were recorded in the translation process described above.
For the validation process, a cohort of patients admitted in different complex operative neurorehabilitation units of an Italian hospital was recruited. Patients aged under 18 years were excluded, as were patients with severe cognitive disabilities, and non-native Italian speakers.
The Italian version of PRPS was administered to 32 patients during the first and the last ten sessions of physical therapy during their stay in a neurorehabilitation hospital (for a total of 640 therapies). Twenty-six of the 32 enrolled patients were further evaluated in their first session by a second therapist blind to the scoring of the first. This last procedure allowed for assessing the inter-rater reliability according to the procedure already employed in the original PRPS standardization [8]. As in that study, we also evaluated the inter-rater reliability by means of Two-Way Random, Single-Measure, Intra-class Correlation Coefficient (ICC(2,1)). The intra-rater reliability was assessed by a single therapist separately evaluating the 10 first and 10 last sessions of 32 patients by computing the One-Way Random, Single-Measure, Intra-class Correlation Coefficient (ICC(1,1)). Furthermore, the Cronbach’s alpha was also computed in our study.
Concurrent validity was measured by comparing the average PRPS assessed in the first and last ten sessions with the admission and discharge scores of the Barthel Index, respectively, and a 36-Item Short Form Survey (SF-36) by means of Spearman’s correlation coefficient (R). The validated Italian version of Barthel Index (BI) was used [15]. BI assesses the independency in the activities of daily living; it is formed of ten items and has a total score ranging from 0 (total dependency) to 100 (total independency). BI was preferred to the functional independence measure used in the original study [8], because BI is more common in neurorehabilitation and especially in Europe [18] (in particular in Italy: many regional healthcare systems adopt the BI as the main standard outcome). The validated Italian version of the SF-36 was used for the assessment of health-related quality of life, covering two main domains: physical and mental health [17].
Predictive validity was assessed by means of the correlation coefficient computed between the mean PRPS averaged among the first 10 sessions, with the effectiveness of rehabilitation evaluated as the percentage change in the scores of BI and SF-36 from admission to discharge, with respect to the maximum obtainable change [19]. Wilcoxon rank test was used to assess the change between admission and discharge scores. Finally, the responsiveness of PRPS was computed by assessing the probability of very good or excellent participation (scores 5 or 6) in the first/last session of therapy associated to the BI score at admission/discharge, respectively (BI score was categorized in groups of 10 points). A parameter logistic model, conventionally used in item response theory, was used for fitting the data by means of the least squares method. All statistical analyses were performed using the Statistical Package of Social Sciences (SPSS), version 23.0 for Windows.
The study was approved by the Independent Local Ethics Committee of the hospital in which data were collected, and all participants signed an informed consent form.
3. Results
The demographic and clinical characteristics of the enrolled sample are shown in Table 1. From admission to discharge, a significant wide improvement was observed for BI score (p < 0.001). Additionally, quality of life slightly, but significantly, improved (SF-36PH: p = 0.018 and SF-36MF: p = 0.005). Participation in rehabilitation assessed with the proposed Italian version of PRPS slightly but significantly varied between the first and the last session of therapy (p = 0.04). Conversely, the PRPS score was not significantly different between the first and the tenth session of therapy.
Table 1.
Mean ± standard deviation or percentages of demographical and clinical features.
| Parameter | Description | Values |
|---|---|---|
| Age | Years | 60.3 ± 18.0 |
| Gender | Male | 62.5% |
| Female | 37.5% | |
| Pathology | Stroke | 37.5% |
| Other Neurological Disorders | 28.1% | |
| Orthopedic Pathologies | 34.4% | |
| Barthel Index | Admission | 59.9 ± 28.0 |
| Discharge | 73.4 ± 25.5 | |
| Effectiveness | 39.4 ± 42.2% | |
| SF-36 Physical Health | Admission | 40.7 ± 7.3 |
| Discharge | 43.8 ± 8.8 | |
| Effectiveness | 5.0 ± 13.0% | |
| SF-36 Mental Health | Admission | 41.1 ± 9.5 |
| Discharge | 46.8 ± 10.3 | |
| Effectiveness | 8.6 ± 16.4% | |
| PRPS | Therapist 1 First session | 4.6 ± 1.3 |
| Therapist 2 First session | 4.8 ± 1.1 | |
| Therapist 1 First 10 sessions | 4.8 ± 1.0 | |
| Therapist 1 Last 10 sessions | 5.0 ± 0.9 | |
| Therapist 1 Last session | 5.1 ± 0.8 |
In the first session of rehabilitation, the two raters assigned the same scores in 77% of cases, with a difference of only one point in the other 23% of cases. The resulting inter-rater reliability for the Italian version of PRPS was statistically significant, with an ICC = 0.926 (Table 2). Additionally, the intra-rater reliability was statistically significant, with values of ICC > 0.7 both in the first and the last ten sessions of physical therapy (Table 2).
Table 2.
Comparisons of the psychometric properties of the Italian version of PRPS and those found in the original study [8] (BI stands for Barthel Index, FIM for motor domain of the functional independence measure, SF-36 for Short Form, PH for physical health, MH for mental health, ICC is intra-class correlation coefficient, R stands for Pearson’s correlation coefficient in the original study and for Spearman correlation coefficient in our study, 10S stands for ten sessions of therapy).
| Psychometric Properties of PRPS | Results of the Italian Version of PRPS | Results of the Original Study on PRPS [8] |
|---|---|---|
| Mean PRPS score | 4.91 ± 1.03 (range: 1–6) | 4.73 ± 0.76 (range not reported) |
| PRPS score increment | From 4.78 ± 1.24 to 4.87 ± 1.13 in 9 sessions (p = 0.47, Wilcoxon test) From to 4.78 ± 1.24 to 5.13 ± 0.79 in all sessions (p = 0.04, Wilcoxon test) |
From 4.29 ± 0.93 to 4.67 ± 1.04 in 9 sessions (p < 0.0001, t-test) |
| Inter-rater reliability | ICC = 0.926 Cronbach’s alpha = 0.962 |
ICC = 0.91 for occupational therapists ICC = 0.96 for physical therapists |
| Intra-rater reliability | ICC = 0.844, Cronbach’s alpha = 0.982 (first 10S) ICC = 0.756, Cronbach’s alpha = 0.969 (last 10S) |
Not assessed |
| Concurrent validity |
R = 0.633 (p < 0.001) with BI R = −0.400 (p = 0.023) with age R = 0.518 (p = 0.002) with SF-36PH R = 0.433 (p = 0.013) with SF-36MH |
R = 0.38 (p < 0.001) with FIM R = −0.21 (p < 0.001) with age |
| Predictive Validity |
R = 0.358 (p = 0.045) with BI-effectiveness R = 0.222 (p = 0.222) with SF36PH-effectiveness R = 0.035 (p = 0.851) with SF36MH-effectiveness |
R = 0.32 (p < 0.001) with change in FIM R = −0.13 (p < 0.05) with length of stay |
Regarding concurrent validity, the scores of the Italian version of PRPS were significantly correlated with the BI scores and SF scores at both admission and discharge (Table 2). Then, the scores of the Italian version of the PRPS assessed in the first 10 sessions were found to be significantly correlated with the effectiveness of therapy in terms of BI scores, but not of SF-36 scores (Table 2).
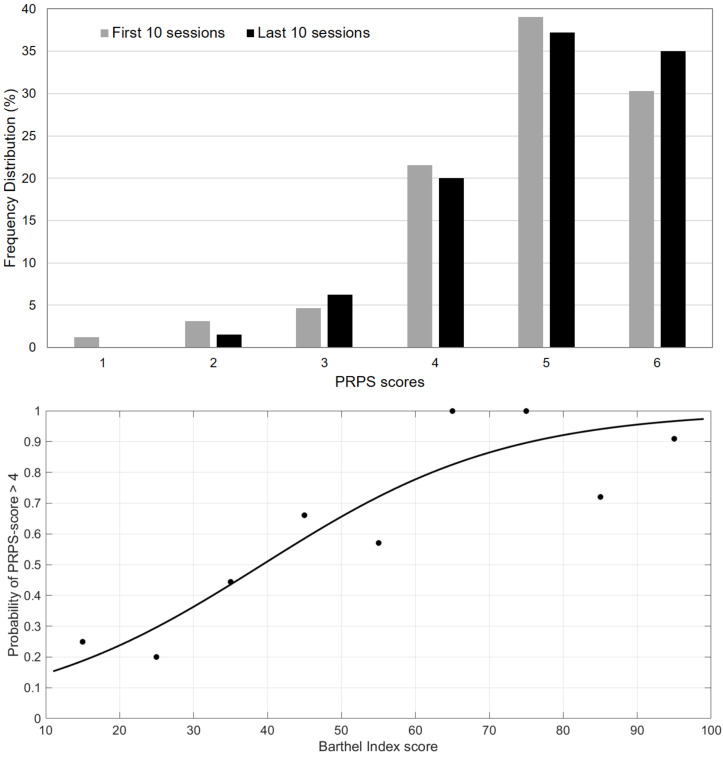
The frequency distribution of the PRPS scores is reported in Figure 1. The upper plot shows that in most of the sessions the scoring ranged from 4 to 6, both in the first and in the last sessions. The minimum score of PRPS (score = 1) was recorded in 1.2% of cases, related to 4 of the first sessions of a single patient. He had a stroke, and he was the most severely affected patient at admission (BI = 10) and the second oldest participant (age = 85 years). However, in the last sessions of therapy, his participation increased to a PRPS score of 5, and he was discharged with a BI score of 30. The lower plot of Figure 1 shows the distribution of PRPS scores with respect to the simultaneous assessment of BI scores (occurring at the first session at admission and at the last session at discharge). According to the paradigm of the item response theory, higher PRPS scores were found more frequently in patients with higher ability in terms of BI scores (as confirmed by a coefficient of determination of the Parameter Logistic Model of 0.815).
Figure 1.
Frequency distribution of PRPS score. In the above plot are the distribution of scores in the first (grey bars) and last (black bars) ten sessions. In the below plot are the percentages of PRPS scores equal to 5 (very good) or 6 (excellent) in the first and last sessions associated to the BI score at admission and discharge, respectively (dots represent data, whereas the curve represents the fit obtained using a Parameter Logistic Model).
4. Discussion
The psychometric analysis of the proposed Italian version of the PRPS showed good results in terms of intra- and inter-rater reliability, concurrent validity, predictive validity, and responsiveness. As shown in Table 2, the psychometric properties of the Italian version of the PRPS were close to those found in the original study [8]. The correlation coefficients evaluated for assessing concurrent validity were even superior in our study, despite being not very high and less significant than those found by Lenze and colleagues [8] for the differences in sample sizes between the two studies. The predictive validity was confirmed by a statistically significant correlation between the average score of the PRPS assessed in the first 10 sessions of physical therapy and the effectiveness of therapy evaluated in terms of improvement in terms of Barthel Index score. This finding was in accordance with previous studies on the potential role of participation as a prognostic factor of rehabilitation outcome [2,4,6]. However, the predictive capacity was not significant in terms of SF-36 scores, neither for physical nor for mental health-related domain. However, it should be noted that patients showed a slight improvement in terms of quality of life (less than 10% of the maximum possible improvement), despite a gain in the independency in the activities of daily living of about 40% of the maximum achievable. The proposed Italian version of PRPS was able to predict this last high improvement.
We also found a significant improvement in the PRPS score from the first to the last sessions of rehabilitation, similar to that observed in the original study [8]. In general, the psychometric properties of the proposed Italian version of the PRPS were in line with those of the PRPS reported in the original study [8]. The inter-rater reliability between physical therapists found for the Italian version was 0.926; it was 0.96 in the original study [8]. The intra-rater reliability, not assessed for the original version of the PRPS, was statistically significant in our study, with values of ICC higher than 0.7 both at admission and discharge. The concurrent validity in our study was assessed by R > 0.58, when the mean PRPS was compared with BI scores at admission or discharge, whereas in the original study it was R = 0.38 when the mean PRPS was compared to the motor domain of the functional independence measure evaluated at admission [8]. The predictive validity in the original study was computed with the correlation between mean PRPS and change in functional independence measure finding an R = 0.32 [8]. We found a similar result when testing the correlation between the mean PRPS evaluated in the first ten sessions and the effectiveness in terms of the Barthel Index, which assesses the independency in the activities of daily living with a similar value of correlation: R = 0.358 [2,8].
Lenze and colleagues found a slight increment of PRPS in the first nine therapy sessions after admission (of about 0.4 points) [8]. We also found a slight improvement in PRPS score from admission to discharge (0.5 points), but in more than twenty sessions. In that study and ours, patients were elderly with neurological (about two-thirds) and orthopedic (about one-third) diseases. These conditions (aging and diseases) are known to often be associated with depression and cognitive difficulties: neurological damages impact physical, cognitive, psychological, and emotional functioning, as well as quality of life [20,21]. According to these observations, and also in our study, neither physical nor mental domains of quality of life showed a wide improvement. However, the mental health at admission was found to be significantly correlated to the participation in rehabilitation treatment.
On average, our PRPS score was slightly higher than that recorded in the original study [8] and increased less in the first nine sessions. It is noteworthy that more than 90% of sessions received a PRPS score equal to 4, 5 or 6. The first three scores were rarely recorded, but they were associated to severely affected patients. On one hand, this low sensitivity may reduce the use of this scale in clinical settings with less severely impaired patients; on the other hand, the sporadic refusal of therapy could be considered as an important alarm for clinicians because it may limit the efficacy of the entire rehabilitation.
Our study confirmed that patient’s participation is one of the most reliable predictors of rehabilitation outcome, and physical therapists should carefully take into account this issue in their clinical practice, when cognitive problems also subsist. The important role of participation in the rehabilitation process should be quantitatively assessed and increased because it may help to reduce long-term disability [2], according to the main aim of rehabilitation as defined by the World Health Organization [22].
The main aim of this study was to propose an Italian version of the PRPS, and we found psychometric properties similar to the original version of PRPS. However, the results of our study should be considered despite its limits. The most important limitation is the reduced size of the enrolled patient sample. It should be noted that the validity and reliability of PRPS was already proven in the original [8] and other [2,4] studies; we just tested the Italian version of this scale, although given our reduced sample size we did not test the PRPS scores among patients with different pathologies, as performed in the original study [8]. Another limitation could be that inter-rater reliability was tested on two therapists. We evaluated the intra-rater reliability: this measure was absent from the original study [8]. The number of evaluated sessions for each patient was higher in our study than in the original (20 vs. 9). Our study also showed a limitation of the scale, related to not-homogenous frequency distribution of its scores, with the upper scores more frequent than the lower ones.
The development of the PRPS and subsequent validations in different languages could be helpful for therapists and clinicians for taking into account the participation of patients in their own therapy sessions, a factor strictly correlated to functional outcomes. Furthermore, with the wide diffusions of innovative rehabilitation methods, especially those involving new technologies, it could be fundamental to assess the active participation of patients to these new approaches [12,13,23,24]. In fact, especially for elderly patients, some technologies could be alienating and generate anxiety, risking patients abandoning therapy [25]. However, cognitive factors could influence the outcome of technological rehabilitation [26]. In this scenario, it is also fundamental for clinical staff to understand the needs and expectations of patients for increasing their motivation during therapy [27]. Properly developing motivating tasks, and also exploiting new technologies, may increase the participation of subjects, therefore reducing perceived fatigue during therapy [28]. Another crucial aspect is that the participation of patients to therapy could depend on their relationship with the therapist. In fact, therapeutic relationships could vary depending on patient’s and therapist’s expected outcomes, on their interpersonal affective bonding, on their reactions to difficulties [29], and it could even vary over time [29]. This relationship may also depend on the patient’s trust in the therapist’s abilities, a factor that may improve active participation in therapy [30], impacting the attitudes and expectations of patients’ familiars and caregivers, and on the eventual presence of psychological support [31]. Diffusion of the PRPS, validated in different languages across the world, could provide a deeper insight in these aspects for improving therapeutic alliance among stakeholders, and hence rehabilitation outcomes.
5. Conclusions
The proposed Italian version of the Pittsburgh Rehabilitation Participation Scale (PRPS) showed concurrent validity, a predictive validity, and an inter-rater reliability similar to those found for the original version of this scale [8]. Additionally, the properties of intra-rater reliability and responsiveness were satisfied by the Italian version of PRPS. Despite the limitations of our study described above and those of this scale, which should be carefully taken into account, the ease of using the PRPS could allow for progressive assessment of patients’ participation in their own rehabilitation.
Supplementary Materials
The original and Italian versions of PRPS are available online at https://www.mdpi.com/2076-3425/11/5/626/s1. Table S1: On the left the original PRPS validated in English, on the right the proposed Italian version of PRPS.
Author Contributions
Conceptualization, G.M., G.F.S. and S.P.; methodology, G.G. and G.F.S.; software, G.G. and M.I.; validation, G.G., M.I., G.A. and G.F.S.; formal analysis, G.G., I.R. and M.I.; investigation, D.D.B. and V.R.; resources, S.P., G.F.S. and G.A.; data curation, D.D.B., V.R. and I.R.; writing—original draft preparation, G.G.; writing—review and editing, M.I.; visualization, M.I, M.T. and I.C.; supervision, S.P. and G.A.; project administration, S.P. and G.A.; funding acquisition, S.P. and G.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research was performed in the framework of Research Line D of IRCCS Fondazione Santa Lucia and Excellence Project PACE (Psychological Adaptation to ever Changing Environments) of Department of Psychology of Sapienza University of Rome.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Independent Ethics Committee of IRCCS Fondazione Santa Lucia (Protocol registered with the code: CE/PROG.743 approved on 10th April 2019).
Informed Consent Statement
Signed informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data of this study are published in a private repository on Zenodo, and can be available upon reasonable request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mead N., Bower P. Patient-centredness: A conceptual framework and review of the empirical literature. Soc. Sci. Med. 2000;51:1087–1110. doi: 10.1016/S0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 2.Paolucci S., Di Vita A., Massicci R., Traballesi M., Bureca I., Matano A., Iosa M., Guariglia C. Impact of participation on rehabilitation results: A multivariate study. Eur. J. Phys. Rehabil. Med. 2012;48:455–466. [PubMed] [Google Scholar]
- 3.MacLean N., Pound P. A critical review of the concept of patient motivation in the literature on physical rehabilitation. Soc. Sci. Med. 2000;50:495–506. doi: 10.1016/s0277-9536(99)00334-2. [DOI] [PubMed] [Google Scholar]
- 4.Salter K.L., Foley N.C., Jutai J.W., Teasell R.W. Assessment of participation outcomes in randomized controlled trials of stroke rehabilitation interventions. Int. J. Rehabil. Res. 2007;30:339–342. doi: 10.1097/MRR.0b013e3282f144b7. [DOI] [PubMed] [Google Scholar]
- 5.Morghen S., Morandi A., Guccione A.A., Bozzini M., Guerini F., Gatti R., Del Santo F., Gentile S., Trabucchi M., Bellelli G. The association between patient participation and functional gain following inpatient rehabilitation. Aging Clin. Exp. Res. 2017;29:729–736. doi: 10.1007/s40520-016-0625-3. [DOI] [PubMed] [Google Scholar]
- 6.Lenze E.J., Munin M.C., Quear T., Dew M.A., Rogers J.C., Begley A.E., Reynolds C.F. Significance of poor patient par-ticipation in physical and occupational therapy for functional outcome and length of stay. Arch. Phys. Med. Rehabil. 2004;85:1599–1601. doi: 10.1016/j.apmr.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 7.Hershkovitz A., Kalandariov Z., Hermush V., Weiss R., Brill S. Factors Affecting Short-Term Rehabilitation Outcomes of Disabled Elderly Patients With Proximal Hip Fracture. Arch. Phys. Med. Rehabil. 2007;88:916–921. doi: 10.1016/j.apmr.2007.03.029. [DOI] [PubMed] [Google Scholar]
- 8.Lenze E.J., Munin M.C., Quear T., Dew M.A., Rogers J.C., Begley A.E., Reynolds C.F. The Pittsburgh Rehabilitation Par-ticipation Scale: Reliability and validity of a clinician-rated measure of participation in acute rehabilitation. Arch. Phys. Med. Rehabil. 2004;85:380–384. doi: 10.1016/j.apmr.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 9.Yang S.-Y., Kong K.H. Level and predictors of participation in patients with stroke undergoing inpatient rehabilitation. Singap. Med. J. 2013;54:564–568. doi: 10.11622/smedj.2013201. [DOI] [PubMed] [Google Scholar]
- 10.Merlo A.R., Goodman A., McClenaghan B.A., Fritz S.L. Participants’ Perspectives on the Feasibility of a Novel, Intensive, Task-Specific Intervention for Individuals with Chronic Stroke: A Qualitative Analysis. Phys. Ther. 2013;93:147–157. doi: 10.2522/ptj.20110147. [DOI] [PubMed] [Google Scholar]
- 11.Gittins M., Vail A., Bowen A., Lugo-Palacios D., Paley L., Bray B., Gannon B., Tyson S. Factors influencing the amount of therapy received during inpatient stroke care: An analysis of data from the UK Sentinel Stroke National Audit Programme. Clin. Rehabil. 2020;34:981–991. doi: 10.1177/0269215520927454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morone G., Paolucci S., Mattia D., Pichiorri F., Tramontano M., Iosa M. The 3Ts of the new millennium neurorehabilita-tion gym: Therapy, technology, translationality. Expert Rev. Med. Devices. 2016;13:785–787. doi: 10.1080/17434440.2016.1218275. [DOI] [PubMed] [Google Scholar]
- 13.Morone G., Spitoni G.F., De Bartolo D., Ghanbari Ghooshchy S., Di Iulio F., Paolucci S., Zoccolotti P., Iosa M. Rehabilitative devices for a top-down approach. Expert Rev. Med. Devices. 2019;16:187–195. doi: 10.1080/17434440.2019.1574567. [DOI] [PubMed] [Google Scholar]
- 14.Souliotis K., Agapidaki E., Peppou L.E., Tzavara C., Varvaras D., Buonomo O.C., Debiais D., Hasurdjiev S., Sarkozy F. Assessing Patient Organization Participation in Health Policy: A Comparative Study in France and Italy. Int. J. Health Policy Manag. 2018;7:48–58. doi: 10.15171/ijhpm.2017.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castiglia S.F., Galeoto G., Lauta A., Palumbo A., Tirinelli F., Viselli F., Santilli V., Sacchetti M.L. The culturally adapted Italian version of the Barthel Index (IcaBI): Assessment of structural validity, inter-rater reliability and responsiveness to clin-ically relevant improvements in patients admitted to inpatient rehabilitation centers. Funct. Neurol. 2017;22:221–228. doi: 10.11138/FNeur/2017.32.4.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Apolone G., Mosconi P. The Italian SF-36 Health Survey: Translation, validation and norming. J. Clin. Epidemiol. 1998;51:1025–1036. doi: 10.1016/S0895-4356(98)00094-8. [DOI] [PubMed] [Google Scholar]
- 17.Carlsson A.M. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. 1983;16:87–101. doi: 10.1016/0304-3959(83)90088-X. [DOI] [PubMed] [Google Scholar]
- 18.Sangha H., Lipson D., Foley N., Salter K., Bhogal S., Pohani G., Teasell R.W. A comparison of the Barthel Index and the Functional Independence Measure as outcome measures in stroke rehabilitation: Patterns of disability scale usage in clinical trials. Int. J. Rehabil. Res. 2005;28:135–139. doi: 10.1097/00004356-200506000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Shah S., Vanclay F., Cooper B. Efficiency, effectiveness, and duration of stroke rehabilitation. Stroke. 1990;21:241–246. doi: 10.1161/01.STR.21.2.241. [DOI] [PubMed] [Google Scholar]
- 20.Cumming T.B., Marshall R.S., Lazar R.M. Stroke, Cognitive Deficits, and Rehabilitation: Still an Incomplete Picture. Int. J. Stroke. 2013;8:38–45. doi: 10.1111/j.1747-4949.2012.00972.x. [DOI] [PubMed] [Google Scholar]
- 21.Park J.H., Kim B.J., Bae H.J., Lee J., Lee J., Han M.K. Impact of Post-Stroke Cognitive Impairment with No Dementia on Health-Related Quality of Life. J. Stroke. 2013;15:49–56. doi: 10.5853/jos.2013.15.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.WHO Expert Committee on Disability Prevention and Rehabilitation. Disability prevention and rehabilitation. World Health Organ. Tech. Rep. Ser. 1981;668:1–39. [PubMed] [Google Scholar]
- 23.Tramontano M., Morone G., Palomba A., De Angelis S., Mercuro A., Caltagirone C., Grasso M.G. Effectiveness of a sensor-based technology in upper limb motor recovery in post-acute stroke neurorehabilitation: A randomized controlled trial. J. Biol. Regul. Homeost. Agents. 2021;34:165–174. [PubMed] [Google Scholar]
- 24.Tramontano M., Morone G., De Angelis S., Casagrande Conti L., Galeoto G., Grasso M.G. Sensor-based technology for upper limb rehabilitation in patients with multiple sclerosis: A randomized controlled trial. Restor. Neurol. Neurosci. 2020;38:333–341. doi: 10.3233/rnn-201033. [DOI] [PubMed] [Google Scholar]
- 25.Bragoni M., Broccoli M., Iosa. M., Morone G., De Angelis D., Venturiero V., Coiro P., Pratesi L., Mezzetti G., Fusco A., et al. Influence of psychologic features on rehabilitation outcomes in patients with subacute stroke trained with robotic-aided walking therapy. Am. J. Phys. Med. Rehabil. 2013;92:e16–e25. doi: 10.1097/PHM.0b013e3182a20a34. [DOI] [PubMed] [Google Scholar]
- 26.De Bartolo D., Spitoni G.F., Iosa M., Morone G., Ciancarelli I., Paolucci S., Antonucci G. From movement to thought and back: A review on the role of cognitive factors influencing technological neurorehabilitation. Funct. Neurol. 2020;34:131–144. [PubMed] [Google Scholar]
- 27.De Bartolo D., Morone G., Lupo A., Aloise F., Baricich A., Di Francesco D., Calderone C., Cisari C., Verdecchia G., Sandrini G., et al. From paper to informatics: The Post Soft Care-App, an easy-to-use and fast tool to help therapists identify unmet needs in stroke patients. Funct. Neurol. 2018;33:200–205. [PubMed] [Google Scholar]
- 28.Iosa M., Aydin M., Candelise C., Coda N., Morone G., Antonucci G., Marinozzi F., Bini F., Paolucci S., Tieri G. The Michelangelo Effect: Art Improves the Performance in a Virtual Reality Task Developed for Upper Limb Neurorehabilitation. Front. Psychol. 2021;11:611956. doi: 10.3389/fpsyg.2020.611956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Horton A., Hebson G., Holman D. A longitudinal study of the turning points and trajectories of therapeutic relationship development in occupational and physical therapy. BMC Heal. Serv. Res. 2021;21:1–14. doi: 10.1186/s12913-021-06095-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vestøl I., Debesay J., Pajalic Z., Bergland A. The importance of a good therapeutic alliance in promoting exercise motivation in a group of older Norwegians in the subacute phase of hip fracture; a qualitative study. BMC Geriatr. 2020;20:118. doi: 10.1186/s12877-020-01518-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van Willigen Z., Ostler C., Thackray D., Cusack R. Patient and family experience of physical rehabilitation on the intensive care unit: A qualitative exploration. Physiotherapy. 2020;109:102–110. doi: 10.1016/j.physio.2020.01.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data of this study are published in a private repository on Zenodo, and can be available upon reasonable request to the corresponding author.