Abstract
Aims
Unicompartmental knee arthroplasty (UKA) is a bone-preserving treatment option for osteoarthritis localized to a single compartment in the knee. The success of the procedure is sensitive to patient selection and alignment errors. Robotic arm-assisted UKA provides technological assistance to intraoperative bony resection accuracy, which is thought to improve ligament balancing. This paper presents the five-year outcomes of a comparison between manual and robotically assisted UKAs.
Methods
The trial design was a prospective, randomized, parallel, single-centre study comparing surgical alignment in patients undergoing UKA for the treatment of medial compartment osteoarthritis (ISRCTN77119437). Participants underwent surgery using either robotic arm-assisted surgery or conventional manual instrumentation. The primary outcome measure (surgical accuracy) has previously been reported, and, along with secondary outcomes, were collected at one-, two-, and five-year timepoints. Analysis of five-year results and longitudinal analysis for all timepoints was performed to compare the two groups.
Results
Overall, 104 (80%) patients of the original 130 who received surgery were available at five years (55 robotic, 49 manual). Both procedures reported successful results over all outcomes. At five years, there were no statistical differences between the groups in any of the patient reported or clinical outcomes. There was a lower reintervention rate in the robotic arm-assisted group with 0% requiring further surgery compared with six (9%) of the manual group requiring additional surgical intervention (p < 0.001).
Conclusion
This study has shown excellent clinical outcomes in both groups with no statistical or clinical differences in the patient-reported outcome measures. The notable difference was the lower reintervention rate at five years for roboticarm-assisted UKA when compared with a manual approach.
Cite this article: Bone Joint J 2021;103-B(6):1088–1095.
Keywords: Knee arthroplasty, Unicompartmental, Robotic arm-assisted, UKA
Introduction
Unicompartmental knee arthroplasty (UKA) is one of the current surgical treatment options for medial compartment knee osteoarthritis (OA). There is continuing debate over the advantages or disadvantages when compared to total knee arthroplasty (TKA) and high tibial osteotomy. UKA has been shown to offer faster postoperative recovery, less postoperative pain, and lower rates of thromboembolism, cerebrovascular events, infection, and 30-day mortality, compared to TKA.1
Those benefits must be balanced against published data from registries showing reduced long-term survivorship of UKA compared to TKA.2-4 Errors in alignment of the UKA implants, poor patient selection, and low-volume centres have been proposed as risk factors for reduced long-term survival.5 In a large, randomized controlled trial (RCT), Beard et al6 demonstrated a substantially lower number of revisions, high satisfaction, and improved cost-effectiveness of manual UKAs compared to TKAs, “when performed by those with adequate experience”.
Data from national joint registries suggest that uptake of UKAs has plateaued at 8% of all primary knees, however advocates of UKA estimate that between 25% and 47% of patients could be eligible.6,7 Inclusion criteria for UKA have been expanded, based on successful outcomes in young patients,8 obese patients,9 patients with patellofemoral disease,10 and those who are very active.11 These wider indications have not led to increased adoption of the procedure.
Robotic arm-assisted UKA surgery is primarily a haptic assistive robotic arm used for bone preparation. The cutting tool movements are restricted within a guided volume defined from a 3D surgical plan from a preoperative CT model of the patient. The device and surgical procedure aims to reduce variance of implant alignment and currently published evidence suggests that robotic arm-assisted surgery delivers more accurate implant positioning.12-16 Improvement in implant placement has been associated with reduced postoperative pain,17 improved function,17,18 and improved early survivorship19 compared with conventional surgery. Robotic arm-assisted surgery may also result in more consistent lower limb alignment and accurate soft tissue balancing which could translate to medium-term clinical difference.20
RCTs and large long-term registry data on all types of UKA techniques will, in time, establish the potential benefits from wider adoption of both UKA and robotic arm-assisted procedures. This RCT has previously reported improved accuracy of implantation,12 improved gait (one year),21 equivalent clinical outcome in all patients (two years),22 and potentially improved clinical outcomes in more active patients compared to a widely used UKA implant (at one- and two-year timepoints).23 These results are consistent with wider literature review of better short-term functional scores, patient satisfaction, and revision rate.24 Currently, no data from an RCT of robotic arm-assisted surgery for UKA has reached mid- or long-term data collection. The aim of this paper is to present the surgical and functional outcomes at five years of a RCT comparing robotic arm-assisted UKA with conventional manual surgery.
Methods
Trial design
This was a prospective, randomized, parallel, single-centre study comparing surgical alignment in patients undergoing UKA for the treatment of medial compartment OA (ISRCTN77119437). Participants underwent surgery using either robotic arm-assisted surgery or conventional manual instrumentation.
The primary outcome measure (surgical accuracy) has previously been reported,12 while secondary outcomes have been reported with one- and two-year follow-up.21-23 The five-year analysis of the secondary clinical outcome measures and follow-up are presented in this analysis.
A total of 139 patients were recruited at the investigative hospital (Glasgow Royal Infirmary, UK) between October 2010 and December 2012. All patients had been listed for a UKA to treat medial OA and were recruited by a research associate. Eligible patients were those deemed suitable for UKA surgery by one of three senior orthopaedic surgeons (MJGB, AM, BJ), could give informed consent, and were willing to attend the scheduled follow-up appointments. Exclusion criteria were ligament insufficiency, inflammatory arthritis, a deformity requiring augmentation, neurological movement disorders, pathology of the feet, ankles, hips, or opposite knee causing significant pain or gait alterations, and patients clearly requiring a TKA preoperatively. There were no changes to the methodology following the start of the trial.
Randomization and blinding
Randomization was performed using a customized online system S-Plus (TIBCO Software, USA) and patients were stratified by a surgeon (MJGB, AM, BJ). Both patients and those researchers recording patient-reported outcome measures (PROMs) had group allocation concealed.
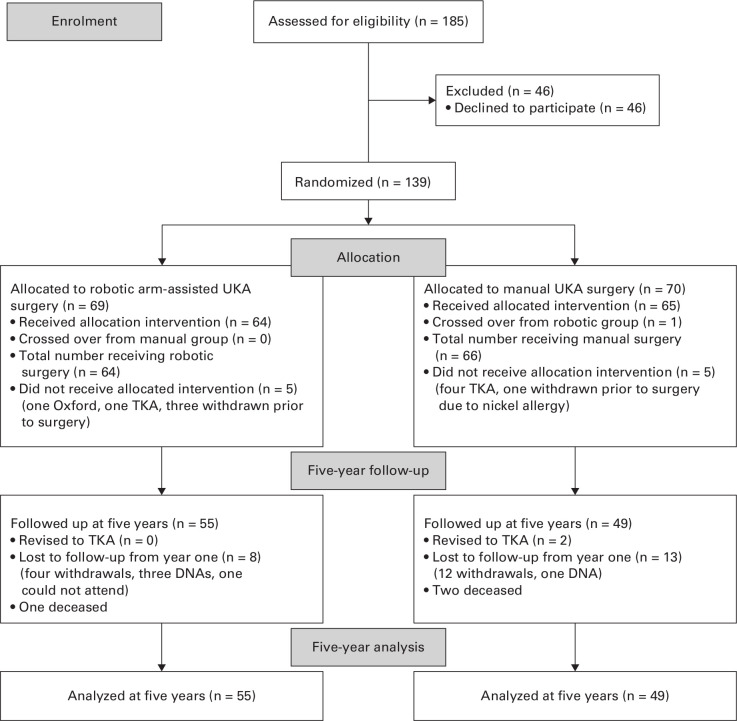
Consort diagram
The CONSORT diagram is presented in Figure 1. One- and two-year timepoints have been previously reviewed.22,23 By five years, 104 (80%) patients of the original 130 that received surgery were available (55 robotic, 49 manual). In the robotic group, three patients returned at the five-year appointment having not attended at two years, six patients did not attend the five-year appointment, and a further three patients missed both appointments. In the manual group, one patient returned at the five-year appointment having not attended at two years, another seven patients did not attend the five-year appointment, and a further ten patients missed both appointments. Two patients in the manual group were revised to TKA after receiving the allocated surgery; both were revised more than two years after primary surgery. By five years, no patients in the robotic arm-assisted group had received a revision. Participants were contacted with two letters and a phone call at each timepoint (preoperative to five years postoperative) with questionnaires being completed remotely where visits were not possible; complete data was recorded in 92 (74%) participants.
Fig. 1.
Consort diagram. DNA, did not attend; TKA, total knee arthroplasty; UKA, unicompartmental knee arthroplasty.
Treatment
Patients received either a Restoris MCK (MAKO Surgical, USA) using the MAKO Robotic-arm Interactive Orthopaedic (RIO) system (robotic arm-assisted group) or an Oxford phase 3 UKA (Zimmer Biomet, USA), implanted using standard manual phase 3 instrumentation (manual group). Surgery was performed and planned by one of the three senior surgical authors (AM, BJ, MJGB), all of whom are specialist knee surgeons with at least five years of experience in independent practice. Surgical planning was carried out by the operating surgeon in collaboration with the MAKO technician (MPS) for the robotic arm-assisted group and digital templating was used for the conventional group. Further details of surgical techniques have been previously reported.23
Follow-up and outcome measures
Data were collected at three months, and one, two, and five years postoperatively. All trial data was collected by independent research associate/research nurses at the Glasgow Royal Infirmary and were not informed of group allocation. Follow-up is ongoing and data will be collected at ten years.
Oxford Knee Score (OKS), American Knee Society Score (AKSS), Forgotten Joint Score (FJS), Pain Catastrophizing Scale, pain visual analogue scale (pain VAS), stiffness VAS, patient satisfaction, range of motion (ROM), University of California Los Angeles (UCLA) Activity Score, complications, and revision rates were all collected at these timepoints.
Sample size calculation
The primary outcome was powered to detect a 1° difference in tibial sagittal positioning with 80% power (α = 0.05), and reached the recruitment target at three months.12 The data in this paper at five-year follow-up represent exploratory analyses of the secondary outcome measures. To ensure retrospective power of any observed effects, a post hoc power calculation was performed (α = 0.05) for minimally important clinical differences (MICDs). AKSS and OKS were chosen for their extensive use in knee surgery. The OKS had sufficient power for this five-year analysis (89% to detect a difference of five points,25 but the AKSS was underpowered for the sample size at five years (51% to detect a difference of ten points).26 This suggests that insignificant results in OKS are still reliable observations as a secondary outcome and following loss to follow-up.
Statistical analysis
Data were assessed for normality with Shapiro-Wilk test. Normally distributed continuous variables were compared using independent-samples t-test. Continuous variables without a normal distribution were analyzed using the Mann-Whitney U test. Categorical variables were compared with chi-squared test. These analyses were performed using SPSS (IBM SPSS Statistics for Windows, Version 25.0; IBM, USA) and MatLab (MatLab and Statistics Toolbox Release 2018b; The MathWorks, USA). Statistical significance was set at p < 0.05 and following correction for multiple testing (n = 20) a more stringent p < 0.0025 is also reviewed.
Patients converted to TKA at the time of surgery or those undergoing revision did not continue in the trial, and were not included in the analysis. Therefore, an intention to treat analysis was not feasible and a per protocol analysis was conducted. Comparison of secondary outcome measures at five years were identical to those previously reported at the one- and two-year timepoints; however, additional longitudinal and survivorship analyses are presented in this five-year analysis.
Survivorship analysis
Proportions of patients with revision of the implant or surgical reintervention were analyzed using a Kaplan-Meier regression model with a log-rank statistic comparison between treatment groups. Revision was defined as explantation of the primary component excluding bearing exchange. All cause reintervention was expanded to include all surgical procedures carried out on the knee.
Longitudinal analysis
Longitudinal studies have the statistical advantage of repeated measures to predict variation, differences, heterogeneity between subjects and account for missing data when trying to determine a model of the data.27 To this extent, longitudinal analysis was also used to review mid-term period differences between the groups. Outcomes were analyzed using linear mixed model if normally distributed or otherwise generalized estimation equation regression models. Models were used to test for differences in the OKS, AKSS, FJS, VAS pain, and VAS stiffness between the treatment groups.
Subgroup analysis
A sub-group analysis was performed on the participants that were deemed to be more active preoperatively i.e. with a UCLA score ≥ 5. At one year and based on binary regression analysis, this analysis had previously shown that a UCLA Activity Score > 5 was predictive of a good clinical outcome.
Results
Review of outcomes
At five years, Table I displays no statistical differences between the treatment groups in any of the patient-reported or clinical outcomes, aside from the re-intervention rate. Compared to our previous studies, there was no difference in the subgroup analyses for more active patients and age at the time of surgery.
Table I.
A statistical comparisons of outcomes between the robotic arm-assisted surgery and manual surgery at five years.
| Variable | Robotic arm-assisted (n = 55) | Manual (n = 49) | p-value |
|---|---|---|---|
| Median American Knee Society Score (IQR) | |||
| Objective, 0 to 100 | 89 (80 to 97) | 88 (83.75 to 98) | 0.817* |
| Function, 0 to 100 | 80 (60 to 90) | 90 (70 to 90) | 0.636* |
| Total, 0 to 200 | 167 (139.75 to 185) | 177 (145 to 188.25) | 0.532* |
| Median Oxford Knee Score, 0 to 48 (IQR) | 40 (35 to 44) | 41 (34.75 to 44) | 0.812* |
| Mean pain VAS, 0 to 100 (SD) | 18.6 (22.6) | 15.9 (22.8) | 0.454* |
| Mean stiffness VAS, 0 to 100 (SD) | 19.1 (22.3) | 23.1 (26.4) | 0.443* |
| Median Forgotten Joint Score, 0 to 100 (IQR) | 50 (22.9 to 85.4) | 52.0 (28.1 to 72.9) | 0.784* |
| Median EQ-5D-3L, -0.594 to 1 (IQR) | 0.72 (0.587 to 1) | 0.8 (0.69 to 1) | 0.353* |
| Mean EQ-5D VAS, 0 to 100 (SD) | 80.3 (16.4) | 76.3 (18.2) | 0.316* |
| Median Pain Catastrophizing Scale, 0 to 10 (IQR) | 1 (0 to 10) | 0 (0 to 7.5) | 0.555* |
| Median ROM, ° (IQR) | 122.5 (115 to 130) | 120 (120 to 130) | 0.856* |
| Median five years to preoperative ROM change, ° (IQR) | 10 (3.75 to 20) | 5 (0 to 20) | 0.208* |
| Revisions, n | 0 | 2 | 0.476† |
| All cause reintervention, n | 0 | 6 | < 0.001† |
Mann-Whitney U test.
Kaplan-Meier regression log-rank statistic.
EQ-5D, EuroQol-five dimension; EQ-5D-3L, EuroQol-five dimension three-level; IQR, interquartile range; ROM, range of motion; SD, standard deviation; VAS, visual analogue scale.
Table II.
Satisfaction assessed using a four-point scale (very satisfied, satisfied, unsatisfied, or very dissatisfied) and statistically compared between surgical group at five years.
| Satisfaction scale | Robotic arm-assisted, n (%) | Oxford, n (%)‡ | p-value |
|---|---|---|---|
| Daily living | |||
| Very satisfied | 29 (52.7) | 19 (38.8) | 0.157* |
| Satisfied | 14 (25.4) | 18 (36.7) | 0.365* |
| Unsatisfied | 9 (16.4) | 10 (20.4) | 0.341* |
| Very unsatisfied | 3 (5.5) | 2 (4.1) | 0.741* |
| Recreational activities | |||
| Very satisfied | 18 (32.7) | 10 (20.4) | 0.160* |
| Satisfied | 20 (36.4) | 22 (44.9) | 0.380* |
| Unsatisfied | 14 (25.6) | 10 (20.4) | 0.532* |
| Very unsatisfied | 3 (5.5) | 7 (14.3) | 0.131* |
| 0.229† |
Proportional chi-squared test.
Chi-squared test for the table.
Oxford phase 3 unicompartmental knee arthroplasty (Zimmer Biomet, USA).
There were no differences in postoperative complications between the two groups, nor in the number of attendances to the hospital outpatient clinic. None of the robotic arm-assisted group required further surgery, with six (9%) of the manual group requiring a reintervention. Of the six patients, two were complete revisions to TKA (one for early tibial loosening at 2.5 years in a patient following a fall, and one for pain). Four underwent arthroscopic procedures; three for pain plus a possible lateral meniscal tear and one for possible infection when a biopsy was carried out. There were no alignment or component position errors identified in any of these six patients. Figure 2 presents the significant Kaplan-Meier estimate of reintervention between the groups.
Fig. 2.
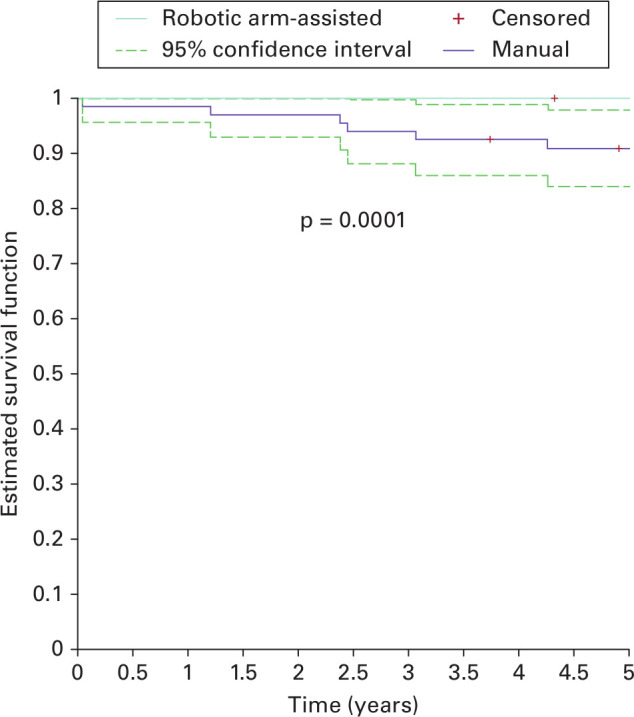
Kaplan-Meier estimate of survival robotic arm-assisted and manual groups.
Satisfaction was assessed using a four-point scale (very satisfied, satisfied, unsatisfied, or very dissatisfied). More patients reported being very satisfied in the robotic arm-assisted group, however no statistical difference for daily living (p = 0.476, chi-squared test) or recreational activities (p = 0.229, chi-squared test) was seen at five years.
Ceiling effects
Ceiling effects were observed in both the functional AKSS scores (24/103, 23%) and the OKS score (28/103, 27%) at five years. Subgroup analysis showed there were no statistical differences between the ceiling effects between the treatment groups at any timepoints.
Relative change over time
Review of all collected outcomes found no significant differences over all timepoints (Figure 3). Linear regression models allow for contribution of all data and predict for missing data. There was no evidence to suggest a significant main effect for any outcome score model (p > 0.500, longitudinal model). Both time since surgery and preoperative scores (OKS, AKSS) had significant effects (p < 0.001, longitudinal model) on the models, confirming they were sensitive to variation and that there was no overall difference between treatment groups over five years for any of the outcomes. Additionally, no difference between the treatment groups from surgery to five years were observed when area under the curve were used to analyze the data (data not shown).
Fig. 3.
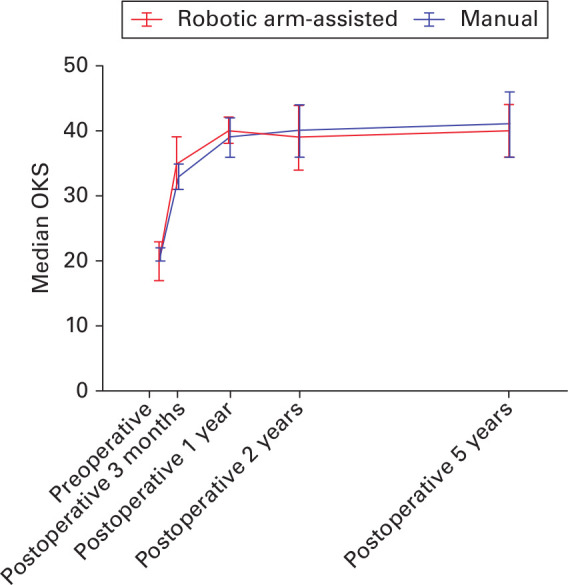
Actual median Oxford Knee Scores (OKS) at all timepoints.
Subgroup analysis
No differences were observed between active patients with a UCLA over ≥ 5 between the treatment groups in any of the outcome measures observed (Table II).
Discussion
To our knowledge, this paper presents the only mid-term clinical outcome of a prospective RCT comparison of robotic arm-assisted UKA with a conventional manual equivalent. The results show both interventions resulted in clinically significant increases from preoperative scores which were maintained to mid-term follow-up. The robotic arm-assisted surgery in UKA has been shown to result in better early postoperative pain and clinical outcomes for up to two years compared with manual UKA surgery (Figure 3).22,23 No difference was found at five years between the groups, including in patients with increased preoperative activity levels. This convergence of outcome between the groups is shown across all the secondary outcome measures used. This is the first study on robotic arm-assisted UKA to report higher reintervention rates in the manual approach group at a five-year follow-up.
The median OKS at five years was 40 for the robotic arm-assisted group and 41 for the manual group (Table I), with preoperative medians of 19.5 (interquartile range (IQR) 14.0 to 25.3) and 21.0 (IQR 15.5 to 24.0), respectively.23 Similarly, the median AKSS at five years was 167 for the robotic arm-assisted group and 177 for the manual, with preoperative medians of 105 and 102, respectively. The PROMs were slightly higher in the manual group, despite this the difference did reached neither statistical nor the MCID threshold. Both PROMs used present with a significant ceiling effect, involving over 25% of the patients (Table III). Large ceiling effects prevent any potential differences between the groups from being detected.28 Although the outcomes show significant improvements and a large proportion of excellent scores, there was no significant difference between the groups.
Table III.
Percentages of scores reaching the ceiling (top score).
| Score | Robotic arm-assisted, % | Manual, % | p-value* |
|---|---|---|---|
| OKS | |||
| Preoperative | 0.0 | 0.0 | N/A |
| Three months | 9.5 | 9.2 | 0.954 |
| Year one | 27.0 | 25.4 | 0.839 |
| Year two | 36.2 | 27.3 | 0.312 |
| Year five | 27.3 | 26.5 | 0.927 |
| AKSS Knee score | |||
| Preoperative | 0.0 | 0.0 | N/A |
| Three months | 0.0 | 0.0 | N/A |
| Year one | 1.6 | 0.0 | 0.325 |
| Year two | 1.8 | 1.9 | 0.969 |
| Year five | 0.0 | 0.0 | N/A |
| AKSS Function score | |||
| Preoperative | 1.6 | 0.0 | 0.310 |
| Three months | 15.9 | 10.8 | 0.397 |
| Year one | 31.7 | 23.8 | 0.322 |
| Year two | 25.9 | 23.6 | 0.786 |
| Year five | 23.6 | 22.4 | 0.887 |
| Total AKSS | |||
| Preoperative | 0.0 | 0.0 | N/A |
| Three months | 0.0 | 0.0 | N/A |
| Year one | 1.6 | 0.0 | 0.324 |
| Year two | 0.0 | 0.0 | N/A |
| Year five | 0.0 | 0.0 | N/A |
Percentages over 15% are considered significant. Subgroup statistical analysis between treatment groups showed no differences.
Proportional chi-squared test.
AKSS, American Knee Society Score; N/A, not applicable; OKS, Oxford Knee Score.
The increase in PROMs scores from two to five years in the manual group may have been due to those lost to follow-up or excluded from follow-up. A sub-analysis of those patients found their PROMs scores were poorer at the one-year timepoint than those who continued in the study.22
Findings at one and two years reported active patients had better outcomes in terms of AKSS and OKS with robotic surgery compared to manual surgery. By five years, a numerical difference remained, but significance had been lost (Table IV). This suggests that active patients in the short term and medium term benefit from robotic arm-assisted surgery, while a less active patient will have equivalent outcomes with either robotic or manual treatment option.
Table IV.
Analysis of outcomes based on preoperative University of California Los Angeles scores equal to and above five.
| Score | Robotic arm-assisted (n = 14) | Manual (n = 19) | p-value* |
|---|---|---|---|
| Median AKSS (IQR) | 186 (177 to 193) | 177 (160.5 to 184) | 0.195 |
| Median FJS (IQR) | 71.8 (39.6 to 91.7) | 62.5 (40.1 to 82.8) | 0.636 |
| Median OKS (IQR) | 43.5 (41 to 46) | 42 (36.75 to 45.5) | 0.314 |
| Mean Pain VAS (SD) | 12.6 (21.2) | 11.5 (15.3) | 0.854 |
| Mean Stiffness VAS (SD) | 13.5 (20.7) | 23.5 (20.3) | 0.133 |
Mann-Whitney U test.
AKSS, American Knee Society Score; FJS, Forgotten Joint Score; IQR, interquartile range; OKS, Oxford Knee Score; SD, standard deviation; VAS, visual analogue scale.
Reviewing patients lost to follow-up by surgical groups continued to show those lost by five years reported poorer scores up to the two-year timepoint. The re-intervention manual group was significantly lower at all-timepoints and across all outcome scores (AKSS, OKS, FJS, and VAS) than those that continued. To account for this missing data, linear models were applied to reduce the effects of bias.
A longitudinal review of the outcome data was warranted to determine differences between the groups over all timepoints. No differences were found in either the area under the curve or the linear modelling of the outcome data. This finding was similar to a comparison of TKA versus UKA study undertaken by Beard et al,6 and ultimately indicates good clinical outcomes could be expected from both UKA procedures used in this trial.
Excellent mid-term (five-year) survivorship is seen both in the robotic arm-assisted group (100%) and manually performed surgery (97%). The superior survivorship in the robotic arm-assisted group was not statistically significant. When survivorship was expanded to include all cause surgical reinterventions, there was a statistically significant difference, with a greater risk of a further surgical procedure in the manual group than the robotic assisted group.
The survivorship of both implants (mobile-bearing vs fixed-bearing) compares favourably with the UK National Joint Registry revision rates of 6.1% at five years for all types of UKA procedure.29 The Australian Orthopaedic Association National Joint Replacement Registry 2019 annual report is the only registry to report on revision rates specifically for robotic arm-assisted UKA surgery.30 Three-year revision rates are reported as 2.5% for the Stryker MAKO procedure, compared to 5.8% in the Oxford and 5.5% for all UKA. Our study reported a 0% revision rate for the MAKO and a 3% rate for the Oxford at five years, and is consistent with results of early survivorship for robotic arm-assisted UKA seen in other studies.19,31,32 The high-volume experience of the surgeons may explain the low revision rates in both groups.
All surgeries were carried out by high-volume UKA surgeons in a high-volume unit. All surgeons had less experience with the robotic arm-assisted technique due to the early adoption of the technology. It is not clear whether these results would apply to low-volume UKA surgeons, or those with more experience with the robotic arm-assisted technology.
Surgeon and hospital variables have been shown to contribute a ten-fold difference in revision risk among some UKA implants.33 This highlights the technical difficulty of the manual UKA approach, with only experienced high-volume surgeons and hospitals achieving optimal outcomes with UKA. The technical difficulty provided by UKA is the main justification for implementing robotic technology. It is not clear whether the low rates of revision seen with the Stryker MAKO technique reflect the high-volume expertise of the early adopters of the technology or if the difference is due to the technology itself. Long-term differences in revision rates may be established by this study at ten years.
It was not possible to blind clinicians who were responsible for decision-making on whether to revise or offer more surgery on either type of implant. This means it was impossible to eliminate bias in that decision-making process. We are unable to tell whether clinicians maintained equipoise over the outcomes of either type of surgery, and whether one type of implant was more likely to be revised or have any further intervention when they presented with problems postoperatively.
Similarly, retrospective assessment of patient blinding was not reviewed throughout the period of follow-up. Patients underwent surgery with spinal and sedation; however, patients undergoing robotic arm-assisted surgery underwent additional preoperative CT scans and additional incisions for the registration pins. These two additional steps may have resulted in the unblinding of observers and patients.
We reported that, due to revisions and dropouts, patients with poor outcomes in the conventional group were lost to follow-up. The lost to follow-up in both treatment groups led to a loss of information longitudinally and made intention to treat analysis unavailable. Bias from re-intervention participants was addressed in the application of longitudinal linear regression models between treatment groups which showed no difference.
Ceiling effect in 25% of patients represents the difficulty with using PROMs to determine differences between well performed procedures. More sensitive, standardized, and objective outcome measures are required for clinical trials using robotic surgery.
While the robotic systems have been shown to account for differences in variation of implant positioning, the difference in implant designs were as a result of a pragmatic study design. The manual (mobile-bearing) is an existing treatment option in the UK. Comparing the robotic arm-assistance (fixed-bearing) with this gold standard treatment should highlight any clinical differences expected as a result of a change in treatment options. It is important to acknowledge some fundamental differences in the procedures and there is limited high-quality evidence of survivorship differences between mobile and fixed-bearing.34,35 The design rationales ultimately lead to different failure mechanisms. The surgical planning of the robotic arm-assisted procedure was performed with a preoperative CT, while manual procedure was performed with digital templating.
This was a small, single centre study sufficiently powered to study postoperative alignment and OKS at five years. Larger multicentre studies, combined with registry data, in the future should provide sufficient data on large enough numbers of patients to allow robust sub-group analyses to determine which patients benefit most from the technology.
This study has shown a lower reintervention rate at five years for robotic arm-assisted UKA when compared with a manual approach. Excellent clinical outcomes were seen in both groups, with no statistical or clinical differences in outcomes was observed at five years.
Take home message
- Lower re-intervention rate at five years for robotic arm-assisted unicompartmental knee arthroplasty when compared with a manual approach.
- Excellent clinical outcomes were seen in both groups with no statistical or clinical differences in outcomes was observed at five years.
Author contributions
M. Banger: Designed the study, Collected and analyzed the data, Prepared and approved the manuscript.
J. Doonan: Analyzed the data, Prepared and approved the manuscript.
P. Rowe: Analyzed the data, Prepared and approved the manuscript.
B. Jones: Performed the operations, Collected and analyzed the data, Prepared and approved the manuscript.
A. MacLean: Performed the operations, Collected and analyzed the data, Prepared and approved the manuscript.
M. J. B. Blyth: Designed the study, Performed the operations, Collected and analyzed the data, Prepared and approved the manuscript.
Funding statement
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. This study was funded with an institutional support grant from the Mako Surgical Corporation (now Stryker), who had oversight of the trial, but no influence on data analysis nor the publication of the findings.
ICMJE COI statement
M. Banger, M. J. B. Blyth, J. Doonan, and B. Jones report a grant from MAKO Surgical and support for travel to meetings from Stryker, which are related to this article; M. J. B. Blyth also declares payment for lecturing at educational meetings by MAKO, which is unrelated. A. Maclean reports a grant and support for travel to meetings from NHS Greater Glasgow and Clyde, which are related to this. P. Rowe declares a grant from MAKO, which is related, and payment for lectures from MAKO, which is unrelated.
Acknowledgements
We would like to thank Sister Pauline May (Research Nurse), Sister Rachael Halifax (Research Nurse), Miss Sinead O’Donnell, Dr Arman Motesharei, Dr Julie McWee née Smith (Research Associate), and Miss Iona Donnelly for their support of this study.
Ethical review statement
The study complied with the principles of the Declaration of Helsinki and was approved by the local ethics committee of the West of Scotland Research Ethics Service (10/S0704/12). The study was registered with the International Standard Randomized Controlled Trial Number Registry (ISRCTN77119437).
Open access statement
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.
This article was primary edited by P. Walmsley.
References
- 1.Liddle AD, Judge A, Pandit H, Murray DW. Adverse outcomes after total and unicompartmental knee replacement in 101 330 matched patients: a study of data from the National Joint Registry for England and Wales. The Lancet. 2014;384(9952):1437–1445. [DOI] [PubMed] [Google Scholar]
- 2.Chawla H, van der List JP, Christ AB, Sobrero MR, Zuiderbaan HA, Pearle AD. Annual revision rates of partial versus total knee arthroplasty: a comparative meta-analysis. Knee. 2017;24(2):179–190. [DOI] [PubMed] [Google Scholar]
- 3.Migliorini F, Tingart M, Niewiera M, Rath B, Eschweiler J. Unicompartmental versus total knee arthroplasty for knee osteoarthritis. Eur J Orthop Surg Traumatol. 2019;29(4):947–955. [DOI] [PubMed] [Google Scholar]
- 4.NJR . NJR 16th annual report 2019. 2019. https://www.njrcentre.org.uk (date last accessed 13 April 2021).
- 5.Vasso M, Antoniadis A, Helmy N. Update on unicompartmental knee arthroplasty. EFORT Open Rev. 2018;3(8):442–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beard DJ, Davies LJ, Cook JA, et al. The clinical and cost-effectiveness of total versus partial knee replacement in patients with medial compartment osteoarthritis (TOPKAT): five-year outcomes of a randomised controlled trial. Lancet. 2019;394(10200):746–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilson HA, Middleton R, Abram SGF, Smith S, Alvand A, Jackson WF. Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ. 2019;364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greco NJ, Lombardi AV, Price AJ, Berend ME, Berend KR. Medial mobile-bearing unicompartmental knee arthroplasty in young patients aged less than or equal to 50 years. J Arthroplasty. 2018;33(8):2435–2439. [DOI] [PubMed] [Google Scholar]
- 9.Lum ZC, Crawford DA, Lombardi AV, et al. Early comparative outcomes of unicompartmental and total knee arthroplasty in severely obese patients. Knee. 2018;25(1):161–166. [DOI] [PubMed] [Google Scholar]
- 10.Berend KR, Lombardi AV, Morris MJ, Hurst JM, Kavolus JJ. Does preoperative patellofemoral joint state affect medial unicompartmental arthroplasty survival? Orthopedics. 2011;34(9):e494–496. [DOI] [PubMed] [Google Scholar]
- 11.Crawford DA, Adams JB, Lombardi AV, Berend KR. Activity level does not affect survivorship of Unicondylar knee arthroplasty at 5-year minimum follow-up. J Arthroplasty. 2019;34(7):1364–1368. [DOI] [PubMed] [Google Scholar]
- 12.Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M. Improved accuracy of component positioning with robotic-assisted Unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am. 2016;98(8):627–635. [DOI] [PubMed] [Google Scholar]
- 13.Cobb J, Henckel J, Gomes P, et al. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br. 2006;88-B(2):188–197. [DOI] [PubMed] [Google Scholar]
- 14.Dunbar NJ, Roche MW, Park BH, Branch SH, Conditt MA, Banks SA. Accuracy of dynamic tactile-guided unicompartmental knee arthroplasty. J Arthroplasty. 2012;27(5):803–808. [DOI] [PubMed] [Google Scholar]
- 15.Mofidi A, Plate JF, Lu B, et al. Assessment of accuracy of robotically assisted unicompartmental arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1918–1925. [DOI] [PubMed] [Google Scholar]
- 16.Kayani B, Konan S, Pietrzak JRT, Huq SS, Tahmassebi J, Haddad FS. The learning curve associated with robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J. 2018;100-B(8):1033–1042. [DOI] [PubMed] [Google Scholar]
- 17.Kayani B, Konan S, Tahmassebi J, Rowan FE, Haddad FS. An assessment of early functional rehabilitation and hospital discharge in conventional versus robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J. 2019;101-B(1):24–33. [DOI] [PubMed] [Google Scholar]
- 18.Clement ND, Bell A, Simpson P, Macpherson G, Patton JT, Hamilton DF. Robotic-assisted unicompartmental knee arthroplasty has a greater early functional outcome when compared to manual total knee arthroplasty for isolated medial compartment arthritis. Bone Joint Res. 2020;9(1):15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pearle AD, van der List JP, Lee L, Coon TM, Borus TA, Roche MW. Survivorship and patient satisfaction of robotic-assisted medial unicompartmental knee arthroplasty at a minimum two-year follow-up. Knee. 2017;24(2):419–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robinson PG, Clement ND, Hamilton D, Blyth MJG, Haddad FS, Patton JT. A systematic review of robotic-assisted unicompartmental knee arthroplasty. Bone Joint J. 2019;101-B(7):838–847. [DOI] [PubMed] [Google Scholar]
- 21.Motesharei A, Rowe P, Blyth M, Jones B, Maclean A. A comparison of gait one year post operation in an RCT of robotic UKA versus traditional Oxford UKA. Gait Posture. 2018;62(8):41–45. [DOI] [PubMed] [Google Scholar]
- 22.Gilmour A, MacLean AD, Rowe PJ, et al. Robotic-arm-assisted vs conventional unicompartmental knee arthroplasty: the two-year clinical outcomes of a randomized controlled trial. J Arthroplasty. 2018;33(7S):S109–S115. [DOI] [PubMed] [Google Scholar]
- 23.Blyth MJG, Anthony I, Rowe P, Banger MS, MacLean A, Jones B. Robotic arm-assisted versus conventional unicompartmental knee arthroplasty: Exploratory secondary analysis of a randomised controlled trial. Bone Joint Res. 2017;6(11):631–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin J, Yan S, Ye Z, Zhao X. A systematic review of MAKO-assisted unicompartmental knee arthroplasty. Int J Med Robot. 2020;16(5):e2124:1–7. [DOI] [PubMed] [Google Scholar]
- 25.Beard DJ, Harris K, Dawson J, et al. Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol. 2015;68(1):73–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee WC, Kwan YH, Chong HC, Yeo SJ. The minimal clinically important difference for knee Society clinical rating system after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3354–3359. [DOI] [PubMed] [Google Scholar]
- 27.Diggle P, Liang K-Y, Zeger SL. Analysis of longitudinal data. Oxford : New York: Clarendon Press, 1994. [Google Scholar]
- 28.Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. [DOI] [PubMed] [Google Scholar]
- 29.NJR . NJR 15th annual report. 2018. https://www.njrcentre.org.uk/ (date last accessed 13 April 2021).
- 30.AOANJRR . The AOANJRR is funded by the Australian government department of health. 2019. https://aoanjrr.sahmri.com (date last accessed 13 April 2021).
- 31.St Mart J-P, de Steiger RN, Cuthbert A, Donnelly W. The three-year survivorship of robotically assisted versus non-robotically assisted unicompartmental knee arthroplasty. Bone Joint J. 2020;102-B(3):319–328. [DOI] [PubMed] [Google Scholar]
- 32.Zambianchi F, Franceschi G, Rivi E, et al. Clinical results and short-term survivorship of robotic-arm-assisted medial and lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2020;28(5):1551–1559. [DOI] [PubMed] [Google Scholar]
- 33.Bini S, Khatod M, Cafri G, Chen Y, Paxton EW, Surgeon PEW. Surgeon, implant, and patient variables may explain variability in early revision rates reported for unicompartmental arthroplasty. J Bone Joint Surg Am. 2013;95(24):2195–2202. [DOI] [PubMed] [Google Scholar]
- 34.Parratte S, Pauly V, Aubaniac J-M, Argenson J-NA. No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin Orthop Relat Res. 2012;470(1):61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peersman G, Stuyts B, Vandenlangenbergh T, Cartier P, Fennema P. Fixed- versus mobile-bearing UKA: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3296–3305. [DOI] [PubMed] [Google Scholar]